What is prosopagnosia
Prosopagnosia is a neurological disorder characterized by the inability to recognize the identity of faces 1. Prosopagnosia is also known as face blindness or facial agnosia. The term prosopagnosia comes from the Greek words for “face” and “lack of knowledge.” Subjects with prosopagnosia, cannot recognize that they have seen a face before, an impairment that affects both faces well known to them and those recently encountered. This is not due to more general problems with vision, object recognition, or memory. Depending upon the degree of impairment, some people with prosopagnosia may only have difficulty recognizing a familiar face; others will be unable to discriminate between unknown faces, while still others may not even be able to distinguish a face as being different from an object. Some people with prosopagnosia are unable to recognize their own face. Prosopagnosia is not related to memory dysfunction, memory loss, impaired vision, or learning disabilities. Prosopagnosia is thought to be the result of abnormalities, damage, or impairment in the right fusiform gyrus, a fold in the brain that appears to coordinate the neural systems that control facial perception and memory.
Prosopagnosia can be either acquired or developmental 1. In acquired prosopagnosia, poor face recognition is the result of brain injury. For example, prosopagnosia can result from stroke, traumatic brain injury, or certain neurodegenerative diseases. In some cases prosopagnosia is a congenital disorder (congenital prosopagnosia), present at birth in the absence of any brain damage.
While the first case of acquired prosopagnosia was reported 150 years ago 2, the modern study of prosopagnosia began with Bodamer’s report in 1947 3, which described impaired face recognition in wounded soldiers. Subsequently, it has been recognized that acquired prosopagnosia can arise from many different pathologies, including trauma, stroke, encephalitis, tumors, degenerative atrophy, or temporal lobe resections 4.
Congenital prosopagnosia (developmental prosopagnosia) has been more recently described and is less well understood. Subjects with congenital prosopagnosia fail to develop face recognition skills despite otherwise normal vision and memory, and do not have obvious lesions on brain imaging 5. Congenital prosopagnosia (developmental prosopagnosia) may have a genetic basis. It can run in families, with some pedigrees showing as many as ten affected members across two generations 6, observations that parallel findings that normal face recognition skills also have a heritable component, with monozygotic twins having more similar face recognition abilities than dizygotic twins 7. While the acquired prosopagnosia is rare, the congenital prosopagnosia may be relatively common. Some suggest that as many as 2.5% of the population has congenital prosopagnosia 8, although this number will vary with the statistical criteria used and may confound those subjects with a developmental problem with those on the low end of normal face recognition ability.
Prosopagnosia can be socially crippling. Individuals with prosopagnosia often have difficulty recognizing family members and close friends. They often use other ways to identify people, such as relying on voice, clothing, or unique physical attributes, but these are not as effective as recognizing a face. Children with congenital prosopagnosia are born with the disability and have never had a time when they could recognize faces. Adults with congenital prosopagnosia often report that their failure to recognize others creates traumatic social experiences, leading to chronic anxiety, feelings of embarrassment and guilt, and a limited social circle 9.
