Contents
What is rapid eye movement sleep
Sleep is a reversible state of disconnection from the environment including reduced consciousness, skeletal muscle mobility, and metabolism 1. All forms of sensory responses are markedly decreased to varying degrees depending on the sleep cycle stage. Although this phenomenon is observed in all species that have been studied and occupies a significant fraction of the human lifespan, the purpose and function of sleep, particularly rapid eye movement (REM) sleep remain poorly understood 2.
Sleep is measured primarily by polysomnography which is considered the gold standard for diagnosing sleep disorders 2. Polysomnography reveals that sleep architecture has several distinct stages that vacillate between the non-rapid eye movement (NREM) stages and rapid eye movement (REM) stages 1. The rapid eye movement (REM) stage is of particular interest due to its association with a wide variety of pathological, psychological, and physiological phenomenon.
The hallmark of sleep physiology is the sleep-wake cycle in which a person vacillates between non-rapid eye movement (NREM) stages and rapid eye movement (REM) sleep throughout the night. The switches between non-rapid eye movement (NREM) stages and rapid eye movement (REM) sleep are controlled by reciprocal inhibition of monoaminergic and cholinergic neurons 1. Cholinergic neurons become highly active during REM. This increase in cholinergic activity is accompanied by a drastic decrease in adrenergic and serotonergic neuron activity and is reversed in NREM sleep. This results in the series of distinct stages of differing wakefulness levels that characterize the different stages of normal sleep.
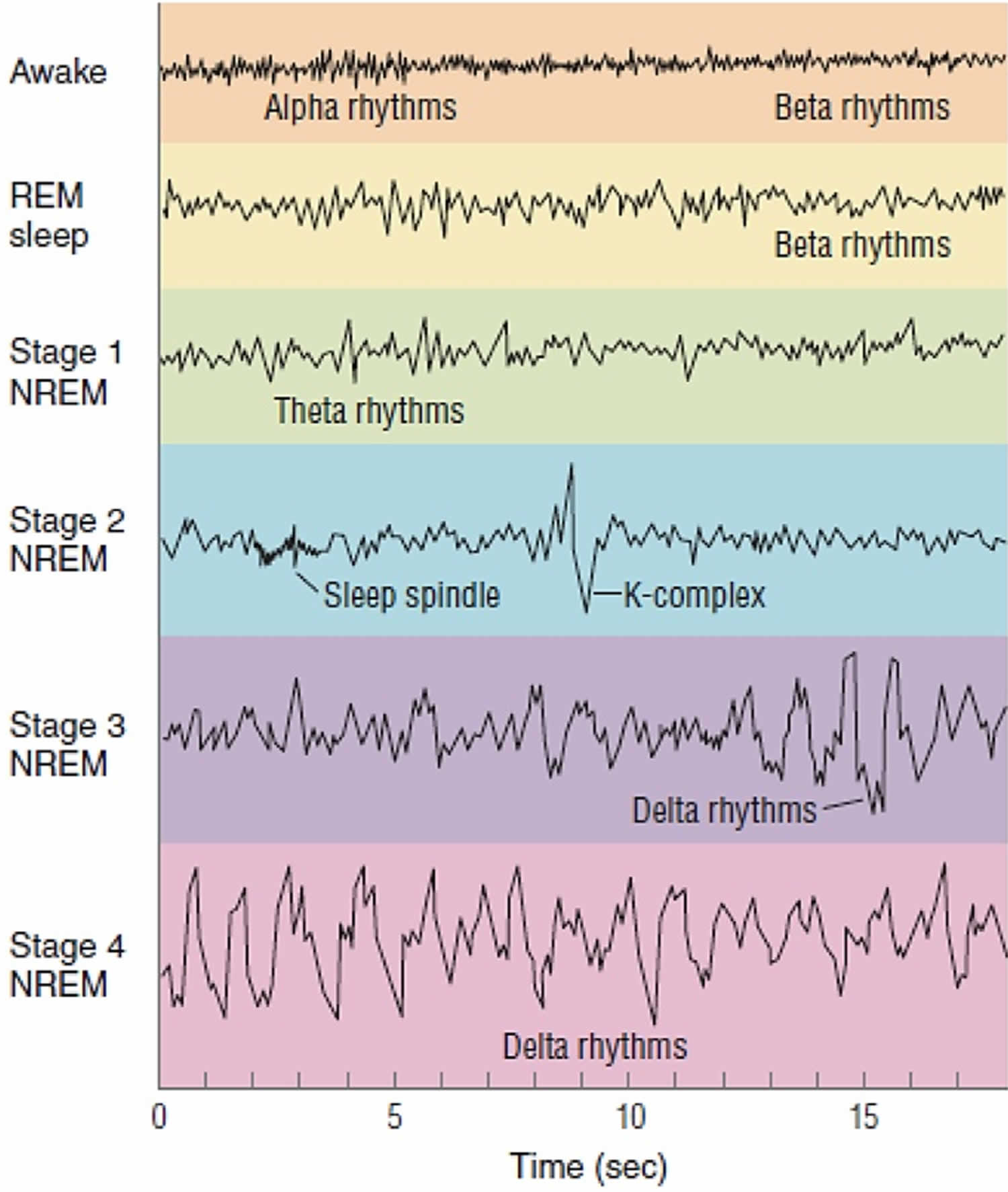
Polysomnogram is used to identify the 3 stages of non-rapid eye movement (NREM) sleep (N1-N3) and rapid eye movement (REM) sleep by measuring specific EEG waveform rhythms and events outlined briefly below 3:
- Alert wakefulness: low-amplitude mixed frequency electroencephalogram (EEG)
- Drowsy wakefulness: alpha waves with 8 to 13 Hz peaks
- N1 stage: 4 to 7 Hz Theta waves (sawtooth)
- N2 stage: 11 to 16 Hz spindles (bursts of waves) and 0.5 to 2 Hz K-complexes (biphasic waves)
- N3 stage: 0.5 to 3 Hz Delta waves (large and slow)
- Rapid eye movement (REM) sleep (stage R): theta waves or wave-like patterns
The onset of sleep begins with wakefulness and progresses rapidly to rapid eye movement (REM) sleep by approximately 60 to 90 minutes 3. This is followed by cyclical alterations between rapid eye movement (REM) and non-rapid eye movement (NREM) every 90 to 120 minutes until awakening. Most rapid eye movement (REM) sleep occurs during the second half of the night, with NREM sleep dominating the first half of the night.
A variety of parameters are used to measure rapid eye movement (REM) sleep including time to onset, length of the rapid eye movement (REM) stage, and amount of eye movement that occurs during rapid eye movement (REM) 3. Rapid eye movement (REM) latency refers to the amount of time that elapses between the onset of sleep to the first REM stage. Rapid eye movement (REM) density refers to the number of eye movements during REM sleep, and changes have been associated with sleep deprivation and depression.
Sleep architecture is influenced by two separate processes: process S and process C 4. Process S is also called the “homeostatic sleep drive” and increases in activity with each hour spent awake. Process C refers to the circadian rhythm and is responsible for maintaining appropriate sleep/wake cycles by promoting sleep during the night and wakefulness during the day. This drive increases throughout the day until bedtime when it begins to decline in order to promote sleep consolidation.
Over 50 million Americans suffer from sleep loss, which is defined as sleep duration less than the average of 7 to 8 hours per night 5. Acute and chronic sleep loss results in a wide variety of detrimental consequences. Acute sleep loss results in a number of deleterious symptoms including daytime somnolence diminished memory and hampered concentration. Chronic sleep loss has been consistently associated with an increased risk of serious diseases including diabetes, obesity, and depression. Moreover, sleep deprivation is associated with significantly increased cardiovascular disease including hypertension, heart attack, and stroke 5. Sleep disorders are readily treatable and are an important factor in the comprehensive care of patients.
