Contents
What are knock knees
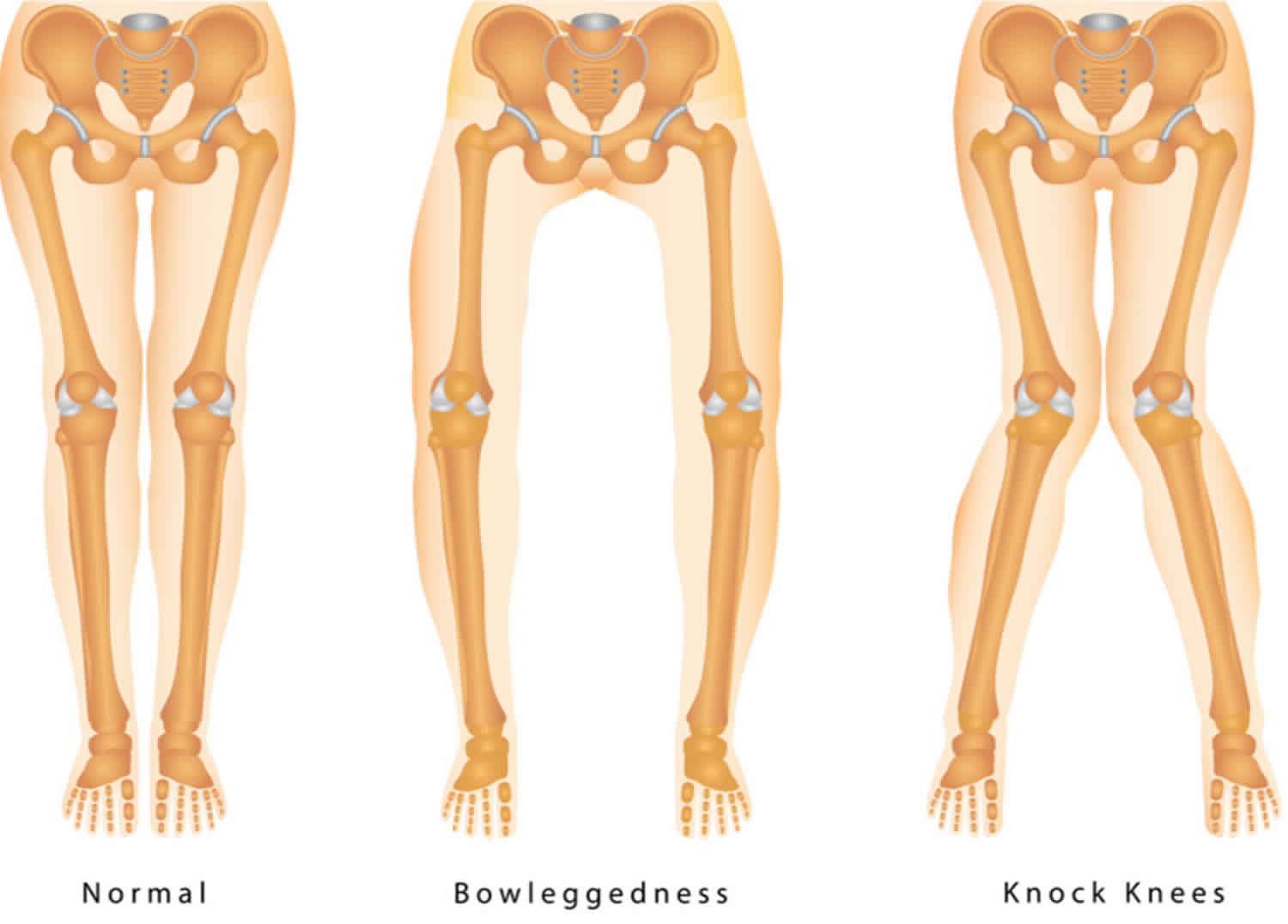
Knock knees is also known as genu valgum, is when a person has a large gap between their feet when they’re standing with their knees together. Knock knees is a type of knee alignment seen when a child (or adult) stands up straight with their knees together, but their feet and ankles stay apart. The opposite type of alignment, called bow legs (genu varum), is when someone stands with their feet and ankles together, and there is a gap between the knees.
