Contents
What is a panniculectomy
Panniculectomy is also called body-contouring surgery, is a surgery done to remove stretched out, excess fat and overhanging skin from your abdomen. This can occur after a person undergoes massive weight loss. The skin may hang down and cover your thighs and genitals. Surgery to remove this skin helps improve your health and appearance. Panniculectomy is not a cosmetic procedure, it is used to change the shape and form of the abdomen on patients with a large overhanging abdominal skin or pannus 1. The intention of the panniculectomy procedure is to remove the excess skin and fat that hangs over your thigh and causes difficulty in personal hygiene, walking, and other physical activities.
A panniculectomy must meet specific criteria to be medically necessary. The pannus must hang below the level of the pubis and be confirmed with photography 1. Patients must fail medical treatment of intertrigo for three months 1. Medical treatment includes good hygiene, topical antifungals, corticosteroids, and antibiotics. The role of panniculectomy is to restore normal function. Patients must maintain a stable weight for at least 6 months. After bariatric surgery, patients must maintain a stable weight for at least 18 months, including the most recent six months 1.
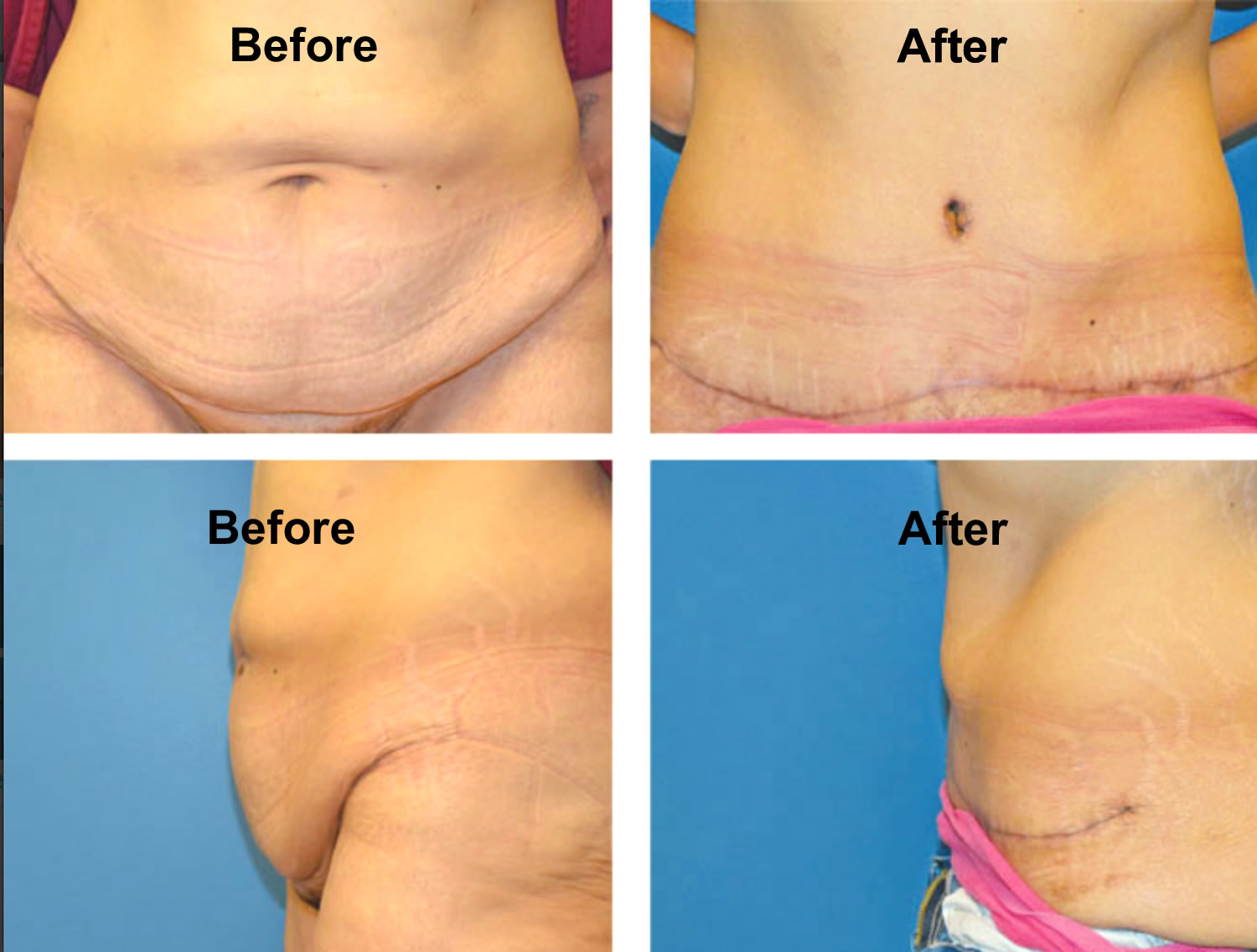
The outcome of panniculectomy is often good. Most people are happy with their new appearance.
