Contents
What is microalbuminuria
Microalbuminuria means that you have an excess of albumin in the urine and is diagnosed when urinary albumin excretion is between 30 and 300 mg/day, or when the microalbumin/creatinine ratio is between 30–300 μg/mg in random urine 1. In most healthy people, the kidneys prevent albumin and other proteins from entering the urine. However, if kidneys are damaged and start to allow proteins to pass from the blood into the urine, the first type of protein to appear in the urine is albumin. This is because albumin molecules are smaller than most other protein molecules.
The consistent presence of small amounts of albumin in the urine is called microalbuminuria and is associated with early-stage kidney disease. Once there are larger amounts of albumin in the urine it is called macroalbuminuria and it could indicate more severe kidney disease. Persistent amounts of albumin and other proteins in the urine (proteinuria) indicate kidney damage.
For many people, albuminuria is the earliest sign of chronic kidney disease. Diabetes and hypertension are the leading causes of chronic kidney disease in adults. Many diseases that cause kidney failure may have their origins in childhood 2. Early detection and appropriate treatment may improve prognosis in all age groups.
Urine and blood tests are used to detect and monitor kidney disease. Currently, the key markers for kidney disease include abnormal urine albumin levels and a persistent reduction in the estimated glomerular filtration rate (eGFR).
1 in 3 American adults is at risk for kidney disease 3. What puts you at risk for kidney disease? Major risk factors include diabetes, high blood pressure, a family history of kidney failure and being age 60 or older 3.
Microalbuminuria has been shown to be an early predictive factor for renal and cardiovascular diseases, not only in patients with diabetes mellitus or hypertension but also in the general population 4. Additionally, increased urinary albumin is thought to be a consequence of kidney disease 5. The mechanisms that make microalbuminuria a predictor of future cardiovascular events remain poorly understood; it is thought that the main cause is related to endothelial dysfunction 6. This potential causal connection is explained as resulting from the increased systemic albumin permeability caused by endothelial dysfunction, and that hemodynamic abnormalities interact with additional factors, such as lipids abnormalities, systemic inflammation, increased activity of renin-angiotensin-aldosterone system, and prothrombin factors, which together can lead to widespread organ damage 6. It is possible that endothelial dysfunction is innate, because increased albumin excretion has been observed in neonates and toddlers with a high variability of individual 5. There remains no consensus, however, as to whether inborn endothelial dysfunction can cause renal and/or cardiovascular disease, or if an acquired risk factor, such as obesity, plays a major role in the development of microalbuminuria and organ damage.
Several studies in obese children and adolescents have established specific risk factors that are associated with microalbuminuria. These include body mass index (BMI), waist circumference, triglyceride, sex and metabolic syndrome in children and adolescents 7. The association between obesity and microalbuminuria in children from these prior studies, however, remains unclear, and a thorough analysis of the general pediatric population is lacking. Additionally, previous studies that have supported a positive association between microalbuminuria and cardiovascular risk factors, such as hypertension in children, sometimes arrived at contradictory conclusions, and it remains questionable as to whether microalbuminuria is an independent predictor of cardiovascular disease in the pediatric population 8. Moreover, few studies have investigated the association between microalbuminuria and surrogate marker of insulin resistance such as hemoglobin A1c (HbA1c), triglyceride/high-density lipoprotein cholesterol (good cholesterol) ratio and serum alanine transaminase (ALT) in pediatric population, which have been widely accepted as risk factors of microalbuminuria in adults 9. Therefore, there is, at present, no well supported evidence to support the routine measurement of microalbuminuria in the pediatric population that presents with obesity or cardiometabolic risk factors 10.
Facts about chronic kidney disease (CKD):
- 30 million American adults have chronic kidney disease and millions of others are at increased risk.
- Early detection can help prevent the progression of kidney disease to kidney failure.
- Heart disease is the major cause of death for all people with chronic kidney disease.
- Glomerular filtration rate (GFR) is the best estimate of kidney function.
- Hypertension causes chronic kidney disease and chronic kidney disease causes hypertension.
- Persistent proteinuria (protein in the urine) means chronic kidney disease is present.
- High risk groups include those with diabetes, hypertension and family history of kidney failure.
- African Americans, Hispanics, Pacific Islanders, American Indians and Seniors are at increased risk.
- Two simple tests can detect chronic kidney disease: blood pressure, urine albumin and serum creatinine.
2 Simple Tests To Check For Kidney Disease
Urine Test
You could help save your kidneys with a simple urine test. Ask your doctor about Urine Albumin-to-Creatinine ratio (UACR) which estimates the amount of a type of protein, albumin, that is in your urine.
