Contents
What is piriformis syndrome
Piriformis syndrome is a clinical condition of sciatic nerve entrapment at the level of the ischial tuberosity 1. While there are multiple factors potentially contributing to piriformis syndrome, the clinical presentation is fairly consistent, with patients often reporting pain in the gluteal/buttock region that may “shoot”, burn, or ache down the back of the leg (i.e. “sciatic”-like pain). In addition, numbness in the buttocks and tingling sensations along the distribution of the sciatic nerve is not uncommon.
Piriformis syndrome may be responsible for 0.3% to 6% of all cases of low back pain and/or sciatica 2. With an estimated amount of new cases of low back pain and sciatica at 40 million annually, the incidence of piriformis syndrome would be roughly 2.4 million per year. In the majority of cases, piriformis syndrome occurs in middle-aged patients with a reported ratio of male to female patients being affected 1:6 2.
Piriformis syndrome is often misdiagnosed and undertreated. Buttock pain is often confused with sciatica, sacroiliitis, lumbar radiculopathy, or trochanteric bursitis. The number of patients with piriformis syndrome has dramatically increased over time. The condition accounts for many cases of partial or total disability. When there is a delay in diagnosis, it leads to chronic pain, hyperesthesia, paresthesias, and muscle weakness.
Symptoms associated with piriformis syndrome occur from compression of the sciatic nerve by the piriformis muscle 2. Sciatic nerve entrapment occurs anterior to the piriformis muscle or posterior to the gemelli-obturator internus complex, which is in line with the anatomical location of the ischial tuberosity. Piriformis can be stressed due to poor body posture chronically or some acute injury that results in a sudden and strong internal rotation of the hip 3. The cause of compression and subsequent sciatic nerve irritation is variable. Piriformis syndrome can result from overuse or repetitive trauma where overtraining or sitting on hard surfaces that can cause direct or indirect injury to the piriformis muscle or sciatic nerve.
Athletes and weightlifters are prone to intermittent symptom exacerbation secondary to increased training requirements and activities. In these cases, the piriformis muscle itself becomes hypertrophied and causes direct pressure on the sciatic nerve 2.
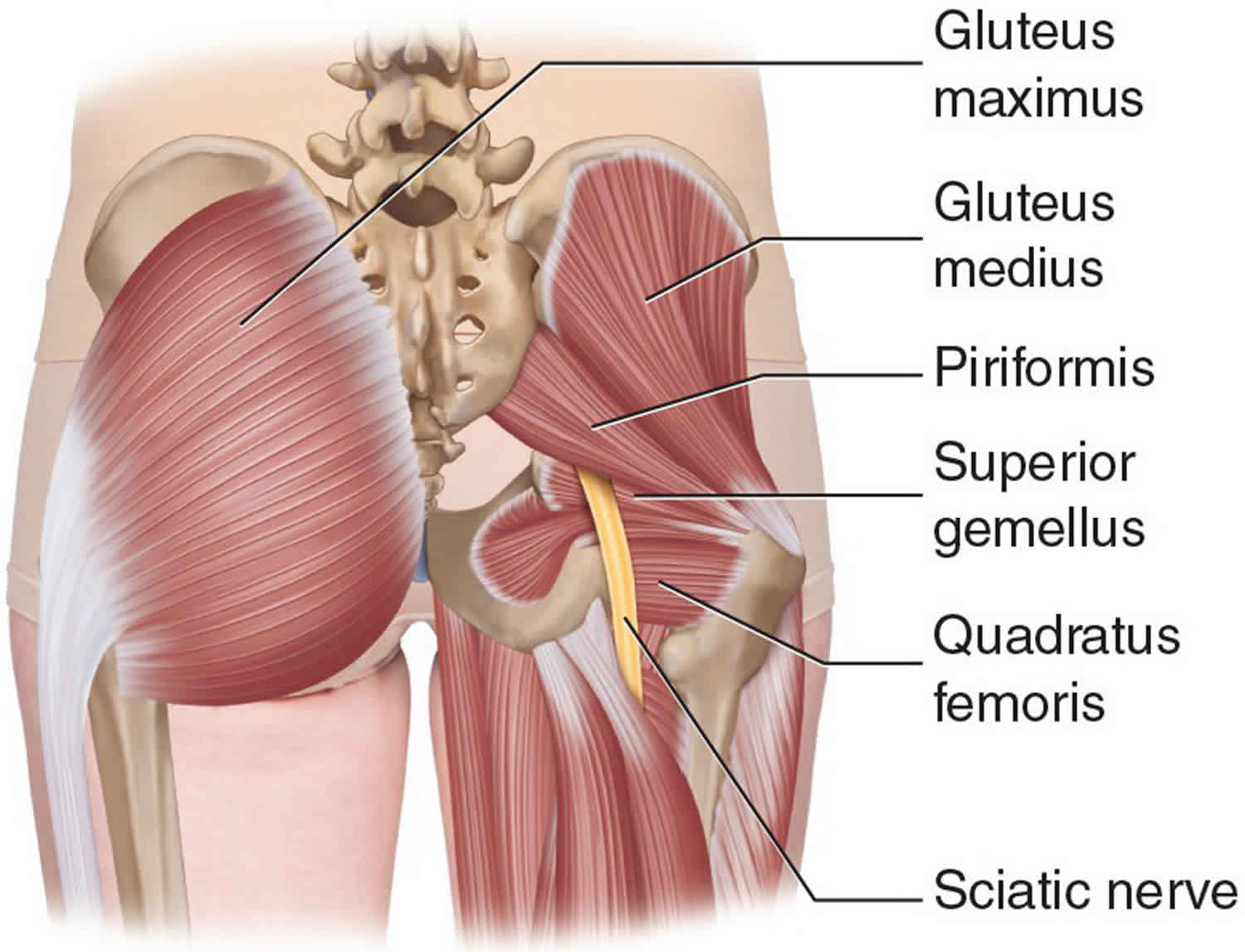
The piriformis muscle is an external (or lateral) rotator of the hip along with the superior and inferior gemellus, quadratus femoris, and obturator internus and externus 4. The piriformis muscle rotates the femur during extension of the hip and abducts the femur during flexion of the hip. The abduction of the femur is critical during walking as it shifts the body weight to the opposite side, which prevents one from falling. The piriformis muscle also serves as a landmark in the gluteal region. As it passes through the greater sciatic foramen, it divides it into a superior and inferior segment. This anatomy also helps name the nerves and vessels of the region. The superior gluteal nerve and artery exit superior to the piriformis. The inferior gluteal nerve and artery exit inferiorly. The sciatic nerve also travels inferior to the piriformis.
