Contents
What is pyuria
Pyuria means pus in the urine. Pyuria is defined as ≥5 urinary white blood cells per high-powered field 1 and it is usually a sign of urinary tract infection (UTI).
The presence of pyuria in a general pediatrics population, in combination with clinical signs and symptoms, is highly suggestive of urinary tract infection (UTI) 2. However, pyuria frequently occurs among children with neurogenic bladder 3. The authors of the Infectious Disease Society of America guidelines for the diagnosis of catheter-associated UTI do not consider the presence of pyuria to be diagnostic of UTI in patients who require clean intermittent catheterization 4. The presence of pyuria in this population is multifactorial; chronic inflammation may result from frequent catheterization9 as well as from changes in the underlying genitourinary epithelium.
Abnormal urinalysis findings of leukocyte esterase and pyuria are common in both urinary tract infections (UTIs) and sexually transmitted infections (STIs) 5. STIs (sexually transmitted infections) have been previously found to be associated with pyuria without bacteriuria 6. Previous studies in emergency department settings evaluating women diagnosed with urinary tract infections (UTIs) have demonstrated that only about 50% will have a positive urine culture and 10 to 50% will have an sexually transmitted infection (STI) 7. Overdiagnosis of urinary tract infection (UTI) was not only a common cause of unnecessary antibiotic use but also contributed to the underdiagnosis of sexually transmitted infection, since 64% of the patients with a missed sexually transmitted infection were diagnosed as having a UTI instead 8.
In this retrospective review of 1,052 women testing positive for Neisseria gonorrhoeae, Chlamydia trachomatis, and/or Trichomonas vaginalis over a five-year period at a large metropolitan emergency department, the authors found that of the cases with pyuria, 74% of those were sterile pyuria 9. That study found a very low overall incidence of positive urine cultures (9.6%) in the setting of women with positive sexually transmitted infections (STIs). Of the patients with pyuria, patients with culture-positive urines vs. culture-negative urines had identical ranges of urine leukocytes (6–100 leukocytes per high-power field), but the mean leukocytes were higher in the culture-positive group (33.842 versus 24.034 leukocytes per high-power field) 9. The same study found that of the 295 patients with confirmed sexually transmitted infections (STIs) who were also prescribed an antibiotic for a presumed UTI, 66% of those were unnecessary, as they had negative urine cultures 9.
Sterile pyuria
Patients who routinely have greater than 20 leukocytes per microlitre, but have no bacteria in urine, are said to have sterile pyuria 10.
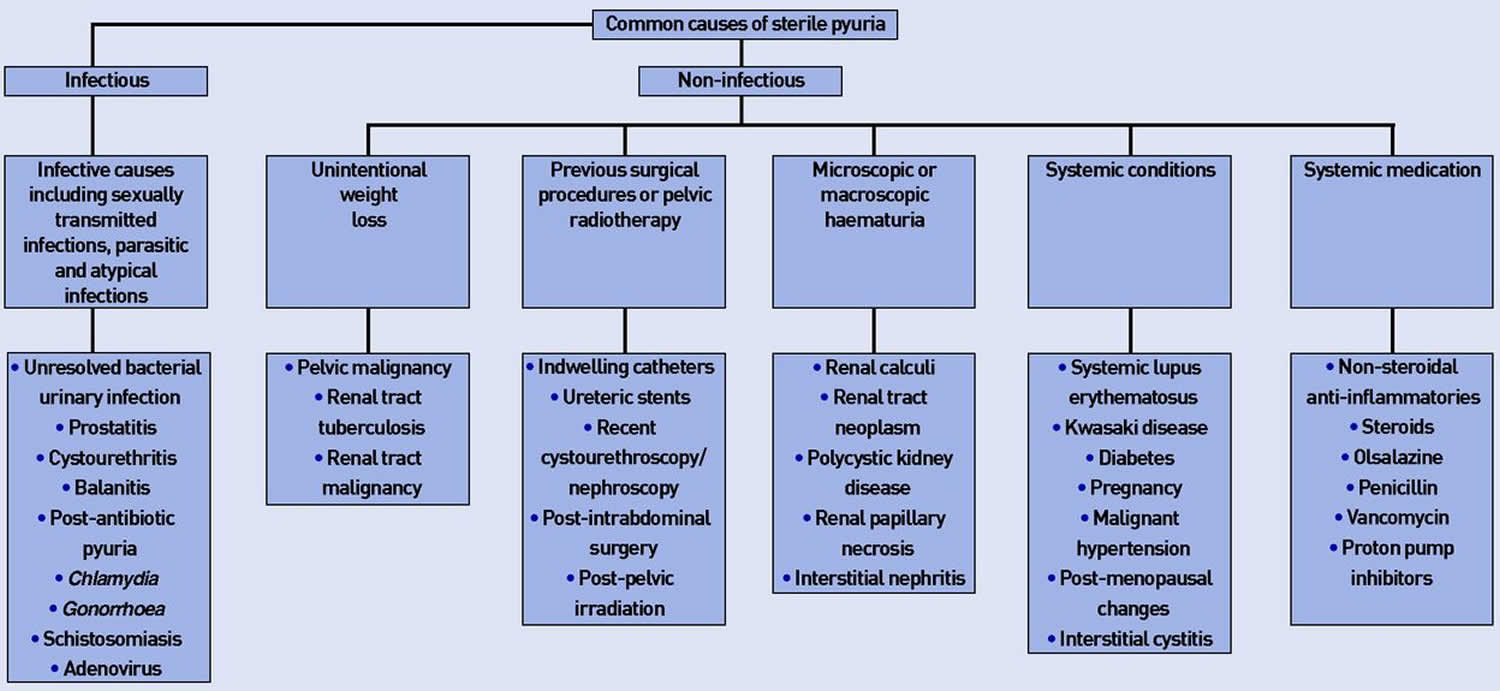
Sterile pyuria causes
Sterile pyuria has been linked to a number of causes including sexually transmitted diseases (STDs), tuberculosis (TB), interstitial cystitis, chlamydia, carcinoma in situ of the bladder and cystitis 11.
