Contents
What is leishmaniasis
Leishmaniasis is a parasitic disease that is caused by infection with Leishmania parasites, which are spread by the bite of phlebotomine sand flies (Phlebotomus papatasi). Leishmaniasis is caused by obligate intracellular protozoa of the genus Leishmania. Human infection is caused by about 21 of 30 species that infect mammals. These include the Leishmania donovani complex with 3 species (Leishmania donovani, Leishmania infantum, and Leishmania chagasi); the Leishmania mexicana complex with 3 main species (Leishmania mexicana, Leishmania amazonensis, and Leishmania venezuelensis); Leishmania tropica; Leishmania major; Leishmania aethiopica; and the subgenus Viannia with 4 main species (Leishmania Viannia braziliensis, Leishmania Viannia guyanensis, Leishmania Viannia panamensis, and Leishmania Viannia peruviana) 1. The different Leishmania species are morphologically indistinguishable, but they can be differentiated by isoenzyme analysis, molecular methods, or monoclonal antibodies. Different Leishmania parasite species can be associated with diverse clinical manifestations and complications. Species identification can facilitate clinical management, such as decisions regarding whether/which treatment is indicated.
There are several different forms of leishmaniasis in people:
- The most common form is cutaneous leishmaniasis, which causes skin sores, ulcers or scabs on exposed body parts such as the wrists, the ankles and lower legs, and the face where the sandflies have fed. Persons who have cutaneous leishmaniasis have one or more sores on their skin. The sores can change in size and appearance over time. They often end up looking somewhat like a volcano, with a raised edge and central crater. A scab covers some sores. The sores can be painless or painful. Some people have swollen glands near the sores (for example, in the armpit if the sores are on the arm or hand).
- Visceral leishmaniasis, which affects several internal organs (usually spleen, liver, and bone marrow). Persons who have visceral leishmaniasis usually have fever, weight loss, and an enlarged spleen and liver (usually the spleen is bigger than the liver). Some patients have swollen glands. Certain blood tests are abnormal. For example, patients usually have low blood counts, including a low red blood cell count (anemia), low white blood cell count, and low platelet count. Some patients develop post kala-azar dermal leishmaniasis. Visceral leishmaniasis is becoming an important opportunistic infection in areas where it coexists with HIV.
Leishmaniasis is found in parts of the tropics, subtropics, and southern Europe 1. Leishmaniasis is found in parts of about 88 countries. Approximately 350 million people live in these areas. Most of the affected countries are in the tropics and subtropics. The settings in which leishmaniasis is found range from rainforests in Central and South America to deserts in West Asia. More than 90 percent of the world’s cases of visceral leishmaniasis are in India, Bangladesh, Nepal, Sudan, and Brazil.
Leishmaniasis is also found in Mexico, Central America, and South America—from northern Argentina to Texas (not in Uruguay, Chile, or Canada), southern Europe (leishmaniasis is not common in travelers to southern Europe), Asia (not Southeast Asia), the Middle East, and Africa (particularly East and North Africa, with some cases elsewhere).