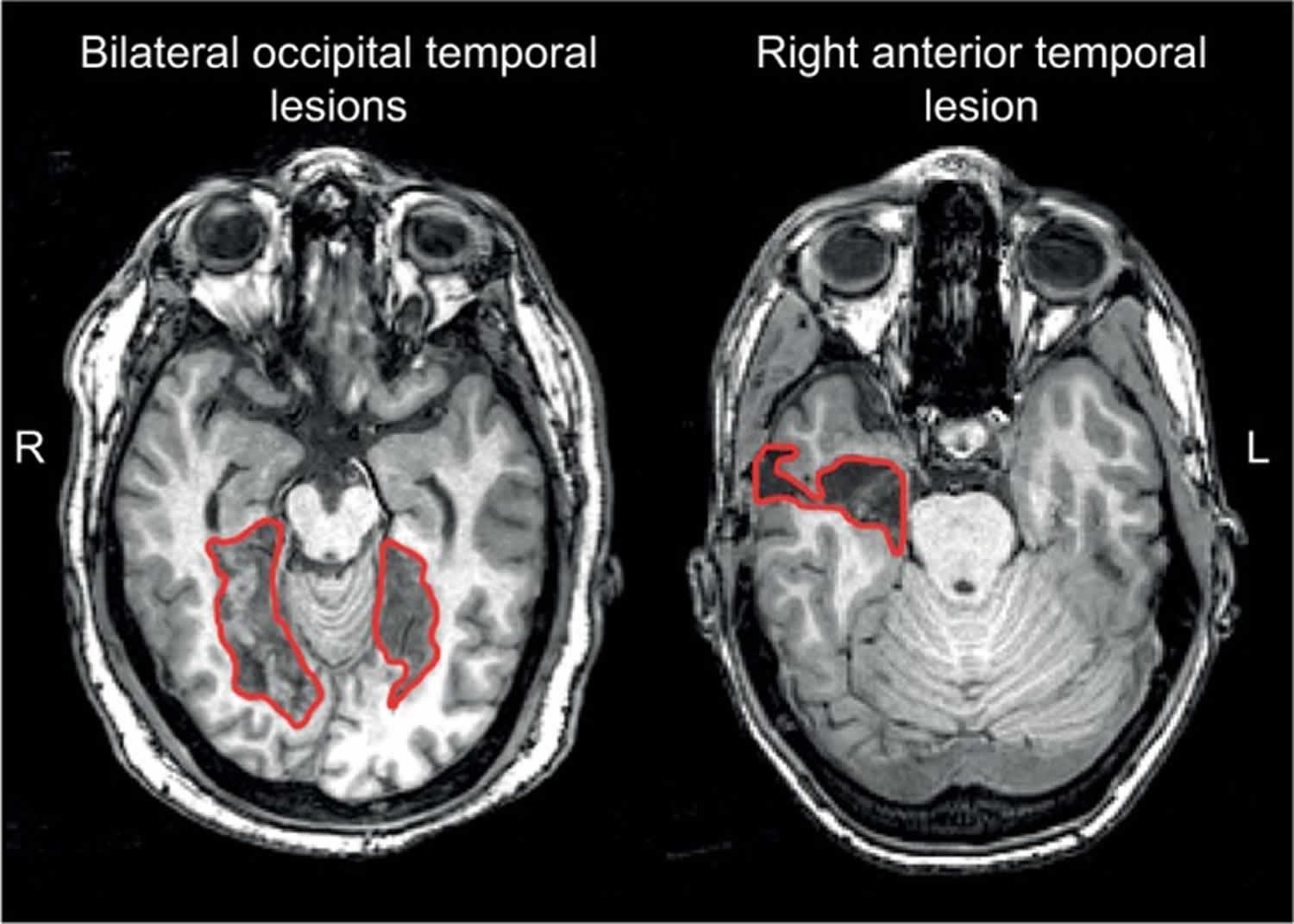
Figure 1. Acquired prosopagnosia (examples of lesions that produce acquired prosopagnosia)
Footnotes: Approximate lesions, as can be seen on a single slice, are outlined in red. Patients with bilateral occipital temporal lesions (left) often experience apperceptive prosopagnosia and those with anterior temporal lesions (right) often experience associative prosopagnosia. These cases demonstrate that acquired prosopagnosia is a family of disorders with different mechanisms and different lesion locations that lead to the same end result of prosopagnosia.
[Source 1 ]Congenital prosopagnosia
Congenital prosopagnosia appears to run in families, which makes it likely to be the result of a genetic mutation or deletion. Some degree of prosopagnosia is often present in children with autism and Asperger’s syndrome, and may be the cause of their impaired social development. Greater awareness of autism, and the autism spectrum disorders, which involve communication impairments such as prosopagnosia, is likely to make the disorder less overlooked in the future.
