Contents
What is neurosarcoidosis
Neurosarcoidosis is a manifestation of sarcoidosis in the nervous system. Sarcoidosis is a chronic inflammatory disorder that typically occurs in adults between 20 and 40 years of age and primarily affects the lungs, but can also impact almost every other organ and system in the body. Neurosarcoidosis is characterized by inflammation and abnormal cell deposits in any part of the nervous system – the brain, spinal cord, or peripheral nerves 1. Neurosarcoidosis most commonly occurs in the cranial and facial nerves, the hypothalamus (a specific area of the brain), and the pituitary gland. Neurosarcoidosis is estimated to develop in 5 to 15 percent of those individuals who have sarcoidosis 1. Neurosarcoidosis has been documented more commonly within Africans and African descent 2. However, about half of patients with sarcoidosis have systemic disease, with 30% to 70% who have concomitant neurologic signs when first diagnosed.
Weakness of the facial muscles on one side of the face (Bell’s palsy) is a common symptom of neurosarcoidosis. The optic and auditory nerves can also become involved, causing vision and hearing impairments. Neurosarcoidosis can cause headache, seizures, memory loss, hallucinations, irritability, agitation, and changes in mood and behavior. Neurosarcoidosis can appear in an acute, explosive fashion or start as a slow chronic illness. Because neurosarcoidosis manifests in many different ways, a diagnosis may be difficult and delayed.
Neurosarcoidosis generally occurs only in cases of sarcoidosis with substantial systemic involvement, and signs of neurologic involvement usually are seen in patients known to have active disease 3.
Definitive diagnosis of neurosarcoidosis requires the exclusion of other causes of neuropathy and the identification of noncaseating sarcoid granulomas by histologic analysis of nerve and muscle biopsy specimens 3.
Neurosarcoidosis has no known cure. Spontaneous remission has been observed, but long-term therapy often is required. Immunosuppression is the principal method of controlling the disease, and corticosteroids are the cornerstone of therapy 3. Corticosteroids such as prednisone are prescribed to reduce inflammation. They are often prescribed until symptoms get better or go away. You may need to take the medicines for months, or even years.
Other medicines may include hormone replacement and medicines that suppress the immune system.
If you have numbness, weakness, vision or hearing problems, or other problems due to damage of the nerves in the head, you may need physical therapy, braces, a cane, or a walker.
Mental disorders or dementia may require medicines for depression, safety interventions, and assistance with care.
Neurosarcoidosis causes
Sarcoidosis is a long-term disorder that affects many parts of the body, mostly the lungs. Sarcoidosis primarily affects the lymphoreticular system, with prominent cervical and mediastinal lymphadenopathy (e.g., perihilar and peritracheal nodes). There is also involvement of the smaller scattered lymphatic collections in solid organs (e.g., spleen, liver) and lymphoid tissue surrounding glandular organs such as the parotid and lacrimal glands.
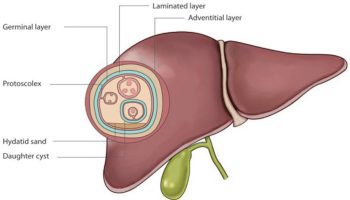
Debate continues as to whether sarcoidosis results from a dysfunctional immune system or a secondary response to environmental antigens. Sarcoidosis is believed to be a hyperactive immune response. Th1 cells stimulate the release of IL-2 and IFN-gamma which then activate macrophages. In turn, the inflammatory response induced by macrophages causes granuloma formation 4. Sarcoid granulomas may be seen in solid organs such as liver, kidney, and spleen. In a small number of people, sarcoid granulomas involves some part of the nervous system. This is called neurosarcoidosis. The lesion consists of lymphocytes and mononuclear phagocytes surrounding a noncaseating epithelioid cell granuloma.
Neurosarcoidosis may affect any part of the nervous system. Sudden, facial weakness (facial palsy) is a common neurological symptom that involves the nerves to the muscles of the face. Any other nerve in the skull can be affected, including those in the eye and those that control taste, smell, or hearing.