Figure 1. Phlebotomine sand fly
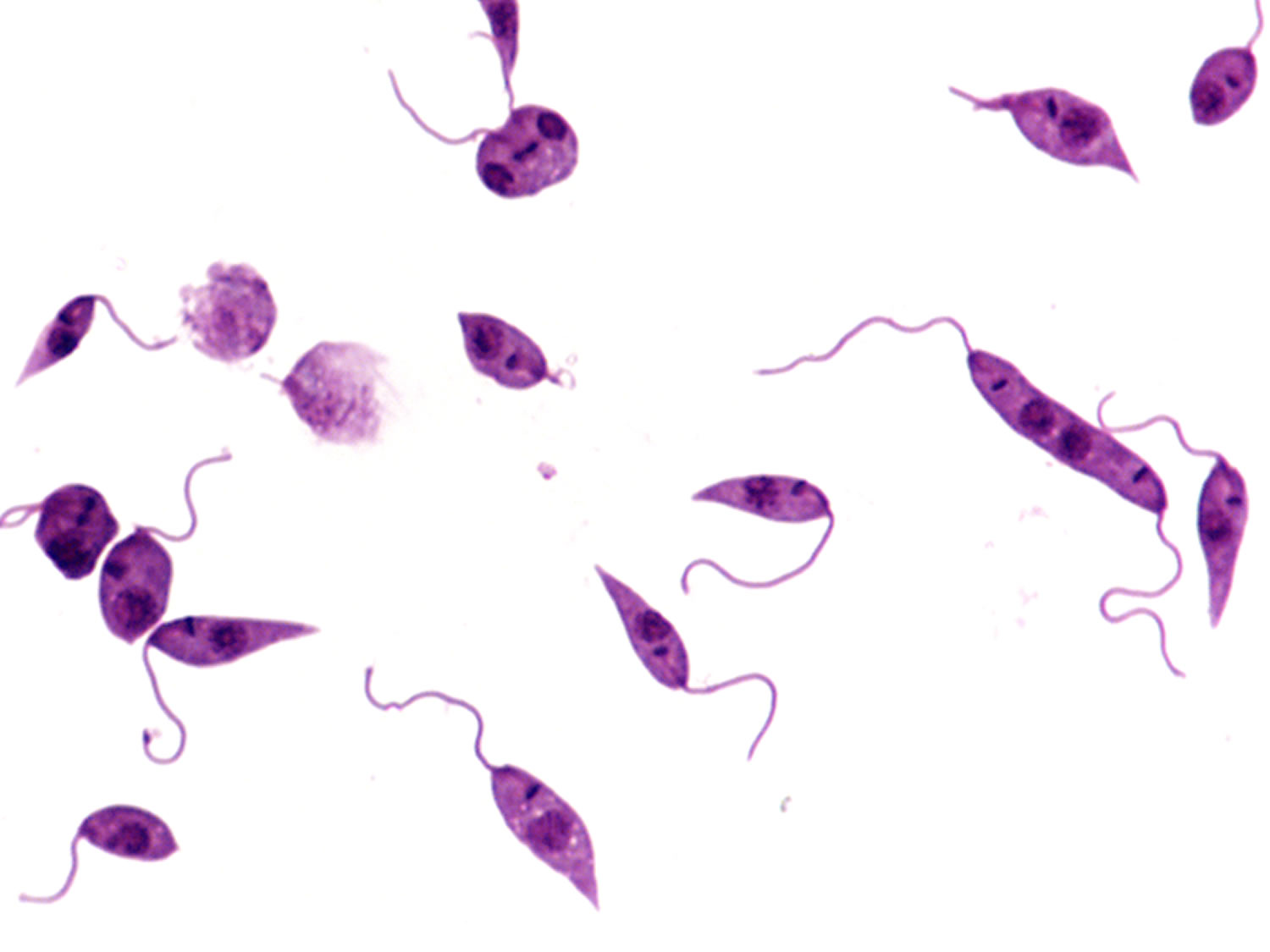
Figure 2. Leishmania donovani
Leishmaniasis life cycle
Leishmaniasis is transmitted by the bite of infected female phlebotomine sandflies (see Figure 1 above). The sandflies inject the infective stage (i.e., promastigotes) from their proboscis during blood meals (1). Promastigotes that reach the puncture wound are phagocytized by macrophages (2) and other types of mononuclear phagocytic cells. Promastigotes transform in these cells into the tissue stage of the parasite (i.e., amastigotes) (3), which multiply by simple division and proceed to infect other mononuclear phagocytic cells (4). Parasite, host, and other factors affect whether the infection becomes symptomatic and whether cutaneous or visceral leishmaniasis results. Phlebotomine sandflies become infected by ingesting infected cells during blood meals (number 5 and 6). In sandflies, amastigotes transform into promastigotes, develop in the gut (7) (in the hindgut for leishmanial organisms in the Viannia subgenus; in the midgut for organisms in the Leishmania subgenus), and migrate to the proboscis (8).
Figure 3. Leishmaniasis life cycle
Leishmaniasis prevention
No vaccines or drugs to prevent leishmaniasis are available.
The best way for travelers to prevent leishmaniasis infection is to protect themselves from sand fly bites. Personal protective measures include minimizing nocturnal outdoor activities, wearing protective clothing, and applying insect repellent to exposed skin.