Prosopagnosia causes
Studies of acquired prosopagnosia have been advanced by the improved functional and structural capabilities of magnetic resonance imaging (MRI). A key fact is that a variety of lesions can cause prosopagnosia 10, an observation that makes sense when one considers the widely distributed networks involved in face processing. Two key observations have been made from the study of acquired prosopagnosia. First, lesions may be bilateral or unilateral, and when unilateral they are far more likely to be on the right 11. A few prosopagnosic subjects with left-sided lesions have been described, but most have been left-handed 12, raising the possibility that they may have had anomalous hemispheric lateralization to begin with. Second, there is a useful division between occipitotemporal and anterior temporal damage. Recent functional MRI work has shown that occipitotemporal damage is associated with loss of activation of core components such as the fusiform face area and occipital face area 13, while activation in anterior areas may be spared 14. Conversely, activation of the fusiform face area and occipital face area may be spared in individuals with anterior temporal lesions 13.
These modern neuroimaging observations have generated structural correlates for functional variants of prosopagnosia that had long been hypothesized 15. Recent studies show that those with fusiform lesions are more likely to have the apperceptive variant 16, whereas those with anterior temporal lesions are more likely to have the associative variant 16. The main conclusion is that acquired prosopagnosia is not a single disorder, but a family of disorders with different mechanisms and different lesions that nevertheless lead to the same end result of impaired face recognition 17.
The structural correlates of congenital prosopagnosia (developmental prosopagnosia) are still debated. By definition, there is no obvious structural lesion, and early studies examining the evidence of abnormal activation of the core face network produced mixed results, with some reporting normal activation 18 and another reporting activation for faces that did not differ from activation for other object types 19. Recent work with more advanced imaging methods has begun to uncover both structural and functional anomalies in developmental prosopagnosia, but there is disagreement. Some have suggested that there are anatomical 20 or functional 21 abnormalities in the fusiform face area and localized differences in white matter fibers around the right fusiform face area 22. Others maintain that the core face network is largely normal and that abnormalities lie instead in the anterior temporal cortex 23, other regions of the extended face network 24, or the long-range white matter tracts that connect the core regions in occipitotemporal cortex with the anterior temporal face area, namely the inferior longitudinal fasciculus 25. Both groups claim that the degree of altered white matter connectivity in their results correlated with behavioral measures of impaired face recognition 26. Whether these discrepancies reflect a real heterogeneity that exists in developmental prosopagnosia remains to be determined.
Prosopagnosia symptoms
Prosopagnosia is characterized by the inability to recognize the identity of faces 1. Subjects with prosopagnosia, cannot recognize that they have seen a face before, an impairment that affects both faces well known to them and those recently encountered. This is not due to more general problems with vision, object recognition, or memory. Depending upon the degree of impairment, some people with prosopagnosia may only have difficulty recognizing a familiar face; others will be unable to discriminate between unknown faces, while still others may not even be able to distinguish a face as being different from an object. Some people with prosopagnosia are unable to recognize their own face. Prosopagnosia is not related to memory dysfunction, memory loss, impaired vision, or learning disabilities.
Prosopagnosia diagnosis
Table 1. Suggested inclusion and exclusion criteria for the diagnosis of acquired and developmental prosopagnosia
| Inclusion criteria | Exclusion criteria | Clarification questions |
|---|---|---|
| • Difficulty with faces evident in everyday life (PI20) • Impairment on at least two measures of face familiarity (CFMT) • Confirmation of lesion by MRI or CT scan (AP cases only) | • Low-level visual impairment that could otherwise explain prosopagnosia • General visual agnosia • General memory impairment • Neuropsychological disorders associated with face recognition impairment • Visible lesion on MRI (DP cases only) | • Does the individual have associative or apperceptive subtype? (Cambridge Face Perception Test or Glasgow Face Matching Test) • Is the disorder prosopagnosia or a multimodal person recognition disorder? (Tests of name and voice familiarity) |
Footnote: Suggested tests for adults are indicated in parentheses, and brackets indicate criteria specific to either acquired prosopagnosia (AP) or developmental prosopagnosia (DP).
Abbreviations: CFMT = Cambridge Face Memory Test; MRI = magnetic resonance imaging; CT = computed tomography.
