Contents
- Psilocybin
- Table 1. Psilocybin effects
- Table 2. Psilocybin additional acute and long-term subjective effects
- Table 3. Psilocybin Treatment Subjective Experiences
- Table 4. Factors that affect therapeutic or clinical outcome of psilocybin administration
- Are Psilocybin mushrooms addictive?
- Are Psilocybin mushrooms illegal?
- How does psilocybin work?
- What are uses of psilocybin?
- Psilocybin side effects
- Is psilocybin safe?
Psilocybin
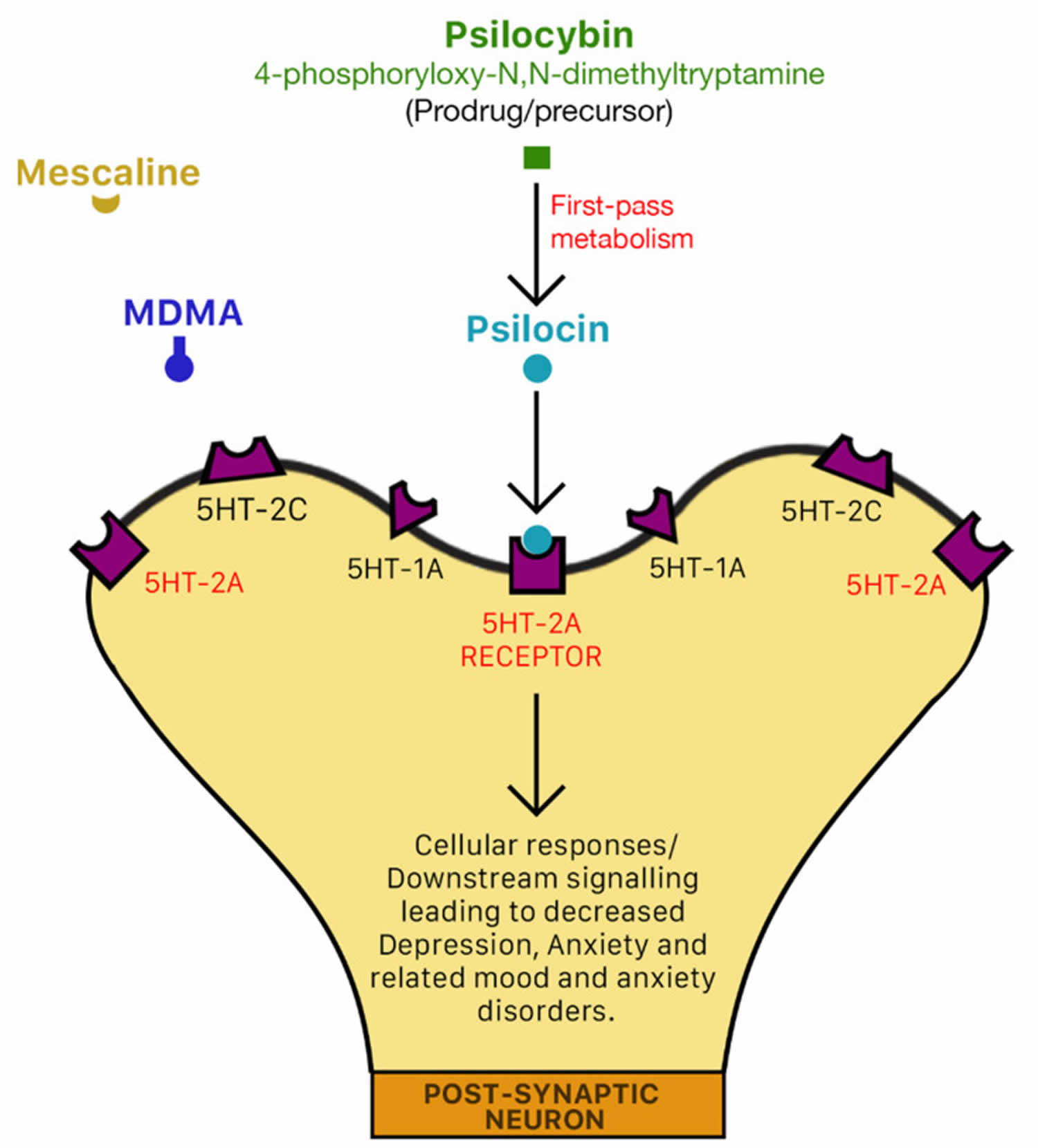
Psilocybin also known as 4-phosphoryloxy-N,N-dimethyltryptamine (4-phosphoryloxy-N,N-DMT), is a type of hallucinogen (classical serotonergic psychedelic) that is extracted from the genus Psilocybe mushrooms or “magic mushroom” (psilocybin-producing mushrooms) (see Figure 1) 1, 2, 3, 4, 5, 6, 7. Psychedelics are substances that exert their effects primarily by an agonist (or partial agonist) action on brain serotonin 5-hydroxytryptamine (5-HT2A) receptors 8. Psilocybin binds with high affinity to brain serotonin 5-hydroxytryptamine (5-HT2A) receptors 9. 5-HT serotonin receptors are densely located in areas of the brain that are responsible for the mediation of mood and anxiety disorders such as the pre-frontal cortex 10. Psychedelics affect all your senses, altering your thinking (introspection, self-consciousness, mystical experiences, altered time passage), sense of time and your mood or emotions (blissful state, euphoria, and joy) 11. Psychedelics can also cause a person to hallucinate (mainly visual effects)—seeing or hearing things that do not exist or are distorted. The intensity and nature of these effects are highly influenced by the set (your personality and internal expectations of the subject), setting (environment in which the substance is used), and dosage 12. Subjects participating in clinical trials often describe mystical experiences and improved mood while under the effects of these substances 13, 14. Although there is accumulating evidence that psychedelics are generally safe in humans 15, it is important to note that these substances can produce side effects and/or unpleasant experiences popularly known as “bad trips”, which involve transitory anxious and psychotic symptoms, confusion, dissociation and depersonalization 12. Of all the psychedelic drugs, psilocybin is reported to have the most favorable safety profile 16. Despite the lack of studies investigating the comparative effectiveness of psilocybin and psychedelic drugs for the treatment of mood and anxiety disorders, the vast evidence-based data that exist for psilocybin alone suggest that psilocybin may be the most efficacious psychedelic drug for treating mood and anxiety disorders 10.
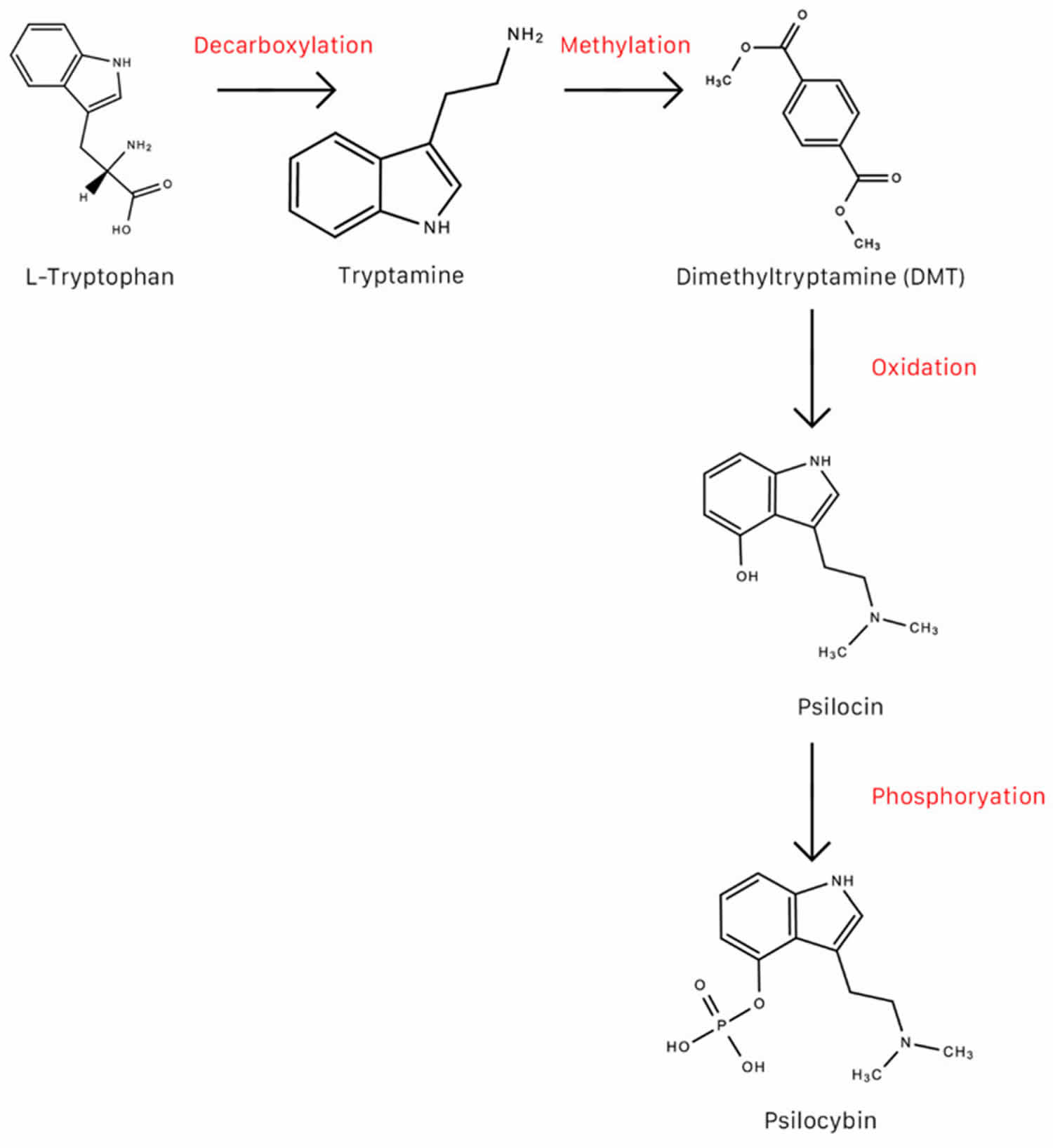
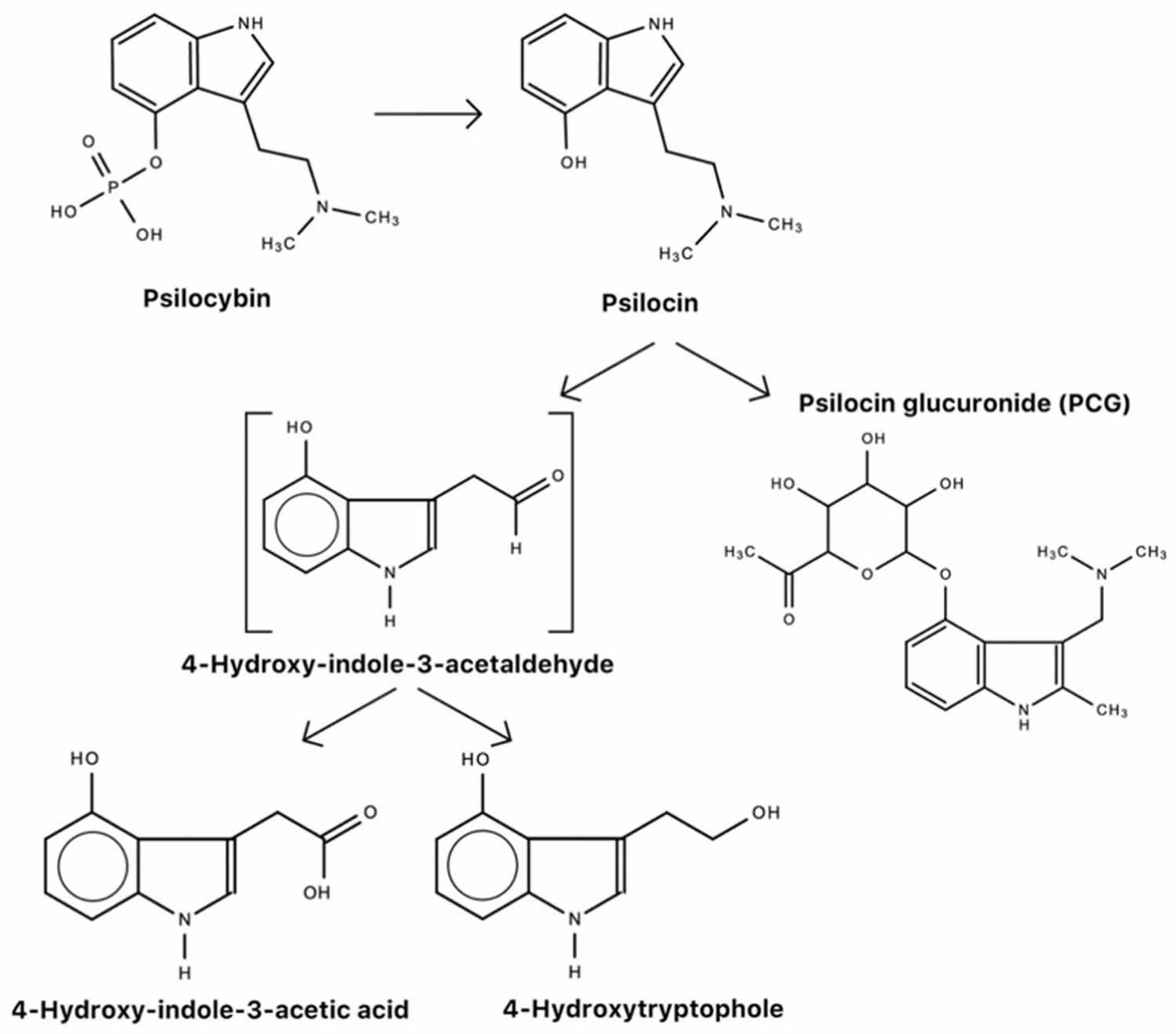
Psilocybin is considered a prodrug to psilocin 17. It is psilocin that is the main pharmacologically active substance in magic mushrooms, not psilocybin 9, 18. In humans, psilocybin is rapidly dephosphorylated to psilocin (4-hydroxy-N,N-dimethyltryptamine) by alkaline phosphatase in the liver 19, 20 and nonspecific esterase in the intestinal mucosa 21.
The effects of magic mushrooms are dependent on the species of mushroom and the concentration of active metabolites in a given species, an individual’s mindset an individual’s body type (particularly weight, metabolism) and an individual’s level of tolerance 10.
The effects of psilocybin may be classified into four categories 22, 23:
- Perceptual
- Cognitive
- Emotional
- Ego Dissolution.
More simply, psilocybin effects may be divided into psychic and somatic effects (see Table 1) 9. The perceptual changes are dose-dependent and could range from mental imagery, distortion, perceptual intensification, illusion, elementary hallucinations, and complex hallucinations 23. Sense of time, location, and causal sequence can lose their usual linear cause–effect relationship 23. Cognitive effects of psilocybin can be paradoxical and enigmatic. Certain cognitive traits associated with creativity can increase, such as divergent thinking, unlikely word associations or language patterns, expansion of semantic activation, and attribution of meaning to musical stimuli. The emotional effects are characterized by intensification of feelings, a broadening in the overall range of emotions felt over the duration of psilocybin exposure, and increased access to emotions such as unique states of euphoria characterized by involuntary grinning, uncontrollable laughter, forgiveness, connectedness, silliness, giddiness, playfulness, exuberance, or negative emotions. The majority of emotional effects of psilocybin in supportive contexts are experienced as positive or bias emotion toward constructive responses to social and environmental stimuli. There can be subtle to drastic ego dissolution experiences in which a sense of self- and ego loss occur, which are also exhibited in a dose-dependent fashion. The notion of self- and identity dissolution, sense of connection with the universe or environment, “mystical-type” experiences may reliably occur at higher doses and can be modulated by external stimuli such as music. This experience is more likely to influence long-term changes in life outlook and personality traits 22.
