Contents
What is Propionibacterium acnes
Propionibacterium acnes recently renamed Cutibacterium acnes, is a Gram-positive, non-spore-forming human skin commensal (normal bacteria of the skin) that prefers anaerobic growth conditions 1. Propionibacterium acnes is a member of the normal skin microbiota along with Propionibacterium avidum, Propionibacterium granulosum, and Propionibacterium humerusii 2. Propionibacterium acnes has long been implicated in the pathophysiology of prostate cancer 3, sarcoidosis 4, infective endocarditis 5, infections involving prosthetic devices (such as prosthetic joints, central nervous system ventricular shunts, and cardiac implantable devices) 6, and acne 7. However, the severity of a person’s acne does not depend on the number of bacteria on the skin surface or in the sebaceous ducts (the passageway from the oil glands). The number and activity of Propionibacterium acnes bacteria varies according to oxygen supply, nutrient supply and the pH level of the skin. Some acne lesion are colonized by Propionibacterium acnes and others are not.
The Propionibacterium acnes genome is 2.5 Mb in size and has been completely sequenced 7. Propionibacterium acnes has genes encoding metabolic enzymes, enabling it to survive in microaerophilic conditions, but also lipases that degrade the lipids of the pilosebaceous follicle, providing the bacterium with the energy it needs 8. Recently, a taxonomic reclassification was proposed in which Propionibacterium acnes was renamed Cutibacterium acnes to account for genomic adaptive changes and to differentiate it from other Propionibacteria species. In particular, specific lipase genes were identified encoding for triacylglycerol lipase and lysophospholipase able to degrade sebum lipids 9. However, it has been proposed that it is taxonomically valid to continue to use the genus name Propionibacterium for the cutaneous group within dermatology specialties for a range of different reasons, including to avoid confusion with the previous name, Corynebacterium acnes 10.
The Propionibacterium acnes bacteria can produce active enzymes and innate inflammatory mediators and these may contribute to the activity of acne in some patients. Activation triggers expression of immune response genes. Inflammatory mediators detected in acne lesions colonised by Propionibacterium acnes include:
- Lipases (enzymes that break down fats)
- Proteases (enzymes that break down proteins)
- Hyaluronate lyase (enzyme that breaks down skin ground substance)
- Phosphatase (enzyme that breaks down phosphates)
- Smooth-muscle contracting substances
- Cytokines, such as IL-12 and IL-8, and defensins (these are chemical messengers).
The lipases can convert triglyceride in sebum to free fatty acids. The free fatty acids increase clumping of bacteria in sebaceous ducts and thus the colonization of the ducts by more of them. The inflammatory mediators provoked by the bacteria penetrate surrounding skin and are a cause of inflammation.
Propionibacterium acnes in acne
Propionibacterium acnes has been regarded as an important member of the cutaneous microbiota. Propionibacterium acnes has been linked to the inflammatory skin condition acne vulgaris for more than 100 years. The four major pathophysiological factors implicated in the pathogenesis of acne include the role of Propionibacterium acnes, increased seborrhea, hyperkeratinization of the pilosebaceous unit, and inflammation 11.
Propionibacterium acnes colonization of the skin is necessary but not sufficient for the establishment of acne pathology. Propionibacterium acnes dominates the microbiota of pilosebaceous units and accounts for 87% of clones in patients with acne and in individuals without acne 12. Propionibacterium acnes has been reported to represent more than 30% of the facial microbiota in patients with acne 13, but another study of 55 patients with facial acne reported lower rates (less than 2%) of sampled bacteria 14. These results should be interpreted with caution given the role of the sampling methodologies used. Different sampling methods, such as swab, scrape, cyanoacrylate gel biopsy, and needle biopsy, are used to collect skin bacteria for testing. Each technique targets different skin structures and anatomical sites. The sampling of superficial and intra-stratum corneum bacterial populations is considered quite straightforward. However, the sampling of hair follicle populations has proven more difficult and a skin biopsy may be required. The use of tape-stripping for hair follicle sampling in acne can be misleading, as multiple superficial and intra-stratum corneum microbial populations are sampled but bacteria may reside in a deeper part of the hair follicle 15. This area is inaccessible with the above-mentioned sampling methodologies, providing very little material from inside the hair follicle and making it difficult to standardize 2. Propionibacterium acnes sampling with bacterial culture may not reliably distinguish between Propionibacterium acnes populations with possibly variable pathogenic potential 16.
