Contents
- Naloxone
- How to use and give naloxone
- How is naloxone given?
- What if I’m not sure if someone has an opioid overdose?
- Is naloxone safe?
- What are the different types of naloxone?
- Is there a preferable naloxone delivery system?
- Where can I get naloxone?
- How much does naloxone cost?
- How does naloxone work?
- Naloxone uses
- Naloxone dosage
- Naloxone side effects
Naloxone
Naloxone is a US Food and Drug Administration (FDA) approved medicine used to quickly reverse an opioid or narcotic overdose 1. Naloxone is available as a nasal spray (Narcan 4mg, Kloxxado 8mg) or an injection (Zimhi 5 mg/0.5 mL). Naloxone is a opioid antagonist that works by attaching to opioid receptors and therefore reverses and blocks the effects of other opioids. Naloxone can quickly restore normal breathing to a person if their breathing has slowed or stopped because of an opioid overdose. But, naloxone has no effect on someone who does not have opioids in their system, and it is not a treatment for opioid use disorder. Examples of opioids sometimes called narcotics are buprenorphine, heroin, fentanyl, oxycodone (OxyContin), hydrocodone (Vicodin, Lortab), codeine, morphine, hydromorphone, meperidine, methadone, oxymorphone, and tramadol. There are no age restrictions on the use of naloxone; it can be used for suspected overdose in infants and children through elderly people. Naloxone saves lives. From 1996 to 2014, at least 26,500 opioid overdoses in the United States were reversed by laypersons using naloxone. Naloxone does not cause physical or psychological dependence and has virtually no effect in a healthy non-dependent person 2.
Naloxone should be used as soon as possible to treat a known or suspected opioid overdose emergency, if there are signs of slowed breathing, severe sleepiness or the person is not able to respond (loss of consciousness). Once naloxone has been given the patient must receive emergency medical care straight away, even if they wake up.
First, recognize signs of an opioid overdose:
- Limp body
- Pale, clammy face
- Blue lips, gums or fingertips
- Vomiting or gurgling sounds
- Inability to speak or be awakened
- Slow and shallow breathing
- Slow or irregular heartbeat or pulse
- Small pupils
- Vomiting
- Unresponsiveness (doesn’t wake up when shaken or called)
- Unconsciousness
If you see these symptoms, call your local emergency services number immediately and consider the use of naloxone if available. If the person has stopped breathing or if breathing is very weak, begin CPR (best performed by someone who has training).
Naloxone is a prescription medicine but in many states, naloxone is available from a pharmacist without a prescription from your doctor, under state Naloxone Access Laws or alternate arrangements. Furthermore, naloxone is not a controlled substance, according to the US Drug Enforcement Administration (DEA).
Naloxone works to reverse opioid overdose in the body for only 30 to 90 minutes. But many opioids remain in the body longer than that. Because of this, it is possible for a person to still experience the effects of an overdose after a dose of naloxone wears off. Also, some opioids are stronger and might require multiple doses of naloxone. Therefore, one of the most important steps to take is to call your local emergency services number for an ambulance so the individual can receive immediate medical attention.
People who are given naloxone should be observed constantly until emergency care arrives. They should be monitored for another 2 hours after the last dose of naloxone is given to make sure breathing does not slow or stop.
People with physical dependence on opioids may have opioid withdrawal symptoms within minutes after they are given naloxone.
Opioid withdrawal symptoms might include:
- headaches,
- changes in blood pressure,
- rapid heart rate,
- sweating,
- nausea,
- vomiting,
- feeling nervous, restless, or irritable
- tremors.
- body aches
- dizziness or weakness
- diarrhea, stomach pain, or nausea
- fever, chills, or goose bumps
- sneezing or runny nose in the absence of a cold
While this is uncomfortable, it is usually not life threatening. The risk of death for someone overdosing on opioids is worse than the risk of having a bad reaction to naloxone.
