Long bone anatomy
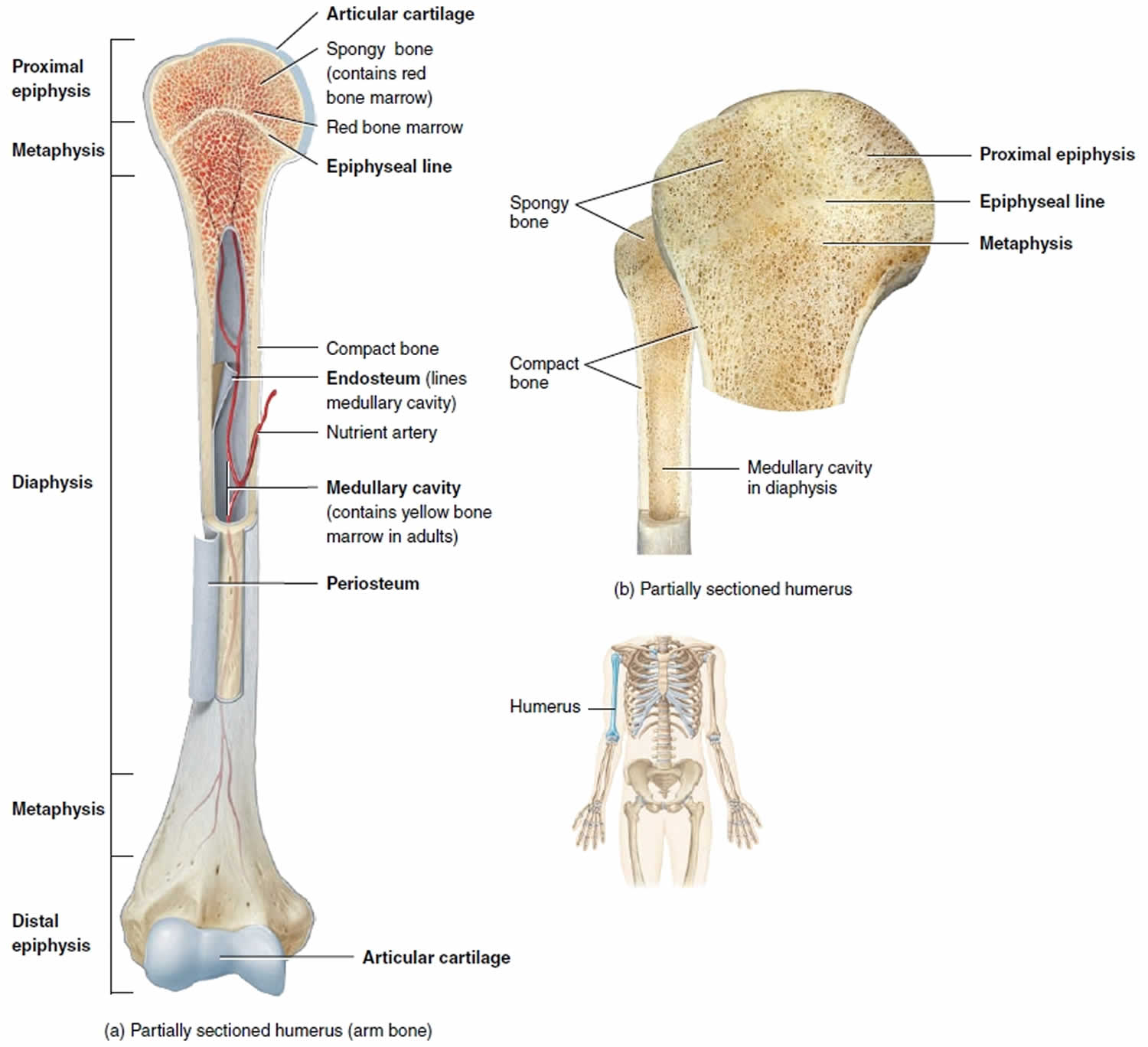
A long bone is a bone that has greater length than width. A long bone has a shaft and 2 ends. Long bones have a thick outside layer of compact bone and an inner medullary cavity containing bone marrow. The ends of a long bone contain spongy bone and an epiphyseal line. The epiphyseal line is a remnant of an area that contained hyaline cartilage that grew during childhood to lengthen the bone.
Long bones contain yellow bone marrow and red bone marrow, which produce blood cells.
The thigh bone (femur) is a long bone. Some bones in the fingers are classified as long bones, even though they are short in length. This is due to the shape of the bones, not their size.
All of the bones in the arms and legs, except the patella, and bones of the wrist, and ankle, are long bones.
Long bone structure
A typical long bone consists of the following parts:
- The diaphysis (growing between) is the shaft of a long bone — the long, cylindrical, main portion of the bone.
- The epiphyses (growing over; singular is epiphysis) are the proximal and distal ends of the bone.