Although there is no quantitative difference of Propionibacterium acnes in the skin of patients with acne compared with controls 12, its phylogenic groups display distinct genetic and phenotypic characteristics in acne 9 and different phylotypes are known to induce distinct immune responses in acne 17. Different Propionibacterium acnes types have been isolated from acne vulgaris, and the type III strains have been associated with progressive macular hypomelanosis, underscoring the importance of genetic division of Propionibacterium acnes and suggesting the involvement of specific Propionibacterium acnes phylotypes in the pathophysiology of acne 18.
Focusing on acne, the typing of Propionibacterium acnes isolates has revealed distinct profiles in patients with acne ( Table 1) 19. A case-control study reported loss of Propionibacterium acnes phylotype diversity in patients with severe inflammatory acne, and there was a predominance of phylotype IA1 compared with healthy controls. With additional molecular typing methods, the single-locus sequence type (SLST) type A1 was predominant in the acne group 20. On the other hand, a small study in 29 patients with mild acne compared with 34 patients with severe acne did not reveal the association of a specific Propionibacterium acnes phylotype with the severity of acne, and phylotype IA1 and SLST type A1 were the predominant types in both groups 21.
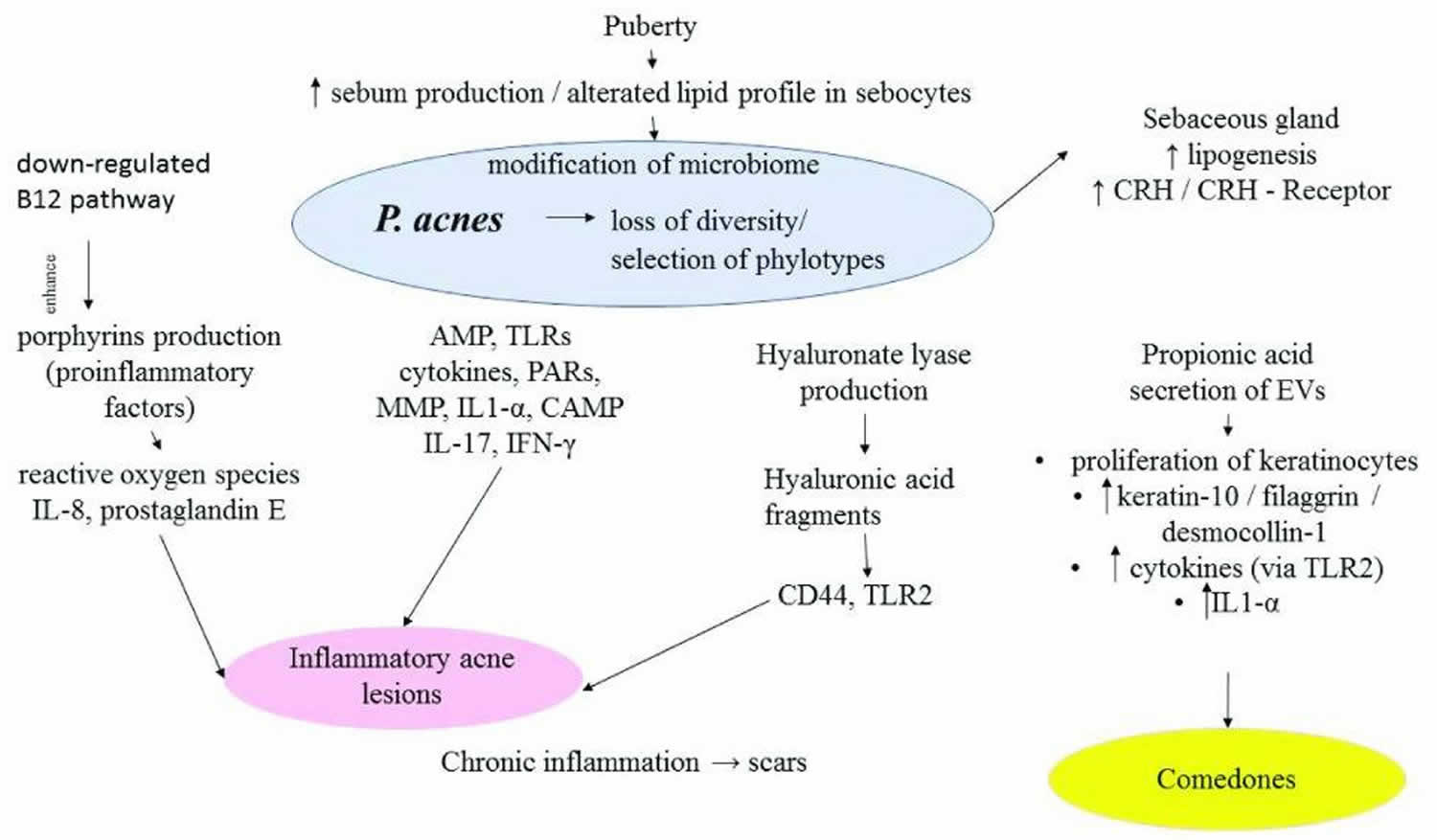
As Propionibacterium acnes modulates the differentiation of keratinocytes and increases local inflammation, it is regarded as an etiological agent of both the microcomedone (a structure invisible to the naked eye) in the early stages of acne and of the inflammatory acne lesions 22. The different target activities of Propionibacterium acnes in acne are summarized in Figure 1.
