Contents
- MALS syndrome
- Median arcuate ligament syndrome causes
- Median arcuate ligament syndrome symptoms
- Median arcuate ligament syndrome complications
- Median arcuate ligament syndrome differential diagnosis
- Median arcuate ligament syndrome diagnosis
- Median arcuate ligament syndrome treatment
- Median arcuate ligament syndrome prognosis
MALS syndrome
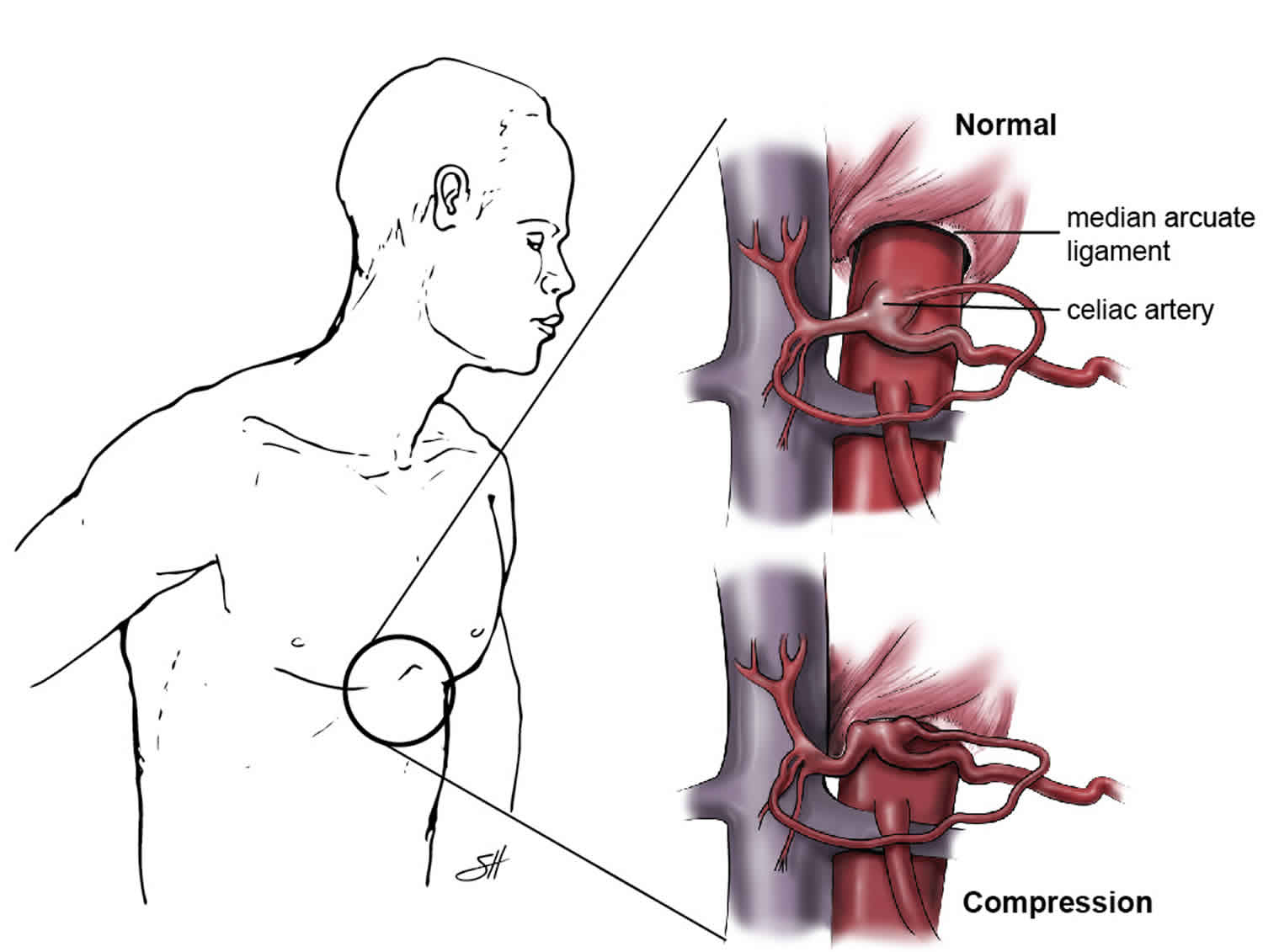
MALS syndrome which is short for “median arcuate ligament syndrome” and also known as “celiac artery compression syndrome”, “celiac artery compression”, “celiac axis syndrome” or “Dunbar syndrome”, is a rare medical condition caused by the median arcuate ligament (MAL) of the diaphragm (arc-shaped fibrous muscular band in the chest area) directly compressing the celiac artery (Figure 1) 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15. Ischemia due to reduced blood flow through the celiac artery and/or neuropathic pain resulting from celiac ganglion compression may result in a range of gastrointestinal symptoms, including nausea, postprandial discomfort, and weight loss. Individuals with MALS syndrome present with signs and symptoms of foregut ischemia, including abdominal pain during body exercise caused by an intermittent visceral ischemia or after meal epigastric pain, nausea, vomiting, and unintentional weight loss 11.
Median arcuate ligament syndrome (MALS) is a rare condition with a reported incidence of 2 per 100,000 population 6. A considerable number of median arcuate ligamentum syndrome patients are overlooked in the diagnosis of patients complaining of abdominal pain 16. Median arcuate ligament syndrome (MALS) is commonly seen in young women between the ages of 30 to 50 years. It has a female to male ratio of 4:1 6. Median arcuate ligament syndrome (MALS) has also been reported in children. The incidence of radiographic compression of the celiac axis has been reported to be between 10% to 24% in some populations; note that symptomatic celiac artery compression exists in a smaller percentage of the population 17.
The location of the median arcuate ligament (MAL) and celiac artery varies slightly from person to person. Typically, the median arcuate ligament (MAL) runs across the largest blood vessel in the body (the aorta). It sits above the celiac artery (see Figure 1). But sometimes the median arcuate ligament (MAL) or the celiac artery may be out of place, causing MALS. The celiac artery develops fibrotic changes in its wall due to the recurrent compression from the median arcuate ligament. The median arcuate ligament (MAL) may also put pressure on the network of nerves surrounding the celiac artery called the celiac plexus (celiac ganglia). The mechanism of the celiac artery compression and its anatomical correlates have been incompletely delineated. However, it has been hypothesized that in 10% to 24% of the population, the MAL (median arcuate ligament) crosses the aorta at an atypically inferior anatomic level and subsequently results in compression by the MAL 18. It is also hypothesized that MALS-related pain is both neuropathic and due to vascular compression in cause; namely, foregut ischemia pain results from decreased blood flow and chronic compression, as well as overstimulation of the celiac plexus (celiac ganglia) contributing to sympathetic neuropathic pain 5. The celiac ganglia are collateral sympathetic ganglia that lie adjacent to the celiac trunk artery along its anterolateral sides 19. The celiac ganglia are the largest sympathetic ganglia in the body, and provide the sympathetic innervation to the foregut organs 19. While the celiac ganglia are typically paired, there can be up to five celiac ganglia, all of which are connected via a complex neural network, the celiac plexus, receiving preganglionic sympathetic fibers from Thoracic T5 to T12 19. Since the celiac ganglia are responsible for sympathetic innervation to, and visceral pain from, the foregut, impingement of the celiac ganglia can result in a range of symptoms including radiating foregut discomfort, nausea, vomiting, epigastric fullness, and delayed gastric emptying 5. Therefore, the MALS symptom complex may include a range of expressions resulting from both vascular ischemia and/or neuropathic pain and overstimulation 4.
