Contents
What is pancolitis
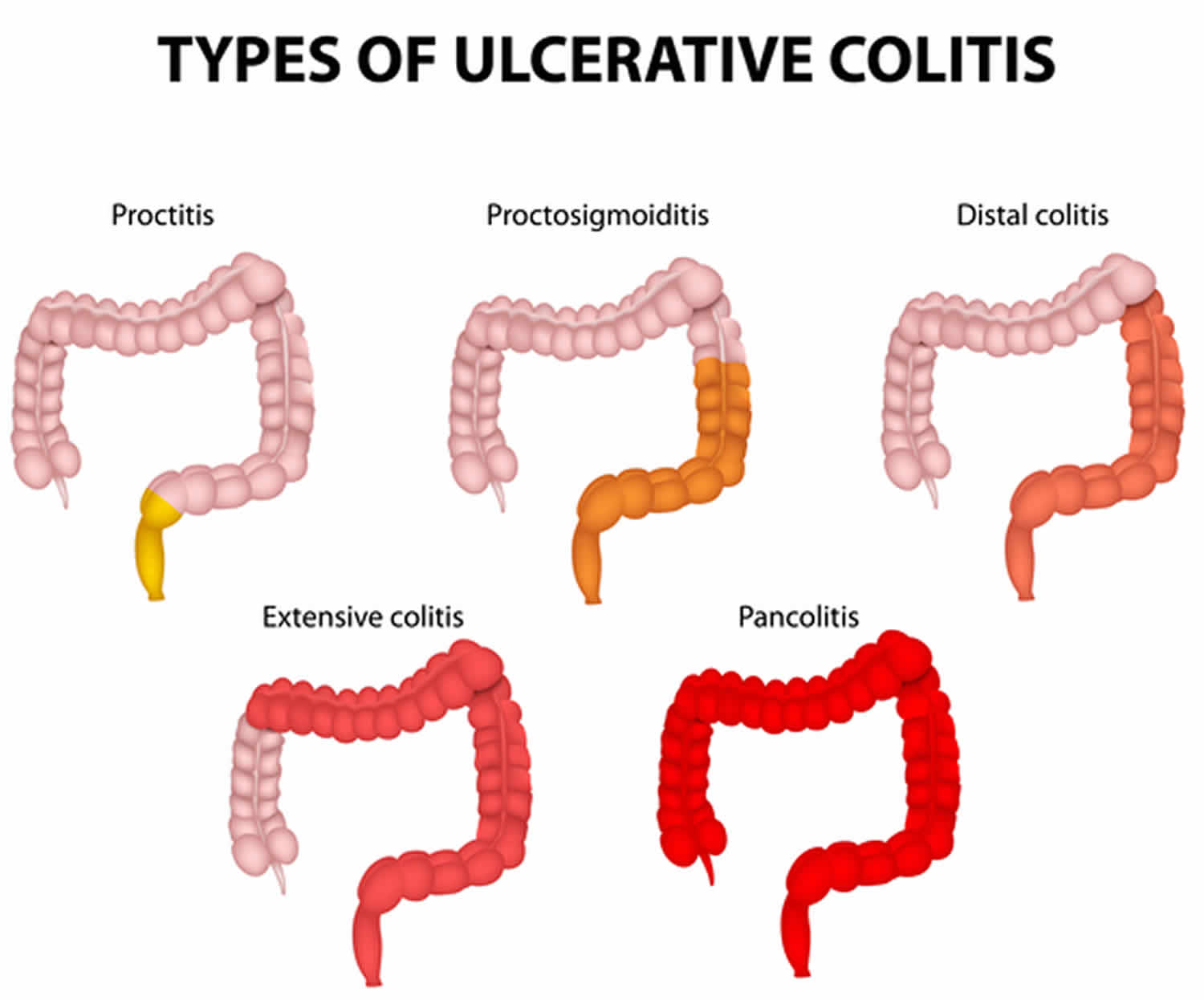
Pancolitis is more commonly known as ulcerative colitis, which is a condition in which the lining of the large intestine (colon) and rectum become inflamed. Pancolitis is a chronic or long lasting disease that causes inflammation—irritation or swelling—and sores called ulcers on the inner lining of the large intestine. Damaged areas are continuous (not patchy) – usually starting at the rectum and spreading further into the colon. Inflammation is present only in the innermost layer of the lining of the colon.