[Source 1 ]Prosopagnosia test
Tests of face familiarity
The hallmark of prosopagnosia is the reduced ability of subjects to realize that they have seen a face before: hence, key diagnostic tests probe the sense of familiarity for previously seen faces. Earlier tests of face recognition may have been less sensitive because their stimuli could allow subjects to use alternative strategies to circumvent poor face recognition, such as remembering hairstyles and clothing 27. Newer tests have addressed those limitations by minimizing those extraneous cues. The most commonly used test of familiarity for recently viewed faces is the Cambridge Face Memory Test (CFMT) 28, a test with high internal reliability 29. While the original version of this test used only adult Caucasian faces, other versions have been created, such as the CFMT-Chinese 30, CFMT-Australian 31 and pediatric versions, such as the CFMT-C 32 and the CFMT-Kids 33.
Tests that use anonymous faces like the Cambridge Face Memory Test (CFMT) have the advantage that, as none of the faces are familiar to subjects prior to learning, all subjects taking the test have the same degree of short-term familiarity with the faces seen during the test. Tests of familiarity for famous faces are also used, but such tests depend on the person having seen those celebrities before, and are therefore affected by age, education, and cultural background. In prosopagnosic subjects, this can be compounded by the fact that these subjects may lose interest in films and television because they cannot keep track of the characters, thus limiting their exposure to newer celebrities.
Tests of face perception
Tests of face perception – that is, the ability to perceive differences between faces – do not establish the diagnosis of prosopagnosia. What they can do is demonstrate if prosopagnosia is due to impaired encoding of the facial structure, and therefore is an apperceptive variant, or if such encoding is intact, which would point to an associative variant. Deficits in face perception have been measured by the Cambridge Face Perception Test 34 and the Glasgow Face Matching Test 35, which involve sorting or matching faces by their identity with minimal demands on memory. The Dartmouth Face Perception Test is useful for children 36.
Questionnaires can evaluate everyday experiences with face recognition. There is a 15-item self-report questionnaire 37 that contains questions on face recognition, attractiveness judgments, and expression recognition, and a more recent 20-item questionnaire for face identity the Prosopagnosia Index “PI20” 38. However, these should be supplemented by objective tests for diagnosis.
Exclusionary tests
Establishing impaired face recognition is not sufficient for the diagnosis of prosopagnosia. One must also show that this is not due to more general problems with vision and memory. The assessment of acuity and visual fields can exclude low-level impairments of vision as a cause of poor face recognition: indeed one of the problems of subjects with macular degeneration is difficulty recognizing faces 39. Beyond this, to exclude a more general visual agnosia, subjects with prosopagnosia should have normal object recognition at a “basic” level (ie, identifying that an object is a face, a bicycle, a lamp, etc). Some may have difficulties identifying specific examples of these objects (i.e., which bicycle or which lamp): this is not grounds for rejecting a diagnosis of prosopagnosia, but is relevant to the debate about whether the recognition problem in prosopagnosia is truly specific for faces alone. For this reason, challenging tests of object recognition that include measures of reaction time and premorbid expertise are useful 40.
Finally, prosopagnosia can occur in the context of other disorders, and the diagnostic process should consider whether any of these are present. In children, this includes conditions such as autism 41 and Turner’s syndrome 42, while in adults impaired face recognition has been reported in schizophrenia 43, Alzheimer’s disease 44, and Parkinson’s disease 45, for example. The diagnosis of prosopagnosia should be reserved for cases in which poor face recognition cannot be explained by one of these other conditions. Suggested criteria for the diagnosis of acquired and developmental prosopagnosia are outlined in Table 1. Greater detail regarding guidelines and available tests can be found in a recent review 46.
Prosopagnosia treatment
The focus of any treatment should be to help the individual with prosopagnosia develop compensatory strategies. Adults who have prosopagnosia as a result of stroke or brain trauma can be retrained to use other clues to identify individuals.
Can training improve prosopagnosia?
The answer may be that it depends. In acquired prosopagnosia, experts speculate that the efficacy of any training could be affected by age at onset, duration since onset, and lesion size, laterality, and location, particularly with regard to how much of the face network and its connections are compromised 47. Given the rarity of acquired prosopagnosia, it will be very difficult to establish the impact of each of these factors. To date, there have been few remedial attempts for the acquired prosopagnosia, and most focus on enhancing coping strategies to circumvent poor face recognition 48. Only one published study attempted to improve face recognition, in a child with diffuse damage after meningococcal meningitis: 18 months of training did not improve matters 49. More recently, two training studies have been reported at conferences. DeGutis et al 49 attempted to train a 46-year-old with a right occipital-temporal lesion to categorize faces based on the distances between face parts. Unfortunately, this did not help. A second study trained 12 subjects to discriminate increasingly subtler differences in face shape across variations in expression and viewpoint, over 11 weeks. Some improvement was found, but this was more modest for the recognition of faces not used during training 50.
