Contents
Ischial bursitis
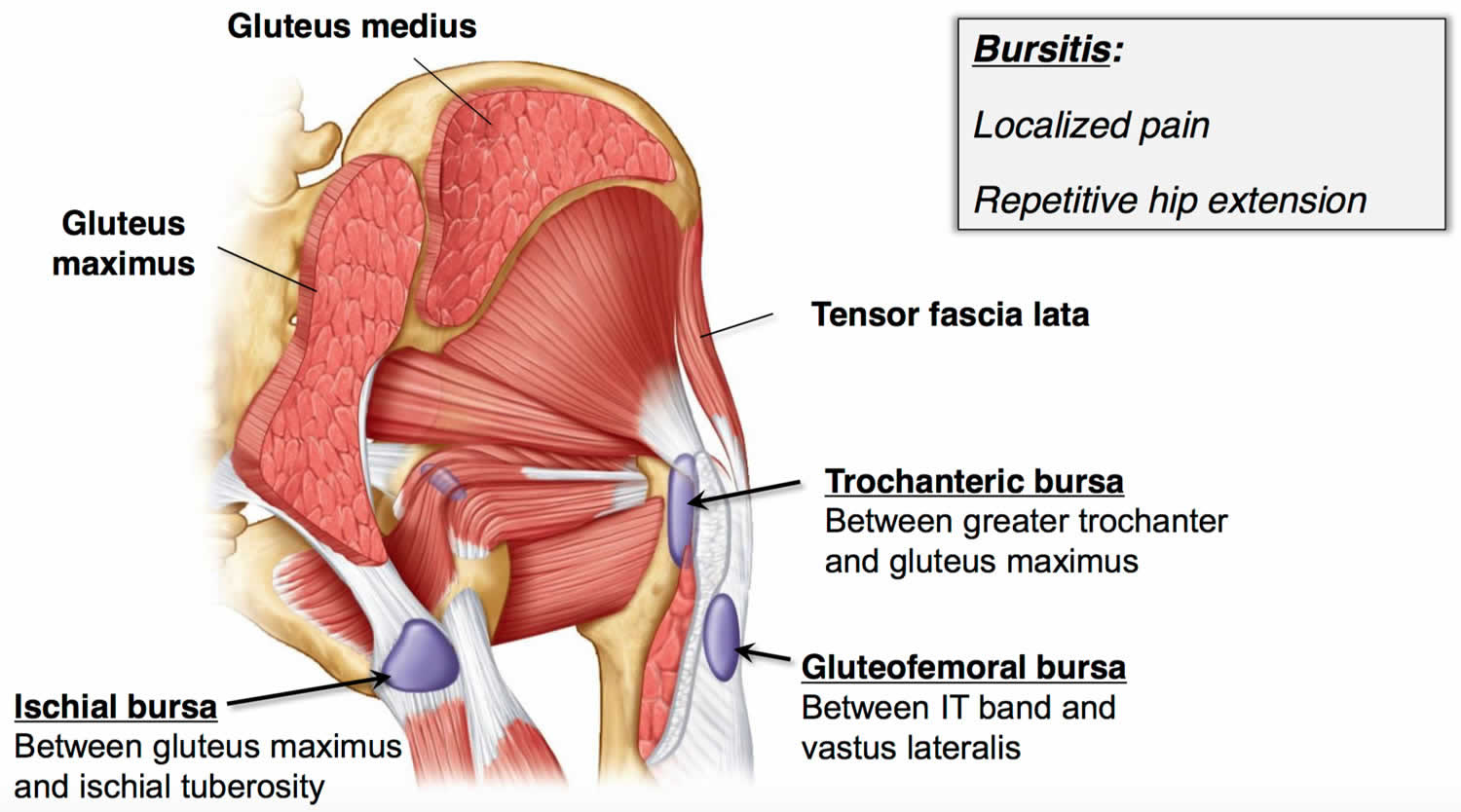
Ischial bursitis also known as “ischiogluteal bursitis” or “weaver’s bottom,” is a rare condition where the bursa that lies between the ischial tuberosity and the gluteus maximus muscle becomes inflamed 1, 2. Bursitis is the swelling and irritation of a bursa. A bursa is a small fluid-filled sac that acts as a cushion between muscles, tendons, and bones 3. Bursa is located throughout the body, including around the shoulder, elbow, hip, knee, and heel. Ischial bursa is present physiologically in order to reduce the amount of frictional force generated between the gluteal muscle and the ischial tuberosity that otherwise might become damaged or irritated by this contact 4. Ischial bursitis is most commonly caused by prolonged pressure on the ischium, as occurs in prolonged sitting or from the repeated movement of the gluteus maximus muscle in such activities as bicycling or running 5, 6. Ischial bursitis or ischiogluteal bursitis has been known to be common in people whose occupations are related with frequent irritation to the bursa, and this irritation can occur during long periods of time spent in the sitting position 7. When vibration is involved in working, such as with heavy powered sewing machine (weavers), tractor-driving or road equipment machines, the ischiogluteal bursa can become inflamed 8, 9. Furthermore, as the ischial tuberosity bears the weight of the body in the supine position (laying on your back), these pressure points may lead to ischial bursitis in debilitated persons, and particularly for those patients with malignancies or paraplegia 10, 11. Ischial bursitis can also be affected by an acute or chronic shearing force on the ischial tuberosity caused by falling on your backsides (buttocks) in athletes, resulting in chronic and sometimes disabling discomfort that can prevent athletes from participating in their sporting activities 12. There are many sports that involve sitting such as canoeing, horseback riding, wheel-chair racing for paraplegic patients and so on 7. These activities cause an inflammatory reaction that results in swelling and tenderness over the lower buttock and upper posterior thigh. Many other differential diagnoses have common presentations such as sciatica, lumbar disc degeneration, piriformis syndrome, sacroiliitis, hip bursitis and tendonitis of hamstring muscles 13, 14, 15.