An abdominal pannus is an apron of skin and fat that hangs down from your abdomen. The excess skin and fat is secondary to weight gain and can sometimes cover the anterior thighs, hips, and knees. A major issue is a large pannus can interfere with activities of daily life. Skin infections and rashes are common complaints of patients with a substantially large pannus due to constant irritation and sweating.
The abdominal pannus size varies from grade 1 to grade 5, which correlates with how far the pannus extends 1. Grade 1 reaches the mons pubis, while a grade 5 extends to or reaches past the knees 1. A panniculectomy is performed to relieve these symptoms and restore formal function. During a panniculectomy, the excess skin and fat are removed. Tightening or plication of the abdominal wall muscle is not performed. An abdominoplasty is a cosmetic procedure, usually involving fascial plication.
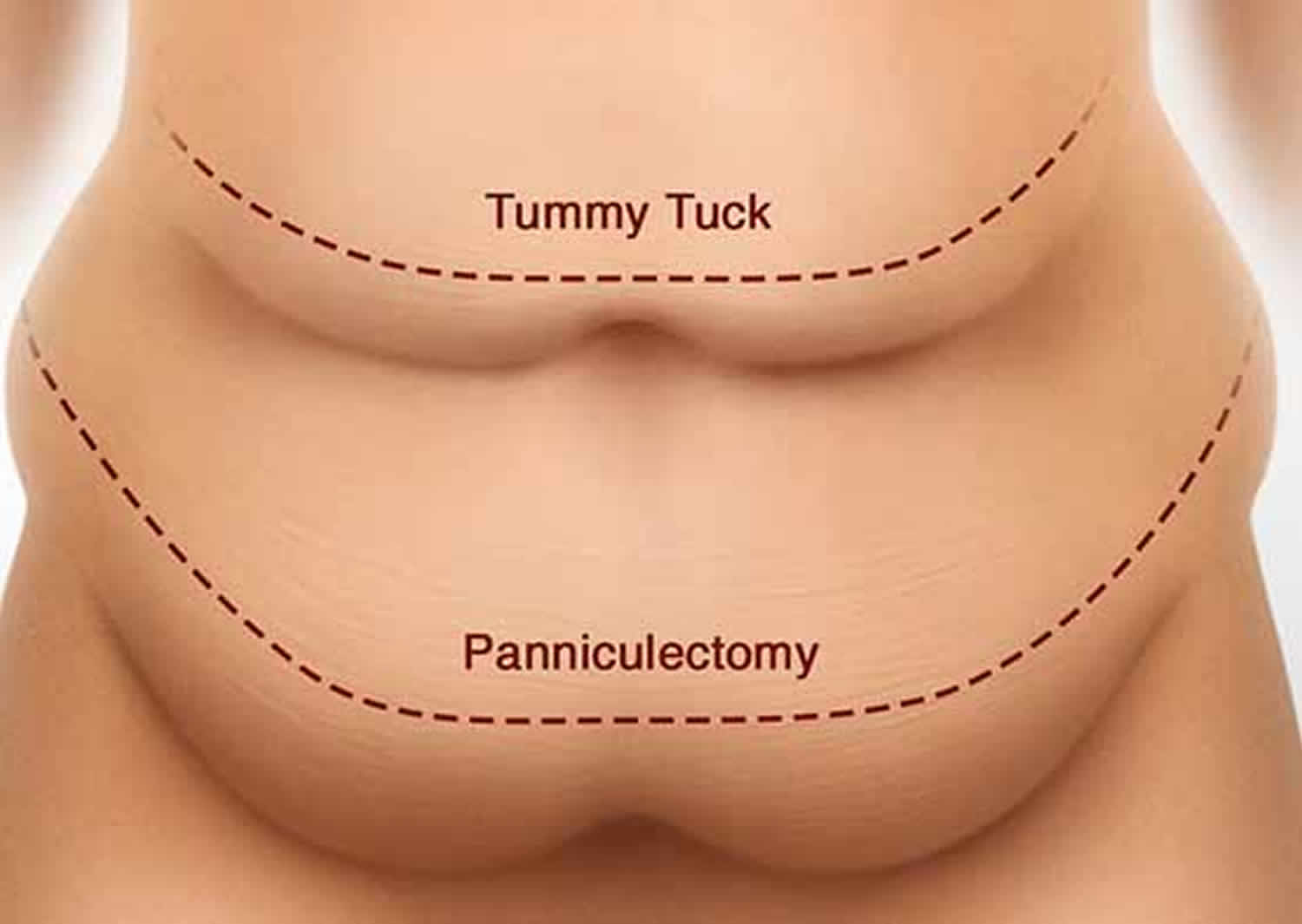
Panniculectomy is different from tummy tuck (abdominoplasty). In tummy tuck (abdominoplasty), your surgeon will remove extra fat and also tighten your abdominal (belly) muscles. Sometimes, both types of surgery are performed at the same time.
Abdominal fat anatomy
Men and women accumulate fat in distinct and predictable patterns. These patterns are genetically and hormonally related. The fat distribution in men is primarily around the abdomen and torso, which is an android pattern. Women accumulate fat around the hips and thighs in a gynoid pattern.
The fat present in cellulite is no different from ordinary subcutaneous fat. The subcutaneous fat in the trunk area is composed of a superficial and deep layer. The superficial layer is dense, compact, and contains multiple fibrous septa. The deep layer is loose, areolar, and contains few septa. The deep layers are located around the umbilical, gluteal, paralumbar, and medial thigh regions. One patient concern is the appearance of cellulite. This is due to the presence of dense vertical septa separating the fat into pockets. As the fat hypertrophies or the skin relaxes with age, the septa cause an accordion appearance of cellulite.
