Contents
What is McArdle disease
McArdle disease also known as glycogen storage disease type 5, is a very rare inherited disorder caused by an inability to break down a complex sugar called glycogen in muscle cells. A lack of glycogen breakdown interferes with the function of muscle cells. Twelve different types of glycogen storage disease have been described (type 0, 1-7, 9, 11-13), which result from defects in glycogen synthesis and breakdown principally in the muscle and liver, although other tissues can also be affected.
McArdle disease is caused by the lack of the muscle glycogen phosphorylase (myophosphorylase) enzyme. Although symptoms typically begin during the first ten years of life, the age of diagnosis can vary significantly. The characteristic symptoms of McArdle disease are exercise intolerance, myalgia (muscle pain), muscle stiffness and contractures, quick fatigue as well as hyperCKemia and myoglobinuria (dark, burgundy-colored urine due to the presence of myoglobin, a protein found in heart and muscles). People with McArdle disease typically experience fatigue, muscle pain, and cramps during the first few minutes of exercise (exercise intolerance). Exercise such as weight lifting or jogging usually triggers these symptoms in affected individuals. These symptoms are usually caused by isometric or uninterrupted aerobic exercise. The discomfort is generally alleviated with rest. If individuals rest after brief exercise and wait for their pain to go away, they can usually resume exercising with little or no discomfort (a characteristic phenomenon known as “second wind”).
Prolonged or intense exercise can cause muscle damage in people with McArdle disease. About half of people with McArdle disease experience breakdown of muscle tissue (rhabdomyolysis). In severe episodes, the destruction of muscle tissue releases a protein called myoglobin, which is filtered through the kidneys and released in the urine (myoglobinuria). Myoglobin causes the urine to be red or brown. This protein can also damage the kidneys, and it is estimated that half of those individuals with McArdle disease who have myoglobinuria will develop life-threatening kidney failure.
The signs and symptoms of McArdle disease can vary significantly in affected individuals. The features of this condition typically begin in a person’s teens or twenties, but they can appear anytime from infancy to adulthood. In most people with McArdle disease, the muscle weakness worsens over time; however, in about one-third of affected individuals, the muscle weakness is stable. Some people with McArdle disease experience mild symptoms such as poor stamina; others do not experience any symptoms.
McArdle disease is a very rare disorder with only a few hundred cases reported in the medical literature; however, its prevalence is unknown. In the Dallas-Fort Worth area of Texas, where the prevalence of McArdle disease has been studied, the condition is estimated to affect 1 in 100,000 individuals and the prevalence in Spain has been reported at 1:170,000. Some researchers believe that it is probably under-diagnosed because of the mildness of the symptoms. The neonatal, early-onset and very late-onset forms are even rarer.
Currently, there is no cure for McArdle disease. To manage McArdle disease, medical professionals suggest that people affected avoid intense exercise and a completely inactive lifestyle, but do engage in consistent, reasonable aerobic exercise.
McArdle disease causes
McArdle disease is caused by mutations in the PYGM gene (glycogen phosphorylase, muscle form) that codes for the myophosphorylase enzyme. The PYGM gene is located on chromosome 11 at 11q13. The myophosphorylase enzyme is found only in muscle cells, where it breaks down glycogen into a simpler sugar called glucose-1-phosphate. Additional steps convert glucose-1-phosphate into glucose, a simple sugar that is the main energy source for most cells.
PYGM gene mutations prevent myophosphorylase from breaking down glycogen effectively. As a result, muscle cells cannot produce enough energy, so muscles become easily fatigued. Reduced energy production in muscle cells leads to the major features of McArdle disease.