In patients with median arcuate ligament syndrome (MALS), the celiac artery is compressed by the median arcuate ligament (MAL) with expiration 7. With inspiration, the celiac artery descends in the abdominal cavity, resulting in a more vertical orientation of the celiac artery, which often relieves the compression 7. With the patient in the upright position, the celiac artery descends farther into the abdominal cavity, which increases the vertical orientation of the celiac artery even more and further relieves compression caused by the median arcuate ligament 20.
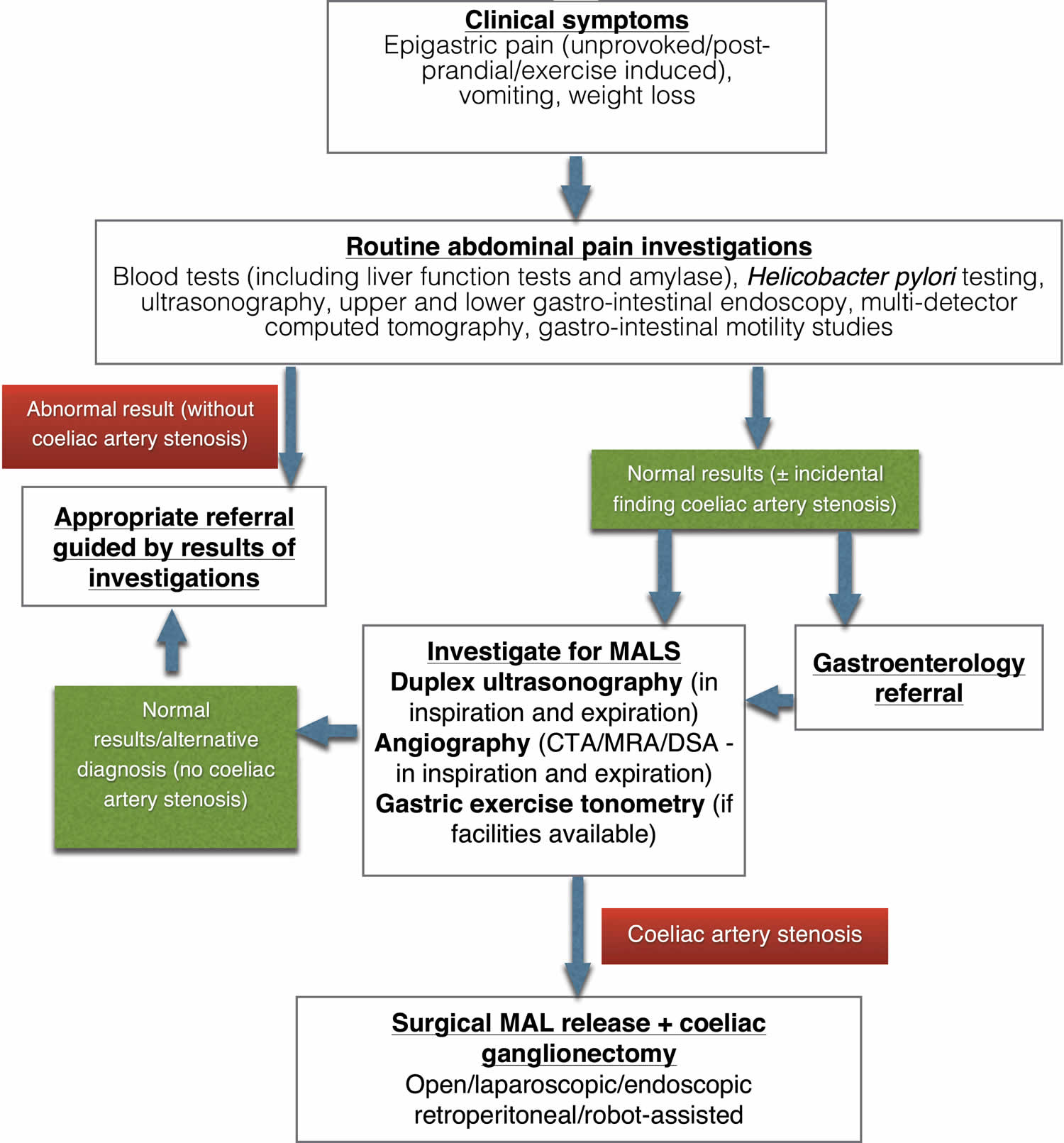
Median arcuate ligament syndrome (MALS) is an uncommon cause of after meal abdominal pain and it is a diagnosis of exclusion. Patients with MALS often undergo a multidisciplinary evaluation with several specialties including gastroenterology, vascular surgery, general surgery, cardiology, anesthesia pain management, interventional radiology, and psychological assessment. The evaluation includes several gastroenterology tests including upper endoscopy and colonoscopy, motility studies, gastric emptying tests, and serology studies. Not all patients require all the above-mentioned tests, but an expert opinion of a gastroenterologist is critical to guide the diagnostic work-up and to establish that MALS is the most likely cause of the pain. A surgical consultation with an expert on MALS treatment is needed once the diagnosis is contemplated. Among patients who are on narcotic pain medication, anesthesia pain clinic consultation and a therapeutic plan to decrease or discontinue the use of narcotics is important prior to proceeding with invasive treatment.
The typical MALS patient presentation is a young, thin woman with symptoms of nausea, vomiting, early satiety, difficulty gaining weight, postprandial epigastric pain, and an abdominal bruit 21, 22. Further workup with Doppler ultrasound and/or computed tomographic (CT-scan) imaging is required for definitive diagnosis 23, 24, 25, 26.