A standing child of average weight whose knees touch, but whose ankles do not, is usually considered to have knock knees. An abnormal walking gait can also be a sign of the condition. Knock knees usually becomes apparent when a child is 2 to 3 years old, and it may increase in severity until about age 4. It usually self-corrects by the time a child is about 7 or 8 years old. But if knock knees doesn’t appear until a child is 6 or older, it could be a sign that there is an underlying bone disease.
Between birth and 18 months, an outward-turning (varus) alignment from hip to knee to ankle is normal. Between about 18 and 24 months, this alignment normally becomes neutral. When the child is between 2 and 5 years old, an inward-turning (valgus) alignment is normal. The alignment returns to neutral as the child grows.
Many young children have knock knees, which tend to be most obvious at around the age of 4. Knock knees is almost always just a normal part of children’s development, and their legs will normally straighten by the age of 6 or 7. Children normally outgrow knock knees without treatment, unless it is caused by a disease. If surgery is needed, the results are most often good.
During early childhood, knock-knees actually help a child to maintain balance, particularly when the child begins to walk, or if the foot rolls inward or turns outward. When a child has knock knees, both knees usually lean inward symmetrically. One knee, however, may “knock” less than the other or may even remain straight.
Occasionally, knock knees persist into adolescence. The condition is slightly more common in girls, although boys can develop it, too.
Slight knock knees can continue into adulthood, but this also isn’t usually anything to worry about unless it causes other problems.
However, knock knees can very occasionally be a sign of an underlying condition that needs treatment, especially if the condition develops in older children or adults, or doesn’t improve with age.
Knock knees can also develop as a result of a medical problem or disease, such as:
- Injury of the shinbone (only one leg will be knock-kneed)
- Osteomyelitis (bone infection)
- Overweight or obesity
- Rickets (a disease caused by a lack of vitamin D)
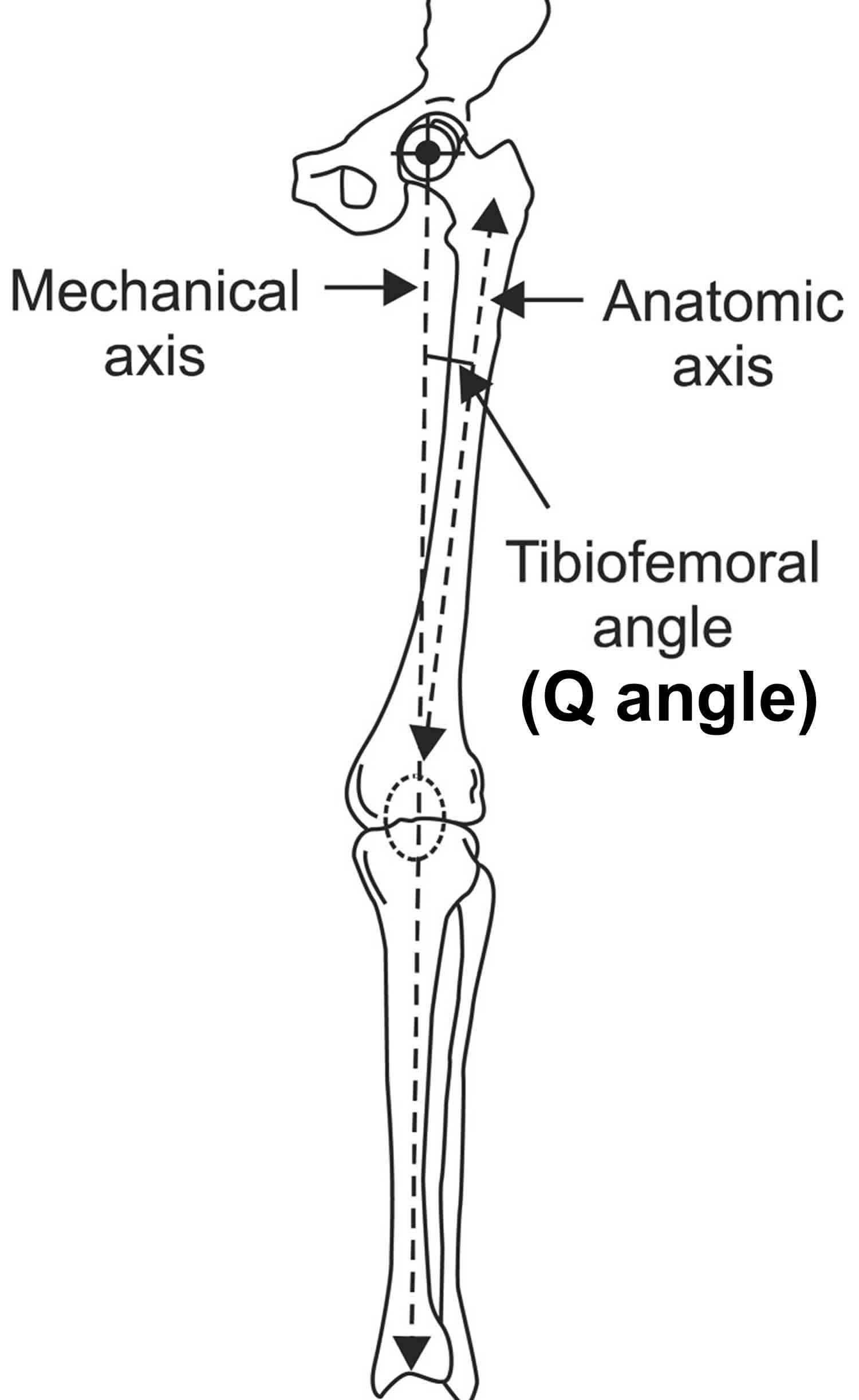
