Contents
What is pinguecula
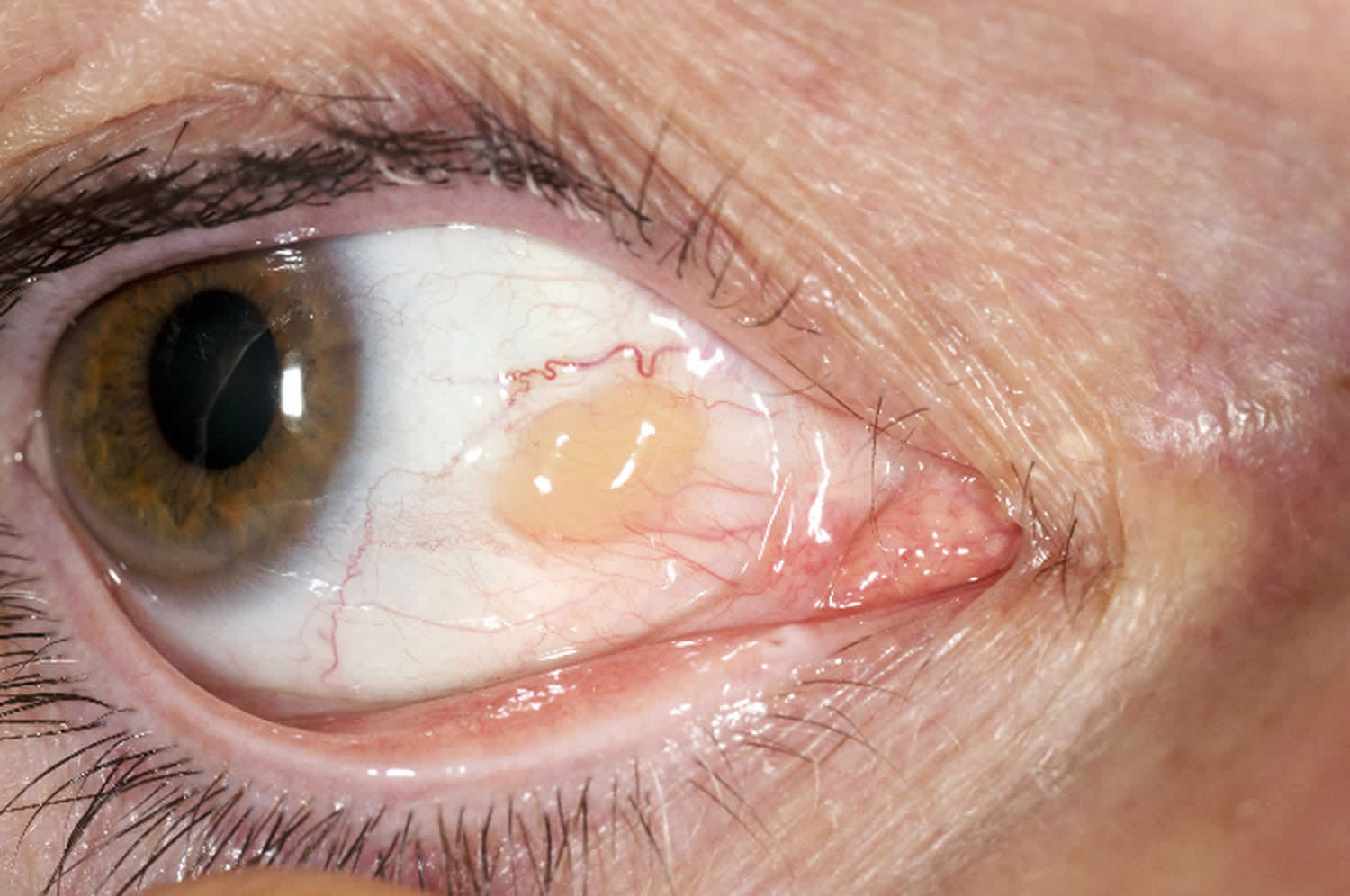
Pinguecula is a relatively common non-malignant, raised yellow-white spot or bump of the interpalpebral bulbar conjunctiva that does not involve the cornea (the clear area over the colored part of your eye) and represents elastoic degeneration of subepithelial collagen with hyalinized connective tissue 1. Pinguecula fleshy lesions are typically found bilaterally and adjacent to the limbus of the nasal bulbar conjunctiva although they can be present temporally as well.