Pancolitis ulcerative colitis is a chronic inflammatory disease of the gastrointestinal (GI) tract, called inflammatory bowel disease (IBD). Another type of inflammatory bowel disease is Crohn disease, which also causes chronic inflammation of the intestines. Unlike pancolitis, which affects only the inner surface of the large intestine, Crohn disease can cause inflammation in any part of the digestive system, and the inflammation extends deeper into the intestinal tissue.
Pancolitis most often begins gradually and can become worse over time. Symptoms can be mild to severe. Most people have periods of remission—times when symptoms disappear—that can last for weeks or years. The goal of care is to keep people in remission long term.
Most people with pancolitis receive care from a gastroenterologist, a doctor who specializes in digestive diseases.
What causes pancolitis?
The exact cause of pancolitis is unknown. Researchers believe the following factors may play a role in causing pancolitis:
- overactive intestinal immune system
- genes
- environment
Overactive intestinal immune system. Scientists believe one cause of pancolitis may be an abnormal immune reaction in the intestine. Normally, the immune system protects the body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. Researchers believe bacteria or viruses can mistakenly trigger the immune system to attack the inner lining of the large intestine. This immune system response causes the inflammation, leading to symptoms.
Genes. Ulcerative colitis sometimes runs in families. Research studies have shown that certain abnormal genes may appear in people with pancolitis. However, researchers have not been able to show a clear link between the abnormal genes and pancolitis.
Environment. Some studies suggest that certain things in the environment may increase the chance of a person getting pancolitis, although the overall chance is low. Nonsteroidal anti-inflammatory drugs 1, antibiotics 1 and oral contraceptives 2 may slightly increase the chance of developing pancolitis. A high-fat diet may also slightly increase the chance of getting pancolitis 3.
Some people believe eating certain foods, stress, or emotional distress can cause pancolitis. Emotional distress does not seem to cause pancolitis. A few studies suggest that stress may increase a person’s chance of having a flare-up of pancolitis. Also, some people may find that certain foods can trigger or worsen symptoms.
Who is more likely to develop pancolitis?
Ulcerative colitis can occur in people of any age. However, it is more likely to develop in people
- between the ages of 15 and 30 4
- older than 60 1
- who have a family member with inflammatory bowel disease (IBD)
- of Jewish descent
Pancolitis symptoms
The most common signs and symptoms of pancolitis are diarrhea with blood or pus and abdominal discomfort. Other signs and symptoms include:
- an urgent need to have a bowel movement
- feeling tired
- nausea or loss of appetite
- weight loss
- fever
- anemia—a condition in which the body has fewer red blood cells than normal
Less common symptoms include:
- joint pain or soreness
- eye irritation
- certain rashes
The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the intestine. When symptoms first appear,
- most people with pancolitis have mild to moderate symptoms
- about 10 percent of people can have severe symptoms, such as frequent, bloody bowel movements; fevers; and severe abdominal cramping 1.
Pancolitis complications
You have a higher risk for small bowel and colon cancer if you have pancolitis. At some point, your provider will recommend tests to screen for colon cancer.
More severe episodes that recur may cause the walls of the intestines to become thickened, leading to:
- Colon narrowing or blockage
- Episodes of severe bleeding
- Severe infections
- Sudden widening (dilation) of the large intestine within one to a few days
- Tears or holes (perforation) in the colon
- Anemia, low blood count
Problems absorbing nutrients may lead to:
- Thinning of the bones (osteoporosis)
- Problems maintaining a healthy weight
- Slow growth and development in children
- Anemia or low blood count
Less common problems that may occur include:
- Type of arthritis that affects the bones and joints at the base of the spine, where it connects with the pelvis (ankylosing spondylitis)
- Liver disease
- Tender, red bumps (nodules) under the skin, which may turn into skin ulcers
- Sores or swelling in the eye
Complications of pancolitis can include:
- rectal bleeding—when ulcers in the intestinal lining open and bleed. Rectal bleeding can cause anemia, which health care providers can treat with diet changes and iron supplements. People who have a large amount of bleeding in the intestine over a short period of time may require surgery to stop the bleeding. Severe bleeding is a rare complication of pancolitis.