Urine Albumin-to-Creatinine ratio (UACR) stands for “urine-albumin-to-creatinine ratio.” Your urine will be tested for albumin. Albumin is a type of protein. Your body needs protein. But it should be in the blood, not the urine. Having protein in your urine may mean that your kidneys are not filtering your blood well enough. This can be a sign of early kidney disease. If your urine test comes back “positive” for protein, the test should be repeated to confirm the results. Three positive results over three months or more is a sign of kidney disease.
Healthy kidneys filter creatinine (a waste product from muscle activity) out of the blood. When kidney function is reduced, creatinine levels rise.
Blood Test
Your blood will be tested for a waste product called creatinine. Creatinine comes from muscle tissue. When the kidneys are damaged, they have trouble removing creatinine from your blood. Testing for creatinine is only the first step. Next, your creatinine result is used in a math formula with your age, race, and sex to find out your Glomerular Filtration Rate (GFR). Your Glomerular Filtration Rate (GFR) number tells your healthcare provider how well your kidneys are working to remove wastes from your blood. It is the best way to check kidney function. Over 90 is good, 60-89 should be monitored, less than 60 for 3 months indicates kidney disease. Check with your doctor about having a GFR test.
Microalbuminuria test
A urine microalbumin test is a test to detect very small levels of a blood protein (albumin) in your urine. A microalbumin test is used to detect early signs of kidney damage in people who are at risk of developing kidney disease.
Healthy kidneys filter waste from your blood and hang on to the healthy components, including proteins such as albumin. Kidney damage can cause proteins to leak through your kidneys and exit your body in your urine. Albumin is one of the first proteins to leak when kidneys become damaged.
Microalbumin tests are recommended for people with an increased risk of kidney disease, such as those with type 1 diabetes, type 2 diabetes or high blood pressure.
A urine albumin-to-creatinine ratio (UACR) on a spot urine specimen is the recommended test to assess and monitor urine albumin 11.
Urine albumin-to-creatinine ratio (UACR) is a ratio between two measured substances.
Urine albumin-to-creatinine ratio (UACR) (mg/g)* = Urine Albumin (mg/dL) / Urine Creatinine (g/dL)
*Urine albumin-to-creatinine ratio (UACR) (mg/g) is approximately equal to Albumin excretion in mg/day.
- Unlike a dipstick test for albumin, urine albumin-to-creatinine ratio (UACR) corrects for variation in urine concentration
- The first morning void is preferred because more concentrated urine allows for enhanced detection of analytes present in small quantities
- A random urine sample, collected while the patient is in the office, is also acceptable if a first morning void is not available
- A 24-hour urine collection is not necessary for routine assessment
Urine albumin is a continuous risk factor. Urine albumin-to-creatinine ratio (UACR) greater than 30 mg/g is considered abnormal. Traditionally, 30–300 mg/g has been called microalbuminuria and greater than 300 mg/g has been called macroalbuminuria. However, the 300 mg/g cut-off merely represents a rough correlation with the lower limit of sensitivity of the traditional urine dipstick for albumin. Thus, the albuminuria cut-offs are derived from laboratory methods rather than clinically relevant endpoints.
Stable or lower levels of albuminuria may indicate therapy is effective. Increasing or elevated levels may indicate progression of chronic kidney disease.
Microalbuminuria test indications
Your doctor may recommend a urine microalbumin test to detect early signs of kidney damage. Treatment may prevent or delay more advanced kidney disease.
How often you need microalbumin tests depends on any underlying conditions and your risk of kidney damage. For example:
- Type 1 diabetes. If you have type 1 diabetes, your doctor may recommend a microalbumin test once a year beginning five years after your diagnosis.
- Type 2 diabetes. If you have type 2 diabetes, your doctor may recommend a microalbumin test once a year beginning immediately after your diagnosis.
- High blood pressure (hypertension). If you have high blood pressure, your doctor may recommend microalbumin tests more regularly. Discuss with your doctor how often to repeat this test.
If your urinary microalbumin level is elevated, your doctor may recommend treatment and more frequent testing.
How you prepare for microalbumin test
The microalbumin test is a simple urine test. You can eat and drink normally before the test.The amount of urine your doctor may want to test may vary — you may only need to provide a random sample, or your doctor may ask you to collect 24 hours’ worth of urine.
During the microalbumin test, you simply need to provide a fresh urine sample. This may be done in several ways:
- 24-hour urine test. Your doctor may ask you to collect all of your urine in a special container over a 24-hour period and submit it for analysis.
- Timed urine test. Your doctor may ask you to provide a urine sample first thing in the morning or after a four-hour period of not urinating.