Psilocybin’s acute psychedelic effects are usually evident within 30 to 60 minutes after ingestion of low to moderate (2–10 g) dosing, but sometimes may not become noticeable for as long as an hour, with a gradual intensification over the first 1-2 hours 24. People may think they didn’t take enough so they take more. To avoid what may be an overly intense experience from a high dose, the “start low, go slow” method is best for anyone using psilocybin mushrooms – especially for people inexperienced with them or other psychedelics.
Psilocybin study reports a range of 3 to 5 mg orally produce sympathomimetic effects, but not hallucinogenic effects 20. Psilocybin’s hallucinogenic effects are produced within a range of 8 to 25 mg within 70 to 90 minutes 20. It has been demonstrated that equimolar amounts of psilocybin and psilocin produce similar psychotropic effects in humans 9, 25. After oral administration, most psilocybin, psilocin and glucoronidated metabolites are excreted via the kidneys, typically after about three hours 26. After about 24 hour, almost all psilocybin and psilocin are excreted from the body 26.
Perceptible psychological effects of psilocin correlate with plasma levels between 4 ng/mL and 6 ng/mL 20. Hasler and colleagues 20 estimate the bioavailability of psilocin to 52.7% after 10–20 mg psilocybin ingestion. After a rapid increase in plasma levels of psilocybin, followed by a plateau for approximately an hour, psilocybin levels wane significantly until barely detectable after 6 hours 20.
Subjective effects of psilocin may last between 3 and 6 hours 9, after which effects subside to negligible levels 24.
In clinical studies, the clinical outcome, and acute and long-term subjective effects of psilocybin administration are measured using questionnaires such as the Subjective experience (5D-ASC) 27, the Beck Depression Inventory (BDI), the Profile of Mood States (POMS) [69], the State-Train Anxiety Inventory (STAI), the Mystical Experience Questionnaire and the Quick Inventory of Depressive Symptoms (QIDS). Table 2 lists additional acute and long-term, subjective effects of psilocybin administration. Table 3 lists participants’ first-hand experiences and subjective perspectives during and after psilocybin in a 2016 phenomenological study conducted by Zamaria and colleagues 3.
Psilocybin, like other psychedelics, often evokes conscious awareness of subconscious thoughts and feelings, such as repressed memories, feelings about life circumstances, fantasies, or deep fears. Therefore, if someone makes the decision to use psilocybin mushrooms, it is important for that person to be prepared to deal with unusual – and perhaps even challenging – thoughts, images, and feelings in an open and thoughtful manner. It is also best to use psilocybin (or any psychedelic) with someone is not under the influence of the substance (a “guide”) who can prevent the user from engaging in dangerous activities 28.
Figure 1. Psilocybin mushrooms (Magic mushrooms)
Footnotes: Examples of Magic mushrooms (psilocybin-producing mushrooms). (a) Psilocybe cubensis (Earle) Singer also known as Stropharia cubensis. (b) Psilocybe caerulescens Murrill also known as Landslide Mushrooms or Derrumbes. (c) Psilocybe mexicana R. Heim also known as Teonanacatl, Pajaritos. (d) Psilocybe caerulipes (Peck) Sacc. also known as Blue Foot Mushroom. (e) Psilocybe stuntzii Guzmán and J. Ott also known as Blue Ringer Mushroom or Stuntz’s Blue Legs. (f) Psilocybe cyanescens Wakef. also known as Wavy Caps. (g) Psilocybe azurescens Stamets and Gartz also known as Flying Saucer Mushrooms. (h) Psilocybe pelliculosa (A.H. Sm.) Singer and A.H. Sm. (i) Psilocybe tampanensis Guzmán and Pollock also known as Magic Truffles or Philosopher’s Stone. (j) Psilocybe baeocystis Singer and A.H. Sm. (k) Psilocybe Hoogshagenii R. Heim nom. inval. also known as Little Birds of the Woods.