- The metaphyses (between; singular is metaphysis) are the regions between the diaphysis and the epiphyses. In a growing bone, each metaphysis contains an epiphyseal (growth) plate, a layer of hyaline cartilage that allows the diaphysis of the bone to grow in length. When a bone ceases to grow in length at about ages 14–24, the cartilage in the epiphyseal plate is replaced by bone; the resulting bony structure is known as the epiphyseal line.
- The articular cartilage is a thin layer of hyaline cartilage covering the part of the epiphysis where the bone forms an articulation (joint) with another bone. Articular cartilage reduces friction and absorbs shock at freely movable joints. Because articular cartilage lacks a perichondrium and lacks blood vessels, repair of damage is limited.
- The periosteum is a tough connective tissue sheath and its associated blood supply that surrounds the bone surface wherever it is not covered by articular cartilage. It is composed of an outer fibrous layer of dense irregular connective tissue and an inner osteogenic layer that consists of cells. Some of the cells enable bone to grow in thickness, but not in length. The periosteum also protects the bone, assists in fracture repair, helps nourish bone tissue, and serves as an attachment point for ligaments and tendons. The periosteum is attached to the underlying bone by perforating fibers or Sharpey’s fibers, thick bundles of collagen that extend from the periosteum into the bone extracellular matrix.
- The medullary cavity (medulla- = marrow), or marrow cavity, is a hollow, cylindrical space within the diaphysis that contains fatty yellow bone marrow and numerous blood vessels in adults. This cavity minimizes the weight of the bone by reducing the dense bony material where it is least needed. The long bones’ tubular design provides maximum strength with minimum weight.
- The endosteum (endo- = within) is a thin membrane that lines the medullary cavity. It contains a single layer of bone-forming cells and a small amount of connective tissue.
Figure 1. Long bone anatomy
Long bone function
Long bones are hard, dense bones that provide strength, structure, and mobility.
Functions of long bone:
- Supports soft tissue and provides attachment for skeletal muscles.
- Protects internal organs.
- Assists in movement, along with skeletal muscles.
- Stores and releases minerals.
- Contains red bone marrow, which produces blood cells.
- Contains yellow bone marrow, which stores triglycerides (fats).
Long bone fracture
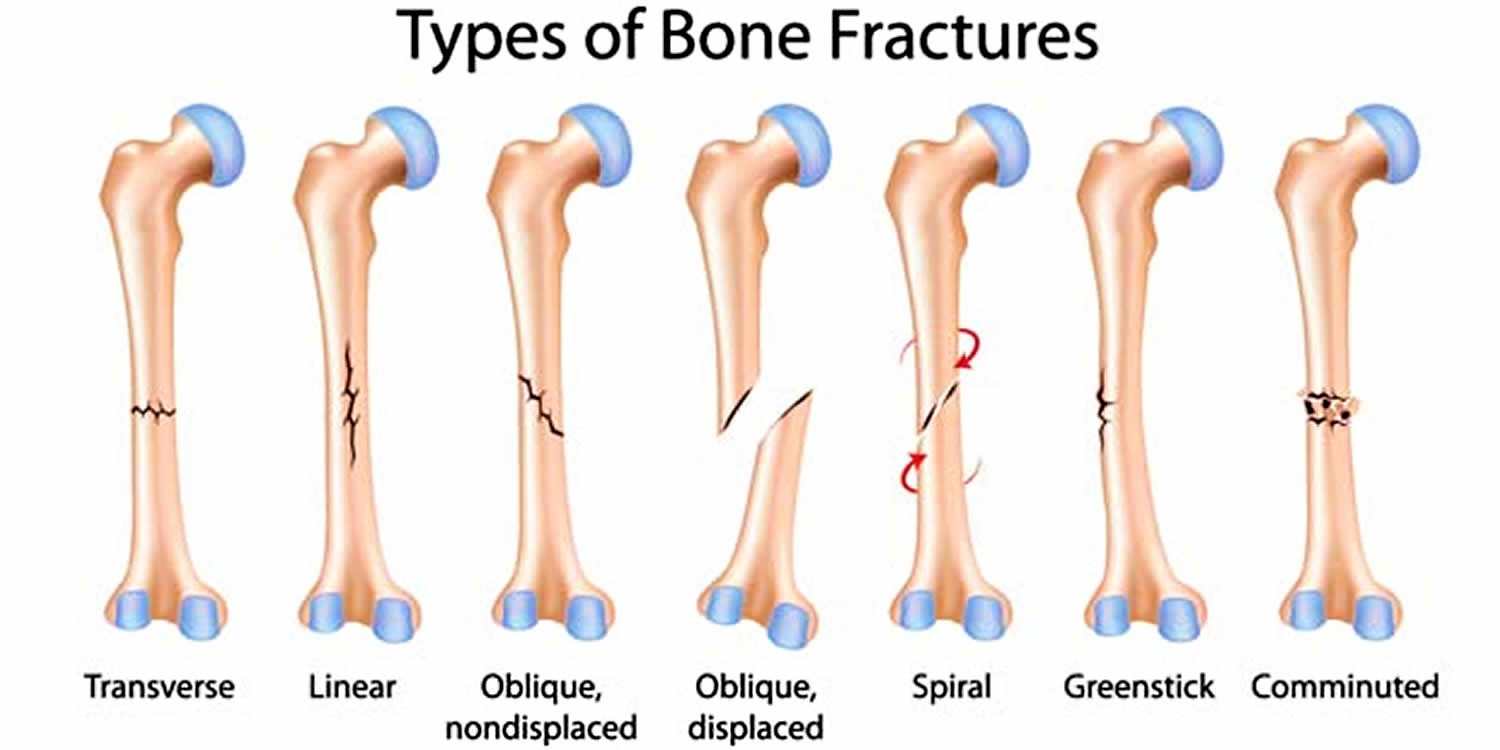
Long bones may suffer from different types of fractures.