Table 1. The potential role of distinct Propionibacterium acnes types in patients with acne
| Study | Propionibacterium acnes phylotypes | Single-locus sequence type types | Acne patients studied | Proposed roles |
|---|---|---|---|---|
| Dagnelie et al. (2018) 20 | Predominance of phylotypes IA1 (84.4%) and II | A1 | 24 patients with severe acne of face and back versus 12 controls | – Decrease of phylotype diversity may be due to hyperseborrhea and qualitative sebum modifications in acne – Loss of diversity may activate innate immunity and trigger inflammatory acne |
| Nakase et al. (2017) 19 | – Isolates of clade A (60.3%) predominated – Strains of clade F more frequent in severe acne (40%) compared with mild acne (23.3%) – Phylogenetic type A5 most frequent (29.4%) | 113 patients with acne | ||
| Paugam et al. (2017) 21 | – Phylotype IA1 the most frequent in mild acne (55.2%) and in severe acne (67.6%) – No difference of phylotypes between mild and severe acne groups | A1 predominance with no difference between acne groups | 29 patients with mild acne and 34 patients with severe acne | – In a small number of patients, the severity of acne was not associated with a specific P. acnes group |
Figure 1. Propionibacterium acnes in acne
Footnote: Propionibacterium acnes induces the production of AMP, TLRs, cytokines, PARs, MMP, IL-1a, CAMP, hyaluronate lyase, and porphyrins, resulting in the formation of inflammatory acne lesions. It modulates the differentiation of keratinocytes by inducing keratin 10, filaggrin, and desmocollin 1 expression. It stimulates the sebaceous glands and sebum synthesis via the CRH/CRH receptor pathway.
Abbreviations: AMP = antimicrobial peptide; CAMP = Christie–Atkins–Munch-Peterson; CRH = corticotropin-releasing hormone; EV = extracellular vesicle; IFNγ = interferon-gamma; IL = interleukin; MMP = matrix metalloproteinase; PAR = protease-activated receptor; TLR = Toll-like receptor.
[Source 7 ]Propionibacterium acnes shows complex interactions with key events implicated in the pathogenesis of acne. It interacts with the innate immunity, including Toll-like receptors (TLRs), antimicrobial peptides (AMPs), protease-activated receptors (PARs), and matrix metalloproteinase (MMP), and upregulates the secretion of pro-inflammatory cytokines, including interleukin-1a (IL-1a), IL-1β, IL-6, IL-8, IL-12, tumor necrosis factor-alpha (TNF-α), and granulocyte-macrophage colony-stimulating factor (GM-CSF), by human keratinocytes, sebocytes, and macrophages 23. Moreover, the production of AMP (LL-37, β-defensin 2), cytokines (IL-1α), and MMP was associated with the increased expression of the G-protein-coupled receptor PAR-2 in keratinocytes from acne-affected skin 24. Propionibacterium acnes extracts are directly able to modulate the differentiation of keratinocytes by inducing b1, a3, a6s, aVb6 integrin expression, and filaggrin expression on keratinocytes, changes seen in the development of acne lesions 25. Interplay between Propionibacterium acnes and macrophages in the perifollicular dermis can induce IL-1β 32, which in turn may further activate the NLRP3-inflammasome pathway in antigen-presenting cells and myeloid cells 15. Recent in vitro studies have revealed that Propionibacterium acnes can induce IL-17 production by T cells (Th1/Th17) 23. Clusters of CD3 + cells have been demonstrated in the vicinity of the Propionibacterium acnes-positive comedones, cells that were absent from the surrounding inflamed lesions. These findings in early acne stage further support the role of Propionibacterium acnes in the initiation of inflammation 26. Propionibacterium acnes releases extracellular vesicles (EVs) which also induce cellular responses via TLR2 signal cascades. These Propionibacterium acnes-derived EVs induce IL-8 and GM-CSF and decrease epidermal keratin-10 and desmocollin, contributing to the development of acne lesions 27.