Genitourinary tuberculosis
Sterile pyuria may also be associated with urinary tract infections such as genitourinary tuberculosis 12. Genitourinary tuberculosis (TB) is seen in approximately 30% of extrapulmonary tuberculosis (TB) cases and is usually the result of dissemination from pulmonary disease 13. Sterile pyuria can be present in up to 46% of males with genitourinary tuberculosis (TB) 14. This has a higher prevalence in the setting of immunosuppression such as in human immunodeficiency virus (HIV) or organ transplant recipients 13. Genitourinary tuberculosis (TB) is difficult to recognize, as bacterial urine culture media are less favorable for mycobacterial growth 13. The gold standard for diagnosis of genitourinary tuberculosis is acid-fast bacilli (AFB) urine culture, which has a 37–79% sensitivity rate. However, this test can take up to 8 weeks for a result. Newer polymerase chain reaction (PCR) techniques have variable sensitivity (25–93 %), with high specificity (95–100%) 13. Overall however, PCR for genitourinary tuberculosis is a rapid, sensitive, specific diagnostic method and avoids a delay in treatment 15.
Radiological findings may direct a diagnosis towards renal tuberculosis. The genitourinary site is the most common site of extrapulmonary tuberculosis 12. Patients may present with dysuria, frequency, microscopic haematuria, flank pain and sterile pyuria 12. Systemic symptoms tend to be less common 12. Radiological evidence of this is present in <50% of patients with renal tuberculosis 12. Computerized tomography (CT) is helpful in renal tuberculosis and is the most sensitive method for identifying renal calcification, which occurs in approximately 40–70% of renal tuberculosis cases 12. Other CT features include various patterns of hydronephrosis, stricture or scarring. Ultrasonography is less sensitive than CT in the evaluation of urogenital tuberculosis 12. The definitive diagnosis still rests on microbiological tests such as finding acid-fast bacilli (AFB) in the urine, urine culture, tissue biopsy and polymerase chain reaction (PCR) for Mycobacterium tuberculosis. Polymerase chain reaction (PCR) for Mycobacterium tuberculosis is a rapid, sensitive, and specific diagnostic method, and avoids a delay in treatment. Polymerase chain reaction (PCR) is recommended for instant diagnosis and screening before further examination 16.
Patients are treated by antituberculous combination drugs, with or without percutaneous nephrostomy. If required, nephrectomy with poor response to isolated medical therapy occurs.
Sterile pyuria may also be the only sign of prostatic tuberculosis. Because the prostate is at the external sphincter, the classic clue of sterile pyuria is only helpful when collected properly using the ‘4 Glass Test’ 17. Prostate massage yields secretions which can be sent for AFB culture; however, only 36% of such cases are positive and thus PCR evaluation may be necessary [Schnack et al. 2014]. Utilizing a ‘provocation test’ may increase the diagnostic yield by 16% 17. Transrectal ultrasound can also be helpful in detection if irregular hyperechoic lesions are found at the periphery of the gland 17.
Sexually transmitted diseases
One of the causes of sterile pyuria may be sexually transmitted diseases (STDs). Young sexually active patients may undergo culture for organisms such as Chlamydia trachomatis. This can cause 10% of cases of sterile pyuria 10. The nucleic acid test (NAT) test is considered the gold standard for diagnosis of C. trachomatis [Matthews et al. 1990], but it has been shown to be only 70% effective at picking up this organism. An enzyme-linked immunosorbent assay (ELISA), however, tends to have 100% sensitivity. Additionally, urinary tract infections may be further investigated by flexible cystoscopy, including those patients with sterile pyuria.
However, the most likely cause of sterile pyuria is recent or incomplete antibiotic use 13. Negative urine cultures can also been seen with atypical infections such as Chlamydia and Ureaplasma species 13. Chlamydia trachomatis was detected in 10% of patients with sterile pyuria, Ureaplasma urealyticum in (5%), Mycoplasma hominis in (3%) and Mycoplasma genitalium in (1%) 18. PCR testing of sterile pyuria showed a significant number of C. trachomatis, Mycoplasma and Ureaplasma infections. Consequently, PCR is recommended for the detection of those microorganisms in urine samples 18.
Rarer causes of sterile pyuria include antiretrovirals. Indinavir therapy is associated with a continuum of crystal-related syndromes including nephrolithiasis, renal colic, flank pain without recognizable stone formation, dysuria and asymptomatic crystalluria 19. The mean duration of indinavir treatment, until sterile pyuria occurred, was 22 weeks 19. Sterile pyuria in patients taking indinavir may help to identify patients being at risk for nephrotoxicity 19.