Celiac artery compression syndrome treatment options include open, laparoscopic or robot-assisted surgery to release the median arcuate ligament (MAL) and open vascular reconstruction restore blood flow through the celiac artery 8. Indication for surgery is established in these otherwise healthy, symptomatic patients by showing a baseline celiac velocity >200 cm/m² and stenosis of the celiac artery on CT-scan or MR angiography 21, 22. Endovascular treatment is currently used only as adjuvant procedure after surgical approach, in refractory cases with residual stenosis of celiac artery 8.
Figure 1. MALS syndrome
Footnotes: Diagrammatic representation of celiac artery (celiac trunk) anatomy, showing: (A) The median arcuate ligament (MAL) compressing the celiac trunk as in median arcuate ligament syndrome; and (B) normal anatomical condition. The diaphragmatic crura (legs of the diaphragm) arise from the anterior surface of the L1 to L4 vertebral bodies on the right and the first two or three lumbar vertebral bodies on the left 27. In addition, the crura arise from the intervertebral disks and anterior longitudinal ligament 19. The crura pass superior and anterior to surround the aortic opening and the crura of the diaphragm are united in the midline by a tendinous band of fascia called the median arcuate ligament (MAL). The aortic hiatus, an opening between the diaphragm and vertebral column around T12, permits passage of the abdominal aorta through the diaphragm 19. However, in 10% to 24% of the population, the median arcuate ligament (MAL) may be lower and therefore cross over the proximal portion of the celiac axis, causing a characteristic indentation 27. Simultaneous to the development of the diaphragm, the celiac artery (celiac trunk), superior mesenteric artery (SMA), and inferior mesenteric artery (IMA) each form when the respective pair of developing segmental arteries converges at the midline of the abdominal aorta 28. The celiac artery (celiac trunk) develops to provide arterial supply to the foregut, the superior mesenteric artery (SMA) to the midgut, and inferior mesenteric artery (IMA) to the hindgut. As the gut tube develops, the origins of these three unpaired visceral branches migrate caudally until they reach their final vertebral level around the end of month two 28. The most common vertebral positions reported in adults are: T12 for the celiac artery (celiac trunk), L1 for superior mesenteric artery (SMA), and L3 for inferior mesenteric artery (IMA) 19. Although the superior mesenteric artery (SMA) is commonly described as originating 1.0 cm inferior to the celiac artery (celiac trunk), several studies have demonstrated the celiac artery (celiac trunk) and superior mesenteric artery (SMA) to be immediately adjacent in 22–58% of cases 29, 30, 31. It is theorized that the close proximity of the two arteries may be evidence of celiac artery (celiac trunk) compression by the MAL. In addition, one study found that up to 37% of cadavers had evidence of kinking of the celiac artery (celiac trunk) 30. A different study on fresh cadaveric specimens demonstrated that the celiac artery (celiac trunk) origin was at or above the MAL in 33% of subjects 32. However, it was unclear whether the celiac artery (celiac trunk) originated more superiorly than normal, if the diaphragm extended further inferiorly, or if there was a combination of the two factors. A final possible indicator of celiac artery (celiac trunk) compression is the celiac artery angle of origination. It has been postulated that if there is an acute deviation of the left and right diaphragmatic crura, the MAL may cause constriction of the celiac artery (celiac trunk) 33. The aortic hiatus, bounded by the median arcuate ligament (MAL), frequently approximates the vertebral level of the celiac artery (celiac trunk), leaving little space between them. In some cases, the median arcuate ligament (MAL) may even overlap the celiac artery (celiac trunk), a condition which may result in impingement of the celiac artery (celiac trunk).
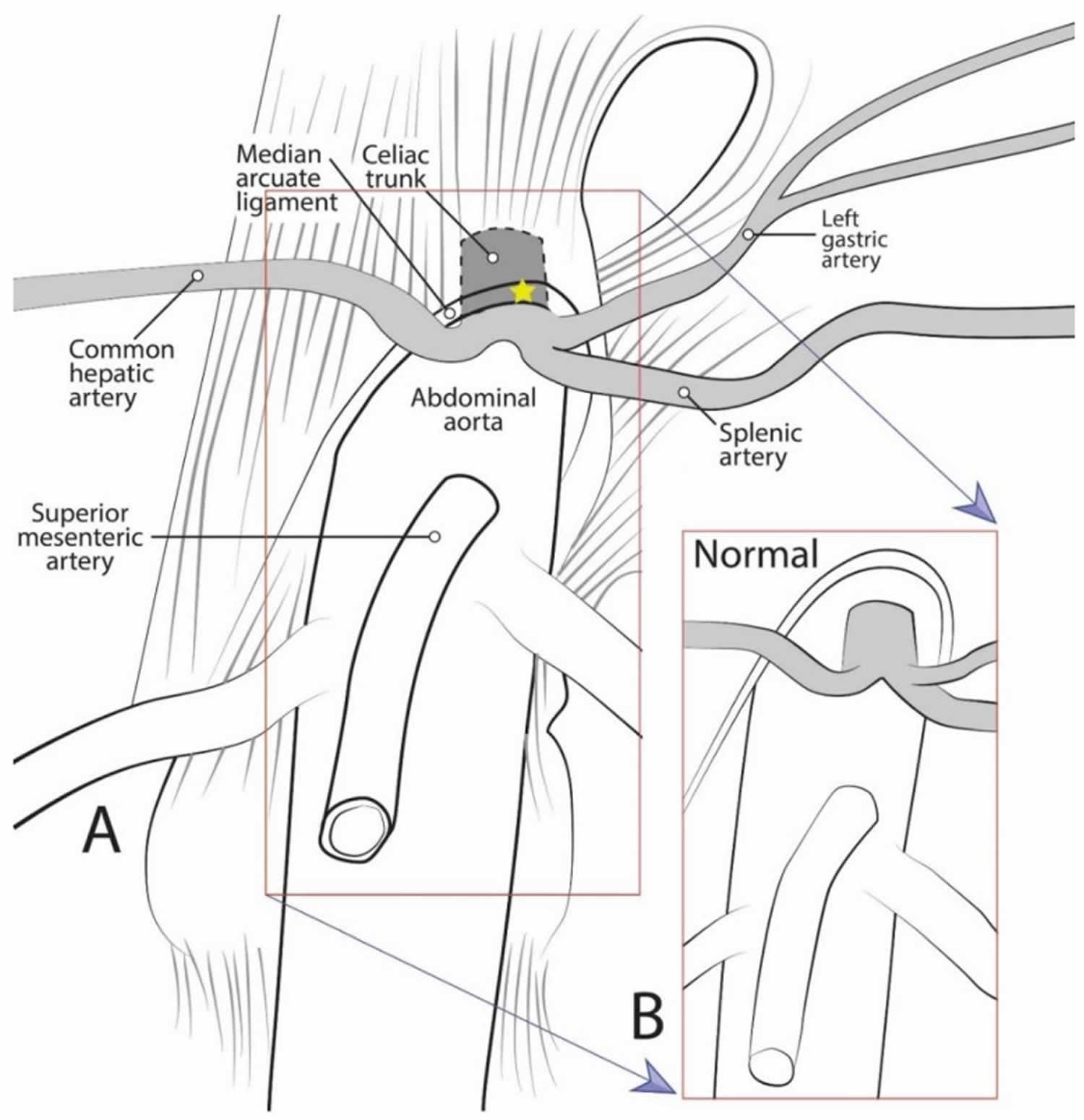
[Source 4 ]Figure 2. Median arcuate ligament syndrome CT scan
Footnote: A 31-year-old woman presented with several episodes of chest pain, palpitations, exercise intolerance, nausea, vertigo, tremors and hypertension. She had a history of chronic and recurrent abdominal pain, especially after meals. Gastrointestinal tract pathologies were ruled out by ultrasonography, gastroscopy and colonoscopy. Abdominal computed tomography (CT) revealed high grade stenosis (>80%) of the celiac artery by the median arcuate ligament, 10mm from its origin from the aorta with poststenotic dilation (arrow). The patient was subsequently diagnosed with median arcuate ligament syndrome and admitted to our department for surgical treatment.