- dehydration and malabsorbtion, which occur when the large intestine is unable to absorb fluids and nutrients because of diarrhea and inflammation. Some people may need IV fluids to replace lost nutrients and fluids.
- changes in bones. Some corticosteroid medications taken to treat pancolitis symptoms can cause:
- osteoporosis—the loss of bone
- osteopenia—low bone density
Health care providers will monitor people for bone loss and can recommend calcium and vitamin D supplements and medications to help prevent or slow bone loss.
- inflammation in other areas of the body. The immune system can trigger inflammation in the:
- joints
- eyes
- skin
- liver
Health care providers can treat inflammation by adjusting medications or prescribing new medications.
- Toxic megacolon—a serious complication that occurs when inflammation spreads to the deep tissue layers of the large intestine. The large intestine swells and stops working. Megacolon can be a life-threatening complication and most often requires surgery. Megacolon is a rare complication of pancolitis.
Pancolitis and colon cancer
People with pancolitis may be more likely to develop colon cancer when:
- pancolitis affects the entire colon
- a person has pancolitis for at least 8 years
- inflammation is ongoing
- people also have primary sclerosing cholangitis, a condition that affects the liver
- a person is male
People who receive ongoing treatment and remain in remission may reduce their chances of developing colon cancer.
People with pancolitis should talk with their health care provider about how often they should get screened for colon cancer. Screening can include colonoscopy with biopsies or a special dye spray called chromoendoscopy.
Health care providers may recommend colonoscopy every 1 to 3 years for people with pancolitis who have:
- the disease in one-third or more or of their colon
- had pancolitis for 8 years
Such screening does not reduce a person’s chances of developing colon cancer. Instead, screening can help diagnose cancer early and improve chances for recovery.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Pancolitis diagnosis
A health care provider diagnoses pancolitis with the following:
- medical and family history
- physical exam
- lab tests
- endoscopies of the large intestine
Your health care provider may perform a series of medical tests to rule out other bowel disorders, such as irritable bowel syndrome, Crohn’s disease, or celiac disease, that may cause symptoms similar to those of pancolitis.
Medical and Family History
Taking a medical and family history can help the health care provider diagnose pancolitis and understand a patient’s symptoms. Your health care provider will also ask the patient about current and past medical conditions and medications.
Physical Exam
A physical exam may help diagnose pancolitis. During a physical exam, a health care provider most often:
- checks for abdominal distension, or swelling
- listens to sounds within the abdomen using a stethoscope
- taps on the abdomen to check for tenderness and pain
Lab Tests
A health care provider may order lab tests to help diagnose pancolitis, including blood and stool tests.
Blood tests. A blood test involves drawing blood at a health care provider’s office or a lab. A lab technologist will analyze the blood sample. A health care provider may use blood tests to look for
- anemia
- inflammation or infection somewhere in the body
- markers that show ongoing inflammation
- low albumin, or protein—common in patients with severe pancolitis
Stool tests. A stool test is the analysis of a sample of stool. A health care provider will give the patient a container for catching and storing the stool at home. The patient returns the sample to the health care provider or to a lab. A lab technologist will analyze the stool sample. Health care providers commonly order stool tests to rule out other causes of GI diseases, such as infection.
Endoscopies of the Large Intestine
Endoscopies of the large intestine are the most accurate methods for diagnosing pancolitis and ruling out other possible conditions, such as Crohn’s disease, diverticular disease, or cancer. Endoscopies of the large intestine include
Colonoscopy. Colonoscopy is a test that uses a long, flexible, narrow tube with a light and tiny camera on one end, called a colonoscope or scope, to look inside the rectum and entire colon. In most cases, light anesthesia and pain medication help patients relax for the test. The medical staff will monitor a patient’s vital signs and try to make him or her as comfortable as possible. A nurse or technician places an intravenous (IV) needle in a vein in the patient’s arm or hand to give anesthesia.