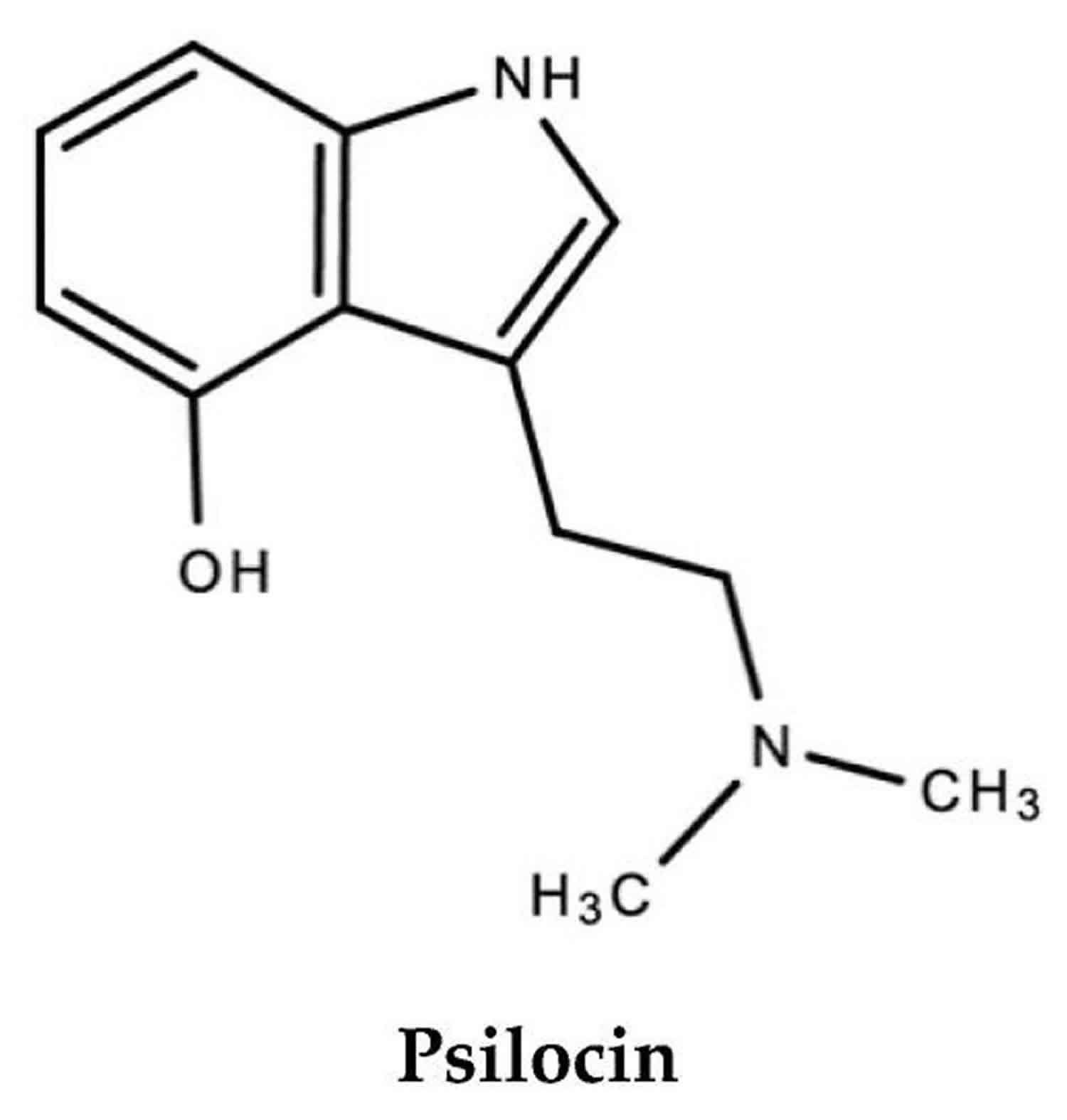
[Source 10 ]Figure 2. Psilocybin
[Source 10 ]Figure 3. Psilocin
Figure 4. Psilocybin synthesis
Footnote: Conversion of L-tryptophan to psilocybin
[Source 10 ]Figure 5. Psilocybin metabolism
[Source 10 ]Figure 6. Psilocybin Mechanism of Action
Footnote: Mechanism of action of psilocin. Psilocybin binds with high affinity to serotonin (5-hydroxytryptamine) type 2A (5-HT2A) receptors 9. 5-HT serotonin receptors are densely located in areas of the brain that are responsible for the mediation of mood and anxiety disorders such as the pre-frontal cortex. Molecular mechanisms of action have not yet been elucidated.
[Source 10 ]Table 1. Psilocybin effects
| Psychic Effects in Humans and Animals (in Medium Dose (12 to 20 mg orally) | Somatic Effects in Humans (Barely Noticeable or Secondary Pharmacological Effects) |
|---|---|
| At 8 to 12 mg oral or intramuscular injection;
At 0.11 mg/kg p.o, similar effects were observed in another study. At 1.5 mg increased to 25 mg orally in three doses per day, for 21 consecutive days, another study reported no significant aberrations in the parameters above. |
Table 2. Psilocybin additional acute and long-term subjective effects
| Effect | |
|---|---|
| 1 | Positive changes in personality and increased altruism. This may, in turn, have wider benefits to society and the global environment. |
| 2 | Enhanced feelings of connectedness |
| 3 | Enhanced-nature relatedness |
| 4 | Pro-environmental behavior |
| 5 | Decreased violent and criminal behavior |
| 6 | Reduced suicidal ideation |
| 7 | Protection against suicidality and psychological distress (lifetime psilocybin-use) |
| 8 | Tempered politically authoritarian views |
| 9 | Increase in personality domain of openness |
| 10 | Ego dissolution. Reduction of egotistical attitudes, narcissism and induces greater prosocial behavior. |
| 11 | Sustained/persisting improvement in attitudes and behavior. One study reports substantial decreases in depressive and anxious symptoms persisting up to 6 months after a single active treatment. In another study, participants report positive persisting effects in areas of mood, behavior, and attitudes after up to 14 months after psilocybin therapy. |
| 12 | Improved psychological flexibility and feelings of personal meaningfulness, and subsequent improved psychological outlook. Ability to reframe how a patient views their medical conditions, themselves, their lives and relationships with others. |
| 13 | Increase in one’s subjective sense of wellbeing. |
| 14 | Quantum change (meaningful personal transformations) |
| 15 | Enhancement of “meaning responses” |
| 16 | Increased meditation depth |
| 17 | Increased incidence of positive self-dissolution |
Table 3. Psilocybin Treatment Subjective Experiences
| Subjective, First-Hand Accounts of Experience with Psilocybin Treatment | |
|---|---|
| 1 | -Transcendental experience -“Mystical” -“Divine” -“Otherworldly experience” -“Felt like I saw God” -“Deep spiritual experience” -“Connection to something spiritual” -“Connection and spirituality with God” -“Continuity and oneness with God” -“Bliss, heaven, nirvana” -“Mystical and transcendental experience akin to a deep or profound state of meditation or an egoless state” -“Amazement” |
| 2 | Changes in outlook -“Major shift in attention and perspective of the world” -“Notable and intense change in perspective of the world” -“Noticeable intricacies in environment” -“Clarity” -“Inspiration for behavioral change” -“Reduction in being too concerned about things, in general. Not neglectful, but hopeful”. -“Acceptance of concern with aging and death”. |
| 3 | -Unity consciousness and ego dissolution -“Perception of life as a deeper, richer experience” -“Greater connection to nature, to other people, and to all living things” -“At one with the universe and all of existence” -“Every particle of existence felt like an extension of myself” -“Increased “connectedness” and “acceptance”” -“Feeling of being able to explore oneself more with others” -“Intense, beautiful feeling of love and joy and gratitude for everything” |
| 4 | Peace and Happiness -“Incredible, profound calmness and stillness” -“Happiness and contentment” -“Persistent happiness and joy” |
| 5 | -Increased introspection -“Greater capacity to motivate and examine oneself” -“Greater understanding of self” -Self-assessment -“Looking at oneself with much more objectivity” -“Reception of thoughts from a wise place” -“Greater insight” -“Greater self-awareness” -“Greater ability to understand what will bring happiness” -“Greater sense of purpose and direction” -“Persisting feeling of self-awareness and insight” -“Greater trust in one’s feelings and experiences” -“Access to deeper parts of oneself” -“Greater connection to core values” -“Feeling more “grounded” -“Persisting insight” -“Awareness of emotions and thoughts and better ability to articulate one’s thoughts and emotions to others. -“Deep appreciation and sense of gratitude” |
| 6 | Physical/Mental -Improvement of mental wellbeing -Increase in patience- Reduction in depressive thoughts -Reduction in anxiety -“Lighter, limber, more energetic” -Persistent reduction in psychological distress (anxiety, worry, and sadness) -“Expedited self-development” -“Healthy and beneficial behavioural changes” -“Ability to understand and deliberately divert focus from/mitigate depressive thoughts” |
Table 4. Factors that affect therapeutic or clinical outcome of psilocybin administration
| Factor | |
|---|---|
| 1 | Extra-pharmacological elements (as with any drug). These include age factors, body weight, body size, muscle mass, genetics, drug tolerance, drug interactions, drug purity, dosage, gender, recreational consumption and inexperience with recreational drug use, past experiences with drug use, mindset, setting (context in which drug is used), experimental setting, social interaction, cultural influences, medical history, placebo design and response to placebo, and drug instrumentalization (instruments used to administer drugs). |
| 2 | Mindset -Patient attitude and expectations (psychological flexibility/ outlook) -Preconceptions of treatment -Affective processes |
| 3 | Setting -Use of music and/or art -Use of religious and spiritual imagery -Engagement with nature -Use of a purpose-built facility |
| 4 | Psychological support -Intensive clinical care/contact -Supportive and reassuring interaction with therapists/sitters. -Reliable induction of “mystical experience” by clinician/therapist. Mystical experiences after psilocybin administration directly correlate with therapeutic outcome and persisting positive subjective effects. |
| 5 | Specific types of psychological experiences |
| 6 | Treatment type -Some patients may require personalized/individualized treatment which may involve combination therapy with other drugs. Drug interactions may likely affect psilocybin treatment. -Treatments with mushroom extracts as opposed to pure isolated psilocybin may also have different outcomes. |
| 7 | Type of mood or anxiety disorder |
| 8 | Degree of suicidality (ideation and actual attempts) in a patient. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. |
| 9 | Patients with a family history of psychotic disorders. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. Psychedelics may augment/compound symptoms of psychoses. |
| 10 | Patients who score high on neuroticism, a Big Five higher-order personality trait. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. |
| 11 | Patients with history or current diagnosis of bipolar disorder and schizophrenia. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. |
| 12 | Patients at high risk for developing psychosis, even though psilocybin does not cause lasting anxiety, depression or psychosis. It is recommended that such patients who will be less likely to benefit from such treatment should be excluded from psychedelic therapy. |
| 13 | Patients on other psychedelic/anti-psychotic/anti-depressant medications such as selective serotonin re-uptake inhibitors (SSRIs), haloperidol, tricyclic anti-depressants, lithium, and monoamine oxidase inhibitors. |
Are Psilocybin mushrooms addictive?