In general, prevention and control measures must be tailored to the local setting and typically are difficult to sustain. Control measures against sand fly vectors or animal reservoir hosts might be effective in some settings.
In many geographic areas where leishmaniasis is found in people, infected people are not needed to maintain the transmission cycle of the parasite in nature; animal reservoir hosts (such as rodents or dogs), along with sand flies, maintain the cycle. For example, in Leishmania infantum/Leishmania chagasi-endemic regions, dogs serve as the main reservoir hosts; control strategies for such areas are being evaluated.
In some parts of the world, infected people are needed to maintain the cycle; this type of transmission (human—sand fly—human) is called anthroponotic. For example, in the Indian Subcontinent (South Asia), the transmission of Leishmania donovani is anthroponotic. In such areas, early detection and effective treatment of infected persons can serve as a control measure; suboptimal treatment can lead to development and spread of drug resistance. Because the transmission is intra- and peridomiciliary (rather than sylvatic), spraying houses with residual-action insecticides and using bed nets treated with long-lasting insecticides may be protective.
Leishmaniasis symptoms
Cutaneous leishmaniasis
This is the most common form of leishmaniasis, both in general and in U.S. travelers. Unless otherwise specified, cutaneous leishmaniasis refers to localized cutaneous leishmaniasis, rather than to much less common forms, such as diffuse cutaneous leishmaniasis and disseminated cutaneous leishmaniasis. Different Leishmania species cause Old World versus New World (American) cutaneous leishmaniasis. In the Old World (the Eastern Hemisphere), the causal agents include Leishmania tropica, Leishmania major, and Leishmania aethiopica, as well as Leishmania infantum and Leishmania donovani, primarily by the former two. The main species in the New World (the Western Hemisphere) are either in the Leishmania mexicana species complex (Leishmania mexicana, Leishmania amazonensis, and Leishmania venezuelensis) or the subgenus Viannia (Leishmania Viannia braziliensis, Leishmania Viannia guyanensis, Leishmania Viannia panamensis, and Leishmania Viannia peruviana); Leishmania infantum/Leishmania chagasi also causes cutaneous leishmaniasis in the New World.
In general, cutaneous leishmaniasis causes skin lesions, which can persist for months, sometimes years. The skin lesions usually develop within several weeks or months after the exposure but occasionally first appear years later (for example, in the context of trauma or immunosuppression). The lesions typically evolve from papules to nodular plaques to ulcerative lesions, with a raised border and central depression, which can be covered by scab or crust; some lesions persist as nodules. The lesions usually are painless but can be painful, especially if ulcerative lesions become infected with bacteria or if the lesions are near a joint. The healing process typically results in atrophic scarring.
Even patients with localized cutaneous leishmaniasis quite commonly develop more than one primary lesion (on the same or different parts of the body), satellite lesions, regional lymphadenopathy (occasionally bubonic), and/or nodular lymphangitis (sporotrichoid-like subcutaneous nodules). Sometimes lymphadenopathy is noticed, before skin lesions develop.
With minor differences, the clinical lesions produced by all these species are similar. Solitary or multiple subcutaneous nodules (smooth, soft, mobile and 0.5-2.0 cm in size) may occur proximal to the skin lesions and usually along the axis between the skin lesions and the regional lymph nodes. This is called sporotrichoid spread of localized cutaneous leishmaniasis 2. Healing usually takes place in 2-6 months in Leishmania major infection and 8-12 months in Leishmania tropica 2. The healing is almost always with a scar that is typically atrophic, hyperpigmented, and irregular. In some cases cutaneous leishmaniasis has been found to remain “active,” i.e., with positive smears, for 24 months or even longer. Such cases have been designated “non-healing chronic cutaneous leishmaniasis” 3. Multiple lesions can be seen and the highest number of lesions reported for a single patient is 425 4. Localized cutaneous leishmaniasis can be differentiated as acute (< 6 months duration), chronic (> 6 months duration) and recidivans (Figure 8). Acute localized cutaneous leishmaniasis can be further divided into three varieties: nodular-including papules and plaques, nodulo-ulcerative and ulcerative. These forms may appear singly or as an overlap picture. They may show all features described for a classical lesion i.e. clustered lesions, paired lesions, skin crease orientation, volcanic nodules, satellite papules, subcutaneous nodules and iceberg nodules 5.