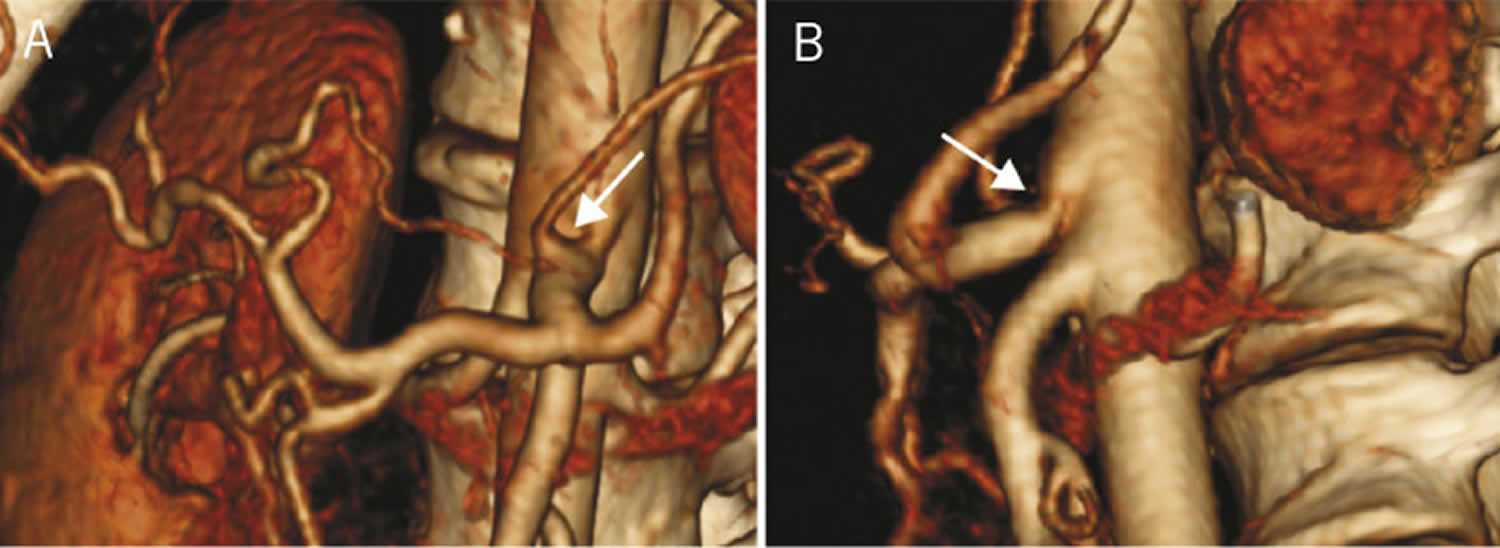
[Source 10 ]Figure 3. Median arcuate ligament syndrome 3D CT scan
Footnote: Three-dimensional computed tomography reconstruction showing anterior (A) and lateral (B) views of compression of celiac trunk by the median arcuate ligament with poststenotic dilation (arrow)
[Source 10 ]Figure 4. Median arcuate ligament syndrome diagnostic and treatment algorithm
[Source 11 ]There are many different causes of stomach pain. If your stomach pain continues despite home care, see your doctor. You’ll need a complete physical exam and tests to determine the specific cause of your stomach pain.
If your stomach pain is severe and activity or movement makes it worse, see your doctor immediately. Seek immediate medical help if your stomach pain occurs with:
- Bloody stools or black stools (melena) that occur as a result of gastrointestinal bleeding
- Fever
- Nausea and vomiting that doesn’t go away
- Severe tenderness when you touch your belly area
- Swelling of the belly area
- Yellowing of the skin or whites of the eyes (jaundice)
Sometimes upper stomach pain can be confused with chest pain. Sometimes it can be due to a heart attack. Get emergency help or call your local emergency services number if you have chest or upper stomach pain with or without any of the following symptoms:
- Pressure, fullness or tightness in your chest
- Crushing or searing pain that spreads to your jaw, neck, shoulders, and one or both arms
- Pain that lasts more than a few minutes or gets worse with activity
- Shortness of breath
- Cold sweats
- Dizziness or weakness
- Nausea or vomiting
Median arcuate ligament syndrome causes
Doctors aren’t exactly sure what causes median arcuate ligament syndrome (MALS). The causes and diagnosis of MALS are a subject of controversy because the anatomic compression of the celiac artery by the median arcuate ligament (MAL) can also be seen in asymptomatic patients. In other words, every patient with this anatomic compression does not develop symptoms 5, 6, 2, 34, 35, 36, 30, 29. Median arcuate ligament syndrome (MALS) is caused when the median arcuate ligament (MAL) descends lower or the celiac artery is anatomically positioned higher on the aorta causing the median arcuate ligament (MAL) to cross over and compress the celiac artery and surrounding tissue which can include the celiac plexus nerves. As of right now there are multiple theories of why MALS occurs within the body. Some of those theories are that this structural anomaly could be congenital, meaning from birth or develop after spinal surgery, abdominal surgery or due to abdominal trauma. Most contemporary literature supports the theory that compression of the celiac artery by the median arcuate ligament (MAL) leads to relative gut ischemia, causing the recurrent abdominal symptoms 37, 38, 39. An alternative “neurogenic” theory suggests that the median arcuate ligament compresses the neural tissue surrounding the celiac artery origin, leading to neuropathic pain 40, 41. During exercise, vascular resistance of the celiac and mesenteric arteries increases, which would worsens ischemia and produce postexertional pain 42. Diaphragmatic movements may also irritate the neural tissue surrounding the celiac artery. Postexertional pain may be a significant outcome predictor because it is a marker for functionally significant vascular compromise caused by compression from the median arcuate ligament that is otherwise asymptomatic.