Yu et al. 17 showed that acne-associated Propionibacterium acnes phylotypes induced distinct cytokine patterns in vitro in peripheral blood mononuclear cells from healthy individuals, including higher levels of inflammatory interferon-gamma (IFN-γ) and IL-17, suggesting a mechanism of inducing acne via both Th1 and Th17 pathways. On the other hand, Propionibacterium acnes phylotypes associated with healthy skin induced higher levels of IL-10. Moreover, there were different expression patterns between phylotypes; acne-associated phylotypes showed higher expression of an adhesion protein, whereas phylotypes associated with healthy skin showed higher expression of a cell surface hydrolase. These identified immune responses and proteomes of different Propionibacterium acnes strains provided deeper insight into how specific Propionibacterium acnes phylotypes influence the pathogenesis of acne 17. In a follow-up study, Agak et al. 28 reported differential effects of acne-affected skin- and healthy skin-associated lineages of Propionibacterium acnes on CD4 + T-cell and Th17 cell responses and suggested that Propionibacterium acnes strains express different antigenic components on their surface structure, possibly explaining the higher IL-17 levels induced in acne-affected skin-associated Propionibacterium acnes strains.
Furthermore, Propionibacterium acnes has been implicated in lipogenesis and sebum production, as it stimulates the sebaceous glands and sebum synthesis via the corticotropin-releasing hormone (CRH)/CRH receptor pathway 29. Expression of the complete CRH system has been described in acne; a study in biopsies from the facial skin of patients with acne reported a stronger expression of CRH in sebocytes of acne-involved skin compared with non-involved and normal skin 30. In particular, CRH augments the synthesis of sebaceous lipids and induces IL-6 and IL-8 release by sebocytes, mediated by the CRH receptor 31.
A recent study reported that a secretory CAMP factor of Propionibacterium acnes has a role in its cytotoxicity, as mutations of CAMP diminished Propionibacterium acnes colonization and inflammation in mice 32. Propionibacterium acnes CAMP factor can induce cell death of sebocytes in sebaceous glands, resulting in amplification of the inflammation response 33. In addition, a study reported that the Propionibacterium acnes surface protein CAMP factor 1 stimulated keratinocytes in vitro by interacting directly with TLR2 34.
Porphyrins are secreted by Propionibacterium acnes and can generate reactive oxygen species that induce inflammation in keratinocytes and result in acne lesions. Johnson et al. 35 showed that acne-associated Propionibacterium acnes strains produced more porphyrins than health-associated strains isolated from individuals and that vitamin B 12 supplementation significantly increased porphyrin production in the acne-associated strains only. Another study showed that the Propionibacterium acnes vitamin B 12 biosynthesis pathway was downregulated in acne patients compared with healthy individuals. Furthermore, intramuscular vitamin B 12 supplementation repressed its own biosynthesis in Propionibacterium acnes and promoted increased porphyrin production in healthy subjects 36.
Hyaluronic acid (HA) lyase is a ubiquitous enzyme with two distinct variants in the Propionibacterium acnes population that differ in their ability to degrade HA and could be involved in the pro-inflammatory responses seen in acne. One variant is present in Propionibacterium acnes type IA strains and is associated with acne, and the other one is in type IB and II strains and is associated mainly with soft and deep tissue infections. HA fragments interact with cell surface receptors such as CD44 and TLR2 and induce the inflammatory response 37.
