Contents
What is oscillopsia?
Oscillopsia is an illusory sensation during walking that your stationary environment is bouncing or unstable when it is not 1, 2, 3, 4, 5, 6, 7, 8, 9, 10. Oscillopsia results in blurred vision when the head is in motion and objects appear to jiggle and bounce since they do not stay fixed at one point in the retina 11. Individuals with oscillopsia are often forced to stop and stay still to read signs. Reading a book may also require great effort since small head movements may cause distortion. Since these people with oscillopsia would need more time to comprehend and process words and letters, undiagnosed children are sometimes wrongly thought to have dyslexia or dyscalculia 12.
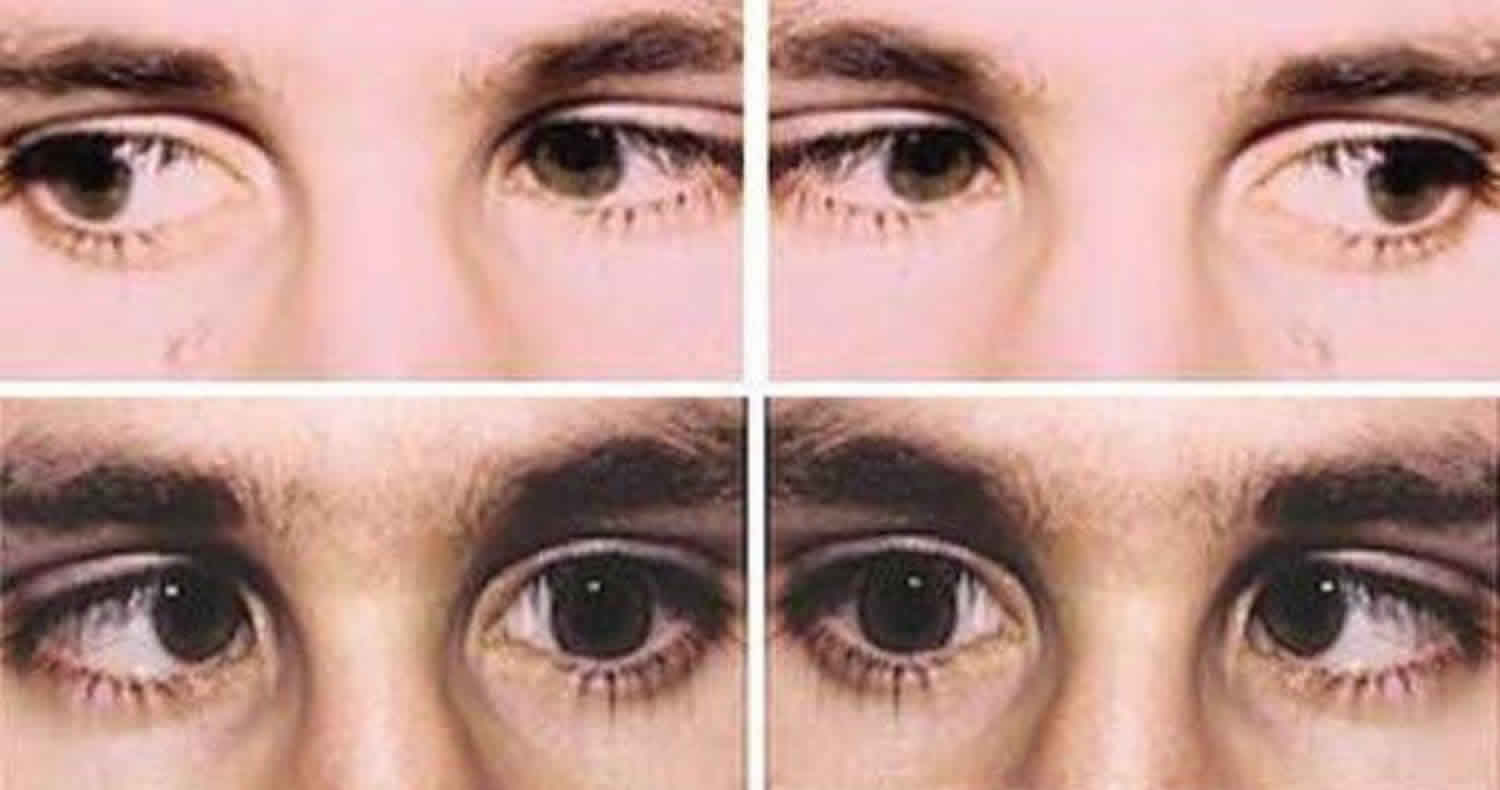
Oscillopsia is usually either caused by abnormal movement of the eyes such as nystagmus or bilateral (both sides) vestibulo-ocular reflex (VOR) function loss when the person’s head is moving 13. Nystagmus is defined by rhythmic, abnormal eye movements with a “slow” eye movement driving the eye off the target followed by a second movement that brings the eye back to the target 14. Oscillopsia occurs when the deficient vestibulo-ocular reflexes (VOR) and the back part of your eye (the retina) cannot keep the visual environment stable and the world appears to bounce or move 13.
A person with oscillopsia may notice the following 13:
- When riding in a car on a bumpy road, it is hard to read street signs.
- It can be hard to recognize faces during movement or walking.
- It may be difficult to focus on objects while quickly turning the head, such as glancing for traffic when crossing the street or looking at side view mirrors while driving.
Abnormal nystagmus may also blur vision because it causes excessive involuntary eye movements (can be in various directions; side to side or up and down) 15, 16. Individuals with vestibulo-ocular reflex (VOR) malfunction are also likely to be clumsy, get motion sick easily, have sensory issues, difficulty maintaining balance, and nausea 12. If the sensory vestibular organs are not fully functional on either side, the brain will receive conflicting signals regarding movement, causing vertigo 17, 18, 19. Vertigo is a sensation that the environment around you is spinning in circles. Vertigo causes dizziness and makes you feel like you’re spinning when you’re not. Vertigo can make you feel dizzy, off-balance, nausea and vomiting.
Patients with oscillopsia currently have few opportunities for relief: there are no reliable treatment options and as a result, they struggle to live independent lives 20, 21, 22, 23. Anecdotally, a frequent complaint among those with oscillopsia is that they feel neglected and struggle to describe the condition and explain the effect it has on their everyday lives.
Your inner ear is a complicated, delicate and essential part of your body. Hearing loss and balance problems can come without warning and can get worse over time. Generally, see your doctor if you experience any recurrent, sudden, severe, or prolonged and unexplained dizziness or vertigo.
Although it’s uncommon for dizziness to signal a serious illness, see your doctor immediately if you experience dizziness or vertigo along with any of the following:
- A new, different or severe headache
- A fever
- Double vision or loss of vision
- Hearing loss
- Trouble speaking
- Leg or arm weakness
- Loss of consciousness
- Falling or difficulty walking
- Numbness or tingling
The signs and symptoms listed above may signal a more serious problem.
Get emergency medical care if you experience new, severe dizziness or vertigo along with any of the following:
- Sudden, severe headache
- Chest pain
- Difficulty breathing
- Numbness or paralysis of arms or legs
- Fainting
- Double vision
- Rapid or irregular heartbeat
- Confusion or slurred speech
- Stumbling or difficulty walking
- Ongoing vomiting
- Seizures
- A sudden change in hearing
- Facial numbness or weakness
Vestibulo-ocular reflex
The Vestibulo-Ocular Reflex is an essential function of your vestibular system that helps you maintain a stable perception of the world around you by maintaining your postural balance and spatial orientation in response to changes in your environment such as while you engage in normal movements throughout your day like walking 12, 24. The vestibulo-ocular reflex keeps you steady and balanced even though your eyes and head are continuously moving when you perform most actions. When you make a head movement, your eye muscles are triggered instantly to create an eye movement opposite to that of your head movement at the exact same speed to readjust your visual world, which, in turn, stabilizes your retinal image (line of sight in space) by keeping your eyes still in space and focused on an object, despite you head moving 25.
The Vestibulo-Ocular Reflex (VOR) involves three parts 25, 26, 27:
- Peripheral sensory apparatus which consists of a set of motion sensors: the semicircular canals (anterior, posterior, horizontal) and the otolith organs (saccule and utricle) (Figures 1 to 5).
- The semicircular canals are tubes coiled within your inner ear filled with liquid called the endolymph and lined with hair cells. Instead of sound waves, these tiny hairs react to sense rotational and angular movements of your head. The semicircular canals are mostly responsible for rotary motion or motion not in a straight line.
- Humans have a total of 6 semicircular canals arranged in three main planes (anterior, posterior, horizontal) on both sides; each plane has a pair of canals. The 3 in the right ear are functionally paired with the 3 in the left ear. The semicircular canals are referred to according to their orientation: lateral (horizontal), anterior (superior), and posterior. These structures are positioned at roughly right angles in relation to one another. The horizontal (lateral) semicircular canal, the shortest of the three, is set at an angle of about 30 degrees to the horizontal plane. The anterior (superior) and posterior loops are in diagonal vertical planes that intersect at a 90-degree angle. The 3 semicircular canals (anterior, posterior, horizontal) are positioned at 90-degree angles to one another and thus can sense rotation in all directions:
- The right horizontal with the left horizontal
- The right anterior with the left posterior
- The right posterior with the left anterior.
- A semicircular canal will get stimulated by head motion towards that semicircular canal 28. When a semicircular canal on one side is activated, there is inhibition of the other one during angular head movements. For example, when turning your head to look over your right shoulder, the right horizontal semicircular canal is excited and the left horizontal is inhibited. When there are head movements and rotation, the velocity of the movements dictates the difference in firing rate between the two semicircular canals 12. Hair cells are embedded in a fluid and gelatinous structure called the ampulla in each semicircular canal. When you rotate your head, the canal will move relative to the fluid inside of it, which will create a force against the ampulla, causing hair cells to bend. When your head is at rest, vestibular afferents have tonic discharge; this results in a balance between the semicircular canal pairs. Cases of nystagmus and ocular misalignment may be interpreted by understanding the organization and structure of the semicircular canals and otolith organs within the head 25. Information regarding linear head acceleration, angular velocity, and orientation of the head relative to gravity are all collected by these peripheral motion sensors. These sensors relay this information to the central nervous system (brain and spinal cord). Here, information from somatosensors (carrying other sensory information) is combined with motion sensory information to calculate head orientation.