Pinguecula is a growth that looks like a yellow spot or bump on the conjunctiva. It often appears on the side of the eye near your nose.
Figure 1. Pinguecula (a pinguecula is a deposit of protein, fat, or calcium that does not affect vision)
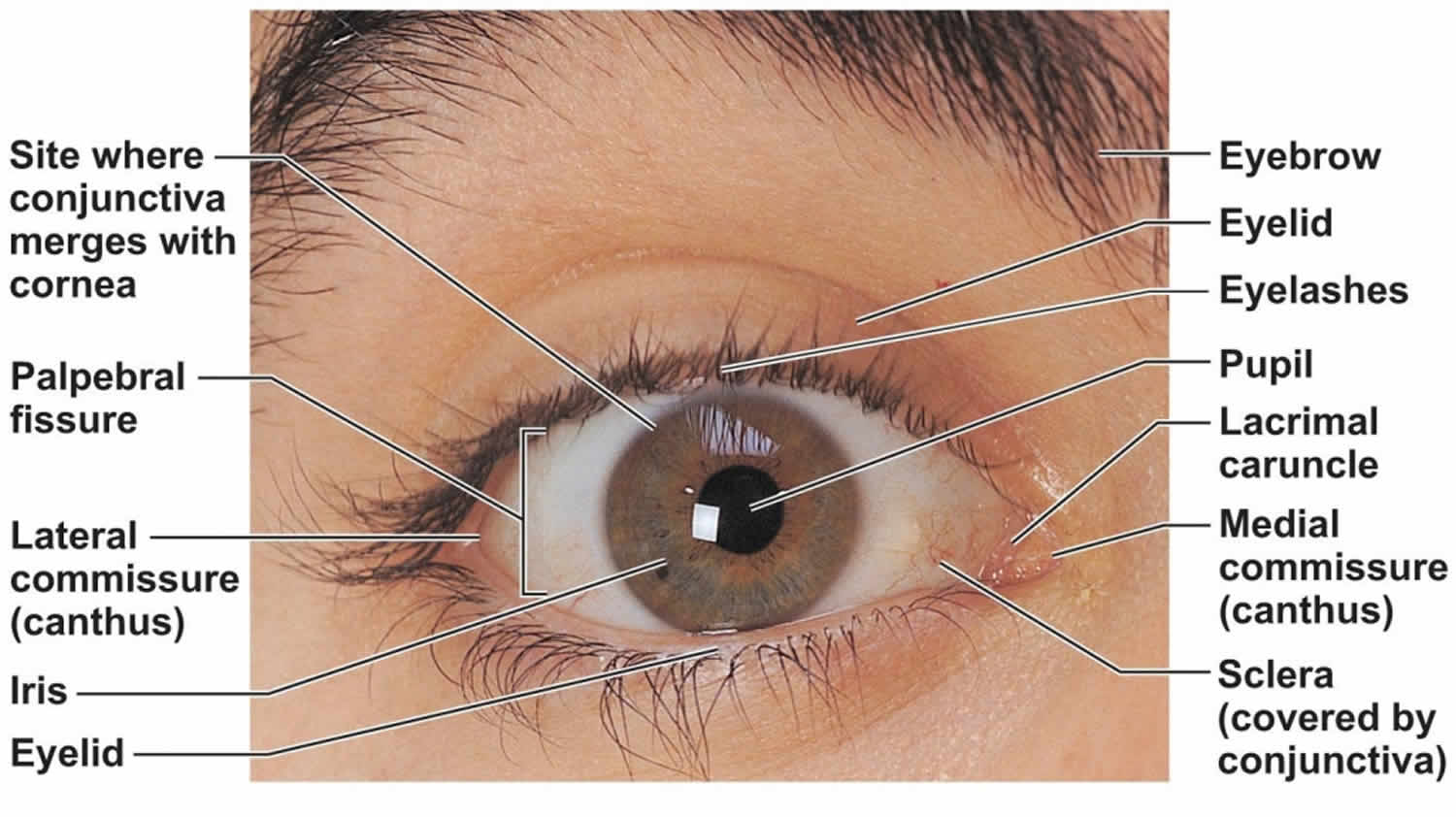
Figure 2. Human eye anatomy
Is it dangerous to leave a pinguecula untreated?
A pinguecula is a typically harmless growth on the white of the eye associated with UV light damage. Pinguecula usually has a yellowish appearance and can be slightly elevated from the surface of the eye. No treatment is necessary as long as it does not get red and irritated. In this case, you should visit an ophthalmologist to determine whether you need anti-inflammatory drops or surgical removal.
