Contents
What is naltrexone
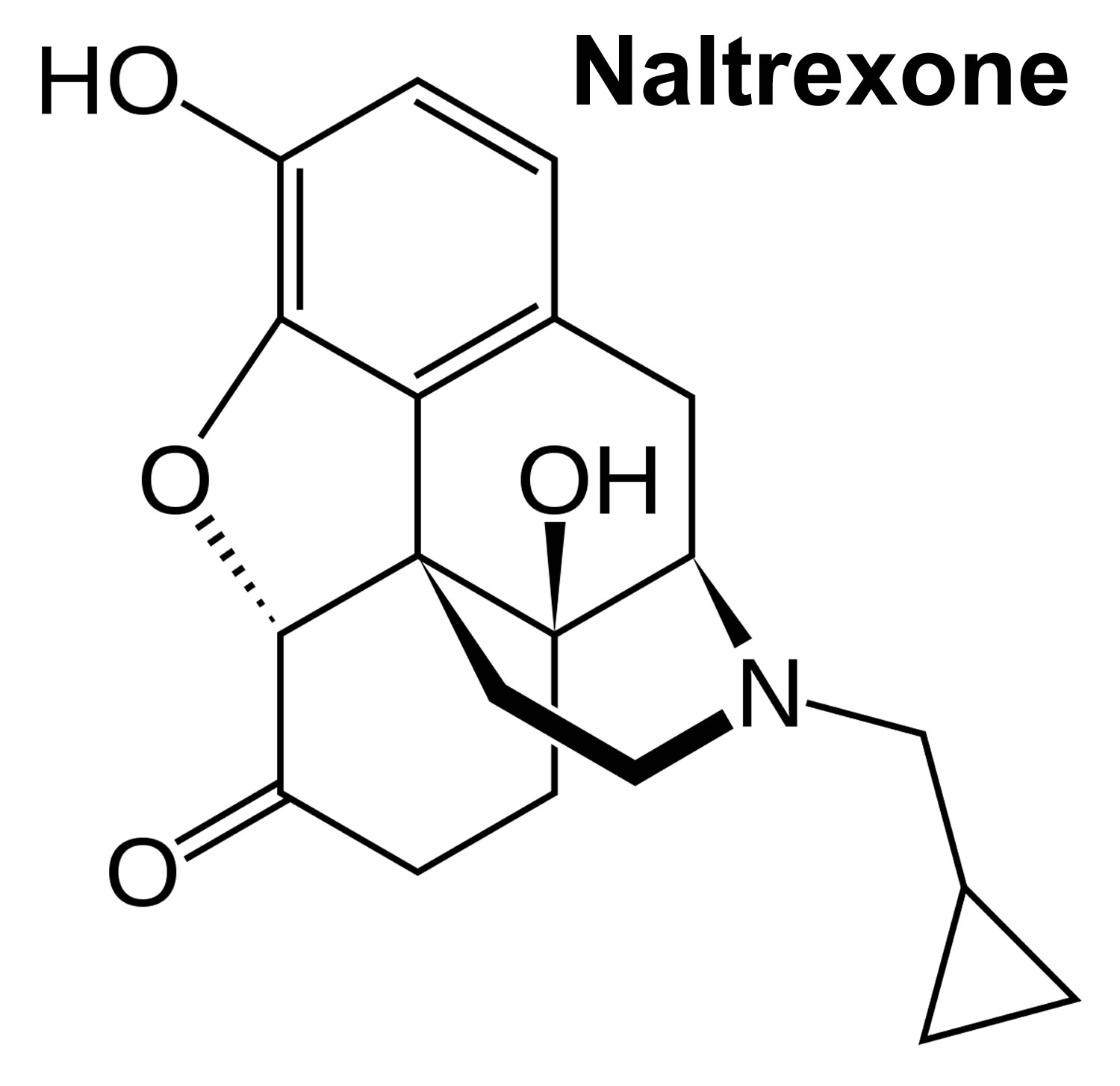
Naltrexone is an opioid antagonist (opioid blocker) which primarily, but not exclusively, targets the μ-opioid receptor 1. Naltrexone is to be given only by or under the direct supervision of your doctor. Naltrexone is used to help narcotic dependents who have stopped taking narcotics to stay drug-free. Naltrexone is also used to help alcoholics stay alcohol-free. Naltrexone is not a cure for addiction and naltrexone is used as part of an overall program that may include counseling, attending support group meetings, and other treatment recommended by your doctor.
Naltrexone is not a narcotic. It works by blocking the effects of narcotics, especially the “high” feeling that makes you want to use them. Naltrexone also may block the “high” feeling that may make you want to use alcohol. Naltrexone will not produce any narcotic-like effects or cause mental or physical dependence. Naltrexone will not prevent you from becoming impaired while drinking alcohol.
Naltrexone will cause withdrawal symptoms in people who are physically dependent on narcotics. Therefore, naltrexone treatment is started after you are no longer dependent on narcotics. The length of time this takes may depend on which narcotic you took, the amount you took, and how long you took it. Before you start using naltrexone, be sure to tell your doctor if you think you are still having withdrawal symptoms.