Fat cells are produced in utero, early childhood, and early adolescence. Once maturity is reached, the number of fat cells remains the same. When fat cells are removed through liposuction or other techniques, new fat cells do not form to replace them; however, the remaining fat cells may hypertrophy, causing the total fat mass in the area to increase. One exception is for patients who are morbidly obese, in these cases the fat cells become hyperplastic and multiply.
The primary blood supply to the abdominal skin is from the superior and inferior epigastric vessels. These vessels run within the rectus muscle and branch off perforating the rectus fascia and abdominal fat, finally reaching the skin. When performing an abdominal flap, the blood supply is interrupted.
A second blood supply to the abdominal skin is located in the fat superficial to the fascia of Scarpa. The lateral intercostal, subcostal, and lumbar vessel are the only blood supply of the central abdominal skin after flap elevation. Previous surgeries put the blood supply to the skin at risk because of interruptions of these vessels by scars.
The lower trunk has three horizontal zones of adherence in the inguinal region, suprapubic, and hip/lateral thighs. The tissue adherence becomes relaxed secondary to aging, pregnancy, and massive weight loss. Due to laxity of these attachments, the tissues descend around the pelvis and migrate centrally.
Panniculectomy procedure indications
Most often, when you experience a dramatic weight loss and the excess lower abdominal skin overhangs your groin and pubic regions. It is possible that it can strike against your thighs as you walk, causing significant discomfort and irritation. This extra skin can make it hard to keep yourself clean and to walk and perform daily activities. It also can cause rashes or sores. Clothing may not fit properly.
When you lose a lot of weight, such as 100 pounds (45 kg) or more after bariatric surgery, your skin may not be elastic enough to shrink back to its natural shape. This can cause the skin to sag and hang. It may cover your thighs and genitals.
Bariatric surgery patients typically achieve stable weight loss in 12 to 18 months, but some patients present in as few as 6 months for panniculectomy due to interference from the overhanging skin.
Panniculectomy is done to remove this extra abdominal skin (pannus). This can help you feel better about yourself and feel more confident in your appearance. Removing extra skin also may reduce your risk for rashes and infection.