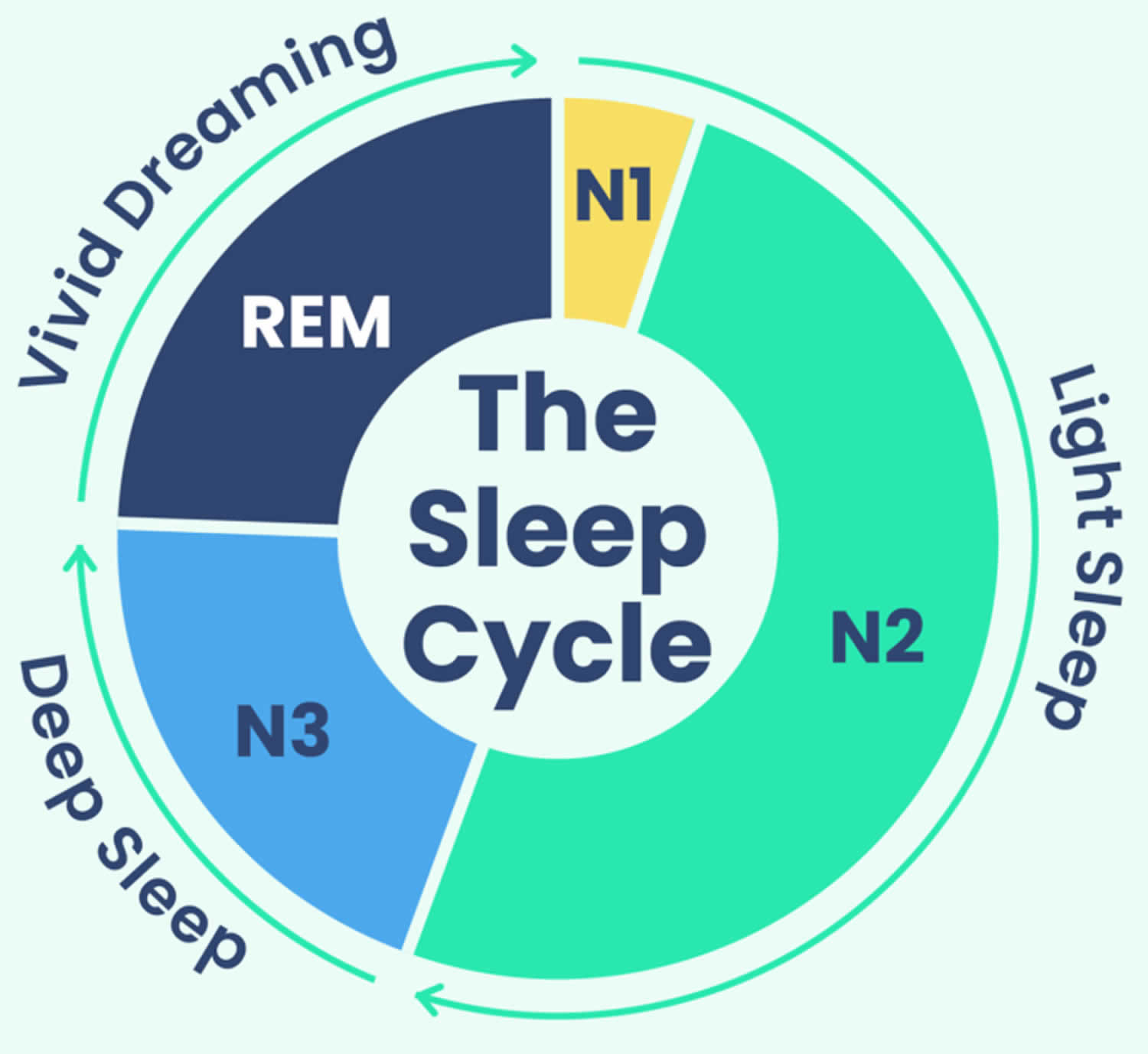
Sleep Stages
Sleep occurs in 2 main phases, Non-Rapid Eye Movement (NREM) sleep, which has three stages (N1, N2, and N3), and Rapid Eye Movement (REM) sleep 6. Each sleep phase and stage of sleep includes variations in muscle tone, brain wave patterns, and eye movements. Your body cycles through all stages approximately 4 to 6 times each night, averaging 90 minutes for each cycle 7. Each sleep stage serves different functions, from the light transition into sleep (N1), to the restorative deep sleep (N3) and the active dreaming of REM sleep.
- Stage 1 (N1 or light sleep) is the lightest stage of sleep and occurs as a person first falls asleep. This brief stage is when your drowsiness gives way to falling asleep. Your heartbeat and breathing start to slow down, but it’s still pretty easy to wake you up during this stage. Average length 1 to 7 minutes.
- Stage 2 (N2 or intermediate sleep) is where the body starts to relax more deeply. Your body temperature drops, your muscles relax, and your breathing and heart rate slow even more. Average length 10 to 25 minutes.
- Stage 3 (N3 or deep sleep) is the deepest and more restorative sleep, allowing your body to recover and grow. In stage 3 sleep, your breathing and pulse are slow and steady. Average length 20 to 40 minutes.
- Stage 4 (REM Sleep) is where most dreaming occurs, brain activity increases almost as if you were awake, and your muscles become temporarily paralyzed. Your heart rate and respiration speed up and become more erratic, and your eyes move quickly behind your eyelids. Dreams are most vivid during the REM stage. Average length 10 to 60 minutes.
Although the sleep stages are described numerically, you don’t always progress through them in this exact order. For example, in many sleep cycles, you transition from stage 3 sleep back to stage 2 sleep before beginning a period of REM sleep.
Sleep occurs in 5 stages: Wake, Non-Rapid Eye Movement (NREM) stage N1, then progress through N2 and N3, and after N3 you enter REM sleep 6. You then return to NREM stages, often starting again at N2. Throughout the night, the REM periods lengthen, and deep N3 sleep decreases, with most N3 sleep occurring in the first half of the night, with each stage leading to progressively deeper sleep. Approximately 75% of sleep is spent in the NREM (Non-Rapid Eye Movement) stages, with the majority spent in the N2 stage 10. A typical night’s sleep consists of 4 to 5 sleep cycles, with the progression of sleep stages in the following order: N1, N2, N3, N2, REM 11. A complete sleep cycle takes roughly 90 to 120 minutes. The first REM period is short, and as the night progresses, longer periods of REM and decreased time in deep sleep (NREM) occur 6. With each new cycle, you spend increasing amounts of time in REM sleep, so most of your REM sleep takes place in the second half of the night.
Sleep isn’t uniform. Sleep cycles can vary from person to person and from night to night based on a wide range of factors such as your age, recent sleep patterns, and alcohol consumption. Over the course of the night, you go through several rounds of the sleep cycle, which is composed of four stages. In a typical night, a person goes through four to six sleep cycles 6. Not all sleep cycles are the same length, but on average they last about 90 minutes each.
The first sleep cycle is often the shortest, ranging from 70 to 100 minutes, while later cycles tend to fall between 90 and 120 minutes. In addition, the composition of each cycle — how much time is spent in each phase of sleep — changes as the night goes along.