Since its approval by the U.S. Food and Drug Administration (FDA) as an adjuvant therapy for the treatment of alcohol‐dependent patients in 1994, naltrexone has been introduced to the market in many countries all over the world. In April 2006, the FDA approved a new extended‐release injectable formulation of naltrexone for the treatment of alcohol dependence. The safety profile of naltrexone is well known when used for approved indications at the standard dose of 50 mg/day. The FDA issued a black box warning concerning hepatotoxicity in high doses (>300 mg/day), but this has not been considered a clinical problem at standard doses 2.
Naltrexone may cause liver damage when taken in large doses. It is not likely that naltrexone will cause liver damage when taken in recommended doses. Tell your doctor if you have or have ever had hepatitis or liver disease. If you experience any of the following symptoms, stop taking naltrexone and call your doctor immediately: excessive tiredness,unusual bleeding or bruising, loss of appetite, pain in the upper right part of your stomach that lasts more than a few days, light-colored bowel movements,dark urine, or yellowing of the skin or eyes.
Keep all appointments with your doctor and the laboratory. Your doctor may order certain laboratory tests to check your body’s response to naltrexone.
Talk to your doctor about the risks of taking naltrexone.
Alcohol dependence is a chronic disease, which can develop when alcohol is heavily consumed over longer periods of time. Alcohol affects various brain regions, including the opioid receptor system, which mediates euphoric and pleasurable effects of alcohol. By blocking alcohol effects at these receptors, the opioid antagonists naltrexone (and nalmefene) can reduce alcohol “liking” and “craving” and thus support alcohol dependent patients in cutting down their drinking 3. A 2010 Cochrane Review 3 of 50 studies with 7793 participants found patients who took naltrexone were able to reduce the amount and frequency of drinking than those who took placebo (i.e. a fake drug). On average, one out of nine patients was helped by naltrexone 3. Furthermore, naltrexone does not have serious side effects, but gastrointestinal symptoms like nausea, stomach pain and loss of appetite are common 3. Some patients also get tired from naltrexone 3. For injectable formulations of naltrexone, which can be advantageous for patients who have problems with taking their medication on schedule, the data is still too sparse to allow final conclusions. Naltrexone does not cause dependency and unlike disulfiram, another medicine that is sometimes used to treat alcohol dependence, naltrexone does not make patients feel sick if they drink alcohol while taking it.
Despite these positive outcomes associated with oral naltrexone treatment, non-compliance with oral naltrexone formulae has been a major impediment to achieving positive clinical outcomes for a significant number of patients. A meta-analysis found that 37% of patients discontinue daily oral naltrexone use by 12 weeks (placebo 43%) 3, with other data indicating more than 80% of patients discontinued use by 6 months 4. Non-compliance is often associated with a patient’s withdrawal from treatment, return to alcohol abuse/dependence 5 and greater use of costly health care services, i.e. emergency departments and hospitals 6. A survey in US showed that 80% of physicians indicated that their decision to prescribe oral naltrexone, albeit for opiate dependence, was based on their opinion about whether the patient would comply with medication 7. A study comparing combined efficacy of behavioral treatment and naltrexone found a doubling in the effect size of the oral naltrexone by therapy interactions when the analysis was performed only on the subgroup of oral naltrexone compliant patients 8. Clearly, if naltrexone treatment for alcohol dependence is to have ‘real world’ clinical utility, attention must be focused on ways to improve medication compliance. For patients, who take naltrexone regularly, therapeutic benefits are likely to exceed those demonstrated in clinical trials.
How does naltrexone work?
Naltrexone likely exerts its actions by blockade of the high concentration of μ-opioid receptors (mu‐opioid receptors) located in areas of the brain that have been implicated in the reward pathway associated with alcohol 9. Naltrexone is originally used for the treatment of opioid dependence to prevent a relapse to opioid use after heroin detoxification and to treat accidental heroin overdose. In animal models of alcohol dependence, naltrexone was shown to decrease the alcohol intake under free‐choice conditions 10 and to prevent the development of a conditioned place preference for alcohol 11 indicating that the opioid antagonist does not only block the immediate release of endorphins and dopamine, but also influences conditioned processes induced by drinking‐associated stimuli, known as “conditioned high” 12.
Alcohol affects various transmitter systems in the brain, including the endogenous opioid receptors, which are assumed to mediate pleasant and euphoric effects of drinking 13. As naltrexone competitively bind to these receptors, they block the endogenous opioids at these sites 14 and thus diminish the pleasant and euphoric effects of drinking. This explains why patients given naltrexone in combination with alcohol reported a reduced “high” compared to former drinking 15. As changes in the opioid system also have a modulator influence on the mesolimbic dopamine system, especially on dopamine neurons in the ventral tegmental area and their projections to the nucleus accumbens in the ventral striatum ‐ the predominant pathway involved in reinforcement and motivation 16 ‐ naltrexone is also assumed to mediate motivational processes including reward anticipation and reinforcement.