Psilocybin is not considered to be addictive nor does it cause compulsive use 29. One reason is that the intense experience, which can be physically and mentally challenging, may cause people using psilocybin to limit their frequency of use 28. Another reason is that the human body quickly builds tolerance to psilocybin, such that people require much higher doses after only a few days of repeated use, making it extremely difficult to have any effect after more than four days of repeated usage 28. And because of the similar brain receptors involved in their effects, cross- tolerance occurs with LSD and psilocybin, which means that if someone takes LSD one day, the effects of taking psilocybin the next day will be diminished 28.
Are Psilocybin mushrooms illegal?
In nearly all cases, yes. Psilocybin and psilocin are listed in Schedule 1 of the Controlled Substances Act, making it illegal to cultivate or possess psilocybin-producing mushrooms for either
personal consumption or distribution. However, they can be used for scientific research under tightly-controlled conditions with a special license from the U.S. Drug Enforcement Administration (DEA). While laws vary by specific substance, the U.S. Drug Enforcement Administration (DEA) lists most psychedelic and dissociative drugs on the U.S. schedule of controlled substances here (https://www.deadiversion.usdoj.gov/schedules).
Because federal law does not list the various species of mushrooms containing psilocybin themselves, some people arrested for criminal possession, cultivation or distribution of mushrooms have claimed innocence. One such case in Florida in 1978 led to a state Supreme Court ruling that the legislature needed to specifically list psilocybin-containing mushrooms as illegal 30. The decision’s precedent led to arguments in subsequent cases in several other states 31. In 2005, an appeals court in New Mexico ruled that growing psilocybin mushrooms for personal consumption could not be considered “manufacturing a controlled substance” under state law 28. Regardless, in most cases psilocybin, and psilocybin-containing mushrooms are illegal federally and statewide, with cultivation, possession and sale offenses being grounds for arrest 28.
How does psilocybin work?
Psilocin reacts agonistically with serotonin (5-hydroxytryptamine) type 2A (5-HT2A) receptors to produce a “mystical-like” hallucinatory effect 9, 23 due to induced frontal hyper-frontality 9, which in turn mediates its anti-depressant and anti-anxiety effects (see Figure 5) 3, 5. One possible anti-depressant mechanism of action of psilocybin is via deactivation or normalization of the hyperactivity of the medial prefrontal cortex (mPFC) 32, 33, 34. During depression, the medial prefrontal cortex (mPFC) is typically hyperactive 35.
Anti-depressant properties of psilocybin are mediated via modulation of the prefrontal and limbic brain regions, with the inclusion of the amygdala 36. The amygdala plays an essential role in perception and emotion-processing networks 34. In cases of depression, an individual typically loses responsiveness to emotional stimuli 37. It is also suggested that the hyper-frontal metabolic pattern produced after psilocybin administration and 5-HT2A receptor activation is comparable to metabolic patterns produced in acute psychotic episodes in chronic schizophrenics 19.
It is also reported that psilocybin binds with high affinity to the 5-HT2A serotonergic receptor subtype, but with low affinity to the 5-HT1A serotonergic receptor subtype 9. The interaction of psilocybin and psilocin with 5-HT2A receptors to produce psychotomimetic effects has been confirmed in experiments with ketanserin, a 5-HT2A antagonist that attenuates the effects of psilocybin 9, 27. In addition to interaction with 5-HT2A receptors, it is also suggested that the psychopharmacological action of psilocybin may also be mediated by non-5HT2 receptors 38, 21, 34. Psilocybin and psilocin also interact with the 5-HT1D and 5-HT2C receptor subtypes 9.
Psilocybin is reported to result in significant changes in brain dynamics and functional connectivity between areas of the brain 36, 39, 40, 41. Psilocybin-induced alteration in brain connectivity involves the disintegration of associative networks and integration of sensory function networks 19. It is suggested that this dissociation may mediate the subjective effects of psilocybin use and a state of unconstrained cognition 19. On the same tangent, a possible mechanism of action behind psilocybin’s psychotomimetic effects are via interactions with feedback loops between the cortex and thalamus 9. Psilocybin administration produces general cortical activation 19. This is confirmed by increased levels of the cerebral metabolic rate of glucose in the prefrontal cortex, anterior cingulate, temporal cortex, and putamen 42. This increase in the prefrontal cortex, anterior cingulate, temporal cortex, and putamen activity is positively correlated with hallucinatory “ego dissolution” 19. The metabolic rate of glucose also increased in distinct right-hemispheric frontotemporal cortical regions 43.
Serotonin 5-HT2A receptors are distributed in multiple areas of the brain that play a role in psychosis and psychotic symptoms, such as the cerebral cortex (prefrontal cortex) and periphery 27, striatum, ventral tegmental area, and thalamus 44.
In addition to the presence of serotonergic cell bodies, dopaminergic cell bodies are also distributed in the ventral tegmental area 45, an area of the brain that plays a role in reward-processed, and regulation of emotion and cognitive behaviors 46. Although the neuropharmacological mechanisms of action of psilocybin are not definitively elucidated, there is evidence that, in addition to interaction with the serotonergic system, psilocybin also seems to interact, though not directly, with the mesolimbic dopaminergic pathway that plays a significant role in the brain’s reward system 45. This proposed indirect mechanism of action is suggested by psilocybin’s low addictive or abuse potential 45. It has also been hypothesized that there is a positive correlation between depression and dopamine deficiency in the mesolimbic pathways 47.
It is also hypothesized that schizophrenia and possibly other mood and anxiety disorders is characterized by dysregulation or disbalance of serotonin and dopamine 48. In acute psychoses, one study even concludes that5-HT2A and 5-HT1A serotonergic receptors play an important role in the modulation of striatal dopamine release. This suggests that psilocybin may have significant potential in the treatment of schizophrenia and possibly other psychiatric disorders 48. In another study, psilocybin was indirectly responsible for an increase in endogenous dopamine via a decrease in 11C-raclopride binding potential bilaterally in the caudate nucleus (19%) and putamen (20%) 49.
A 2021 study by Grandjean and colleagues 50 investigated the effects of psilocybin on functional connectivity across the entire brain region in mice. One possible mechanism of action by which psilocybin produces anti-depressant effects is via interaction with or alteration of the default-mode network 51. Using resting-state functional MRI (fMRI), psilocybin was shown to decrease functional connectivity within dopamine (DA)-associated striatal networks, in addition to demonstrating alteration (increase) of functional connectivity between serotonin (5-HT) associated networks and cortical areas 50. This study confirms the interaction of psilocybin with the mesolimbic dopaminergic pathway to produce neural and psychological effects 50. Data presented in another mice study suggest that psilocin, an active metabolite of psilocybin, has been shown to increase the concentrations of both extracellular dopamine and serotonin (5-HT) in the mesoaccumbens and/or mesocortical pathway 52. This presents yet another possible mechanism of anti-depressant action of psilocybin/psilocin, that is, the ability to increase dopamine, a neurotransmitter that is responsible for the regulation of emotions and even an individual’s physical well-being 53. Concentrations of both extracellular dopamine and serotonin (5-HT) in the ventral tegmental area (VTA) were not affected 52. This further suggests that, in addition to the ventral tegmental area (VTA), the brain’s reward circuity may also be influenced by other regions of the brain.
Serotonin (5-hydroxytryptamine) type 2A (5-HT2A) receptors activation and subsequent activation of postsynaptic glutamatergic alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptors by psilocybin is associated with increased glutamate concentration. Glutamate is responsible for normal, healthy brain functioning 54.
Psilocybin treatment, in some cases with psychological support, also resulted in increased responsiveness to positive emotional stimuli in the right amygdala 37, 55 and decreased or normalization of responsiveness to negative or neutral emotional stimuli 56, 34, 57, 58, 59, 60. Psilocybin was also shown to attenuate amygdala activation in response to threat-related visual stimuli 58 and reduced threat-induced modulation of the primary visual cortex by the amygdala 58. The amygdala modulates the primary visual cortex via top-down connectivity 58.
In contrast, other selective serotonin reuptake inhibitors (SSRIs) may produce anti-depressant effects by attenuating the hyper-responsiveness of the amygdala to fearful emotional stimuli, thereby inhibiting negative emotions 37. Hyperactivity of the amygdala to fearful emotional stimuli is typically characteristic of depression 61. SSRIs mitigate this hyperactivity to emotional stimuli 61 whereas psilocybin is suggested to increase amygdala activation to positive emotional stimuli 61, 62. In another study, psilocybin treatment also reduced anhedonia (the inability to feel pleasure) 63.
Barrett and colleagues 56 also suggest that psilocybin may even influence brain plasticity as confirmed by the persisting positive effect and increased amygdala response to positive emotional stimuli up to one month post psilocybin treatment.