While some degree of celiac artery and surrounding tissue compression can be seen in the general population without symptoms, these people should be followed closely as people can become symptomatic at any age. Compromised blood flow and inflammation results in changes in oxygen levels (hypoxia/HIF factor and oxidative stress) and nutrients to the abdominal organs and nerves which can result in consequential damage. Nerve irritation and or damage can cause disturbances with myenteric electrical activity to the stomach resulting in the MALS symptoms.
The vast majority of patients with partial celiac artery (celiac trunk) compression are asymptomatic because collateral circulation typically prevents the development of symptoms 43. If the compression is severe and symptomatic, however, a diagnosis of MALS is considered 4.
Although the superior mesenteric artery (SMA) is commonly described as originating 1.0 cm inferior to the celiac artery (celiac trunk), several studies have demonstrated the celiac artery (celiac trunk) and superior mesenteric artery (SMA) to be immediately adjacent in 22–58% of cases 29, 30, 31. It is theorized that the close proximity of the two arteries may be evidence of celiac artery (celiac trunk) compression by the MAL. In addition, one study found that up to 37% of cadavers had evidence of kinking of the celiac artery (celiac trunk) 30. A different study on fresh cadaveric specimens demonstrated that the celiac artery (celiac trunk) origin was at or above the MAL in 33% of subjects 32. However, it was unclear whether the celiac artery (celiac trunk) originated more superiorly than normal, if the diaphragm extended further inferiorly, or if there was a combination of the two factors. A final possible indicator of celiac artery (celiac trunk) compression is the celiac artery angle of origination. It has been theorized that if there is an acute deviation of the left and right diaphragmatic crura, the MAL may cause constriction of the celiac artery (celiac trunk) 33.
Risk factors for median arcuate ligament syndrome
Because the cause of MALS is poorly understood, the risk factors for the syndrome are unclear. MALS has been seen in children, even twins, which might mean genetics plays a role.
Some people have developed MALS after pancreatic surgery and blunt injury to the upper stomach area.
Median arcuate ligament syndrome symptoms
Median arcuate ligament syndrome symptoms varies and is case specific to each person’s symptoms 37, 44. Often, people with compression of the celiac artery don’t have any symptoms. However, individuals with median arcuate ligament syndrome (MALS) can have long-term (chronic) abdominal pain that can range from intermittent mild to chronic debilitating that are triggered after eating or exercise and often with nausea, vomiting, and unintentional weight loss. These symptoms may be due to a lack of blood flow through the celiac artery or compression on celiac nerves in the area.
Symptoms of MALS include:
- Pain in the upper middle stomach area, which may go away when leaning forward
- Stomach pain after eating, exercising or changing body position
- Nausea and vomiting
- Bloating
- Diarrhea
- Fear of eating food due to pain, leading to significant weight loss — usually greater than 20 pounds (9.1 kilograms)
MALS pain may make it difficult for you to eat, exercise, sleep and do everyday tasks.
Median arcuate ligament syndrome complications
MALS complications include long-term pain, especially after meals. The pain can lead to a fear of eating and significant weight loss. The pain and related depression or anxiety can greatly impact quality of life. MALS symptoms may be vague and can mimic other conditions. It may take some time to get an accurate diagnosis.
Median arcuate ligament syndrome differential diagnosis
Celiac artery compression syndrome may mimic several other medical conditions posing a diagnostic challenge for the physician. It can be mistaken for other conditions that can cause post-prandial pain such as gallbladder disease including biliary dyskinesia and cholecystitis. Other intra-abdominal pathologies such as appendicitis, colorectal malignancy, hepatitis, gastroparesis and gastritis/peptic ulcer disease can also mimic celiac artery compression syndrome. Furthermore, chronic mesenteric ischemia secondary to atherosclerotic disease may have a similar presentation as celiac artery compression syndrome. Some of these conditions may co-exist simultaneously as well. Presence for abdominal bruit on examination may lead to consideration for other entities such as renal artery stenosis or arteriovenous malformations.
Some common misdiagnoses of MALS include:
- Gastroesophageal reflux disease (GERD): MALS can cause abdominal pain and discomfort that may be mistaken for GERD, a more common condition in which stomach acid irritates the esophagus.
- Irritable bowel syndrome (IBS): MALS patients often experience abdominal pain, bloating, and changes in bowel habits, which can be similar to the symptoms of IBS.
- Functional dyspepsia: This condition is characterized by chronic or recurrent pain in the upper abdomen, which can be similar to the pain experienced by MALS patients.
- Peptic ulcer disease: Peptic ulcers, which are sores in the lining of the stomach or duodenum, can cause abdominal pain similar to that experienced in MALS.
- Gallbladder disease: MALS symptoms can be mistaken for gallbladder issues, such as gallstones, which can also cause abdominal pain and discomfort.
- Pancreatitis: Inflammation of the pancreas can cause abdominal pain and other symptoms that may be mistaken for MALS.
- Splanchnic artery syndrome: This rare condition occurs when blood flow to the digestive organs is reduced, leading to symptoms that can be similar to MALS.
- Pelvic congestion syndrome: This condition, which involves the pooling of blood in pelvic veins, can cause chronic pelvic pain that may be mistaken for MALS.
- Nutcracker syndrome: This rare vascular disorder results from the compression of the left renal vein and can cause symptoms similar to MALS, including abdominal pain.
- Endometriosis: A condition in which endometrial tissue grows outside the uterus, endometriosis can cause pelvic pain and other symptoms that may be misinterpreted as MALS.
Median arcuate ligament syndrome diagnosis
There’s no specific test to diagnose median arcuate ligament syndrome. Median arcuate ligament syndrome (MALS) is still commonly considered a diagnosis of exclusion, so patients are usually sent for many tests most of which turn out “normal.” Unfortunately, MALS symptoms can all too often be dismissed by clinicians as non-specific, psychosomatic, or psychiatric, leaving many patients to suffer for months and years longer than they need to.
Your doctor will carefully examine you and ask questions about your symptoms and health history. Bloodwork and imaging tests help your doctor rule out other causes of your stomach pain.
Your doctor may hear a whooshing sound known as an abdominal bruit or thrill in the same epigastric area when listening to your upper stomach area with a stethoscope. The sound occurs when a blood vessel is blocked or narrowed.
Physical examination may activate tenderness in the epigastric region when palpated. Observations may include weight loss and malnutrition may be evident. Once MALS is suspected, a diagnostic workup is initiated to include various tests indicative of a diagnosis of MALS and rule out cardiovascular and gastrointestinal issues.