Oral naltrexone is relatively safe and has a moderate to good clinical efficacy in the management of persons with alcohol dependence 17. Meta-analysis studies have concluded that the use of naltrexone is most appropriate where controlled drinking is the desired outcome 18. Another study suggests that the treatment effectiveness of naltrexone is greater during active alcohol consumption and depends on aversive side effects 19. Naltrexone is also associated with significant improvements on a number of other clinical measures including increased time to alcohol relapse, number of drinks per drinking day, improved liver function indicators [γ-glutamyl transferase (GGT), aspartate aminotransferase (AST)] and reduction in alcohol craving 20. An evaluation of the comparative cost of treating alcohol dependence with either cognitive behavioural therapy (CBT) alone or cognitive behavioural therapy combined with oral naltrexone over a 12 week treatment programme showed that the addition of naltrexone significantly improved abstinence rates (36.1% cognitive behavioural therapy, 62.6% cognitive behavioural therapy + naltrexone) and although adding 54% to treatment costs, was found to be the most effective treatment option 21. Despite the aforementioned there are few data on oral naltrexone treatment beyond 12 weeks and limited long term follow-up data 20. Therefore, it is speculative to generalize to ‘real world’ utility of naltrexone.
A growing body of research has sought to evaluate mental health outcomes of patients following naltrexone pharmacotherapy treatment, both those with a history of psychiatric morbidity, and the emergence of psychiatric morbidity in those without previous mental health morbidity. Specifically, concern has been raised of a possible increase in the incidence of depression or dysphoric mood disorder following treatment with naltrexone, due to its antagonistic effect on endogenous opioid receptors 22. However, the evidence for this has been mixed, with some investigators reporting mild dysphoria in ‘healthy, drug free’ persons following administration of naltrexone 23, while others have reported no change in incidence of depression [44] or an improvement in depressive symptoms among depressed alcoholics 24.
Data on mental health outcomes associated with sustained release naltrexone are limited. As noted earlier, a review of 124 alcohol dependent patients treated with naltrexone implant showed a significant reduction in mental health admissions (64.1%) in the 12 months post- compared with pre-treatment 9. Given the high prevalence of mental health disorders amongst persons with problem alcohol use there is an urgent need to determine mental health following naltrexone implant treatment for alcohol.
Low dose naltrexone
In the past two decades, naltrexone in low doses (<5 mg/day or 3 to 5 mg per day, have often been termed low dose naltrexone) has gained popularity among some patients and doctors as off-label treatment of multiple sclerosis (MS) and other autoimmune diseases like Crohn’s disease, amyotrophic lateral sclerosis (ALS), fibromyalgia, cancer, inflammatory bowel disease, chronic fatigue syndrome, psoriasis, and rheumatoid arthritis 25, 26. Few studies have investigated the efficacy of low dose naltrexone in multiple sclerosis (MS), hence low dose naltrexone should be considered an experimental, alternative therapy.
Ringerike and colleagues 25 have summarized the data from a systematic review and several randomized controlled and prospective controlled studies in order to investigate the effect of using naltrexone in low doses on illness, and on functioning in daily life and to examine the risk of side effects.
Ringerike and colleagues have identified studies for people with:
- Crohn’s disease (one systematic review, two studies)
- multiple sclerosis (two studies)
- fibromyalgia (two studies)
- cancer (one study)
- HIV (one study)
- various pain conditions (three studies)
- opioid dependence (six studies)
All studies were either small, of short duration, or had other methodological limitations. The review authors considered the documentation to have very low quality. Based on current the evidence, it is not possible to determine whether low-dose naltrexone is effective and safe for any of the above conditions. Neither is it possible to determine whether there are differences in efficacy between different patient groups. There is a need for well-planned and well-conducted randomized controlled trials of long enough duration to reliably capture any effects, to investigate whether effects persists over time, and if side effects occur during long-term use.
A 2018 Cochrane Review 27 found insufficient evidence to allow any firm conclusions regarding the efficacy and safety of low-dose naltrexone used to treat patients with active Crohn’s disease. Data from one small study suggests that low dose naltrexone may provide a benefit in terms of clinical and endoscopic response in adult patients with active Crohn’s disease. Data from two small studies suggest that low-dose naltrexone does not increase the rate of specific adverse events relative to placebo. However, these results need to be interpreted with caution as they are based on small numbers of patients and the overall quality of the evidence was rated as low due to serious imprecision.
Naltrexone vs Naloxone
Naloxone is a short-acting, broad opioid receptor antagonist that is used in the treatment of opioid overdose to reverse the respiratory and central nervous system-depressant effects of the opioid 28. Naloxone binds to opioid receptors with high affinity and becomes a competitive antagonist of opioid receptors 29. Naloxone is an opioid antagonist—meaning that it binds to opioid receptors and can reverse and block the effects of other opioids. Naloxone can very quickly restore normal respiration to a person whose breathing has slowed or stopped as a result of overdosing with heroin or prescription opioid pain medications. When administered in low doses, naloxone can reverse opioid side effects such as respiratory depression, sedation and hypotension without significantly reversing analgesia. At high doses, however, naloxone can block opioid analgesia causing precipitated opioid withdrawal 30.