Ischial bursitis symptoms may include mass-like sensation along the buttock, or as buttock pain radiating down the lower leg 16. Patients with ischiogluteal bursitis often complain of mild-to-moderate pain in the buttocks with occasional pain radiating down the gluteal/thigh area, often worsening with prolonged sitting or exercise. Forward bending of the hip joint or standing on the tiptoes can exacerbate pain 17. Physical examinations showed the tenderness of ischial tuberosity area in 59 (92.2%) patients, but no specific findings were confirmed in 5 patients (7.8%) 18. As the ischiogluteal bursa lies in a close contact with the sciatic and posterior femoral cutaneous nerves, ischial bursitis can mimic the symptoms of radiculopathy 18, 19. Enlargement of ischiogluteal bursa could clinically mimic a soft tissue neoplasm 20, 21, 22.
The ischiogluteal bursa is an adventitial bursa located between the ischial tuberosity and the gluteus maximus muscle, smoothing movement by reducing friction between the two 8, 23. An adventitial bursa is a non-native structure which develops later in life through a process of myxoid degeneration of fibrous tissue secondary to abnormal stress and friction between adjacent structures 22. Adventitial bursa does not have lining cells 22. Ischial bursa is synovial, meaning it is composed of a fatty connective tissue capsule filled with synovial fluid 8, 24. When infection or irritation occurs, cells of the synovia proliferate, resulting in increased production of synovial fluid. Inflammatory mediators such as cyclooxygenase, cytokines, and metalloproteases mediate this process. The result is a thick fluid-filled cavity with high amounts of fibrin, resulting in the formation of granulation tissue 25. Over time, this tissue will gradually interfere with the normal motion and activity of the surrounding tissues whether they are muscle, bone, or tendon.
Ischial bursitis is a relatively uncommon clinical condition nowadays, and it is often overlooked as a cause of buttock pain 15, 9. Ischial bursitis is often diagnosed after exclusion of other causes of pain at the buttock 26, 18. In addition, the symptoms of ischial bursitis are varied and often non-specific, making it difficult to diagnose and confused with many other diseases 18. Moreover, it is difficult to predict cases of chronic progression or poor treatment response.
Although there are no specific radiographic findings that are diagnostic of ischiogluteal bursitis, the most common findings in a long-standing ischiogluteal bursitis would be irregularity of the cortex of the ipsilateral ischial tuberosity, or any calcification projecting over or near the tuberosity 15, 27. Prior imaging should be reviewed to identify other potential causes of pain in this region such as referred pain, calcium hydroxyapatite deposition, or other masses including myxoid tumor, schwannoma, or neurofibroma 6. Although the diagnosis is often unrecognized, it may be seen in patients of all ages. Bursitis as whole accounts for less than one percent of total primary care visits. Ischial bursitis is most common in persons with sedentary careers with constant irritation of the ischial bursa due to prolonged periods of time sitting on hard surfaces which gives this condition it’s colloquial name “weaver’s bottom.” Weaving as a profession has been around since approximately 6000 BCE, and people have been suffering from this condition for as many years 28.
Most previous studies reported on conservative treatment of ischiogluteal bursitis, including administration of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, aspiration, and bursal injection of steroids or local analgesics 18, 2. Among these treatments, lifestyle modification and avoidance of triggering activities was found to be the most fundamental treatment 27. It is important to educate the patient on lifestyle changes including weight loss and regular exercise. Recurrences are common in patients who lead a sedentary lifestyle 29.
Cold compresses may help in the short term to minimize pain from swelling. In most cases, a satisfactory response is obtained from conservative treatment, with the expectation of a favorable prognosis thereafter; however, improvement of symptoms is slow in some cases, showing chronic progression 18. If the pain is unbearable or unrelenting, an intrabursal corticosteroid injection with lidocaine may be administered 30, 31, 32. The lidocaine will help by providing immediate relief from the pain by blocking the sodium channels in the surrounding tissue, inhibiting the transmission of the pain signal 33.
Surgical treatment should be considered in cases of refractory ischiogluteal bursitis, and in this study, encouraging results were obtained after performance of surgical excision in all cases 34.