Renal tract stones
In addition, urinary tract infections need to be excluded when urinalysis and an imaging study show sterile pyuria and calcifications, hypercalcaemia, hypercalciuria, primary hyperparathyroidism, sarcoidosis and diuretics abuse 20. Sterile pyuria may also be a sign of staghorn calculi 21.
Alkaline-encrusted pyelitis is a urinary tract infection characterized by encrustations in the wall of the urinary tract 22. It is caused by fastidious growing urea splitting microorganisms, mainly Corynebacterium group D2. The diagnosis should be evoked on the basis of sterile pyuria, alkaline urine pH and calcifications of the urinary excretion ways on the CT scan, and then confirmed by prolonged culture 22.
Intra-abdominal infections
Additionally, sterile pyuria can be a sign of intra-abdominal infection unrelated to the urinary tract. In patients with abdominal pain, pyuria is often found and attributed to a urinary tract infection 23. The sterile pyuria rate in acute appendicitis was found to be 87.5%, while the sterile pyuria rate in acute diverticulitis was 72.7% 23. In both appendicitis and diverticulitis, pyuria was significantly more common in females 23. In acute appendicitis, pyuria was also more likely in older patients 23. Pyuria was more common in women and in patients with gynecological infections 24. Sterile pyuria can also be a sign of upper tract transitional cell carcinoma 25.
Kawasaki’s disease and autoimmune diseases
Although Kawasaki’s disease is another disease which often presents with sterile pyuria, bacterial pyuria (urinary tract infection) occasionally occurs. Sterile pyuria in Kawasaki’s disease may originate from the urethra and/or from the kidney as a result of mild and subclinical renal injury possibly due to transcatheter urine 26. Positive and negative predictive values of sterile pyuria as a predictor of a urinary tract infection were 19% and 93.9%, respectively 27. However, pyuria was not always sterile in patients with Kawasaki’s disease. urinary tract infection should be considered and evaluated in Kawasaki’s disease patients with pyuria, a positive nitrite test or a positive result of urine culture. If a urinary tract infection is definitively diagnosed, the patient should be treated for a urinary tract infection as well as for Kawasaki’s disease and complete post-urinary tract infection workup is recommended. Although sterile pyuria with fever is often found in Kawasaki’s disease, before definitive symptoms of Kawasaki’s disease are found or pyuria is proved sterile, consideration of urinary tract infection is essential. Kawasaki’s disease should be one of the differential diagnoses in patients who are suspected of having a urinary tract infection and do not respond to antibiotic therapy, or who have negative urine culture 27.
Additionally sterile pyuria can be a manifestation of systemic lupus erythematosus (SLE); 23% of SLE patients had at least one episode of isolated sterile pyuria 28.
Medications
Drug intake is one of the forgotten yet common causes of sterile pyuria 29. Olsalazine and nitrofurantoin have been reported to cause sterile pyuria 30. The use of penicillin-based antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs) 31, aspirin, proton pump inhibitors (PPIs), and diuretics has also been involved in acute drug reactions, causing tubulointerstitial nephritis with an sterile pyuria.
Sterile pyuria diagnosis
First, urinalysis is the prime investigation for sterile pyuria 29. Importantly, sterile pyuria is not always sterile, so repeating cultures often yields a positive result on subsequent testing. Contamination, especially with vaginal leukocytes in females, is common, and samples should always be collected as a midstream clean catch. The use of antiseptic solutions prior to collection should be avoided to limit false-negative tests.
Practice nurses may also encounter a previously undiagnosed sterile pyuria during routine screening tests, or disease monitoring in patients with long-term conditions like diabetes. At this juncture, sending urine for culture and sensitivity is recommended, with onward advice to see their doctor for further investigation, pending results.
Second, routine hematological tests including a full blood count, renal, and liver function tests are of paramount importance. Swabs for Chlamydia and Gonorrhoea are recommended for sexually active patients. If urinary tuberculosis is suspected, three consecutive first-void morning samples are required for acid-fast bacilli and polymerase chain reaction (PCR) testing 32.
Eosinophilia is an important marker of drug-induced interstitial nephritis, but may also be seen in schistosomiasis. In suspected schistosomiasis, a terminal urine sample should be collected between noon and 3 pm, to coincide with maximal egg excretion.
Third, the choice of imaging modality depends on the history and findings on examination. A renal tract ultrasound scan or computerised tomography is recommended when renal stones, masses, or nephritis are differential diagnoses. Endourological procedures such as rigid or flexible cystourethroscopy and tissue sampling are undertaken if tumours are suspected, but they also have the advantage of diagnosing and treating benign pathologies such as bladder stones.
Figure 1. Sterile pyuria diagnostic algorithm
[Source 29 ]Pyuria causes
Urinary tract infections typically occur when bacteria enter the urinary tract through the urethra and begin to multiply in the bladder. Although the urinary system is designed to keep out such microscopic invaders, these defenses sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
The most common UTIs occur mainly in women and affect the bladder and urethra.