Tests used to rule out other conditions and diagnose MALS syndrome may include:
- Blood tests. These tests are done to check for problems with the liver, pancreas, kidneys and other parts of the body. A complete blood cell count shows the level of white and red blood cells. A high white blood cell count can mean there’s an infection.
- Ultrasound of the abdomen. This noninvasive test uses high-frequency sound waves to determine how blood is flowing through the blood vessels. It can show if the celiac artery is compressed, especially when breathing in and out deeply.
- Upper endoscopy called esophagogastroduodenoscopy (EGD). It’s done to view the esophagus, stomach and upper part of the small intestine (duodenum). During an EGD, the provider gently guides a long, flexible tube with a camera on the end (endoscope) down the throat after numbing medication is applied. If needed, the provider can take tissue samples (biopsy) during this procedure.
- Gastric emptying studies. Compression of the celiac artery can slow the rate of stomach emptying. Gastric emptying studies are done to determine how fast the stomach empties its contents. Slow or delayed gastric emptying may be from other medical conditions.
- Magnetic resonance imaging (MRI). An MRI uses powerful magnets and radio waves to produce detailed images of the body area being studied. Sometimes, dye is injected into a blood vessel to more clearly show how blood moves through the arteries and veins (magnetic resonance angiogram).
- Computerized tomography (CT) of the abdomen. A CT scan uses X-rays to create cross-sectional images of specific parts of the body. An abdominal CT scan can show if the celiac artery is narrowed or blocked. Sometimes a provider injects dye into a blood vessel to better see blood flow in the arteries and veins (CT angiogram).
Evaluation of other gastrointestinal disorders:
- HIDA (hepatobiliary iminodiacetic acid) scan of gallbladder
- Colonoscopy with biopsies
- 24-hour pH impedance probe
- Esophageal manometry
- Gastric tonometry
- Blood work panels
- Chest X-ray
- Electrocardiogram (ECG)
- Stool tests
Median arcuate ligament syndrome treatment
Surgery is the only treatment option for median arcuate ligament syndrome 45, 46. The most common procedure is called median arcuate ligament release or median arcuate ligament decompression. Celiac ganglionectomy rather than simple neurolysis is recommended as a means of addressing the neuropathic pain associated with median arcuate ligament syndrome. It’s usually done as an open surgery. Sometimes it can be done as a minimally invasive (laparoscopic or robotic) procedure. While you’re under general anesthesia, a surgeon splits the median arcuate ligament and network of nerves in the stomach area (celiac plexus). Doing so provides more room for the celiac artery. It restores blood flow and relieves pressure on the celiac nerves. In some cases, an omentum fat wrap may be used during surgery to assist with keeping the artery in the correct anatomical position and reduce scar tissue development. Persistent stenosis of the celiac artery after decompression may be appreciated with intraoperative handheld Doppler assessment, angiography, or duplex ultrasound. Ultrasound may be used to show restoration of normal blood flow which verifies adequate release of the artery at the time of surgery. This can be addressed with arterial reconstruction, examples of which include an aortoceliac bypass or a celiac artery patch angioplasty. Conversion from laparoscopic to open surgery is typically required for vascular reconstruction. Percutaneous transluminal angioplasty with or without stenting provides an adjunctive endovascular approach to revascularization of a persistent stenosis after MAL release.
A systematic review by Jimenez et al 46 found that the majority of patients treated with either open decompression or laparoscopic decompression of the median arcuate ligament syndrome experienced immediate postoperative pain relief. However, the laparoscopic approach is becoming more widely adopted owing to benefits such as shorter hospital stay, decreased time to feeding, smaller risk of postoperative complications,6 decreased blood loss, greater postoperative pain relief and better cosmetic outcomes 47, 48.
Some people with MALS syndrome may need an open surgery to repair or replace a blocked celiac artery and fully restore blood flow (revascularization).
For patients with recurrent or persistent abdominal pain re-evaluation for possible narrowing of the celiac artery either due to the formation of scar tissue within the celiac artery wall (intravascular web) or the integrity of the vessel wall has been compromised due to the mechanical compression. Additional procedures called co-surgical procedures may be pursued. These include celiac artery bypass (such as an aorto celiac or aorto hepatic bypass), superior mesenteric artery transposition, splenic artery transposition, balloon angioplasty with or without stenting, and para-spinal ganglion nerve blocks. Angioplasty with or without stenting is typically reserved for refractory cases where the first-line surgical therapies may have proven unsuccessful in providing symptomatic relief 49. Percutaneous Transluminal Angioplasty (PTA) or endovascular stent placement is not recommended before surgical division of the median arcuate ligament due to failure from the external compression crushing the stent which can add increased risk for artery wall damage and or dissection.
If you have MALS release surgery, you’ll usually stay in the hospital for 2 to 3 days. You’ll need an ultrasound about a month after surgery to confirm that blood flow through the celiac artery is fully restored. Several studies have shown that surgery to release the median arcuate ligament is safe, even in children with MALS. It often results in immediate pain relief and improves the person’s quality of life.
Median arcuate ligament syndrome prognosis
Following surgical intervention, about 65% to 87% of median arcuate ligament syndrome (MALS) patients report symptom relief 6, 40, 38, 50, 51, 52. Symptom relief has been reported to be immediate in some instances. In others, it may take up to a few months for the resolution of the pain 6. 41% of patients remained asymptomatic 3 to 11 years later 53. Although late recurrence is frequently seen, this seems to be milder than the presenting symptoms. In another study reported by Reilly et al. 39, patients with median arcuate ligament syndrome (MALS) were symptom-free with a mean of 9 years after surgery.
The presence of abdominal pain after exercise has been shown to be correlated with symptomatic improvement after surgery, while the presence of vomiting and unprovoked abdominal pain preoperatively has been shown to be associated with suboptimal surgical outcomes postoperatively 54. Patients who have a good response to a diagnostic celiac plexus block preoperatively also seem to report better symptom relief following surgical intervention 6. The presence of atherosclerotic risk factors may predict poorer outcomes postoperatively 54.
