Contents
What is myoglobinuria
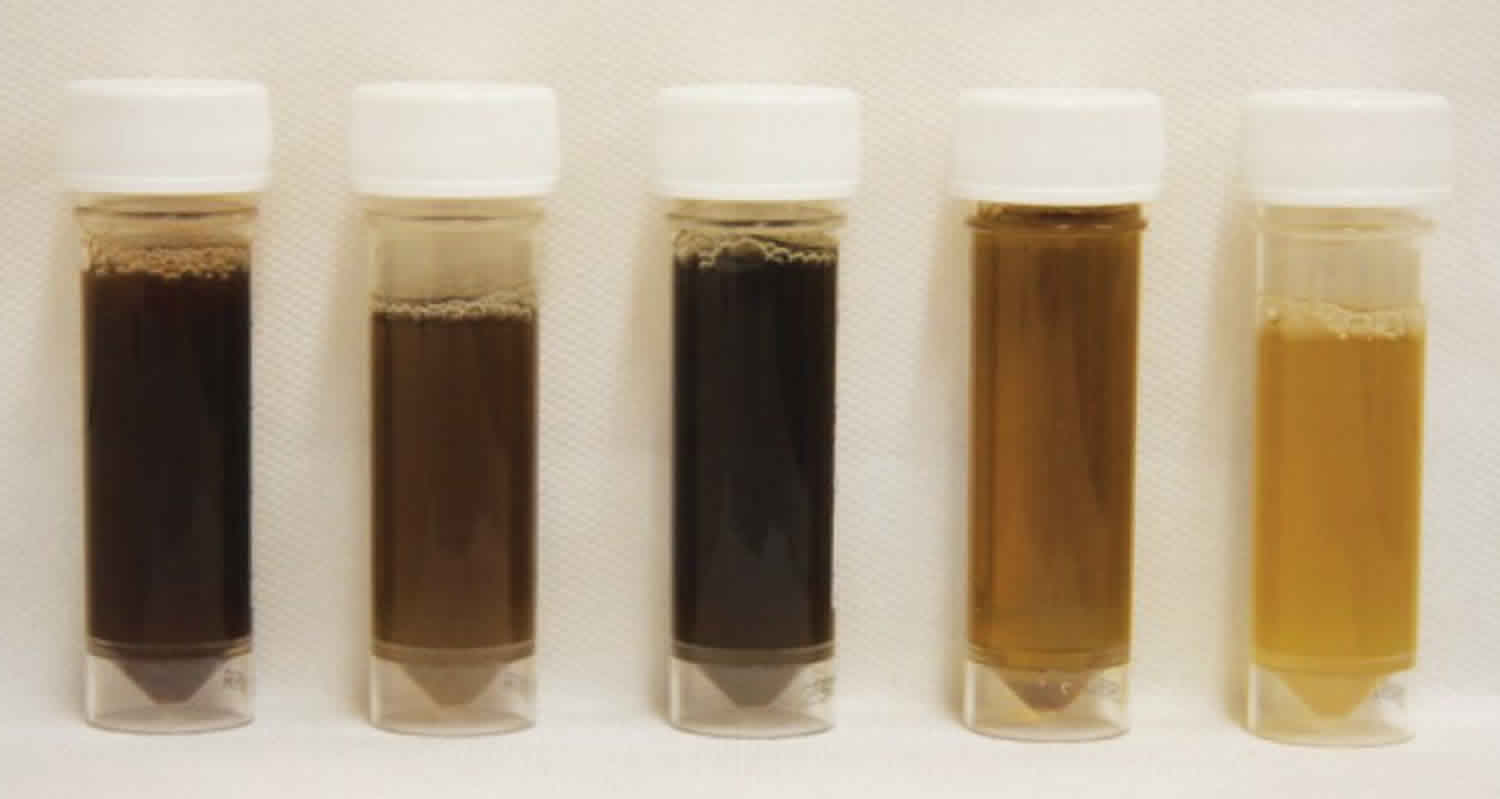
Myoglobinuria refers to an abnormal pathologic state in which there is an excessive amount of myoglobin is found in the urine, imparting a cola-like urine color. Myoglobin is a dark, small, oxygen-binding red cytoplasmic heme protein found only in heart and skeletal muscles 1. Myoglobin functions as an oxygen-storage unit, trapping oxygen within muscle cells and providing oxygen to the working muscles. When heart or skeletal muscle is injured, myoglobin is released into the blood. Under normal conditions, myoglobin circulates in the blood bound to plasma globulins which are maintained at a level of 0-0.003 mg/dL. Once serum myoglobin levels reach a level above 0.5 to 1.5 mg/dL, the rate of metabolism, endocytosis, and serum protein binding capacity is overwhelmed, and myoglobin is rapidly excreted in the urine. Myoglobin levels are normally very low or not detectable in the urine. High levels of urine myoglobin indicate an increased risk for kidney damage and failure. Additional tests, such as blood urea nitrogen (BUN), creatinine, and urinalysis, are done to monitor kidney function in these people.