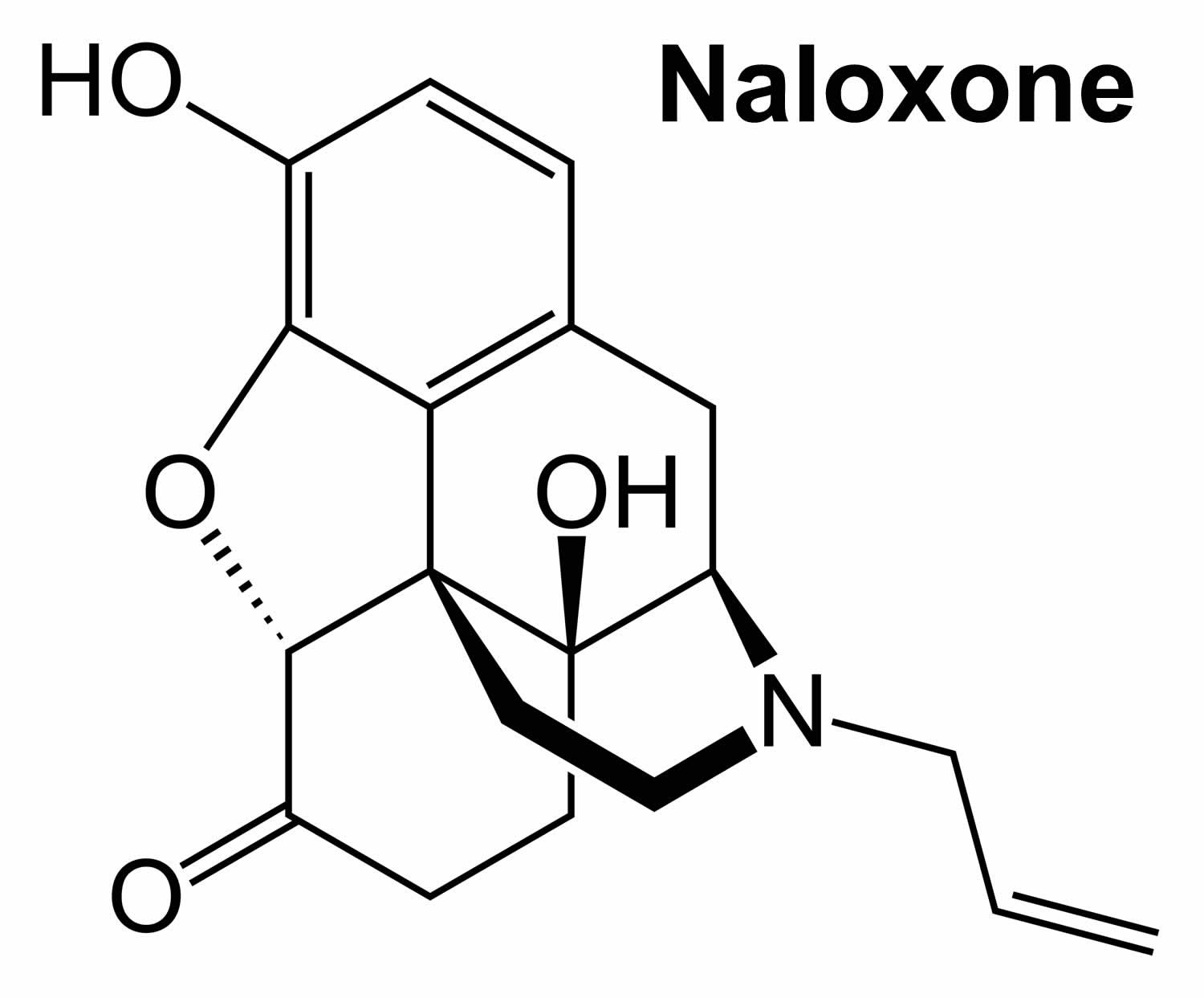
Figure 1. Naloxone chemical structure
How to use and give naloxone
Home preparations include a naloxone nasal spray (Narcan 4mg, Kloxxado 8mg) given to someone while they lie on their back or a device that automatically injects naloxone (Zimhi 5 mg/0.5 mL) into the thigh. Sometimes more than one dose is needed. You may need another naloxone injection every 2 to 3 minutes until emergency help arrives.
The person’s breathing also needs to be monitored. If the person stops breathing, consider rescue breaths and CPR if you are trained until first responders arrive.