Knock knees are usually assessed by directly measuring the angle of the shin bone to the thigh bone (tibiofemoral angle) or by measuring the distance between the ankles (intermalleolar distance). Sometimes photographs or x-rays can be taken to calculate these measures.
Knock knees (and bow legs) are a normal part of a child’s growth and development. The classic pattern of changes at the knee with age in Caucasian children is bow legs at birth, straightening out at two years, going into knock knees at four years, and straightening out between six to 11 years.
There might be some ethnic and gender variation to the timing and severity of knock knees. For example, the knees of south Indian children tend to straighten out sooner after birth, and go into knock knees earlier but with less severe angles. Girls seem to show a higher knock knee angle than boys at all ages.
However knock knees can be a problem. While most cases are a normal variant of growth (physiological knock knees), further investigation is needed (pathological knock knees) if the knock knee angle is large, if they appear late or worsen after eight years of age, occur on only one leg, are painful or cause a limp. In knock knees, the majority of the body’s weight passes through the lateral (outside) portion of the joint. Potentially directly making the medial collateral ligaments (MCLs) more susceptible to injury.
Figure 1. Knock knees
Figure 2. Tibiofemoral angle
Pathologic knock knees refers to the pathologic condition of persistent or worsening knock knees in a patient older than 7 years of age. This needs to be differentiated from physiologic knock knees, which is normal during early childhood growth and generally resolves by age 7 1.
Physiologic knock knees first becomes apparent at 2 years of age and increases to a maximum of generally 8-10 degrees (tibiofemoral angle) by 3-4 years of age 2. This valgus then gradually decreases over the next few years reaching a stable adult knee valgus of 5-7 degrees by 7 years of age 1. However, a broad range of physiologic knock knees has been reported 1. At 3 to 4 years of age, a tibiofemoral angle from 2 degrees varus to 20 degrees valgus is considered normal while neutral to 12 degrees valgus is normal over the age of 7 3.