Unlike indoleamine LSD and other hallucinogens that that bind to dopamine D2 receptors to produce the typical dopaminergic “psychotic” experiences, psilocybin and psilocin have no affinity for dopamine D2 receptors 9, 23, 64, despite the existence of a functional interaction between the serotoninergic and central dopaminergic systems 9. This functional interaction between the serotoninergic and central dopaminergic systems has been demonstrated in experiments with haloperidol, a D2 receptor antagonist that attenuates the psychotomimetic effects of psilocybin 9.
A study by Carhart-Harris 51 investigated the effects of psilocybin on cerebral blood flow and blood-oxygen-level-dependent resting-state functional connectivity (RSFC) via functional magnetic resonance imaging (fMRI). Post psilocybin treatment, authors reported decreased amygdala cerebral blood flow associated with reduced symptoms of depression, and increased resting-state functional connectivity within the default-mode network 65, increased resting-state functional connectivity in the ventromedial prefrontal cortex-bilateral interior lateral parietal cortex, and decreased resting-state functional connectivity in the parahippocampal–prefrontal cortex 51. Alteration of the default mode network is characteristic of mood and anxiety disorders 66 and another possible mechanism of action by which psilocybin produces anti-depressant effects is via interaction with the default-mode network 51, via disruption of functional connectivity between the medial temporal lobe (MTL) and the default-mode network 67.
Another functional magnetic resonance imaging (fMRI) study 62 reports a decreased functional connectivity between the amygdala and the ventromedial prefrontal cortex (vmPFC) in response to fearful and neutral (but not happy) faces after psilocybin treatment. The ventromedial prefrontal cortex (vmPFC) is responsible for emotional processing, action, cognitive behaviour and goal-orientation, and demonstrates top-down inhibitory control on the amygdala 62. It is suggested then that psilocybin treating, which decreases functional connectivity between amygdala and the ventromedial prefrontal cortex (vmPFC) in response to fearful and neutral (but not happy) faces, also decreases the top-down inhibitory control that the ventromedial prefrontal cortex (vmPFC) has on the amygdala, and ultimately results in increased amygdala activity 62. In medication-naïve individuals, decreased functional connectivity between the amygdala and the left rostral prefrontal cortex (left rPFC) is characteristic of major depressive disorder 68.
Also characteristic of depression and schizophrenia is an alteration of serotonergic signalling 69. Therefore, drugs that target serotonergic receptors in the prefront cortex may be of clinical importance 69.
What are uses of psilocybin?
Mushrooms used non-medically are usually taken orally either by eating dried caps and stems, or steeped in hot water and drunk as a tea, with a common dose around 1 to 2.5 grams, though
potency may vary regardless of the amount 70. Dried mushrooms are typically more potent than fresh ones. Risk of fatal overdose is virtually nonexistent with psilocybin mushrooms; however, risky behaviors sometimes occur while people are under the influence.
Research conducted in the mid-20th century found that carefully monitored and controlled use of psilocybin may be beneficial for many psychiatric disorders, personal and spiritual development, and creative enhancement 71. However, after psilocybin was banned in 1970, clinical research to evaluate its medical safety and efficacy of psychedelics was effectively halted until the late 90s and early 2000s 72.
There are dozens of studies taking place to evaluate the medical safety and effectiveness of psychedelics, including psilocybin. Much of the earlier research did not stand up to today’s standards, as they often lacked a placebo control group or double-blinding procedures (in which neither the subject of the research nor the investigators knew whether the subject received psilocybin or placebo). Nevertheless, their promising findings have been revisited and spurred a resurgence of new, more rigorous research on the potential benefits of psychedelics as a treatment for cluster headache 73, anxiety, addiction to alcohol and other drugs 74, depression 75, obsessive-compulsive disorder (OCD) 76, as well as neuroimaging experiments furthering the understanding of psychedelic effects on the brain 77.
Because of the expensive and labyrinthian approval process for research with Schedule 1 drugs, as well as the political influence of the war on drugs, research evaluating psilocybin’s beneficial uses does not receive funding from academic or government institutions and this has left many unanswered questions regarding the pharmacology and toxicology of psilocybin 78.
Psilocybin side effects
The risks associated with psychedelic drugs are mostly psychological, not physical. Physically, psilocybin mushrooms are considered to be one of the least toxic drugs known 28. Although lethal doses have been determined from experiments in several animal models 79, recorded cases of death exclusively attributed to usual doses of psilocybin mushrooms in humans are extremely rare 80.
Physical effects of psilocybin mushrooms are minor but varied and can be unique from person to person. The most consistent reactions of psilocybin mushrooms, such as dilated pupils (mydriasis), elevated blood pressure (hypertension) and increased heart rate (tachycardia), are usually mild, and considered side effects of emotional intensification. However, these along with other reported symptoms like nausea, increased perspiration, numbing and tremors, can sometimes make psychological symptoms like anxiety, panic attacks, paranoia, and mood swings seem worse 81. Long-term physical effects of psilocybin mushrooms are directly attributed to the pharmacology of psilocybin are rare, and research suggests they may also be due to latent psychological disorders 28.
However, predicting what kind of experience a person will have after taking psilocybin is difficult, so experts recommend that people with a personal or family history of mental illness should be aware of their vulnerability to potential latent psychological issues emerging or being triggered.
Comprehensive reviews of the thousands of sessions using psilocybin and other psychedelics in legal clinical research settings during the 1950s and 60s have consistently found extremely low incidences of acute and chronic problems among individuals lacking pre-existing severe psychopathology. Recent reviews of the clinical literature also suggest that chronic problematic effects, when they do occur, are most often linked to psychological instability present prior to use 82.
Hallucinogen Persisting Perception Disorder (HPPD), sometimes mistakenly referred to as “flashbacks”, is a condition unique to psychedelics, involving perceptual changes lasting weeks or months following the use of a drug like psilocybin. Though exact prevalence is unknown, Hallucinogen Persisting Perception Disorder (HPPD) is considered relatively rare, with no physical changes or neurological damage associated as the cause 83.
Is psilocybin safe?
Due to the lack of quality control regulations under prohibition and the risk of consuming things growing in nature, there is potential for people attempting to pick psilocybin mushrooms in the wild to accidentally take poisonous mushrooms instead 28. Similarly, though also very unlikely, poisonous mushrooms are sometimes misrepresented and sold as psilocybin, and these do come with more physical risks, including fatal overdose 28.
There is no safe level of drug use. Use of any drug always carries some risk. It’s important to be careful when taking any type of drug. While more research is needed, the reported incidence of serious adverse events from professionally supervised use of specific psychedelic drugs, such as in clinical trials, is relatively low 84, 85, 86, 87. However, many past clinical studies on these drugs have not adequately assessed or reported on adverse events 88.
Psilocybin is a Schedule 1 controlled substance as defined by the United Nations 1971 Convention on Psychotropic Substances. By this definition, psilocybin is considered to have a high abuse potential and is currently not accepted medically 10. In uncontrolled settings such as in recreation, abuse of psilocybin may lead to what is referred to as a “bad trip” 10. This is an undesired or even traumatic physical and emotional experiences characterized by altered visual perception, extreme distress, fear, lack of coordination, derealization, depersonalization, paraesthesiae, heightened fright, panic-attacks, traumatic flashbacks, paranoia, delirium, short-term psychosis and other symptomology characteristics of schizophrenia 89, 90, 91, 92. This undesired physical experience may also be accompanied by nausea, vomiting, dilated pupils (mydriasis), headache, chills and drowsiness 89. Some symptoms may even persist. A “bad trip” is typically treated with benzodiazepines 10.
Mushroom toxicity is also a risk associated with some species of psilocybin mushrooms 10. Though rare and typically accidental, mushroom poisoning is also a risk, and may lead to minor gastrointestinal illness such as gastroenteritis, erythromelalgia, rhabdomyolysis, intestinal fibrosis, hypertension, hyperreflexia, liver failure, renal failure, convulsions, bradycardia, and tachycardia 89, 93. Mushroom poison may also require medical intervention or emergency hospitalization 89, 90. In general, alcohol and other drugs may worsen the psychological and physical risks of psilocybin abuse 10. On the same tangent, individuals with a personal or family history of severe psychotic and psychiatric disorders are discouraged from using psilocybin, and by extension, other psychedelics 94.
In general, psilocybin is reported to have the most favourable safety profile of all psychedelic drugs 16, 95, 96. Thousands of years of anecdotal evidence in addition to modern-day scientific studies confirm that psilocybin has low physiological toxicity, low abuse or addictive ability, safe psychological responses, no associated persisting adverse physiological or psychological effects during or after use 97, 9, 98, 99. Psilocybin overdose is very rare 28, 100. One such report of psilocybin overdose and subsequent fatality was specifically due to cardiac arrest, some 2 to 3 hours after psilocybin ingestion, in a 24-year-old female who, 10 years prior, had a heart transplant due to end-stage rheumatic heart disease 101.
In patients with mental or psychiatric disorders, suicidal ideation and auto-mutilation are possible risks of magic mushroom ingestion and have been documented in the literature 102. Another risk is the possibility of exacerbating psychotic symptoms 103. As a result, having psychotic disorders such as schizophrenic tendencies is a contraindication for undergoing psychedelic-assisted psychotherapy, particularly psilocybin-assisted psychotherapy 104.
It is also reported that repeated psilocybin use will build high tolerability but will not lead to physical dependence 9, 34, 105. Cross-tolerance with other psychedelics such as LSD and mescaline is also a possibility 38, 106. Discontinued psilocybin use does not typically cause adverse physical effects or symptomology related to drug withdrawal 10. There is also a chance that psychological withdrawal may occur 10.
The Registry of Toxic Effects of Chemical Substances (RTECS) has assigned psilocybin a therapeutic index of 641, associated with a relatively better safety profile in comparison to nicotine and aspirin, with values of 21 and 199, respectively 98. Essentially, this means that psilocybin has very low chronic toxicity, moderate acute toxicity, negligible public health and criminal effects 92. To date, there is no standard value for a lethal dose at neither the recreational nor medicinal levels in humans 99.
