Contents
What is adrenal myelolipoma
Adrenal myelolipoma is a rare benign (non-cancerous) tumor predominantly composed of mature adipose tissue and intermixed hematopoietic myeloid tissue 1. Myelolipomas are most often encountered in the adrenal gland but may rarely occur in other sites 1. Extra-adrenal sites for myelolipomas include the retroperitoneum, thorax, and pelvis. Adrenal myelolipoma tumors are frequently detected incidentally and are usually asymptomatic and hormonally inactive 2. Adrenal myelolipoma is found incidentally in 0.08% to 0.25% subjects during autopsy 3. Recently, myelolipomas are increasingly detected in living patients by incidental imaging, such as ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) 4. Adrenal myelolipoma usually occurs as a single, unilateral lesion, ranging from 1 to 34 cm, however they can also involve both adrenals 5.
Most adrenal myelolipomas do not show symptoms but continued growth of tumor without local invasion can lead to compression of nearby structures, causing persistent pain 6 and are rarely reported with hormonal disorders such as Cushing syndrome, congenital adrenal hyperplasia, or aldosterone-producing adenoma 7.
Myelolipomas are usually less than 4 cm in size occasionally they be huge, measuring more than 10 cm in size 1. The largest adrenal myelolipoma reported to date weighed 6 kg. On gross pathologic examination, a cut section of a myelolipoma has a variegated appearance consisting of bright yellow areas of fat, dark red areas of hematopoietic myeloid tissue and areas with intermixed red and yellow components. On histopathologic examination, myelolipomas are predominantly composed of fatty areas with interspersed hematopoietic tissue components. These fatty elements and hematopoietic areas may be clearly separated, or they are often intermixed. Tissue analysis often reveals a variable amalgamation of myeloid and erythroid cells, megakaryocytes, and occasionally lymphocytes. In an isolated adrenal myelolipoma, a peripheral rim of normal adrenal cortical tissue can be commonly identified distinctly from the mass. Rarely the myelolipomas can contain osteoid tissue in addition to the myeloid tissue. The hemorrhagic areas may be partly replaced by fibrotic tissue or may undergo calcification 8. Although myelolipoma is a benign tumor, if patient suffers from persistent pain due to local mass effect, surgical resection is required.
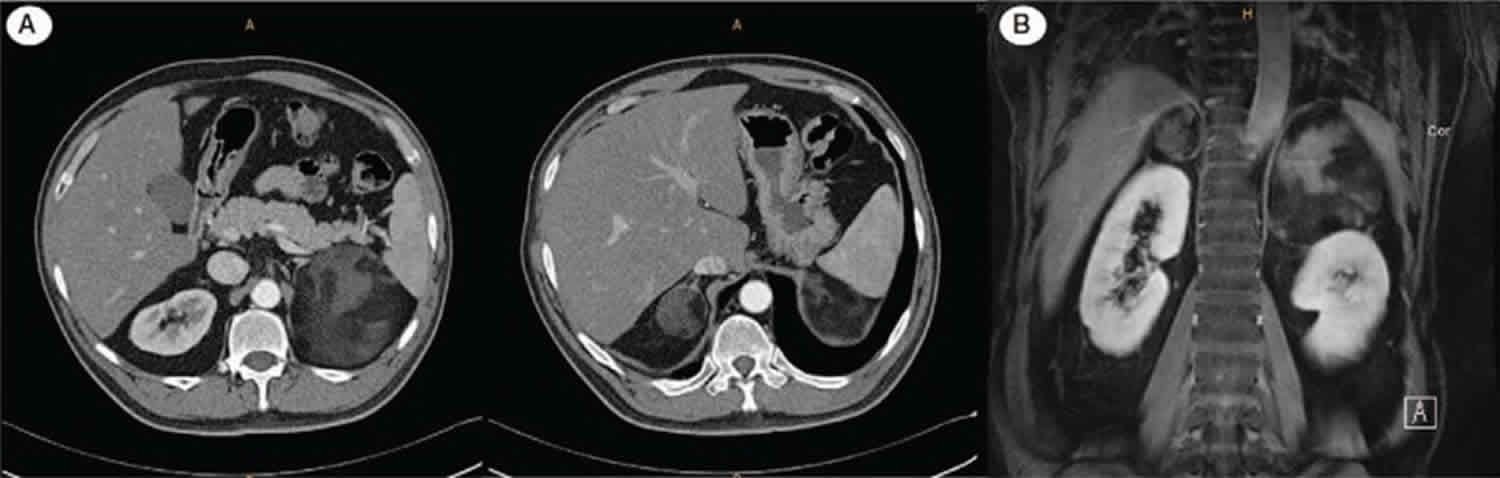
Figure 1. Adrenal myelolipoma
Footnote: There is an oval mass in the right suprarenal space, adjacent to the right adrenal gland, which contains macroscopic fat. This is compatible with an adrenal myelolipoma.