Figure 1. Ischial bursitis
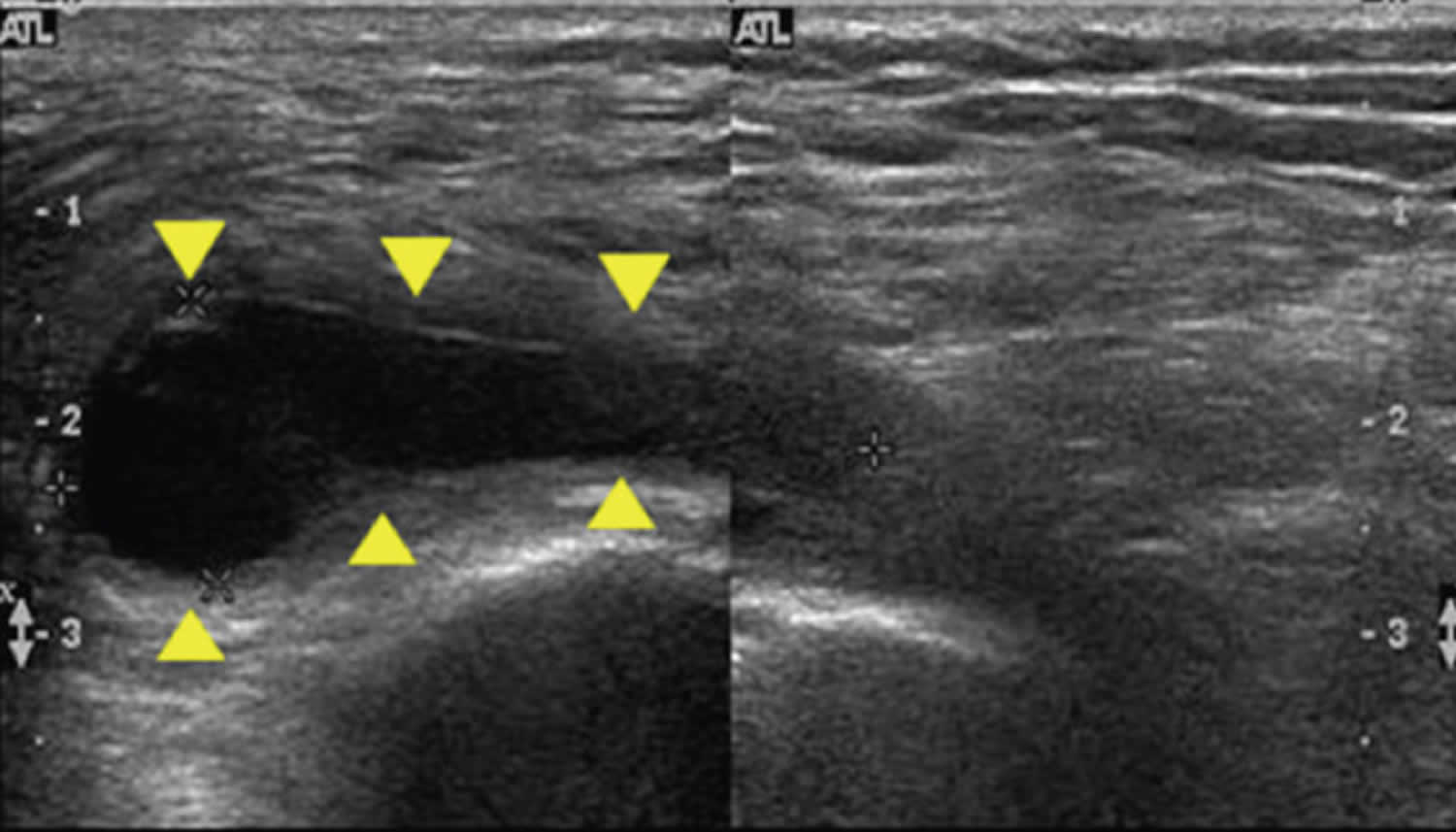
Figure 2. Ischial bursitis ultrasound
Footnote: Ischiogluteal bursitis ultra-sonography in a 76-year female shows hypoechoic lesion (yellow arrows) with acoustic enhancement.