- Naloxone is administered when a patient is showing signs of opioid overdose. The medication can be given by intranasal spray, intramuscular (into the muscle), subcutaneous (under the skin), or intravenous injection.
- Naloxone is effective if opioids are misused in combination with other sedatives or stimulants. It is not effective in treating overdoses of benzodiazepines or stimulant overdoses involving cocaine and amphetamines.
- Pregnant women can be safely given naloxone in limited doses under the supervision of a doctor.
- A doctor or pharmacist can show patients, their family members, or caregivers how to administer naloxone. Intravenous injection every two to three minutes is recommended in emergencies.
- Patients given an automatic injection device or nasal spray should keep the item available at all times. Medication should be replaced when the expiration date passes.
- Naloxone is also added to buprenorphine to decrease the likelihood of diversion and misuse of the combination drug product.
Opioid overdose can happen:
- When a patient misunderstands the directions for use, accidentally takes an extra dose, or deliberately misuses a prescription opioid or an illicit drug like heroin
- If a person takes opioid medications prescribed for someone else
- If a person mixes opioids with other medications, alcohol, or over-the-counter drugs
Opioid overdose is life-threatening and requires immediate emergency attention. Recognizing the signs of opioid overdose is essential to saving lives.
Naloxone injection is traditionally given by intravenous, intramuscular, and subcutaneous routes. Paramedics also administer naloxone injection intranasally in the prehospital setting to treat suspected opioid overdose. The nasal mucosa has a rich blood supply that allows for efficient drug absorption and the avoidance of first-pass hepatic metabolism that would be seen with oral administration. Obtaining vascular access can be difficult in known drug users, prolonging the time required to administer the antidote. Patients awakening from an overdose may be agitated, confused, and even combative, thus increasing the risk of needle-stick injury to first responders. The intranasal route avoids the need for establishing vascular access and can be associated with speedier patient recovery. In two randomized controlled trials, intranasal naloxone alone was shown to be sufficient for reversing opioid-induced respiratory depression in 74% and 72% of the respective study populations of patients experiencing opioid overdose. In addition, the safety profile of intranasal naloxone appears to be no different than that of naloxone injection in the treatment of opioid overdose in the prehospital setting 28.
How is naloxone given?
There are three FDA-approved formulations of naloxone:
Injectable (professional training required)
Generic brands of injectable naloxone vials are offered by a variety of companies that are listed in the FDA Orange Book under “naloxone” (look for “injectable”).
Note: There has been widespread use of improvised emergency kits that combine an injectable formulation of naloxone with an atomizer that can deliver naloxone intranasally. Use of this product requires the user to be trained on proper assembly and administration. These improvised intranasal devices may not deliver naloxone levels equivalent to FDA-approved products. In fact, the manufacturer of an internasal atomizer device issued a voluntary recall on 10/27/2016 (http://www.ct.gov/dmhas/lib/dmhas/newsworthy/mad_recall.pdf) noting that some of the devices “may not deliver a fully atomized plume of medication, making the drug potentially less effective.” An approved, prefilled nasal spray is now available (see below).
Autoinjectable
EVZIO® is a prefilled auto-injection device that makes it easy for families or emergency personnel to inject naloxone quickly into the outer thigh. Once activated, the device provides verbal instruction to the user describing how to deliver the medication, similar to automated defibrillators.
Prepackaged Nasal Spray
NARCAN® Nasal Spray is a prefilled, needle-free device that requires no assembly and is sprayed into one nostril while patients lay on their back.
Note: Both NARCAN® Nasal Spray and EVZIO® are packaged in a carton containing two doses to allow for repeat dosing if needed. They are relatively easy to use and suitable for home use in emergency situations.
Who can give naloxone to someone who has overdosed?
The liquid for injection is commonly used by paramedics, emergency room doctors, and other specially trained first responders. To facilitate ease of use, NARCAN® Nasal Spray is now available, which allows for naloxone to be sprayed into the nose. While improvised atomizers have been used in the past to convert syringes for use as nasal spray, these may not deliver the appropriate dose. Depending on the state you live in, friends, family members, and others in the community may give the auto-injector and nasal spray formulation of naloxone to someone who has overdosed. Some states require a physician to prescribe naloxone; in other states, pharmacies may distribute naloxone in an outpatient setting without bringing in a prescription from a physician.
What dose can be provided?
The dose varies depending on the formulation, and sometimes more than one dose is needed to help the person start breathing again. Anyone who may have to use naloxone should carefully read the package insert that comes with the product. You can find copies of the package insert for EVZIO® (https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/205787Orig1s000Lbl.pdf) and NARCAN® (https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208411lbl.pdf) Nasal Spray on the FDA website.
What precautions are needed when giving naloxone?