- The semicircular canals (anterior, posterior, horizontal) sense angular head acceleration are responsible for detecting head rotation and the otolith organs (saccule and utricle) sense linear head acceleration and therefore detect the position of your head relative to gravity and head translation, providing your internal cues for orientation of position in space, movement, gaze stabilization, and postural control. Body movements cause the fluid in the semicircular canals to move and stimulate cilia on sensory hair cells. This triggers transmission of neural signals to the brain to initiate appropriate reflex responses for the eyes, head, and postural adjustments. These reflexive movements allow you to see things clearly when your head and body are in motion and keep you from falling.
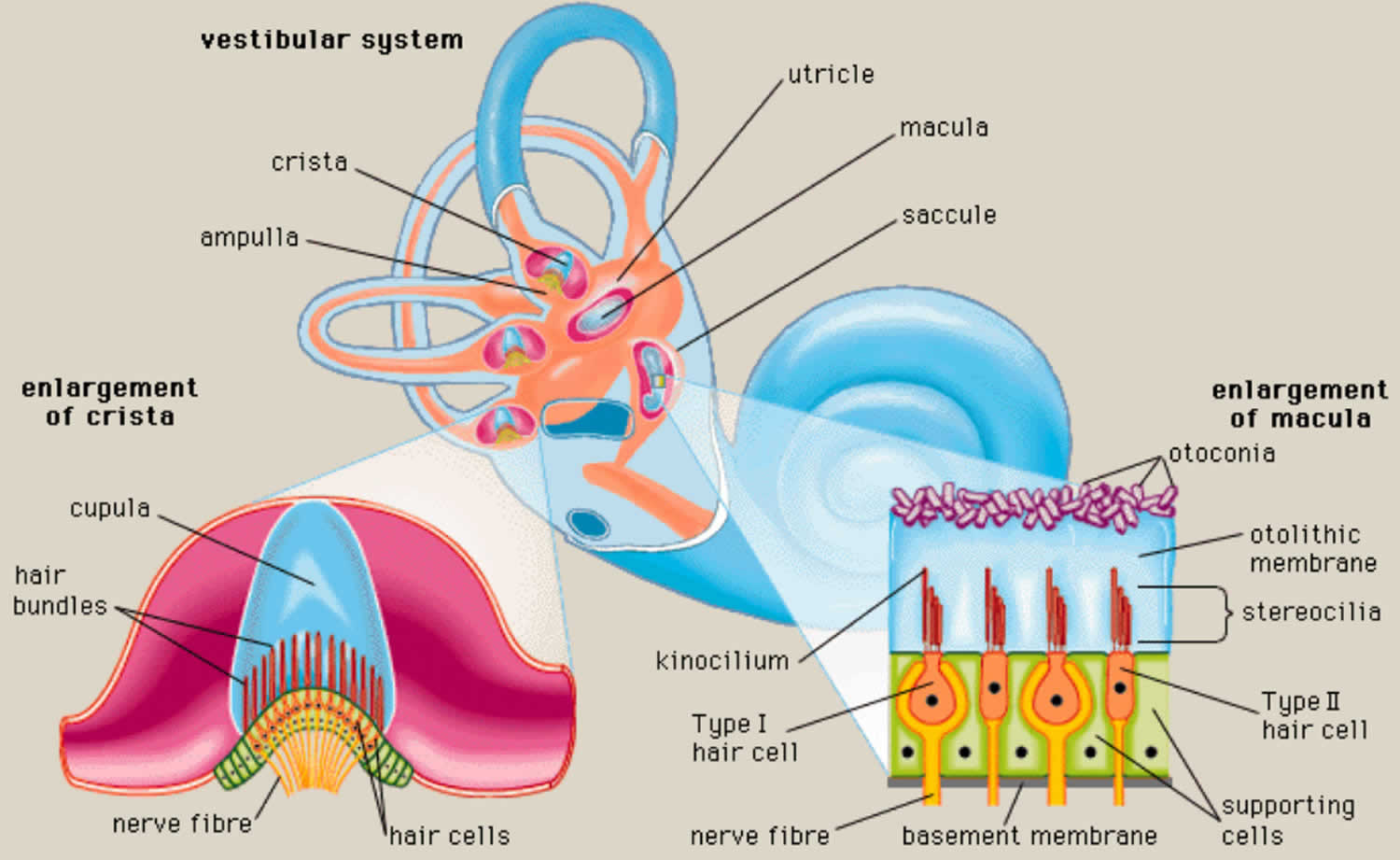
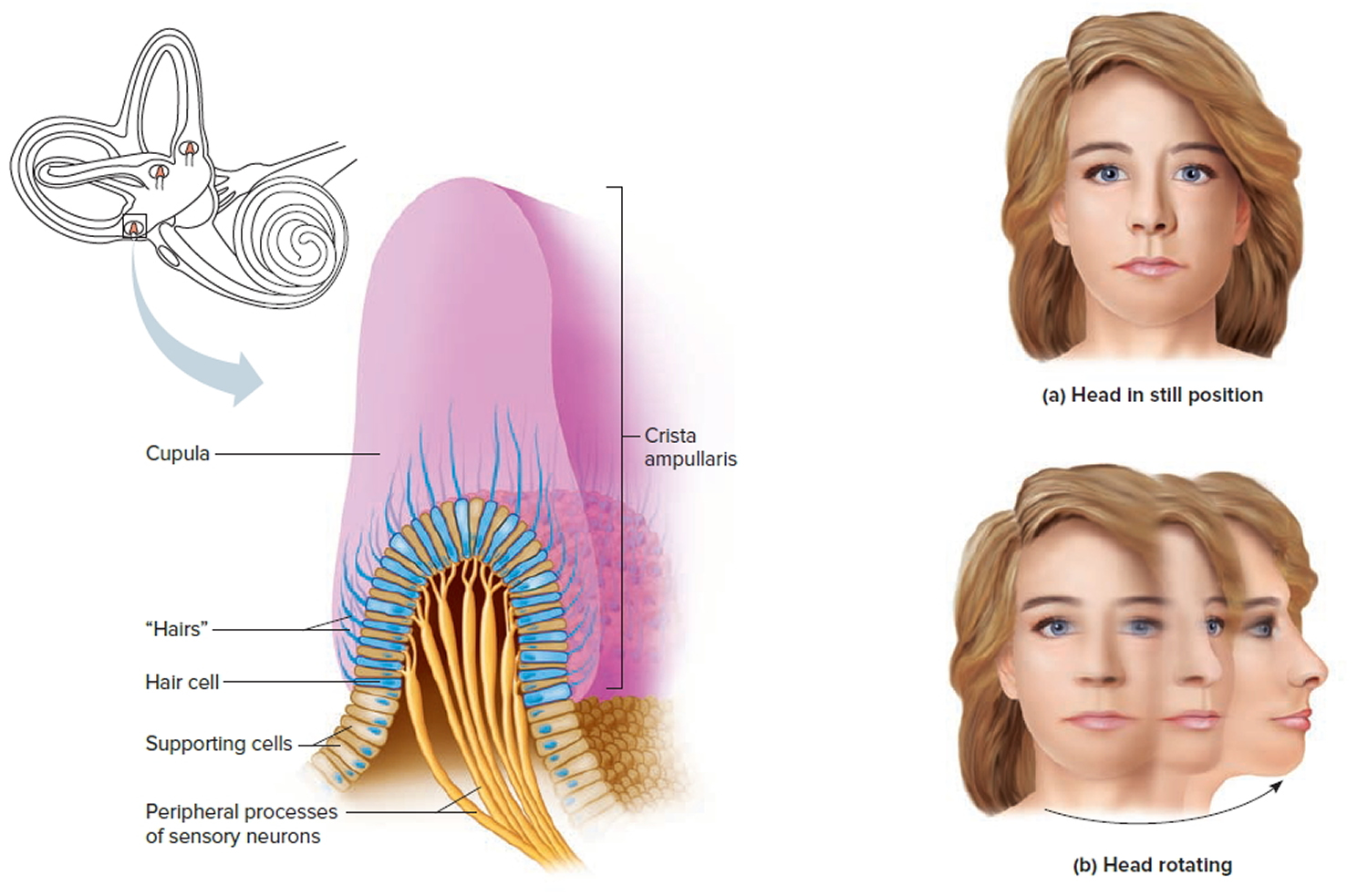
- Each semicircular canal has an ampulla, an expanded bulb-shaped structure that contains the hair cells (crista ampullaris), as well as a fan-like structure known as the cupula, which separates the semicircular canal from the vestibule (see Figures 1 and 3). The ampulla contains a fluid known as endolymph, which is also present in the cochlea, and the crista, a cone-shaped structure lined with hair cells and supporting cells. The hair cells form stereocilia, protrusions that extend into the crista. The longest of the stereocilia are the kinocilia, which point in a single direction and are sensitive to movement. The kinocilia extend from the crista into the cupula, a jellylike mass that surrounds the hair cells completely, separating them from the endolymph. The crista is flexible. When your head moves, endolymph pushes the cupula one way or the other, which in turn displaces the hairs and alters the electrical potential of the hair cells.
- The cupula has the same density as the endolymph and therefore semicircular canal does not respond to changes in the orientation of the head with respect to gravity. With angular head movements, however, the inertia of the endolymph results in a pressure on the cupula, which stimulates the hair cells through facilitation (increased firing rate) or inhibition (decreased firing rate). If the fluid is moving toward the ampulla, the horizontal canal is facilitated, while the semicircular canals in the vertical plane on the same side are inhibited. Hence, neural activities of the semicircular canal pairs are opposite, which results in a push–pull mechanism of facilitation on one side and inhibition on the other 29. The resting firing rate in the absence of motion would therefore be equal for the right and left labyrinths.
- Humans have a total of 6 semicircular canals arranged in three main planes (anterior, posterior, horizontal) on both sides; each plane has a pair of canals. The 3 in the right ear are functionally paired with the 3 in the left ear. The semicircular canals are referred to according to their orientation: lateral (horizontal), anterior (superior), and posterior. These structures are positioned at roughly right angles in relation to one another. The horizontal (lateral) semicircular canal, the shortest of the three, is set at an angle of about 30 degrees to the horizontal plane. The anterior (superior) and posterior loops are in diagonal vertical planes that intersect at a 90-degree angle. The 3 semicircular canals (anterior, posterior, horizontal) are positioned at 90-degree angles to one another and thus can sense rotation in all directions:
- The otolith organs (saccule and utricle) contain dense crystals called otoconia resting on top of the sensory organs, are gravity-sensitive and provide sensory neural input related to linear head acceleration.