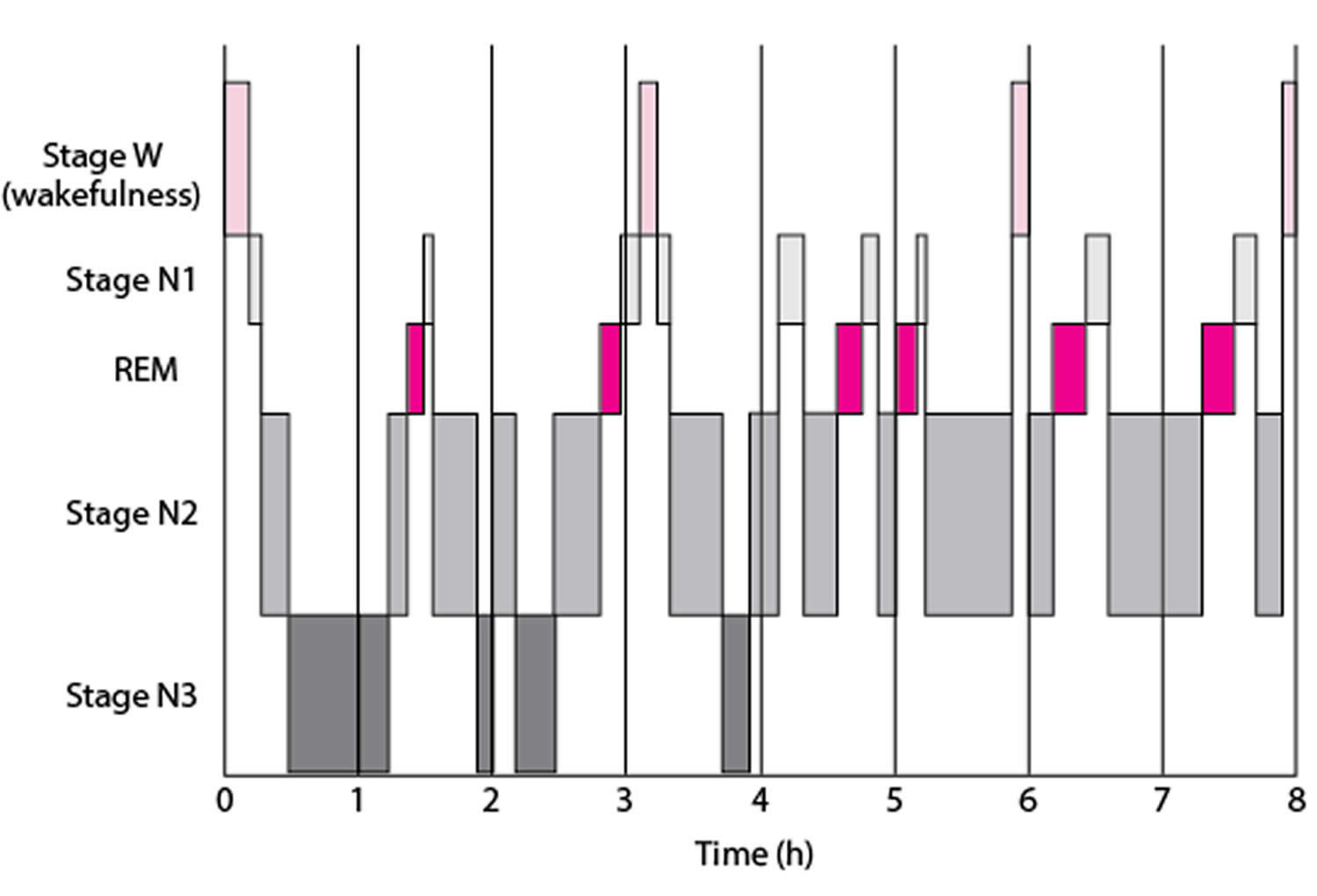
Figure 1. Sleep Stages
Footnotes: A sleep episode begins with a short period of NREM stage N1 progressing through stage N2, followed by stage N3 and finally to REM. However, individuals do not remain in REM sleep the remainder of the night but, rather, cycle between stages of NREM and REM throughout the night. NREM sleep constitutes about 75 to 80 percent of total time spent in sleep, and REM sleep constitutes the remaining 20 to 25 percent. The average length of the first NREM-REM sleep cycle is 70 to 100 minutes. The second, and later, cycles are longer lasting—approximately 90 to 120 minutes 12. In normal adults, REM sleep increases as the night progresses and is longest in the last one-third of the sleep episode. As the sleep episode progresses, stage 2 begins to account for the majority of NREM sleep, and stages 3 and 4 may sometimes altogether disappear.
[Source 8 ]Figure 2. Typical Sleep Pattern in Young Adults
Footnotes: Average times and sequences of sleep cycles during the night. Over the course of a period of sleep, NREM and REM sleep alternate cyclically. The function of alternations between these two types of sleep is not yet understood, but irregular cycling and/or absent sleep stages are associated with sleep disorders 13. For example, instead of entering sleep through NREM, as is typical, individuals with narcolepsy enter sleep directly into REM sleep 14. Rapid eye movement (REM) sleep occurs cyclically throughout the night every 90 to 120 minute. Brief periods of wakefulness (stage W) occur periodically. Sleep time is spent as follows:
- Stage N1: 2–5%
- Stage N2: 45–55%
- Stage N3: 13–23%
- REM: 20–25%
Figure 3. EEG activity of the four stages of sleep
Footnotes: EEG activity during wakefulness with eyes open and closed and during the different stages of sleep. Brainwave activity changes drastically over the course of the different stages of sleep. REM sleep brain activity most closely resembles brain activity while awake.
- Alpha activity is a smooth electrical activity of 8-12 Hz recorded from the brain; generally associated with a state of relaxation during wakefulness.
- Beta activity is a irregular electrical activity of 13-30 Hz recorded from the brain; generally associated with a state of alertness during wakefulness.
- Theta activity is EEG activity of 3.5-7.5 Hz that occurs intermittently during lighter stages of NREM sleep.
- Delta activity is a regular, synchronous electrical activity of less than 4 Hz recorded from the brain; occurs during the deepest stages of slow-wave sleep.
- Sleep spindle is a short burst of 12 to 14 cycle per-second waves observed during NREM sleep, decrease brain’s sensitivity to sensory input and keeps person asleep.
- K complex are single delta waves, sudden sharp wave forms, 1 per minute but can be triggered by noise.
Your sleep-wake cycle is regulated by the circadian rhythm (your body’s natural internal 24-hour clock that manages your sleep-wake cycle and other vital functions, like hormone release and body temperature, by synchronizing with the day-night cycle), which is driven by the suprachiasmatic nucleus (SCN) of the hypothalamus that acts as a “master clock” or “circadian pacemaker”, receiving light cues from your eyes to control the circadian rhythm 17, 18, 19. The circadian rhythm also controls the nocturnal release of adrenocorticotropic hormone (ACTH), prolactin, melatonin, and norepinephrine (NE) 20. External factors like light exposure, meal timing, and activity can influence the circadian rhythm, and disruptions to the circadian rhythm, such as from shift work or jet lag, can negatively affect your health.
The suprachiasmatic nucleus (SCN) of the hypothalamus receives input from nerve cells in the retina that detect light to regulate the circadian rhythm and sleep via multiple pathways that cause the nocturnal release of adrenocorticotropic hormone (ACTH), prolactin, melatonin, and norepinephrine 21. One of the most commonly recognized pathways by which this occurs is via the stimulation of norepinephrine release by the suprachiasmatic nucleus (SCN), which in turn stimulates the pineal gland to release melatonin 22, 19. Wakefulness is maintained by subcortical structures and pathways activating the cortical system 22. This system is termed the “ascending arousal system” and utilizes several major neurochemicals, including:
- Norepinephrine (locus ceruleus)
- Serotonin (midline raphe nuclei)
- Histamine (tuberomammillary nucleus)
- Dopamine (ventral periaqueductal gray matter)
- Acetylcholine (pedunculopontine tegmentum and laterodorsal tegmentum of the pons)
- Orexin (perifornical area)
Transitions between sleep and wake states are influenced by multiple brain structures, including 6:
- Hypothalamus: controls onset of sleep
- Hippocampus: memory region active during dreaming
- Amygdala: emotion center active during dreaming
- Thalamus: prevents sensory signals from reaching the cortex
- Reticular formation: regulates the transition between sleep and wakefulness
- Pons: helps initiate REM sleep. The extraocular movements (eye movements) that occur during REM sleep are due to the activity of PPRF (paramedian pontine reticular formation/conjugate gaze center).
Although it is apparent that humans need sleep, the current understanding of why sleep is an essential part of life is still yet to be determined 6. The current hypotheses on the function of sleep include 23:
- Neural maturation
- Facilitation of learning or memory
- Targeted erasure of synapses to “forget” unimportant information that might clutter the synaptic network
- Cognition
- Clearance of metabolic waste products generated by neural activity in the awake brain
- Conservation of metabolic energy.
Wake or Alert Stage
The first stage is the wake stage or stage W, which further depends on whether your eyes are open or closed. During wakefulness, the EEG is characterized by waves of low amplitude and high frequency. This kind of EEG pattern is known as low-voltage fast activity or activated. During eye-open wakefulness, beta waves predominate. Alpha waves (8–13 Hz) become the predominant pattern as you become drowsy and close your eyes, particularly in occipital regions 24. The Electromyography (EMG, a test that measures the electrical activity of muscles) reveals tonic muscle activity with additional phasic activity related to voluntary movements.