While physiologic knock-knee normally occurs during early childhood and spontaneously resolves by age 7, knock knees refers to the pathologic condition that tends to develop in early adolescence and does not spontaneously resolve after age 7. Asymmetric knock knees is more likely to be pathologic than physiologic. Most children younger than 6 years of age who are being evaluated for knock knees actually have physiologic knock-knee and are considered normal. While valgus deformity can arise from the distal femur or the proximal tibia, it is most often primarily from the femur.
Clinical examination should include torsional profile. In the prone position, the amount of femoral anteversion and tibial torsion should be assessed and recorded. Often the appearance of knock-knee alignment in adolescents and younger children is due to increased femoral anteversion and external tibial torsion. However, if the patellae are positioned pointing directly forward, knock knees may not be present.
Knock knees may appear worse clinically than radiographically. Besides deformity, knee pain is the most common patient complaint. Other associated features may include an out-toed gait and lateral patellar subluxation. The presence or absence of knee pain and/or functional limits with activities should be determined.
Physiologic knock-knee is expected to spontaneously resolve and therefore managed conservatively with observation. Since pathologic knock knees does not self-correct and may cause significant morbidity, surgical treatment is indicated.
Key points:
- Pathologic knock knees is defined as persistent or worsening knock knees in a patient older than 7 years of age
- Physiologic knock knees is greatest at 3-4 years of age and should spontaneously resolve by age 7. In the course of developing normal alignment of their lower extremities, all young children have knock knees to some degree for a period of time. At the age of 3, more than 20 percent of children have at least a 5-centimeter gap between their ankles. By the age of 7, only 1 percent of children have this gap.
- An anterior-posterior standing long-length plain film is recommended in evaluating the mechanical axis and angular deformities of the femur and tibia
- Physiologic knock knees should be managed conservatively
- Hemiepiphysiodesis is the treatment of choice for pathologic knock knees in a skeletally immature patient
- Osteotomy is the treatment of choice for immediate correction or in a skeletally mature patient
Knock knees in children aren’t usually a cause for concern and should improve as your child gets older.
However, visit your doctor if:
- the gap between the ankles is greater than 8cm while standing with the knees together
- there’s a big difference between the angle of the lower legs when standing compared with the upper legs
- the problem seems to be getting worse
- a child under the age of 2 or over the age of 7 has knock knees
- only one leg is affected
- there are other symptoms, such as knee pain or difficulty walking
- you have any other concerns about the way your child stands or walks
- you develop knock knees in adulthood
Your doctor will examine your or your child’s legs, ask about any pain or walking difficulties, and may take some measurements.
They may refer you to an orthopaedic surgeon (a specialist in bone and joint problems) and arrange an X-ray of your legs and blood tests to check for underlying problems.
What causes knock knees
Knock knees are fairly common in healthy children under the ages of 6 or 7, and are just a normal part of growth and development.
The legs will usually gradually straighten as the child grows, although mild knock knees can last into adulthood.
Some cases of knock knees, especially in a child who’s 6 or older, may be a sign of an underlying bone disease, such as osteomalacia or rickets. Obesity can contribute to knock knees—or can cause gait (walking) problems that resemble, but aren’t actually, knock knees. Knock knees can occasionally result from an injury to the growth area of the shin bone (tibia), which may result in just one knocked knee.
Knock knees that develop later in childhood or don’t improve with age can sometimes be associated with an underlying problem, such as:
- Rickets – problems with bone development resulting from a lack of vitamin D and calcium
- Excessive pressure on the knees – for example, as a result of obesity or loose knee ligaments (the bands of tissue around joints that connect bones to one another)
- An injury or infection affecting the knees or leg bones
- Genetic conditions affecting the development of the bones or joints
Adults can sometimes develop knock knees. These cases are often associated with joint problems such as osteoarthritis or rheumatoid arthritis.