Figure 4. Cutaneous leishmaniasis (acute, wet type of cutaneous leishmaniasis)
Figure 5. Cutaneous leishmaniasis (acute, wet type of cutaneous leishmaniasis)
Figure 6. Cutaneous leishmaniasis of face
[Source 2]Figure 7. Cutaneous leishmaniasis (a large solitary nodular plaque of cutaneous leishmanisis arising from lower lip)
Figure 8. Chronic cutaneous leishmaniasis of face with areas of scarring and reactivation of disease (Leishmaniasis recidivans)
[Source 2]Mucocutaneous leishmaniasis
Mucocutaneous leishmaniasis also called espundia, is a serious and occasionally a life threatening form of leishmaniasis, found mainly in the New World (the Western Hemisphere or Americas). Mucosal leishmaniasis is traditionally refer to a metastatic complication of New World cutaneous infection, which results from dissemination of parasites from the skin to the naso-oropharyngeal mucosa. Mucosal leishmaniasis is caused by species in the Viannia subgenus (especially Leishmania Viannia braziliensis but also Leishmania Viannia panamensis and sometimes Leishmania Viannia peruviana); it also can be caused by Leishmania amazonensis. Adequate systemic treatment of cutaneous leishmaniasis caused by these species may reduce the risk for mucosal disease, but some risk may remain. The magnitudes and determinants (parasite and host factors) of the risks for mucosal dissemination and for mucosal disease per se are poorly understood; even for the same species (for example, Leishmania Viannia braziliensis), the risks appear to vary among geographic regions in the Americas.
Mucosal leishmaniasis usually becomes clinically evident within several years (sometimes as long as decades) of the original cutaneous lesions, which typically were not treated at all or were treated suboptimally. However, mucosal and skin lesions may be noted concomitantly (mucocutaneous leishmaniasis), and some patients had subclinical cutaneous infection.
The initial manifestations of mucosal leishmaniasis usually are persistent, unusual nasal symptoms (such as stuffiness or bleeding), although oral or pharyngeal symptoms sometimes are noticed first. If untreated, the disease can progress to ulcerative destruction of the naso-oropharyngeal mucosa (such as perforation of the nasal septum).
Figure 9. Mucocutaneous leishmaniasis
Visceral leishmaniasis
The general term visceral leishmaniasis encompasses a broad spectrum of severity and manifestations. Although the incubation period generally ranges from weeks to months, asymptomatic infection can become clinically manifest years to decades after the exposure in people who become immunocompromised for other medical reasons (such as HIV/AIDS). Visceral leishmaniasis usually is caused by the species Leishmania donovani and Leishmania infantum (Leishmania chagasi generally is considered synonymous with Leishmania infantum) and affects internal organs (particularly, spleen, liver, and bone marrow).
The stereotypical manifestations of clinically manifest visceral infection include:
- Fever
- Weight loss (cachexia; wasting)
- Hepatosplenomegaly (usually, the spleen is more prominent than the liver)
- Pancytopenia—i.e., anemia, leukopenia, and thrombocytopenia
- A high total protein level and a low albumin level, with hypergammaglobulinemia
Lymphadenopathy may be noted, particularly in some geographic regions, such as Sudan and South Sudan.
HIV-coinfected patients may have atypical manifestations, such as involvement of the gastrointestinal tract and other organ systems.
The term kala-azar—which means black (kala) fever (azar) in Hindi—often is reserved for severe (advanced) cases of visceral leishmaniasis, although the terms kala-azar and visceral leishmaniasis sometimes are used interchangeably. If untreated, severe cases of visceral leishmaniasis typically are fatal, either directly from the disease or indirectly from complications, such as secondary (myco)bacterial infection or hemorrhage.