Risks associated with psilocybin may be prevented or alleviated with the implementation of a medically supervised setting, preparatory counseling to induce the right patient mindset, and adequate professional clinical psychological and physiological support 107. Due to the low physiological toxicity, low abuse/addictive liability, safe psychological responses, no associated persisting adverse physiological or psychological effects during or after use, it is hypothesized that the lethal dose of psilocybin is far greater than the effective dose 108, 109, 110, 26.
How risky are Psilocybin mushrooms compared to other drugs?
Psilocybin is considered to have extremely low toxicity, and cases of death have been extremely rare. But beginning in the 1960s and continuing today, sensationalized media coverage of psychedelic-related deaths misattributed the role of psychedelics like psilocybin in causing suicide or accidental death 28.
Recent results from epidemiological studies have actually shown lower rates of mental health disorders and suicide among people who have used psychedelics like psilocybin 111, 112, 113.
The risks from psilocybin are dependent on set (your personality and internal expectations of the subject), setting (environment in which the substance is used) and the dose and differ from other types of drugs, including alcohol, benzodiazepines, and opiates, which produce relatively predictable physical and psychological effects 28. The consequences of negative or challenging experiences can be minimized by education and awareness of psilocybin’s effects, with particular attention paid to issues around set and setting prior to the experience.
- Nichols, D.E. Psilocybin: from ancient magic to modern medicine. J Antibiot 73, 679–686 (2020). https://doi.org/10.1038/s41429-020-0311-8[↩]
- Schindler E.A.D., Gottschalk C.H., Weil M.J., Shapiro R.E., Wright D.A., Sewell R.A. Indoleamine Hallucinogens in Cluster Headache: Results of the Clusterbusters Medication Use Survey. J. Psychoact. Drugs. 2015;47:372–381. doi: 10.1080/02791072.2015.1107664[↩]
- Zamaria J.A. A Phenomenological Examination of Psilocybin and its Positive and Persisting Aftereffects. NeuroQuantology. 2016;14 doi: 10.14704/nq.2016.14.2.943[↩][↩][↩]
- Stafford P. Psychedelics Encyclopedia, Third ed. Ronin Publishing; Berkeley, CA, USA: 2013.[↩]
- Mithoefer M.C., Grob C.S., Brewerton T.D. Novel psychopharmacological therapies for psychiatric disorders: Psilocybin and MDMA. Lancet Psychiatry. 2016;3:481–488. doi: 10.1016/S2215-0366(15)00576-3[↩][↩]
- Carod-Artal F.J. Hallucinogenic drugs in pre-Columbian Mesoamerican cultures. Neurologia (Barcelona, Spain) 2015;30:42–49. doi: 10.1016/j.nrl.2011.07.003[↩]
- Hofmann A. LSD, My Problem Child: Reflections on Sacred Drugs, Mysticism, and Science. 4th ed. Multidisciplinary Association for Psychedelic Studies (MAPS); Santa Cruz, CA, USA: 2009.[↩]
- Nichols D. E. (2016). Psychedelics. Pharmacological reviews, 68(2), 264–355. https://doi.org/10.1124/pr.115.011478[↩]
- Passie T., Seifert J., Schneider U., Emrich H.M. The pharmacology of psilocybin. Addict. Biol. 2002;7:357–364. doi: 10.1080/1355621021000005937[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Lowe H, Toyang N, Steele B, Valentine H, Grant J, Ali A, Ngwa W, Gordon L. The Therapeutic Potential of Psilocybin. Molecules. 2021 May 15;26(10):2948. doi: 10.3390/molecules26102948[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Dos Santos RG, Hallak JEC. Therapeutic use of serotoninergic hallucinogens: A review of the evidence and of the biological and psychological mechanisms. Neurosci Biobehav Rev. 2020 Jan;108:423-434. doi:10.1016/j.neubiorev.2019.12.001[↩]
- Bogenschutz MP, Ross S. Therapeutic Applications of Classic Hallucinogens. Curr Top Behav Neurosci. 2018;36:361-391. doi: 10.1007/7854_2016_464[↩][↩]
- Dos Santos RG, Bouso JC, Alcázar-Córcoles MÁ, Hallak JEC. Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety, and substance-use disorders: a systematic review of systematic reviews. Expert Rev Clin Pharmacol. 2018 Sep;11(9):889-902. doi: 10.1080/17512433.2018.1511424[↩]
- Timmermann, C., Roseman, L., Williams, L., Erritzoe, D., Martial, C., Cassol, H., Laureys, S., Nutt, D., & Carhart-Harris, R. (2018). DMT Models the Near-Death Experience. Frontiers in psychology, 9, 1424. https://doi.org/10.3389/fpsyg.2018.01424[↩]
- Dos Santos RG, Hallak JEC. Therapeutic use of serotoninergic hallucinogens: A review of the evidence and of the biological and psychological mechanisms. Neurosci Biobehav Rev. 2020 Jan;108:423-434. doi: 10.1016/j.neubiorev.2019.12.001[↩]
- Hendricks P.S., Johnson M.W., Griffiths R.R. Psilocybin, psychological distress, and suicidality. J. Psychopharmacol. 2015;29:1041–1043. doi: 10.1177/0269881115598338[↩][↩]
- Horita A. Some biochemical studies on psilocybin and psilogin. J. Neuropsychiatr. 1963;4:270–273.[↩]
- Nichols D.E. Psychedelics. Pharmacol. Rev. 2016;68:264–355. doi: 10.1124/pr.115.011478[↩]
- Nichols D.E. Psilocybin: From ancient magic to modern medicine. J. Antibiot. 2020;73:679–686. doi: 10.1038/s41429-020-0311-8[↩][↩][↩][↩][↩][↩]
- Hasler F., Bourquin D., Brenneisen R., Bär T., Vollenweider F.X. Determination of psilocin and 4-hydroxyindole-3-acetic acid in plasma by HPLC-ECD and pharmacokinetic profiles of oral and intravenous psilocybin in man. Pharm. Acta Helv. 1997;72:175–184. doi: 10.1016/S0031-6865(97)00014-9[↩][↩][↩][↩][↩][↩]
- Tylš F., Pálenîcek T., Horácek J. Psilocybin Summary of knowledge and new perspectives. Eur. Neuropsychopharmacol. 2014;24:342–356. doi: 10.1016/j.euroneuro.2013.12.006[↩][↩]
- Vollenweider, F., Kometer, M. The neurobiology of psychedelic drugs: implications for the treatment of mood disorders. Nat Rev Neurosci 11, 642–651 (2010). https://doi.org/10.1038/nrn2884[↩][↩]
- Kargbo R.B. Psilocybin Therapeutic Research: The Present and Future Paradigm. ACS Med. Chem. Lett. 2020;11:399–402. doi: 10.1021/acsmedchemlett.0c00048[↩][↩][↩][↩][↩]
- Carhart-Harris R.L., Bolstridge M., Rucker J., Day C.M.J., Erritzoe D., Kaelen M., Bloomfield M., A Rickard J., Forbes B., Feilding A., et al. Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. Lancet Psychiatry. 2016;3:619–627. doi: 10.1016/S2215-0366(16)30065-7[↩][↩]
- Quetin A. Psilocybin in clinical and experimental psychiatry. Impr. Modern. 1960 doi: 10.1002/hup.2742[↩]
- Hasler F., Bourquin D., Brenneisen R., Vollenweider F.X. Renal excretion profiles of psilocin following oral administration of psilocybin: A controlled study in man. J. Pharm. Biomed. Anal. 2002;30:331–339. doi: 10.1016/S0731-7085(02)00278-9[↩][↩][↩]
- Thomas K., Malcolm B., Lastra D. Psilocybin-Assisted Therapy: A Review of a Novel Treatment for Psychiatric Disorders. J. Psychoact. Drugs. 2017;49:446–455. doi: 10.1080/02791072.2017.1320734[↩][↩][↩]
- How risky are Psilocybin Mushrooms Compared to other Drugs? https://drugpolicy.org/wp-content/uploads/2023/05/2023.04.05_psilocybin_factsheet.pdf[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Psychedelic and Dissociative Drugs. https://nida.nih.gov/research-topics/psychedelic-dissociative-drugs[↩]
- Psilocybin Mushrooms Legal Status. https://erowid.org/plants/mushrooms/mushrooms_law.shtml[↩]
- Boire, Richard Glen, Esq. Sacred Mushrooms and the Law. Berkeley, CA: Ronin, 2002.[↩]
- Hassan Z., Bosch O.G., Singh D., Narayanan S., Kasinather B.V., Seifritz E., Kornhuber J., Quednow B.B., Müller C.P. Novel Psychoactive Substances—Recent Progress on Neuropharmacological Mechanisms of Action for Selected Drugs. Front. Psychiatry. 2017;8 doi: 10.3389/fpsyt.2017.00152[↩]
- Chávez-Castillo M., Núñez V., Nava M., Ortega Á., Rojas M., Bermúdez V., Rojas-Quintero J. Depression as a Neuroendocrine Disorder: Emerging Neuropsychopharmacological Approaches beyond Monoamines. Adv. Pharmacol. Sci. 2019;2019:1–20. doi: 10.1155/2019/7943481[↩]
- Mahapatra A., Gupta R. Role of psilocybin in the treatment of depression. Ther. Adv. Psychopharmacol. 2017;7:54–56. doi: 10.1177/2045125316676092[↩][↩][↩][↩][↩]