Blood levels of myoglobin can rise very quickly with severe muscle damage and can also be measured within a few hours following an injury.
Myoglobin belongs to the super globin family of proteins and is composed of a single polypeptide chain of 154 amino acids as well as a porphyrin ring containing a central ferrous iron molecule. Similar to hemoglobin, myoglobin functions to reversibly bind oxygen and can form oxymyoglobin, carboxy myoglobin, or metmyoglobin. Unlike hemoglobin, however, myoglobin has only one binding site for oxygen, the affinity of which is comparatively very high. As a result, myoglobin can receive oxygen from hemoglobin at the tissue level via the Bohr Effect, and either store oxygen or deliver it to muscle cells during periods of hypoxia, anoxia, or increased metabolic activity.
Myoglobin is filtered from the blood by the kidneys and is released into the urine. Large quantities of myoglobin are toxic to the kidneys. If significant amounts of myoglobin are released into the bloodstream, which can happen after severe trauma or muscle injuries, the excess myoglobin may cause damage to the kidneys and eventually result in kidney failure. Measurement of myoglobin in urine helps to detect myoglobinuria.
Although myoglobin is normally easily filtered by the glomerulus and quickly excreted in the urine, the presence of large amounts of myoglobin in renal tubules can lead to an interaction of the hemoprotein with Tamm-Horsfall proteins and subsequent precipitation and tubular obstruction. This process occurs most favorably in conditions where acidic urine is present. In addition, damage to both muscle tissues and kidney epithelial cells promotes the production of reactive oxygen species, which can, in turn, lead to oxidation of ferrous oxide to ferric oxide, a hydroxyl radical. Both tubular obstruction and oxidative damage, as a result of myoglobinuria, can alone or in combination lead to acute kidney injury.
Myoglobin release from muscle tissues occurs as a result of damage to muscle cells and a change in skeletal muscle cell membrane permeability. Damage to muscle cells results in dysregulation of sodium-calcium channel functioning, ultimately elevating intracellular free ionized calcium. This causes a resultant activation of calcium-dependent enzymes which go on to further metabolize and destroy the muscle cell membrane and allow for the release of intracellular contents, including myoglobin and creatine kinase.
Myoglobinuria is produced by multiple causes: any condition that accelerates the use or interferes with the availability of oxygen or energy substrates to muscle cells can result in myoglobinuria, as can events that produce direct muscle injury, either mechanical or chemical.
Acute renal failure is the most serious complication, which can be prevented by prompt, aggressive treatment. In patients surviving acute attacks, recovery of muscle and renal function is usually complete.
Myoglobinuria vs Hemoglobinuria
Hemoglobinuria means the presence of hemoglobin in the urine. Normally, hemoglobin does not appear in the urine. Hemoglobin is a molecule attached to red blood cells. Hemoglobin helps move oxygen and carbon dioxide through the body.
Red blood cells have an average life span of 120 days. After this time, they are broken down into parts that can make a new red blood cell. This breakdown takes place in the spleen, bone marrow, and liver. If the red blood cells break down in the blood vessels, their parts move freely in the bloodstream.
If the level of hemoglobin in the blood rises too high, then hemoglobin begins to appear in the urine. This is called hemoglobinuria.
Hemoglobinuria may be a result of any of the following:
- A kidney disorder called acute glomerulonephritis
- Burns
- Crushing injury
- Hemolytic uremic syndrome (HUS)
- Kidney infection
- Kidney tumor
- Malaria
- Paroxysmal nocturnal hemoglobinuria
- Paroxysmal cold hemoglobinuria
- Sickle cell anemia
- Thalassemia
- Thrombotic thrombocytopenic purpura (TTP)
- Transfusion reaction
- Tuberculosis
Myoglobinuria causes
Myoglobinuria is usually the result of rhabdomyolysis or muscle destruction. The cause can be either hereditary or acquired.