McArdle disease inheritance pattern
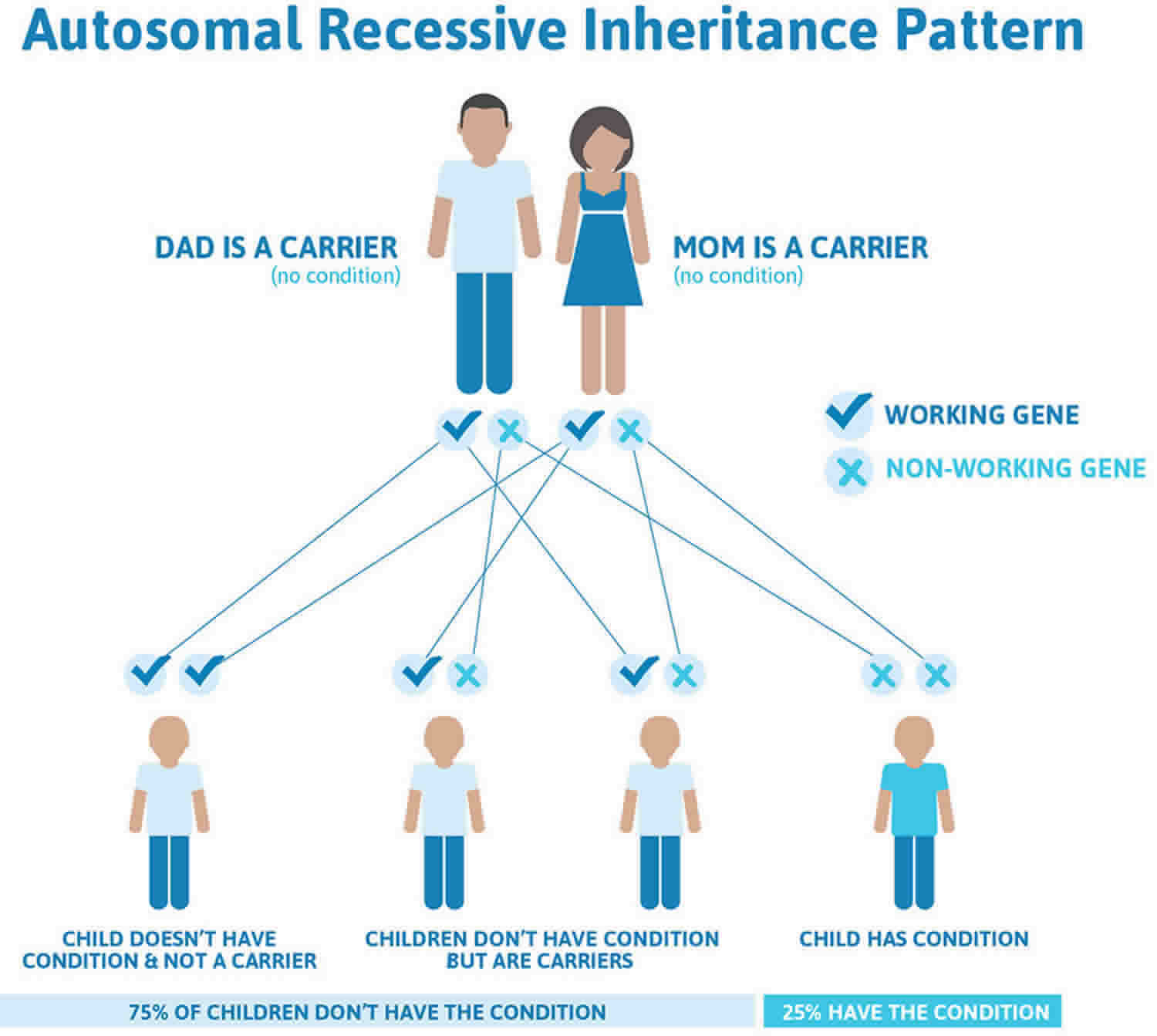
McArdle disease is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 1. McArdle disease autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
McArdle disease symptoms
McArdle disease is characterized by exercise intolerance. This typically consists in acute crises of early fatigue and muscle stiffness and contractures, especially at the start of the exercise, that usually disappear if exercise is stopped or the intensity is reduced. Symptoms usually present within the first ten years of life, but there is a wide range of clinical onset and severity. Some McArdle disease patients have mild symptoms while another form progresses quickly and is apparent shortly after the person is born. Progressively weak muscles, in some individuals, do not manifest until the age of sixty to seventy years old.
Muscles of affected patients usually function normally while at rest or during moderate exercise. Only during strenuous exercise do severe muscle cramps occur. Exercising in the presence of severe pain results in muscle damage (rhabdomyolysis) and myoglobinuria in about 50% of those affected. The myoglobin protein can also damage the kidneys and lead to develop life-threatening kidney failure if not treated promptly.
A unique feature of the disease is the so-called “second wind” phenomenon, which most patients refers to as the ability to resume dynamic, large mass exercise, if they take a brief rest upon the appearance of premature fatigue early in exercise. This “second wind” phenomenon is present in approximately ~90% of people with McArdle disease.
A severity scale has been developed to describe the variation in clinical features:
- Type 0= asymptomatic or virtually asymptomatic (mild exercise intolerance but not functional limitation in any daily life activity).
- Type 1= exercise intolerance, contractures, myalgia, and limitation of acute strenuous exercise and occasionally in daily life activities; no record of myoglobinuria, no muscle wasting or weakness.