- Infection of the bladder (cystitis). This type of UTI is usually caused by Escherichia coli (E. coli), a type of bacteria commonly found in the gastrointestinal (GI) tract. However, sometimes other bacteria are responsible. Sexual intercourse may lead to cystitis, but you don’t have to be sexually active to develop it. All women are at risk of cystitis because of their anatomy — specifically, the short distance from the urethra to the anus and the urethral opening to the bladder.
- Infection of the urethra (urethritis). This type of UTI can occur when GI bacteria spread from the anus to the urethra. Also, because the female urethra is close to the vagina, sexually transmitted infections, such as herpes, gonorrhea, chlamydia and mycoplasma, can cause urethritis.
Sexually transmitted infections (STIs) are infections that are passed from one person to another through sexual contact. The causes of sexually transmitted infections (STIs) are bacteria, parasites, yeast, and viruses. There are more than 20 types of sexually transmitted infections (STIs), including
- Chlamydia
- Genital herpes
- Gonorrhea
- HIV/AIDS
- HPV
- Syphilis
- Trichomoniasis
An STI can be passed from one person to another through sexual contact, including vaginal, anal and oral sex. Sexually transmitted infections (STIs) can pass between men and women, and from women to women and men to men.
Most sexually transmitted infections affect both men and women, but in many cases the health problems they cause can be more severe for women. If a pregnant woman has an sexually transmitted infection (STI), it can cause serious health problems for the baby.
Antibiotics can treat sexually transmitted infections (STIs) caused by bacteria, yeast, or parasites. Some, such as HIV, have no cure, but can be treated to prevent them getting worse.
You cannot tell by looking at someone (including yourself) whether they have an sexually transmitted infection (STI), so it’s important to get a check-up if you have had unprotected sex or think you might be at risk.
Correct usage of latex condoms greatly reduces, but does not completely eliminate, the risk of catching or spreading sexually transmitted infections (STIs). The most reliable way to avoid infection is to not have anal, vaginal, or oral sex.
Risk factors for pyuria
Urinary tract infections are common in women, and many women experience more than one infection during their lifetimes. Risk factors specific to women for UTIs include:
- Female anatomy. A woman has a shorter urethra than a man does, which shortens the distance that bacteria must travel to reach the bladder.
- Sexual activity. Sexually active women tend to have more UTIs than do women who aren’t sexually active. Having a new sexual partner also increases your risk.
- Certain types of birth control. Women who use diaphragms for birth control may be at higher risk, as well as women who use spermicidal agents.
- Menopause. After menopause, a decline in circulating estrogen causes changes in the urinary tract that make you more vulnerable to infection.
Other risk factors for UTIs include:
- Urinary tract abnormalities. Babies born with urinary tract abnormalities that don’t allow urine to leave the body normally or cause urine to back up in the urethra have an increased risk of UTIs.
- Blockages in the urinary tract. Kidney stones or an enlarged prostate can trap urine in the bladder and increase the risk of UTIs.
A suppressed immune system. Diabetes and other diseases that impair the immune system — the body’s defense against germs — can increase the risk of UTIs. - Catheter use. People who can’t urinate on their own and use a tube (catheter) to urinate have an increased risk of UTIs. This may include people who are hospitalized, people with neurological problems that make it difficult to control their ability to urinate and people who are paralyzed.
- A recent urinary procedure. Urinary surgery or an exam of your urinary tract that involves medical instruments can both increase your risk of developing a urinary tract infection.
Pyuria prevention
You can take these steps to reduce your risk of urinary tract infections:
- Drink plenty of liquids, especially water. Drinking water helps dilute your urine and ensures that you’ll urinate more frequently — allowing bacteria to be flushed from your urinary tract before an infection can begin.
- Drink cranberry juice. Although studies are not conclusive that cranberry juice prevents UTIs, it is likely not harmful.
- Wipe from front to back. Doing so after urinating and after a bowel movement helps prevent bacteria in the anal region from spreading to the vagina and urethra.
- Empty your bladder soon after intercourse. Also, drink a full glass of water to help flush bacteria.
- Avoid potentially irritating feminine products. Using deodorant sprays or other feminine products, such as douches and powders, in the genital area can irritate the urethra.
- Change your birth control method. Diaphragms, or unlubricated or spermicide-treated condoms, can all contribute to bacterial growth.
How you can prevent sexually transmitted diseases:
- The most reliable way to avoid infection is to not have sex (i.e., anal, vaginal or oral).
- Reducing your number of sex partners can decrease your risk for STIs. It is still important that you and your partner get tested, and that you share your test results with one another.
- Correct and consistent use of the male latex condom is highly effective in reducing STI transmission. Use a condom every time you have anal, vaginal, or oral sex. If you have latex allergies, synthetic non-latex condoms can be used. But it is important to note that these condoms have higher breakage rates than latex condoms. Natural membrane condoms are not recommended for STI prevention.
- Vaccines are safe, effective, and recommended ways to prevent hepatitis B and HPV. HPV vaccines for males and females can protect against some of the most common types of HPV. It is best to get all three doses (shots) before becoming sexually active.
Pyuria symptoms
Urinary tract infections don’t always cause signs and symptoms, but when they do they may include:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing frequent, small amounts of urine
- Urine that appears cloudy
- Urine that appears red, bright pink or cola-colored — a sign of blood in the urine
- Strong-smelling urine
- Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
UTIs may be overlooked or mistaken for other conditions in older adults.