Given the lack of overt brain damage, one might wonder whether training may be more effective in developmental prosopagnosia. One group trained 25 subjects with developmental prosopagnosia 51 to perceive the spacing between facial features and found improvements that generalized to new faces but did not help recognition when viewpoint varied 52. A different therapeutic approach was used in a randomized, placebo-controlled, double-blind study examining the effect of intranasal inhalation of oxytocin, a drug associated with the regulation of social behaviors, on face identity processing 53. The authors reported transient improvement of face perception and recognition in ten subjects with developmental prosopagnosia after oxytocin administration.
While these reports are encouraging, there may be limitations. Given the heterogeneity of deficits in prosopagnosia, it may be that a specific training program will not be appropriate for all subjects. How much of a residual face network one needs in acquired prosopagnosia to benefit from training is unknown. The belief that the subtler structural alterations of developmental prosopagnosia imply a better chance of having the neural substrate to generate benefit from training is unproven.
- Corrow SL, Dalrymple KA, Barton JJ. Prosopagnosia: current perspectives. Eye Brain. 2016;8:165-175. Published 2016 Sep 26. doi:10.2147/EB.S92838 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5398751/[↩][↩][↩][↩][↩]
- Quaglino’s 1867 case of prosopagnosia. Quaglino A, Borelli GB, Della Sala S, Young AW. Cortex. 2003 Jun; 39(3):533-40.[↩]
- BODAMER J. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr. 1947; 118(1-2):6-53.[↩]
- Structure and function in acquired prosopagnosia: lessons from a series of 10 patients with brain damage. Barton JJ. J Neuropsychol. 2008 Mar; 2(Pt 1):197-225.[↩]
- Developmental prosopagnosia: a window to content-specific face processing. Duchaine BC, Nakayama K. Curr Opin Neurobiol. 2006 Apr; 16(2):166-73.[↩]
- Cognitive heterogeneity in genetically based prosopagnosia: a family study. Schmalzl L, Palermo R, Coltheart M. J Neuropsychol. 2008 Mar; 2(Pt 1):99-117[↩]
- Human face recognition ability is specific and highly heritable. Wilmer JB, Germine L, Chabris CF, Chatterjee G, Williams M, Loken E, Nakayama K, Duchaine B. Proc Natl Acad Sci U S A. 2010 Mar 16; 107(11):5238-41.[↩]
- First report of prevalence of non-syndromic hereditary prosopagnosia (HPA). Kennerknecht I, Grueter T, Welling B, Wentzek S, Horst J, Edwards S, Grueter M. Am J Med Genet A. 2006 Aug 1; 140(15):1617-22.[↩]
- Psychosocial consequences of developmental prosopagnosia: a problem of recognition. Yardley L, McDermott L, Pisarski S, Duchaine B, Nakayama K. J Psychosom Res. 2008 Nov; 65(5):445-51.[↩]
- Damasio AR, Tranel D, Damasio H. Face agnosia and the neural substrates of memory. Annu Rev Neurosci. 1990;13:89–109.[↩]
- Damasio AR, Damasio H, Van Hoesen GW. Prosopagnosia: anatomic basis and behavioral mechanisms. Neurology. 1982;32(4):331–341.[↩]
- Barton JJ. Prosopagnosia associated with a left occipitotemporal lesion. Neuropsychologia. 2008;46(8):2214–2224.[↩]
- Davies-Thompson J, Pancaroglu R, Barton J. Acquired prosopagnosia: structural basis and processing impairments. Front Biosci (Elite Ed) 2014;6:159–174[↩][↩]
- Yang H, Susilo T, Duchaine B. The anterior temporal face area contains invariant representations of face identity that can persist despite the loss of right FFA and OFA. Cereb Cortex. 2016;26(3):1096–1107.[↩]