Muscle injury is caused by direct or indirect injury to muscle tissue, such as:
- Trauma or crush injuries, for example, from a car accident
- Taking illegal drugs such as cocaine, amphetamines or heroin
- Extreme muscle exertion, for example, running marathons
- A side effect of some medicines, such as statins (although the risk is very low)
- Prolonged muscle pressure, for example when someone is lying unconscious on a hard surface
- Very high body temperature (hyperthermia) or heat stroke.
- Electrical shock from a high-voltage sources
- Serious and/or extensive burns
- Blood clot (thrombosis) that blocks blood flow to tissues and organs
- Exposure to toxins such as heavy metals, snake venom, or carbon monoxide
- Infections such as HIV, influenza, Streptococcus (this can more commonly occur in children than adults)
- Genetic or metabolic disorders that affect muscles e.g., myoglobinuria recurrent & myoglobinuria dominant form
- Diseases such as muscular dystrophy or underlying conditions such as diabetes that is not well controlled, hypothyroidism, or hyperthyroidism
- Several drugs. Some examples include:
- Drugs of abuse such as alcohol (ethanol), heroin and cocaine
- Antibiotics (amphotericin B, ampicillin)
- Anesthetics
- Antidepressants
- Antihistamines
- Aspirin (salicylates)
- Corticosteroids
- Lidocaine
- Lithium
- Statins (used to treat high cholesterol)
- Theophylline
Myoglobinuria in adults most often is encountered in cases of trauma or alcohol and drug abuse and generally as a result of muscle necrosis as a result of prolonged immobilization or pressure from the weight of the body 2. Furthermore, excessive physical activity; metabolic disorders; viral infections, such as influenza, HIV, or herpes simplex; toxin-producing bacterial infections; connective tissue disease; seizures; electrical shock injury, including lightning strikes; third-degree burns; venom from a snake or insect bite; certain medications, such as statins or antipsychotics; or prolonged alcohol or drug use, as with heroin, cocaine, or amphetamines all can create an imbalance in muscle energy production and consumption which result in muscle damage and destruction.
Contrastingly, rhabdomyolysis or myoglobinuria in children most often is associated with viral myositis as well as trauma, excessive muscular exertion, drug overdose, seizures, connective disuse disease, or metabolic disorders 2.
The incidence of myoglobinuria in the United States varies depending on the incidence of traumas or natural disasters. An increased incidence of viral myositis such as that caused by an epidemic, in certain regions may cause a temporary increase in the incidence of rhabdomyolysis and myoglobinuria. Excessive heat or higher temperatures such as in the summer months or warmer geographic areas which cause heat stroke, especially in those who are more active; or that caused by malignant hyperthermia or neuroleptic malignant syndrome, may additionally increase the incidence of stress or exertion-induced rhabdomyolysis.
Myoglobinuria symptoms
A typical myoglobinuria presents classical triad of symptoms like muscle pain (myalgia), muscle weakness and tea red color urine 3. Though this triad is seen in less than 10 % of cases, fatigue, fever, tachycardia, nausea and vomiting may be seen in many cases 4.
Common myoglobinuria symptoms include:
- muscle pain or tenderness, especially in the shoulders, thighs or lower back
- muscle weakness or stiffness, or trouble moving arms or legs
- confusion, dehydration or fever
- lack of consciousness
- dark red or brown urine, or reduced or no urine output.
If not treated early, myoglobinuria can lead to complications, such as:
- very high potassium levels in the blood (hyperkalemia); this can lead to an irregular heartbeat or cardiac arrest
- kidney failure or problems with the liver
- compartment syndrome; this occurs when too much pressure builds up in the injured group of muscles (compartment). The extreme pressure hinders blood flow to and from the affected tissues and can cause further muscle damage and death.
Myoglobinuria test
Blood and urine samples are usually used to diagnose myoglobinuria.
Urinalysis should be employed to evaluate for myoglobinuria, such as with acute kidney injury, and assess the severity of renal damage, if present. Furthermore, if kidney damage is suspected, as a result of rhabdomyolysis, the level of serum creatinine should be assessed, as it is often quickly elevated during rhabdomyolysis when compared to other causes of kidney injury. In addition to this, the blood urea nitrogen to creatinine ratio is also generally low.
A myoglobin blood test may be used detect muscle damage. Blood levels of myoglobin can rise very quickly with severe muscle damage and can be measured within a few hours following an injury.