Each type of UTI may result in more-specific signs and symptoms, depending on which part of your urinary tract is infected.
Many people with sexually transmitted infections (STIs) do not get symptoms, so it’s worth getting tested even if you feel fine. If you think you have an STI, the earlier you’re tested, the sooner treatment can be given if it’s needed.
Table 1. Types of urinary tract infection
| Part of urinary tract affected | Signs and symptoms |
|---|---|
| Kidneys (acute pyelonephritis) |
|
| Bladder (cystitis) |
|
| Urethra (urethritis) |
|
Sexually transmitted disease (STD) symptoms
Many STIs have no signs or symptoms (asymptomatic). Even with no symptoms, however, you can pass the infection to your sex partners. So it’s important to use protection, such as a condom, during sex. And visit your doctor regularly for STI screening, so you can identify and treat an infection before you can pass it on.
Some of the following diseases, such as hepatitis, can also be transmitted without sexual contact, by coming into contact with an infected person’s blood. Others, such as gonorrhea, can only be transmitted through sexual contact.
Chlamydia symptoms
Chlamydia is a bacterial infection of your genital tract. Chlamydia may be difficult to detect because early-stage infections often cause few or no signs and symptoms. When they do occur, they usually start one to three weeks after you’ve been exposed to chlamydia. Even when signs and symptoms occur, they’re often mild and passing, making them easy to overlook.
Signs and symptoms may include:
- Painful urination
- Lower abdominal pain
- Vaginal discharge in women
- Discharge from the penis in men
- Pain during sexual intercourse in women
- Bleeding between periods in women
- Testicular pain in men
Gonorrhea symptoms
Gonorrhea is a bacterial infection of your genital tract. It can also grow in your mouth, throat, eyes and anus. The first gonorrhea symptoms generally appear within 10 days after exposure. However, some people may be infected for months before signs or symptoms occur.
Signs and symptoms of gonorrhea may include:
- Thick, cloudy or bloody discharge from the penis or vagina
- Pain or burning sensation when urinating
- Heavy menstrual bleeding or bleeding between periods
- Painful, swollen testicles
- Painful bowel movements
- Anal itching
Trichomoniasis symptoms
Trichomoniasis is a common STI caused by a microscopic, one-celled parasite called Trichomonas vaginalis. This organism spreads during sexual intercourse with someone who already has the infection.
The organism usually infects the urinary tract in men, but often causes no symptoms. Trichomoniasis typically infects the vagina in women. When trichomoniasis causes symptoms, they may appear within five to 28 days of exposure and range from mild irritation to severe inflammation.
Signs and symptoms may include:
- Clear, white, greenish or yellowish vaginal discharge
- Discharge from the penis
- Strong vaginal odor
- Vaginal itching or irritation
- Itching or irritation inside the penis
- Pain during sexual intercourse
- Painful urination
HIV symptoms
HIV is an infection with the human immunodeficiency virus. HIV interferes with your body’s ability to fight off viruses, bacteria and fungi that cause illness, and it can lead to AIDS, a chronic, life-threatening disease.
When first infected with HIV, you may have no symptoms. Some people develop a flu-like illness, usually two to six weeks after being infected. Still, the only way you know if you have HIV is to be tested.
Early signs and symptoms of HIV
Early HIV signs and symptoms may include:
- Fever
- Headache
- Sore throat
- Swollen lymph glands
- Rash
- Fatigue
These early signs and symptoms usually disappear within a week to a month and are often mistaken for those of another viral infection. During this period, you’re highly infectious. More-persistent or -severe symptoms of HIV infection may not appear for 10 years or more after the initial infection.
As the virus continues to multiply and destroy immune cells, you may develop mild infections or chronic signs and symptoms such as:
- Swollen lymph nodes — often one of the first signs of HIV infection
- Diarrhea
- Weight loss
- Fever
- Cough and shortness of breath
Late-stage HIV infection
Signs and symptoms of late-stage HIV infection include:
- Persistent, unexplained fatigue
- Soaking night sweats
- Shaking chills or fever higher than 100.4 F (38 C) for several weeks
- Swelling of lymph nodes for more than three months
- Chronic diarrhea
- Persistent headaches
- Unusual, opportunistic infections
Genital herpes symptoms
Highly contagious, genital herpes is caused by a type of the herpes simplex virus (HSV) that enters your body through small breaks in your skin or mucous membranes. Most people with HSV never know they have it, because they have no signs or symptoms or the signs and symptoms are so mild they go unnoticed.
When signs and symptoms are noticeable, the first episode is generally the worst. Some people never have a second episode. Others, however, can have recurrent episodes for decades.
When present, genital herpes signs and symptoms may include:
- Small red bumps, blisters (vesicles) or open sores (ulcers) in the genital, anal and nearby areas
- Pain or itching around the genital area, buttocks and inner thighs
The initial symptom of genital herpes usually is pain or itching, beginning within a few weeks after exposure to an infected sexual partner. After several days, small red bumps may appear. They then rupture, becoming ulcers that ooze or bleed. Eventually, scabs form and the ulcers heal.
In women, sores can erupt in the vaginal area, external genitals, buttocks, anus or cervix. In men, sores can appear on the penis, scrotum, buttocks, anus or thighs, or inside the tube from the bladder through the penis (urethra).