In at least a fifth of the population, the piriformis is pierced in different parts by the sciatic nerve. However, in some cases, it may be penetrated by the common peroneal nerve. In a few people, the muscle may integrate with the gluteus medius and minimus muscles. The piriformis may also have one or two attachments to the sacrum or capsule of the hip joint.
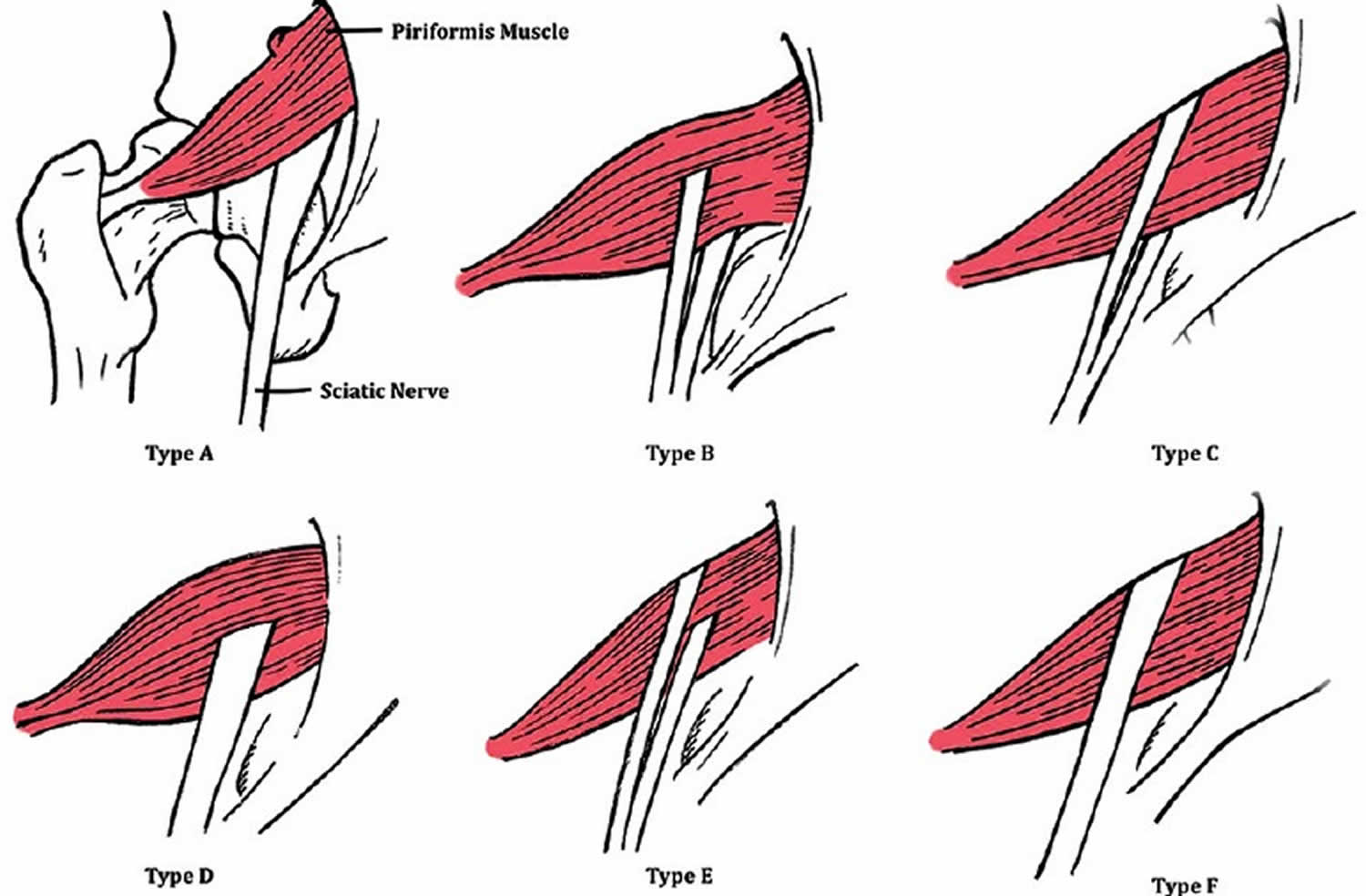
Acute trauma like blunt forces can also result in hematoma formation and subsequent scarring between the sciatic nerve and the short external rotators (piriformis, superior and inferior gemelli, quadratus femoris). Anomalous anatomic relationships of the sciatic nerve with the piriformis muscle have also been implicated where the sciatic nerve is more susceptible to compression because of the variant anatomy 2. Beaton and Anson 5 originally described 6 different anatomic relationships between the sciatic nerve and piriformis muscle. In >80% of the population, the sciatic nerve passes deep and exits inferiorly to the inferior edge of the muscle belly/tendon 6. Notable variations include early (proximal) divisions of the sciatic nerve into its tibial and common peroneal components, with these branches passing through and below the piriformis muscle or above and below the muscle. These anomalous sciatic nerve variants are all a potential cause of piriformis syndrome 7.