- The utricle senses linear movements of the head in the horizontal plane.
- The saccule senses linear movements of the head in the vertical plane.
- Additionally, the utricle and saccule convey information about spinal and leg muscles for balance strategies (ankle, hip, and stepping) via the Vestibulo-Spinal Reflex (VSR), which is primarily to maintain upright posture during movement. The otoliths (otoconia) further convey information regarding the direction of gravity through head tilt, which is incorporated into locomotion. The function of the otolith organs is accomplished by otoconia (otoliths) – calcium carbonate crystals that are denser than the surrounding endolymph – remaining partially stable while the head moves around them (Figure 4). It is important to note that the utricle and saccule also have connections with eyes muscles as noted with the semicircular canal. However, the direct pathways of rotational compensatory eye movements are much greater than those of linear translation, resulting in minimal contributions from the otoliths to the Vestibulo-Ocular Reflex (VOR) as compared to the semicircular canal. With linear head movements (e.g., leaning to your side), the otoconia move, signaling reflexive responses similar to those of the semicircular canals to maintain eye, head, and body equilibrium.
- If otoconia (otoliths) become displaced from the utricle into the semicircular canals, then brief spells of vertigo are experienced related to position changes, a condition called benign paroxysmal positional vertigo (BPPV). Traumatic brain injury is a common cause of benign paroxysmal positional vertigo (BPPV) in the adult population, although it rarely occurs in adolescents 30, 31, 32.
- The first-order information processing from the inner ear involves a number of associated reflexes: the Vestibulo-Collic Reflex (VCR), the Cervico-Ocular Reflex (COR), the Cervico-Spinal Reflex (CSR), and the Cervico-Collic Reflex (CCR) 27. The Vestibulo-Collic Reflex (VCR) acts on the neck muscles to stabilize the head in space during body movements and is considered a righting reflex 27. The Vestibulo-Collic Reflex (VCR) lessens head oscillations that occur in more rapid, dynamic movements 33. Although the neural pathways and actions are not fully understood, it is suspected that Vestibulo-Collic Reflex (VCR) is mediated through the otolith organs and medial Vestibulo-Spinal Reflex (VSR) 34. The Cervico-Ocular Reflex (COR) acts on eye movements similar to the Vestibulo-Ocular Reflex (VOR), receiving input from the neck proprioceptors, and is of particular importance as a compensatory strategy if bilateral vestibular nerve loss occurs. The Cervico-Ocular Reflex (COR) is not thought to make any notable contributions to gaze stability in normal subjects because the gain is notably less than the Vestibulo-Ocular Reflex (VOR) 35. The Cervico-Spinal Reflex (CSR) acts on the extremities and is synonymous with the tonic neck reflex. The Cervico-Spinal Reflex (CSR) interacts with the Vestibulo-Spinal Reflex (VSR) 36. Finally, the Cervico-Collic Reflex (CCR) acts on deep neck muscles to assist in head stabilization during head and body movements. Body rotation with the head stabilized elicits the Cervico-Collic Reflex (CCR), whereas head rotation with the body stabilized elicits the Vestibulo-Ocular Reflex (VOR) 37.
- The semicircular canals are tubes coiled within your inner ear filled with liquid called the endolymph and lined with hair cells. Instead of sound waves, these tiny hairs react to sense rotational and angular movements of your head. The semicircular canals are mostly responsible for rotary motion or motion not in a straight line.
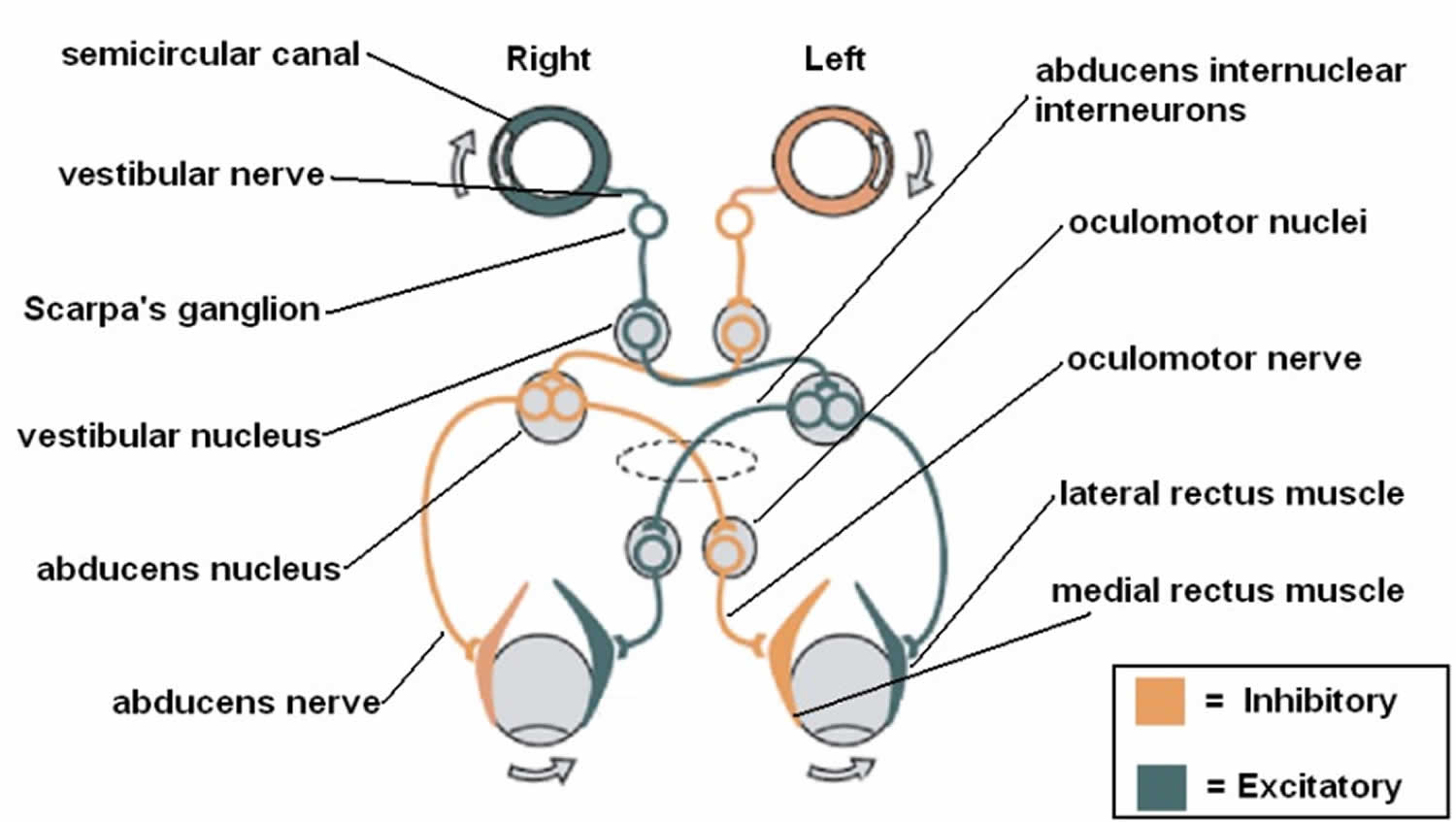
- A central processing mechanism
- Vestibular information is primarily processed in the brainstem via the cranial nerve eight (CN VIII) also known as vestibulocochlear nerve that consists of the vestibular and cochlear nerves 12, 38. The signals enter the vestibular nuclear complex, located in the medulla and pons 38. Four main nuclei comprise the vestibular nuclear complex (superior, inferior, medial, and lateral) 29, 39, 40. Most of the semicircular canal inputs synapse with the superior and medial vestibular nuclei via first-order sensory neurons of cranial nerve eight (CN VIII), while second-order sensory neurons send signals ipsilaterally and contralaterally via the medial longitudinal fasciculus to the oculomotor cranial nerves, oculomotor nerve (the third cranial nerve; CN III), trochlear nerve (fourth cranial nerve; CN IV), and abducens nerve (sixth cranial nerve; (CN VI). Lastly, a third motor neuron excites the extraocular muscles, causing conjugate eye movements that are equal to and opposite of head movements 41, 27. This results in gaze stabilization during head movements.
- The vestibular system is unique in that it also sends information via the inferior cerebellar peduncle to the cerebellum to modulate or fine-tunine the Vestibulo-Ocular Reflex (VOR). The flocculonodular lobe and fastigial nuclei are responsible for this fine-tuning. Vestibular data is also processed by the cerebellum, which then aids in the regulation of vestibular reflexes, maintaining posture, and coordination 42, 39. Other connections to the cerebral cortex, thalamus, and reticular formation assist in coordinating efforts between other central networks and the vestibular system, allowing for enhanced spatial awareness 27.
- There are additional vestibular connections to the thalamus, cerebral (vestibular) cortex, and reticular formation. These extensive connections result in a coordinated effort between the vestibular system and other central networks to contribute to arousal and conscious awareness of the head and body in space 41.
- A motor output which are the eye muscles.
- The central nervous system (brain and spinal cord) is the central processing mechanism, which sends its outputs to the spinal cord and eye muscles to generate the Vestibulo-Ocular Reflex. Each semicircular canal has excitatory projections to a pair of extraocular muscles in each eye and inhibitory projections to an antagonistic pair of muscles 28. In addition to the Vestibulo-Ocular Reflex (VOR), you also have a Vestibulo-Spinal Reflex (VSR), which prevents falls by maintaining head and postural stability. It does this by creating compensatory body movements 25. To attain an even better orientation, this information also goes to cortical structures (posterior insular vestibular cortex) for further integration with tactile, auditory, and proprioceptive inputs. Actions of the Vestibulo-Ocular Reflex (VOR) and Vestibulo-Spinal Reflex (VSR) become controlled and continuously adjusted as needed by the central nervous system (brain and spinal cord) 25.
The inner ear is innervated by cranial nerve eight (CN VIII) also known as vestibulocochlear nerve that consists of the vestibular nerve and cochlear nerve 38. The vestibular nerve is primarily responsible for maintaining body balance and eye movements, while the cochlear nerve is responsible for hearing 43. Damage to the vestibular nerve results in vertigo, a balance disorder, and nystagmus 43.