- Type 2= same as 1 and also recurrent exertional myoglobinuria, moderate restriction in exercise and limitation in daily life activities.
- Type 3= same as 2 and also fixed muscle weakness, with or without wasting, and severe limitations on exercise and most daily life activities.
McArdle disease diagnosis
Traditionally, diagnosis has been based on the inability of the patient to produce lactate during a forearm exercise test, lack of muscle glycogen phosphorylase on muscle biopsy (generally from vastus lateralis or biceps brachialis muscles), and more recently DNA studies to look for mutations in the PYGM gene. Additionally, the measure of plasma CK (creatine kinase) levels as well as the determination of the “second wind” phenomenon help to precisely provide a correct diagnosis. Currently, the diagnosis of McArdle disease is mainly based on the molecular analysis of DNA obtained from blood samples. This is a minimally invasive method, and given the accumulated knowledge on the genetics of this disease in different populations, it can be highly targeted. Gene sequencing after PCR amplification is the most frequently utilized technique for screening the different PYGM mutations.
McArdle disease treatment
At present there is no curative therapy for McArdle disease, but several different therapeutic approaches have been utilized.
Nutritional supplements and drugs
No significant beneficial effects have been reported in McArdle disease patients receiving branched chain aminoacids, depot glucagon, dantrolene sodium, verapamil, vitamin B6 or high-dose oral ribose. More controversial results have been obtained for creatine supplementation; low dose supplementation (60 mg/kg/day for 4 weeks) reduced muscle complaints in five of nine patients tested, but higher doses (150 mg/kg/day) actually increased exercise induced myalgia.
Increasing copies of the D allele at the ACE locus is associated with disease severity, especially in women; the preliminary results of a study based on this observation suggest that treatment with the ACE inhibitor ramipril is beneficial 1.
However, a beneficial intervention for alleviating exercise intolerance symptoms and protecting the muscle from rhabdomyolysis consists of ensuring that sufficient blood glucose is constantly made available to patients during daytime. This can be achieved by adopting a diet with high proportion (65%) of complex carbohydrates (as those found in vegetables, fruit, cereals, pasta and rice) and low fat (20%). A different strategy could be the ingestion of simple carbohydrates before engaging in a strenuous exercise (75 g of sucrose 30-40 min pre-exercise).
Exercise interventions
McArdle disease patients adapt favorably to regular exercise, with a significant increase in VO2 peak after supervised aerobic exercise. In fact, it has been shown that physically active patients are much more likely to improve their clinical course over a four year period compared with their inactive peers.
Carefully supervised, regular, aerobic exercise of low-to-moderate intensity is a safe, recommended therapeutic option.
McArdle disease diet
At present, the most beneficial intervention for patients with McArdle disease, in combination with aerobic conditioning, is ensuring that sufficient blood glucose is constantly available to patients’ working muscles during the daytime 2. This is achieved by adopting a diet with a high proportion (65%) of complex carbohydrates (such as those found in vegetables, fruits, cereals, bread, pasta, and rice) and a low proportion (20%) of fat. In addition, the ingestion of simple carbohydrates (20–40 g of glucose or fructose in adults and 20 g in children) approximately 5 minutes before engaging in strenuous exercise, such as brisk walking or physical education in younger patients, can be helpful. In general, vigorous dynamic exercise should be performed only by the more fit patients and should be combined with pre-exercise carbohydrate ingestion. Very intense exercises, particularly those involving high loads on low muscle mass, are strongly discouraged in these patients.
Another problem is that glucose that isn’t immediately burned up for energy can get stored as glycogen, which the person with a glycogen-processing disorder can’t use.
Even though McArdle patients can’t break down glycogen in muscle, they can do so in the liver, and the resulting glucose can then travel to the muscles through the circulation.
Until a definitive cure is found, patients can benefit from adopting a diet rich in complex carbohydrates and ingesting simple carbohydrates before strenuous exercise.
- Randomized, placebo-controlled, double-blind pilot trial of ramipril in McArdle’s disease. Martinuzzi A, Liava A, Trevisi E, Frare M, Tonon C, Malucelli E, Manners D, Kemp GJ, Testa C, Barbiroli B, Lodi R. Muscle Nerve. 2008 Mar; 37(3):350-7.[↩]
- Leite A, Oliveira N, Rocha M. McArdle disease: a case report and review. Int Med Case Rep J. 2012;5:1–4. Published 2012 Jan 20. doi:10.2147/IMCRJ.S28664 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3658246/[↩]