Apart from its target activities in acne, Propionibacterium acnes has an intriguing role in the homeostasis of the skin’s microbiome, interacting with other cutaneous microorganisms such as Staphylococcus epidermidis, Streptococcus pyogenes, and Pseudomonas species . In the microbiome of healthy skin, Staphylococcus epidermidis may limit the overcolonization with Propionibacterium acnes strains and reduce Propionibacterium acnes-induced IL-6 and TNF-α production by keratinocytes. On the other hand, Propionibacterium acnes may limit the proliferation of Staphylococcus aureus and Streptococcus pyogenes by promoting triglyceride hydrolysis and propionic acid secretion. As a result, an acidic pH is maintained in the pilosebaceous follicle. A change of the microbiome composition may lead to a disturbed skin barrier and inflammation. In acne, a modified profile of Propionibacterium acnes is noticed; different phylotypes differ between patients with and without acne 38. Hall et al. 39 showed in cutaneous samples that when Propionibacterium acnes was present, Pseudomonas species typically were not, and vice versa. Interestingly, antibiotic treatment for acne that decreases Propionibacterium acnes colonization on the skin may also result in Gram-negative folliculitis caused by Pseudomonas 40. Megyeri et al. recently proposed that Propionibacterium acnes strains may be implicated in antimicrobial defense pathways by triggering a local increase in the autophagic activity of keratinocytes 41.
Propionibacterium acnes symptoms
Propionibacterium acnes has long been implicated in the pathophysiology of prostate cancer 3, sarcoidosis 4, infective endocarditis 5, infections involving prosthetic devices (such as prosthetic joints, central nervous system ventricular shunts, and cardiac implantable devices) 6, and acne 7. However, the severity of a person’s acne does not depend on the number of bacteria on the skin surface or in the sebaceous ducts (the passageway from the oil glands). The number and activity of Propionibacterium acnes bacteria varies according to oxygen supply, nutrient supply and the pH level of the skin. Some acne lesion are colonized by Propionibacterium acnes and others are not.
Propionibacterium acnes treatment
Antimicrobials such as topical benzoyl peroxide and oral tetracyclines suppress Propionibacterium acnes in patients with acne. They also have non-antibiotic anti-inflammatory activity.
Mild acne
- Topical antiacne agents, such as benzoyl peroxide and/or tretinoin or adapalene gel. New bioactive proteins may also prove successful.
- Low-dose combined oral contraceptive
- Antiseptic or keratolytic washes containing salicylic acid
- Light / laser therapy
Moderate acne
- As for mild acne plus a tetracycline such as doxycycline 50–200 mg daily for 6 months or so
- Erythromycin or trimethoprim if doxycycline intolerant
- Antiandrogen therapy with long-term cyproterone acetate + ethinylestradiol and/or spironolactone, may be considered in women not responding to low-dose combined oral contraceptive, particularly for women with polycystic ovaries
- Isotretinoin is often used if acne is persistent or treatment resistant.
Severe acne
- Referral to a dermatologist
- If fever, arthralgia, bone pain, ulcerated or extensive skin lesions, blood count should be arranged and referral is urgent
- Oral antibiotics are often used in higher doses than normal
- Oral isotretinoin is usually recommended in suitable patients
- Thiboutot DM, Layton AM, Anne Eady E: IL-17: a key player in the P. acnes inflammatory cascade? J Invest Dermatol. 2014;134(2):307–10. 10.1038/jid.2013.400[↩]
- Omer H, McDowell A, Alexeyev OA: Understanding the role of Propionibacterium acnes in acne vulgaris: The critical importance of skin sampling methodologies. Clin Dermatol. 2017;35(2):118–29. 10.1016/j.clindermatol.2016.10.003[↩][↩]