- Random urine test. A random urine test can be taken at any time. But to improve accuracy of the results, it’s often combined with a urine test for creatinine — a waste product usually filtered by the kidneys.
The urine sample is sent to a lab for analysis. After you provide the urine sample, you can return to your usual activities immediately.
Microalbuminuria test results
Results of the microalbumin test are measured as milligrams (mg) of protein leakage over 24 hours. Generally:
- Less than 30 mg is normal
- Thirty to 300 mg may indicate early kidney disease (microalbuminuria)
- More than 300 mg indicates more advanced kidney disease (macroalbuminuria)
Discuss your test result with your doctor and what it means for your health. If your urinary microalbumin level is higher than normal, your doctor may recommend repeating the test.
Several factors can cause higher than expected urinary microalbumin results, such as:
- Blood in your urine (hematuria)
- Certain medications
- Fever
- Recent vigorous exercise
- Urinary tract infection
- Other kidney diseases
Your doctor will want to pinpoint your diagnosis and check your kidney function to help plan your treatment. The doctor may do the following:
- Calculate your Glomerular Filtration Rate (GFR), which is the best way to tell how much kidney function you have. You do not need to have another test to know your GFR. Your doctor can calculate it from your blood creatinine, your age, race, gender and other factors. Your GFR tells your doctor your stage of kidney disease and helps the doctor plan your treatment.
- Perform an ultrasound or CT scan to get a picture of your kidneys and urinary tract. This tells your doctor whether your kidneys are too large or too small, whether you have a problem like a kidney stone or tumor and whether there are any problems in the structure of your kidneys and urinary tract.
- Perform a kidney biopsy, which is done in some cases to check for a specific type of kidney disease, see how much kidney damage has occurred and help plan treatment. To do a biopsy, the doctor removes small pieces of kidney tissue and looks at them under a microscope.
Your doctor may also ask you to see a kidney specialist who will consult on your case and help manage your care.
Microalbuminuria causes
Because kidney damage is generally irreversible, it is important to identify the cause as early as possible. Specific treatments are available in many cases (e.g., membraneous nephropathy, lupus nephropathy) and a diagnosis will guide management.
Although diabetes is the most common cause of chronic kidney disease, it is important not to assume that a patient with diabetes and chronic kidney disease has diabetic kidney disease. However, non-diabetic kidney disease is unlikely in a person with diabetes of long duration with other diabetic complications, physical findings of end-organ diabetic damage, and negative screening laboratory studies.
Chronic kidney disease includes conditions that damage your kidneys and decrease their ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, wastes can build to high levels in your blood and make you feel sick. You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. Also, kidney disease increases your risk of having heart and blood vessel disease. These problems may happen slowly over a long period of time. Chronic kidney disease may be caused by diabetes, high blood pressure and other disorders. Early detection and treatment can often keep chronic kidney disease from getting worse. When kidney disease progresses, it may eventually lead to kidney failure, which requires dialysis or a kidney transplant to maintain life.
What causes chronic kidney disease
The two main causes of chronic kidney disease are diabetes and high blood pressure, which are responsible for up to two-thirds of the cases. Diabetes happens when your blood sugar is too high, causing damage to many organs in your body, including the kidneys and heart, as well as blood vessels, nerves and eyes. High blood pressure, or hypertension, occurs when the pressure of your blood against the walls of your blood vessels increases. If uncontrolled, or poorly controlled, high blood pressure can be a leading cause of heart attacks, strokes and chronic kidney disease. Also, chronic kidney disease can cause high blood pressure.
Other conditions that affect the kidneys are:
- Glomerulonephritis, a group of diseases that cause inflammation and damage to the kidney’s filtering units. These disorders are the third most common type of kidney disease.
- Inherited diseases, such as polycystic kidney disease, which causes large cysts to form in the kidneys and damage the surrounding tissue.
- Malformations that occur as a baby develops in its mother’s womb. For example, a narrowing may occur that prevents normal outflow of urine and causes urine to flow back up to the kidney. This causes infections and may damage the kidneys.
- Lupus and other diseases that affect the body’s immune system.
- Obstructions caused by problems like kidney stones, tumors or an enlarged prostate gland in men.
- Repeated urinary infections.
Other problems that can cause kidney failure include 12:
- Autoimmune diseases, such as lupus and IgA nephropathy
- Genetic diseases (diseases you are born with), such as polycystic kidney disease
- Nephrotic syndrome
- Urinary tract problems
Sometimes the kidneys can stop working very suddenly (within two days). This type of kidney failure is called acute kidney injury or acute renal failure. Common causes of acute renal failure include:
- Heart attack
- Illegal drug use and drug abuse
- Not enough blood flowing to the kidneys
- Urinary tract problems
This type of kidney failure is not always permanent. Your kidneys may go back to normal or almost normal with treatment and if you do not have other serious health problems.