Does pinguecula go away?
No. Pinguecula eye may grow slowly over time but are associated with minimal ocular morbidity
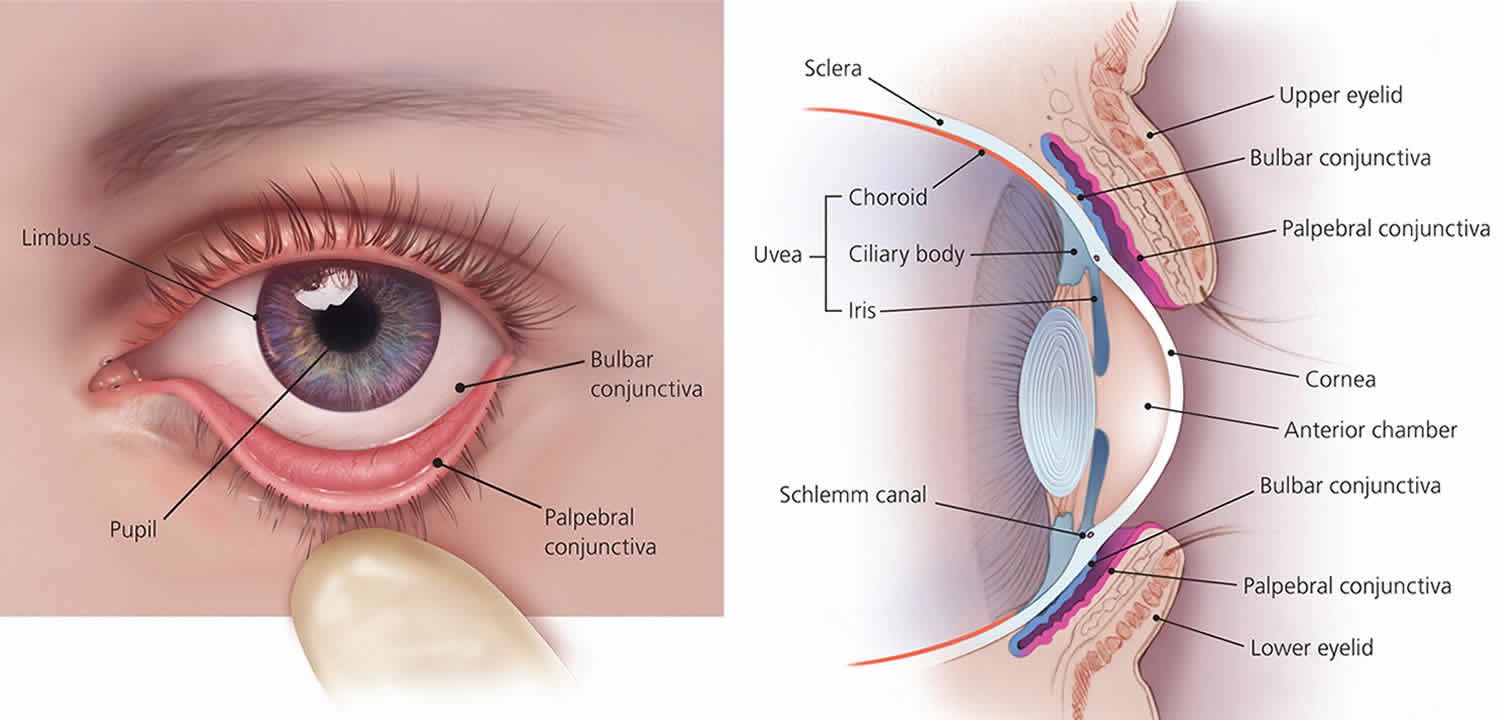
Pterygium vs Pinguecula
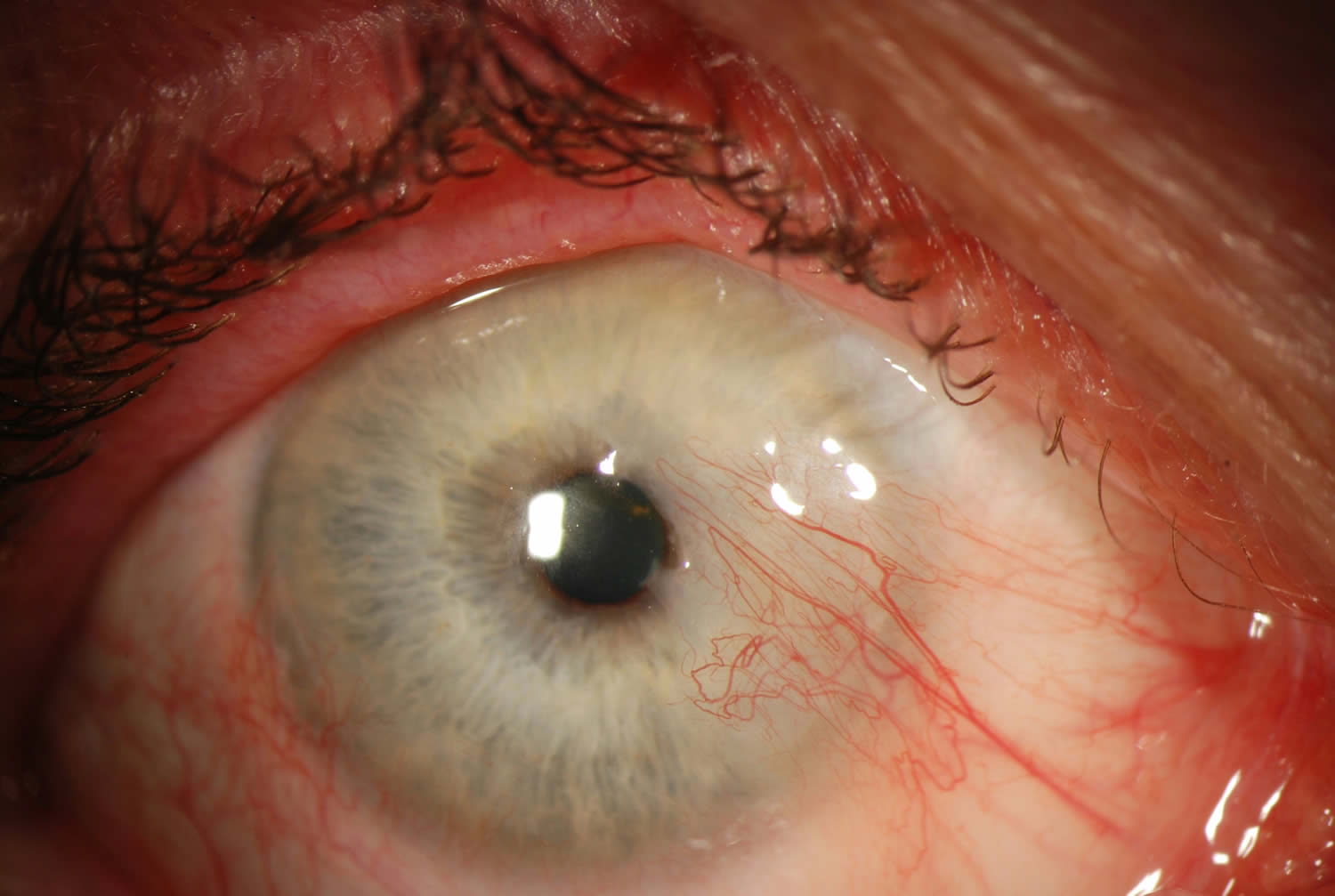
Pterygium sometimes called surfer’s eye, is a growth of fleshy tissue that may start as a pinguecula. It can remain small or grow large enough to cover part of the cornea. When this happens, it can affect your vision.
Both pinguecula and pterygium are believed to be caused by a combination of dry eyes and exposure to wind, dust, and ultraviolet (UV) light from the sun.
Since the conjunctival component of a pterygium is identical to a pinguecula, it has been claimed by some pathologists that the pterygium originates from a pinguecula.
Figure 3. Pterygium eye
Pterygium causes
It is not known exactly what causes a pterygium to develop, but dusty, sandy and sunny environments (with high UV exposure) are contributing factors. An increased incidence is noted in latitudes nearer the equator and in individuals with a history of increased UV exposure. Some studies have shown a slightly higher incidence in males than females, which may only reflect a higher rate of UV radiation.
The increased prevalence in hot dry climates and regions nearer to the equator suggest a role of environmental factors such as UV radiation and dryness. Actinic changes seen on histopathology similar to actinic keratoses on the skin also supports the role of UV radiation. It has been suggested that radiation activated fibroblasts may result in excessive production of material resulting in pterygia. Other proposed theories include choline deficiency, an inflammatory disorder, disregulation of angiogenesis, immune system abnormalities, tear film abnormalities, as well as the possible role of a viral stimulus.