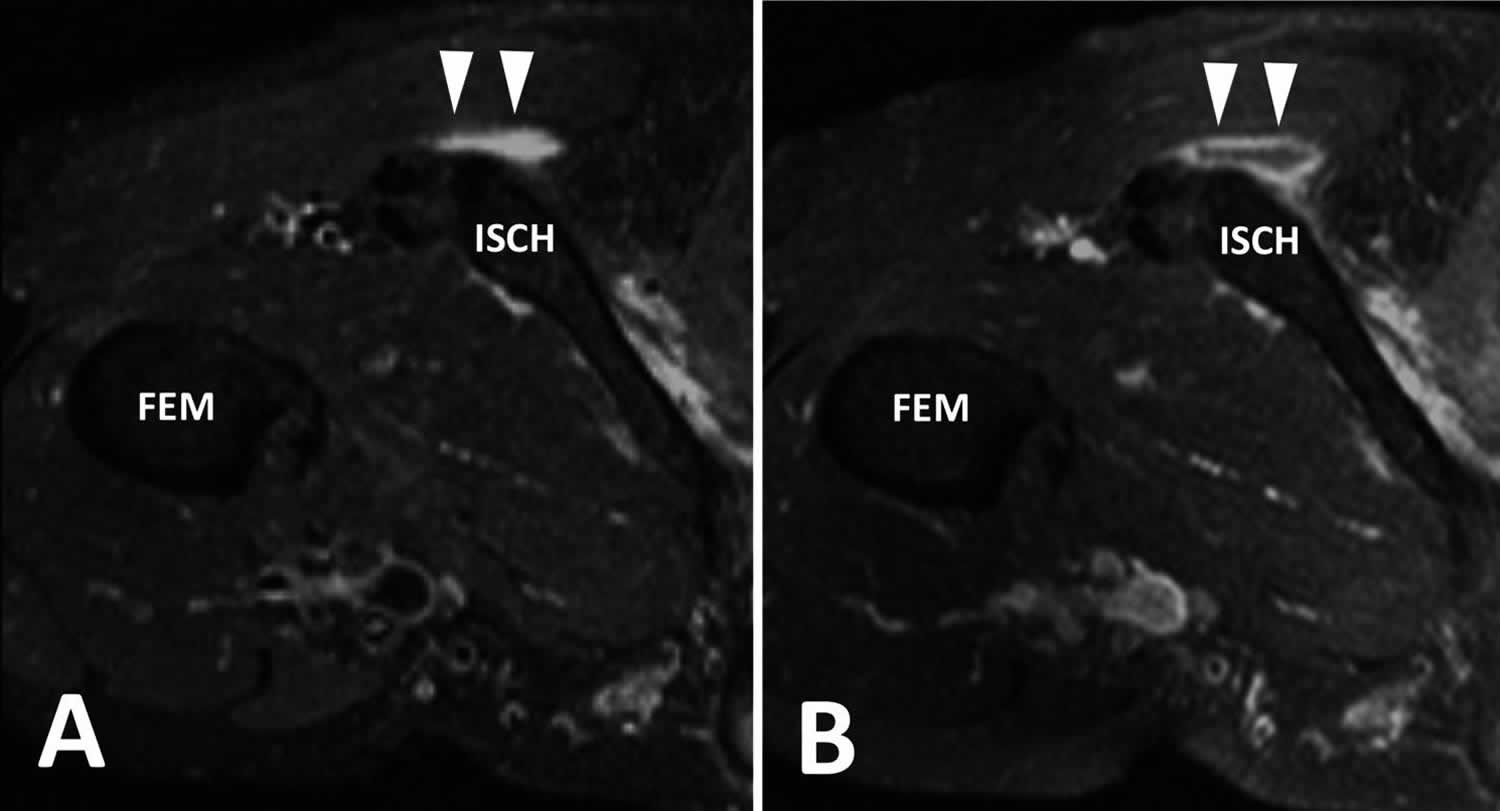
[Source 18 ]Figure 3. Ischial bursitis MRI
Footnote: Ischial bursitis MRI findings. (A) Rotated axial T2 fat-saturated and (B) T1 fat-saturated post contrast MRI images demonstrate a rim enhancing fluid collection adjacent to the ischial tuberosity within the ischial bursa.
[Source 26 ]Ischial bursitis causes
The origin of ischial bursitis can be seen in the original name of the condition, “weaver’s bottom” 35. Ischial bursitis was first seen in workers that sat for long periods of time on hard surfaces. Another colloquial name for this condition is “tailor’s bottom.” Ischial bursitis may occur in various conditions, much like many other bursal inflammations. Although chronic microtrauma from chronic repetitive friction on the tissue overlying the bursa around the ischial tuberosity, the cause of ischial bursitis remains unclear 36, 37, 38. Roh et al. 18 reported that inflammatory disease is an independent risk factor for refractory ischiogluteal bursitis. Involvement of autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and scleroderma among others, are also likely to cause ischiogluteal bursitis; however, few studies have been reported thus far 39.
Ischial bursitis may also be caused by uremia seen in conditions such as gout and chronic kidney disease 18. Ischial bursa is a deep bursa, meaning it is less susceptible to the contiguous spread of infectious organisms. Although rare, infectious etiologies of ischial bursitis include septicemia and septic arthritis 40. Direct inoculation of the bursa by bacteria would be very rare due to its location in the body 35.
Ischial bursitis symptoms
Patients with ischial bursitis will present with gluteal pain and/or upper posterior thigh pain following prolonged sitting or exercise 2. The patient will most commonly complain of a low grade, pinpoint, aching pain that is worsened by sitting down or stretching the gluteus maximus muscle 41. Patients may complain of problems sleeping because of the pain. Patients also may have reduced mobility and swelling associated with this condition. On physical exam, tenderness over the buttock may be noted. Patients may have pain with passive flexion at the hip joint 2. The patient also may have an inability to extend the hip 41. The patient may feel pain with stretching 42. A soft tissue mass, which tends to be well-defined, non-mobile, and slightly tender, may be present in the gluteal region of the affected hip 43. When redness (erythema) overlying the gluteal regions is a major clinical presentation, infectious causes such as cellulitis or septic joint should be suspected 18. In a study by Roh et al 18, tenderness on ischial tuberosity was positive in 59 patients (92.2%) during a physical examination, while no specific findings were confirmed in the 5 patients (7.8%). Therefore, even if there is no tenderness of ischial tuberosity in physical examination, ischial bursitis should not be completely excluded 18.
Ischial bursitis complications
Ischial bursitis can result in problems with 2:
- Walking
- Running
- Sitting
- Stretching
Subsequent avoidance of activity and exercise may lead to overall poor conditioning and negatively affect other conditions that respond well to or are prevented at some level by exercise and activity.