EEG recording: beta waves – highest frequency, lowest amplitude (alpha waves are seen during quiet/relaxed wakefulness)
Non-Rapid Eye Movement (NREM) Sleep Stages
- Stage N1 (Light Sleep): This is the transition between wakefulness and sleep, characterized by slowing heart rate and breathing.
- Stage N2 (Intermediate Sleep): Your heart rate and body temperature decrease further, and your body relaxes.
- Stage N3 (Deep Sleep): This is the deepest stage of Non-Rapid Eye Movement (NREM) sleep, when your body performs restorative work, and it is crucial for feeling rested.
Stage 1 or N1 Sleep
NREM Stage 1 (N1) or Light Sleep serves a transitional role in sleep-stage cycling. This is the lightest stage of sleep and begins when more than 50% of the alpha waves are replaced with low-amplitude mixed-frequency (LAMF) activity. Muscle tone is present in the skeletal muscle, and breathing occurs regularly. This stage lasts around 1 to 7 minutes in the initial cycle, comprising 5% of total sleep time and is easily interrupted by a disruptive noise.
Brain activity on the EEG in stage 1 transitions from wakefulness (marked by rhythmic alpha waves) to low-voltage, mixed-frequency waves. Alpha waves are associated with a wakeful relaxation state and are characterized by a frequency of 8 to 13 cycles per second 14.
EEG recording: Theta waves – low voltage.
Stage 2 or N2 Sleep
NREM Stage 2 (N2) represents deeper sleep as the heart rate and body temperature drop 6. The presence of sleep spindles, K-complexes, or both characterizes it 6. Sleep spindles are brief, powerful bursts of neuronal firing in the superior temporal gyri, anterior cingulate, insular cortices, and thalamus, inducing calcium influx into cortical pyramidal cells. This mechanism is believed to be integral to synaptic plasticity. Numerous studies suggest that sleep spindles are essential in memory consolidation, specifically procedural and declarative memory 25. Individuals who learn a new task have a significantly higher density of sleep spindles than those in a control group 26.
K-complexes are long delta waves that last approximately one second and are known to be the longest and most distinct of all brain waves. K-complexes are shown to function in maintaining sleep and memory consolidation 27.
Stage 2 sleep lasts approximately 10 to 25 minutes in the initial cycle and lengthens with each successive cycle, eventually constituting between 45 to 55 percent of the total sleep episode. Stage 2 sleep is when bruxism (teeth grinding) occurs. An individual in stage 2 sleep requires more intense stimuli than in stage 1 to awaken. Brain activity on an EEG shows relatively low-voltage, mixed-frequency activity characterized by the presence of sleep spindles and K-complexes.
EEG recording: Sleep spindles and K complexes.
Stage 3 or N3 Sleep (Deepest Non-REM Sleep)
Sleep stage 3 or N3 sleep is also known as slow-wave sleep (SWS). This is considered the deepest stage of sleep and is characterized by signals with lower frequencies and higher amplitudes, known as delta waves 6. Sleep stage 3 or N3 sleep is the most difficult to awaken from; for some people, loud noises (> 100 decibels) will not lead to an awake state 6. As people age, they spend less time in this slow, delta-wave sleep and more time in stage N2 sleep 6. Although this stage has the greatest arousal threshold, if someone is awoken during this stage, they will have a transient phase of mental fogginess, known as sleep inertia 6. Cognitive testing shows that individuals awakened during this stage tend to have moderately impaired mental performance for 30 minutes to 1 hour 28. Sleep stage 3 or N3 sleep stage is when the body repairs and regrows tissues, builds bone and muscle, and strengthens the immune system. Sleep stage 3 or N3 sleep is also the stage when sleepwalking, night terrors, and bedwetting occur 29.
Sleep stage 3 or N3 sleep lasts only a few minutes and constitutes about 3 to 8 percent of sleep. The EEG shows increased high-voltage, slow-wave activity.
EEG recording: Delta waves – lowest frequency, highest amplitude.
Rapid Eye Movement (REM) Sleep Stage
Rapid eye movement sleep or REM sleep is the fourth and final stage of sleep and is when you have your most vivid and intense dreams. During REM sleep your brain activity increases to near-waking levels, your eyes dart quickly under your eyelids with fluctuating in your breathing and heart rate and most vivid dreams occur in this phase of sleep. Your muscles become limp (atonia) to prevent you from acting out your dreams. EEG recording shows beta waves – similar to brain waves during wakefulness. You experience your first period of REM sleep about 60 to 90 minutes after falling asleep 21.
REM sleep is defined by the presence of desynchronized (low-voltage, mixed-frequency) brain wave activity, muscle atonia, and bursts of rapid eye movements 14. “Sawtooth” wave forms, theta activity (3 to 7 counts per second), and slow alpha activity also characterize REM sleep 12. During the initial cycle, the REM period may last only 1 to 5 minutes; however, it becomes progressively prolonged as the sleep episode progresses 12.
Most adults need about 2 hours of REM sleep each night, which contributes to brain development, brain function, memory consolidation, and emotional health 30, 31.
Infants and children need more REM sleep, because their brains are still rapidly developing. For example, newborn babies spend around eight hours in REM sleep each day.
How much time you actually spend in REM sleep can vary from night to night. On a night when you’re short of sleep, your total REM time can get cut short. This can trigger your brain to initiate more REM sleep the following night, which is known as a REM rebound 32. Some research also suggests that REM sleep may increase after learning new information 33.
Because REM sleep enables better brain function, memory, and emotional regulation, a lack of REM sleep can cause a range of issues. On top of that, a lack of REM sleep circumvents healthy sleep overall, contributing to sleep deprivation. In the short term, signs of sleep deprivation can include 34:
- Difficulty concentrating
- Excessive daytime sleepiness
- Forgetfulness or poor memory
- Irritability or frustration
- Greater risk of accidents
Over the long term, insufficient sleep can weaken your immune system and raise your risk of conditions like heart disease, diabetes, depression, and anxiety.
How Much Deep Sleep Do I Need?
Different people need different amounts of sleep. Most adults need 7 to 8 hours of sleep a night for good health and mental functioning. Some adults need up to 9 hours a night 35. During a healthy night’s sleep for most adults, deep sleep (stage 3 or N3 sleep) makes up between 10% and 20% of total sleeping time 36. People who sleep less than approximately 7 hours a night are at a greater risk for heart disease, stroke, asthma, arthritis, depression, and diabetes. Nearly 20% of all car crashes, both fatal and nonfatal, are attributed to drowsy driving. Without enough sleep, your brain may struggle to perform basic functions. You may find it hard to concentrate or remember things. You may become moody and lash out at co-workers or people you love.
If you’re not sure about how much sleep you really need, you can use an online Sleep Calculator (https://www.sleepfoundation.org/sleep-calculator). However, your doctor is in the best position to make a detailed sleep recommendation for you based on your age, your overall health and your unique situation.
Table 1. Recommended Sleep Duration
| Age Range | Recommended Daily Sleep | |
|---|---|---|
| Infant | 4–12 months | 12-16 hours (including naps) |
| Toddler | 1–2 years | 11-14 hours (including naps) |
| Preschool | 3–5 years | 10-13 hours (including naps) |
| School-age | 6-12 years | 9-12 hours |
| Teens | 13-18 years | 8-10 hours |
| Adults | 18 years and older | 7 or more hours |
Just as your brain needs sleep to restore itself, so does your body. When you do not have enough sleep, your risk goes up for several illnesses.
- Diabetes. Your body does not do as well controlling blood sugar when you do not get enough sleep.
- Heart disease. Lack of sleep can lead to high blood pressure and inflammation, two things that can damage your heart.
- Obesity. When you do not get enough rest from sleep, you are more prone to overeat. It is also harder to resist foods high in sugar and fat.
- Infection. Your immune system needs you to sleep so it can fight colds and keep you healthy.
- Mental health. Depression and anxiety often make it hard to sleep. They also can become worse after a string of sleepless nights.