Naloxone works to reverse opioid overdose in the body for only 30 to 90 minutes. But many opioids remain in the body longer than that. Because of this, it is possible for a person to still experience the effects of an overdose after a dose of naloxone wears off. Also, some opioids are stronger and might require multiple doses of naloxone. Therefore, one of the most important steps to take is to call your local emergency services number for an ambulance so the individual can receive immediate medical attention.
People who are given naloxone should be observed constantly until emergency care arrives. They should be monitored for another 2 hours after the last dose of naloxone is given to make sure breathing does not slow or stop.
People with physical dependence on opioids may have withdrawal symptoms within minutes after they are given naloxone. Withdrawal symptoms might include headaches, changes in blood pressure, rapid heart rate, sweating, nausea, vomiting, and tremors. While this is uncomfortable, it is usually not life threatening. The risk of death for someone overdosing on opioids is worse than the risk of having a bad reaction to naloxone.
Naloxone injection instructions
- Each naloxone injection contains only one dose of medicine and cannot be reused.
- Place the patient on their back and when you are ready to inject, pull off cap to expose needle.
- Do not put your finger on top of the device. For a child under the age of 1 years old, pinch the thigh muscle while administering the dose.
- Hold naloxone injection by finger grips only and slowly insert the needle into the thigh.
- After needle is in thigh you should push the plunger all the way down until it clicks and then hold for 2 seconds.
- Right after the injection, using one hand with fingers behind the needle, slide the safety guard over the needle. You should not use two hands to activate the safety guard. Put the used syringe into the blue case and close the case.
Naloxone nasal spray instructions
To give naloxone nasal spray, follow these steps:
- Lay the person on their back to give the medication. Support their neck with your hand and allow the head to tilt back before giving the nasal spray.
- Remove the naloxone nasal spray from the box. Peel back the tab to open the spray.
- Do not prime the nasal spray before using it.
- Hold the naloxone nasal spray with your thumb on the bottom of the plunger and your first and middle fingers on either side of the nozzle.
- Gently insert the tip of the nozzle into one nostril, until your fingers on either side of the nozzle are against the bottom of the person’s nose. Provide support to the back of the person’s neck with your hand to allow the head to tilt back.
- Press the plunger firmly to release the medication.
- Remove the nasal spray nozzle from the nostril after giving the medication.
- Turn the person on their side (recovery position) and call for emergency medical assistance immediately after giving the first naloxone dose.
- If the person does not respond by waking up, to voice or touch, or breathing normally or responds and then relapses, give another dose. If needed, give additional doses (repeating steps 2 through 7) every 2 to 3 minutes in alternate nostrils with a new nasal spray each time until emergency medical assistance arrives.
- Put the used nasal spray(s) back in the container and out of reach of children until you can safely dispose of it.
Ask your pharmacist or doctor for a copy of the manufacturer’s information for the patient.
After giving a dose of naloxone
- You need to get emergency medical help as soon as you have given the injection or nasal spray.
- Tell the healthcare provider that you have given a dose of naloxone.
- Turn the patient on their side to place them in the recovery position after giving them the naloxone.
- If symptoms continue or return after using the naloxone, an additional dose may be needed.
- If you are giving additional doses, use a new naloxone nasal spray or new naloxone injection every 2 to 3 minutes and continue to closely watch the person until emergency help has arrived.
- You may need to perform CPR (cardiopulmonary resuscitation) on the person while you are waiting for emergency help to arrive.
- Using naloxone does not take the place of emergency medical care.
Figure 2. Recovery position
How is naloxone given?
Naloxone should be given to any person who shows signs of an opioid overdose or when an opioid overdose is suspected. Naloxone can be given as a nasal spray (Narcan 4mg, Kloxxado 8mg) or it can be injected (Zimhi 5 mg/0.5 mL) into the muscle, under the skin, or into the veins. Sometimes more than one dose is needed. You may need another naloxone injection every 2 to 3 minutes until emergency help arrives.
The person’s breathing also needs to be monitored. If the person stops breathing, consider rescue breaths and CPR if you are trained until first responders arrive.
Naloxone works to reverse opioid overdose in the body for only 30 to 90 minutes. But many opioids remain in the body longer than that. Because of this, it is possible for a person to still experience the effects of an overdose after a dose of naloxone wears off. Also, some opioids are stronger and might require multiple doses of naloxone. Therefore, one of the most important steps to take is to call your local emergency services number for an ambulance so the individual can receive immediate medical attention.