Panniculectomy vs abdominoplasty
Abdominoplasty is an abdominal wall surgery, which is a procedure that improves the appearance of flabby, stretched-out abdominal (belly) muscles and skin. Abdominoplasty surgery is also called a tummy tuck. Abdominoplasty surgery can range from a simple mini-abdominoplasty to more extensive surgery. Abdominoplasty is able to eliminate excess skin and stubborn excess deposits of fat in the midsection. Abdominoplasty surgery can also repair abdominal muscle separation, known as diastasis recti. Abdominoplasty surgery can help you achieve a tighter, flatter, more fit appearance of the abdomen and flanks (love handles).
Most of the time, abdominoplasty surgery is an elective or cosmetic procedure because it is an operation you choose to have. Abdominoplasty surgery is not usually needed for health reasons. Cosmetic abdomen repair can help improve appearance, particularly after a lot of weight gain or loss. Abdominoplasty surgery helps flatten the lower abdomen and tighten stretched skin.
You might consider a abdominoplasty if:
- You have excess skin that’s accumulated around the area of your bellybutton
- You have a weak lower abdominal wall
- Liposuction didn’t adequately improve the appearance of your abdomen
- You previously had a C-section and have retracted scarring
If you’ve previously had a Caesarean section, your plastic surgeon might be able to incorporate your existing C-section scar into your abdominoplasty scar.
An abdominoplasty can also be done in combination with other body contouring cosmetic procedures, such as breast surgery.
The best candidates for an abdominoplasty have loose skin around their abdomen, as well as loose abdominal muscles (diastasis recti) or excess fatty deposits. Most frequently, abdominoplasty patients are women who have been pregnant, but the procedure can also benefit men or women who have lost a significant amount of weight that left them with baggy skin and an unflattering midsection. A consultation with a board certified plastic surgeon (American Board of Plastic Surgery) will help you better understand the results you can expect to see from an abdominoplasty surgery and whether you might be a good candidate
During an abdominoplasty surgery, the surgeon will make a cut in the fold under the belly. This is the “bikini line.” Skin is also cut around the belly button. A large area of fat and skin are then pulled away from the muscle.
Panniculectomy differs from standard abdominoplasty by the amount of skin and adipose tissue undermining superior to the tissue being excised, which is extremely limited for this procedure. The abdominal flaps with massive weight loss often demonstrate a compromised vascular status, and undermining is associated with a high rate of skin loss and seroma formation. The excision can almost be thought of as a wedge excision of the tissue to be removed. Previous scars must be carefully noted because these also predispose to tissue loss. If the tissue needed to be removed extends above the umbilicus, an umbilectomy is discussed with the patient as well.
Figure 1. Panniculectomy vs tummy tuck
Panniculectomy contraindications
Panniculectomy is an elective procedure where medical problems must be under control before the operation. Cigarette smoking affects blood supply and wound healing, and surgery should be avoided in active smokers and any patient with an uncontrolled cardiac disease, lung disease, or diabetes.
Patients with morbid obesity who are postbariatric have more severe deformities, excess skin, laxity, and poor tone. These patients are at greater risk of complications with medical comorbidities, surgical scars, and nutritional deficiencies.
Panniculectomy procedure
Before the panniculectomy procedure
Your surgeon will ask about your detailed medical history. The surgeon will examine the excess skin and old scars, if any. Tell your doctor about any prescription and over-the-counter medicines, herbs, or supplements you are taking.
Your doctor will ask you to quit smoking if you smoke. Smoking slows recovery and increases the risks of problems. Your doctor may suggest you quit smoking before having this surgery.
During the week before your surgery:
- Several days before surgery, you may be asked to stop taking medicines that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), warfarin (Coumadin), and others.
- Ask your doctor about medicines you should still take on the day of your surgery.
On the day of your panniculectomy surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
Note that panniculectomy is not always covered by health insurance. It is mostly a cosmetic procedure done to change your appearance. If it is done for a medical reason, such as hernia, your bills may be covered by your insurance company. Be sure to check with your insurance company before the surgery to find out about your benefits.
Panniculectomy surgery
Panniculectomy surgery will take place in a hospital or a surgery center. Panniculectomy surgery may take several hours.
- You will receive general anesthesia. This will keep you asleep and pain-free during the procedure.
- The surgeon may make a cut from under your breast bone to just above your pelvic bone.
- A horizontal cut is made in your lower belly, just above the pubic area.