The cancer research branch of the World Health Organization has determined that disruption of regular sleep is “probably carcinogenic to humans”, putting it in the same risk category as the infectious agents malaria and human papillomavirus (HPV), as well as the biochemical weapon mustard gas. Sexual health is affected by sleep deprivation as well, as men with the worst sleeping habits have significantly lower sperm counts, decreased circulating testosterone, and even testicular shrinkage.
Adults generally need about 1.5 to 2 hours of deep sleep per night, which equates to roughly 13-23% of their total recommended sleep time. This stage of sleep is crucial for physical recovery, immune function, and cognitive health, so ensure you are getting sufficient overall sleep and practicing healthy sleep habits to obtain enough deep sleep
Why Deep Sleep is Important?
While all stages of sleep are necessary for good health, deep sleep is important because it is when your body undergoes essential physical restoration, immune system strengthening, and hormone production, while your brain processes and stores memories, consolidates learning, and clears waste products 9. During deep sleep, your body works to build and repair tissue, muscles, and bones, including by producing high levels of growth hormone 38. Achieving sufficient deep sleep helps you wake feeling refreshed, promotes long-term physical and mental health, and supports healthy weight and cardiovascular function 9. Deep sleep also promotes immune system functioning. Research suggests that it helps you build stronger immune responses and reduce unwanted chronic inflammation 39.
Slow-wave sleep also helps regulate blood sugar levels. As a result, the risk of developing type 2 diabetes may be higher if you don’t get enough deep sleep 40. And a shortage of deep sleep has also been linked to high blood pressure 41.
Deep sleep is important for cognitive function and memory. Although brain activity slows during deep sleep, this may actually facilitate learning by keeping the brain from becoming oversaturated with information. Evidence suggests that deep sleep also helps eliminate waste material from the brain, which may help protect against dementia 42.
Because deep sleep is an essential component of your nightly rest, a shortage of deep sleep contributes to broader impacts of sleep deprivation. In addition to causing tiredness, a shortage of deep sleep can cause general symptoms of sleep deprivation, including 43:
- Reduced alertness and attention
- Trouble learning and remembering things
- Irritability
- Symptoms of depression or anxiety
- Increased likelihood of accidents and injuries
On top of these immediate effects, a chronic lack of quality sleep can increase the likelihood of multiple health problems, such as:
- Infections and reduced immune system function
- Obesity
- Type 2 diabetes
- Cardiovascular problems, including high blood pressure, stroke, and heart disease
- Kidney disease
If you want to get more deep sleep, focus on enhancing your overall sleep. If your sleep quality and quantity are good, it usually means you’re getting plenty of restorative deep sleep. You get the most deep sleep during the early part of the night.
One of the most reliable ways to improve your sleep is by practicing good sleep hygiene. Good habits include 44:
- Establishing a consistent bedtime and wake-up time
- Ensuring you have a quiet, cool, and dark sleep environment
- Creating a relaxing bedtime routine to wind down in the evening
- Reducing caffeine intake in the afternoon and evening
- Limiting use of mobile devices, tablets, laptops, and other screens for 30 minutes or more before bedtime
There are some additional steps you can try to encourage more deep sleep:
- Take a warm bath: Some research suggests that heating your body with a warm bath before bedtime may induce more slow-wave sleep 45. A warm bath raises body temperature, which promotes blood circulation, and the subsequent cooling may help ease the transition to sleep.
- Change your diet: What you eat and drink before bedtime impacts your sleep. One small study found that people eating a diet high in saturated fats obtained less slow-wave sleep 46. People who ate more fiber were more likely to have increased amounts of deep sleep.
- Listen to binaural beats: Binaural beats are created by listening to two slightly different tones, one in each ear. The difference between the frequencies of those tones creates a perceived third tone, or binaural beat. Limited research suggests that listening to certain binaural beats may contribute to more stage 3 sleep 47.
Rapid eye movement sleep pathophysiology
There are a broad variety of pathologies that interrupt normal sleep physiology. A few of the most common are are included below:
Physiological disruptions of sleep
Narcolepsy is the result of the inherited loss of orexin-releasing neurons in the lateral hippocampus which causes somnolence, sleep cycle disruptions and cataplexy 48. A hallmark feature of narcolepsy is episodes of uncontrollable sleepiness that results in waking refreshed referred to as “sleep attacks.” This is due to aberrant activation of REM sleep circuits that result in the paralysis or hypotonia characteristic of narcolepsy 48. Cataplexy is pathognomic for this condition and consists of loss of muscle tone that is often induced by stressors such as loud noises or heightened emotions. Hypnagogic (upon going to sleep) and hypnopompic (upon waking) hallucinations are more common in narcoleptics than the general patient population as is sleep paralysis (most common upon waking).
Obstructive sleep apnea (OSA) is the cessation of airflow despite normal respiratory effort due to partial or complete obstruction of the upper airway 49. Polysomnography is the gold standard test to diagnose obstructive sleep apnea (OSA). Rapid eye movement (REM) sleep has been correlated with the severity of sleep apnea secondary to the differences in sleep positions between REM and NREM sleep 49. In particular, apneic episodes can be observed with PSG and are more prevalent during rapid eye movement (REM) sleep due to the prevalence of patients sleeping in the supine position. This is associated with increased frequency of apneic episodes with no effect on the duration of episodes.
Psychiatric disruptions of sleep
Major depressive disorder has been associated with decreases in REM latency, increased REM density, and a prolonged first REM cycle 50. Multiple studies have shown that antidepressants (including selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants) and cognitive behavioral therapy both serve to normalize sleep architecture. Nearly all antidepressants cause increased REM latency and reduce total REM sleep time. Interestingly, shortened REM latency persists during remission and is even present in patients with a strong family history of depression who do not present with symptoms of major depressive disorder.
Bipolar disorder is characterized by the broad range of sleep disturbances that are observed as a patient fluctuates between episodes of mania, bipolar depression, and euthymia 50. REM latency is shorter, and REM density increased in both the manic and depressed episodes. Euthymic bipolar disorder patients experience similarly shortened REM latencies, yet experience increased total REM sleep. Of note are the positive correlations that exist between the duration of the first REM period with manic symptoms and REM density with depressive symptoms that last greater than three months.
Schizophrenia is associated with several changes in REM sleep, including reduced REM latency, higher REM density, and the failure to rebound from REM sleep deprivation 50. These changes have not been proven to be consistent, however. Appropriate treatment with antipsychotics has been associated with increased total sleep time and REM latency. Several differences exist between typical and atypical antipsychotics which suggests that the second-generation antipsychotics have additional beneficial effects of sleep via management of other psychiatric symptoms such as depression and cognitive impairment.
Parasomnias are a class of pathologies defined as behavioral manifestations of partial arousals from sleep, particularly REM sleep 51. Parasomnias can present with physiological abnormalities that occur during the REM stage including impaired or painful sleep-related erections, bradycardia, and cardiac sinus-arrest. Other parasomnias include phenomena that are associated with REM sleep such as dreaming and can manifest as nightmare disorder. Other disorders involve the aberrations of REM-related muscle atonia which results in behavioral disorders such as recurrent isolated sleep paralysis and REM behavior disorder.
Insomnia is characterized by the dysfunction of sleep onset or maintenance that are not caused by substances or secondary medical conditions 52. Studies have shown that insomnia is associated with decreased total REM sleep and slow wave sleep. Sedative-hypnotics that promote GABA signaling such as zolpidem or triazolam are the first-line treatment for patients experiencing sleep-onset type insomnia, although 5-HT2 (serotonin) inhibitors are recently being developed as potential treatments for insomnia 53.
Several common substances and medications are associated with rapid eye movement sleep disruption. Alcohol is commonly used substances for self-medication and significantly delays the first onset of REM sleep 3.
Rapid eye movement sleep behavior disorder
Rapid eye movement sleep behavior disorder is a rapid eye movement (REM) sleep parasomnia characterized by dream enactment during sleep and loss of muscle atonia during REM sleep 54. Patients act out during their dreams while being in the rapid eye movement (REM) stage of the sleep. This enactment may be violent and can lead to injury to themselves or others without any conscious awareness. A patient can recall the contents of the dream upon awakening. Most patient’s with rapid eye movement (REM) behavior disorder will eventually manifest neurodegenerative diseases like parkinsonism, Lewy body dementia, Parkinson disease and multiple system atrophy (MSA) 1. In fact, several studies have shown that the majority of patients who experience rapid eye movement sleep behavior disorder are subsequently diagnosed with one or more of these syndromes.