For the test, the patient will lie on a table or stretcher while the gastroenterologist inserts a colonoscope into the patient’s anus and slowly guides it through the rectum and into the colon. The scope inflates the large intestine with air to give the gastroenterologist a better view. The camera sends a video image of the intestinal lining to a monitor, allowing the gastroenterologist to carefully examine the tissues lining the colon and rectum. The gastroenterologist may move the patient several times and adjust the scope for better viewing. Once the scope has reached the opening to the small intestine, the gastroenterologist slowly withdraws it and examines the lining of the colon and rectum again.
A colonoscopy can show irritated and swollen tissue, ulcers, and abnormal growths such as polyps—extra pieces of tissue that grow on the inner lining of the intestine. If the gastroenterologist suspects pancolitis, he or she will biopsy the patient’s colon and rectum. A biopsy is a procedure that involves taking small pieces of tissue for examination with a microscope.
A health care provider will give patients written bowel prep instructions to follow at home before the test. The health care provider will also give patients information about how to care for themselves following the procedure.
Flexible sigmoidoscopy. Flexible sigmoidoscopy is a test that uses a flexible, narrow tube with a light and tiny camera on one end, called a sigmoidoscope or scope, to look inside the rectum, the sigmoid colon, and sometimes the descending colon. In most cases, a patient does not need anesthesia.
For the test, the patient will lie on a table or stretcher while the health care provider inserts the sigmoidoscope into the patient’s anus and slowly guides it through the rectum, the sigmoid colon, and sometimes the descending colon. The scope inflates the large intestine with air to give the health care provider a better view. The camera sends a video image of the intestinal lining to a monitor, allowing the health care provider to examine the tissues lining the sigmoid colon and rectum. The health care provider may ask the patient to move several times and adjust the scope for better viewing. Once the scope reaches the end of the sigmoid colon, the health care provider slowly withdraws it while examining the lining of the colon and rectum again.
The health care provider will look for signs of bowel diseases and conditions such as irritated and swollen tissue, ulcers, and polyps.
If the health care provider suspects pancolitis, he or she will biopsy your colon and rectum.
A health care provider will give you written bowel prep instructions to follow at home before the test. Your health care provider will also give you information about how to care for yourself following the procedure.
Pancolitis treatment
A health care provider treats pancolitis with:
- medications
- surgery
Which treatment a person needs depends on the severity of the disease and the symptoms. Each person experiences pancolitis differently, so health care providers adjust treatments to improve the person’s symptoms and induce, or bring about, remission.
Medications
While no medication cures pancolitis, many can reduce symptoms. The goals of medication therapy are:
- inducing and maintaining remission
- improving the person’s quality of life
Many people with pancolitis require medication therapy indefinitely, unless they have their colon and rectum surgically removed.
Health care providers will prescribe the medications that best treat a person’s symptoms:
- aminosalicylates
- corticosteroids
- immunomodulators
- biologics, also called anti-TNF therapies
- other medications
Depending on the location of the symptoms in the colon, health care providers may recommend a person take medications by:
- enema, which involves flushing liquid medication into the rectum using a special wash bottle. The medication directly treats inflammation of the large intestine.
- rectal foam—a foamy substance the person puts into the rectum like an enema. The medication directly treats inflammation of the large intestine.
- suppository—a solid medication the person inserts into the rectum to dissolve. The intestinal lining absorbs the medication.
- mouth.
- IV (intravenous).
Aminosalicylates
Aminosalicylates are medications that contain 5-aminosalicyclic acid (5-ASA), which helps control inflammation. Health care providers typically use aminosalicylates to treat people with mild or moderate symptoms or help people stay in remission. Aminosalicylates can be prescribed as an oral medication or a topical medication—by enema or suppository. Combination therapy—oral and rectal—is most effective, even in people with extensive pancolitis 5. Aminosalicylates are generally well tolerated.
Aminosalicylates include:
- balsalazide
- mesalamine
- olsalazine
- sulfasalazine—a combination of sulfapyridine and 5-aminosalicyclic acid (5-ASA)
Some of the common side effects of aminosalicylates include:
- abdominal pain
- diarrhea
- headaches
- nausea
Health care providers may order routine blood tests for kidney function, as aminosalicylates can cause a rare allergic reaction in the kidneys.