There have also been numerous case reports that show that other conditions have been associated with piriformis syndrome which includes pyomyositis, aberrant fibrous bands, myositis ossificans, and pseudoaneurysms 2.
Piriformis syndrome is associated with pain in the buttocks with sporadic, referred pain along the distribution of the sciatic nerve. Individuals in whom the sciatic nerve pierces the piriformis muscle are prone to sciatica. Sciatica will present with tingling, numbness, or pain deep in the buttock area and along the sciatic nerve. Prolonged sitting, climbing stairs, stretching, and performing squatting can also worsen the pain. The patient’s history and clinical exam make the diagnosis of piriformis syndrome. MRI and nerve conduction studies are done to exclude other pathologies. Once diagnosed, piriformis syndrome is treated with physical therapy and stretching exercises. Rarely, corticosteroids or botulinum toxin may be injected into the piriformis muscle. Surgery for nerve decompression is the last resort for the treatment of piriformis syndrome.
Most people who have piriformis syndrome get better with treatment and lifestyle changes. Failure to treat piriformis syndrome can lead to permanent sciatic nerve damage, so be sure to follow your doctor’s instructions.
Self-care tips for piriformis syndrome include the following:
- Temporarily stop doing activities that cause pain, such as running or bicycling.
- If you have to sit for a long period of time, take regular breaks to walk around and stretch.
- Use cold packs and warm packs. Start by using a cold pack on the affected area several times a day for about 15 minutes at a time. After using a cold pack for a couple of days, switch to a warm pack or heating pad. If you continue to have pain, alternate between a cold pack and a warm pack.
- Take a nonsteroidal anti-inflammatory drug (also called an NSAID), such as ibuprofen (two brand names: Advil, Motrin), aspirin or naproxen (one brand name: Aleve), to help relieve your pain. You can also take acetaminophen (brand name: Tylenol) for pain relief.
- Do exercises to stretch the piriformis muscle. Your doctor can give you information about what stretches will help.
- Massage the affected area.
If your pain doesn’t get better with self-treatment, your doctor may inject a steroid medicine where the piriformis muscle and the sciatic nerve meet. This may help reduce your pain.
You may find that piriformis syndrome comes and goes, depending on your activity level. Try to recognize those activities that seem to trigger it. That way, you can be sure to do exercises to stretch the piriformis muscles before and after those activities.
If you have severe piriformis syndrome, you may need surgery to relieve the pressure on your sciatic nerve.
Mild piriformis syndrome usually goes away over time. See your doctor if self-care measures fail to ease your symptoms or if your pain lasts longer than a week, is severe or becomes progressively worse. Get immediate medical care if:
- You have sudden, severe pain in your low back or your leg, and you have muscle weakness or numbness in your leg.
- The pain follows a violent injury, such as a traffic accident
- Your pain starts after you have been injured in a traumatic event.
- You have trouble controlling your bowels or bladder
- Your pain lasts longer than a few weeks.
Figure 1. Piriformis syndrome
Figure 2. Beaton and Anson classification between the sciatic nerve and piriformis muscle
Footnote: Six anatomic variations of the Beaton and Anson’s classification system demonstrated anatomic relationships between the sciatic nerve and piriformis muscle (posterior view). Illustrations are ordered from most common to least common, respectively, with the Type A being the most classic anatomical structure. Type B classification is the uncommon form.