Rapid eye movement sleep behavior disorder can be a disturbing disorder for both patients and their bed partners. Both are prone to injuries due to violent behavior 55. Patients may be advised to create a safer environment in the bedroom to avoid injuries.
There are also secondary cases of rapid eye movement sleep behavior disorder associated with narcolepsy or use of antidepressant medications 55. Secondary causes of rapid eye movement sleep behavior disorder may need to be evaluated through a complete sleep history and review of medications. Any precipitating factors or medications causing or exacerbating rapid eye movement sleep behavior disorder need to be avoided. In proper clinical settings, brain imaging with MRI and EEG may be recommended to evaluate for a secondary cause of rapid eye movement sleep behavior disorder. This is the only parasomnia where polysomnography is required to diagnose rapid eye movement sleep behavior disorder and rule out severe obstructive sleep apnea (OSA) as a cause of “pseudo rapid eye movement sleep behavior disorder.”
The overall prevalence of “spontaneous” rapid eye movement sleep behavior disorder is estimated to be about 1% in the general population and 2% in older individuals 56. Rapid eye movement sleep behavior disorder is more prevalent in elderly males than females with a male to female ratio of 9 to 1 57. There is a strong association of rapid eye movement sleep behavior disorder with many neurodegenerative disorders. rapid eye movement sleep behavior disorder can be a precursor to more serious conditions involving alpha-synuclein neuropathies such as parkinsonism, multiple system atrophy or dementia with Lewy body where prevalence can be as high as 76% to 81% of affected individuals 58. In a case series, about half of the patients with rapid eye movement sleep behavior disorder converted to a neurologic disorder within 12 years 59.
Patients should be informed that they are at risk of developing neurodegenerative disorders. Most patients with spontaneous rapid eye movement sleep behavior disorder can eventually develop a neurodegenerative disorder. The rate of conversion is about 50% every 10 years 60.
Treatment consists of preventive measures while sleeping to avoid injury to the patient as well as the bed partner. In severe cases, the patient may be prescribed melatonin or clonazepam 55. Melatonin is the first-line treatment, and in refractory cases, clonazepam in lower doses may be tried.
Rapid eye movement sleep behavior disorder causes
Rapid eye movement sleep behavior disorder occurs because of the failure to inhibit spinal motor neuron during rapid eye movement (REM) sleep 55. A strong association between rapid eye movement sleep behavior disorder and future development of a neurodegenerative disorder has been well established 61. Neurodegenerative disorders linked to alpha-synuclein positive intracellular inclusions, for example, parkinsonism, Lewy body dementia, and multiple system atrophy (MSA), are associated with alpha-synucleinopathies. Nuclei in the pons control rapid eye movement (REM) sleep. Lesions in pons can lead to the development of these synucleinopathies and rapid eye movement sleep behavior disorder 58. A progressive degeneration of these nuclei may explain the rapid eye movement sleep behavior disorder as a prodrome before full onset of the disease spectrum. Neuroimaging studies have shown progressive dopaminergic abnormalities in patients with rapid eye movement sleep behavior disorder 62. Dopaminergic agents like antidepressants may, therefore, worsen rapid eye movement sleep behavior disorder. In narcolepsy, about 50% of patients may manifest rapid eye movement sleep behavior disorder. Lack of orexin in narcolepsy may fail to stabilize REM sleep and results in a lack of muscle atonia during rapid eye movement (REM) sleep 63.
Causes of “secondary” rapid eye movement sleep behavior disorder, especially in younger individuals, include narcolepsy or use of antidepressant medications. Prevalence of rapid eye movement sleep behavior disorder in narcolepsy has been reported to be to be as high as 36% 63. Antidepressant medications can precipitate rapid eye movement sleep behavior disorder-type symptoms in up to 6% of cases 64. Other secondary causes of rapid eye movement sleep behavior disorder may include vascular lesions, tumors, demyelinating disease, autoimmune, or inflammatory disorders.
Obstructive sleep apnea (OSA) may mimic rapid eye movement sleep behavior disorder and is referred to as “pseudo rapid eye movement sleep behavior disorder” 65.
Rapid eye movement sleep behavior disorder pathophysiology
There are 2 systems involved in normal rapid eye movement (REM) sleep; one generates muscle atonia and other for suppresses motor-skeletal activity. Muscle atonia involves active inhibition by neurons in the medulla. Locomotion involves input from forebrain, and the thalamus influences spinal motor neurons. Several brainstem pontine regions have been implicated in rapid eye movement sleep behavior disorder pathophysiology including the peri-locus coeruleus region, pedunculo-pontine nucleus and laterodorsal tegmental nucleus 66. Supra-spinal mechanism handles rapid eye movement (REM) atonia. During rapid eye movement (REM) sleep, nuclei from the pons excite neurons in the medulla, which then transmit descending inhibitory projections to spinal alpha motor-neurons resulting in hyperpolarization and muscle atonia. It is the disinhibition of these neurons that leads to muscle activity during the REM stage of sleep 61.
Rapid eye movement sleep behavior disorder symptoms
Physicians should get a thorough sleep history regarding nocturnal movements to assess the nature of parasomnia. Sleep history may help to identify whether the symptoms are happening during the REM or non-REM stage of the sleep. A history of epileptic activity may be explored. Patients themselves may not know of motor activity during sleep. In a study of 203 patients 67 with rapid eye movement sleep behavior disorder, only about half of the patients knew of their symptoms. The movements may be short and range in severity. These may include punching, kicking, falling out of bed, gesturing, or knocking over the nightstand. Patients may have vocalizations during an attack. Schenck et al. 68 reported dream enactment in 87% of their study population. Patients had the vivid, intense, action-filled and, violent dreams coincident with the onset of rapid eye movement sleep behavior disorder. Sleep-related injuries occurred in 79% of patients in this series of patients.
Symptoms predominantly occur in the second half of the night when the rapid eye movement (REM) sleep is most prevalent and usually occur during the last REM sleep period.
In milder forms, patients may sleep through the event, but in severe cases, patients may transiently wake up but then fall asleep.
Patients may be examined for the development of any neurodegenerative disorders.
Rapid eye movement sleep behavior disorder diagnosis
According to the third edition of the International Classification of Sleep Disorders (ICSD-3), a diagnosis of rapid eye movement sleep behavior disorder requires all of the following 69:
- Repeated episodes of sleep-related vocalization and/or complex motor behaviors
- Behaviors are documented by polysomnography to occur during REM sleep or, based on the clinical history of dream enactment, are presumed to occur during REM sleep
- Presence of REM sleep without atonia (RSWA) on polysomnography
- An absence of epileptiform activity during REM sleep, unless rapid eye movement sleep behavior disorder can be clearly distinguished from any concurrent REM sleep-related seizure disorder
- Sleep disturbance not better explained by another sleep disorder, medical or neurologic disorder, mental disorder, medication use, or substance use disorder
Rapid eye movement sleep behavior disorder is the only parasomnia which requires an in-facility polysomnogram to diagnose rapid eye movement sleep behavior disorder.
The characteristic polysomnographic finding of rapid eye movement sleep behavior disorder is REM sleep without atonia (RSWA). It is an elevation of motor tone during REM sleep as measured by electromyography (EMG) activity in the chin and/or limb leads 70.
Formal polysomnographic criteria for REM sleep without atonia developed by the American Academy of Sleep Medicine require either of the following 69:
- Sustained elevation of chin electromyography (EMG) activity during REM sleep (greater than 50% of the 30-second epoch duration compared with minimum amplitude in non-REM sleep)
- Excessive bursts of transient muscle activity in the chin or limb electromyography (EMG) during REM sleep, defined by the presence of 5 (50%) or more mini-epochs (30-second epoch is divided into 10 sequential 3-second mini-epochs), containing bursts of transient muscle activity. In rapid eye movement sleep behavior disorder, excessive transient muscle activity bursts last 0.1 to 5.0 seconds and are at least 4 times as high in amplitude as the background empirical mode decomposition (EMD) activity.