Corticosteroids
Corticosteroids, also known as steroids, help reduce the activity of the immune system and decrease inflammation. Health care providers prescribe corticosteroids for people with more severe symptoms and people who do not respond to aminosalicylates. Health care providers do not typically prescribe corticosteroids for long-term use.
Corticosteroids are effective in bringing on remission; however, studies have not shown that the medications help maintain long-term remission. Corticosteroids include:
- budesonide
- hydrocortisone
- methylprednisone
- prednisone
Side effects of corticosteroids include:
- acne
- a higher chance of developing infections
- bone mass loss
- death of bone tissue
- high blood glucose
- high blood pressure
- mood swings
- weight gain
People who take budesonide may have fewer side effects than with other steroids.
Immunomodulators
Immunomodulators reduce immune system activity, resulting in less inflammation in the colon. These medications can take several weeks to 3 months to start working. Immunomodulators include:
- azathioprine
- 6-mercaptopurine, or 6-MP
Health care providers prescribe these medications for people who do not respond to 5-aminosalicyclic acid (5-ASA). People taking these medications may have the following side effects:
- abnormal liver tests
- feeling tired
- infection
- low white blood cell count, which can lead to a higher chance of infection
- nausea and vomiting
- pancreatitis
- slightly increased chance of lymphoma
- slightly increased chance of nonmelanoma skin cancers
Health care providers routinely test blood counts and liver function of people taking immunomodulators. People taking these medications should also have yearly skin cancer exams.
People should talk with their health care provider about the risks and benefits of immunomodulators.
Biologics
Biologics—including adalimumab, golimumab, and infliximab—are medications that target a protein made by the immune system called tumor necrosis factor (TNF). These medications decrease inflammation in the large intestine by neutralizing TNF. Anti-TNF therapies work quickly to bring on remission, especially in people who do not respond to other medications. Infliximab is given through an IV; adalimumab and golimumab are given by injection.
Health care providers will screen patients for tuberculosis and hepatitis B before starting treatment with anti-TNF medications.
Side effects of anti-TNF medications may include:
- a higher chance of developing infections—especially tuberculosis or fungal infection
- skin cancer—melanoma
- psoriasis
Doctors may treat patients with vedolizumab when they do not respond to or cannot tolerate other medicines. Vedolizumab works by blocking cells that cause inflammation.
Side effects of vedolizumab may include:
- infections—common cold, flu, bronchitis, throat infection, or sinus infection
- headache
- pain in the back, arms, legs, or joints
- skin rash or itching
Other medications
Other medications to treat symptoms or complications may include:
- acetaminophen for mild pain. People with pancolitis should avoid using ibuprofen, naproxen, and aspirin since these medications can make symptoms worse.
- antibiotics to prevent or treat infections.
- loperamide to help slow or stop diarrhea. In most cases, people only take this medication for short periods of time since it can increase the chance of developing megacolon. People should check with a health care provider before taking loperamide, because those with significantly active pancolitis should not take this medication 6.
- cyclosporine—health care providers prescribe this medication only for people with severe pancolitis because of the side effects. People should talk with their health care provider about the risks and benefits of cyclosporine.
Surgery
Some people will need surgery to treat their pancolitis when they have:
- colon cancer
- dysplasia, or precancerous cells in the colon
- complications that are life threatening, such as megacolon or bleeding
- no improvement in symptoms or condition despite treatment
- continued dependency on steroids
- side effects from medications that threaten their health
Removal of the entire colon, including the rectum, “cures” pancolitis. A surgeon performs the procedure at a hospital. A surgeon can perform two different types of surgery to remove a patient’s colon and treat pancolitis:
- proctocolectomy and ileostomy
- proctocolectomy and ileoanal reservoir
Full recovery from both operations may take 4 to 6 weeks.
The surgeon will recommend one of the operations based on a person’s symptoms, severity of disease, expectations, age, and lifestyle. Before making a decision, the person should get as much information as possible by talking with:
- health care providers
- enterostomal therapists, nurses who work with colon-surgery patients
- people who have had one of the surgeries
Patient-advocacy organizations can provide information about support groups and other resources.