Ewald’s three laws for vestibular diagnostic testing 27
- Stimulation of a semicircular canal generates eye movements in the plane of that canal.
- In the horizontal semicircular canals, movement of the endolymph toward the ampulla (ampullopetal) causes deflection of the cupula toward the utricle (utriculopetal) and results in excitation (greater neural activity) compared to movement away from the utricle (utriculofugal).
- In the vertical semicircular canals (anterior and posterior), movement of the endolymph away from the ampulla (ampullofugal) causes greater deflection of the cupula away from the utricle (utriculofugal) and results in a greater excitation compared to utriculopetal movement, which is opposite to that in the horizontal canals.
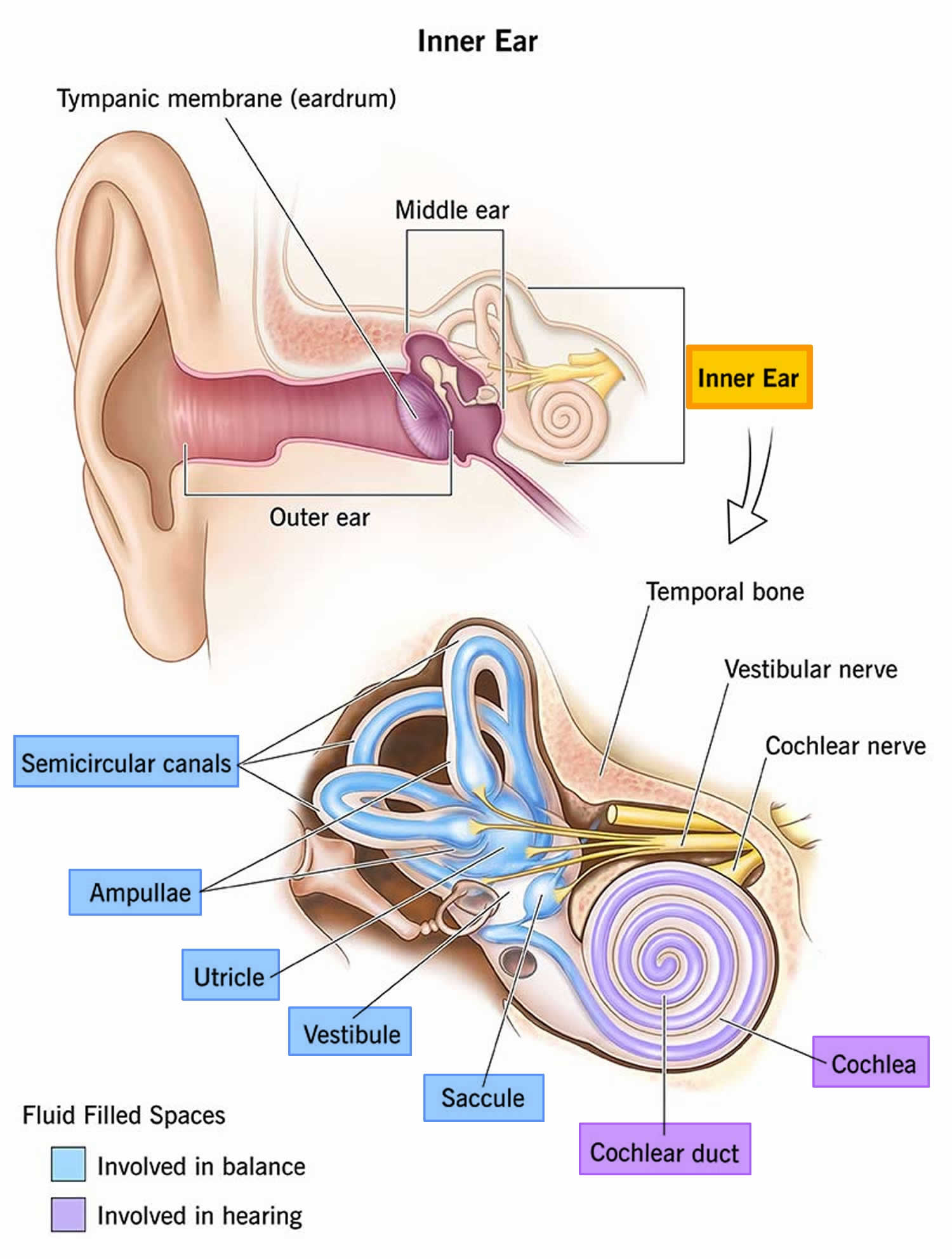
Figure 1. Inner ear anatomy
Footnotes: Representation of the ear from the outer ear to the middle ear and to the inner ear. The inner ear (internal ear) is the innermost part of your ear consisting of the cochlea (the snail-shaped portion on the right), and the semicircular canals on the left represent the vestibular system. The inner ear is mainly responsible for sound detection and balance. The inner ear consists of the bony labyrinth, a hollow cavity in the temporal bone of the skull with a system of passages comprising two main functional parts: (1) The cochlea, dedicated to hearing; converting sound pressure patterns from the outer ear into electrochemical impulses which are passed on to the brain via the auditory nerve. (2) The vestibular system, dedicated to balance. The inner ear is innervated by cranial nerve eight (CN VIII) also known as vestibulocochlear nerve that consists of the vestibular and cochlear nerves 38. The vestibular nerve is primarily responsible for maintaining body balance and eye movements, while the cochlear nerve is responsible for hearing 43. Damage to the vestibular nerve results in vertigo, a balance disorder, and nystagmus 43. The endolymph (blue and purple fluid) is the fluid contained in the membranous labyrinth of the inner ear and has a higher level of potassium than sodium.
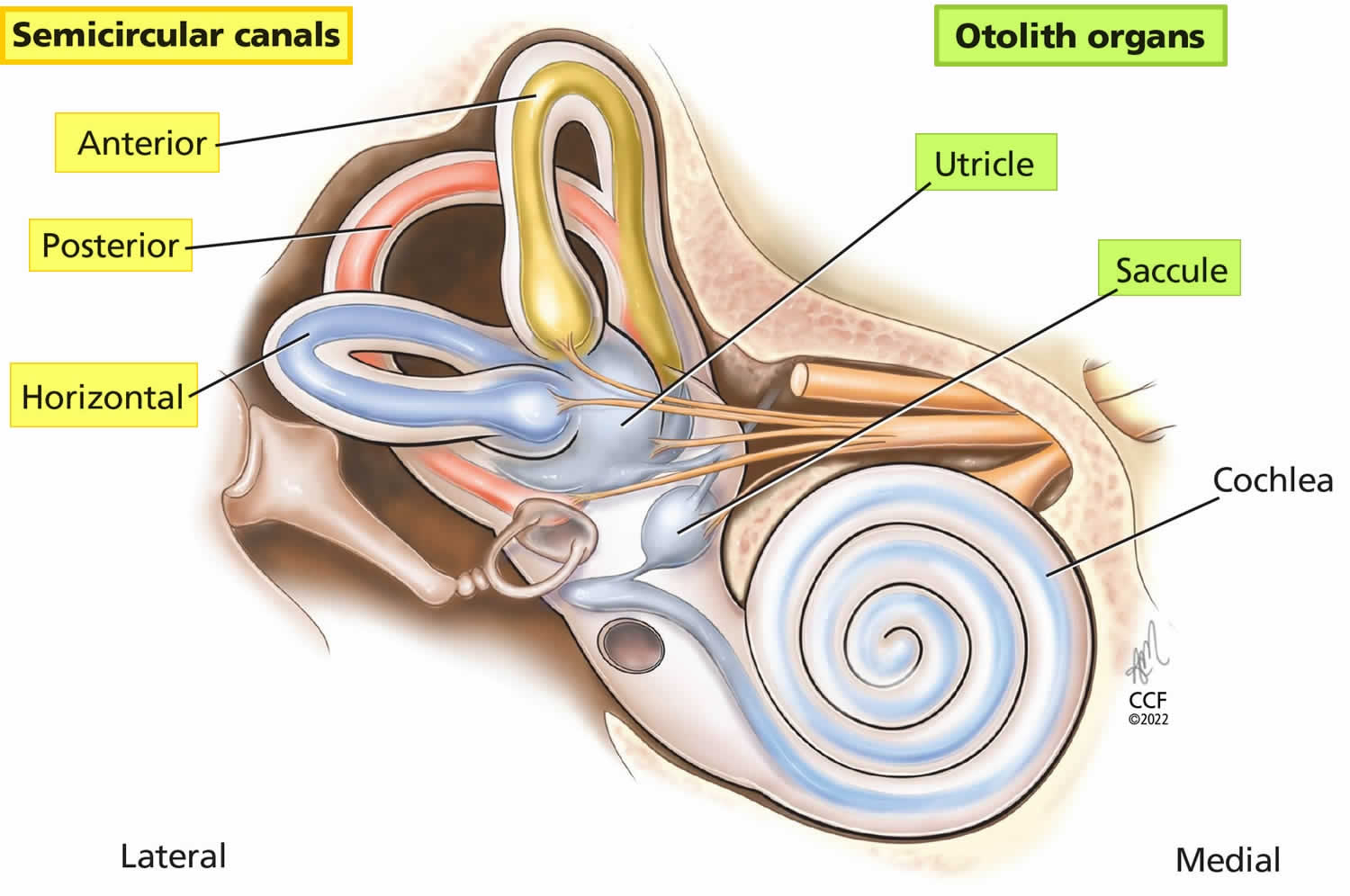
Figure 2. Semicircular canals and the otolith organs
Footnote: The 3 semicircular canals (anterior, posterior, horizontal) sense angular head accelerations and the otolith organs (saccule, uticle) sense linear head accelerations, providing internal cues for orientation of position in space, movement, gaze stabilization, and postural control.
[Source 26 ]Figure 3. Semicircular canal anatomy
Footnote: The semicircular canals are part of the vestibular system of the inner ear. The semicircular canals are curved, looped structures that are referred to according to their orientation: lateral (horizontal), anterior (superior), and posterior. These structures are positioned at roughly right angles in relation to one another. The lateral semicircular canal, the shortest of the three, is set at an angle of about 30 degrees to the horizontal plane. The anterior and posterior loops are in diagonal vertical planes that intersect at a 90-degree angle.