- Dunbar JD, Molnar W, Beman FF, Marable SA. Compression of the celiac trunk and abdominal angina. Am J Roentgenol Radium Ther Nucl Med. 1965 Nov;95(3):731-44. doi: 10.2214/ajr.95.3.731[↩]
- Goodall R, Langridge B, Onida S, Ellis M, Lane T, Davies AH. Median arcuate ligament syndrome. J Vasc Surg. 2020 Jun;71(6):2170-2176. doi: 10.1016/j.jvs.2019.11.012[↩][↩]
- Martinez JP, Hogan GJ. Mesenteric ischemia. Emerg Med Clin North Am. 2004 Nov;22(4):909-28. doi: 10.1016/j.emc.2004.05.002[↩]
- Dyches RP, Eaton KJ, Smith HF. The Roles of Celiac Trunk Angle and Vertebral Origin in Median Arcuate Ligament Syndrome. Diagnostics (Basel). 2020 Jan 31;10(2):76. doi: 10.3390/diagnostics10020076[↩][↩][↩][↩]
- Kim E.N., Lamb K., Relles D., Moudgill N., DiMuzio P.J., Eisenberg J.A. Median arcuate ligament syndrome—Review of this rare disease. JAMA Surg. 2016;151:471–477. doi: 10.1001/jamasurg.2016.0002[↩][↩][↩][↩]
- Saleem T, Katta S, Baril DT. Celiac Artery Compression Syndrome. [Updated 2023 Apr 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470601[↩][↩][↩][↩][↩][↩][↩]
- Lynch K. Celiac Artery Compression Syndrome: A Literature Review. Journal of Diagnostic Medical Sonography. 2014;30(3):143-148. doi:10.1177/8756479314528753[↩][↩][↩]
- Camacho N, Alves G, Bastos Gonçalves F, Abreu R, Ferreira R, Catarino J, Correia R, Bento R, Ferreira ME. Median Arcuate Ligament Syndrome – Literature Review and Case Report. Rev Port Cir Cardiotorac Vasc. 2017 Jul-Dec;24(3-4):111.[↩][↩][↩]
- Chaum M, Shouhed D, Kim S, Walts AE, Marchevsky AM. Clinico-pathologic findings in patients with median arcuate ligament syndrome (celiac artery compression syndrome). Ann Diagn Pathol. 2021 Jun;52:151732. https://doi.org/10.1016/j.anndiagpath.2021.151732[↩]
- Rubinkiewicz M, Ramakrishnan PK, Henry BM, Roy J, Budzynski A. Laparoscopic decompression as treatment for median arcuate ligament syndrome. Ann R Coll Surg Engl. 2015 Sep;97(6):e96-9. doi: 10.1308/rcsann.2015.0025[↩][↩][↩]
- Goodall R, Langridge B, Onida S, Ellis M, Lane T, Davies AH. Median arcuate ligament syndrome. J Vasc Surg. 2020 Jun;71(6):2170-2176. https://www.jvascsurg.org/article/S0741-5214(19)32642-4/fulltext[↩][↩][↩]
- Grotemeyer D, Duran M, Iskandar F, Blondin D, Nguyen K, Sandmann W. Median arcuate ligament syndrome: vascular surgical therapy and follow-up of 18 patients. Langenbecks Arch Surg. 2009 Nov;394(6):1085-92. doi: 10.1007/s00423-009-0509-5[↩]
- Balaban DH, Chen J, Lin Z, Tribble CG, McCallum RW. Median arcuate ligament syndrome: a possible cause of idiopathic gastroparesis. The American Journal of Gastroenterology. 1997 Mar;92(3):519-523.[↩]
- San Norberto EM, Romero A, Fidalgo-Domingos LA, García-Saiz I, Taylor J, Vaquero C. Laparoscopic treatment of median arcuate ligament syndrome: a systematic review. Int Angiol. 2019 Dec;38(6):474-483. doi: 10.23736/S0392-9590.19.04161-0[↩]
- What is MALS? https://www.malsfoundation.org/what-is-mals[↩]
- Kim JE, Rhee PL. Median arcuate ligamentum syndrome: Four case reports. World J Clin Cases. 2022 Feb 26;10(6):1991-1997. doi: 10.12998/wjcc.v10.i6.1991[↩]
- Koç M, Artaş H, Serhatlıoğlu S. The investigation of incidence and multidetector computed tomography findings of median arcuate ligament syndrome. Turk J Med Sci. 2018 Dec 12;48(6):1214-1218. doi: 10.3906/sag-1701-17[↩]
- Loukas M., Pinyard J., Vaid S., Kinsella C., Tariq A., Tubbs R.S. Clinical anatomy of celiac artery compression syndrome: A review. Clin. Anat. 2007;20:612–617. doi: 10.1002/ca.20473[↩]
- Moore K.L., Dalley A.F., Moore A. Clinically Oriented Anatomy. 8th ed. Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2017. pp. 1–1168.[↩][↩][↩][↩][↩][↩]
- Wolfman D, Bluth EI, Sossaman J. Median arcuate ligament syndrome. J Ultrasound Med. 2003 Dec;22(12):1377-80. doi: 10.7863/jum.2003.22.12.1377[↩]
- Duncan A.A. Median arcuate ligament syndrome. Curr Treat. Options Cardiovasc. Med. 2008;10:112–116. doi: 10.1007/s11936-008-0012-2[↩][↩]
- Jimenez J.C., Harlander-Locke M., Dutson E.P. Open and laparoscopic treatment of median arcuate ligament syndrome. J. Vasc Surg. 2012;56:869–873. doi: 10.1016/j.jvs.2012.04.057[↩][↩]
- Aswani Y., Thakkar H., Anandpara K.M. Imaging in median arcuate ligament syndrome. BMJ Case Rep. 2015:bcr2014207856. doi: 10.1136/bcr-2014-207856[↩]
- Horton K.M., Talamini M.A., Fishman E.K. Median arcuate ligament syndrome: Evaluation with CT angiography. Radiographics. 2005;25:1177–1182. doi: 10.1148/rg.255055001[↩]
- Gruber H, Loizides A, Peer S, Gruber I. Ultrasound of the median arcuate ligament syndrome: a new approach to diagnosis. Med Ultrason. 2012 Mar;14(1):5-9. https://www.medultrason.ro/assets/Medultrason-2012-vol14-no1/02Gruber.pdf[↩]
- Ozel A, Toksoy G, Ozdogan O, Mahmutoglu AS, Karpat Z. Ultrasonographic diagnosis of median arcuate ligament syndrome: a report of two cases. Med Ultrason. 2012 Jun;14(2):154-7. https://www.medultrason.ro/assets/Magazines/Medultrason-2012-vol14-no2/12-Ozel.pdf[↩]
- Horton KM, Talamini MA, Fishman EK. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics. 2005 Sep-Oct;25(5):1177-82. doi: 10.1148/rg.255055001[↩][↩]
- Pansky B. Review of Medical Embryology. Macmillan; New York, NY, USA: 1982. pp. 1–527.[↩][↩]