Proctocolectomy and ileostomy
A proctocolectomy is surgery to remove a patient’s entire colon and rectum. An ileostomy is a stoma, or opening in the abdomen, that a surgeon creates from a part of the ileum—the last section of the small intestine. The surgeon brings the end of the ileum through an opening in the patient’s abdomen and attaches it to the skin, creating an opening outside of the patient’s body. The stoma most often is located in the lower part of the patient’s abdomen, just below the beltline.
A removable external collection pouch, called an ostomy pouch or ostomy appliance, connects to the stoma and collects intestinal contents outside the patient’s body. Intestinal contents pass through the stoma instead of passing through the anus. The stoma has no muscle, so it cannot control the flow of intestinal contents, and the flow occurs whenever peristalsis occurs. Peristalsis is the movement of the organ walls that propels food and liquid through the GI tract.
People who have this type of surgery will have the ileostomy for the rest of their lives.
Proctocolectomy and ileoanal reservoir
An ileoanal reservior is an internal pouch made from the patient’s ileum. This surgery is a common alternative to an ileostomy and does not have a permanent stoma. Ileoanal reservoir is also known as a J-pouch, a pelvic pouch, or an ileoanal pouch anastamosis. The ileoanal reservior connects the ileum to the anus. The surgeon preserves the outer muscles of the patient’s rectum during the proctocolectomy. Next, the surgeon creates the ileal pouch and attaches it to the end of the rectum. Waste is stored in the pouch and passes through the anus.
After surgery, bowel movements may be more frequent and watery than before the procedure. People may have fecal incontinence—the accidental passing of solid or liquid stool or mucus from the rectum. Medications can be used to control pouch function. Women may be infertile following the surgery.
Many people develop pouchitis in the ileoanal reservoir. Pouchitis is an irritation or inflammation of the lining of the ileoanal reservoir. A health care provider treats pouchitis with antibiotics. Rarely, pouchitis can become chronic and require long-term antibiotics or other medications.
Pancolitis diet
Researchers have not found that eating, diet, and nutrition play a role in causing pancolitis symptoms. Good nutrition is important in the management of pancolitis, however. Dietary changes can help reduce symptoms. A health care provider may recommend dietary changes such as:
- avoiding carbonated drinks
- avoiding popcorn, vegetable skins, nuts, and other high-fiber foods while a person has symptoms
- drinking more liquids
- eating smaller meals more often
- keeping a food diary to help identify troublesome foods
Health care providers may recommend nutritional supplements and vitamins for people who do not absorb enough nutrients.
To help ensure coordinated and safe care, people should discuss their use of complementary and alternative medical practices, including their use of dietary supplements and probiotics, with their health care provider.
Depending on a person’s symptoms or medications, a health care provider may recommend a specific diet, such as a:
- high-calorie diet
- lactose-free diet
- low-fat diet
- low-fiber diet
- low-salt diet
People should speak with a health care provider about specific dietary recommendations and changes.
Pancolitis prognosis
Symptoms are mild in about half of people with pancolitis. More severe symptoms are less likely to respond well to medicines.
Cure is only possible through complete removal of the large intestine.
The risk of colon cancer increases in each decade after pancolitis is diagnosed.
- Shanahan F. Ulcerative colitis. In: Hawkey CJ, Bosch J, Richter JE, Garcia-Tsao G, Chan FKL, eds. Textbook of Clinical Gastroenterology and Hepatology. 2nd ed. Oxford: Wiley-Blackwell; 2012:355–371[↩][↩][↩][↩]
- Ko Y, Butcher R, Leong RW. Epidemiological studies of migration and environmental risk factors in the inflammatory bowel diseases. World Journal of Gastroenterology. 2014;20(5):1238–1247[↩]
- Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. American Journal of Gastroenterology. 2011;106(4):563–573[↩]
- Inflammatory bowel disease (IBD). https://www.cdc.gov/ibd[↩]
- Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. American Journal of Gastroenterology. 2010;105(3):501–523.[↩]
- Walfish AE, Sachar DB. Ulcerative colitis. The Merck Manual website. www.merckmanuals.com . Updated December 2012. Accessed July 23, 2014[↩]