[Source 8 ]Sciatic nerve anatomy
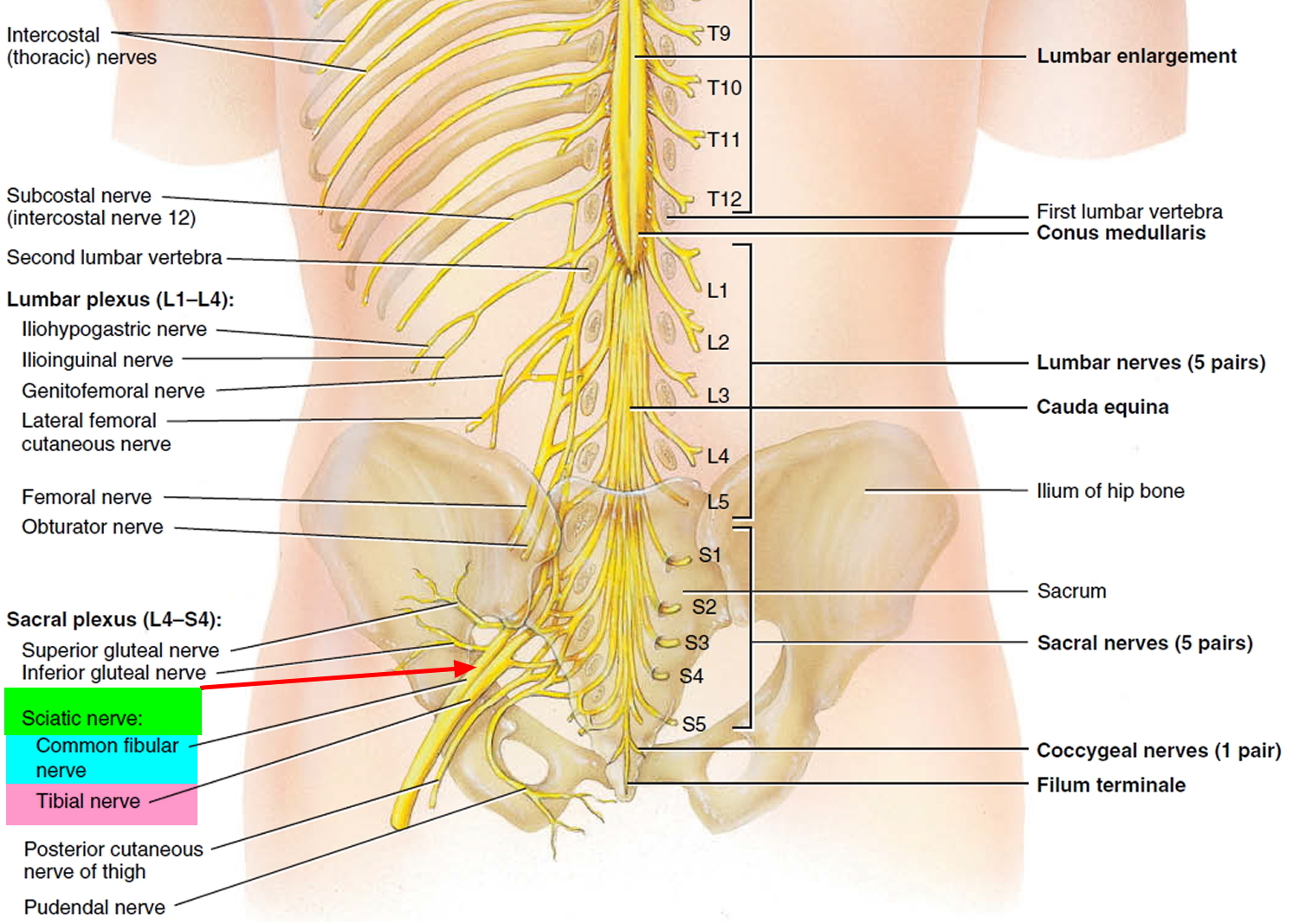
The sciatic nerve is the largest nerve in humans (size of a little finger), originating from the L4-S3 spinal column in the lower back and traveling posteriorly behind the hip joint, down the buttock and down the back of the leg to the lateral aspect of the foot. The sciatic nerve innervates a significant portion of the skin and muscles of the thigh, leg, and foot 9. The sciatic nerve is actually two nerves—tibial nerve and common fibular nerve — bound together by common sheath of connective tissue; splits into its two divisions, usually at the knee. As sciatic nerve descends through thigh, it sends branches to hamstring muscles and adductor magnus.
The nerve originates from the ventral rami of spinal nerves L4 through S3 and contains fibers from both the posterior and anterior divisions of the lumbosacral plexus. After leaving the lower vertebrae, the nerve fibers converge to form a single nerve. It exits the pelvis through the greater sciatic foramen inferior to the piriformis muscle along with the pudendal nerve and vessels, inferior gluteal nerve and vessels, nerve to obturator internus, and posterior cutaneous nerve. The sciatic nerve then progresses down the posterior compartment of the thigh deep to the long head of the biceps femoris muscle, superficial to adductor magnus and short head of biceps femoris muscle, and laterally to semitendinosus and semimembranosus muscles. Just before reaching the popliteal fossa, it divides into 2 important branches. One branch is the tibial nerve, which continues to descend in the posterior compartment of leg and foot. The other branch is the common peroneal nerve, which travels down the lateral and anterior compartment of the leg and foot.
The sciatic nerve runs just adjacent to the piriformis muscle, which functions as an external rotator of the hip 1. Hence, whenever the piriformis muscle is irritated or inflamed, it also affects the sciatic nerve, which then results in sciatica-like pain. The diagnosis of piriformis syndrome is not easy and is based on the clinical history and presentation. Other conditions that can also mimic the symptoms of piriformis syndrome include lumbar canal stenosis, disc inflammation, or pelvic causes 10.
The sciatic nerve provides motor innervation to the posterior compartment of the thigh 11. This includes the biceps femoris, semimembranosus, semitendinosus, and the ischial portion of the adductor magnus which allow for knee flexion and hip adduction. The tibial nerve innervates the posterior compartment of the leg and foot which includes the gastrocnemius, soleus, plantaris, popliteus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior. These muscles are primarily responsible for plantarflexion and flexion of the toes. The common peroneal nerve innervates the anterior and lateral compartments of the leg and foot. The anterior compartment includes tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius. These muscles are primarily responsible for dorsiflexion of the foot and extension of toes. The lateral compartment includes peroneus longus and brevis, which are responsible for foot eversion 10.
The sciatic nerve also provides sensory innervation to the skin of the foot and the lower leg (except for the medial leg which is innervated by the saphenous nerve). The tibial nerve further divides into the medial and lateral plantar nerves, which are responsible for the sensation of the sole. The common peroneal nerve further divides into the superficial peroneal nerve and deep peroneal nerve. The superficial peroneal nerve provides sensory innervation to the lateral leg and dorsum of the foot. The deep peroneal nerve is responsible for sensation in between the first and second toes. The medial and lateral sural nerves are made up of collateral branches from both the tibial and common peroneal nerves and provide sensation to the calf and a small lateral portion of the foot.