- Davidsson S, Mölling P, Rider JR, et al. : Frequency and typing of Propionibacterium acnes in prostate tissue obtained from men with and without prostate cancer. Infect Agents Cancer. 2016;11:26. 10.1186/s13027-016-0074-9[↩][↩]
- Schupp JC, Tchaptchet S, Lützen N, et al. : Immune response to Propionibacterium acnes in patients with sarcoidosis– in vivo and in vitro. BMC Pulm Med. 2015;15:75. 10.1186/s12890-015-0070-7[↩][↩]
- Yamamoto R, Miyagawa S, Hagiya H, et al. : Silent Native-valve Endocarditis Caused by Propionibacterium acnes. Intern Med. 2018;57(16):2417–20. 10.2169/internalmedicine.9833-17[↩][↩]
- Achermann Y, Goldstein EJC, Coenye T, et al. : Propionibacterium acnes: from commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev. 2014;27(3):419–40. 10.1128/CMR.00092-13 [↩][↩]
- Platsidaki E, Dessinioti C. Recent advances in understanding Propionibacterium acnes ( Cutibacterium acnes) in acne. F1000Res. 2018;7:F1000 Faculty Rev-1953. Published 2018 Dec 19. doi:10.12688/f1000research.15659.1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305227[↩][↩][↩][↩][↩]
- Liu J, Cheng A, Bangayan NJ, et al. : Draft Genome Sequences of Propionibacterium acnes Type Strain ATCC6919 and Antibiotic-Resistant Strain HL411PA1. Genome Announc. 2014;2(4): pii: e00740-14. 10.1128/genomeA.00740-14[↩]
- Dréno B, Pécastaings S, Corvec S, et al. : Cutibacterium acnes ( Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol. 2018;32(Suppl 2):5–14. 10.1111/jdv.15043[↩][↩]
- Alexeyev OA, Dekio I, Layton AM, et al. : Why we continue to use the name Propionibacterium acnes. Br J Dermatol. 2018;179(5):1227. 10.1111/bjd.17085[↩]
- Dessinioti C, Katsambas AD: The role of Propionibacterium acnes in acne pathogenesis: facts and controversies. Clin Dermatol. 2010;28(1):2–7. 10.1016/j.clindermatol.2009.03.012[↩]
- Fitz-Gibbon S, Tomida S, Chiu BH, et al. : Propionibacterium acnes strain populations in the human skin microbiome associated with acne. J Invest Dermatol. 2013;133(9):2152–60. 10.1038/jid.2013.21[↩][↩]
- Grice EA, Kong HH, Conlan S, et al. : Topographical and temporal diversity of the human skin microbiome. Science. 2009;324(5931):1190–2. 10.1126/science.1171700[↩]
- Dreno B, Martin R, Moyal D, et al. : Skin microbiome and acne vulgaris: Staphylococcus, a new actor in acne. Exp Dermatol. 2017;26(9):798–803. 10.1111/exd.13296[↩]
- Alexeyev OA: Bacterial landscape of human skin: seeing the forest for the trees. Exp Dermatol. 2013;22(7):443–6. 10.1111/exd.12160[↩][↩]
- Jahns AC, Lundskog B, Ganceviciene R, et al. : An increased incidence of Propionibacterium acnes biofilms in acne vulgaris: a case-control study. Br J Dermatol. 2012;167(1):50–8. 10.1111/j.1365-2133.2012.10897.x[↩]
- Yu Y, Champer J, Agak GW, et al. : Different Propionibacterium acnes Phylotypes Induce Distinct Immune Responses and Express Unique Surface and Secreted Proteomes. J Invest Dermatol. 2016;136(11):2221–8. 10.1016/j.jid.2016.06.615[↩][↩][↩]
- Barnard E, Liu J, Yankova E, et al. : Strains of the Propionibacterium acnes type III lineage are associated with the skin condition progressive macular hypomelanosis. Sci Rep. 2016;6: 31968. 10.1038/srep31968[↩]
- Nakase K, Hayashi N, Akiyama Y, et al. : Antimicrobial susceptibility and phylogenetic analysis of Propionibacterium acnes isolated from acne patients in Japan between 2013 and 2015. J Dermatol. 2017;44(11):1248–54. 10.1111/1346-8138.13913[↩][↩]
- Dagnelie MA, Corvec S, Saint-Jean M, et al. : Decrease in Diversity of Propionibacterium acnes Phylotypes in Patients with Severe Acne on the Back. Acta Derm Venereol. 2018;98(2):262–7. 10.2340/00015555-2847[↩][↩]
- Paugam C, Corvec S, Saint-Jean M, et al. : Propionibacterium acnes phylotypes and acne severity: an observational prospective study. J Eur Acad Dermatol Venereol. 2017;31(9):e398–e399. 10.1111/jdv.14206[↩][↩]