Having one of the health problems that can lead to kidney failure does not mean that you will definitely have kidney failure.
Kidney failure does not happen overnight. It is the end result of a gradual loss of kidney function. In fact, some people do not even know they have kidney disease until their kidneys fail. Why not? Because people with early kidney disease may not have any symptoms. Symptoms usually show up late in the progression of the disease.
Risk factors for microalbuminuria
Main risk factors:
- Diabetes (self or family)
- High blood pressure (self or family)
- Cardiovascular disease (self or family)
- Family history of kidney disease or diabetes or high blood pressure
Additional risk factors:
- African-American heritage
- Native American heritage
- Hispanic, Asian, Pacific Islander heritage
- Age 60 or older
- Obesity
- Low birth weight
- Prolonged use of NSAIDs (nonsteroidal anti-inflammatory drugs), a type of painkillers, such as ibuprofen and naproxen
- Lupus, other autoimmune disorders
- Chronic urinary tract infections
- Kidney stones
Microalbuminuria and diabetes
When your body digests the protein you eat, the process creates waste products. In the kidneys, millions of tiny blood vessels (capillaries) with even tinier holes in them act as filters. As blood flows through the blood vessels, small molecules such as waste products squeeze through the holes. These waste products become part of the urine. Useful substances, such as protein and red blood cells, are too big to pass through the holes in the filter and stay in the blood.
Diabetes can damage this system. High levels of blood glucose make the kidneys filter too much blood. All this extra work is hard on the filters. After many years, they start to leak and useful protein is lost in the urine. Having small amounts of protein in the urine is called microalbuminuria.
Not everyone with diabetes develops kidney disease. Factors that can influence kidney disease development include genetics, blood glucose control, and blood pressure.
The better a person keeps diabetes and blood pressure under control, the lower the chance of getting kidney disease.
When kidney disease is diagnosed early, during microalbuminuria, several treatments may keep kidney disease from getting worse. Having larger amounts of protein in the urine is called macroalbuminuria. When kidney disease is caught later during macroalbuminuria, end-stage renal disease (ESRD), usually follows.
In time, the stress of overwork causes the kidneys to lose their filtering ability. Waste products then start to build up in the blood. Finally, the kidneys fail. This failure, end-stage renal disease (ESRD), is very serious. A person with end-stage renal disease (ESRD) needs to have a kidney transplant or to have the blood filtered by machine (dialysis).
How can I prevent microalbuminuria and diabetes?