Figure 3. Sciatic nerve
Figure 4. Sciatic nerve branches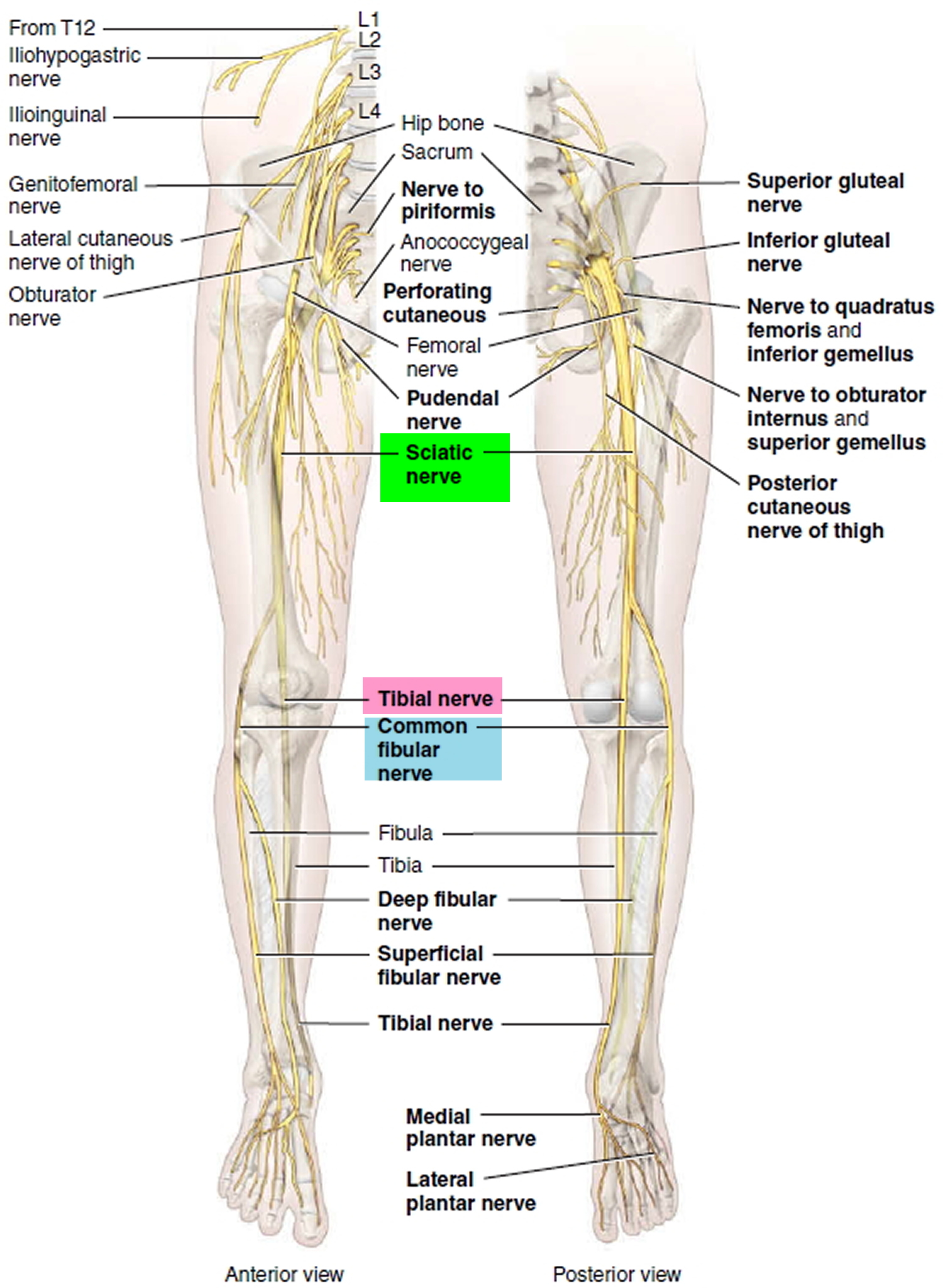
Piriformis syndrome causes
The piriformis muscle is involved in nearly every movement you make with your lower body, from walking to shifting weight from one foot to the other. Beneath the muscle is the sciatic nerve. This nerve runs from your lower spine down the back of your leg to your foot.
You can develop piriformis syndrome from everyday activities, such as sitting for long periods of time, climbing stairs, walking, or running. You can also develop it after a traumatic event, such as a car accident or a fall.
Injuring or irritating the piriformis muscle can cause muscle spasms.The muscle may also swell or tighten from the spasms. This puts pressure on the sciatic nerve beneath it, causing pain.
Overuse can irritate or injure the piriformis muscle. Muscle spasms may come from:
- Sitting for long periods
- Over exercising
- Running, walking, or doing other repetitive activities
- Playing sports
- Climbing stairs
- Lifting heavy objects
Trauma can also cause piriformis muscle irritation and damage. This may be caused by:
- Car accidents
- Falls
- Sudden twisting of the hip
- Penetrating wounds
Sciatic nerve entrapment occurs anterior to the piriformis muscle or posterior to the gemelli-obturator internus complex at the level of the ischial tuberosity 1. The piriformis can be stressed due to poor body mechanics in a chronic condition or an acute injury with the forceful internal rotation of the hip. There are also anatomic anomalies that may contribute to compression including a bipartite piriformis, direct invasion by a tumor, anatomical variations of the course of the sciatic nerve course, direct tumor invasion, or an inferior gluteal artery aneurysm that may compress the nerve.