- Isard O, Knol AC, Ariès MF, et al. : Propionibacterium acnes activates the IGF-1/IGF-1R system in the epidermis and induces keratinocyte proliferation. J Invest Dermatol. 2011;131(1):59–66. 10.1038/jid.2010.281[↩]
- Kistowska M, Gehrke S, Jankovic D, et al. : IL-1β drives inflammatory responses to propionibacterium acnes in vitro and in vivo. J Invest Dermatol. 2014;134(3):677–85. 10.1038/jid.2013.438[↩][↩]
- Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, et al. : Acne vulgaris. Nat Rev Dis Primers. 2015;1: 15029. 10.1038/nrdp.2015.29[↩]
- Jarrousse V, Castex-Rizzi N, Khammari A, et al. : Modulation of integrins and filaggrin expression by Propionibacterium acnes extracts on keratinocytes. Arch Dermatol Res. 2007;299(9):441–7. 10.1007/s00403-007-0774-5[↩]
- Alexeyev OA, Lundskog B, Ganceviciene R, et al. : Pattern of tissue invasion by Propionibacterium acnes in acne vulgaris. J Dermatol Sci. 2012;67(1):63–6. 10.1016/j.jdermsci.2012.03.004[↩]
- Choi EJ, Lee HG, Bae IH, et al. : Propionibacterium acnes-Derived Extracellular Vesicles Promote Acne-Like Phenotypes in Human Epidermis. J Invest Dermatol. 2018;138(6):1371–9. 10.1016/j.jid.2018.01.007[↩]
- Agak GW, Kao S, Ouyang K, et al. : Phenotype and Antimicrobial Activity of Th17 Cells Induced by Propionibacterium acnes Strains Associated with Healthy and Acne Skin. J Invest Dermatol. 2018;138(2):316–24. 10.1016/j.jid.2017.07.842[↩]
- Zouboulis CC: Propionibacterium acnes and sebaceous lipogenesis: a love-hate relationship? J Invest Dermatol. 2009;129(9):2093–6. 10.1038/jid.2009.190[↩]
- Ganceviciene R, Graziene V, Fimmel S, et al. : Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol. 2009;160(2):345–52. 10.1111/j.1365-2133.2008.08959.x[↩]
- Krause K, Schnitger A, Fimmel S, et al. : Corticotropin-releasing hormone skin signaling is receptor-mediated and is predominant in the sebaceous glands. Horm Metab Res. 2007;39(2):166–70. 10.1055/s-2007-961811[↩]
- Wang Y, Hata TR, Tong YL, et al. : The Anti-Inflammatory Activities of Propionibacterium acnes CAMP Factor-Targeted Acne Vaccines. J Invest Dermatol. 2018;138(11):2355–64. 10.1016/j.jid.2018.05.032[↩]
- Liu PF, Nakatsuji T, Zhu W, et al. : Passive immunoprotection targeting a secreted CAMP factor of Propionibacterium acnes as a novel immunotherapeutic for acne vulgaris. Vaccine. 2011;29(17):3230–8. 10.1016/j.vaccine.2011.02.036[↩]
- Lheure C, Grange PA, Ollagnier G, et al. : TLR-2 Recognizes Propionibacterium acnes CAMP Factor 1 from Highly Inflammatory Strains. PLoS One. 2016;11(11):e0167237. 10.1371/journal.pone.0167237[↩]
- Johnson T, Kang D, Barnard E, et al. : Strain-Level Differences in Porphyrin Production and Regulation in Propionibacterium acnes Elucidate Disease Associations. mSphere. 2016;1(1): pii: e00023-15. 10.1128/mSphere.00023-15[↩]
- Kang D, Shi B, Erfe MC, et al. : Vitamin B 12 modulates the transcriptome of the skin microbiota in acne pathogenesis. Sci Transl Med. 2015;7(293):293ra103. 10.1126/scitranslmed.aab2009[↩]
- Nazipi S, Stødkilde-Jørgensen K, Scavenius C, et al. : The Skin Bacterium Propionibacterium acnes Employs Two Variants of Hyaluronate Lyase with Distinct Properties. Microorganisms. 2017;5(3): pii: E57. 10.3390/microorganisms5030057[↩]
- Dréno B: What is new in the pathophysiology of acne, an overview. J Eur Acad Dermatol Venereol. 2017;31 Suppl 5:8–12. 10.1111/jdv.14374[↩]
- Hall JB, Cong Z, Imamura-Kawasawa Y, et al. : Isolation and Identification of the Follicular Microbiome: Implications for Acne Research. J Invest Dermatol. 2018;138(9):2033–40. 10.1016/j.jid.2018.02.038[↩]
- Böni R, Nehrhoff B: Treatment of gram-negative folliculitis in patients with acne. Am J Clin Dermatol. 2003;4(4):273–6. 10.2165/00128071-200304040-00005[↩]
- Megyeri K, Orosz L, Bolla S, et al. : Propionibacterium acnes Induces Autophagy in Keratinocytes: Involvement of Multiple Mechanisms. J Invest Dermatol. 2018;138(4):750–9. 10.1016/j.jid.2017.11.018[↩]