Some patients develop post kala-azar dermal leishmaniasis (PKDL), a syndrome characterized by skin lesions (such as erythematous or hypopigmented macules, papules, nodules, and patches), typically first noticed and most prominent on the face, that develop at variable intervals after (or during) therapy for visceral leishmaniasis. Persons with chronic post kala-azar dermal leishmaniasis can serve as important reservoir hosts of infection. Post kala-azar dermal leishmaniasis (PKDL) is a rare sequel to visceral leishmaniasis that has been apparently cured after adequate treatment. Post kala-azar dermal leishmaniasis (PKDL) is caused by Leishmania donovani and Leishmania aethiopica in the Old World (the Eastern Hemisphere) and is endemic in East Africa and India. In India the rash of PKDL occurs in 20 percent of patients and appears 1-2 years after treatment of the original disease and may persist for as long as 20 years. In Africa, this usually appear during or shortly after treatment and persists only for a few months. Skin lesions are categorized into 3 types, often in sequence: (i) hypopigmented macules markedly similar to the lesions of lepromatous leprosy, (ii) erythematous macules develop, which develop next, and (iii) yellowish pink nodules that finally appear, mostly on the face. These replace the hypopigmented and erythematous macules after a variable period of months or years. The rash is progressive over many years and seldom heals spontaneously. Cases of post kala-azar dermal leishmaniasis are more resistant to treatment, requiring higher doses of systemic medication 3.
Leishmaniasis diagnosis
Various laboratory methods can be used to diagnose leishmaniasis—to detect the parasite and to identify the Leishmania species. Some of the methods are available only in reference laboratories. In the United States, the Centers for Disease Control and Prevention (CDC) provides reference diagnostic services for leishmaniasis.
Leishmaniasis is diagnosed by detecting Leishmania parasites (or DNA) in tissue specimens—such as from skin lesions, for cutaneous leishmaniasis or from bone marrow, for visceral leishmaniasis—via light-microscopic examination of stained slides, molecular methods, and specialized culture techniques.
Identification of the Leishmania species also can be important, particularly if more than one species is found where the patient lived or traveled and if they can have different clinical and prognostic implications. The species can be identified by various approaches, such as molecular methods and biochemical techniques (isoenzyme analysis of cultured parasites).
For visceral leishmaniasis, serologic testing can provide supportive evidence for the diagnosis. The performance of various serologic assays may vary by geographic region and by host factors (for example, the sensitivity of serologic testing generally is lower in HIV-coinfected patients, particularly if the HIV infection was acquired before the Leishmania infection). Most serologic assays do not reliably distinguish between active and quiescent infection.
No leishmanin skin-test preparation has been approved for use in the United States.
Note: For visceral leishmaniasis, although the diagnostic sensitivity typically is higher for splenic aspirates than for specimens from other organs/tissues, splenic aspiration can be associated with life-threatening hemorrhage, even if conducted under radiologic guidance. Bone marrow aspiration is much safer. Examples of other potential sources of specimens for diagnostic testing include liver, lymph node, and whole blood or buffy coat. Among HIV-infected patients, the parasite also may be found in atypical sites (such as the gastrointestinal tract).
Laboratory diagnostic findings
Microscopy
In the human host, only the amastigotes stage is seen upon microscopic examination of tissue specimens. Amastigotes can be visualized with both Giemsa and hematoxylin and eosin (H&E) stains. The amastigotes of Leishmania spp. are morphologically indistinguishable from those of Trypanosoma cruzi. Amastigotes are ovoid and measure 1-5 micrometers long by 1-2 micrometers wide. They possess both a nucleus and kinetoplast.
Isoenzyme analysis
Isolation can be done using the biphasic medium which includes a solid phase composed of blood agar base (e.g., NNN medium), with defribinated rabbit blood. After isolation parasites can be characterized to the complex and sometimes to the species level using isoenzyme analysis, which is the conventional diagnostic approach for Leishmania species identification. Diagnostic identification of Leishmania using this approach may take several weeks.
Serology
Antibody detection can prove useful in visceral leishmaniasis but is of limited value in cutaneous disease, since most patients do not develop a significant antibody response. In addition, cross reactivity can occur with Trypanosoma cruzi, a fact to consider when investigating Leishmania antibody response in patients who have been in Central or South America.