Causes of piriformis syndrome include the following 12:
- Trauma to the hip or buttock area
- Piriformis muscle hypertrophy (often seen in athletes during periods of increased weightlifting requirements or pre-season conditioning)
- Sitting for prolonged periods (taxi drivers, office workers, bicycle riders)
- Anatomic anomalies:
- Bipartite piriformis muscle
- Sciatic nerve course/branching variations with respect to the piriformis muscle
- In >80% of the population, the sciatic nerve courses deep to and exits inferiorly to the piriformis muscle belly/tendon 13
- Early (proximal) divisions of the sciatic nerve into its tibial and common peroneal components can predispose patients to piriformis syndrome, with these branches passing through and below the piriformis muscle or above and below the muscle 14
Can piriformis syndrome be prevented or avoided?
Once your symptoms improve, you may need to change your activities to avoid developing piriformis syndrome again. The following are some tips to help prevent piriformis syndrome:
- Exercise regularly.
- Maintain good posture when you are sitting, driving or standing.
- Don’t lift by bending over. Lift an object by bending your knees and squatting to pick up the object. Keep your back straight and hold the object close to your body. Avoid twisting your body while lifting.
- Avoid sitting or lying down for long periods of time in a position that puts too much pressure on your buttocks.
- Use proper form and equipment when doing sports or other physical activities.
- Warm up and stretch before exercising. Then gradually increase the intensity of your activity.
- If something causes you pain, stop doing it. Don’t push through the pain. Rest until the pain passes.
Piriformis syndrome exercises to avoid
Avoid activities that cause pain, such as biking or running. Avoid running or exercising on hills or uneven surfaces. You can resume these activities after the pain is gone.
Piriformis syndrome symptoms
The symptoms of piriformis syndrome include pain deep in the buttock, and pain radiating down the back of the thigh.
Patients with piriformis syndrome will present with the following symptoms:
- Chronic pain in the buttock and hip area
- Pain when getting out of bed
- Inability to sit for a prolonged time
- Pain in the buttocks that is worsened by hip movements
- Tenderness or a dull ache in the buttock
- Tingling or numbness in the buttock and along the back of the leg
- Pain from sitting that grows worse as you continue to sit
- Pain that gets worse with activity
- Lower body pain that is so severe it becomes disabling
The pain usually affects just one side of the lower body. But it can also occur on both sides at the same time.
Patients will often present with symptoms of sciatica, and it can often be difficult to differentiate the origin of the radicular pain secondary to spinal stenosis versus the piriformis syndrome. The pain may radiate into the back of the thigh, but at times it may also occur in the lower leg at dermatomes L5 or S1 15.
Pain that radiates from your lower (lumbar) spine to your buttock and down the back of your leg is the hallmark of sciatica. You might feel the discomfort almost anywhere along the nerve pathway, but it’s especially likely to follow a path from your low back to your buttock and the back of your thigh and calf.
The pain can vary widely, from a mild ache to a sharp, burning sensation or excruciating pain. Sometimes it can feel like a jolt or electric shock. It can be worse when you cough or sneeze, and prolonged sitting can aggravate symptoms. Usually only one side of your body is affected.
Some people also have numbness, tingling or muscle weakness in the affected leg or foot. You might have pain in one part of your leg and numbness in another part.
The patient may also complain of buttock pain, and typically the palpation may reveal mild to moderate tenderness around the sciatic notch. By performing FAIR (flexion, adduction, and internal rotation), your health care provider may be able to reproduce the piriformis syndrome symptoms.
Piriformis syndrome diagnosis
Your doctor will perform a physical exam. He or she will move the affected leg into several different positions to check your pain level.
If your doctor thinks something other than piriformis syndrome is causing your sciatica, he or she may order additional tests. Computerized tomography (CT) and magnetic resonance imaging (MRI) scans cannot diagnose piriformis syndrome. However, they may show your doctor if something else is pressing on your sciatic nerve.
No definitive diagnostic criteria has been validated and established for piriformis syndrome. Piriformis syndrome remains a diagnosis of exclusion, but many of the following exam findings can aid the clinician in honing in on this diagnosis:
- Unilateral or bilateral buttock pain with fluctuating periods of pain throughout the day
- No lower back pain,
- No pain upon palpation of axial spine
- Negative results for straight leg raise
- Prolonged sitting triggering gluteal pain or sciatica
- Fluctuating sciatica through the course of the day
- Buttock pain near projection of the piriformis reproduced by FAIR (flexion, adduction, internal rotation) or Freiberg (forceful internal rotation of the extended thigh) sign or Beatty (deep buttock pain produced by the side-lying patient holding a flexed knee several inches off the table) sign, or palpitations
- The absence of perineal irradiation
- Sciatica reproduced by FAIR, Freiberg sign, or Beatty sign.
On physical examination, your doctor should try to perform stretching maneuvers to irritate the piriformis muscle. Furthermore, manual pressure around the sciatic nerve may help reproduce the symptoms.
These stretches include:
- Freiberg (forceful internal rotation of the extended thigh)
- Pace (resisted abduction and external rotation of the thigh)
- Beatty (deep buttock pain produced by the side-lying patient holding a flexed knee several inches off the table)
- FABER (flexion, abduction, external rotation)
- FAIR (flexion, adduction, internal rotation) maneuvers
Some of the disorders that also need to be ruled out include facet arthropathy, herniated nucleus pulposus, lumbar muscle strain, and spinal stenosis.