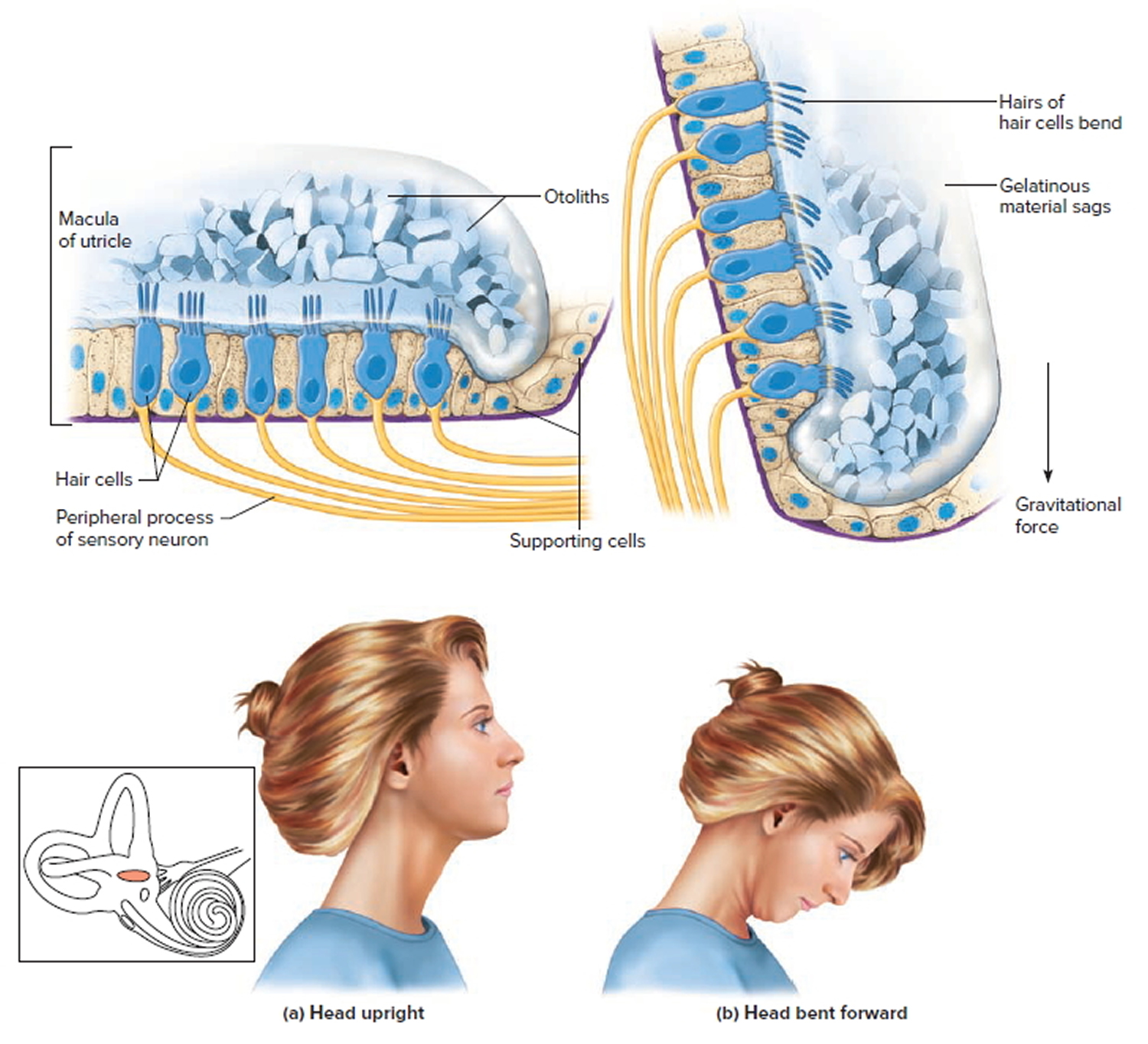
Figure 4. Inner ear maculae respond to changes in head position
Note:The hair cells within the utricle are surrounded by a gelatinous substance and hold the microscopic otoliths (otoconia). (a) Orientation of hair cells within the macula of the utricle with the head in an upright position. (b) Macula of the utricle with the head bent forward, which results in a deflection of the hair cells due to a gravitational pull.
Figure 5. Dynamic inner ear balance organs (crista ampullaris) within the Semicricular ducts
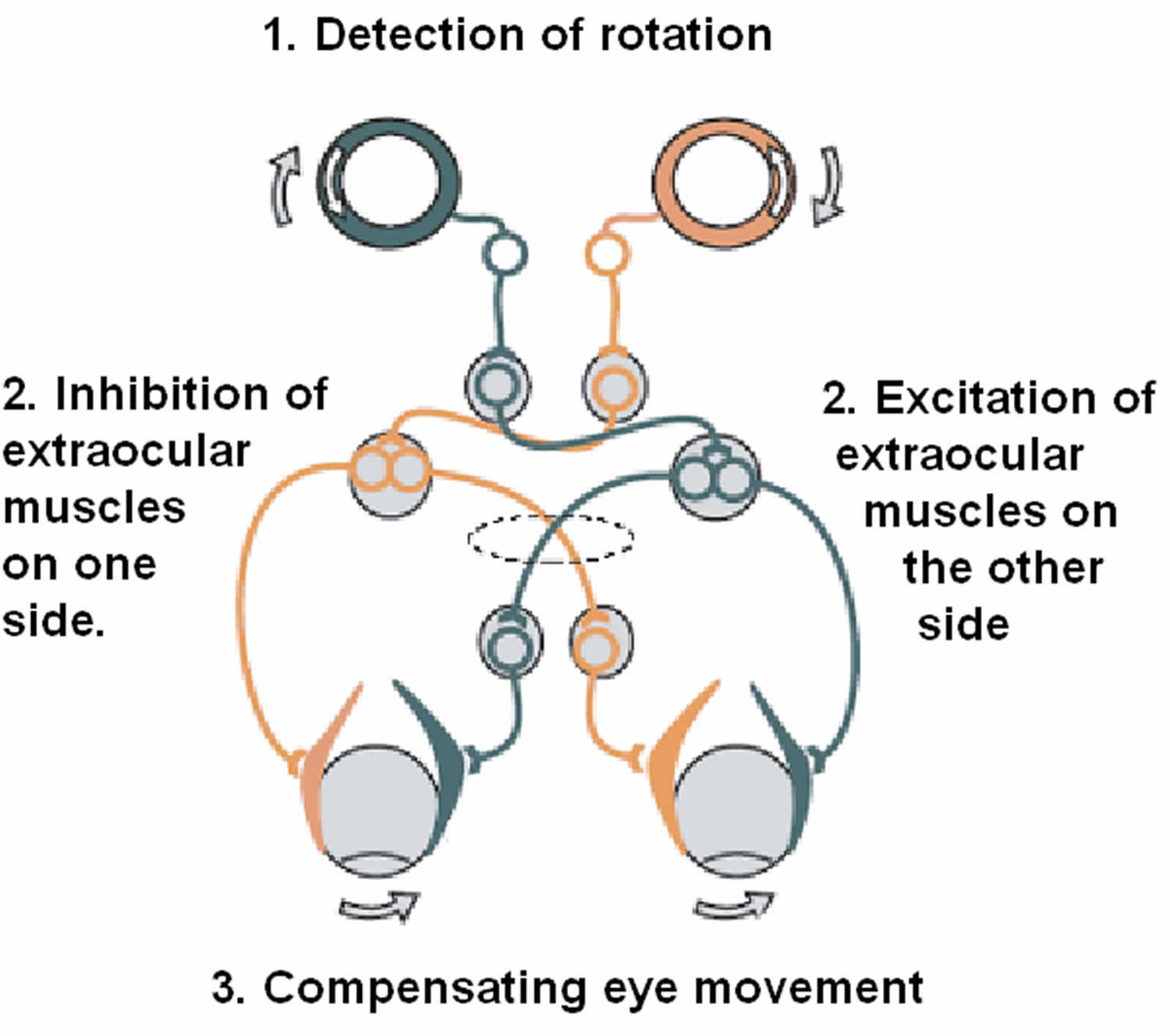
Figure 6. Vestibulo-ocular reflex (VOR)
Footnote: The vestibulo-ocular reflex (VOR). A rotation of the head is detected, which triggers an inhibitory signal to the extraocular muscles on one side and an excitatory signal to the muscles on the other side. The result is a compensatory movement of the eyes.
[Source 12 ]Oscillopsia causes
Oscillopsia usually results from diseases affecting the inner ear balance mechanisms or the back part of the brain (brainstem or cerebellum). Damage of the vestibulo-ocular reflex (VOR) leads to oscillopsia 44. The incoordination between the vestibular and ocular systems prevents the information about head and body movements from reaching the oculomotor centers. As a result, the patient has difficulty fixating on a target point while the head turns. Bilateral loss of vestibular function leads the patient to believe that the world is moving with head movements. Vertigo, dizziness, and imbalance are common symptoms of oscillopsia 4.
Although the reason for many cases is never determined, bilateral loss of vestibular function can be due to:
- Toxic side effect of an antibiotic, usually an aminoglycoside medication such as gentamicin.
- Certain infections, especially viral illness or meningitis in children.
- Meniere’s disease.
- Labyrinthitis. Labyrinthitis is inflammation of the inner ear labyrinth or semi-circular canals. Symptoms may include sudden dizziness, tinnitus, and hearing loss.
- Vertigo. Vertigo is a way to describe feeling dizzy or off balance. True vertigo involves a sensation of spinning. It’s a symptom of various conditions but isn’t a condition itself.
- Vestibular neuritis. Vestibular neuritis is inflammation of the vestibulocochlear nerve in your inner ear. It can cause sudden severe vertigo, dizziness, nausea and vomiting. It’s usually treated with medication to help with nausea and dizziness.
- Benign paroxysmal positional vertigo (BPPV). BPPV happens when the crystals in your vestibule move into your semicircular canals and become trapped. When that happens, you might be more sensitive to movement that usually doesn’t bother you, such as rolling over in bed or when looking up towards the ceiling. BPPV can go away on its own, but it may return. The most effective treatment includes physical therapy exercises. Your healthcare provider can tell you how to manage any symptoms you might have.
Jerk nystagmus usually results from diseases affecting the inner ear balance mechanisms (vestibulo-ocular reflex) or the back part of the brain (brainstem or cerebellum). Pendular nystagmus can result from brain diseases such as multiple sclerosis, but can be a congenital problem as well.
Oscillopsia is also a potential complication following skull base tumor resection 3.