Molecular diagnosis
Molecular approaches have the potential to be more sensitive and rapid; e.g., the results can be available within days versus weeks. The Centers for Disease Control and Prevention (CDC) has incorporated molecular methods in the algorithm for the laboratory diagnosis of leishmaniasis. The method is based on PCR amplification using generic primers that amplify a segment of the rRNA internal transcribed spacer 2 from multiple Leishmania species. DNA sequencing analysis is performed on the amplified fragment for species identification. This approach allows the differentiation among Viannia spp., namely, Leishmania Viannia braziliensis, Leishmania Viannia guyanensis and Leishmania Viannia panamensis as well as Leishmania aethiopica, Leishmania amazonensis, Leishmania donovani, Leishmania infantum/chagasi, Leishmania major, Leishmania mexicana and Leishmania tropica.
Leishmaniasis treatment
Treatment decisions should be individualized, with expert consultation. In general, all clinically manifest cases of visceral leishmaniasis and mucosal leishmaniasis should be treated, whereas not all cases of cutaneous leishmaniasis require treatment.
The treatment approach depends in part on host and parasite factors. Some approaches/regimens are effective only against certain Leishmania species/strains and only in particular geographic regions. Even data from well-conducted clinical trials are not necessarily generalizable to other settings. Of particular note, data from the many clinical trials of therapy for visceral leishmaniasis in parts of India are not necessarily directly applicable to visceral leishmaniasis caused by Leishmania donovani in other areas, to visceral leishmaniasis caused by other species, or to treatment of cutaneous and mucosal leishmaniasis.
Special groups (such as young children, elderly persons, pregnant/lactating women, and persons who are immunocompromised or who have other comorbidities) may need different medications or dosage regimens.
The relative merits of various treatment approaches/regimens can be discussed with CDC staff. In addition, in the United States, special considerations apply regarding the availability of particular medications to treat leishmaniasis. For example 6:
- Pentavalent antimonial (SbV) compounds—the traditional mainstays for treating leishmaniasis since the 1940s—have not been approved by the Food and Drug Administration (FDA) and are not commercially available in the United States. However, the pentavalent antimonial (SbV) compound sodium stibogluconate (Pentostam®) is available to U.S.-licensed physicians through the CDC Drug Service, under an IND (Investigational New Drug) protocol. Although Pentostam® is not new or investigational, the IND mechanism makes it possible for CDC to stock and provide the drug in the United States. CDC’s IND protocol covers intravenous (IV) and intramuscular (IM) administration (not intralesional). In the United States, the most common route of administration is IV (vs. IM), because the volume per dose is relatively high (for example, 14 mL for a 70-kg patient). Of note: Pentostam® is the only antileishmanial medication available through CDC; none of the other medications discussed below are available through CDC.
- One parenteral agent, liposomal amphotericin B (AmBisome®), which is administered by IV infusion, is FDA-approved for treatment of visceral leishmaniasis per se (i.e., the approved indications do not include cutaneous or mucosal leishmaniasis). This approval for visceral leishmaniasis dates back to 1997.
- In 2014, FDA approved the oral agent miltefosine for treatment of cutaneous, mucosal, and visceral leishmaniasis caused by particular Leishmania species (see below for details), in adults and adolescents at least 12 years of age who weigh at least 30 kg (66 pounds). The FDA-approved treatment regimen for persons who weigh from 30 to 44 kg is as follows: one 50-mg oral capsule of miltefosine twice a day (total of 100 mg per day) for 28 consecutive days. The FDA-approved treatment regimen for persons who weigh at least 45 kg (99 pounds) is one 50-mg capsule three times a day (total of 150 mg per day) for 28 consecutive days. Miltefosine is contraindicated in pregnant women. Women of reproductive potential should have a negative pregnancy test before starting therapy; they should be advised to use effective contraception during the treatment course and for 5 months thereafter. Nursing mothers should be advised not to breastfeed during the treatment course or for 5 months thereafter.
- Some medications that might have merit for treating selected cases of leishmaniasis are commercially available in the United States but the FDA-approved indications do not include leishmaniasis. Examples of such medications include the parenteral agents amphotericin B deoxycholate and pentamidine isethionate, as well as the orally administered “azoles” (ketoconazole, itraconazole, and fluconazole).
- Other medications that might have merit for treating selected cases of leishmaniasis currently are not available in the United States (such as the parenteral formulation of the aminoglycoside paromomycin)—or—are potentially available only through special mechanisms. For example, particular topical formations of paromomycin may be available through compounding pharmacies or may be imported under a single-patient treatment protocol.