- Holtzheimer P.E., Mayberg H.S. Stuck in a rut: Rethinking depression and its treatment. Trends Neurosci. 2011;34:1–9. doi: 10.1016/j.tins.2010.10.004[↩]
- Grimm O., Kraehenmann R., Preller K., Seifritz E., Vollenweider F. Psilocybin modulates functional connectivity of the amygdala during emotional face discrimination. Eur. Neuropsychopharmacol. 2018;28:691–700. doi: 10.1016/j.euroneuro.2018.03.016[↩][↩]
- Roseman L., Nutt D.J., Carhart-Harris R.L. Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression. Front. Pharmacol. 2018;8 doi: 10.3389/fphar.2017.00974[↩][↩][↩]
- Halberstadt A.L., Geyer M.A. Multiple receptors contribute to the behavioral effects of indoleamine hallucinogens. Neuropharmacology. 2011;61:364–381. doi: 10.1016/j.neuropharm.2011.01.017[↩][↩]
- Tagliazucchi E., Carhart-Harris R., Leech R., Nutt D., Chialvo D.R. Enhanced repertoire of brain dynamical states during the psychedelic experience. Hum. Brain Mapp. 2014;35:5442–5456. doi: 10.1002/hbm.22562[↩]
- Lord L.-D., Expert P., Atasoy S., Roseman L., Rapuano K., Lambiotte R., Nutt D.J., Deco G., Carhart-Harris R.L., Kringelbach M.L., et al. Dynamical exploration of the repertoire of brain networks at rest is modulated by psilocybin. NeuroImage. 2019;199:127–142. doi: 10.1016/j.neuroimage.2019.05.060[↩]
- Müller F., Liechti M.E., Lang U.E., Borgwardt S. Advances and challenges in neuroimaging studies on the effects of serotonergic hallucinogens: Contributions of the resting brain. Prog. Brain Res. 2018;242:159–177. doi: 10.1016/bs.pbr.2018.08.004[↩]
- Inaba D., Cohen W.E. Uppers, Downers, All Arounders: Physical and Mental Effects of Psychoactive Drugs. 7th ed. CNS Productions; Medford, OR, USA: 2014.[↩]
- Gouzoulis-Mayfrank E., Schreckenberger M., Sabri O., Arning C., Thelen B., Spitzer M., Kovar K.-A., Hermle L., Büll U., Sass H. Neurometabolic Effects of Psilocybin, 3,4-Methylenedioxyethylamphetamine (MDE) and d-Methamphetamine in Healthy Volunteers A Double-Blind, Placebo-Controlled PET Study with [18F]FDG. Neuropsychopharmacology. 1999;20:565–581. doi: 10.1016/S0893-133X(98)00089-X[↩]
- Bortolozzi A., Masana M., Díaz-Mataix L., Cortés R., Scorza M.C., Gingrich J.A., Toth M., Artigas F. Dopamine release induced by atypical antipsychotics in prefrontal cortex requires 5-HT1A receptors but not 5-HT2A receptors. Int. J. Neuropsychopharmacol. 2010;13:1299–1314. doi: 10.1017/S146114571000009X[↩]
- De Veen B.T., Schellekens A.F., Verheij M.M., Homberg J.R. Psilocybin for treating substance use disorders? Expert Rev. Neurother. 2016;17:203–212. doi: 10.1080/14737175.2016.1220834[↩][↩][↩]
- Nagaeva E., Zubarev I., Gonzales C.B., Forss M., Nikouei K., De Miguel E., Elsilä L., Linden A.-M., Hjerling-Leffler J., Augustine G.J., et al. Heterogeneous somatostatin-expressing neuron population in mouse ventral tegmental area. eLife. 2020;9 doi: 10.7554/eLife.59328[↩]
- Dailly E., Chenu F., Renard C.E., Bourin M. Dopamine, depression and antidepressants. Fundam. Clin. Pharmacol. 2004;18:601–607. doi: 10.1111/j.1472-8206.2004.00287.x[↩]
- Vollenweider F.X., Vontobel P., Hell D., Leenders K.L. 5-HT Modulation of Dopamine Release in Basal Ganglia in Psilocybin-Induced Psychosis in Man—A PET Study with [11C]raclopride. Neuropsychopharmacology. 1999;20:424–433. doi: 10.1016/S0893-133X(98)00108-0[↩][↩]
- Maust D.T., Bonar E.E., Ilgen M.A., Blow F.C., Kales H.C. Agitation in Alzheimer Disease as a Qualifying Condition for Medical Marijuana in the United States. Am. J. Geriatr. Psychiatry. 2016;24:1000–1003. doi: 10.1016/j.jagp.2016.03.006[↩]
- Grandjean J., Buehlmann D., Buerge M., Sigrist H., Seifritz E., Vollenweider F.X., Pryce C.R., Rudin M. Psilocybin exerts distinct effects on resting state networks associated with serotonin and dopamine in mice. NeuroImage. 2021;225 doi: 10.1016/j.neuroimage.2020.117456[↩][↩][↩]
- Carhart-Harris R.L., Erritzoe D., Williams T., Stone J.M., Reed L.J., Colasanti A., Tyacke R.J., Leech R., Malizia A.L., Murphy K., et al. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc. Natl. Acad. Sci. USA. 2012;109:2138–2143. doi: 10.1073/pnas.1119598109[↩][↩][↩][↩]
- Sakashita Y., Abe K., Katagiri N., Kambe T., Saitoh T., Utsunomiya I., Horiguchi Y., Taguchi K. Effect of Psilocin on Extracellular Dopamine and Serotonin Levels in the Mesoaccumbens and Mesocortical Pathway in Awake Rats. Biol. Pharm. Bull. 2015;38:134–138. doi: 10.1248/bpb.b14-00315[↩][↩]
- Coull J.T., Cheng R.-K., Meck W.H. Neuroanatomical and Neurochemical Substrates of Timing. Neuropsychopharmacology. 2010;36:3–25. doi: 10.1038/npp.2010.113[↩]
- Hindley G., Beck K., Borgan F., Ginestet C.E., McCutcheon R., Kleinloog D., Ganesh S., Radhakrishnan R., D’Souza D.C., Howes O.D. Psychiatric symptoms abused by cannabis constituents: A systematic review and meta-analysis. Lancet Psychiatry. 2020;7:344–353. doi: 10.1016/S2215-0366(20)30074-2[↩]
- Carhart-Harris R.L., Roseman L., Bolstridge M., Demetriou L., Pannekoek J.N., Wall M.B., Tanner M., Kaelen M., McGonigle J., Murphy K. Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms. Sci. Rep. 2017:7. doi: 10.1038/s41598-017-13282-7[↩]
- Barrett F.S., Krimmel S.R., Griffiths R.R., Seminowicz D.A., Mathur B.N. Psilocybin acutely alters the functional connectivity of the claustrum with brain networks that support perception, memory, and attention. NeuroImage. 2020;218 doi: 10.1016/j.neuroimage.2020.116980[↩][↩]
- Geyer M.A. Lysergic Acid Diethylamide and Psilocybin Revisited. Biol. Psychiatry. 2015;78:516–518. doi: 10.1016/j.biopsych.2015.08.003[↩]
- Kraehenmann R., Preller K.H., Scheidegger M., Pokorny T., Bosch O.G., Seifritz E., Vollenweider F.X. Psilocybin-Induced Decrease in Amygdala Reactivity Correlates with Enhanced Positive Mood in Healthy Volunteers. Biol. Psychiatry. 2015;78:572–581. doi: 10.1016/j.biopsych.2014.04.010[↩][↩][↩][↩]
- Kraehenmann R., Schmidt A., Friston K., Preller K.H., Seifritz E., Vollenweider F.X. The mixed serotonin receptor agonist psilocybin reduces threat-induced modulation of amygdala connectivity. Neuroimage Clin. 2016;11:53–60. doi: 10.1016/j.nicl.2015.08.009[↩]
- DeRubeis R.J., Siegle G.J., Hollon S.D. Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nat. Rev. Neurosci. 2008;9:788–796. doi: 10.1038/nrn2345[↩]
- Magic Mushrooms and the Amygdala. https://neuroscientificallychallenged.com/posts/magic-mushrooms-and-the-amygdala[↩][↩][↩]
- Mertens L.J., Wall M.B., Roseman L., Demetriou L., Nutt D.J., Carhart-Harris R.L. Therapeutic mechanisms of psilocybin: Changes in amygdala and prefrontal functional connectivity during emotional processing after psilocybin for treatment-resistant depression. J. Psychopharmacol. 2020;34:167–180. doi: 10.1177/0269881119895520[↩][↩][↩][↩]
- Stroud J.B., Freeman T.P., Leech R., Hindocha C., Lawn W., Nutt D., Curran H., Carhart-Harris R.L. Psilocybin with psychological support improves emotional face recognition in treatment-resistant depression. Psychopharmacol. 2018;235:459–466. doi: 10.1007/s00213-017-4754-y[↩]
- Creese I., Burt D.R., Synder S.H., Snyder S.H. The dopamine receptor: Differential binding of d-LSD and related agents to agonist and antagonist states. Life Sci. 1975;17:1715–1719. doi: 10.1016/0024-3205(75)90118-6[↩]
- Roseman L., Leech R., Feilding A., Nutt D.J., Carhart-Harris R.L. The effects of psilocybin and MDMA on between-network resting state functional connectivity in healthy volunteers. Front. Hum. Neurosci. 2014;8 doi: 10.3389/fnhum.2014.00204[↩]
- Coutinho J.F., Fernandesl S.V., Soares J.M., Maia L., Gonçalves Ó F., Sampaio A. Default mode network dissociation in depressive and anxiety states. Brain Imaging Behav. 2016;10:147–157. doi: 10.1007/s11682-015-9375-7[↩]
- Carhart-Harris R.L., Leech R., Hellyer P.J., Shanahan M., Feilding A., Tagliazucchi E., Chialvo D.R., Nutt D. The entropic brain: A theory of conscious states informed by neuroimaging research with psychedelic drugs. Front. Hum. Neurosci. 2014;8 doi: 10.3389/fnhum.2014.00020[↩]
- Kong L., Chen K., Tang Y., Wu F., Driesen N., Womer F., Fan G., Ren L., Jiang W., Cao Y., et al. Functional connectivity between the amygdala and prefrontal cortex in medication-naive individuals with major depressive disorder. J. Psychiatry Neurosci. 2013;38:417–422. doi: 10.1503/jpn.120117[↩]