Adrenal myelolipoma causes
Regarding the cause and pathogenesis of adrenal myelolipoma, several rationales have been proposed. One hypothesis suggests that stimuli, such as necrosis, inflammation, infection, or stress could cause adrenocortical cell metaplasia and if chronically present these stimulants lead to the development of neoplasms. This hypothesis is supported by the increased incidence of the lesion in the advanced years of life. Adrenal myelolipoma is often associated with conditions like Cushing disease, obesity, hyperlipidemia, hypertension, and diabetes which can be considered as adrenal stimulants. Other theories propose that stressful lifestyle and an unbalanced diet may also play a role in the natural history of the tumor 9.
Adrenal myelolipoma symptoms
Myelolipomas usually present with one of the four recognizable clinicopathologic patterns: (1) isolated adrenal myelolipoma, (2) adrenal myelolipoma with acute hemorrhage, (3) extra-adrenal myelolipoma, and (4) myelolipoma associated with other adrenal diseases.
Isolated Adrenal Myelolipoma
Myelolipomas occurring in an otherwise normal adrenal gland are the most common pattern of presentation. They are asymptomatic and are incidentally identified during the imaging investigation performed for some other reason.
Adrenal Myelolipoma with Acute Hemorrhage
Retroperitoneal hemorrhage is the most common complication occurring in adrenal myelolipoma. Isolated larger lesions (typically over 4 cm in size) and those predominantly composed of fat (greater than 50%) have a greater propensity for a hemorrhagic event.
Extra-adrenal Myelolipoma
Myelolipomas occurring outside the adrenal gland are most commonly found in the retroperitoneum where presacral or perirenal location are reported as the most common. Patients usually have no endocrine disorder or acute hemorrhage.
Adrenal Myelolipoma with Associated Adrenal Disease
Less commonly patients with adrenal myelolipoma tend to have an endocrine disorder such as hypercortisolism (Cushing syndrome) and 21-hydroxylase deficiency with adrenal hyperplasia have been reported in patients with symptomatic adrenal myelolipomas.
Adrenal myelolipoma diagnosis
Ultrasound scan, CT scan and MRI scan all are highly beneficial in the diagnosis of adrenal myelolipoma, with CT scan being the most sensitive for identification of fat within the lesions 1. As these tumors are nonfunctional, endocrinological tests are not useful as these lesions are mostly functionally inert. The differential diagnosis of fat containing retroperitoneal masses would include retroperitoneal lipoma or liposarcoma and renal angiomyolipoma.
At ultrasound scan, myelolipoma has the typical appearance of a hyperechoic mass with intermixed hypoechoic regions. Echogenicity is mainly determined by the variable proportions of the constituent elements in the lesion. The areas of intermixed fatty and myeloid tissue are the most echogenic, whereas regions of pure fat may appear hypoechoic. Because of inhomogeneous architecture, myelolipomas often have heterogeneous echogenicity. Calcification foci appear hyperechoic with acoustic shadowing. Myelolipoma has vague and no appreciable margins due having almost the same echogenicity as surrounding retroperitoneal fat. Hemorrhage alters the sonographic picture, with hemorrhagic areas appearing hypoechoic compared with fat 10.
Computed Tomography scan: At CT hypodense fat is the hallmark of adrenal myelolipoma. Almost all myelolipomas have some focus of fat, although the fatty tissue focus may be very small. Large amounts of fat are frequently encountered with “smoky” or “variegated” areas of interspersed higher-attenuation tissue. This denser tissue has attenuation values of 20 HU to 30 HU, inferring the presence of both of fat and myeloid elements. Myelolipomas are usually relatively well circumscribed, however, due to the presence of abundant fat they can be difficult to distinguish from surrounding retroperitoneal fat. Foci of punctate calcification may be seen in 25% to 30% of cases. CT is the most sensitive for detecting hemorrhage which may be hyper to hypodense depending on the age of evolution.