Optimally, both upper and lower extremity EMG should be used when evaluating for rapid eye movement sleep behavior disorder. Alternate EMG derivations that make use of upper extremity EMG to improve sensitivity for detecting REM sleep without atonia are reviewed separately.
The disorder needs to be differentiated from other parasomnias including both REM and non-REM sleep parasomnias including nightmares, night terrors, sleepwalking and sleep talking. Periodic leg movements may present with limb movement while sleeping but generally occur during the non-REM stage of the sleep and have distinctive diagnostic criteria on polysomnography.
Epileptic disorders like sleep-related hyperosmolar epilepsy (frontal lobe epilepsy) may present with motor activity during sleep. However, compared with rapid eye movement sleep behavior disorder, these patients are generally younger and unaware of their symptoms.
Rapid eye movement sleep behavior disorder treatment
The primary goal of treatment is to provide patients with a safe sleeping environment for them and their bed partners. Healthcare professionals can achieve this through non-pharmacologic approaches and pharmacotherapy if needed.
It is important to counsel patients and their bed partners on avoidance of potentially hazardous and injuries objects near the patients, for example, firearms or glass objects. Bed partners should be educated on the disease, and the patient’s enactments during dreams are not under voluntary control.
Sleeping alone may be advisable in severe cases. Many patients may require padded bed rails or must sleep in a sleeping bag 71.
Patients may be advised to stop SSRI and tricyclic antidepressants that are known to cause or exacerbate rapid eye movement sleep behavior disorder 72.
Regarding pharmacotherapy, melatonin is now considered the first-line therapy in the treatment of rapid eye movement sleep behavior disorder 73. Its mechanism of action is unknown, but in doses between 6 to 18 mg, it augments REM atonia and improves rapid eye movement sleep behavior disorder symptoms. Patients are typically started at doses of 3 mg, and then doses are increased in 3-mg increments until the rapid eye movement sleep behavior disorder symptoms resolve.
Low-dose clonazepam (0.5 to 1 mg at bedtime) has been traditionally used to control rapid eye movement sleep behavior disorder symptoms. Its mechanism of action is not clear either but may help suppress unpleasant dreams 72. Its use may be limited due to side effects. In one study, 39% of patients reported side effects 67.
- Carley DW, Farabi SS. Physiology of Sleep. Diabetes Spectr. 2016 Feb;29(1):5-9[↩][↩][↩][↩]
- Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014 Jan 08;81(1):12-34[↩][↩]
- Anderson KN, Bradley AJ. Sleep disturbance in mental health problems and neurodegenerative disease. Nat Sci Sleep. 2013;5:61-75[↩][↩][↩][↩]
- España RA, Scammell TE. Sleep neurobiology from a clinical perspective. Sleep. 2011 Jul 01;34(7):845-58.[↩]
- Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. National Academies Press (US); Washington (DC): 2006[↩][↩]
- Patel AK, Reddy V, Shumway KR, et al. Physiology, Sleep Stages. [Updated 2024 Jan 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Memar P, Faradji F. A Novel Multi-Class EEG-Based Sleep Stage Classification System. IEEE Trans Neural Syst Rehabil Eng. 2018 Jan;26(1):84-95. doi: 10.1109/TNSRE.2017.2776149[↩]
- Stages of Sleep: What Happens in a Normal Sleep Cycle? https://www.sleepfoundation.org/stages-of-sleep[↩][↩]
- How Much Deep Sleep Do You Need? https://www.sleepfoundation.org/stages-of-sleep/deep-sleep[↩][↩][↩]
- Malik J, Lo YL, Wu HT. Sleep-wake classification via quantifying heart rate variability by convolutional neural network. Physiol Meas. 2018 Aug 20;39(8):085004. doi: 10.1088/1361-6579/aad5a9[↩]
- Feinberg I, Floyd TC. Systematic trends across the night in human sleep cycles. Psychophysiology. 1979 May;16(3):283-91. doi: 10.1111/j.1469-8986.1979.tb02991.x[↩]
- Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 2, Sleep Physiology. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19956[↩][↩][↩]
- Zepelin H, Siegel JM, Tobler I. Mammalian sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier/Saunders; 2005. pp. 91–100.[↩]
- Carskadon M, Dement W. Normal human sleep: An overview. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier Saunders; 2005. pp. 13–23.[↩][↩][↩]
- Approach to the Patient With a Sleep or Wakefulness Disorder. https://www.msdmanuals.com/professional/neurologic-disorders/sleep-and-wakefulness-disorders/approach-to-the-patient-with-a-sleep-or-wakefulness-disorder[↩]
- Electroencephalogram (EEG) techniques measuring sleep activity and sleep stages. https://quizlet.com/au/336073417/electroencephalogram-eeg-techniques-measuring-sleep-activity-and-sleep-stages-diagram[↩]
- Reddy S, Reddy V, Sharma S. Physiology, Circadian Rhythm. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519507[↩]
- Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014 Jan 8;81(1):12-34. doi: 10.1016/j.neuron.2013.12.025[↩]
- España RA, Scammell TE. Sleep neurobiology from a clinical perspective. Sleep. 2011 Jul 1;34(7):845-58. doi: 10.5665/SLEEP.1112[↩][↩]
- Zajac A, Skowronek-Bała B, Wesołowska E, Kaciński M. Napadowe zaburzenia snu u dzieci w wideo/polisomnografii [Sleep paroxysmal events in children in video/polysomnography]. Przegl Lek. 2010;67(9):762-9. Polish.[↩]
- Feriante J, Araujo JF. Physiology, REM Sleep. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531454[↩][↩]
- Carley DW, Farabi SS. Physiology of Sleep. Diabetes Spectr. 2016 Feb;29(1):5-9. doi: 10.2337/diaspect.29.1.5[↩][↩]
- Frank, M.G., Heller, H.C. (2018). The Function(s) of Sleep. In: Landolt, HP., Dijk, DJ. (eds) Sleep-Wake Neurobiology and Pharmacology . Handbook of Experimental Pharmacology, vol 253. Springer, Cham. https://doi.org/10.1007/164_2018_140[↩]
- Varga B, Gergely A, Galambos Á, Kis A. Heart Rate and Heart Rate Variability during Sleep in Family Dogs (Canis familiaris). Moderate Effect of Pre-Sleep Emotions. Animals (Basel). 2018 Jul 2;8(7):107. doi: 10.3390/ani8070107[↩]
- Antony JW, Schönauer M, Staresina BP, Cairney SA. Sleep Spindles and Memory Reprocessing. Trends Neurosci. 2019 Jan;42(1):1-3. doi: 10.1016/j.tins.2018.09.012[↩]
- Gais S, Mölle M, Helms K, Born J. Learning-dependent increases in sleep spindle density. J Neurosci. 2002 Aug 1;22(15):6830-4. doi: 10.1523/JNEUROSCI.22-15-06830.2002[↩]
- Gandhi MH, Emmady PD. Physiology, K Complex. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557469[↩]
- Hilditch CJ, McHill AW. Sleep inertia: current insights. Nat Sci Sleep. 2019 Aug 22;11:155-165. doi: 10.2147/NSS.S188911[↩]
- El Shakankiry HM. Sleep physiology and sleep disorders in childhood. Nat Sci Sleep. 2011 Sep 6;3:101-14. doi: 10.2147/NSS.S22839[↩]
- Blumberg MS, Lesku JA, Libourel PA, Schmidt MH, Rattenborg NC. What Is REM Sleep? Curr Biol. 2020 Jan 6;30(1):R38-R49. doi: 10.1016/j.cub.2019.11.045[↩]