Diagnostic modalities such as ultrasound, MRI, CT, and EMG are mostly useful in excluding other conditions, as above.
- X-ray. An X-ray of your spine may reveal an overgrowth of bone (bone spur) that may be pressing on a nerve. Standard radiographs of the pelvis and hip should be done to rule out underlying hip pathology.
- MRI. This procedure uses a powerful magnet and radio waves to produce cross-sectional images of your back. An MRI produces detailed images of bone and soft tissues such as herniated disks. During the test, you lie on a table that moves into the MRI machine. MRI of the lumbar spine is also recommended to evaluate for a discogenic causes of lumbar radiculopathy and to rule out other sources of compression (e.g. soft tissue tumors or masses). MRI can also evaluate for spinal stenosis, herniated disks, facet arthrosis, SI joint pathology, occult pelvic fractures, and any surrounding tendinopathies or bursitides.
- CT scan. When a CT is used to image the spine, you may have a contrast dye injected into your spinal canal before the X-rays are taken — a procedure called a CT myelogram. The dye then circulates around your spinal cord and spinal nerves, which appear white on the scan.
- Electromyography (EMG). This test measures the electrical impulses produced by the nerves and the responses of your muscles. This test can confirm nerve compression caused by herniated disks or narrowing of your spinal canal (spinal stenosis). EMG is often normal in patients with acute piriformis syndrome presentations, however, chronically, EMG/nerve conduction study can be useful in identifying neuropathic changes and abnormal results in muscles innervated by the sciatic nerve 16.
The electrophysiologic approach has been used to diagnose piriformis syndrome by noting the presence of H waves. However, magnetic resonance neurography may show the presence of irritation of the sciatic nerve just adjacent to the sciatic notch. At this location, the sciatic nerve crosses just inferior to the piriformis muscle. Magnetic resonance neurography is not readily available in all clinics and is considered an experimental study. Private insurance may not reimburse the costs of the study 17.
Piriformis syndrome test
There are individual tests that stretch the piriformis and can be used to help aid in the diagnosis of exclusion. One of these is the Freiberg sign, which is performed by putting the hip in extension and internal rotation and having the patient externally rotate against resistance. The positive exam will reproduce pain around the piriformis. This test will have positive results in up to 63% of patients. Another individual test called the Pace sign is performed by resisting abduction and external rotation of the hip while the patient is in a seated position. Pace sign occurs in 30% to 74% in piriformis syndrome. FAIR test or also known as the piriformis stretch may elicit pain. Beatty sign has also been described and is accomplished by elevating the flexed leg on the irritated side while the patient lies on the asymptomatic side. Pain and reproduction of the symptoms are a positive test result.
The FAIR (flexion, adduction, and internal rotation) test is done by examining the patient in the supine position. Then one should ask the patient to flex the hip and move it along the midline. At the same time, the investigator should rotate the lower leg- this maneuver will apply tension to the piriformis muscle. At the same time, palpation will reveal tenderness over the muscle belly that stretches from the sacrum to the greater trochanter of the femur.
Piriformis syndrome treatment
Nonoperative treatment
Piriformis syndrome treatment includes short-term rest (not more than 48 hours), use of muscle relaxants, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy 1. Try ice and heat. Use an ice pack for 15 to 20 minutes every few hours. Wrap the ice pack in a towel to protect your skin. Alternate the cold pack with a heating pad on low setting. Don’t use a heating pad for longer than 20 minutes at a time.
In some patients, injection of steroids around the piriformis muscle may help decrease the inflammation and pain 18.
Anecdotal reports suggest that botulinum toxin may help relieve symptoms. However, the duration of pain relief is short-lived, and repeat injections are required 19.
Treatment for piriformis syndrome begins with nonoperative modalities including:
- Oral analgesics (e.g. NSAIDs, muscle relaxants, and gabapentin)
- Physical therapy:
- Regimens include nerve stretches, isometric exercises, gluteal muscle strengthening
- Injections
- Diagnostic and therapeutic modalities
- Agents used include cortisone, local anesthetic, or botulinum toxin
- A recent study reported positive outcomes in patients managed with physical therapy and Botulinum toxin injection
Piriformis syndrome exercises
Piriformis syndrome stretch
Piriformis syndrome surgery
Surgery is the last consideration in patients with piriformis syndrome after exhausting nonoperative modalities. Surgery should only be considered in patients who have failed conservative therapy including physical exercise. The surgery may help decompress the nerve if there is any impingement or the surgeon may lyse any adhesions or remove scars from the nerve. However, the results after surgery are not always predictable, and some patients continue to have pain 20.
A 2005 study reported surgical outcomes in 64 patients managed with surgical intervention for refractory symptoms 21:
- 82% reported initial improvement
- 76% had long-term positive outcomes
- 92% of those managed with surgery returned to work or presurgical baseline activity levels within 2 weeks of the surgery
Piriformis syndrome recovery time
Athletes with piriformis syndrome may return to activities when they can demonstrate the pain-free range of motion, increased strength of the affected side, and performance without any discomfort. Patients must stretch and warm-up before the activity. The time to return to exercise or sporting events depends on the severity of symptoms and the type of treatment undertaken. In general, the longer one does not seek medical care or physical therapy, the longer is the course of rehabilitation 22.
Patients with piriformis syndrome should adhere to the following:
- Avoid prolonged sitting
- Stretch exercises 2 to 3 times a day and before participating in sports
- The patient should be educated on a continual basis. Patients should be told about the importance of maintaining compliance if they want a positive outcome.