Diabetic kidney disease can be prevented by keeping blood glucose in your target range. Research has shown that tight blood glucose control reduces the risk of microalbuminuria by one third. In people who already had microalbuminuria, the risk of progressing to macroalbuminuria was cut in half. Other studies have suggested that tight control can reverse microalbuminuria.
Can microalbuminuria be reversed?
Yes and it depends of the cause(s), because kidney disease does not happen overnight. If kidney disease is found and treated early, you can help slow or even stop it from getting worse.
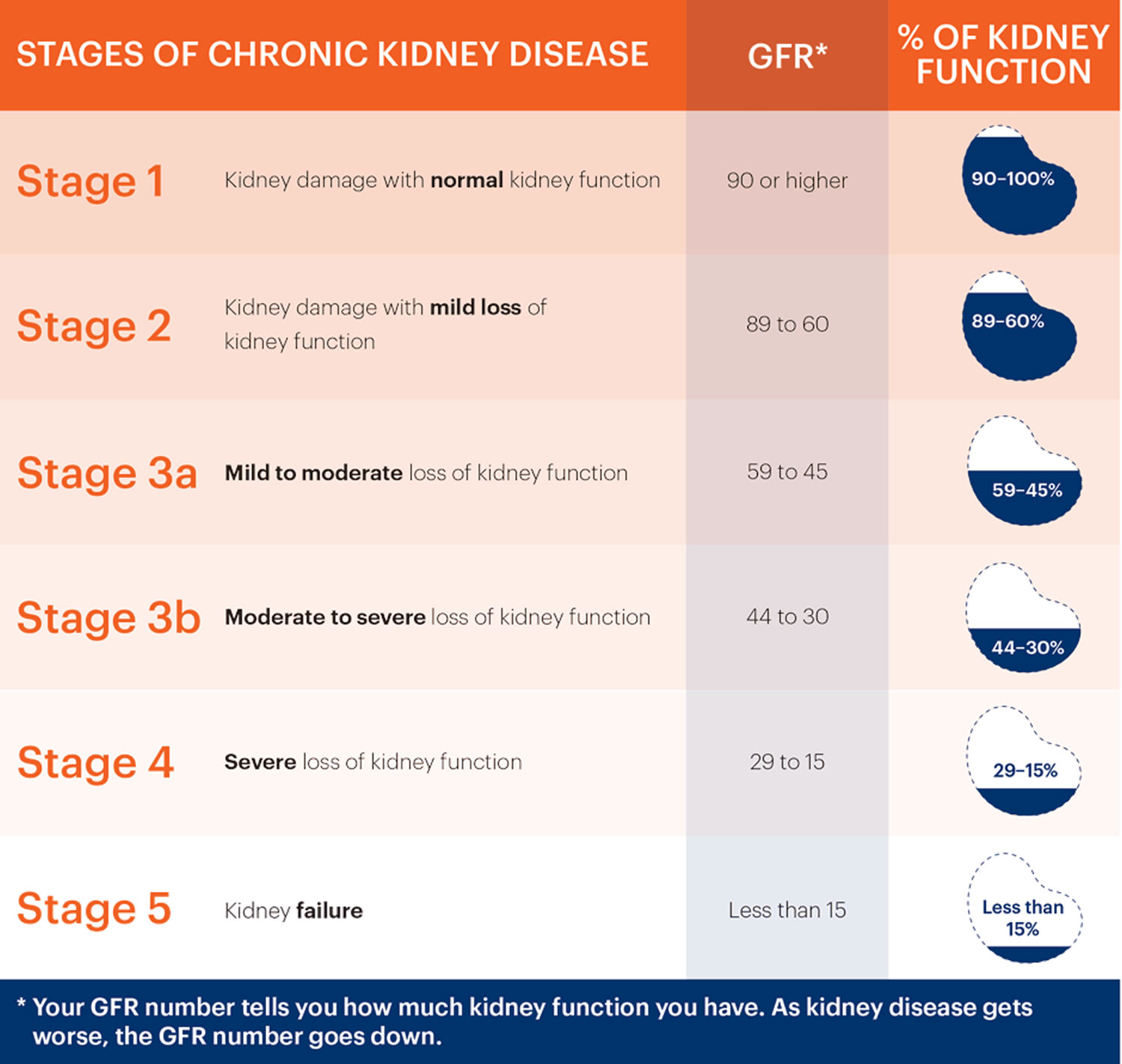
Kidney disease happens slowly over many years, and in stages. There are five stages of kidney disease. In each stage, the kidneys don’t work as well as the stage before. With treatment and lifestyle changes, you can help slow or stop your kidney disease from getting worse.
Each stage of chronic kidney disease is related to the level of kidney function and kidney damage.
- Stage 1 – a normal eGFR greater than or equal to 90 ml per minute per 1.73 m2, and albuminuria, hematuria, a pathological abnormality or a structural abnormality.
- Stage 2 – a slightly decreased eGFR between 60 and 89 ml per minute per 1.73 m2, and albuminuria, hematuria, a pathological abnormality or a structural abnormality.
Note: If your kidney function is at stage 1 or 2, you only have chronic kidney disease if you have albuminuria, hematuria, a pathological abnormality or a structural abnormality.
- Stage 3a – a mild to moderate decrease in eGFR between 45 and 59 ml per minute per 1.73 m2.
- Stage 3b – a moderate to severe decrease in eGFR between 30 and 44 ml per minute per 1.73 m2.
- Stage 4 – a severe decrease in eGFR between 15 and 29 ml per minute per 1.73 m2.
- Stage 5 – end stage kidney disease, as eGFR decreases to less than 15 ml per minute per 1.73 m2 or dialysis is started.
Microalbuminuria symptoms
Most people may not have any symptoms until their kidney disease is very advanced, which is why early testing is critical. A simple urine test can tell you if you have kidney disease.
By the time symptoms appear, kidney disease may be advanced, and symptoms can be misleading. However, you may notice that you:
- feel more tired and have less energy
- have trouble concentrating
- have a poor appetite
- have trouble sleeping
- have muscle cramping at night
- have swollen feet and ankles
- have puffiness around your eyes, especially in the morning
- have dry, itchy skin
- need to urinate more often, especially at night.
Anyone can get chronic kidney disease at any age. However, some people are more likely than others to develop kidney disease. You may have an increased risk for kidney disease if you:
- have diabetes
- have high blood pressure
- have a family history of kidney failure
- are older
- belong to a population group that has a high rate of diabetes or high blood pressure, such as African Americans, Hispanic Americans, Asian, Pacific Islanders, and American Indians.