The differential diagnosis for the cause of knock knees includes idiopathic, metabolic bone diseases such as rickets, skeletal dysplasias, physeal injury, and post-traumatic knock knees 4. The most common skeletal dysplasias associated with knock knees are chondroectodermal dysplasia, spondyloepiphyseal dysplasia, and Morquio’s syndrome 5. Injury to the lateral physis of the distal femur or proximal tibia can cause lateral growth disturbance and relative medial overgrowth leading to progressive knock knees. Proximal tibial metaphyseal fractures (Cozen’s fracture) are also associated with late valgus deformity and should be monitored for 1 to 2 years for the development of this complication 4.
Knock knees prevention
There is no known prevention for normal knock knees.
Knock knees symptoms
If someone with knock knees stands with their knees together, their lower legs will be spread out so their feet and ankles are further apart than normal.
A small distance between the ankles is normal, but in people with knock knees this gap can be up to 8cm (just over 3 inches) or more.
Knock knees don’t usually cause any other problems, although a few severe cases may cause knee pain, a limp or difficulty walking.
Knock knees that don’t improve on their own can also place your knees under extra pressure, which may increase your risk of developing arthritis.
Knock knees possible complications
Knock knees complications may include:
- Difficulty walking (very rare)
- Self-esteem changes related to cosmetic appearance of knock knees
- If left untreated, knock knees can lead to early arthritis of the knee
Knock knees diagnosis
A health care provider will examine your child. Tests will be done if there are signs that knock knees are not a part of normal development.
Knock knees become apparent when a child stands with legs straight and toes pointed forward. Your child’s doctor can determine the severity of the knock knees by observing the position of the legs, knees and ankles and by measuring the distance between the inner ankle bones. The condition is considered more severe the wider the distance between the ankles.
The doctor’s exam for diagnosing knock knees may include:
- measurements of your child’s length and height
- measurements of weight and body mass index (BMI)
- measurements taken of knee extensions and rotations
- assessment of leg-lengths and leg symmetry
- observation and assessment of gait.
If your child is within the normal age for knock knees, has a normal exam with a typical appearance and no functional problems, doctors don’t usually take x-rays, preferring to avoid unnecessary radiation. If your child is older than the usual age range or if the legs aren’t symmetrical, your doctor will usually opt for standing x-rays.
Imaging Studies
An anterior-posterior standing long-length film (bilateral hips to ankles) is recommended when clinical examination is consistent with pathologic knock knees. It allows for assessment of the mechanical axis and joint deviation. The mechanical axis of the lower extremity is defined as the line from the center of the femoral head through the center of the ankle mortise, and generally passes through the medial tibial spine of the knee.
The proximal tibia can be divided into 4 equal-width partitions based upon a center-line between the tibial spines. The lateral 2 partitions are assigned positive values whereas the medial 2 partitions are assigned negative values. A normal mechanical axis passes through the middle half of the knee (Zone +1 or -1). Genu valgum that causes a mechanical axis to pass lateral to the tibial plateau (Zone +3) is considered pathologic. Correction of pathologic knock knees will not only improve appearance and mechanical axis, but also will generally improve pain in the symptomatic patient 6.
When evaluating any knee deformity it is important to determine whether the deformity originates from the femur or tibia. The mLDFA (mechanical lateral distal femoral angle) is the lateral angle between a line from the center of the femoral head to the center of the tibia spines versus a line along the distal femoral condyles. The MPTA (medial proximal tibial angle) is the medial angle between a line from the center of the tibia spines to the center of the ankle mortise versus a line along the tibial plateau. Both angles are considered normal at 87°, and are definitively abnormal if they fall outside of the normative ranges of 85 to 90 degrees 7.