Ulcers can make urination painful. You may also have pain and tenderness in your genital area until the infection clears. During an initial episode, you may have flu-like signs and symptoms, such as a headache, muscle aches and fever, as well as swollen lymph nodes in your groin.
In some cases, the infection can be active and contagious even when sores aren’t present.
Human papillomavirus (HPV) infection and genital warts symptoms
HPV infection is one of the most common types of STIs. Some forms put women at high risk of cervical cancer. Other forms cause genital warts. HPV usually has no signs or symptoms. The signs and symptoms of genital warts include:
- Small, flesh-colored or gray swellings in your genital area
- Several warts close together that take on a cauliflower shape
- Itching or discomfort in your genital area
- Bleeding with intercourse
Often, however, genital warts cause no symptoms. Genital warts may be as small as 1 millimeter in diameter or may multiply into large clusters.
In women, genital warts can grow on the vulva, the walls of the vagina, the area between the external genitals and the anus, and the cervix. In men, they may occur on the tip or shaft of the penis, the scrotum, or the anus. Genital warts can also develop in the mouth or throat of a person who has had oral sex with an infected person.
Hepatitis symptoms
Hepatitis A, hepatitis B and hepatitis C are all contagious viral infections that affect your liver. Hepatitis B and C are the most serious of the three, but each can cause your liver to become inflamed.
Some people never develop signs or symptoms. But for those who do, signs and symptoms may occur several weeks after exposure and may include:
- Fatigue
- Nausea and vomiting
- Abdominal pain or discomfort, especially in the area of your liver on your right side beneath your lower ribs
- Loss of appetite
- Fever
- Dark urine
- Muscle or joint pain
- Itching
- Yellowing of your skin and the whites of your eyes (jaundice)
Syphilis symptoms
Syphilis is a bacterial infection. The disease affects your genitals, skin and mucous membranes, but it can also involve many other parts of your body, including your brain and your heart.
The signs and symptoms of syphilis may occur in four stages — primary, secondary, latent and tertiary. There’s also a condition known as congenital syphilis, which occurs when a pregnant woman with syphilis passes the disease to her unborn infant. Congenital syphilis can be disabling, even life-threatening, so it’s important for a pregnant woman with syphilis to be treated.
Primary syphilis
The first sign of syphilis, which may occur from 10 days to three months after exposure, may be a small, painless sore (chancre) on the part of your body where the infection was transmitted, usually your genitals, rectum, tongue or lips. A single chancre is typical, but there may be multiple sores.
The sore typically heals without treatment, but the underlying disease remains and may reappear in the second (secondary) or third (tertiary) stage.
Secondary syphilis
Signs and symptoms of secondary syphilis may begin three to six weeks after the chancre appears, and may include:
- Rash marked by red or reddish-brown, penny-sized sores over any area of your body, including your palms and soles
- Fever
- Enlarged lymph nodes
- Fatigue and a vague feeling of discomfort
- Soreness and aching
These signs and symptoms may disappear without treatment within a few weeks or repeatedly come and go for as long as a year.
Latent syphilis
In some people, a period called latent syphilis — in which no symptoms are present — may follow the secondary stage. Signs and symptoms may never return, or the disease may progress to the tertiary stage.
Tertiary syphilis
Without treatment, syphilis bacteria may spread, leading to serious internal organ damage and death years after the original infection.
Some of the signs and symptoms of tertiary syphilis include:
- Lack of coordination
- Numbness
- Paralysis
- Blindness
- Dementia
Neurosyphilis
At any stage, syphilis can affect the nervous system. Neurosyphilis may cause no signs or symptoms, or it can cause:
- Headache
- Behavior changes
- Movement problems
If you suspect you have an STI, see your doctor
If you suspect you have these or other STIs or that you may have been exposed to one, see your doctor for testing. Timely diagnosis and treatment are important to avoid or delay more-severe, potentially life-threatening health problems and to avoid infecting others.
Pyuria complications
When treated promptly and properly, lower urinary tract infections rarely lead to complications. But left untreated, a urinary tract infection can have serious consequences.
Complications of a UTI may include:
- Recurrent infections, especially in women who experience two or more UTIs in a six-month period or four or more within a year.
- Permanent kidney damage from an acute or chronic kidney infection (pyelonephritis) due to an untreated UTI.
- Increased risk in pregnant women of delivering low birth weight or premature infants.
- Urethral stricture (narrowing of the urethra) in men from recurrent urethritis, previously seen with gonococcal urethritis.
- Sepsis, a potentially life-threatening complication of an infection, especially if the infection works its way up your urinary tract to your kidneys.
Pyuria diagnosis
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample. Your doctor may ask for a urine sample for lab analysis to look for white blood cells, red blood cells or bacteria. To avoid potential contamination of the sample, you may be instructed to first wipe your genital area with an antiseptic pad and to collect the urine midstream.
- Growing urinary tract bacteria in a lab. Lab analysis of the urine is sometimes followed by a urine culture. This test tells your doctor what bacteria are causing your infection and which medications will be most effective.
- Creating images of your urinary tract. If you are having frequent infections that your doctor thinks may be caused by an abnormality in your urinary tract, you may have an ultrasound, a computerized tomography (CT) scan or magnetic resonance imaging (MRI). Your doctor may also use a contrast dye to highlight structures in your urinary tract.