Microalbuminuria treatment
Self-care
Important treatments for kidney disease are tight control of blood glucose and blood pressure. Blood pressure has a dramatic effect on the rate at which the disease progresses. Even a mild rise in blood pressure can quickly make kidney disease worsen. Four ways to lower your blood pressure are losing weight, eating less salt, avoiding alcohol and tobacco, and getting regular exercise.
Drugs
When these methods fail, certain medicines may be able to lower blood pressure. There are several kinds of blood pressure drugs, however, not all are equally good for people with diabetes. Some raise blood glucose levels or mask some of the symptoms of low blood glucose. Doctors usually prefer people with diabetes to take blood pressure drugs called ACE inhibitors.
ACE inhibitors are recommended for most people with diabetes, high blood pressure and kidney disease. Recent studies suggest that ACE inhibitors, which include captopril and enalapril, slow kidney disease in addition to lowering blood pressure. In fact, these drugs are helpful even in people who do not have high blood pressure.
Diet
Another treatment some doctors use with macroalbuminuria is a low-protein diet. Protein seems to increase how hard the kidneys must work. A low-protein diet can decrease protein loss in the urine and increase protein levels in the blood. Never start a low-protein diet without talking to your health care team.
Things you should do:
- Lower high blood pressure
- Keep blood-sugar levels under control if diabetic
- Reduce salt intake
- Avoid NSAIDs, a type of painkillers
- Moderate protein consumption
- Get an annual flu shot
- Exercise regularly
- Control weight
- Follow a balanced diet
- Quit smoking
- Drink only in moderation
- Stay hydrated
- Monitor cholesterol levels
- Get an annual physical
- Know your family medical history
Microalbuminuria diet
Most patients in the early stages of kidney disease need to limit the amount of sodium in their diet. Some patients may be told to limit protein in their diet as well. The DASH diet is often recommended for patients with kidney disease. Be sure to talk with your healthcare provider about your specific nutrition needs.
If your kidney disease gets worse, you may also need to limit potassium or phosphorus in your diet. Talk with your healthcare provider about your specific nutrition needs.
What is potassium and why is it important to you?
Potassium is a mineral found in many of the foods you eat. It plays a role in keeping your heartbeat regular and your muscles working right. It is the job of healthy kidneys to keep the right amount of potassium in your body. However, when your kidneys are not healthy, you often need to limit certain foods that can increase the potassium in your blood to a dangerous level. You may feel some weakness, numbness and tingling if your potassium is at a high level. If your potassium becomes too high, it can cause an irregular heartbeat or a heart attack.
A normal amount of potassium in a typical diet of a healthy American is about 3500 to 4500 milligrams per day. A potassium restricted diet is typically about 2000 milligrams per day. Your physician or dietitian will advise you as to the specific level of restriction you need based on your individual health. A kidney dietitian is trained to help you make modifications to you diet in order to prevent complications for kidney disease.
What foods are high in potassium (greater than 200 milligrams per portion)?
The following table lists foods that are high in potassium. The portion size is ½ cup unless otherwise stated. Please be sure to check portion sizes. While all the foods on this list are high in potassium, some are higher than others.
Table 1. High-Potassium Foods
| Fruits | Vegetables | Other Foods |
| Apricot, raw (2 medium) dried (5 halves) | Acorn Squash | Bran/Bran products |
| Avocado (¼ whole) | Artichoke | Chocolate (1.5-2 ounces) |
| Banana (½ whole) | Bamboo Shoots | Granola |
| Cantaloupe | Baked Beans | Milk, all types (1 cup) |
| Dates (5 whole) | Butternut Squash | Molasses (1 Tablespoon) |
| Dried fruits | Refried Beans | Nutritional Supplements: Use only under the direction of your doctor or dietitian. |
| Figs, dried | Beets, fresh then boiled | |
| Grapefruit Juice | Black Beans | |
| Honeydew | Broccoli, cooked | Nuts and Seeds (1 ounce) |
| Kiwi (1 medium) | Brussels Sprouts | Peanut Butter (2 tbs.) |
| Mango(1 medium) | Chinese Cabbage | Salt Substitutes/Lite Salt |
| Nectarine(1 medium) | Carrots, raw | Salt Free Broth |
| Orange(1 medium) | Dried Beans and Peas | Yogurt |
| Orange Juice | Greens, except Kale | Snuff/Chewing Tobacco |
| Papaya (½ whole) | Hubbard Squash | |
| Pomegranate (1 whole) | Kohlrabi | |
| Pomegranate Juice | Lentils | |
| Prunes | Legumes | |
| Prune Juice | White Mushrooms, cooked (½ cup) | |
| Raisins | Okra | |
| Parsnips | ||
| Potatoes, white and sweet | ||
| Pumpkin | ||
| Rutabagas | ||
| Spinach, cooked | ||
| Tomatoes/Tomato products | ||
| Vegetable Juices |
What foods are low in potassium?