Recurrent pterygia appear to be more related to surgical trauma than UV radiation as avoidance of UV radiation has not been shown to affect the incidence of recurrence. The actinic damage noted histologically on primary pterygia is characteristically absent from recurrent pterygia, supporting this theory.
Risk factors for developing pterygium
UV radiation, proximity to the equator, dry climates, outdoor lifestyle.
Pterygium symptoms
A pterygium can go unnoticed for many years, or it may be dismissed as a general irritation of the eye. As pterygium progresses, it can start to spread across the cornea. A pterygium can become inflamed and cause ocular surface irritation. Many patients will disclose their dislike of the appearance of the pterygium when questioned directly. As the lesion progresses vision may be affected by induction of astigmatism or obscuration of the visual axis.
Common symptoms include:
- Localized redness
- Irritation
- Itching
- Foreign-body sensation
- Corneal scarring
Some people with a pterygium may find it difficult to wear contact lenses, while others dislike the look of the growth on their eye and may seek surgical treatment to have it removed.
Pterygium diagnosis
The diagnosis is made by slit-lamp examination of the typical limbal growth at the characteristic location within the palpebral fissure. The diagnosis is most often clear clinically, but histopathologic confirmation is performed routinely.
The diagnosis of pterygium is based on the clinical appearance of the lesion. Typical findings include:
- Fibrovascular conjunctival growth within the palpebral fissure extending onto the corneal surface
- Triangular shape with the apex, or head, extending onto the cornea
- Vascular straightening in the direction of the advancing head of the pterygium on the corneal surface.
- May be a thin translucent membrane or significantly thickened with an elevated mound of gelatinous material.
- It may affect the nasal and temporal limbus of both eyes or only a single location.
- Raised lesion, white to pink in color depending on vascularity
- Ranges from a fine transparent area with very mild elevation, few vessels, and minimal corneal involvement in the early stages to a thick opaque vascular growth extending to the visual axis in later stages
- Pinguecula are often present in the ipsilateral or contralateral eye
- A pigmented epithelial iron line (Stocker’s line) adjacent to a pterygium is evidence of chronicity.
It is unusual for pterygia to deviate from the characteristic locations of three and nine o’clock within the palpebral fissure. Pterygioid lesions in other locations should elevate suspicion for alternate diagnoses.
A complete eye exam should be performed on all patients with apparent pterygia focusing on assessment of visual and refractive impact as well as the exclusion of less common alternate diagnoses.
- Visual acuity with current correction and manifest refraction
- External examination (lids, lashes, lacrimal apparatus)
- Examination of bulbar and palpebral conjunctiva as well as fornices
- Slit lamp biomicroscopy of the ocular surface and anterior segment
- Keratometry
- Corneal Topography
- Motility Exam
- The remainder of a comprehensive eye exam to include pupil exam, visual fields, intraocular pressure, and dilated funduscopic exam
Pterygium treatment
Initially, the corneal extension of the pterygium should be measured and followed every 1 to 2 years to determine the rate of growth toward the visual axis. In many cases, simple eye drops can be used to treat symptoms, such as inflammation, mild pain, itching or a feeling of having grit in the eye. Treatment for a minor irritation includes eye drops or ointments that help to lubricate and soothe the cornea. For severe inflammation, you may be prescribed a short course of steroid eye drops. These medications only ease the symptoms and are not a cure.
Pterygium surgery
If the pterygium growth is significant and continues to spread across the cornea or causes other problems, surgery is usually recommended to eliminate associated symptoms and avoid adverse effects on vision. Some people choose to have surgery for cosmetic reasons.
Excision: simple excision or simple conjunctival closure will result in a recurrence rate as high as 80% and is now considered unacceptable.
Excision together with adjunctive therapies such as radiotherapy, mitomycin and 5FU: the use of these adjunctive agents will reduce the 80% recurrence of simple excision to about 10% but bring with them some visually threatening complications. The only real advantage of these methods is the simplicity and speed of the surgery.
Conjunctival Flap/Graft : this is considered the Gold Standard of care and carries an approximate rate of recurrence of 5-10% with minimal complications. However, it is a lengthier procedure and technically slightly more complicated than those methods above. Recently a major modification of a routine autograft, known as P.E.R.F.E.C.T. for PTERYGIUM, has reduced the recurrence rate to 1/1000 and results in a cosmetic result where the appearance of the eye after this procedure is indistinguishable from that of a normal eye.