Knock knees treatment
In most cases, knock knees don’t need to be treated because the problem tends to correct itself as a child grows. Your child doesn’t need to avoid physical activity, wear supportive leg braces or shoes, or do any special exercises. Doctors treat most children who have knock knees with close observation during those years when this condition is a natural part of a child’s leg development (typically ages 2 to 5), since the condition usually corrects itself with time. As a child grows, walking patterns become normal or near-normal by 7 to 8 years of age (or occasionally by the time the child becomes a teen).
If the problem continues after age 7, the child may use a night brace. This brace is attached to a shoe.
Mild knock knees that persist into adulthood don’t need to be treated unless they’re causing problems, such as knee pain.
Surgery may be considered for knock knees that are severe and continue beyond late childhood.
Non-surgical options for knock knees
In a very few cases, knock knees may be severe and may not self-correct. Splints and other devices aren’t usually needed for a child at a natural stage of valgus up to age 7. These devices can be useful if the child’s natural valgus doesn’t straighten out on its own by about the time your child is 7 or 8 years old — or if the knock knees has an underlying systemic or metabolic condition causing it.
For children with severe, unresolved knock knees, doctors may recommend:
- a night brace, particularly if a family history of knock knees exists; the brace attaches to a shoe and works by pulling the knee up into a straight position
- orthopedic shoes, usually equipped with a heel wedge and occasionally an arch pad
Treating the underlying cause of knock knees
If knock knees are caused by an underlying condition, treatment for this may be necessary. For example, rickets can be treated with vitamin D and calcium supplements.
Adults with arthritis may benefit from wearing leg braces or special insoles to reduce the strain on their knees.
Knock knees surgery
Surgery for knock knees is rarely necessary, although it may be recommended if the condition is severe or persistent.
In the rare event that natural growth, braces or shoes don’t correct your child’s knock knees, your doctor may recommend surgery. The surgery may involve either influencing bone growth (called a “guided growth” procedure) or cutting and straightening the thigh bone or shin bone (osteotomy of the femur or tibia).
There are 2 main types of operation that may be carried out:
- Guided growth surgery – where small metal plates are placed on the inside of the knees, which helps correct their growth over a period of around 12 months; the plates will be removed once the treatment is complete. Guided growth surgery means stopping the growth on the bent side of the bone (for knock knees, the inside of the knee). This is often done by implanting small metal devices that tether the medial/inside part of the growth centers around the knee, allowing the lateral/outer part to grow and straighten the knee. Children usually have guided-growth surgery when they’re approaching puberty (approximately age 11 in girls and 13 in boys). This allows time for the child’s bones to continue to straighten on their own during the remaining growing years. This is a minimal day-surgery procedure with immediate weight bearing and a rapid return to sports allowed.
- An osteotomy – where a thin wedge of bone is removed from the leg bones so they’re realigned into the correct position; plates and screws are used to fix the bones in their new position. Osteotomy surgery is needed for more severe deformities or after growth is finished. After surgery, your child will probably stay in the hospital for a couple of days and be given pain medication. When your child goes home, limit weight-bearing activities. Crutches or a walker may be needed for a six to eight weeks. Physical therapy will help restore muscle strength. Typically, after six months, full activities, including sports may be resumed.
Children with persistent knock knees who are still rapidly growing are more likely to be offered the guided growth operation. Osteotomies are mainly used for adults with severe knock knees.
Both procedures are carried out under general anesthetic, which means you or your child will be unconscious while having the operation.
A child can usually start walking again within a few days of having a guided growth procedure and return to sports within a few weeks. It can take a few months to return to all your normal activities after having an osteotomy.
Surgical correction of a pathologic knock knees with a mechanical axis lateral to the tibial plateau (Zone +3) or through the lateral fourth of the tibial plateau (Zone +2) with associated knee pain will not only improve appearance and mechanical axis, but may also delay the potential development of early-onset arthritis 7. The threshold severity of knock knees sufficient to cause degenerative changes is unknown.