- Peever J, Fuller PM. The Biology of REM Sleep. Curr Biol. 2017 Nov 20;27(22):R1237-R1248. doi: 10.1016/j.cub.2017.10.026[↩]
- Feriante J, Singh S. REM Rebound Effect. [Updated 2024 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560713[↩]
- Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013 Apr;93(2):681-766. doi: 10.1152/physrev.00032.2012[↩]
- Sleep and your health. https://medlineplus.gov/ency/patientinstructions/000871.htm[↩]
- Consensus Conference Panel; Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015 Jun 15;11(6):591-2. doi: 10.5664/jcsm.4758[↩]
- Normal Sleep, Sleep Physiology, and Sleep Deprivation. https://emedicine.medscape.com/article/1188226-overview#showall[↩]
- https://www.sleepfoundation.org/sleep-calculator[↩]
- Dijk DJ. Regulation and functional correlates of slow wave sleep. J Clin Sleep Med. 2009 Apr 15;5(2 Suppl):S6-15. https://pmc.ncbi.nlm.nih.gov/articles/PMC2824213[↩]
- Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012 Jan;463(1):121-37. doi: 10.1007/s00424-011-1044-0[↩]
- Vlahoyiannis A, Aphamis G, Bogdanis GC, Sakkas GK, Andreou E, Giannaki CD. Deconstructing athletes’ sleep: A systematic review of the influence of age, sex, athletic expertise, sport type, and season on sleep characteristics. J Sport Health Sci. 2021 Jul;10(4):387-402. doi: 10.1016/j.jshs.2020.03.006[↩]
- Javaheri S, Zhao YY, Punjabi NM, Quan SF, Gottlieb DJ, Redline S. Slow-Wave Sleep Is Associated With Incident Hypertension: The Sleep Heart Health Study. Sleep. 2018 Jan 1;41(1):zsx179. doi: 10.1093/sleep/zsx179[↩]
- Zhang Y, Gruber R. Can Slow-Wave Sleep Enhancement Improve Memory? A Review of Current Approaches and Cognitive Outcomes. Yale J Biol Med. 2019 Mar 25;92(1):63-80. https://pmc.ncbi.nlm.nih.gov/articles/PMC6430170[↩]
- Healthy Sleep. https://medlineplus.gov/healthysleep.html[↩]
- Changing your sleep habits. https://medlineplus.gov/ency/patientinstructions/000757.htm[↩]
- Maeda T, Koga H, Nonaka T, Higuchi S. Effects of bathing-induced changes in body temperature on sleep. J Physiol Anthropol. 2023 Sep 8;42(1):20. doi: 10.1186/s40101-023-00337-0[↩]
- St-Onge MP, Roberts A, Shechter A, Choudhury AR. Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep. J Clin Sleep Med. 2016 Jan;12(1):19-24. doi: 10.5664/jcsm.5384[↩]
- Lee M, Song CB, Shin GH, Lee SW. Possible Effect of Binaural Beat Combined With Autonomous Sensory Meridian Response for Inducing Sleep. Front Hum Neurosci. 2019 Dec 2;13:425. doi: 10.3389/fnhum.2019.00425[↩]
- Fleetham JA, Fleming JA. Parasomnias. CMAJ. 2014 May 13;186(8):E273-80.[↩][↩]
- Iranzo A, Fernández-Arcos A, Tolosa E, Serradell M, Molinuevo JL, Valldeoriola F, Gelpi E, Vilaseca I, Sánchez-Valle R, Lladó A, Gaig C, Santamaría J. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS ONE. 2014;9(2):e89741[↩][↩]
- Fraigne JJ, Grace KP, Horner RL, Peever J. Mechanisms of REM sleep in health and disease. Curr Opin Pulm Med. 2014 Nov;20(6):527-32[↩][↩][↩]
- Oksenberg A, Arons E, Nasser K, Vander T, Radwan H. REM-related obstructive sleep apnea: the effect of body position. J Clin Sleep Med. 2010 Aug 15;6(4):343-8[↩]
- Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: effects on normal sleep. Alcohol. Clin. Exp. Res. 2013 Apr;37(4):539-49.[↩]
- Carley DW, Farabi SS. Physiology of Sleep. Diabetes Spectr. 2016 Feb;29(1):5-9.[↩]
- Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. 1986 [classical article]. Sleep. 2002 Mar 15;25(2):293-308[↩]
- Khawaja I, Singh S. REM Sleep Behavior Disorder. [Updated 2018 Dec 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534239[↩][↩][↩][↩]
- Haba-Rubio J, Frauscher B, Marques-Vidal P, Toriel J, Tobback N, Andries D, Preisig M, Vollenweider P, Postuma R, Heinzer R. Prevalence and Determinants of REM Sleep Behavior Disorder in the General Population. Sleep. 2017 Dec 05[↩]
- Bjørnarå KA, Dietrichs E, Toft M. REM sleep behavior disorder in Parkinson’s disease–is there a gender difference? Parkinsonism Relat. Disord. 2013 Jan;19(1):120-2[↩]
- Boeve BF. REM sleep behavior disorder: Updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann. N. Y. Acad. Sci. 2010 Jan;1184:15-54[↩][↩]
- Postuma RB, Gagnon JF, Vendette M, Fantini ML, Massicotte-Marquez J, Montplaisir J. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology. 2009 Apr 14;72(15):1296-300[↩]
- Postuma RB, Gagnon JF, Vendette M, Fantini ML, Massicotte-Marquez J, Montplaisir J. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology. 2009 Apr 14;72(15):1296-300.[↩]
- Boeve BF, Silber MH, Saper CB, Ferman TJ, Dickson DW, Parisi JE, Benarroch EE, Ahlskog JE, Smith GE, Caselli RC, Tippman-Peikert M, Olson EJ, Lin SC, Young T, Wszolek Z, Schenck CH, Mahowald MW, Castillo PR, Del Tredici K, Braak H. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007 Nov;130(Pt 11):2770-88[↩][↩]
- Shin HY, Joo EY, Kim ST, Dhong HJ, Cho JW. Comparison study of olfactory function and substantia nigra hyperechogenicity in idiopathic REM sleep behavior disorder, Parkinson’s disease and normal control. Neurol. Sci. 2013 Jun;34(6):935-40[↩]
- Nightingale S, Orgill JC, Ebrahim IO, de Lacy SF, Agrawal S, Williams AJ. The association between narcolepsy and REM behavior disorder (RBD). Sleep Med. 2005 May;6(3):253-8[↩][↩]
- Teman PT, Tippmann-Peikert M, Silber MH, Slocumb NL, Auger RR. Idiopathic rapid-eye-movement sleep disorder: associations with antidepressants, psychiatric diagnoses, and other factors, in relation to age of onset. Sleep Med. 2009 Jan;10(1):60-5[↩]
- Iranzo A, Santamaría J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005 Feb;28(2):203-6[↩]
- Hendricks JC, Morrison AR, Mann GL. Different behaviors during paradoxical sleep without atonia depend on pontine lesion site. Brain Res. 1982 May 06;239(1):81-105[↩]
- Fernández-Arcos A, Iranzo A, Serradell M, Gaig C, Santamaria J. The Clinical Phenotype of Idiopathic Rapid Eye Movement Sleep Behavior Disorder at Presentation: A Study in 203 Consecutive Patients. Sleep. 2016 Jan 01;39(1):121-32[↩][↩]
- Schenck CH, Mahowald MW. REM sleep behavior disorder: clinical, developmental, and neuroscience perspectives 16 years after its formal identification in SLEEP. Sleep. 2002 Mar 15;25(2):120-38.[↩]
- Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, Troester MT, Vaughn BV. AASM Scoring Manual Updates for 2017 (Version 2.4). J Clin Sleep Med. 2017 May 15;13(5):665-666[↩][↩]
- Neikrug AB, Ancoli-Israel S. Diagnostic tools for REM sleep behavior disorder. Sleep Med Rev. 2012 Oct;16(5):415-29[↩]
- Howell MJ. Parasomnias: an updated review. Neurotherapeutics. 2012 Oct;9(4):753-75[↩]
- Postuma RB, Gagnon JF, Tuineaig M, Bertrand JA, Latreille V, Desjardins C, Montplaisir JY. Antidepressants and REM sleep behavior disorder: isolated side effect or neurodegenerative signal? Sleep. 2013 Nov 01;36(11):1579-85[↩][↩]
- Boeve BF, Silber MH, Ferman TJ. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med. 2003 Jul;4(4):281-4[↩]