The spinal cord is another part of the nervous system that sarcoidosis can affect. People may have weakness in their arms and legs, and difficulty walking or controlling their urine or bowels.
The condition can also affect the parts of the brain involved in regulating many body functions, such as temperature, sleep, and stress responses.
Muscle weakness or sensory losses can occur with peripheral nerve involvement. Other areas of the brain, including the pituitary gland at the base of the brain, or the spinal cord may also be involved.
Neurosarcoidosis prevention
Aggressive treatment of sarcoidosis turns off the body’s faulty immune response before your nerves become damaged. This may reduce the chance that neurological symptoms will occur.
Neurosarcoidosis symptoms
Neurosarcoidosis symptoms vary. Any part of the nervous system can be affected.
Involvement of the pituitary gland can cause:
- Changes in menstrual periods
- Excessive tiredness or fatigue
- Excessive thirst
- High urine output
Involvement of the brain or cranial nerves can cause:
- Confusion, disorientation
- Decreased hearing
- Dementia
- Delirium
- Dizziness, vertigo, or abnormal sensations of movement
- Double vision or other vision problems
- Facial palsy (weakness, drooping)
- Headache
- Loss of sense of smell
- Loss of sense of taste, abnormal tastes
- Mental disturbances
- Seizures
- Speech impairment
Involvement of one or more peripheral nerves can lead to:
- Abnormal sensations in any body part
- Loss of movement of any body part
- Loss of sensation in any body part
- Weakness of any body part.
Neurosarcoidosis possible complications
Neurosarcoidosis complications vary depending on which part of the nervous system is involved and how you respond to treatment. Slowly worsening or permanent loss of neurological function is possible. In rare cases, the brainstem may be involved. This is life threatening.
Neurosarcoidosis diagnosis
Neurosarcoidosis should be considered in patients with sarcoidosis who develop neurologic abnormalities. However, the index of suspicion is lower and thus much more difficult in cases where a patient is not known to have sarcoid but has neurologic abnormalities. Unfortunately, there is no diagnostic marker for neurosarcoidosis 4.
An exam may show problems with one or more nerves.
A history of sarcoidosis followed by nerve-related symptoms highly suggests neurosarcoidosis. However, symptoms of the condition can mimic other medical disorders, including diabetes insipidus, hypopituitarism, optic neuritis, meningitis, and certain tumors. Sometimes, the nervous system can be affected before a person is known to have sarcoidosis, or without affecting the lungs or other organs at all.
If neurosarcoidosis is suspected, it is important to assess for signs of systemic diseases, such as the skin, lymph nodes, and lungs. Tests to conduct include ophthalmologic exam (including optical coherence tomography), nasal/sinus examination, chest x-ray (for perihilar lymphadenopathy), angiotensin-converting enzyme (ACE) assay (not specific), and in rare cases a magnetic resonance, gallium or fluorodeoxyglucose emission tomographic scan for areas of inflammation that may be biopsied.
Blood tests are not very helpful in diagnosing the condition. A lumbar puncture may show signs of inflammation. Increased levels of angiotensin-converting enzyme may be found in the blood or cerebrospinal fluid (CSF). However, this is not a reliable diagnostic test.