The following table list foods which are low in potassium. A portion is ½ cup unless otherwise noted. Eating more than 1 portion can make a lower potassium food into a higher potassium food.
Table 2. Low-Potassium Foods
| Fruits | Vegetables | Other Foods |
| Apple (1 medium) | Alfalfa sprouts | Rice |
| Apple Juice | Asparagus (6 spears raw) | Noodles |
| Applesauce | Beans, green or wax Broccoli (raw or cooked from frozen) | Pasta |
| Apricots, canned in juice | Cabbage, green and red Carrots, cooked | Bread and bread products (Not Whole Grains) |
| Blackberries | Cauliflower | Cake: angel, yellow |
| Blueberries | Celery (1 stalk) | Coffee: limit to 8 ounces |
| Cherries | Corn, fresh (½ ear) frozen (½ cup) | Pies without chocolate or high potassium fruit |
| Cranberries | Cucumber | Cookies without nuts or chocolate |
| Fruit Cocktail | Eggplant | Tea: limit to 16 ounces |
| Grapes | Kale | |
| Grape Juice | Lettuce | |
| Grapefruit (½ whole) | Mixed Vegetables | |
| Mandarin Oranges | White Mushrooms, raw (½ cup) | |
| Peaches, fresh (1 small) canned (½ cup) | Onions | |
| Pears, fresh (1 small) canned (½ cup) | Parsley | |
| Pineapple | Peas, green | |
| Pineapple Juice | Peppers | |
| Plums (1 whole) | Radish | |
| Raspberries | Rhubarb | |
| Strawberries | Water Chestnuts, canned | |
| Tangerine (1 whole) | Watercress | |
| Watermelon (limit to 1 cup) | Yellow Squash | |
| Zucchini Squash |
What is a safe level of potassium in my blood?
Ask your doctor or dietitian about your monthly blood potassium level and enter it here:
- If potassium level is 3.5-5.0: You are in the SAFE zone
- If potassium level is 5.1-6.0: You are in the CAUTION zone
- If potassium level is higher than 6.0: You are in the DANGER zone
How can I keep my potassium level from getting too high?
- You should limit foods that are high in potassium. Your renal dietitian will help you plan your diet so you are getting the right amount of potassium.
- Eat a variety of foods but in moderation.
- If you want to include some high potassium vegetable in your diet, leach them before using. Leaching is a process by which some potassium can be pulled out of the vegetable. Instructions for leaching selected high potassium vegetables can be found at the end of this fact sheet. Check with your dietitian on the amount of leached high potassium vegetables that can be safely included in your diet.
- Do not drink or use the liquid from canned fruits and vegetables, or the juices from cooked meat.
- Remember that almost all foods have some potassium. The size of the serving is very important. A large amount of a low potassium food can turn into a high- potassium food.
- If you are on dialysis, be sure to get all the treatment or exchanges prescribed to you.
How do I get some of the potassium out of my favorite high-potassium vegetables?
The process of leaching will help pull potassium out of some high-potassium vegetables. It is important to remember that leaching will not pull all of the potassium out of the vegetable. You must still limit the amount of leached high-potassium vegetables you eat. Ask your dietitian about the amount of leached vegetables that you can safely have in your diet.
How to leach vegetables.
For Potatoes, Sweet Potatoes, Carrots, Beets, Winter Squash, and Rutabagas:
- Peel and place the vegetable in cold water so they won’t darken.
- Slice vegetable 1/8 inch thick.
- Rinse in warm water for a few seconds.
- Soak for a minimum of two hours in warm water. Use ten times the amount of water to the amount of vegetables. If soaking longer, change the water every four hours.
- Rinse under warm water again for a few seconds.
- Cook vegetable with five times the amount of water to the amount of vegetable.
What is phosphorus and why is it important to you?
Phosphorus is a mineral found in your bones. Along with calcium, phosphorus is needed to build strong healthy bones, as well as, keeping other parts of your body healthy.
Normal working kidneys can remove extra phosphorus in your blood. When you have chronic kidney disease (CKD), your kidneys cannot remove phosphorus very well. High phosphorus levels can cause damage to your body. Extra phosphorus causes body changes that pull calcium out of your bones, making them weak. High phosphorus and calcium levels also lead to dangerous calcium deposits in blood vessels, lungs, eyes, and heart. Phosphorus and calcium control are very important for your overall health.
What is a safe blood level of phosphorus?