People who are given naloxone should be observed constantly until emergency care arrives and for at least 2 hours by medical personnel after the last dose of naloxone to make sure breathing does not slow or stop.
What are the side effects of naloxone?
Naloxone is an extremely safe medication that only has a noticeable effect in people with opioids in their systems. Naloxone can (but does not always) cause withdrawal symptoms which may be uncomfortable, but are not life-threatening; on the other hand, opioid overdose is extremely life-threatening. Withdrawal symptoms may include headache, changes in blood pressure, rapid heart rate, sweating, nausea, vomiting, and tremors.
Use of naloxone may cause symptoms of opioid withdrawal, including:
- Feeling nervous, restless, or irritable
- Body aches
- Dizziness or weakness
- Diarrhea, stomach pain, or nausea
- Fever, chills, or goose bumps
- Sneezing or runny nose in the absence of a cold
How much does naloxone cost?
The cost varies depending on where and how you get it. Patients with insurance should check with their insurance company to see what their co-pay is for EVZIO® or NARCAN® Nasal Spray. Patients without insurance can check on the retail costs with their local pharmacies. Kaleo, the maker of EVZIO®, has a cost assistance program (https://evzio.com/patient/index.php) for patients with financial difficulties and no insurance.
Where can I get naloxone?
Naloxone is a prescription drug. You can buy naloxone in many pharmacies, in some cases without bringing in a prescription from a physician. Law enforcement, EMS, and community-based naloxone distribution programs can apply to be a Qualified Purchaser to order naloxone or work with their state or local health departments. Here are some resources to help you find naloxone in your area:
- Naloxone finder (http://www.getnaloxonenow.org/find.html) – This website also offers access to training for first responders and potential bystanders.
Some states have their own website:
- Pennsylvania (https://www.overdosefreepa.pitt.edu/find-local-resources/find-naloxone/)
- Washington (http://stopoverdose.org/section/find-naloxone-near-you/#inwa)
Some pharmacies offer naloxone in an outpatient setting (without bringing in a prescription from a physician). Check with your local pharmacy. Here is a sampling:
- CVS stores – no prescription needed in Ohio, Arkansas, California, Minnesota, Mississippi, Montana, New Jersey, North Dakota, Pennsylvania, South Carolina, Tennessee, Utah, and Wisconsin
- Walgreens stores – available in many states without a prescription by the end of 2016
- Discount program for EVZIO®
- NARCAN® Nasal Spray.
Naltrexone uses
Naltrexone is a medication approved by the Food and Drug Administration (FDA) to treat opioid use disorders and alcohol use disorders. Naltrexone is to be prescribed as part of a comprehensive treatment plan that includes counseling and participation in social support programs. Naltrexone comes in a pill form or as an injectable. The pill form of naltrexone (ReVia, Depade) can be taken at 50 mg once per day. The injectable extended-release form of the drug (Vivitrol) is administered at 380 mg intramuscular once a month. Naltrexone can be prescribed by any health care provider who is licensed to prescribe medications. To reduce the risk of precipitated withdrawal, patients are warned to abstain from illegal opioids and opioid medication for a minimum of 7-10 days before starting naltrexone. If switching from methadone to naltrexone, the patient has to be completely withdrawn from the opioids.
Naltrexone blocks the euphoric and sedative effects of drugs such as heroin, morphine, and codeine. It works differently in the body than buprenorphine and methadone, which activate opioid receptors in the body that suppress cravings. Naltrexone binds and blocks opioid receptors, and is reported to reduce opioid cravings. There is no abuse and diversion potential with naltrexone.
If a person relapses and uses the problem drug, naltrexone prevents the feeling of getting high. People using naltrexone should not use any other opioids or illicit drugs; drink alcohol; or take sedatives, tranquilizers, or other drugs.
Patients on naltrexone may have reduced tolerance to opioids and may be unaware of their potential sensitivity to the same, or lower, doses of opioids that they used to take. If patients who are treated with naltrexone relapse after a period of abstinence, it is possible that the dosage of opioid that was previously used may have life-threatening consequences, including respiratory arrest and circulatory collapse.
Naltrexone for Opioid Use Disorders
Extended-release injectable naltrexone is approved for treatment of people with opioid use disorder. Extended-release injectable naltrexone can be prescribed by any healthcare provider who is licensed to prescribe medications, special training is not required. It is important that medical managed withdrawal (detoxification) from opioids be completed at least 7 to 10 days before extended-release injectable naltrexone is initiated or resumed. Research has shown that naltrexone decreases reactivity to drug-conditioned cues and decreases craving. Patients who have been treated with extended-release injectable naltrexone may have reduced tolerance to opioids and may be unaware of their potential sensitivity to the same, or lower, doses of opioids that they used to take. Extended-release naltrexone should be part of a comprehensive management program that includes psychosocial support.
Naltrexone for Alcohol Dependence
When used as a treatment for alcohol dependency, naltrexone blocks the euphoric effects and feelings of intoxication. This allows people with alcohol addiction to reduce their drinking behaviors enough to remain motivated to stay in treatment and avoid relapses. Naltrexone is not addictive nor does it react adversely with alcohol.