- De Renzi E, Faglioni P, Grossi D, Nichelli P. Apperceptive and associative forms of prosopagnosia. Cortex. 1991;27(2):213–221[↩]
- Barton JJ. Structure and function in acquired prosopagnosia: lessons from a series of 10 patients with brain damage. J Neuropsychol. 2008;2(Pt 1):197–225.[↩][↩]
- Davies-Thompson J, Pancaroglu R, Barton J. Acquired prosopagnosia: structural basis and processing impairments. Front Biosci (Elite Ed) 2014;6:159–174.[↩]
- Avidan G, Hasson U, Malach R, Behrmann M. Detailed exploration of face-related processing in congenital prosopagnosia: 2. functional neuroimagining findings. J Cogn Neurosci. 2005;17(7):1150–1167.[↩]
- Face-selective activation in a congenital prosopagnosic subject. J Cogn Neurosci. 2003;15(3):419–431.[↩]
- Developmental prosopagnosia: should it be taken at face value? Nunn JA, Postma P, Pearson R. Neurocase. 2001; 7(1):15-27.[↩]
- Zhang J, Liu J, Xu Y. Neural decoding reveals impaired face configural processing in the right fusiform face area of individuals with developmental prosopagnosia. J Neurosci. 2015;35(4):1539–1548.[↩]
- Gomez J, Pestilli F, Witthoft N, et al. Functionally defined white matter reveals segregated pathways in human ventral temporal cortex associated with category-specific processing. Neuron. 2015;85(1):216–227[↩]
- Avidan G, Tanzer M, Hadj-Bouziane F, Liu N, Ungerleider LG, Behrmann M. Selective dissociation between core and extended regions of the face processing network in congenital prosopagnosia. Cereb Cortex. 2014;24(6):1565–1578[↩]
- Avidan G, Behrmann M. Functional MRI reveals compromised neural integrity of the face processing network in congenital prosopagnosia. Curr Biol. 2009;19(13):1146–1150.[↩]
- Avidan G, Tanzer M, Hadj-Bouziane F, Liu N, Ungerleider LG, Behrmann M. Selective dissociation between core and extended regions of the face processing network in congenital prosopagnosia. Cereb Cortex. 2014;24(6):1565–1578.[↩]
- Song S, Garrido L, Nagy Z, et al. Local but not long-range micro-structural differences of the ventral temporal cortex in developmental prosopagnosia. Neuropsychologia. 2015;78:195–206.[↩]
- Duchaine BC, Nakayama K. Developmental prosopagnosia and the benton facial recognition test. Neurology. 2004;62(7):1219–1220.[↩]
- Duchaine B, Nakayama K. The Cambridge Face Memory Test: results from neurologically intact individuals and an investigation of its validity using inverted stimuli and prosopagnosic participants. Neuropsychologia. 2006;44(4):576–585[↩]
- Esins J, Schultz J, Stemper C, Kennerknecht I, Bülthoff I. Face perception and test reliabilities in congenital prosopagnosia in seven tests. Iperception. 2016;7(1):1–37[↩]
- McKone E, Stokes S, Liu J, et al. A robust method of measuring other-race and other-ethnicity effects: the Cambridge Face Memory Test format. PLoS One. 2012;7(10):e47956[↩]
- McKone E, Hall A, Pidcock M, et al. Face ethnicity and measurement reliability affect face recognition performance in developmental prosopagnosia: evidence from the Cambridge Face Memory Test-Australian. Cogn Neuropsychol. 2011;28(2):109–146.[↩]
- Croydon A, Pimperton H, Ewing L, Duchaine BC, Pellicano E. The Cam-bridge Face Memory Test for Children (CFMT-C): a new tool for measuring face recognition skills in childhood. Neuropsychologia. 2014;62:60–67.[↩]
- Dalrymple K, Gomez J, Duchaine B. CFMT-Kids: a new test of face memory for children. J Vis. 2012;12(9):492.[↩]