Masticatory oscillopsia has been reported in up to a third of patients following orbital decompression resulting from transmission of temporalis contractions to the globe through the resultant orbital defect 45, 46. Patients who undergo traumatic orbital wall fracture may develop orbital meningoencephalocele and experience ocular pulsation 47. Mettu et al. 48 described two cases of tumor-related oscillopsia.
Oscillopsia symptoms
Oscillopsia is an illusory sensation that your stationary environment is moving 8, 9, 10. Oscillopsia is usually either caused by abnormal movement of the eyes such as nystagmus or bilateral (both sides) vestibular loss when the person’s head is moving 13. Nystagmus is defined by rhythmic, abnormal eye movements with a “slow” eye movement driving the eye off the target followed by a second movement that brings the eye back to the target 14. Oscillopsia occurs when the deficient vestibulo-ocular reflexes (VOR) and the back part of your eye (the retina) cannot keep the visual environment stable and the world appears to bounce or move 13.
Oscillopsia is often incapacitating, typically resulting in nausea, vertigo and loss of balance; disabling effective interaction with the world around them 49.
The other major symptom of the bilateral loss of vestibulo-ocular reflex (VOR) is lack of balance and a risk of falls 50. Falls are most likely when walking in the dark or on soft surfaces such as carpeting, sand or grass. Because people affected with vestibular function loss have trouble orienting themselves and the position of their bodies, swimming can be dangerous. They should never swim alone, especially at night or on a cloudy or dark day, because when they are under water, they may not be able to sense up from down due to the lack of visual and other sensory cues.
Oscillopsia diagnosis
The diagnosis of oscillopsia is made through a combination of your history, clinical and/or radiological findings. Your doctor may do a series of tests to determine the cause of your oscillopsia. In addition, you may be given blood tests to check for infection and other tests to check heart and blood vessel health.
Most people visiting their doctor because of oscillopsia will first be asked about their symptoms and medications and then be given a physical examination. During this exam, your doctor will check how you walk and maintain your balance and how the major nerves of your central nervous system are working.
During a physical exam, your doctor will likely look for:
- Signs and symptoms of dizziness that are prompted by eye or head movements and then decrease in less than one minute
- Dizziness with specific eye movements that occur when you lie on your back with your head turned to one side and tipped slightly over the edge of the examination bed
- Involuntary movements of your eyes from side to side
- Inability to control your eye movements
Ewald’s three laws for vestibular diagnostic testing 27
- Stimulation of a semicircular canal generates eye movements in the plane of that canal.
- In the horizontal semicircular canals, movement of the endolymph toward the ampulla (ampullopetal) causes deflection of the cupula toward the utricle (utriculopetal) and results in excitation (greater neural activity) compared to movement away from the utricle (utriculofugal).
- In the vertical semicircular canals (anterior and posterior), movement of the endolymph away from the ampulla (ampullofugal) causes greater deflection of the cupula away from the utricle (utriculofugal) and results in a greater excitation compared to utriculopetal movement, which is opposite to that in the horizontal canals.
Doctors use several tests to diagnose inner ear problems, particularly problems with balance. Here are a few examples of inner ear tests:
- Eye movement testing. Your doctor may watch the path of your eyes when you track a moving object. And you may be given an eye motion test in which water or air is placed in your ear canal.
- Head movement testing. If your doctor suspects your vertigo is caused by benign paroxysmal positional vertigo (BPPV), he or she may do a simple head movement test called the Dix-Hallpike maneuver to verify the diagnosis.
- Fukuda-Unterberger test. Your healthcare provider will ask you to march in place for 30 seconds with your eyes closed. If you rotate or lean to one side, it could mean that you have an issue with your inner ear labyrinth. This could cause vertigo.
- Romberg’s test. During this assessment, your provider will ask you to close your eyes while standing with your feet together and your arms to your side. If you feel unbalanced or unsteady, it could mean that you have an issue with your central nervous system (your brain or spinal cord).
- Head impulse test. For this test, your provider will gently move your head to each side while you focus your eyes on a stationary target (for example a spot on the wall or your provider’s nose). As they move your head, they’ll pay close attention to your eye movements. This can tell them if there’s an issue with the balance system in your inner ear.
- Vestibular test battery. This includes several different tests to check the vestibular portion of your inner ear system. A vestibular test battery can help determine whether your symptoms are a result of an inner ear issue or a brain issue.
- Posturography. This test tells your doctor which parts of the balance system you rely on the most and which parts may be giving you problems. You stand in your bare feet on a platform and try to keep your balance under various conditions.
- Rotary chair testing. During this test you sit in a computer-controlled chair that moves very slowly in a full circle. At faster speeds, it moves back and forth in a very small arc.
- Vestibular test battery: This includes several different tests that assess how well the vestibular part of your inner ear and eye reflexes are functioning. Testing may include videonystagmography (VNG), vestibular evoked myogenic potentials (VEMPs), rotary chair and video head impulse testing (vHIT). People taking most of these tests will need to wear goggles around their eyes so doctors can monitor eye movement.
- Electronystagmography (ENG) or videonystagmography (VNG). The purpose of these tests is to detect abnormal eye movement. Electronystagmography (ENG) which uses electrodes) or videonystagmography (VNG) which uses small cameras can help determine if your dizziness is due to inner ear disease by measuring involuntary eye movements while your head is placed in different positions or your balance organs are stimulated with water or air.
- Audiometry tests: In this test, which checks hearing, people sit in a sound booth. They respond to soft sounds and repeat words so audiologists can evaluate their ability to hear and understand. This test helps audiologists to discuss the type and degree of hearing loss that people have and how that hearing loss may affect their daily life.
- Auditory brainstem response (ABR) testing: This test involves placing small electrodes on people’s foreheads or behind their ears so audiologists can measure how people’s hearing nerve responds to sound.
- Otoacoustic emissions (OAEs): This test evaluates how well your outer hair cells work. It involves playing sounds into your ears and recording the sounds’ echoes.
- Magnetic resonance imaging (MRI). This test uses a magnetic field and radio waves to create cross-sectional images of your head and body. Your doctor can use these images to identify and diagnose a range of conditions. MRI may be performed to rule out other possible causes of vertigo.
If your doctor suspects you are having or may have had a stroke, are older or suffered a blow to the head, he or she may immediately order an CT (computed tomography) scan or MRI (magnetic resonance imaging).
Oscillopsia test
Assessment of the vestibulo-ocular reflex (VOR) takes place using the Halmagyi-Curthoys test also known as the head impulse test or rapid impulse test 51. To perform the head impulse test, the physician will rapidly move the patient’s head in one direction (left or right), and the eyes should remain in place focused on a particular object in front of them despite the head movement. If a patient’s vestibulo-ocular reflex (VOR) has damage on one side when their head turns to that direction with force, their eyes will follow the direction of the head movement before coming back to their focal point; this would imply some issue in the vestibulo-ocular reflex arc 51. The vestibulo-ocular reflex (VOR) may also be tested using the caloric reflex test, where cold water or warm water is poured into the patient’s external auditory canal using a syringe to induce nystagmus. When using cold water, the fast phase of nystagmus should be to the opposite side of the ear filled with the water. However, when using warm water, the fast phase of nystagmus should be on the same side as the water-filled ear. If this eye movement is abnormal and not occurring as described in the patient, there is likely vestibular dysfunction in the side being stimulated by water 52. Brain death is a complete loss of cerebral function 53. If performing the caloric reflex test and the vestibulo-ocular reflex (VOR) is absent in the patient, this is likely a serious indicator of brain death 54.
Oscillopsia treatment
Oscillopsia treatment is directed at the underlying cause 55, 56, 57, 58. Treatment for bilateral loss of vestibular function is physical rehabilitation with an individualized program designed by a vestibular rehabilitation specialist. Depending on the degree of the problem, therapy works to improve vestibular function or help the person develop alternative sensory cues such as from the neck, feet or eyes that can substitute for the missing sensations from the labyrinth. Tai chi or other balance exercises may also help patients regain balance over time.
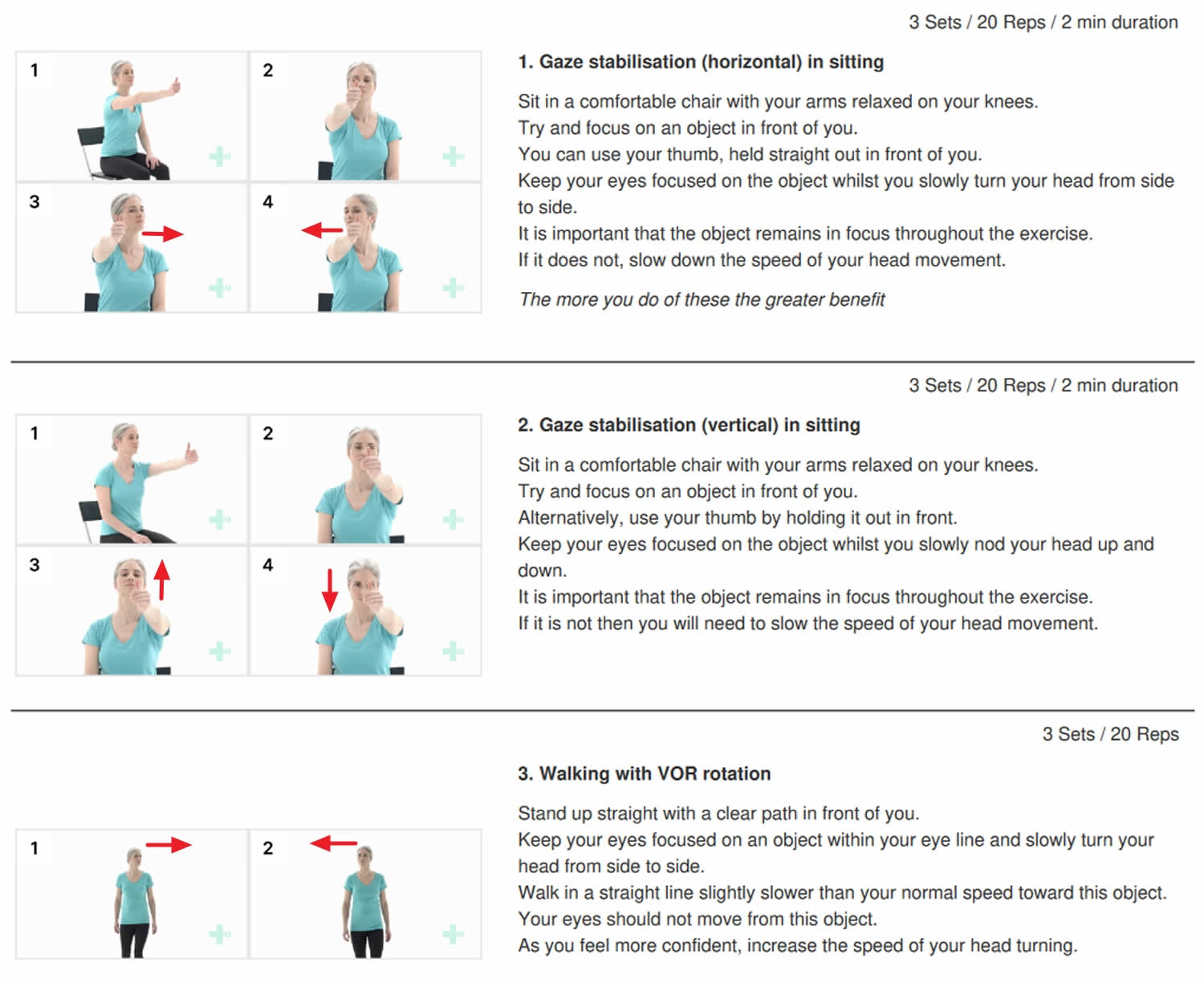
Vestibular rehabilitation therapy (Balance therapy)
You may learn specific exercises to help make your balance system less sensitive to motion. It is used for people with dizziness from inner ear conditions such as vestibular neuritis. However, it is challenging to restore the vestibulo-ocular reflex (VOR) function at high velocities in severe cases of vestibular loss 59. The goal of vestibular rehabilitation therapy (balance therapy) is to practice head and eye movements with different activities and postures. They should repeat movements that stimulate vertigo and continue to expose patients to different types of sensory and motor environments 60. The vestibulo-ocular reflex (VOR) exercises should start with patients in a seated, still position to assess if there is an aggravation of symptoms such as dizziness, nausea, and anxiety. The exercises can slowly increase in velocity. By gradually increasing the intensity, the capacity of the vestibulo-ocular reflex (VOR) system will not be overwhelmed. Research has indicated that the therapeutic exercises mentioned above are effective in reducing dizziness symptoms and the associated psychological consequences 61.