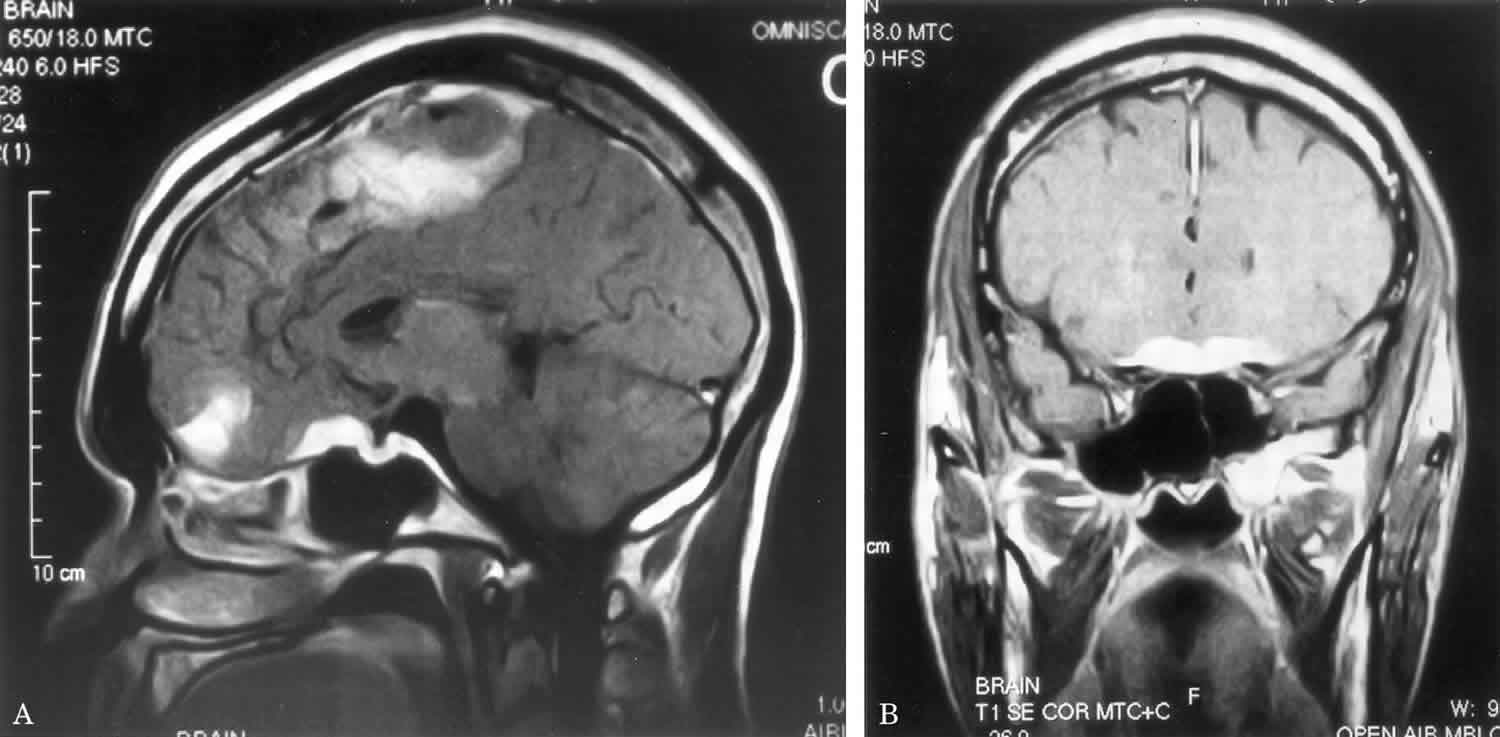
MRI of the brain may be helpful. A chest x-ray often reveals signs of sarcoidosis of the lungs. If the diagnosis remains uncertain, biopsies of the meninges, brain or spinal cord may be indicated 5. However, biopsies of the skin, lymph node, and lung are less risky and thus, are more preferred. A biopsy may also be considered for patients who do not respond to therapy.
As with other inflammatory states, ESR may be elevated. Creatinine kinase and aldolase may also be used to evaluate for myopathy. Liver function testing may also be abnormal, thereby reflecting the systemic involvement of sarcoidosis. If the pituitary-hypothalamic axis is affected, endocrine studies should be done. In recent years, F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) imaging have been used to evaluate for neurosarcoidosis. F-18 FDG PET/CT is gaining popularity in patients with suspected systemic sarcoidosis, especially with pulmonary or cardiac involvement. It can provide valuable information to the site of involvement by the disease and selection of more surgically accessible sites for biopsy.
Neurosarcoidosis treatment
There is no known cure for sarcoidosis. Treatment is given if symptoms are severe or are getting worse. The goal of treatment is to reduce symptoms.