People who are given naloxone should be observed constantly until emergency care arrives. They should be monitored for another 2 hours after the last dose of naloxone is given to make sure breathing does not slow or stop.
People with physical dependence on opioids may have withdrawal symptoms within minutes after they are given naloxone. Withdrawal symptoms might include headaches, changes in blood pressure, rapid heart rate, sweating, nausea, vomiting, and tremors. While this is uncomfortable, it is usually not life threatening. The risk of death for someone overdosing on opioids is worse than the risk of having a bad reaction to naloxone.
What if I’m not sure if someone has an opioid overdose?
Giving someone naloxone, who is suspected to have an opioid overdose, in an emergency won’t hurt them, but it could save their life! Naloxone will not harm someone who does not have opioids in their system. Naloxone is a opioid antagonist that works in the brain only at the opioid receptor, binding to the receptors and blocking the opioids and the effects of opioids. If someone is having a different medical emergency – such as a diabetic coma or cardiac arrest – and you give them naloxone, the drug won’t have any effect or harm them.
Naloxone is being used more by police officers, emergency medical technicians, and non-emergency first responders than before. In most states, people who are at risk or who know someone at risk for an opioid overdose can be trained on how to give naloxone. Families can ask their pharmacists or health care provider how to use the naloxone devices.
Is naloxone safe?
Yes. There is no evidence of significant adverse reactions to naloxone 3. Administering naloxone in cases of opioid overdose can cause withdrawal symptoms when the person is dependent on opioids; this is uncomfortable without being life threatening 4, 5. The risk that someone overdosing on opioids will have a serious adverse reaction to naloxone is far less than their risk of dying from overdose 6, 7, 8, 9. Naloxone works if a person has opioids in their system and has no harmful effect if opioids are absent. Naloxone should be given to any person who shows signs of an opioid overdose or when an opioid overdose is suspected 10.
What are the different types of naloxone?
Naloxone comes in two FDA-approved forms: injectable naloxone (Zimhi 5 mg/0.5 mL) and prepackaged nasal spray naloxone (Narcan 4mg, Kloxxado 8mg). No matter what dosage form you use, it’s important to receive training on how and when to use naloxone. You should also read the product instructions and check the expiration date.
- Injectable brands of naloxone (Zimhi 5 mg/0.5 mL). Typically, the proper dose must be drawn up from a vial. Usually, it is injected with a needle into muscle, although it also may be administered into a vein or under the skin. The FDA recently approved Zimhi, a single-dose, prefilled syringe that can be injected into the muscle or under the skin.
- Note: Some people use an improvised nasal spray emergency kit not approved by the FDA that combines injectable naloxone with an attachment designed to deliver naloxone through the nose. However, this improvised intranasal device is not easy to assemble, especially when under pressure in an emergency, and requires training beforehand. Additionally, the FDA-approved naloxone devices have been shown to produce substantially higher blood levels of naloxone than the improvised nasal spray. These outcomes suggest that the approved prepackaged nasal spray technology is preferable over non-FDA-approved forms.
- Prepackaged Nasal Spray (generic naloxone, Narcan 4mg, Kloxxado 8mg), is an FDA-approved prefilled, needle-free device that requires no assembly and is sprayed into one nostril while the person lays on their back. This device can also be easier for loved ones and bystanders without formal training to use. (In Europe, Nalscue 1 mg, Nyxoid 2 mg, Ventizolve 1.4 mg).
Is there a preferable naloxone delivery system?
All FDA-approved forms: injectable naloxone (Zimhi 5 mg/0.5 mL) and prepackaged nasal spray naloxone (Narcan 4mg, Kloxxado 8mg) used by first responders deliver the stated dose of naloxone and can be highly effective in reversing an opioid overdose. Study findings released in March 2019 11 suggests that the FDA-approved naloxone devices deliver higher blood levels of naloxone than the improvised nasal devices.
Where can I get naloxone?
Many pharmacies carry naloxone. In some states, you can get naloxone from a pharmacist even if your doctor did not write you a prescription for it. It is also possible to get naloxone from community-based distribution programs, local public health groups, or local health departments, free of charge.
To find naloxone in your area, go to the Naloxone Finder (https://www.getnaloxonenow.org/#getnaloxone)
How much does naloxone cost?