Doctors describe fractures to other doctors using classification systems.
- The location of the fracture (the tibial shaft is divided into thirds: distal, middle, and proximal)
- The pattern of the fracture (for example, the bone can break in different directions, such as crosswise, lengthwise, or in the middle)
- Whether the skin and muscle over the bone is torn by the injury (open fracture)
Simple fracture – a fracture which does not break the skin.
Greenstick fracture – a fracture in which one side of the bone is broken while the other is bent.
Spiral fracture occurs when the bone is twisted apart.
Comminuted fracture which occurs when the bone is splintered or crushed.
Transverse fracture is characterized by a horizontal maxillary fracture.
Figure 2. Long bone fracture types
Greenstick fracture
A greenstick fracture occurs when a bone bends and cracks, instead of breaking completely into separate pieces. Greenstick fracture looks similar to what happens when you try to break a small, “green” branch on a tree.
Most greenstick fractures occur in children younger than 10 years of age. This type of broken bone most commonly occurs in children because their bones are softer and more flexible than are the bones of adults.
Even mild greenstick fractures are usually immobilized in a cast. In addition to holding the cracked pieces of the bone together so they can heal, a cast can help prevent the bone from breaking all the way through if the child falls on it again.
Greenstick fracture causes
Childhood fractures most commonly occur with a fall. Arm fractures are more common than leg fractures, since the common reaction is to throw out your arms to catch yourself when you fall.
Risk factors for greenstick fracture
The risk of greenstick fractures is higher in young children because their bones are softer and more flexible than adult bones. In a greenstick fracture, the bone bends and cracks instead of breaking into separate pieces. Most greenstick fractures occur in children under age 10.
Greenstick fracture symptoms
Signs and symptoms will vary, depending on the severity of the greenstick fracture. Mild fractures might be mistaken for sprains or bruises. More-severe greenstick fractures may cause an obvious deformity, accompanied by significant pain and swelling.
Contact your doctor if your child has persistent pain in an injured limb. Seek immediate medical attention if a child is unable to bear weight or if there is obvious pain, deformity and swelling.
Greenstick fracture diagnosis
During the physical exam, your doctor will inspect the affected area for tenderness, swelling, deformity, numbness or an open wound. Your child may be asked to move his or her fingers into certain patterns or motions to check for nerve damage. Your doctor may also examine the joints above and below the fracture.
X-rays can reveal most greenstick fractures. Your doctor may want to take X-rays of the uninjured limb, for comparison purposes.
Greenstick fracture treatment
Depending on the severity of the greenstick fracture, the doctor may need to straighten the bone manually so it will heal properly. Your child will receive pain medication and possibly sedation drugs for this procedure.
Greenstick fractures have a high risk of breaking completely through the bone, so most of these types of fractures are immobilized in a cast during healing.
On occasion, your doctor may decide that a removable splint could work just as well, particularly if the break is mostly healed. The benefit of a splint is that your child might be able to take it off briefly for a bath or shower.
X-rays are required in a few weeks to make sure the fracture is healing properly, to check the alignment of the bone, and to determine when a cast is no longer needed. Most greenstick fractures require four to eight weeks for complete healing, depending on the break and the age of the child.
Spiral fracture
Spiral fracture is caused by a twisting force. The fracture line encircles the shaft like the stripes on a candy cane.
Comminuted fracture
Comminuted fractureis where the bone breaks into three or more pieces.
Open fracture or compound fracture
If a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the broken bone, the fracture is called an open or compound fracture. Open fractures often involve much more damage to the surrounding muscles, tendons, and ligaments. They have a higher risk for complications—especially infections—and take a longer time to heal.
Transverse fracture
In this transverse fracture, the break is a straight horizontal line going across the tibial shaft.
Oblique fracture
Oblique fracture has an angled line across the shaft.