Cutaneous leishmaniasis treatment
Decisions about whether and how to treat should be individualized. The treatment approach depends in part on the Leishmania species/strain and the geographic area in which infection was acquired; the natural history of infection, the risk for mucosal dissemination/disease, and the parasite’s drug susceptibilities in the pertinent setting; and the number, size, location, evolution, and other clinical characteristics of the patient’s skin lesions.
Treatment of cutaneous leishmaniasis may be indicated to:
- Decrease the risk for mucosal dissemination/disease (particularly for New World species in the Viannia subgenus; see Disease);
- Accelerate healing of the skin lesions;
- Decrease the risk for relapse (clinical reactivation) of the skin lesions;
- Decrease the local morbidity caused by large or persistent skin lesions, particularly those on the face or ears or near joints; and/or
- Decrease the reservoir of infection in geographic areas where infected persons (vs. non-human animals) serve as reservoir hosts (such as in Kabul, Afghanistan, and other Leishmania tropica-endemic areas, where transmission is anthroponotic).
In general, the first sign of a therapeutic response to adequate treatment is decreasing induration (lesion flattening). The healing process for large, ulcerative lesions often continues after the end of therapy. Relapse (clinical reactivation) typically is noticed first at the margin of the lesion.
Systemic therapy (parenteral)
For pentavalent antimonial (SbV) therapy, see above about CDC’s IND protocol for sodium stibogluconate (Pentostam®). The standard daily dose is 20 mg of SbV per kg, administered IV or IM. The traditional duration of therapy is 20 days for cutaneous leishmaniasis (10 days may suffice in some settings) and 28 days for mucosal (and visceral) leishmaniasis. For some patients, adjustment of the daily dose or the duration of therapy may be indicated.
Conventional amphotericin B deoxycholate traditionally has been used as rescue therapy for cutaneous (and mucosal) leishmaniasis. Lipid formulations of amphotericin B typically are better tolerated than conventional amphotericin B. However, the data supporting their use for treatment of cutaneous (and mucosal) leishmaniasis are from case reports/series rather than from controlled clinical trials; standard dosage regimens have not been established. When liposomal amphotericin B has been used for treatment of cutaneous leishmaniasis, patients typically have received 3 mg per kg daily, by IV infusion, for a total of 6 to 10 or more doses.
In the United States, pentamidine isethionate is uncommonly used for treatment of cutaneous leishmaniasis. Its limitations include the potential for irreversible toxicity and variable effectiveness.
Systemic therapy (oral)
In 2014, FDA approved the oral agent miltefosine for treatment of cutaneous leishmaniasis in adults and adolescents who are not pregnant or breastfeeding. The FDA-approved indications are limited to infection caused by three particular species, all three of which are New World species in the Viannia subgenus—namely, Leishmania (V.) braziliensis, L. (V.) panamensis, and L. (V.) guyanensis. Even for these species, the effectiveness of miltefosine therapy has been variable in different geographic regions. Use of miltefosine for treatment of infection caused by other Leishmania species in the New World or by any species in the Old World would constitute off-label use, as would treatment of children less than 12 years of age. See above for additional perspective and considerations regarding miltefosine.
The “azoles” ketoconazole, itraconazole, and fluconazole—administered orally—have been used with mixed results, in various settings. For example:
- Ketoconazole (adult regimen: 600 mg daily for 28 days) showed modest activity against L. mexicana and L. (V.) panamensis infection in small studies in Guatemala and Panama, respectively. However, itraconazole (adult regimen: 200 mg twice daily for 28 days) was ineffective against L. (V.) panamensis infection in a clinical trial in Colombia.
- Use of fluconazole (adult regimen: 200 mg daily for 6 weeks) for treatment of L. major infection in various countries in the Old World has been associated with mixed results. Preliminary data from Iran suggested that a higher daily dose (400 vs. 200 mg) might be more effective against L. major infection. In northeastern Brazil, a low response rate to treatment with fluconazole (6.5–8.0 mg per kg per day for 28 days) was noted among adults infected with L. (V.) braziliensis.