- Ali Mirjalili S., McFadden S.L., Buckenham T., Stringer M.D. A reappraisal of adult abdominal surface anatomy. Clin. Anat. 2012;25:844–850. doi: 10.1002/ca.22119[↩][↩][↩]
- Katz-Summercorn A., Bridger J. A cadaveric study of the anatomical variation of the origins of the celiac trunk and the superior mesenteric artery: A role in median arcuate ligament syndrome? Clin. Anat. 2013;26:971–974. doi: 10.1002/ca.22243[↩][↩][↩][↩][↩]
- Paz Z., Rak Y., Rosen A. Anatomical basis for celiac trunk and superior mesenteric artery entrapment. Clin. Anat. 1991;4:256–264. doi: 10.1002/ca.980040404[↩][↩]
- Lindner H.H., Kemprud E. A clinicoanatomical study of the arcuate ligament of the diaphragm. Arch. Surg. 1971;103:600–605. doi: 10.1001/archsurg.1971.01350110102016[↩][↩]
- Schweizer P., Berger S., Schweizer M., Schaefer J., Beck O. Arcuate ligament vascular compression syndrome in infants and children. J. Pediatr Surg. 2005;40:1616–1622. doi: 10.1016/j.jpedsurg.2005.06.040[↩][↩]
- White R.D., Weir-McCall J.R., Sullivan C.M., Mustafa S.A.R., Yeap P.M., Budak M.J., Sudarshan T.A., Zealley I.A. The celiac axis revisited: Anatomic variants, pathologic features, and implications for modern endovascular management. Radiographics. 2015;35:879–898. doi: 10.1148/rg.2015140243[↩]
- Sugae T., Fujii T., Kodera Y., Kanzaki A., Yamamura K., Yamada S., Sugimoto H., Nomoto S., Takeda S., Nakao A. Classification of the celiac axis stenosis owing to median arcuate ligament compression, based on severity of the stenosis with subsequent proposals for management during pancreatoduodenectomy. Surgery. 2012;151:543–549. doi: 10.1016/j.surg.2011.08.012[↩]
- Nasr L.A., Faraj W.G., Al-Kutoubi A., Hamady M., Khalifeh M., Hallal A., Halawani H.M., Wazen J., Haydar A.A. Median arcuate ligament syndrome: A single-center experience with 23 patients. Cardiovasc. Intervent Radiol. 2017;40:664–670. doi: 10.1007/s00270-016-1560-6[↩]
- Bech FR. Celiac artery compression syndromes. Surg Clin North Am. 1997 Apr;77(2):409-24. doi: 10.1016/s0039-6109(05)70558-2[↩][↩]
- Roseborough GS. Laparoscopic management of celiac artery compression syndrome. J Vasc Surg. 2009 Jul;50(1):124-33. doi: 10.1016/j.jvs.2008.12.078[↩][↩]
- Reilly LM, Ammar AD, Stoney RJ, Ehrenfeld WK. Late results following operative repair for celiac artery compression syndrome. J Vasc Surg. 1985 Jan;2(1):79-91. https://doi.org/10.1016/0741-5214(85)90177-6[↩][↩]
- Brandt LJ, Boley SJ. Celiac axis compression syndrome. A critical review. Am J Dig Dis. 1978 Jul;23(7):633-40. doi: 10.1007/BF01072599[↩][↩]
- Carey JP, Stemmer EA, Connolly JE. Median arcuate ligament syndrome. Experimental and clinical observations. Arch Surg. 1969 Oct;99(4):441-6. doi: 10.1001/archsurg.1969.01340160021005[↩]
- Perko MJ, Nielsen HB, Skak C, Clemmesen JO, Schroeder TV, Secher NH. Mesenteric, coeliac and splanchnic blood flow in humans during exercise. J Physiol. 1998 Dec 15;513 ( Pt 3)(Pt 3):907-13. doi: 10.1111/j.1469-7793.1998.907ba.x[↩]
- Berney T., Pretre R., Chassot G., Morel P. The role of revascularization in celiac occlusion and pancreatoduodenectomy. Am. J. Surg. 1998;176:352–356. doi: 10.1016/S0002-9610(98)00195-0[↩]
- Duffy AJ, Panait L, Eisenberg D, Bell RL, Roberts KE, Sumpio B. Management of median arcuate ligament syndrome: a new paradigm. Ann Vasc Surg. 2009 Nov-Dec;23(6):778-84. doi: 10.1016/j.avsg.2008.11.005[↩]
- Duncan AA. Median arcuate ligament syndrome. Curr Treat Options Cardiovasc Med. 2008 Apr;10(2):112-6. doi: 10.1007/s11936-008-0012-2[↩]
- Jimenez JC, Harlander-Locke M, Dutson EP. Open and laparoscopic treatment of median arcuate ligament syndrome. J Vasc Surg. 2012 Sep;56(3):869-73. doi: 10.1016/j.jvs.2012.04.057[↩][↩]
- Tulloch AW, Jimenez JC, Lawrence PF. et al. . Laparoscopic versus open celiac ganglionectomy in patients with median arcuate ligament syndrome. J Vasc Surg 2010. ; 52: 1,283 – 1 , 289.[↩]
- Baccari P, Civilini E, Dordoni L, Melissano G, Nicoletti R, Chiesa R. Celiac artery compression syndrome managed by laparoscopy. J Vasc Surg. 2009 Jul;50(1):134-9. doi: 10.1016/j.jvs.2008.11.124[↩]
- Coelho JCU, Hosni AVE, Claus CM, Aguilera YSH, Abot GP, Freitas ATC, Costa MARD. Treatment of median arcuate ligament syndrome: outcome of laparoscopic approach. Arq Bras Cir Dig. 2020;33(1):e1495. doi: 10.1590/0102-672020190001e1495[↩]
- van Petersen AS, Vriens BH, Huisman AB, Kolkman JJ, Geelkerken RH. Retroperitoneal endoscopic release in the management of celiac artery compression syndrome. J Vasc Surg. 2009 Jul;50(1):140-7. doi: 10.1016/j.jvs.2008.12.077[↩]
- Szilagyi DE, Rian RL, Elliott JP, Smith RF. The celiac artery compression syndrome: does it exist? Surgery. 1972 Dec;72(6):849-63.[↩]
- Williams S, Gillespie P, Little JM. Celiac axis compression syndrome: factors predicting a favorable outcome. Surgery. 1985 Nov;98(5):879-87.[↩]
- Evans WE. Long-term evaluation of the celiac band syndrome. Surgery. 1974 Dec;76(6):867-71.[↩]
- Ho KKF, Walker P, Smithers BM, Foster W, Nathanson L, O’Rourke N, Shaw I, McGahan T. Outcome predictors in median arcuate ligament syndrome. J Vasc Surg. 2017 Jun;65(6):1745-1752. https://www.jvascsurg.org/article/S0741-5214(16)31858-4/fulltext[↩][↩]