- Duchaine B, Yovel G, Nakayama K. No global processing deficit in the Navon task in 14 developmental prosopagnosics. Soc Cogn Affect Neurosci. 2007;2:104–113[↩]
- Burton A, White D, McNeill A. The Glasgow Face Matching Test. Behav Res Methods. 2010;42(1):286–291.[↩]
- Dalrymple KA, Garrido L, Duchaine B. Dissociation between face perception and face memory in adults, but not children, with developmental prosopagnosia. Dev Cogn Neurosci. 2014;10:10–20.[↩]
- Kennerknecht I, Ho NY, Wong VC. Prevalence of hereditary prosopagnosia (HPA) in Hong Kong Chinese population. Am J Med Genet A. 2008;146A(22):2863–2870[↩]
- The 20-item prosopagnosia index (PI20): a self-report instrument for identifying developmental prosopagnosia. Shah P, Gaule A, Sowden S, Bird G, Cook R. R Soc Open Sci. 2015 Jun; 2(6):140343.[↩]
- Barnes CS, De l’Aune W, Schuchard RA. A test of face discrimination ability in aging and vision loss. Optom Vis Sci. 2011;88(2):188–199[↩]
- Barton JJ, Hanif H, Ashraf S. Relating visual to verbal semantic knowledge: the evaluation of object recognition in prosopagnosia. Brain. 2009;132(Pt 12):3456–3466[↩]
- Weigelt S, Koldewyn K, Kanwisher N. Face identity recognition in autism spectrum disorders: a review of behavioral studies. Neurosci Biobehav Rev. 2012;36(3):1060–1084.[↩]
- Hong D, Scaletta Kent J, Kesler S. Cognitive profile of turner syndrome. Dev Disabil Res Rev. 2009;15(4):270–278[↩]
- Frith CD, Stevens M, Johnstone EC, Owens DG, Crow TJ. Integration of schematic faces and other complex objects in schizophrenia. J Nerv Ment Dis. 1983;171(1):34–39.[↩]
- Hodges JR, Salmon DP, Butters N. Recognition and naming of famous faces in Alzheimer’s disease: a cognitive analysis. Neuropsychologia. 1993;31(8):775–788.[↩]
- Dewick HC, Hanley JR, Davies AD, Playfer J, Turnbull C. Perception and memory for faces in Parkinson’s disease. Neuropsychologia. 1991;29(8):785–802[↩]
- Dalrymple KA, Palermo R. Guidelines for studying developmental prosopagnosia in adults and children. Wiley Interdiscip Rev Cogn Sci. 2016;7(1):73–87[↩]
- Bate S, Bennetts RJ. The rehabilitation of face recognition impairments: a critical review and future directions. Front Hum Neurosci. 2014;8:491.[↩]
- DeGutis JM, Chiu C, Grosso ME, Cohan S. Face processing improvements in prosopagnosia: successes and failures over the last 50 years. Front Human Neurosci. 2014;8:561.[↩]
- DeGutis J, Cohan S, Kahn DA, Aguirre GK, Nakayama K. Facial expression training improves emotion recognition and changes neural tuning in a patient with acquired emotion recognition deficits and prosopagnosia. J Vis. 2013;13(9):993–993.[↩][↩]
- Davies-Thompson J, Fletcher K, Hills C, Corrow S, Pancaroglu R, Barton JJS. Perceptual training of faces in rehabilitation of acquired prosopagnosia; Paper presented at: 38th European Conference on Visual Percpetion; August 23–27; 2015; Liverpool, United Kingdom.[↩]
- DeGutis JM, Bentin S, Robertson LC, D’Esposito M. Functional plasticity in ventral temporal cortex following cognitive rehabilitation of a congenital prosopagnosic. J Cogn Neurosci. 2007;19(11):1790–1802[↩]
- DeGutis J, Cohan S, Nakayama K. Holistic face training enhances face processing in developmental prosopagnosia. Brain. 2014;137(Pt 6):1781–1798[↩]
- Bate S, Cook SJ, Duchaine B, Tree JJ, Burns EJ, Hodgson TL. Intranasal inhalation of oxytocin improves face processing in developmental prosopagnosia. Cortex. 2014;50:55–63[↩]