Long-term naltrexone therapy extending beyond three months is considered most effective by researchers, and therapy may also be used indefinitely.
Naltrexone dosage
Before using naltrexone Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Precautions
Naltrexone may cause hepatic injury when taken in excess or by people who develop liver disease from other causes. Patients that develop abdominal pain lasting more than a few days, white bowel movements, dark urine, or yellowing of the eyes, should stop taking naltrexone immediately and see a doctor as soon as possible. There may be a higher risk of hepatocellular injury with single doses greater than 50 mg, and use of higher doses and extended dosing intervals should balance the possible risks against the probable benefits.
Safety and effectiveness have not been established in pediatric patients (less than 18 years of age).
Pregnancy (All Trimesters)
Pregnancy Category C: Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Children
Appropriate studies have not been performed on the relationship of age to the effects of naltrexone injection in the pediatric population. Safety and efficacy have not been established.
Older Adults
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of naltrexone injection in the elderly.
Adult Dose for Alcohol Dependence
- Oral Tablets: 50 mg orally once a day
- Extended-release injectable suspension: 380 mg every 4 weeks (or once a month) via intramuscular gluteal injection, alternating buttocks
Adult Dose for Opiate Dependence
Treatment should not be attempted unless the patient has remained free of opioids for at least 7 to 10 days. Opioid abstinence should be verified by analysis of urine for absence of opioids. The patient should not be manifesting withdrawal signs or reporting withdrawal symptoms. If there is any question of occult opioid dependence, perform a naloxone challenge test and do not initiate naltrexone therapy until the naloxone challenge is negative. The naloxone challenge test should not be performed in a patient showing clinical signs or symptoms of opioid withdrawal, or whose urine contains opioids. The naloxone challenge can be repeated in 24 hours.
- Initial dose: 25 mg orally one time.
- Maintenance dose: If no withdrawal signs occur, 50 mg orally once a day may be started.
- Alternative dose schedules: (to improve compliance) 50 mg orally on week days and 100 mg orally on Saturday; or 100 mg orally every other day; or 150 mg orally every third day.
- Extended-release injectable suspension: 380 mg every 4 weeks (or once a month) via intramuscular gluteal injection, alternating buttocks
Renal Dose Adjustments
Urinary excretion is the primary route of elimination for the active metabolites of naltrexone. Data are lacking concerning the safety and disposition of oral naltrexone in patients with renal dysfunction, and there are no data on the recommended oral dose of naltrexone in patients with renal dysfunction.
No dosage adjustment is required in patients with mild renal dysfunction (CrCl 50 to 80 mL/min) who are receiving the extended-release injectable suspension. However, there are no data on the pharmacokinetic disposition of injectable naltrexone in patients with moderate to severe renal dysfunction (CrCl less than 50 mL/min).
Liver Dose Adjustments
Naltrexone undergoes extensive hepatic metabolism and has the potential to cause further hepatic injury in patients with liver dysfunction. Therefore, the use of naltrexone is not recommended in patients with acute hepatitis or liver failure and should be used with caution in patients with active liver disease.
No dosage adjustment is required in patients with mild or moderate liver dysfunction who are receiving the extended-release suspension.
Naltrexone side effects
People taking naltrexone may experience side effects, but they should not stop taking the medication. Instead, they should consult their health care provider or substance misuse treatment practitioner to adjust the dose or change the medication. Some side effects include:
- Upset stomach or vomiting
- Diarrhea
- Headache
- Nervousness
- Sleep problems/tiredness
- Joint or muscle pain
Seek a health care provider right away for:
- Liver injury: Naltrexone may cause liver injury. Seek evaluation if have symptoms and or signs of liver disease.
- Injection site reactions: This may occur from the injectable naltrexone. Seek evaluation for worsening skin reactions.
- Allergic pneumonia: It may cause an allergic pneumonia. Seek evaluation for signs and symptoms of pneumonia.