The cost varies depending on where you get the naloxone, how you get it, and what type you get. Patients with insurance should check with their insurance company to see if this medicine is covered. Patients without insurance can check the retail costs at their local pharmacies. Some drug companies have cost assistance programs for patients unable to pay for it.
How does naloxone work?
Naloxone is an opioid antagonist, which means that it binds to opioid receptors and reverses or blocks the effects of other opioids. Naloxone is so strongly attracted to the receptors that it knocks other opioids off. When opioids are sitting on their receptors, they change the activity of the cell.
Opioid receptors are found on nerve cells all around the body:
- In the brain, opioids produce feelings of comfort and sleepiness.
- In the brainstem, opioids relax breathing and reduce cough.
- In the spinal cord and peripheral nerves, opioids slow down pain signals.
- In the gastrointestinal tract, opioids are constipating.
These opioid actions can be helpful. The body actually produces its own opioids called “endorphins,” which help calm the body in times of stress. Endorphins help produce the “runner’s high” that helps marathon runners get through grueling races. But opioid drugs, like prescription pain medications or heroin, have much stronger opioid effects. And they are more dangerous.
Over time, frequent opioid use makes the body dependent on the drugs. When the opioids are taken away, the body reacts with withdrawal symptoms such as headache, racing heart, soaking sweats, vomiting, diarrhea, and tremors. For many, the symptoms feel unbearable.
Over time, opioid receptors also become less responsive and the body develops tolerance to the drugs. More drugs are needed to produce the same effects, which makes overdose more likely.
Opioid overdose is dangerous especially for its effect in the brainstem, relaxing breathing. Breathing can be relaxed so much that it stops, leading to death.
Naloxone knocks opioids off their receptors all around the body. In the brainstem, naloxone can restore the drive to breathe. And save a life.
But even if naloxone is successful, opioids are still floating around, so expert medical care should be sought as soon as possible. Naloxone works for 30-90 minutes before the opioids return to their receptors.
Naloxone may promote withdrawal because it knocks opioids off their receptors so quickly. But otherwise naloxone is safe and unlikely to produce side effects.
Naloxone uses
Naloxone is used to treat a known or suspected opioid overdose emergency in children or adults. Signs of an opioid overdose may include:
- slowed breathing, or no breathing;
- very small or pinpoint pupils in the eyes;
- slow heartbeats; or
- extreme drowsiness, especially if you cannot wake the person from sleep.
Even if you are not sure an opioid overdose has occurred, if the person is not breathing or is unresponsive, give the naloxone right away and then seek emergency medical care.
Naloxone has different uses when used in multi-ingredient medications including buprenorphine with naloxone (Suboxone, Zubsolv, Bunavail) which is used to treat opioid addiction, and naloxone with oxycodone (Targiniq ER) which is used for pain.
Buprenorphine and naloxone
Buprenorphine and naloxone is a combination medicine used to treat Opioid Use Disorder or opioid addiction to short-acting opioids such as heroin, morphine, and codeine, as well as semi-synthetic opioids like oxycodone and hydrocodone. Buprenorphine is an opioid partial agonist (a weak opioid medication). Buprenorphine produces effects such as euphoria or respiratory depression at low to moderate doses. With buprenorphine, however, these effects are weaker than full opioid agonists such as methadone and heroin. Naloxone is a opioid antagonist that works by attaching to opioid receptors, which means that it blocks opioid receptors from being activated. Naloxone is so strongly attracted to the opioid receptors that it knocks other opioids off. Buprenorphine and naloxone operate to normalize brain chemistry, block the euphoric effects of opioids, relieve physiological cravings, and normalize body functions without the negative and euphoric effects of the substance used.
Buprenorphine and naloxone are safe to use for months, years, or even a lifetime. As with any medication, consult your doctor before discontinuing use.