Ischial bursitis diagnosis
Most ischial bursitis cases can be diagnosed and treated clinically without the need for further testing 2. Most cases of ischial bursitis are self-limiting and will resolve with time. Blood work should only be ordered if an infection or autoimmune condition is suspected. In the case of bursitis, lab values will most likely be within normal range. If other conditions are suspected, such as septic joint, a joint aspiration is indicated, and antibiotic treatment should be initiated.
Radiological evaluation is helpful when the clinical diagnosis is obscured for patients having buttock pain and/or a mass 7. When imaging is indicated for the diagnosis, MRI and/or ultrasound is the first choice of modality 7. There are at least two advantages for using MRI in this situation. The first is that MRI is sensitive for bursitis and MRI provides a global view for finding causative lesions of buttock pain or a mass in the pelvis, hip, and soft tissue, or for excluding the possibility of spinal diseases 7. The second is that the T2-weighted MRI images clearly identify and localize the inflamed bursa according to the characteristic MRI findings of bursitis at the expected location 12. However, MRI is expensive and unnecessary most of the time when diagnosing and treating ischial bursitis. MRI is only indicated if there are other possible differentials such as tumors. Ultrasound, similarly, is unnecessary unless aspiration is indicated, then it is useful to guide the procedure ensuring aspiration is performed in the appropriate place 44.
It is important to differentiate ischiogluteal bursitis from peri-rectal or buttock abscess, hematoma, epidermoid cyst, dermoid cyst or hydatid cyst when the lesion shows a cystic appearance 7. The typical location of ischiogluteal bursitis might be a very important diagnostic criterion for separating bursitis from the other cystic masses 7. The common hamstring tendon is typically located lateral to the inflamed ischiogluteal bursa, and it possibly acts as a barrier to prevent the extension of the bursitis 7. Instead, the enlarged bursa usually spreads inferomedially to the ischiorectal fossa 7.
Ischial bursitis or ischiogluteal bursitis, when it occurs in cancer patients, it may clinically mimic a soft-tissue or bone metastasis from the primary malignancy 10, 45. Whenever the possibility of tumor is in the differential diagnosis, biopsy or surgical intervention should be performed for confirmation 7. In addition, an enlarged bursa should be aspirated to exclude an infectious process whenever this is suspected 7.
Tuberculosis, gout, rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis and Reiter’s syndrome have also been reported to involve the ischiogluteal bursa 7, 46, 47, 48, 49, 45, 9, 50.
Ischial bursitis treatment
Initially, the common nature of ischial bursitis should indicate minor, low-cost interventions such as nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen and rest 2. If ischial bursitis persists, therapeutic mixed steroid and anesthetic injections may be considered 2. Only if the condition continues to be resistant or other causes are indicated by the workup for this patient presentation should more invasive and/or expensive test be used.
Treatment of ischial bursitis is relatively symptom driven 2. Primary treatment is lifestyle modification by stopping the activity that caused bursitis in the first place, whether it was a physical activity or sitting for long periods of time on hard surfaces. Nonsteroidal anti-inflammatory drugs such as naproxen work well to decrease inflammation, and a regiment of daily intake for two weeks may be followed to prevent further inflammation. Naproxen also may help reduce pain associated with this condition. Cold compresses may help in the short term to minimize pain from swelling.
The rate of recovery is highly depending on the severity of patient symptoms and modality of treatment chosen. Recurrence is likely without lifestyle change 35.
Ischial bursitis injection
If the pain is unbearable or unrelenting, an intrabursal corticosteroid injection with lidocaine may be administered (Table 1) 2. The lidocaine will help by providing immediate relief from the pain by blocking the sodium channels in the surrounding tissue, inhibiting the transmission of the pain signal 2. The corticosteroid will provide prolonged anti-inflammatory protection by inhibiting the inflammatory mediators. Patients will most likely be symptom-free within days to weeks without treatment 51.
While injectable steroids are frequently used to treat pain, there is no consensus regarding the superiority of a specific agent, for bursal injections 26. Commonly used steroids, however, do contain slightly different properties. For example, particulate steroids such as methylprednisone, triamcinolone and betamethasone have lower solubility and therefore, theoretically last longer at the injection site compared to non-particulates such as dexamethasone 26.
Injection of the ischial bursa is typically performed with the patient in the prone position 26. The ultrasound probe is then used to identify the hamstring muscles which are followed superiorly to the ischial tuberosity while noting the location of the sciatic nerve 26. The transducer is placed in the transverse plane over the most lateral aspect of the ischial tuberosity, and the needle is directed towards the space between the ischial tuberosity and gluteus maximus. Once the needle is at the peri-bursal fat, a mixture of 40 mg of triamcinolone or methylprednisolone and 4 mL of lidocaine is then injected into the bursa 26. Although steps are taken to avoid major neurovascular structures, it is still possible for some of the injectate to reach the sciatic nerve. Therefore, the use of shorter acting anesthetics is preferred, and patients are instructed to avoid operating a vehicle immediately following the appointment 26.