Some side effects of naltrexone may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More Common
- abdominal or stomach cramping or pain (mild or moderate)
- anxiety, nervousness, restlessness or trouble sleeping
- headache
- joint or muscle pain
- nausea or vomiting
- unusual tiredness
Less Common
- chills
- constipation
- cough, hoarseness, runny or stuffy nose, sinus problems, sneezing, or sore throat
- diarrhea
- dizziness
- fast or pounding heartbeat
- increased thirst
- irritability
- loss of appetite
- sexual problems in males
- skin rash
Rare
- abdominal or stomach pain (severe)
- blurred vision, aching, burning, or swollen eyes
- chest pain
- confusion
- discomfort while urinating or frequent urination
- fever
- hallucinations or seeing, hearing, or feeling things that are not there
- itching
- mental depression or other mood or mental changes
- ringing or buzzing in the ears
- shortness of breath
- swelling of the face, feet, or lower legs
- weight gain
Nervous system
- Very common (10% or more): Headache (25%), dizziness/syncope (13%)
- Common (1% to 10%): Somnolence/sedation
- Frequency not reported: Lethargy, cerebral arterial aneurysm, convulsions, disturbance in attention, dysgeusia, mental impairment, migraine, ischemic stroke, paresthesia
Psychiatric
- Very common (10% or more): Insomnia/sleep disorder (14%), anxiety (12%)
- Common (1% to 10%): Depression
- Uncommon (0.1% to 1%): Suicide attempt/ideation
- Frequency not reported: Irritability, abnormal dreams, agitation, alcohol withdrawal syndrome, euphoric mood, delirium, libido decreased
Gastrointestinal
- Very common (10% or more): Nausea (33%), vomiting NOS (14%), diarrhea (13%), abdominal pain (11%)
- Common (1% to 10%): Dry mouth, toothache
- Frequency not reported: Abdominal discomfort, colitis, constipation, flatulence, gastroesophageal reflux disease, gastrointestinal hemorrhage, hemorrhoids, pancreatitis acute, paralytic ileus
Hepatic
- Very common (10% or more): Alanine aminotransferase increased (13%), aspartate aminotransferase increased (10%)
- Common (1% to 10%): Gamma-glutamyltransferase increased
- Frequency not reported: Lymphadenopathy including cervical adenitis, white blood cell count increased, cholecystitis acute, cholelithiasis
Local
- Very common (10% or more): Injection site tenderness (45%), injection site induration (35%), injection site pain (17%), other injection site reaction (primarily nodules, swelling) (15%), injection site pruritus (10%)
- Common (1% to 10%): Injection site ecchymosis
Musculoskeletal
- Very common (10% or more): Arthralgia/arthritis/joint stiffness (12%)
- Common (1% to 10%): Back pain/stiffness, muscle cramps
- Frequency not reported: Chills, joint stiffness, muscle spasms, myalgia, pain in limb
Other
- Very common (10% or more): Asthenic conditions (23%)
- Frequency not reported: Chest pain, chest tightness, abortion missed
Cardiovascular
- Frequency not reported: Angina pectoris, angina unstable, atrial fibrillation, cardiac failure congestive, coronary artery atherosclerosis, myocardial infarction, palpitations, deep vein thrombosis
Respiratory
- Frequency not reported: Chronic obstructive pulmonary disease, dyspnea, pharyngolaryngeal pain, sinus congestion
Dermatologic
- Common (1% to 10%): Rash
- Frequency not reported: Face edema, night sweats, pruritus, sweating increased
Metabolic
- Very common (10% or more): Anorexia/appetite decreased NOS/appetite disorder NOS (14%)
- Frequency not reported: Weight decreased, weight increased, appetite increased, dehydration
Renal
- Very common (10% or more): Abnormal creatinine phosphokinase levels (17%)
Ocular
- Frequency not reported: Conjunctivitis, vision blurred
Hematologic
- Frequency not reported: Eosinophil counts increased, decreased platelet count
Hypersensitivity
- Frequency not reported: Hypersensitivity reaction (including angioneurotic edema and urticaria)
- Postmarketing reports: Anaphylaxis
Immunologic
- Very common (10% or more): Pharyngitis (11%)
- Common (1% to 10%): Nasopharyngitis
- Frequency not reported: Seasonal allergies
- Preston KL, Bigelow GE. Differential naltrexone antagonism of hydromorphone and pentazocine effects in human volunteers. Journal of Pharmacology and Experimental Therapeutics 1993;264(2):813‐23. https://www.ncbi.nlm.nih.gov/pubmed/7679737[↩]
- Efficacy and tolerability of naltrexone in the management of alcohol dependence. Garbutt JC. Curr Pharm Des. 2010; 16(19):2091-7. https://www.ncbi.nlm.nih.gov/pubmed/20482515/[↩]
- Rösner S, Hackl‐Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No.: CD001867. DOI: 10.1002/14651858.CD001867.pub3. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001867.pub3/full[↩][↩][↩][↩][↩][↩]
- Kranzler HR, Armeli S, Feinn R, Tennen H. Targeted naltrexone treatment moderates the relations between mood and drinking behavior among problem drinkers. J Consult Clin Psychol. 2004;72:317–327.[↩]