There is no agreed upon standard of treatment for neurosarcoidosis. Doctors generally recommend corticosteroid therapy as first-line therapy for individuals with neurosarcoidosis. For facial nerve palsy or aseptic meningitis, prednisone is given every day for 2 weeks usually. In cases of meningeal, parenchymal mass lesion or myopathy or neuropathy, prednisone should be given for at least 4 weeks. For deteriorating patients, intravenous (IV) methylprednisolone is given for 3 days followed by prednisone for 2 to 4 weeks. The steroid dose should be tapered over several months with follow up by a neurologist every 3 to 6 months.
Additional treatment with immunomodulatory drugs such as hydroxychloroquine, pentoxyfilline, thalidomide, and infliximab, and immunosuppressive drugs such as methotrexate, azathioprine, cyclosporin, and cyclophosphamide, have benefited some individuals. While the use of corticosteroids and other immunosuppressive drugs is effective, these medications also have undesirable side effects. Side effects and experience with certain drugs may play a role in medication choices.
There have been anecdotal reports of improvement with intravenous immunoglobulin therapy in patients in whom conventional therapy has failed 6. The response may be related to amelioration of vasculitic neuropathy.
In patients with brain involvement, low-dose radiation has produced clear symptomatic benefits in some patients 7. Since the adverse effects of low-dose cranial irradiation are minimal, using radiation therapy may be prudent for patients whose disease is refractory to steroids or who have had adverse responses to high-dose steroids. Removal of the space-occupying lesions in the brain has little or no benefit and should be attempted only in extreme cases. Hydrocephalus may require ventriculoperitoneal shunting.
Adjunctive measures for specific neurologic manifestations include the following:
- Dementia: safety intervention and assistance
- Hypopituitarism: hormone replacement therapy
- Psychosis: risperidone and other antipsychotic drugs
- Foot involvement or balance problems: physical therapy with activity recommendations for decreasing falls
Neurosarcoidosis prognosis
The prognosis for patients with neurosarcoidosis varies. Neurosarcoidosis may present as either a monophasic illness, a relapsing-remitting course, or as a progressive disease with episodes of deteriorations. Approximately two-thirds of those with neurosarcoidosis will recover completely in 4 to 6 months; the remainder will have a chronically progressing or on-and-off course of illness for the rest of the person’s life.
Usually, patients with facial nerve palsy or other cranial mononeuropathies will improve. In contrast, cases with aseptic meningitis or meningeal/parenchymal mass lesions have a longer course. Hypothalamic vegetative symptoms rarely resolve although may respond to treatment.
Encephalopathy/vasculopathy tends to have a relapsing-remitting course with deterioration. Cases with hydrocephalus may either be asymptomatic or cause rapid deterioration. Remissions are possible in peripheral neuropathy and myopathy cases, however, the course usually is chronic and progressive.
Neurosarcoidosis can cause permanent disability and, in some cases, death. Complications resulting from immunosuppressive treatments, such as cryptococcal and tuberculous meningitis, progressive multifocal leukoencephalopathy, and inclusion body myositis, may be fatal for a small percentage of individuals.
- Neurosarcoidosis Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Neurosarcoidosis-Information-Page[↩][↩]
- Lacomis D. Neurosarcoidosis. Curr Neuropharmacol. 2011 Sep;9(3):429-36.[↩]
- Neurosarcoidosis. https://emedicine.medscape.com/article/1147324-overview[↩][↩][↩]
- Pirau L, Lui F. Neurosarcoidosis. [Updated 2018 Nov 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534768[↩][↩]
- Peeples DM, Stern BJ, Jiji V, Sahni KS. Germ cell tumors masquerading as central nervous system sarcoidosis. Arch. Neurol. 1991 May;48(5):554-6[↩]
- Levy Y, Uziel Y, Zandman G, Rotman P, Amital H, Sherer Y, et al. Response of vasculitic peripheral neuropathy to intravenous immunoglobulin. Ann N Y Acad Sci. 2005 Jun. 1051:779-86[↩]
- Sundaresan P, Jayamohan J. Stereotactic radiotherapy for the treatment of neurosarcoidosis involving the pituitary gland and hypothalamus. J Med Imaging Radiat Oncol. 2008 Dec. 52(6):622-6[↩]