Side effects are usually mild and may include facial flushing, skin reaction/hypopigmentation, soft tissue atrophy, steroid flare, transient increase in blood sugar 52, 53, adverse psychiatric effects 54, 55 and allergic reaction ranging from mild to anaphylaxis. Allergy to injectable steroids is rare and may be related to a medication additive rather than the steroid itself 56. For extra-articular steroid injections, major adverse events have been reported as occurring 0–5.8% with minor adverse events ranging from 0 to 81% 57. Pain following injection is the most common minor adverse event 57, described as a transient issue, not requiring intervention. Infection is an extremely rare complication, with an incidence rate of 0.0046% 58.
Table 1. Commonly used injectable steroids and local anesthetics
| Steroids | Anesthetics |
|---|---|
| Methylprednisolone acetate (40 mg/mL or 80 mg/mL) | Lidocaine (1%) |
| Triamcinolone acetonide (40 mg/mL) | Bupivacaine (0.25%) |
| Betamethasone acetate (6 mg/mL) | Ropivacaine (0.5%) |
| Dexamethasone sodium phosphate (4 mg/mL) |
Surgical treatment
Surgical treatment is recommended in patients with persistent or repeated superficial bursitis and significant enlargement of bursa causing functional disability 18. Surgical treatment includes open or endoscopic bursectomy and partial excision of the underlying bony tissue 18.
Ischial bursitis prognosis
Unless the underlying inflammatory diseases that cause of ischial bursitis is accurately identified and addressed, ischial bursitis will usually not spontaneously recover 2. The pain may abate with a period of lay-off or treatment, but reinitiating activity will still lead to excessive friction on the ischio-gluteal bursa, causing inflammation and the recurrence of pain 2. Patients with underlying inflammatory diseases, such as rheumatoid arthritis, gout, and skin infection, showed less responsiveness to conservative management, and two of the patients in this study required open surgical intervention due to failure of medical treatment 18, 59.
- Van Mieghem, I.M., Boets, A., Sciot, R. et al. Ischiogluteal bursitis: an uncommon type of bursitis. Skeletal Radiol 33, 413–416 (2004). https://doi.org/10.1007/s00256-004-0789-3[↩]
- Johnson DB, Varacallo M. Ischial Bursitis. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482285[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Hudson K, Delasobera BE. Bursae. In: Birrer RB, O’Connor FG, Kane SF, eds. Musculoskeletal and Sports Medicine For The Primary Care Practitioner 4th ed Boca Raton, Fla: CRC Press, Taylor & Francis Group; 2016:111–116.[↩]
- Johnson DB, Varacallo M. Ischial Bursitis. [Updated 2019 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482285[↩]
- Hitora T, Kawaguchi Y, Mori M, Imaizumi Y, Akisue T, Sasaki K, et al. Ischiogluteal bursitis: a report of three cases with MR findings. Rheumatol Int. 2009;29(4):455–458. doi: 10.1007/s00296-008-0680-y[↩]
- Van Mieghem IM, Boets A, Sciot R, Van Breuseghem I. Ischiogluteal bursitis: an uncommon type of bursitis. Skeletat Radiol. 2004;33(7):413–416. doi: 10.1007/s00256-004-0789-3[↩][↩]
- Cho KH, Lee SM, Lee YH, Suh KJ, Kim SM, Shin MJ, Jang HW. Non-infectious ischiogluteal bursitis: MRI findings. Korean J Radiol. 2004 Oct-Dec;5(4):280-6. doi: 10.3348/kjr.2004.5.4.280[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Larsson LG, Baum J. The syndromes of bursitis. Bull Rheum Dis. 1986;36(1):1-8.[↩][↩][↩]
- Swartout R, Compere EL. Ischiogluteal Bursitis: The Pain in the Arse. JAMA. 1974;227(5):551–552. doi:10.1001/jama.1974.03230180049013[↩][↩][↩]
- Mills GM, Baethge BA. Ischiogluteal bursitis in cancer patients: an infrequently recognized cause of pain. Am J Clin Oncol. 1993 Jun;16(3):229-31. doi: 10.1097/00000421-199306000-00007[↩][↩]
- Rubayi S, Montgomerie JZ. Septic ischial bursitis in patients with spinal cord injury. Paraplegia. 1992 Mar;30(3):200-3. doi: 10.1038/sc.1992.55.[↩]
- Berquist TH. In: Imaging of sports injuries. Berquist TH, editor. Gaithersburg, Maryland: Aspen Publishers; 1992. pp. 93–94.[↩][↩]
- Kubota K, Yamashita H, Mimori A. Clinical Value of FDG-PET/CT for the Evaluation of Rheumatic Diseases: Rheumatoid Arthritis, Polymyalgia Rheumatica, and Relapsing Polychondritis. Semin Nucl Med. 2017 Jul;47(4):408-424[↩]