Local therapy
Some cases of cutaneous leishmaniasis might be candidates for local therapy, in part depending on the risk, if any, for mucosal dissemination/disease and on the number, location, size, and other characteristics of the skin lesions. Examples of local therapies that might have utility in some settings include cryotherapy (with liquid nitrogen), thermotherapy (use of localized current field radiofrequency heat), intralesional administration of SbV (to date, not covered by CDC’s IND protocol for Pentostam®), and topical application of particular formulations of paromomycin.
Visceral Leishmaniasis
The use of highly effective systemic therapy for leishmaniasis is important, as is supportive care—for example, therapy for malnutrition, anemia/bleeding, and intercurrent infections. For HIV-coinfected patients, antiretroviral therapy (ART) should be started or optimized according to standard practice; appropriate use of ART may delay relapses and improves survival.
Liposomal amphotericin B is FDA-approved for treatment of visceral leishmaniasis and generally is the treatment of choice for U.S. patients. Although various regimens have been suggested in the published literature, the FDA-approved regimen for immunocompetent patients consists of 3 mg per kg daily, by IV infusion, on days 1–5, 14, and 21 (total dose of 21 mg/kg). The FDA-approved regimen for immunosuppressed patients consists of 4 mg per kg daily on days 1–5, 10, 17, 24, 31, and 38 (total dose of 40 mg/kg). Some immunosuppressed patients may need even higher total doses and/or secondary prophylaxis (chronic maintenance therapy), in particular, HIV-coinfected patients with CD4 counts <200 cells/mm3. However, standard approaches to antileishmanial treatment and secondary prophylaxis have not been established—for example, the optimal agent, dose, and dosing interval for maintenance therapy.
Conventional amphotericin B deoxycholate is highly effective therapy for visceral leishmaniasis but generally is more toxic than liposomal amphotericin B.
In 2014 , FDA approved the oral agent miltefosine for treatment of visceral leishmaniasis caused by Leishmania donovani, in adults and adolescents who are not pregnant or breastfeeding. Use of miltefosine for visceral leishmaniasis caused by other species (e.g., L. infantum) would constitute off-label use, as would treatment of children less than 12 years of age. See above for additional perspective and considerations regarding miltefosine.
Pentavalent antimonial (SbV) therapy generally remains highly effective therapy for visceral leishmaniasis in most geographic regions, with the notable exception of parts of South Asia. See above about CDC’s IND protocol for sodium stibogluconate (Pentostam®). The standard dosage regimen for immunocompetent patients consists of 20 mg of SbV per kg daily, IV or IM, for 28 days. For some patients, adjustment of the daily dose or the duration of therapy may be indicated.
Other parenteral agents that have merit in some settings include paromomycin sulfate (the chemical equivalent of aminosidine), which is not available for parenteral administration in the United States—and—pentamidine isethionate, a second-line agent whose limitations include suboptimal effectiveness (most notably, in parts of South Asia) and the potential for irreversible toxicity.
- Parasites – Leishmaniasis. https://www.cdc.gov/parasites/leishmaniasis/[↩][↩]
- Clinical spectrum of cutaneous leishmaniasis: An overview from Pakistan. Dermatology Online Journal 18 (2): 4. https://escholarship.org/uc/item/8k3992kr[↩][↩][↩][↩][↩]
- Ghosn SH, Kurban AK. Leishmaniasis and Other Protozoan Infections. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA. Paller AS, Leffell DJ. Eds. Fitzpatrick’s Dermatology in General Medicine. Vol. 2, 7th ed. Mcgraw Hill Inc. 2008: 2001-9.[↩][↩]
- Couppie P, Clyti E, Sainte-Marie D, Dedet JP, Carme B, Pradinaud R. Disseminated cutaneous leishmaniasis due to Leishmania guyanensis: case of a patient with 425 lesions. Am J Trop Med Hyg 2004; 71: 558-60.[↩]
- Manzoor A. Cutaneous leishmaniasis. J Pak Assoc Dermatol 2005; 15: 161-71.[↩]
- Parasites – Leishmaniasis. Resources for Health Professionals. https://www.cdc.gov/parasites/leishmaniasis/health_professionals/index.html[↩]