Other methods to rehabilitate the vestibulo-ocular reflex (VOR) function are under development. For example, researchers found that artificial restoration of the vestibulo-ocular reflex (VOR) function is possible by electrically stimulating the lateral ampullary nerve (LAN) branch of the vestibular branch in humans 62.
7. Vestibular rehabilitation therapy (vestibulo-ocular reflex exercises)
Surgical procedures
Surgery is not the first-line of treatment for vestibulo-ocular reflex (VOR) malfunction. It’s rare, but you might need surgery when a serious underlying health issue — like a brain tumor or neck injury — causes vertigo. Doctors typically only recommend surgery when other treatments don’t work. Your surgeon will tell you which type of procedure you need and what to expect.
- Injections. Your doctor may inject your inner ear with the antibiotic gentamicin to disable the balance function. The unaffected ear takes over that function.
- Alternatively, injection of botulinum toxin to selected extraocular muscles has been reported to provide some symptomatic relief specifically those with oscillopsia due to ataxic disconjugate nystagmus. While not a cure, the transient therapeutic effect of the botulinum toxin makes it a suitable option for the management of complex ocular motility problems during the rehabilitation period 63, 64.
- Removal of the inner ear sense organ. A procedure that’s rarely used is called labyrinthectomy. It disables the vestibular labyrinth in the affected ear. The other ear takes over the balance function. This technique may be used if you have serious hearing loss and your dizziness hasn’t responded to other treatments.
Oscillopsia prognosis
The ability to restore the vestibulo-ocular reflex (VOR) function varies. Due to neuroplasticity, it usually improves spontaneously with time, and no intervention is needed. Oscillopsia prognosis is dependent on the underlying cause. Recovering from a bilateral loss of vestibular function depends on many factors, including:
- How fast the loss of function progressed — the slower the loss, the more readily the brain can adapt to compensate for it.
- Your age — younger people tend to adapt more easily.
- The amount of remaining function — more function makes it easier to compensate.
- The other ways the brain determines where a person is in space (in addition to the vestibular system) are through the visual and proprioceptive/joint position sensor systems. If one or both of these are also compromised, recovery and compensation will be more difficult.
Recovering from bilateral loss of vestibular function takes time and commitment, as well as the help of a supportive team. Continued exercises and practice can help people compensate for their condition, improve balance and improve quality of life.
- Anson ER, Kiemel T, Carey JP, Jeka JJ. Eye Movements Are Correctly Timed During Walking Despite Bilateral Vestibular Hypofunction. J Assoc Res Otolaryngol. 2017 Aug;18(4):591-600. doi: 10.1007/s10162-017-0626-8[↩]
- Handelsman J.A. Vestibulotoxicity: Strategies for clinical diagnosis and rehabilitation. Int. J. Audiol. 2018;57:S69–S77. doi: 10.1080/14992027.2018.1468092[↩]
- Goethe EA, Hartford J, Foroozan R, Patel AJ. Oscillopsia following orbitotomy for intracranial tumor resection. Surg Neurol Int. 2021 Sep 13;12:459. doi: 10.25259/SNI_498_2021[↩][↩]
- Tilikete C, Vighetto A. Oscillopsia: causes and management. Curr Opin Neurol. 2011 Feb;24(1):38-43. doi: 10.1097/WCO.0b013e328341e3b5[↩][↩]
- Anson ER, Gimmon Y, Kiemel T, Jeka JJ, Carey JP. A Tool to Quantify the Functional Impact of Oscillopsia. Front Neurol. 2018 Mar 15;9:142. doi: 10.3389/fneur.2018.00142[↩]
- Brantberg K, Löfqvist L. Preserved vestibular evoked myogenic potentials (VEMP) in some patients with walking-induced oscillopsia due to bilateral vestibulopathy. J Vestib Res. 2007;17(1):33-8. DOI: 10.3233/VES-2007-17104[↩]
- Strupp M, Kim JS, Murofushi T, Straumann D, Jen JC, Rosengren SM, et al.. Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the Barany society. J Vestib Res. (2017) 27:177–89. 10.3233/VES-170619[↩]
- Abadi RV, Whittle JP, Worfolk R. Oscillopsia and tolerance to retinal image movement in congenital nystagmus. Invest Ophthalmol Vis Sci. 1999 Feb;40(2):339-45. https://iovs.arvojournals.org/article.aspx?articleid=2181134[↩][↩]
- Leigh RJ, Dell’Osso LF, Yaniglos SS, Thurston SE. Oscillopsia, retinal image stabilization and congenital nystagmus. Invest Ophthalmol Vis Sci. 1988 Feb;29(2):279-82. https://iovs.arvojournals.org/article.aspx?articleid=2178051[↩][↩]
- Wist ER, Brandt T, Krafczyk S. Oscillopsia and retinal slip. Evidence supporting a clinical test. Brain. 1983 Mar;106 (Pt 1):153-68. doi: 10.1093/brain/106.1.153[↩][↩]
- Eckhardt-Henn A, Breuer P, Thomalske C, Hoffmann SO, Hopf HC. Anxiety disorders and other psychiatric subgroups in patients complaining of dizziness. J Anxiety Disord. 2003;17(4):369-88. doi: 10.1016/s0887-6185(02)00226-8[↩]
- Somisetty S, M Das J. Neuroanatomy, Vestibulo-ocular Reflex. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545297[↩][↩][↩][↩][↩][↩]
- Bilateral Loss of Labyrinthine Function. https://www.hopkinsmedicine.org/health/conditions-and-diseases/bilateral-loss-of-labyrinthine-function[↩][↩][↩][↩][↩]
- Nystagmus. https://eyewiki.org/Nystagmus[↩][↩]
- Cha YH, Lee H, Santell LS, Baloh RW. Association of benign recurrent vertigo and migraine in 208 patients. Cephalalgia. 2009 May;29(5):550-5. doi: 10.1111/j.1468-2982.2008.01770.x[↩]
- Takahashi M, Okada Y, Saito A, Takei Y, Tomizawa I, Uyama K, Takeuti I, Kanzaki J. Roles of head, gaze, and spatial orientation in the production of oscillopsia. J Vestib Res. 1990-1991;1(3):215-22.[↩]
- Kaminski HJ, Leigh RJ. International Symposium for Therapy of Ocular Motility and Related Visual Disturbances. Neurology. 1997 May;48(5):1178-84. doi: 10.1212/wnl.48.5.1178[↩]
- Guinand N, Pijnenburg M, Janssen M, Kingma H. Visual acuity while walking and oscillopsia severity in healthy subjects and patients with unilateral and bilateral vestibular function loss. Arch Otolaryngol Head Neck Surg. 2012 Mar;138(3):301-6. doi: 10.1001/archoto.2012.4[↩]
- Lambert S, Sigrist A, Delaspre O, Pelizzone M, Guyot JP. Measurement of dynamic visual acuity in patients with vestibular areflexia. Acta Otolaryngol. 2010 Jul;130(7):820-3. doi: 10.3109/00016480903426592[↩]
- Tilikete, C and Vighetto, A. 2011. Oscillopsia: causes and management. Current Opinion in Neurology, 24(1): 38–43. DOI: 10.1097/WCO.0b013e328341e3b5[↩]
- Anson, ER, et al. 2018. A Tool to Quantify the Functional Impact of Oscillopsia. Frontiers in Neurology, 9(142). DOI: 10.3389/fneur.2018.00142[↩]
- Rowe, FJ, et al. 2018. Interventions for eye movement disorders due to acquired brain injury. Cochrane Database of Systematic Reviews, 3: pub2. DOI: 10.1002/14651858.CD011290.pub2[↩]
- Tse, BC, McKeown, CA and Tse, DT. 2017. Titanium T-Plate as a Platform for Globe Stabilization in Acquired Nystagmus and Oscillopsia Without a Null Zone. Ophthalmic Plastic and Reconstructive Surgery, 33(3): e61–e63. DOI: 10.1097/IOP.0000000000000750[↩]
- Yoo H, Mihaila DM. Neuroanatomy, Vestibular Pathways. [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557380[↩]
- Fetter M. Vestibulo-ocular reflex. Dev Ophthalmol. 2007;40:35-51. https://doi.org/10.1159/000100348[↩][↩][↩][↩][↩]
- Benign paroxysmal positional vertigo: Effective diagnosis and treatment. Shayna R. Cole, Julie A. Honaker. Cleveland Clinic Journal of Medicine Nov 2022, 89 (11) 653-662; https://doi.org/10.3949/ccjm.89a.21057[↩][↩]