- Using a scope to see inside your bladder. If you have recurrent UTIs, your doctor may perform a cystoscopy, using a long, thin tube with a lens (cystoscope) to see inside your urethra and bladder. The cystoscope is inserted in your urethra and passed through to your bladder.
Pyuria treatment
Antibiotics usually are the first line treatment for urinary tract infections. Which drugs are prescribed and for how long depend on your health condition and the type of bacteria found in your urine.
Urinary tract infections can be painful, but you can take steps to ease your discomfort until antibiotics treat the infection. Follow these tips:
- Drink plenty of water. Water helps to dilute your urine and flush out bacteria.
- Avoid drinks that may irritate your bladder. Avoid coffee, alcohol, and soft drinks containing citrus juices or caffeine until your infection has cleared. They
- can irritate your bladder and tend to aggravate your frequent or urgent need to urinate.
- Use a heating pad. Apply a warm, but not hot, heating pad to your abdomen to minimize bladder pressure or discomfort.
Many people drink cranberry juice to prevent UTIs. There’s some indication that cranberry products, in either juice or tablet form, may have infection-fighting properties. Researchers continue to study the ability of cranberry juice to prevent UTIs, but results are not conclusive.
If you enjoy drinking cranberry juice and feel it helps you prevent UTIs, there’s little harm in it. For most people, drinking cranberry juice is safe, but some people report an upset stomach or diarrhea.
However, don’t drink cranberry juice if you’re taking blood-thinning medication, such as warfarin.
Simple infection
Drugs commonly recommended for simple UTIs include:
- Trimethoprim/sulfamethoxazole (Bactrim, Septra, others)
- Fosfomycin (Monurol)
- Nitrofurantoin (Macrodantin, Macrobid)
- Cephalexin (Keflex)
- Ceftriaxone
The group of antibiotic medicines known as fluoroquinolones — such as ciprofloxacin (Cipro), levofloxacin (Levaquin) and others — isn’t commonly recommended for simple UTIs, as the risks of these medicines generally outweigh the benefits for treating uncomplicated UTIs. In some cases, such as a complicated UTI or kidney infection, your doctor might prescribe a fluoroquinolone medicine if no other treatment options exist.
Often, symptoms clear up within a few days of treatment. But you may need to continue antibiotics for a week or more. Take the entire course of antibiotics as prescribed.
For an uncomplicated UTI that occurs when you’re otherwise healthy, your doctor may recommend a shorter course of treatment, such as taking an antibiotic for one to three days. But whether this short course of treatment is enough to treat your infection depends on your particular symptoms and medical history.
Your doctor may also prescribe a pain medication (analgesic) that numbs your bladder and urethra to relieve burning while urinating, but pain usually is relieved soon after starting an antibiotic.
Frequent infections
If you have frequent UTIs, your doctor may make certain treatment recommendations, such as:
- Low-dose antibiotics, initially for six months but sometimes longer
- Self-diagnosis and treatment, if you stay in touch with your doctor
- A single dose of antibiotic after sexual intercourse if your infections are related to sexual activity
- Vaginal estrogen therapy if you’re postmenopausal
Severe infection
For a severe UTI, you may need treatment with intravenous antibiotics in a hospital.
- Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 Months. Pediatrics Sep 2011, 128 (3) 595-610; DOI: 10.1542/peds.2011-1330 http://pediatrics.aappublications.org/content/128/3/595.long[↩]
- Hoberman A, Wald ER, Reynolds EA, Penchansky L, Charron M. Is urine culture necessary to rule out urinary tract infection in young febrile children? Pediatr Infect Dis J. 1996;15(4):304–309[↩]
- Forster CS, Haslam DB, Jackson E, Goldstein SL. Utility of a routine urinalysis in children who require clean intermittent catheterization. J Pediatr Urol. 2017;13(5): 488.e1–488.e5[↩]
- Hooton TM, Bradley SF, Cardenas DD, et al. ; Infectious Diseases Society of America. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663[↩]
- Prentiss KA, Newby PK, Vinci RJ. 2011. Adolescent female with urinary symptoms. a diagnostic challenge for the pediatrician. Pediatr Emerg Care 27:789–794. doi:10.1097/PEC.0b013e31822c10f6[↩]
- Centers for Disease Control and Prevention. 2013. Sexually transmitted disease surveillance 2012. Centers for Disease Control and Prevention, Atlanta, GA https://www.cdc.gov/std/stats/[↩]