- The surgeon will remove the overhanging extra skin and fat, called an apron or pannus.
- The surgeon will close your cut with sutures (stitches).
- Small tubes, called drains, may be inserted to allow fluid to drain out of the wound as the area heals. These will be removed later.
- A dressing will be placed over your abdomen.
An incision is made in the patient’s natural suprapubic crease. The incision is extended laterally towards the anterior superior iliac spine, stopping at the lateral edges of the pubic hair. The incision is deepened, and dissection is continued through the Scarpa fascia and down to the muscle. Following the musculoaponeurotic fascial plan superiorly, the abdominal skin and subcutaneous tissue are excised. The wound is closed in multiple layers with attention paid to the Scarpa fascia, deep dermis, and intradermal layers. Permanent or long-lasting absorbable sutures are used in these strength layers. When closing the wound, avoiding dog-ears on the lateral aspects is very important. Before the wound is closed, suction drains are placed under the flap and brought out through a small incision in the pubic region. To prevent seroma formation, compression garments should be worn while drains are present. Once the output of the drain is less than 30 mL/day, they can be removed, and compression garments can be continued for patient comfort.
Panniculectomy recovery
You will need to stay at hospital for about two days after the surgery. You may need to stay longer if your surgery is more complex.
After you recover from the anesthesia, you will be asked to get up to walk a few steps.
You will have pain and swelling for days after surgery. Your doctor will give you pain killers to help relieve the pain. You may also experience numbness, bruising, and tiredness during that time. It may help to rest with your legs and hips bent during recovery to reduce pressure on your abdomen.
Panniculectomy recovery time
After a day or so, your doctor may have you wear an elastic support, like a girdle, to provide extra support while you heal. You should avoid strenuous activity and anything that makes you strain for 4 to 6 weeks. You will probably be able to return to work in about 4 weeks.
It takes about 3 months for swelling to go down and wounds to heal. But it can take up to 2 years to see the final results of the surgery and for scars to fade.
Panniculectomy complications
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, or infection
Risks of panniculectomy surgery are:
- Scarring
- Infection
- Nerve damage
- Loose skin
- Skin loss
- Poor wound healing
- Fluid buildup under the skin
- Tissue death
Wound healing is the most common complication after a panniculectomy including cellulitis, seromas, hematomas, wound dehiscences, and tissue necrosis. Conservative management and wound care are usually the treatment of choice, but some patients require surgical intervention.
Seromas are the most common complication, especially after a larger dissection. Once a flap is created, the body tries to fill the empty space with fluid which is why suction drains are placed during the procedure. The best preventative management is the preservation of the Scarpa fascia with minimal dissection. Postoperatively, compression garments and reduction of activity can reduce seroma occurrence. Once a seroma occurs, management is observation and serial aspirations. Some patients require catheter insertions and sclerosing agents.
Simple cellulitis is a skin infection that will respond to antibiotics and follow-up. Complicated cellulitis with abscess formation will require surgical drainage and washout. When performing serial aspirations of seromas, there is a risk of introducing bacteria with each needle puncture, and the practitioner must weigh the risks versus the benefits. The patient will have a seroma and overlying cellulitis, fever, and drainage. Infected seromas require intravenous antibiotics and surgical drainage.
A hematoma is the accumulation of blood under the abdominal flap. Surgical drains placed during the operation do not prevent hematomas but allow the surgeon to track the amount and rate of postoperative bleeding. The drains evacuate the hematoma, and management is conservative. If the bleeding does not spontaneously stop or the hematoma is expanding, surgical drainage and obtaining hemostasis is required.
Wound dehiscence is the separation of a wound which can occur at any level down to the fascia. Postoperatively, patients are instructed to remain bent at the waist 30 degrees in semi-fowler position for a week and slowly return to the full upright position. The slow return to standing position allows the wound to form scar tissue and prevents the sutures that are holding the wound together from breaking. Patients should be instructed about careful ambulation during the first few weeks postoperatively.
Blood supply to the wound is key to wound healing. Vascular compromise can lead to tissue necrosis and wound breakdown. Risk factors include extensive lateral dissection, excessive liposuction, thin flap, and extreme tension. Once skin necrosis occurs, local wound care is the treatment to allow the wound to heal by secondary intention. After a scar forms, discussion about scar revision is an option.