- Puig M.V., Gulledge A.T. Serotonin and Prefrontal Cortex Function: Neurons, Networks, and Circuits. Mol. Neurobiol. 2011;44:449–464. doi: 10.1007/s12035-011-8214-0[↩][↩]
- Nutt D.; King L. A.; Saulsbury W.; Blakemore C. Developing of a rational scale to assess the harm of drugs of potential misuse. Lancet 2007, 369, 1047. 10.1016/S0140-6736(07)60464-4[↩]
- Nichols DE. Hallucinogens. Pharmacol Ther. 2004 Feb;101(2):131-81. doi: 10.1016/j.pharmthera.2003.11.002[↩]
- Ellens, J. Harold, and Thomas B. Roberts. The psychedelic policy quagmire: health, law, freedom, and society. Santa Barbara, CA: Praeger an Imprint of ABC- CLIO, LLC, 2015.[↩]
- Sewell RA, Halpern JH, Pope HG Jr. Response of cluster headache to psilocybin and LSD. Neurology. 2006 Jun 27;66(12):1920-2. doi: 10.1212/01.wnl.0000219761.05466.43[↩]
- Bogenschutz MP, Johnson MW. Classic hallucinogens in the treatment of addictions. Prog Neuropsychopharmacol Biol Psychiatry. 2016 Jan 4;64:250-8. doi: 10.1016/j.pnpbp.2015.03.002[↩]
- Carhart-Harris RL, Bolstridge M, Rucker J, Day CM, Erritzoe D, Kaelen M, Bloomfield M, Rickard JA, Forbes B, Feilding A, Taylor D, Pilling S, Curran VH, Nutt DJ. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016 Jul;3(7):619-27. doi: 10.1016/S2215-0366(16)30065-7[↩]
- Moreno FA, Wiegand CB, Taitano EK, Delgado PL. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006 Nov;67(11):1735-40. doi: 10.4088/jcp.v67n1110[↩]
- Carhart-Harris RL, Leech R, Hellyer PJ, Shanahan M, Feilding A, Tagliazucchi E, Chialvo DR, Nutt D. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci. 2014 Feb 3;8:20. doi: 10.3389/fnhum.2014.00020[↩]
- Kargbo RB. Psilocybin Therapeutic Research: The Present and Future Paradigm. ACS Med Chem Lett. 2020 Mar 2;11(4):399-402. doi: 10.1021/acsmedchemlett.0c00048[↩]
- Usdin, Earl, and Daniel H. Efron. Psychotropic Drugs and Related Compounds. Rockville, MD: National Institute of Mental Health, 1972.[↩]
- Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512[↩]
- Carbonaro TM, Bradstreet MP, Barrett FS, MacLean KA, Jesse R, Johnson MW, Griffiths RR. Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. J Psychopharmacol. 2016 Dec;30(12):1268-1278. doi: 10.1177/0269881116662634[↩]
- Nichols DE. Psychedelics. Pharmacol Rev. 2016 Apr;68(2):264-355. doi: 10.1124/pr.115.011478. Erratum in: Pharmacol Rev. 2016 Apr;68(2):356.[↩]
- Halpern JH, Lerner AG, Passie T. A Review of Hallucinogen Persisting Perception Disorder (HPPD) and an Exploratory Study of Subjects Claiming Symptoms of HPPD. Curr Top Behav Neurosci. 2018;36:333-360. doi: 10.1007/7854_2016_457[↩]
- Johnson MW, Hendricks PS, Barrett FS, Griffiths RR. Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol Ther. 2019;197:83-102. doi:10.1016/j.pharmthera.2018.11.010[↩]
- Vollenweider FX, Smallridge JW. Classic Psychedelic Drugs: Update on Biological Mechanisms. Pharmacopsychiatry. 2022;55(3):121-138. doi:10.1055/a-1721-2914[↩]
- Studerus E, Gamma A, Kometer M, Vollenweider FX. Prediction of psilocybin response in healthy volunteers. PLoS One. 2012;7(2):e30800. doi:10.1371/journal.pone.0030800[↩]
- Goldberg SB, Shechet B, Nicholas CR, et al. Post-acute psychological effects of classical serotonergic psychedelics: a systematic review and meta-analysis. Psychol Med. 2020;50(16):2655-2666. doi:10.1017/S003329172000389X[↩]
- Breeksema JJ, Kuin BW, Kamphuis J, van den Brink W, Vermetten E, Schoevers RA. Adverse events in clinical treatments with serotonergic psychedelics and MDMA: A mixed-methods systematic review. J Psychopharmacol. 2022;36(10):1100-1117. doi:10.1177/02698811221116926[↩]
- Peden N.R., Pringle S.D., Crooks J. The Problem of Psilocybin Mushroom Abuse. Hum. Toxicol. 1982;1:417–424. doi: 10.1177/096032718200100408[↩][↩][↩][↩]
- Hyde C., Glancy G., Omerod P., Hall D., Taylor G.S. Abuse of Indigenous Psilocybin Mushrooms: A New Fashion and Some Psychiatric Complications. Br. J. Psychiatry. 1978;132:602–604. doi: 10.1192/bjp.132.6.602[↩][↩]
- Vollenweider F.X., Vollenweider-Scherpenhuyzen M.F.I., Bäbler A., Vogel H., Hell D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. NeuroReport. 1998;9:3897–3902. doi: 10.1097/00001756-199812010-00024[↩]
- Van Amsterdam J., Opperhuizen A., Brink W.V.D. Harm potential of magic mushroom use: A review. Regul. Toxicol. Pharmacol. 2011;59:423–429. doi: 10.1016/j.yrtph.2011.01.006[↩][↩]
- Jo W.-S., Hossain A., Park S.-C. Toxicological Profiles of Poisonous, Edible, and Medicinal Mushrooms. Mycobiology. 2014;42:215–220. doi: 10.5941/MYCO.2014.42.3.215[↩]
- Dos Santos R.G., Bouso J.C., Alcázar-Córcoles M.Á., Hallak J.E.C. Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety, and substance-use disorders: A systematic review of systematic reviews. Expert Rev. Clin. Pharmacol. 2018;11:889–902. doi: 10.1080/17512433.2018.1511424[↩]
- Gable R.S. Toward a Comparative Overview of Dependence Potential and Acute Toxicity of Psychoactive Substances Used Nonmedically. Am. J. Drug Alcohol Abus. 1993;19:263–281. doi: 10.3109/00952999309001618[↩]
- Gable R.S. Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction. 2004;99:686–696. doi: 10.1111/j.1360-0443.2004.00744.x[↩]
- Johnson M.W., Griffiths R.R. Potential Therapeutic Effects of Psilocybin. Neurotherapeutics. 2017;14:734–740. doi: 10.1007/s13311-017-0542-y[↩]
- Griffiths R.R., Richards W.A., McCann U., Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology. 2006;187:268–283. doi: 10.1007/s00213-006-0457-5[↩][↩]
- Fantegrossi W.E., Woods J.H., Winger G. Transient reinforcing effects of phenylisopropylamine and indolealkylamine hallucinogens in rhesus monkeys. Behav. Pharmacol. 2004;15:149–157. doi: 10.1097/00008877-200403000-00007[↩][↩]
- Johnson M.W., Griffiths R.R., Hendricks P.S., Henningfield J.E. The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act. Neuropharmacology. 2018;142:143–166. doi: 10.1016/j.neuropharm.2018.05.012[↩]
- Lim T.H., Wasywich C.A., Ruygrok P.N. A fatal case of ‘magic mushroom’ ingestion in a heart transplant recipient. Intern. Med. J. 2012;42:1268–1269. doi: 10.1111/j.1445-5994.2012.02955.x[↩]
- Müller K., Püschel K., Iwersen-Bergmann S. Suizid unter Psilocin-Einfluss [Suicide under the influence of “magic mushrooms”] Arch. Kriminol. 2013;231:193–198. German.[↩]
- James E., Robertshaw T.L., Hoskins M., Sessa B. Psilocybin occasioned mystical-type experiences. Hum. Psychopharmacol. Clin. Exp. 2020;35 doi: 10.1002/hup.2742[↩]
- Byock I. Taking Psychedelics Seriously. J. Palliat. Med. 2018;21:417–421. doi: 10.1089/jpm.2017.0684[↩]
- Appel J.B., Freedman D.X. Tolerance and cross-tolerance among psychotomimetic drugs. Psychopharmacol. 1968;13:267–274. doi: 10.1007/BF00401404[↩]
- Passie T., Halpern J.H., Stichtenoth D.O., Emrich H.M., Hintzen A. The Pharmacology of Lysergic Acid Diethylamide: A Review. CNS Neurosci. Ther. 2008;14:295–314. doi: 10.1111/j.1755-5949.2008.00059.x[↩]
- Johnson M.W., Richards W.A., Griffiths R.R. Human hallucinogen research: Guidelines for safety. J. Psychopharmacol. 2008;22:603–620. doi: 10.1177/0269881108093587[↩]
- Strassman R. Inner Paths to Outer Space: Journeys to Alien Worlds through Psychedelics and Other Spiritual Technologies. Paperback Edition; Park Street Press; Rochester, VT, USA: 2008.[↩]
- Freye E. Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs. Springer Science and Business Media LLC; Berlin/Heidelberg, Germany: 2009. The Mushroom Psilocybin with Psychedelic Properties; pp. 221–223.[↩]
- Gable R.S. The Toxicity of Recreational Drugs. Am. Sci. 2006;94:207. doi: 10.1511/2006.59.206[↩]
- Cormier, Z. No link found between psychedelics and psychosis. Nature (2015). https://doi.org/10.1038/nature.2015.16968[↩]
- Hendricks PS, Thorne CB, Clark CB, Coombs DW, Johnson MW. Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. J Psychopharmacol. 2015 Mar;29(3):280-8. doi: 10.1177/0269881114565653[↩]
- Krebs TS, Johansen PØ. Psychedelics and mental health: a population study. PLoS One. 2013 Aug 19;8(8):e63972. doi: 10.1371/journal.pone.0063972[↩]