Hemiepiphysiodesis and osteotomy are the operative treatments of choice 8. Hemiepiphysiodesis is used in skeletally immature children and is most often achieved by placement of medial physeal-spanning plates. Fixation can be placed on the distal femur, proximal tibia, or both depending on the location of deformity and expected growth time remaining. Fixation position is very important, with the plates placed extraperiosteally. Fixative devices should be placed centrally on the lateral view to prevent sagittal plane deformity, unless additional sagittal deformity is present and correction is desirable. Other techniques such as transphyseal screw and tension band screw placement have been reported 9.
Close follow-up every 3-4 months after hemiepiphysiodesis fixation placement is important to monitor for abnormal angular or rotational correction as well as overcorrection. Fixation removal within 24 months is sometimes recommended to prevent permanent physeal growth arrest, although this time interval has not be rigorously studied. Slight overcorrection before removal of fixation may be considered in children who begin hemiepiphysiodesis treatment before the age of 10 due to the risk of rebound medial overgrowth and loss of correction. Radiolographic rebound of knock knees has been reported following implant removal 10. However, factors leading to rebound still need to be better defined, and treatment of children under 10 years of age is reasonable as long as the patients and families are aware that repeat treatment is a possibility.
Osteotomy can be performed when immediate correction of the valgus deformity is desired or if the patient is skeletally mature 11. While a variety of osteotomy techniques are available, it is advisable to correct the bone(s) with deformity based on analysis of mLDFA and MPTA. While the distal femur is most often the site of correction; when correction of valgus is performed in the tibia, the peroneal nerve is at risk, and decompression of the peroneal nerve with a larger acute correction or gradual correction with external fixation should be considered.
Knock knees prognosis
Since knock knees are self-correcting in up to 99 percent of cases, the long-term outlook is very positive for most children with the condition. For children who need surgery for severe forms of the condition, the outlook is also excellent. The procedures are quite safe — and children’s bones usually heal faster and more reliably than adults. For children with surgically-repaired knock knees caused by an underlying condition (pathologic valgus), adulthood can bring can risks of arthritis, meniscal tears, pain or dislocation.
- Green WB. Genu varum and genu valgum in children. In: SchaferM, ed. AAOS Instructional Course Lectures, Vol. 43. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:151.[↩][↩][↩]
- Heath CH. Staheli LT. Normal limits of knee angle in white children. J Pediatr Orthop 1993; 13:259.[↩]
- Hensinger RN. Standards in orthopedics. New York: Raven Press, 1986.[↩]
- McCarthy JJ, Kim DH, Eilert RE. Posttrauamtic genu valgum: operative versus nonoperative treatment. J Pediatr Orthop 1998; 18:518.[↩][↩]
- Kopits SE. Orthopaedic complications of dwarfism. Clin Orthop Relat Res 1976; 114:153.[↩]
- Stevens PM, MacWilliams B, Mohr RA. Gait analysis of stapling for genu valgum. J Pediatr Orthop 2004; 24:70.[↩]
- Paley D, Tetsworth K. Mechanical Axis Deviation of the Lower Limbs: Preoperative Planning of the Uniapical Angular Deformities of the Tibia or Femur. Clin Orthop Relat Res 1992; 280:48.[↩][↩]
- Paley D. Principles of Deformity Correction. New York: Springer-Verlag, 2002.[↩]
- Park, Hoon, et. al. Hemiepiphysiodesis for Idiopathic Genu Valgum: Percutaneous Transphyseal Screw Versus Tension-band Plate. J Pediatr Orthop 2016[↩]
- Farr, Sebastian, et. al. Rebound of frontal plane malalignment after tension band plating. J Pediatr Orthop 2016[↩]
- Davis CA, Maranji K, Frederick N, et al. Comparison of crossed pins and external fixation for correction of angular deformities about the knee in children. J Pediatr Orthop 1998; 18:502.[↩]