Myoglobin is filtered from the blood by the kidneys and is released into the urine. Sometimes, a urine test is ordered to evaluate myoglobin levels in people who have had extensive damage to their skeletal muscles (rhabdomyolysis). Urine myoglobin levels reflect the degree of muscle injury and, since myoglobin is toxic to the kidneys, reflect the risk of kidney damage.
Sometimes, a myoglobin blood test may be used along with a troponin test as a cardiac biomarker to help detect a heart attack early, but in the U.S., it is used less frequently for this purpose.
The level of myoglobin in the blood starts to rise within 2-3 hours of a heart attack or other muscle injury, reaches its highest levels within 8-12 hours, and generally falls back to normal within one day. An increase in myoglobin is detectable sooner than troponin, but it is not as specific for heart damage and it will not stay elevated as long as troponin.
Although a negative myoglobin result effectively rules out a heart attack, a positive result must be confirmed by testing for troponin.
When is myoglobinuria ordered?
Myoglobinuria test may be ordered when a person has experienced damage to muscles caused by, for example, trauma or muscular dystrophy.
Urine myoglobin may be ordered when there has been extensive injury to skeletal muscle, resulting in the rapid breakdown of muscle, and damage to the kidneys is suspected.
Myoglobin is not widely used for diagnosing heart attacks because it has largely been replaced by troponin, which is much more specific. If the myoglobin test is available, it may be ordered to assess persons with chest pain who are suspected of having a heart attack. Blood samples are drawn when a person with signs and symptoms, such as chest pain, first arrives at the emergency room, followed by a series of tests done over several hours.
Myoglobinuria diagnosis
Urinalysis should be employed to evaluate for myoglobinuria, such as with acute kidney injury, and assess the severity of renal damage, if present.
Furthermore, if kidney damage is suspected, as a result of rhabdomyolysis, the level of serum creatinine should be assessed, as it is often quickly elevated during rhabdomyolysis when compared to other causes of kidney injury. In addition to this, the blood urea nitrogen to creatinine ratio is also generally low.
Hematology, as well as blood chemistries, prothrombin time and activated partial thromboplastin time, should be employed to assess serum myoglobin and creatine kinase. Liver and and renal function also may be assessed if complications secondary to rhabdomyolysis are concerning.
Though imaging is not generally indicated in cases of rhabdomyolysis, given that it is a clinical syndrome often diagnosed with supportive laboratory tests, MRI, bone scintigraphy, ultrasound, or CT can be used to demonstrate some changes in muscle tissue.
An ECG is necessary to detect cardiac arrhythmias that may result from electrolyte abnormalities due to rhabdomyolysis. An assessment of blood chemistries also may help point towards this, in addition to an arterial blood gas analysis if metabolic acidosis is suspected.
A thorough history and physical examination are extremely important to form a diagnosis of rhabdomyolysis, though they are not always useful in determining the underlying cause. If infectious causes are suspected, one should assess complete blood count, appropriate cultures, and any additional serologic studies that may help confirm or point toward a diagnosis. Blood chemistries and endocrine assays may be useful if an underlying endocrine abnormality is suspected. If drugs or toxins are a potential underlying cause, the appropriate screening for toxins should be performed.
In patients with repeated instances of rhabdomyolysis, genetic testing, a muscle biopsy, or the forearm ischemic exercise test may reveal an underlying myopathy or metabolic disorder.
The caffeine halothane contracture test can help detect an individual’s risk of developing malignant hypothermia.
Myoglobinuria treatment
Myoglobinuria is usually treated in hospital, with intravenous fluids to help you produce enough urine and prevent kidney failure.
Rarely, dialysis is needed if kidney function is poor. If you have compartment syndrome, you may need immediate surgery to avoid further muscle death or nerve damage.
Early diagnosis and treatment of myoglobinuria and its causes increases your chances of a full recovery.
- Trivedi DJ, Kulkarni SP, Mudaraddi R. Primary Myoglobinuria: Differentiate Myoglobinuria from Hemoglobinuria. Indian J Clin Biochem. 2016;32(3):367-369. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539002[↩]
- Foris LA, Richards JR. Serum Myoglobin. [Updated 2019 Jan 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470441[↩][↩]
- Barca E, Valentina E, Salvatore DM. Metabolic myoglobinuria. Curr Neurol Neurosci Rep. 2015;15(10):69. doi: 10.1007/s11910-015-0590-9[↩]
- Dalakas MC. Toxic drug induced myopathies. J Neurol Neurosurg Psychiatry. 2009;80(8):832–838. doi: 10.1136/jnnp.2008.168294.[↩]