MRI scan: The predominantly fatty areas in myelolipoma appear hyperintense on T1 MR images and intermediate to hyperintense on T2. Admixed marrowlike elements have medium intensity signals similar to that of the spleen. Fat-suppression techniques are best for demonstrating the fat in a myelolipoma with MR imaging. The presence of marrow like elements or hemorrhage results in persistent areas of increased signal intensity on fat-suppressed MR images. Opposed-phase imaging demonstrates signal loss in admixed voxels containing both fat and myeloid tissue which is also described for adrenal adenoma and other masses with mixed components. At MR imaging, the signal intensity will vary depending on the presence and age of hemorrhage. Post-contrast images show striking enhancement. The imaging features of extra-adrenal myelolipoma are similar to those of adrenal myelolipoma and do not allow distinction extra-adrenal myelolipoma from other fat-containing tumors.
Nuclear Medicine: Adrenal myelolipomas typically do not demonstrate an avid fluoro-deoxyglucose (FDG) uptake, which is usually less than that of the liver. However, in rare instances, the adenomatous and hematopoietic elements can show an increased FDG uptake.
Adrenal myelolipoma treatment
Management of adrenal myelolipoma should be decided upon the size of lesion and presence of symptoms. Small lesions measuring less than 5 cm, and those who are asymptomatic are usually monitored via imaging over a period of one to two years 1. According to various studies, it is suggested that symptomatic tumors or myelolipomas larger than 7 cm should undergo elective surgical excision 1. The approach is based on the reported incidence of life-threatening emergencies caused by spontaneous rupture and hemorrhage within large lesions. Conventional or endoscopic access may be chosen according to the size of the tumor. Mini-invasive and endoscopic techniques are best utilized for smaller-sized lesions, depending on the expertise of the operator. Conventional methods including transabdominal, lumbar, subcostal or posterior access laparotomy operations have all been described in the literature. An extraperitoneal approach is preferable as it leads to quicker recovery of the patient and lesser postoperative complications. The midline approach is indicated for masses larger than 10 cm or in cases where there are adhesions and infiltration of the surrounding structures. Follow up is mandatory regardless of which surgical method has been employed. There is no evidence of malignant transformation in the literature 11.
- Bokhari MR, Garla VV. Adrenal Myelolipoma. [Updated 2019 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436011[↩][↩][↩][↩][↩][↩]
- Park SY, Kwak MK, Kim HJ, et al. Case report of a bilateral adrenal myelolipoma associated with Cushing disease. Medicine (Baltimore). ;96(52):e9455. doi:10.1097/MD.0000000000009455 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6392800[↩]
- Olsson CA, Krane RJ, Klugo RC, et al. Adrenal myelolipoma. Surgery 1973;73:665–70.[↩]
- Musante F, Derchi LE, Bazzocchi M, et al. MR imaging of adrenal myelolipomas. J Comput Assist Tomogr 1991;15:111–4.[↩]
- Umpierrez MB, Fackler S, Umpierrez GE, et al. Adrenal myelolipoma associated with endocrine dysfunction: review of the literature. Am J Med Sci 1997;314:338–41[↩]
- Cho MH, Mandaliya R, Liang J, Patel M. A case report of symptomatic presacral myelolipoma. Medicine (Baltimore). ;97(15):e0337. doi:10.1097/MD.0000000000010337 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5908593[↩]
- Caliumi C, De Toma G, Bossini A, et al. A rare combination consisting of aldosterone-producing adenoma and adrenal myelolipoma in a patient with heterozygosity for retinoblastoma (RB) gene. J Renin Angiotensin Aldosterone Syst 2004;5:45–8.[↩]
- Littrell LA, Carter JM, Broski SM, Wenger DE. Extra-adrenal myelolipoma and extramedullary hematopoiesis: Imaging features of two similar benign fat-containing presacral masses that may mimic liposarcoma. Eur J Radiol. 2017 Aug;93:185-194.[↩]
- Decmann Á, Perge P, Tóth M, Igaz P. Adrenal myelolipoma: a comprehensive review. Endocrine. 2018 Jan;59(1):7-15.[↩]
- Wilson B, Becker A, Estes T, Keshavamurthy J, Pucar D. Adrenal Hemangioma Definite Diagnosis on CT, MRI, and FDG PET in a Patient With Primary Lung Cancer. Clin Nucl Med. 2018 Jun;43(6):e192-e194[↩]
- Baisakh MR, Chattoraj A, Narayanan R, Mohanty R, Mishra M. Adrenal myelolipoma: A rare lesion of adrenal gland. Indian J Cancer. 2015 Oct-Dec;52(4):597-8[↩]