A normal phosphorus level is 2.5 to 4.5 mg/dL. Ask your doctor or dietitian what your last phosphorus level was and write it down to help keep track of it.
How can I control my phosphorus level?
You can keep you phosphorus level normal by understanding your diet and medications for phosphorus control. Phosphorus can be found naturally in foods (organic phosphorus) and is naturally found in protein-rich foods such as meats, poultry, fish, nuts, beans and dairy products. Phosphorus found in animal foods is absorbed more easily than phosphorus found in plant foods.
Phosphorus that has been added to food in the form of an additive or preservative (inorganic phosphorus) is found in foods such as fast foods, ready to eat foods, canned and bottle beverages, enhanced meats, and most processed foods. Phosphorus from food additives is completely absorbed. Avoiding phosphorus additives can lower your intake of phosphorus. Phosphorus additives are found on the list of ingredients on the nutrition facts label. Look for “PHOS” to find phosphorus additives in the food.
Phosphorus additives found in foods include:
- Dicalcium phosphate
- Disodium phosphate
- Monosodium phosphate
- Phosphoric acid
- Sodium hexameta-phosphate
- Trisodium phosphate
- Sodium tripolyphosphate
- Tetrasodium pyrophosphate
Your dietitian and doctor will help you with this.
Table 3. High phosphorus food to limit or avoid
| Beverages | beer/ale | chocolate drinks |
| cocoa | dark colas
| |
| drinks made with milk canned iced teas | pepper type soda (Dr Pepper) | |
| bottled beverages with phosphate additives | ||
| Dairy Products | cheese | liquid nondairy creamer |
| custard | ice cream | |
| milk | pudding | |
| cream soups | yogurt (Greek type acceptable) | |
| Protein | oysters | sardines |
| beef liver | chicken liver | |
| fish roe | organ meats | |
| Other foods | chocolate candy caramels oat bran muffin | most processed/prepared foods pizza brewer’s yeast |
- Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): a position paper of the National Kidney Foundation. Keane WF, Eknoyan G. Am J Kidney Dis. 1999 May; 33(5):1004-10.[↩]
- Identify & Evaluate Patients with Chronic Kidney Disease. https://www.niddk.nih.gov/health-information/communication-programs/nkdep/identify-manage-patients/evaluate-ckd[↩]
- Kidney Disease Prevention. https://www.kidney.org/prevention[↩][↩]
- Rademacher ER, Sinaiko AR. Albuminuria in children. Curr Opin Nephrol Hypertens. 2009;18: 246–251. doi: 10.1097/MNH.0b013e3283294b98[↩]
- Gracchi V, van den Belt SM, Kupers LK, Corpeleijn E, de Zeeuw D, Heerspink HJ. Prevalence and distribution of (micro)albuminuria in toddlers. Nephrol Dial Transplant. 2016;31: 1686–1692. doi: 10.1093/ndt/gfv407[↩][↩]
- Pontremoli R, Leoncini G, Ravera M, Viazzi F, Vettoretti S, Ratto E, et al. Microalbuminuria, cardiovascular, and renal risk in primary hypertension. J Am Soc Nephrol. 2002;13 Suppl 3: S169–172.[↩][↩]
- Goknar N, Oktem F, Ozgen IT, Torun E, Kucukkoc M, Demir AD, et al. Determination of early urinary renal injury markers in obese children. Pediatr Nephrol. 2015;30: 139–144. doi: 10.1007/s00467-014-2829-0[↩]
- Nguyen S, McCulloch C, Brakeman P, Portale A, Hsu CY. Being overweight modifies the association between cardiovascular risk factors and microalbuminuria in adolescents. Pediatrics. 2008;121: 37–45. doi: 10.1542/peds.2007-3594[↩]
- Huang X, Zhou Y, Xu B, Sun W, Lin L, Sun J, et al. Glycated haemoglobin A1c is associated with low-grade albuminuria in Chinese adults. BMJ Open. 2015;5: e007429 doi: 10.1136/bmjopen-2014-007429[↩]
- Cho H, Kim JH. Prevalence of microalbuminuria and its associated cardiometabolic risk factors in Korean youth: Data from the Korea National Health and Nutrition Examination Survey. PLoS One. 2017;12(6):e0178716. Published 2017 Jun 2. doi:10.1371/journal.pone.0178716 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5456094/[↩]
- Assess Urine Albumin. https://www.niddk.nih.gov/health-information/communication-programs/nkdep/identify-manage-patients/evaluate-ckd/assess-urine-albumin[↩]
- Kidney failure. American Kidney Fund. http://www.kidneyfund.org/kidney-disease/kidney-failure/[↩]