The following buprenorphine products are FDA approved for the treatment of Opioid Use Disorder (opioid addiction):
- Generic Buprenorphine/naloxone sublingual tablets
- Buprenorphine sublingual tablets (Subutex)
- Buprenorphine and naloxone sublingual films (Suboxone)
- Buprenorphine and naloxone sublingual tablets (Zubsolv)
- Buprenorphine and naloxone buccal film (Bunavail)
- Buprenorphine implants (Probuphine)
- Buprenorphine extended-release injection (Sublocade)
When taken as prescribed, buprenorphine is safe and effective. Buprenorphine has unique pharmacological properties that help:
- Diminish the effects of physical dependency to opioids, such as withdrawal symptoms and cravings
- Increase safety in cases of overdose
- Lower the potential for misuse
Naloxone dosage
Adult dose for opioid overdose
Auto-injector
- Administer 0.4 mg (1 actuation) IM or subcutaneously into the anterolateral aspect of the thigh (through clothing if necessary)
- If the desired response is not achieved, a second dose may be administered after 2 or 3 minutes; additional doses may be administered every 2 to 3 minutes until emergency medical assistance arrives
Nasal Spray:
- Administer 1 spray intranasally into 1 nostril
- If the desired response is not achieved after 2 or 3 minutes, give a second dose intranasally into alternate nostril; additional doses may be administered every 2 to 3 minutes in alternating nostrils until emergency medical assistance arrives
Comments:
- IV route is recommended in emergency situations since it has the most rapid onset of action.
- The duration of action of some opioids exceed that of this drug, therefore, repeat doses may be needed; the need for repeat doses will depend on the amount, type, and route of administration of the opioid being antagonized.
Children dose for opioid overdose
Neonates
- Initial dose: 0.01 mg/kg IV, IM, or subcutaneously; repeat dose every 2 to 3 minutes as needed
Children
- Initial dose: 0.01 mg/kg IV; if desired response is not obtained, may give 0.1 mg/kg IV
- If IV route is not available may give IM or subcutaneously in divided doses.
- Administer 0.4 mg (1 actuation) IM or subcutaneously into the anterolateral aspect of the thigh (through clothing if necessary); if desired response is not achieved, a second dose may be administered after 2 or 3 minutes; additional doses may be administered every 2 to 3 minutes until emergency medical assistance arrives
- Under 1 year of age: Thigh muscle should be pinched while administering injection
Comments:
- Neonatal opioid withdrawal syndrome may be life-threatening and should be treated according to protocols developed by neonatology experts.
- To avoid precipitating opioid withdrawal symptoms, consider use of a naloxone product that can be dosed according to weight and titrated to effect.
- The duration of action of some opioids will exceed that of this drug, therefore, repeat doses may be needed; the need for repeat doses will depend on the amount, type, and route of administration of the opioid being antagonized.
- Patients should remain under continued surveillance; if a patients responds and relapses back into respiratory depression, additional doses should be given.
- Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
Naloxone side effects
Side effects from naloxone are rare, but people might have allergic reactions to naloxone or any ingredients in naloxone. You should not be treated with naloxone if you are allergic to naloxone or any ingredients in naloxone injection or naloxone nasal spray. Get emergency medical help if you have signs of an allergic reaction to naloxone: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
In general, naloxone is a safe medicine. But it only reverses an overdose in people with opioids in their systems and will not reverse overdoses from other drugs like cocaine or methamphetamine.
Naloxone nasal spray may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- headache
- nasal dryness, nasal swelling, or congestion
- muscle pain
Some naloxone side effects can be serious. If you experience any of these symptoms, get emergency medical treatment:
- signs of opiate withdrawal such as body aches, diarrhea, fast, pounding, or irregular heartbeat, fever, runny nose, sneezing, sweating, yawning, nausea, vomiting, nervousness, restlessness, irritability, shivering, trembling, stomach cramps, weakness, and the appearance of hair on the skin standing on end
- seizures
- loss of consciousness
- crying more than usual (in babies treated with naloxone nasal spray)
- stronger than normal reflexes (in babies treated with naloxone nasal spray)
Because naloxone reverses opioid effects, the administration may cause sudden opioid withdrawal symptoms such as:
- nausea, vomiting, diarrhea, stomach pain;
- fever, sweating, body aches, weakness;
- tremors or shivering, fast heart rate, pounding heartbeats, increased blood pressure;
- goose bumps, shivering;
- runny nose, yawning; or
- feeling nervous, restless, or irritable.