- Wilbanks MD, Galbraith JW, Geisler WM. 2014. Dysuria in the emergency department: missed diagnosis of Chlamydia trachomatis. West J Emerg Med 15:227–230. doi:10.5811/westjem.2013.12.18989[↩]
- Tomas ME, Getman D, Donskey CJ, Hecker MT. Overdiagnosis of Urinary Tract Infection and Underdiagnosis of Sexually Transmitted Infection in Adult Women Presenting to an Emergency Department. J Clin Microbiol. 2015;53(8):2686-92. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4508438/[↩]
- Shipman SB, Risinger CR, Evans CM, Gilbertson CD, Hogan DE. High Prevalence of Sterile Pyuria in the Setting of Sexually Transmitted Infection in Women Presenting to an Emergency Department. West J Emerg Med. 2018;19(2):282-286. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851500/[↩][↩][↩]
- Sterile pyuria and Chlamydia trachomatis. Matthews RS, Bonigal SD, Wise R. Lancet. 1990 Aug 11; 336(8711):385.[↩][↩]
- Goonewardene S, Persad R. Sterile pyuria: a forgotten entity. Ther Adv Urol. 2015;7(5):295-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4549703/[↩]
- The case | Sterile pyuria and an abnormal abdominal film. “Autonephrectomy” of right kidney. Lin YL, Fan YC, Cheng CY, Sue YM, Hsu YH, Hou CC, Chen TH, Chen TW. Kidney Int. 2008 Jan; 73(1):131-3.[↩][↩][↩][↩][↩][↩][↩]
- Newby C., Barhaghi K., Maylin M. (2014) Sterile pyuria – a classic tale with a modern twist. J Gen Intern Med 29: S438–S439.[↩][↩][↩][↩][↩][↩]
- Garcia-Tello A., Cacho J., Hernandez E., Palou J., Sanchez-Chapado M., Mavric H. (2010) Descriptive analysis of a series of male genital tuberculosis with emphasis on diagnostic and therapeutic data. Eur Urol 9: 173.[↩]
- Ahmad M., Ullah S. (2011) Role of polymerase chain reaction in diagnosing urinary bladder tuberculosis. J Urol 1: e473.[↩]
- Ahmed S., Begum S., Hannan A., Sarker K., Ira A. (1999) Renal tuberculosis: report of two cases. Bangladesh Renal J 18: 53–57.[↩]
- Schnack J., Mittal A., Chang C. (2014) Prostatic tuberculosis: a rare cause of Fournier’s gangrene. Chest 145(3 Meeting Abstracts): 128A.[↩][↩][↩]
- Detection of Chlamydia trachomatis and Mycoplasma hominis, genitalium and Ureaplasma urealyticum by polymerase chain reaction in patients with sterile pyuria. Nassar FA, Abu-Elamreen FH, Shubair ME, Sharif FA. Adv Med Sci. 2008; 53(1):80-6.[↩][↩]
- Pyuria in patients treated with indinavir is associated with renal dysfunction. Sarcletti M, Petter A, Romani N, Lhotta K, König P, Maier H, Zangerle R. Clin Nephrol. 2000 Oct; 54(4):261-70.[↩][↩][↩]
- Transition of overlooked sterile pyuria. Hwang HP, Lee HB, Kang KP, Kim W, Park SK, Lee S. Nephrology (Carlton). 2013 Nov; 18(11):744-5.[↩]
- Staghorn calculus presenting as sterile pyuria. Rowen D, Carne CA, Sonnex C. Genitourin Med. 1992 Dec; 68(6):403-4.[↩]
- Alkaline-encrusted pyelitis and cystitis: an easily missed and life-threatening urinary infection. Lieten S, Schelfaut D, Wissing KM, Geers C, Tielemans C. BMJ Case Rep. 2011 Mar 29; 2011.[↩][↩]
- Chan V., Dorfman M., Chan S. (2014) Sterile pyuria in acute appendicitis and diverticulitis. Acad Emerg Med 21(Suppl. S1): S206.[↩][↩][↩][↩]
- Sterile pyuria in patients admitted to the hospital with infections outside of the urinary tract. Hooker JB, Mold JW, Kumar S. J Am Board Fam Med. 2014 Jan-Feb; 27(1):97-103.[↩]
- Upper tract urothelial cell carcinoma presenting as fever of unknown origin and acid-sterile pyuria. Di Capua M, Ieranò P, Marrone E, Cerbone AM, Di Minno G. Intern Emerg Med. 2012 Sep; 7 Suppl 2():S117-8.[↩]
- Sterile pyuria in patients with Kawasaki disease originates from both the urethra and the kidney. Watanabe T, Abe Y, Sato S, Uehara Y, Ikeno K, Abe T. Pediatr Nephrol. 2007 Jul; 22(7):987-91.[↩]
- Sterile pyuria in Kawasaki disease. Wirojanan J, Sopontammarak S, Vachvanichsanong P. Pediatr Nephrol. 2004 Mar; 19(3):363.[↩][↩]
- Significance of isolated hematuria and isolated pyuria in systemic lupus erythematosus. Rahman P, Gladman DD, Ibanez D, Urowitz MB. Lupus. 2001; 10(6):418-23.[↩]
- Sterile pyuria: a practical management guide. Peter Glen, Akash Prashar, Amr Hawary. Br J Gen Pract 2016; 66 (644): e225-e227. DOI: 10.3399/bjgp16X684217 https://bjgp.org/content/66/644/e225[↩][↩][↩]
- Dieter RS. (2000) Sterile pyuria: a differential diagnosis. Compr Ther 26(3):150–152.[↩]
- Rossert J. (2001) Drug-induced acute interstitial nephritis. Kidney Int 60(2):804–817.[↩]
- Nassar FA, Abu-Elamreen FH, Shubair ME, Sharif FA. (2008) Detection of Chlamydia trachomatis and Mycoplasma hominis, genitalium and Ureaplasma urealyticum by polymerase chain reaction in patients with sterile pyuria. Adv Med Sci 53(1):80–86.[↩]