- In most cases, recurrent pain can be prevented by performing stretching exercises for at least 5 to 10 minutes prior to full participation and avoiding risk factors like prolonged seating.
Piriformis syndrome prognosis
Piriformis syndrome when not treated can be disabling and leads to a poor quality of life. However, when treated, the prognosis for most patients is excellent. Most people become symptom-free within 1-3 weeks after starting an exercise program, but unfortunately, relapse of symptoms is very common when compliance with exercise is low. The key is to avoid prolonged sitting. The role of surgery to manage piriformis syndrome remains debatable and is almost never the first choice treatment 23.
A number of patients with piriformis syndrome will show symptomatic improvement after local trigger-point injection. If this is combined with rehabilitation exercises, then recurrences are rare.
Individuals who undergo surgery for release of adhesions and scars may take a few months to return to full activity.
- Hicks BL, Varacallo M. Piriformis Syndrome. [Updated 2018 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172[↩][↩][↩][↩]
- Chang A, Varacallo M. Piriformis Injection. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448193[↩][↩][↩][↩][↩][↩]
- Huang ZF, Yang DS, Shi ZJ, Xiao J. [Pathogenesis of piriformis syndrome: a magnetic resonance imaging-based comparison study]. Zhonghua Yi Xue Za Zhi. 2018 Jan 02;98(1):42-45.[↩]
- Chang C, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Piriformis Muscle. [Updated 2018 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519497[↩]
- Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: A review. Clin Anat. 2010;23:8–17.[↩]
- Cassidy L, Walters A, Bubb K, Shoja MM, Tubbs RS, Loukas M. Piriformis syndrome: implications of anatomical variations, diagnostic techniques, and treatment options. Surg Radiol Anat. 2012 Aug;34(6):479-86.[↩]
- Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: a review. Clin Anat. 2010 Jan;23(1):8-17.[↩]
- Ro TH, Edmonds L. Diagnosis and Management of Piriformis Syndrome: A Rare Anatomic Variant Analyzed by Magnetic Resonance Imaging. J Clin Imaging Sci. 2018;8:6. Published 2018 Feb 21. doi:10.4103/jcis.JCIS_58_17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5843966/[↩]
- Ribeiro FS, Bettencourt Pires MA, Silva Junior EX, Casal D, Casanova-Martinez D, Pais D, Goyri-O’Neill JE. [Rethinking Sciatica In View of a Bilateral Anatomical Variation of the Sciatic Nerve, with Low Origin and High Division: Historical, Anatomical and Clinical Approach]. Acta Med Port. 2018 Oct 31;31(10):568-575.[↩]
- Siddiq MAB. Piriformis Syndrome and Wallet Neuritis: Are They the Same?. Cureus. 2018;10(5):e2606. Published 2018 May 10. doi:10.7759/cureus.2606 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039217/[↩][↩]
- Giuffre BA, Jeanmonod R. Anatomy, Sciatic Nerve. [Updated 2018 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482431[↩]
- Chang A, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 27, 2018. Piriformis Injection.[↩]
- Cassidy L, Walters A, Bubb K, Shoja MM, Tubbs RS, Loukas M. Piriformis syndrome: implications of anatomical variations, diagnostic techniques, and treatment options. Surg Radiol Anat. 2012 Aug;34(6):479-86[↩]
- Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: a review. Clin Anat. 2010 Jan;23(1):8-17[↩]
- Hopayian K, Danielyan A. Four symptoms define the piriformis syndrome: an updated systematic review of its clinical features. Eur J Orthop Surg Traumatol. 2018 Feb;28(2):155-164.[↩]
- Kraus E, Tenforde AS, Beaulieu CF, Ratliff J, Fredericson M. Piriformis Syndrome With Variant Sciatic Nerve Anatomy: A Case Report. PM R. 2016 Feb;8(2):176-9.[↩]
- Misirlioglu TO, Palamar D, Akgun K. Letter to the editor involving the article ‘Piriformis muscle syndrome: A cross-sectional imaging study in 116 patients and evaluation of therapeutic outcome’. Eur Radiol. 2018 Dec;28(12):5354-5355[↩]
- Ro TH, Edmonds L. Diagnosis and Management of Piriformis Syndrome: A Rare Anatomic Variant Analyzed by Magnetic Resonance Imaging. J Clin Imaging Sci. 2018;8:6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5843966/[↩]
- Safarpour Y, Jabbari B. Botulinum toxin treatment of pain syndromes -an evidence based review. Toxicon. 2018 Jun 01;147:120-128.[↩]
- Nazlıkul H, Ural FG, Öztürk GT, Öztürk ADT. Evaluation of neural therapy effect in patients with piriformis syndrome. J Back Musculoskelet Rehabil. 2018;31(6):1105-1110.[↩]
- Filler AG, Haynes J, Jordan SE, Prager J, Villablanca JP, Farahani K, McBride DQ, Tsuruda JS, Morisoli B, Batzdorf U, Johnson JP. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2005 Feb;2(2):99-115.[↩]
- Vassalou EE, Katonis P, Karantanas AH. Piriformis muscle syndrome: A cross-sectional imaging study in 116 patients and evaluation of therapeutic outcome. Eur Radiol. 2018 Feb;28(2):447-458.[↩]
- Kay J, de Sa D, Morrison L, Fejtek E, Simunovic N, Martin HD, Ayeni OR. Surgical Management of Deep Gluteal Syndrome Causing Sciatic Nerve Entrapment: A Systematic Review. Arthroscopy. 2017 Dec;33(12):2263-2278.e1[↩]