- Volpicelli JR, Rhines KC, Rhines JS, Volpicelli LA, Alterman AI, O’Brien CP. Naltrexone and alcohol dependence. Role of subject compliance. Arch Gen Psychiatry. 1997;54:737–742.[↩]
- Kranzler HR, Stephenson JJ, Montejano L, Shaohung W, Gastfriend DR. Persistence with oral naltrexone for alcohol treatment: implications for health-care utilization. Addiction. 2008;103:1801–1808.[↩]
- Mark TL, Kranzler HR, Poole VH, Hagen CA, McLeod C, Crosse S. Barriers to the use of medications to treat alcoholism. Am J Addict. 2003;12:281–294.[↩]
- Baros AM, Latham PK, Moak DH, Voronin K, Anton RF. What role does measuring medication compliance play in evaluating the efficacy of naltrexone? Alcohol Clin Exp Res. 2007;31:596–603.[↩]
- Hulse GK. Improving clinical outcomes for naltrexone as a management of problem alcohol use. British Journal of Clinical Pharmacology. 2013;76(5):632-641. doi:10.1111/j.1365-2125.2012.04452.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3853523/[↩][↩]
- Ulm RR, Volpicelli JR, Volpicelli LA. Opiates and alcohol self‐administration in animals. Journal of Clinical Psychiatry 1995;56(7):5‐14.[↩]
- Middaugh LD, Bandy AL. Naltrexone effects on ethanol consumption and response to ethanol conditioned cues in C57BL/6 mice. Psychopharmacology (Berl) 2000;151(4):321‐7.[↩]
- Childress AR, McLellan AT, O’Brien CP. Role of conditioning factors in the development of drug dependence. Psychiatric Clinics of North America 1986;9(3):413‐25.[↩]
- Gianoulakis C. Endogenous opioids and addiction to alcohol and other drugs of abuse. Current Topics in Medicinal Chemistry 2004;4(1):39‐50.[↩]
- Clintron R. Product Announcement: ReVia TM , Naltrexone HCL. Distributed by DuPont Pharma1995.[↩]
- Volpicelli JR, Watson NT, King AC, Sherman CE, O’Brien CP. Effect of naltrexone on alcohol “high” in alcoholics. American Journal of Psychiatry 1995;152(4):613‐15.[↩]
- Adcock RA, Thangavel A, Whitfield‐Gabrieli S, Knutson B, Gabrieli JD. Reward‐motivated learning: mesolimbic activation precedes memory formation. Neuron 2006;50(3):507‐17.[↩]
- Latt NC, Jurd S, Houseman J, Wutzke SE. Naltrexone in alcohol dependence: a randomised controlled trial of effectiveness in a standard clinical setting. Med J Aust. 2002;176:530–534.[↩]
- Garbutt JC. Efficacy and tolerability of naltrexone in the management of alcohol dependence. Curr Pharm Des. 2010;16:2091–2097. https://www.ncbi.nlm.nih.gov/pubmed/20482515[↩]
- Mitchell JM, Bergren LJ, Chen KS, Rowbotham MC, Fields HL. Naltrexone aversion and treatment efficacy are greatest in humans and rats that actively consume high levels of alcohol. Neurobiol Dis. 2009;33:72–80[↩]
- Carmen B, Angeles M, Ana M, Maria AJ. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction. 2004;99:811–828.[↩][↩]
- Walters D, Connor J, Feeney GF, Yooung RM. The cost effectiveness of naltrexone added to cognitive-behavioral therapy in the treatment of alcohol dependence. J Addict Dis. 2009;28:137–144. https://www.ncbi.nlm.nih.gov/pubmed/19340676[↩]
- Ritter AJ. Naltrexone in the treatment of heroin dependence: relationship with depression and risk of overdose. Aust N Z J Psychiatry. 2002;36:224–228.[↩]
- Crowley TJ, Wagner JE, Zerbe G, Macdonald MJ. Naltrexone-induced dysphoria in former opioid addicts. Am J Psychiatry. 1985;142:1081–1084[↩]
- Pettinati HM, Oslin DW, Kampman KM, Dundon WD, Xie H, Gallis TL, Dackis CA, O’Brien CP. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occuring depression and alcohol dependence. Am J Psychiatry. 2010;167:668–675[↩]
- The Use of Naltrexone in Low Doses Beyond the Approved Indication. https://www.fhi.no/en/publ/2015/the-use-of-naltrexone-in-low-doses-beyond-the-approved-indication/[↩][↩]
- [Naltrexone–high expectations to low dosages]. Raknes G, Giverhaug T. Tidsskr Nor Laegeforen. 2011 May 6; 131(8):844-6. https://tidsskriftet.no/2011/05/kronikk/naltrekson-hoye-forventninger-til-lave-doser[↩]
- Parker CE, Nguyen TM, Segal D, MacDonald JK, Chande N. Low dose naltrexone for induction of remission in Crohn’s disease. Cochrane Database of Systematic Reviews 2018, Issue 4. Art. No.: CD010410. DOI: 10.1002/14651858.CD010410.pub3. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010410.pub3/full[↩]
- Intranasal naloxone administration for treatment of opioid overdose. Am J Health Syst Pharm. 2014 Dec 15;71(24):2129-35. doi: 10.2146/ajhp130798. http://www.ajhp.org/content/71/24/2129.full[↩][↩]
- Chen KY, Chen L, Mao J. BUPRENORPHINE-NALXONE THERAPY IN PAIN MANAGEMENT. Anesthesiology. 2014;120(5):1262-1274. doi:10.1097/ALN.0000000000000170. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999180/[↩]
- Levine JD, Gordon NC, Fields HL. Naloxone dose dependently produces analgesia and hyperalgesia in postoperative pain. Nature. 1979;278:740–1.[↩]