Naloxone injection may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- pain, burning, or redness at the injection site
- sweating
- hot flashes or flushing
Some naloxone injection side effects can be serious. If you experience any of these symptoms, get emergency medical treatment:
- rapid, pounding, or irregular heartbeat
- seeing things or hearing voices that do not exist (hallucinations)
- loss of consciousness
- seizures
- signs of opiate withdrawal such as body aches, diarrhea, fast heart beat, fever, runny nose, sneezing, sweating, yawning, nausea, vomiting, nervousness, restlessness, irritability, shivering or trembling, stomach cramps, weakness, and the appearance of hair on the skin standing on end
- crying more than usual (in babies treated with naloxone injection)
- stronger than normal reflexes (in babies treated with naloxone injection)
Using naloxone while you are pregnant may cause opioid withdrawal effects in your unborn baby. However, having an opioid overdose can be fatal to both mother and baby. It is much more important to treat an overdose in the mother. You must get emergency medical help after using naloxone. Be sure all emergency medical caregivers know that you are pregnant.
In an emergency, you may not be able to tell caregivers if you are pregnant or breastfeeding. Make sure any doctor caring for your pregnancy or your baby knows you received naloxone.
If you use opioid medicine while you are pregnant, your baby could become dependent on the drug. This can cause life-threatening withdrawal symptoms in the baby after it is born. Babies born dependent on opioids may need medical treatment for several weeks.
Sudden opioid withdrawal symptoms in a baby younger than 4 weeks old may be life-threatening if not treated the right way. Symptoms include crying, stiffness, overactive reflexes, and seizures. Call your doctor or get emergency medical help if you are unsure how to properly give naloxone to a baby.
- Narcan (naloxone nasal spray) Approved to Reverse Opioid Overdose. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/narcan-naloxone-nasal-spray-approved-reverse-opioid-overdose[↩]
- Strang J, McDonald R, Campbell G, Degenhardt L, Nielsen S, Ritter A, Dale O. Take-Home Naloxone for the Emergency Interim Management of Opioid Overdose: The Public Health Application of an Emergency Medicine. Drugs. 2019 Sep;79(13):1395-1418. doi: 10.1007/s40265-019-01154-5[↩]
- Wermeling DP. Review of naloxone safety for opioid overdose: practical considerations for new technology and expanded public access. Ther Adv Drug Saf. 2015 Feb;6(1):20-31. doi: 10.1177/2042098614564776[↩]
- Belz D, Lieb J, Rea T, Eisenberg MS. Naloxone use in a tiered-response emergency medical services system. Prehosp Emerg Care. 2006 Oct-Dec;10(4):468-71. doi: 10.1080/10903120600885134[↩]
- Buajordet I, Naess AC, Jacobsen D, Brørs O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emerg Med. 2004 Feb;11(1):19-23. doi: 10.1097/00063110-200402000-00004[↩]
- Kerr, D., Kelly, A.-M., Dietze, P., Jolley, D. and Barger, B. (2009), Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction, 104: 2067-2074. https://doi.org/10.1111/j.1360-0443.2009.02724.x[↩]
- Waraich, B.K., Chavan, B.S. and Raj, L. (2003), Inhalant abuse: a growing public health concern in india. Addiction, 98: 1169-1169. https://doi.org/10.1046/j.1360-0443.2003.00469.x[↩]
- Osterwalder JJ. Naloxone–for intoxications with intravenous heroin and heroin mixtures–harmless or hazardous? A prospective clinical study. J Toxicol Clin Toxicol. 1996;34(4):409-16. doi: 10.3109/15563659609013811[↩]
- Strang J, Darke S, Hall W, Farrell M, Ali R. Heroin overdose: the case for take-home naloxone. BMJ. 1996 Jun 8;312(7044):1435-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2351168/pdf/bmj00545-0009.pdf[↩]
- Still Not Enough Naloxone Where It’s Most Needed. https://www.cdc.gov/media/releases/2019/p0806-naloxone.html[↩]
- Krieter, P.A., Chiang, C.N., Gyaw, S. and McCann, D.J. (2019), Comparison of the Pharmacokinetic Properties of Naloxone Following the Use of FDA-Approved Intranasal and Intramuscular Devices Versus a Common Improvised Nasal Naloxone Device. The Journal of Clinical Pharmacology, 59: 1078-1084. https://doi.org/10.1002/jcph.1401[↩]