- Butcher JD, Salzman KL, Lillegard WA. Lower extremity bursitis. Am Fam Physician. 1996 May 15;53(7):2317-24. Erratum in: Am Fam Physician 1996 Aug;54(2):468.[↩]
- Chafetz N, Genant HK, Hoaglund FT. Ischiogluteal tuberculous bursitis with progressive bony destruction. J Can Assoc Radiol. 1982 Jun;33(2):119-20.[↩][↩][↩]
- Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35(11):991–1014. doi: 10.2165/00007256-200535110-00005[↩]
- Mills GM, Baethge BA. Ischiogluteal bursitis in cancer patients: an infrequently recognized cause of pain. Am J Clin Oncol. 1993;16:229–231. doi: 10.1097/00000421-199306000-00007[↩]
- Roh YH, Yoo SJ, Choi YH, Yang HC, Nam KW. Effects of Inflammatory Disease on Clinical Progression and Treatment of Ischiogluteal Bursitis: A Retrospective Observational Study. Malays Orthop J. 2020 Nov;14(3):32-41. doi: 10.5704/MOJ.2011.007[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Schon L, Zuckerman JD. Hip pain in the elderly: evaluation and diagnosis. Geriatrics. 1988 Jan;43(1):48-62.[↩]
- Rask MR. “Snapping bottom”: subluxation of the tendon of the long head of the biceps femoris muscle. Muscle Nerve. 1980;3(3):250–1. doi: 10.1002/mus.880030311[↩]
- Fujisawa Y, Ito M, Nakamura Y, Furuta J, Ishii Y, Kawachi Y, Otsuka F. Perforated ischiogluteal bursitis mimicking a gluteal decubitus ulcer in patients with spinal cord injury: report of 2 cases. Arch Dermatol. 2010 Aug;146(8):932-4. doi: 10.1001/archdermatol.2010.179[↩]
- Schuh A, Narayan CT, Schuh R, Hönle W. Calcifying Bursitis ischioglutealis: A Case report. J Orthop Case Rep. 2011 Oct-Dec;1(1):16-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4701112[↩][↩][↩]
- Le Floch P. La bourse séreuse ischiatique [Serous ischial bursa]. Bull Assoc Anat (Nancy). 1982 Mar;66(192):89-94. French.[↩]
- Ripani M, Continenza MA, Cacchio A, Barile A, Parisi A, De Paulis F. The ischiatic region: normal and MRI anatomy. J Sports Med Phys Fitness. 2006 Sep;46(3):468-75.[↩]
- Navarro-Zarza JE, Villaseñor-Ovies P, Vargas A, Canoso JJ, Chiapas-Gasca K, Hernández-Díaz C, Saavedra MÁ, Kalish RA. Clinical anatomy of the pelvis and hip. Reumatol Clin. 2012 Dec-2013 Jan;8 Suppl 2:33-8[↩]
- McGill KC, Patel R, Chen D, Okwelogu N. Ultrasound-guided bursal injections. Skeletal Radiol. 2023 May;52(5):967-978. doi: 10.1007/s00256-022-04153-y[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Hitora T, Kawaguchi Y, Mori M, Imaizumi Y, Akisue T, Sasaki K, Yamada E, Yamamoto T. Ischiogluteal bursitis: a report of three cases with MR findings. Rheumatol Int. 2009 Feb;29(4):455-8. doi: 10.1007/s00296-008-0680-y[↩][↩]
- Ekiz T, Biçici V, Hatioglu C, Yalçın S, Cingöz K. Ischial Pain and Sitting Disability Due to Ischiogluteal Bursitis: Visual Vignette. Pain Physician. 2015 Jul-Aug;18(4):E657-8[↩]
- Bard H. [Periarticular pathology of the hip]. Rev Prat. 2002 Mar 15;52(6):627-31[↩]
- Blaichman JI, Chan BY, Michelin P, Lee KS. US-guided musculoskeletal interventions in the hip with MRI and US correlation. Radiographics. 2020;40(1):181–199. doi: 10.1148/rg.2020190094[↩]
- Wisniewski SJ, Hurdle M, Erickson JM, Finnoff JT, Smith J. Ultrasound-guided ischial bursa injection: technique and positioning considerations. PM R. 2014;6(1):56–60. doi: 10.1016/j.pmrj.2013.08.603[↩]
- Roh YH, Yoo SJ, Choi YH, Yang HC, Nam KW. Effects of inflammatory disease on clinical progression and treatment of ischiogluteal bursitis: a retrospective observational study. Malays Orthop J. 2020;14(3):32–41. doi: 10.5704/MOJ.2011.007[↩]
- Chen B, Rispoli L, Stitik T, Leong M. Successful Treatment of Gluteal Pain from Obturator Internus Tendinitis and Bursitis with Ultrasound-Guided Injection. Am J Phys Med Rehabil. 2017 Oct;96(10):e181-e184[↩]
- Lee SH, Jang WY, Lee MS, Yoon TR, Park KS. Surgical Excision for Refractory Ischiogluteal Bursitis: A Consecutive Case Series of 21 Patients. Hip Pelvis. 2023 Mar;35(1):24-31. doi: 10.5371/hp.2023.35.1.24[↩]
- Chen B, Rispoli L, Stitik T, Leong M. Successful Treatment of Gluteal Pain from Obturator Internus Tendinitis and Bursitis with Ultrasound-Guided Injection. Am J Phys Med Rehabil. 2017 Oct;96(10):e181-e184. doi: 10.1097/PHM.0000000000000702[↩][↩][↩]
- Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35(11):991–1014. doi: 10.2165/00007256-20053511000005[↩]
- Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016;25(1):158–67. doi: 10.1016/j.jse.2015.08.032[↩]
- Nguyen BD, Roarke MC. F-18 FDG PET/CT incidental finding of large ischiogluteal bursitis. Clin Nucl Med. 2007;32:535–537. doi: 10.1097/RLU.0b013e3180646ad3[↩]
- Samura K, Morioka T, Hashiguchi K, et al. Bursal cyst (bursitis) of the coccygeal region clinically mimics sacrococcygeal meningocele. Childs Nerv Syst. 2008;24:533–535. doi: 10.1007/s00381-007-0567-3[↩]
- Aaron DL, Patel A, Kayiaros S, Calfee R. Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg. 2011;19(6):359–67. doi: 10.5435/00124635-201106000-00006[↩]
- Mills GM, Baethge BA. Ischiogluteal bursitis in cancer patients: an infrequently recognized cause of pain. Am J Clin Oncol. 1993;16(3):229–31. doi: 10.1097/00000421-199306000-00007[↩][↩]
- Swartout R, Compere EL. Ischiogluteal bursitis. The pain in the arse. JAMA. 1974;227(5):551–2. doi: 10.1001/jama.227.5.551[↩]
- Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol. 2013;201(5):1083–6. doi: 10.2214/AJR.12.10038[↩]
- Chen B, Rispoli L, Stitik T, Leong M. Successful Treatment of Gluteal Pain from Obturator Internus Tendinitis and Bursitis with Ultrasound-Guided Injection. Am J Phys Med Rehabil. 2017 Oct;96(10):e181-e184.[↩]
- Völk M, Gmeinwieser J, Hanika H, Manke C, Strotzer M. Ischiogluteal bursitis mimicking soft-tissue metastasis from a renal cell carcinoma. Eur Radiol. 1998;8(7):1140-1. doi: 10.1007/s003300050522[↩][↩]
- Anderson CR. Weaver’s bottom[letter to the editor] JAMA. 1974;228:565.[↩]
- Crenshaw AH., Jr . Non-traumatic disorders. In: Canale ST, editor. Campbell’s operative orthopedics. 9th ed. St. Louis: Mosby; 1998. pp. 782–783.[↩]
- Garcia-Porrua C, Gonzalez-Gay MA, Corredoira J, Vazquez-Caruncho M. Hip pain. Ann Rheum Dis. 1999 Mar;58(3):148-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1752842/pdf/v058p00148.pdf[↩]
- Lambie P, Kaufman R, Beardmore T. Septic ischial bursitis in systemic lupus erythematosus presenting as a perirectal mass. J Rheumatol. 1989 Nov;16(11):1497-9.[↩]
- Resnick D, Niwayama G. Osteomyelitis, septic arthritis, and soft tissue infection: organisms. In: Resnick D, editor. Diagnosis of bone and joint disorders. 4th ed. Philadelphia: Saunders; 2002. pp. 2510–2624.[↩]
- Navarro-Zarza JE, Villaseñor-Ovies P, Vargas A, Canoso JJ, Chiapas-Gasca K, Hernández-Díaz C, Saavedra MÁ, Kalish RA. Clinical anatomy of the pelvis and hip. Reumatol Clin. 2012 Dec-2013 Jan;8 Suppl 2:33-8. doi: 10.1016/j.reuma.2012.10.006[↩]
- Choudhry MN, Malik RA, Charalambous CP. Blood glucose levels following intra-articular steroid injections in patients with diabetes: a systematic review. JBJS Rev. 2016;4(3):e5. doi: 10.2106/JBJS.RVW.O.00029[↩]
- Waterbrook AL, Balcik BJ, Goshinska AJ. Blood glucose levels after local musculoskeletal steroid injections in patients with diabetes mellitus: a clinical review. Sports Health. 2017;9(4):372–374. doi: 10.1177/1941738117702585[↩]
- Malladi AS, Gratton SB, Stone D, Scalapino KJ, Charles JF. Recurrent adverse psychiatric effects following intra-articular corticosteroid injection. J Clin Rheumatol. 2011;17(5):284–285. doi: 10.1097/RHU.0b013e318227ab11[↩]
- Patten S, Neutel C. Corticosteroid-induced adverse psychiatric effects. Drug Saf. 2000;22(2):111–122. doi: 10.2165/00002018-200022020-00004[↩]
- Kubin ME, Riekki R. Benzyl alcohol allergy mimicking corticosteroid allergy. Contact Dermatitis. 2016;75(1):58–59. doi: 10.1111/cod.12562[↩]
- Brinks A, Koes BW, Volkers AC, Verhaar JA, Bierma-Zeinstra SM. Adverse effects of extra-articular corticosteroid injections: a systematic review. BMC Musculoskelet Disord. 2010;11:206. doi: 10.1186/1471-2474-11-206[↩][↩]
- Pal B, Morris J. Perceived risks of joint infection following intra-articular corticosteroid injections: a survey of rheumatologists. Clin Rheumatol. 1999;18:264–265. doi: 10.1007/s100670050098[↩]
- Lee YB, Kim DH, Jung JH, Park JY. Chronic Open Infective Lateral Malleolus Bursitis Management Using Local Rotational Flap. Biomed Res Int. 2017;2017:2728092. doi: 10.1155/2017/2728092[↩]