- Wallace B, Lifshitz J. Traumatic brain injury and vestibulo-ocular function: current challenges and future prospects. Eye Brain. 2016 Sep 6;8:153-164. doi: 10.2147/EB.S82670[↩][↩][↩][↩][↩][↩][↩]
- Sherman KR, Keller EL. Vestibulo-ocular reflexes of adventitiously and congenitally blind adults. Invest Ophthalmol Vis Sci. 1986 Jul;27(7):1154-9. https://iovs.arvojournals.org/article.aspx?articleid=2177479[↩][↩]
- Jacobson GP, Shepard NT. Balance Function Assessment and Management. 2nd ed. California: Plural Publishing, Inc; 2016.[↩][↩]
- Ernst A, Basta D, Seidl RO, Todt I, Scherer H, Clarke A. Management of posttraumatic vertigo. Otolaryngol Head Neck Surg. 2005 Apr;132(4):554-8. doi: 10.1016/j.otohns.2004.09.034[↩]
- Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol. 1952;61:987–1016. doi: 10.1177/000348945206100403[↩]
- Dorigueto RS, Mazzetti KR, Gabilan YP, Ganança FF. Benign paroxysmal positional vertigo recurrence and persistence. Braz J Otorhinolaryngol. 2009 Jul-Aug;75(4):565-72. doi: 10.1016/s1808-8694(15)30497-3[↩]
- Goldberg JM, Cullen KE. Vestibular control of the head: possible functions of the vestibulocollic reflex. Exp Brain Res. 2011 May;210(3-4):331-45. doi: 10.1007/s00221-011-2611-5[↩]
- Pozzo T, Berthoz A, Papvov C. In: Taguchi K, Igarashi M, Mori S, editors. The effect of gravity on the coordination between posture and movement; Vestibular and Neural Front, Proceedings of the 12th International Symposium on Posture and Gait; Amsterdam: Elsevier; 1994. pp. 589–602.[↩]
- Bronstein AM, Hood JD. The cervico-ocular reflex in normal subjects and patients with absent vestibular function. Brain Res. 1986 May 14;373(1-2):399-408. doi: 10.1016/0006-8993(86)90355-0[↩]
- Pompeiano O. The tonic neck reflex: supraspinal control. In: Peterson BW, Richmond FJ, editors. Control of Head Movement. New York: Oxford University Press; 1988. pp. 108–119.[↩]
- Peterson BW, Goldberg J, Bilotto G, Fuller JH. Cervicocollic reflex: its dynamic properties and interaction with vestibular reflexes. J Neurophysiol. 1985 Jul;54(1):90-109. doi: 10.1152/jn.1985.54.1.90[↩]
- Bordoni B, Mankowski NL, Daly DT. Neuroanatomy, Cranial Nerve 8 (Vestibulocochlear) [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537359[↩][↩][↩][↩]
- Carleton SC, Carpenter MB. Afferent and efferent connections of the medial, inferior and lateral vestibular nuclei in the cat and monkey. Brain Res. 1983 Nov 14;278(1-2):29-51. doi: 10.1016/0006-8993(83)90223-8[↩][↩]
- Brandt, T. and Dieterich, M. (1994), Vestibular syndromes in the roll plane: Topographic diagnosis from brainstem to cortex. Ann Neurol., 36: 337-347. https://doi.org/10.1002/ana.410360304[↩]
- Brandt T, Dieterich M. Vestibular syndromes in the roll plane: topographic diagnosis from brainstem to cortex. Ann Neurol. 1994 Sep;36(3):337-47. doi: 10.1002/ana.410360304[↩][↩]
- Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Central vestibular pathways: eye, head, and body reflexes Neuroscience. 2nd ed. Sunderland, MA: Sinauer Associates; 2001.[↩]
- Benoudiba F, Toulgoat F, Sarrazin JL. The vestibulocochlear nerve (VIII). Diagn Interv Imaging. 2013 Oct;94(10):1043-50. https://doi.org/10.1016/j.diii.2013.08.015[↩][↩][↩][↩]
- Lucieer F, Vonk P, Guinand N, Stokroos R, Kingma H, van de Berg R. Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol. (2016) 7:26. 10.3389/fneur.2016.00026[↩]
- Fayers T, Barker LE, Verity DH, Rose GE. Oscillopsia after lateral wall orbital decompression. Ophthalmology. 2013 Sep;120(9):1920-3. doi: 10.1016/j.ophtha.2013.01.063[↩]
- Porrúa-Tubío L, Sales-Sanz A, de-Arriba-Palomero P, Felix-Espinar B, de-Arriba-Palomero F, Alonso-Formento N, Albandea-Jiménez A, Rodríguez-Del-Valle JM, Sales-Sanz M. Oscillopsia After Isolated Lateral Wall Decompression Versus Balanced or 3-Wall Decompression. Ophthalmic Plast Reconstr Surg. 2021 Mar-Apr 01;37(2):141-144. doi: 10.1097/IOP.0000000000001716[↩]
- Ha AY, Mangham W, Frommer SA, Choi D, Klinge P, Taylor HO, Oyelese AA, Sullivan SR. Interdisciplinary Management of Minimally Displaced Orbital Roof Fractures: Delayed Pulsatile Exophthalmos and Orbital Encephalocele. Craniomaxillofac Trauma Reconstr. 2017 Mar;10(1):11-15. doi: 10.1055/s-0036-1584395[↩]
- Mettu P, Bhatti MT, El-Dairi MA, Price EB, Lin AY, Alaraj A, Setabutr P, Moss HE. Orbito-Masticatory Syndrome. J Neuroophthalmol. 2016 Sep;36(3):308-12. doi: 10.1097/WNO.0000000000000354[↩]
- Randall D, Griffiths H, Arblaster G, Bjerre A, Fenner J. Simulation of Oscillopsia in Virtual Reality. Br Ir Orthopt J. 2018 Jun 19;14(1):45-49. doi: 10.22599/bioj.112[↩]
- Fife TD, Tusa RJ, Furman JM, Zee DS, Frohman E, Baloh RW, Hain T, Goebel J, Demer J, Eviatar L. Assessment: vestibular testing techniques in adults and children: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2000 Nov 28;55(10):1431-41. doi: 10.1212/wnl.55.10.1431[↩]
- McGarvie LA, MacDougall HG, Halmagyi GM, Burgess AM, Weber KP, Curthoys IS. The Video Head Impulse Test (vHIT) of Semicircular Canal Function – Age-Dependent Normative Values of VOR Gain in Healthy Subjects. Front Neurol. 2015 Jul 8;6:154. doi: 10.3389/fneur.2015.00154[↩][↩]
- Gonçalves DU, Felipe L, Lima TM. Interpretation and use of caloric testing. Braz J Otorhinolaryngol. 2008 May-Jun;74(3):440-6. doi: 10.1016/s1808-8694(15)30580-2[↩]
- Wijdicks EF. Determining Brain Death. Continuum (Minneap Minn). 2015 Oct;21(5 Neurocritical Care):1411-24. doi: 10.1212/CON.0000000000000221. Erratum in: Continuum (Minneap Minn). 2015 Dec;21(6 Neuroinfectious Disease):1550.[↩]
- Meneses E, Sampaio A, Venosa A, Tauil P, Dias M, Oliveira C. Vestibulo-ocular reflex as predictor of cerebral death in comatose patients. Int Tinnitus J. 2010;16(1):8-13.[↩]
- van de Berg R, Guinand N, Ranieri M, Cavuscens S, Khoa Nguyen TA, Guyot JP, et al.. The vestibular implant input interacts with residual natural function. Front Neurol. (2017) 8:644. 10.3389/fneur.2017.00644[↩]
- van de Berg R, Guinand N, Nguyen TA, Ranieri M, Cavuscens S, Guyot JP, et al. The vestibular implant: frequency-dependency of the electrically evoked vestibulo-ocular reflex in humans. Front Syst Neurosci. (2014) 8:255 10.3389/fnsys.2014.00255[↩]
- van de Berg R, Guinand N, Stokroos RJ, Guyot JP, Kingma H. The vestibular implant: quo vadis? Front Neurol. (2011) 2:47. 10.3389/fneur.2011.00047[↩]
- Guinand N, Van de Berg R, Cavuscens S, Stokroos R, Ranieri M, Pelizzone M, et al.. Restoring visual acuity in dynamic conditions with a vestibular implant. Front Neurosci. (2016) 10:577. 10.3389/fnins.2016.00577[↩]
- Curthoys IS, Halmagyi GM. Vestibular compensation: a review of the oculomotor, neural, and clinical consequences of unilateral vestibular loss. J Vestib Res. 1995 Mar-Apr;5(2):67-107.[↩]
- Han BI, Song HS, Kim JS. Vestibular rehabilitation therapy: review of indications, mechanisms, and key exercises. J Clin Neurol. 2011 Dec;7(4):184-96. doi: 10.3988/jcn.2011.7.4.184[↩]
- Pavlou M, Lingeswaran A, Davies RA, Gresty MA, Bronstein AM. Simulator based rehabilitation in refractory dizziness. J Neurol. 2004 Aug;251(8):983-95. doi: 10.1007/s00415-004-0476-2[↩]
- Perez Fornos A, Guinand N, van de Berg R, Stokroos R, Micera S, Kingma H, Pelizzone M, Guyot JP. Artificial balance: restoration of the vestibulo-ocular reflex in humans with a prototype vestibular neuroprosthesis. Front Neurol. 2014 Apr 29;5:66. doi: 10.3389/fneur.2014.00066[↩]
- Kipioti A, Taylor RH. Botulinum toxin treatment of “one and a half syndrome”. Br J Ophthalmol. 2003 Jul;87(7):918-9. doi: 10.1136/bjo.87.7.918-a[↩]
- Murthy R, Dawson E, Khan S, Adams GG, Lee J. Botulinum toxin in the management of internuclear ophthalmoplegia. J AAPOS. 2007 Oct;11(5):456-9. doi: 10.1016/j.jaapos.2007.03.005[↩]