Pterygium surgical follow up
Intensive postoperative topical steroids may be required. Patients need to be followed for one year if a recurrence is to be identified. 97% of all recurrences occur in the first year after surgery.
Pinguecula causes
Pinguecula are thought to arise as a result of the effects of environmental irritants such as wind and dust and are associated with UV-light exposure and aging, however the evidence of the association between UV-light exposure and pinguecula remains limited 2. It is thought that both pteryigium and pinguecula arise more commonly on the nasal side because light passing medially through the cornea focuses on the area of the nasal limbus while the shadow of the nose reduces the intensity of light transmitted to the area of the temporal limbus 1.
Pinguecula prevention
Avoidance of UV-light exposure may decrease the incidence of pinguecula 3.
- When outdoors, wear good-quality, wrap-around sunglasses as recommended by an optometrist. Choose sunglasses that meet the American Standard and have an Eye Protection Factor (EPF) UV rating of either 9 or 10. The single most important thing to look for when buying sunglasses to protect your eyes is a sticker or tag indicating that they block 100 percent of UV rays. Less expensive pairs marked as 100 percent UV-blocking can be just as effective as pricier options.
- The more coverage from sunglasses, the less sun damage inflicted on the eyes. Consider buying oversized glasses or wraparound-style glasses, which help cut down on UV entering the eye from the side.
- Polarization reduces glare coming off reflective surfaces like water or pavement. This does not offer more protection from the sun, but can make activities like driving or being on the water safer or more enjoyable.
- Surfers and others involved in water sports should always wear sunglasses during these activities.
- A wide-brimmed hat will also protect your eyes from sun and wind exposure.
- Keep your eyes protected in dry, dusty conditions with wraparound glasses, goggles or other protective eyewear.
- Lubricate your eyes as often as possible in dry conditions by using artificial tears.
Pinguecula symptoms
Most pinguecula are asymptomatic but may cause ocular surface irritation including foreign body sensation, tearing, burning or itching. Some may find these lesions cosmetically unacceptable.
Pinguecula diagnosis
The diagnosis is usually made clinically by slit-lamp biomicroscopy. Pinguecula eye classic growth is raised and yellow-white in color, found in the interpalpebral fissure and is more common nasally than temporally. Pinguecula eye lesion may be highly vascularized and injected or associated with punctuate epithelial erosions or dellen (thinning of adjacent cornea due to drying) 4.
Diagnostic procedures
Biopsy with hisopathologic confirmation is not usually necessary but may be indicated for atypical cases where the diagnosis remains questionable.
Laboratory test
Not indicated
Pinguecula treatment
Lubrication with artificial tears and ointment can help with ocular surface irritation. Excision is indicated only when pinguecula are cosmetically unacceptable or when they become chronically inflamed or interfere with successful contact lens wear. Long-term use of topical steroid therapy should be discouraged due to adverse side-effects but can but used judiciously in patients with inflamed pingeucula termed “pingueculitis”. Topical indomethicin has also been demonstrated at reducing symptoms of inflammation 5.
Pinguecula surgery
Laser photocoagulation and surgical excision of pinguecula have both been used successfully with similar cosmetic outcomes 6.
- Weisenthal, Robert W, Afshari, Natalie A, Bouchard, Charles S, Colby, Kathyrn A, Rootman, David S, Tu, Elmer Y, 2013, External Disease and Cornea, AAO, BCSC, Chapter 12, Depositions and Degenerations.[↩][↩]
- Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2013 May: 14(2)187-94[↩]
- Bergmanson JP, Söderberg PG, The significance of ultraviolet radiation for eye diseases. A review with comments on the efficacy of UV-blocking contact lenses. Ophthalmic Physiol Opt. 1995 Mar;15(2):83-91 [↩]
- Ehlers, J.P, Shah, C.P, The Wills eye manual: office and emergency room diagnosis and treatment of eye disease. Lippincott Williams & Wilkins. 2008: (4.9) 66-67[↩]
- Frucht-Pery J, Solomon A, Siganos CS, Shvartzenberg T, Richard C, Trinquand C. Treatment of inflamed pterygium and pinguecula with topical indomethacin 0.1% solution. Cornea. 1997 Jan;16(1):42-7[↩]
- Ahn SJ, Shin KH, Kim MK, Wee WR, Kwon JW, One-year outcome of argon laser photocoagulation of pinguecula. Cornea. 2013 Jul;32(7):971-5[↩]