Contents
- What is the renal pelvis
- What is the function of the renal pelvis?
- Renal pelvis cancer
- Renal pelvis obstruction
- Renal pelvis stone
What is the renal pelvis
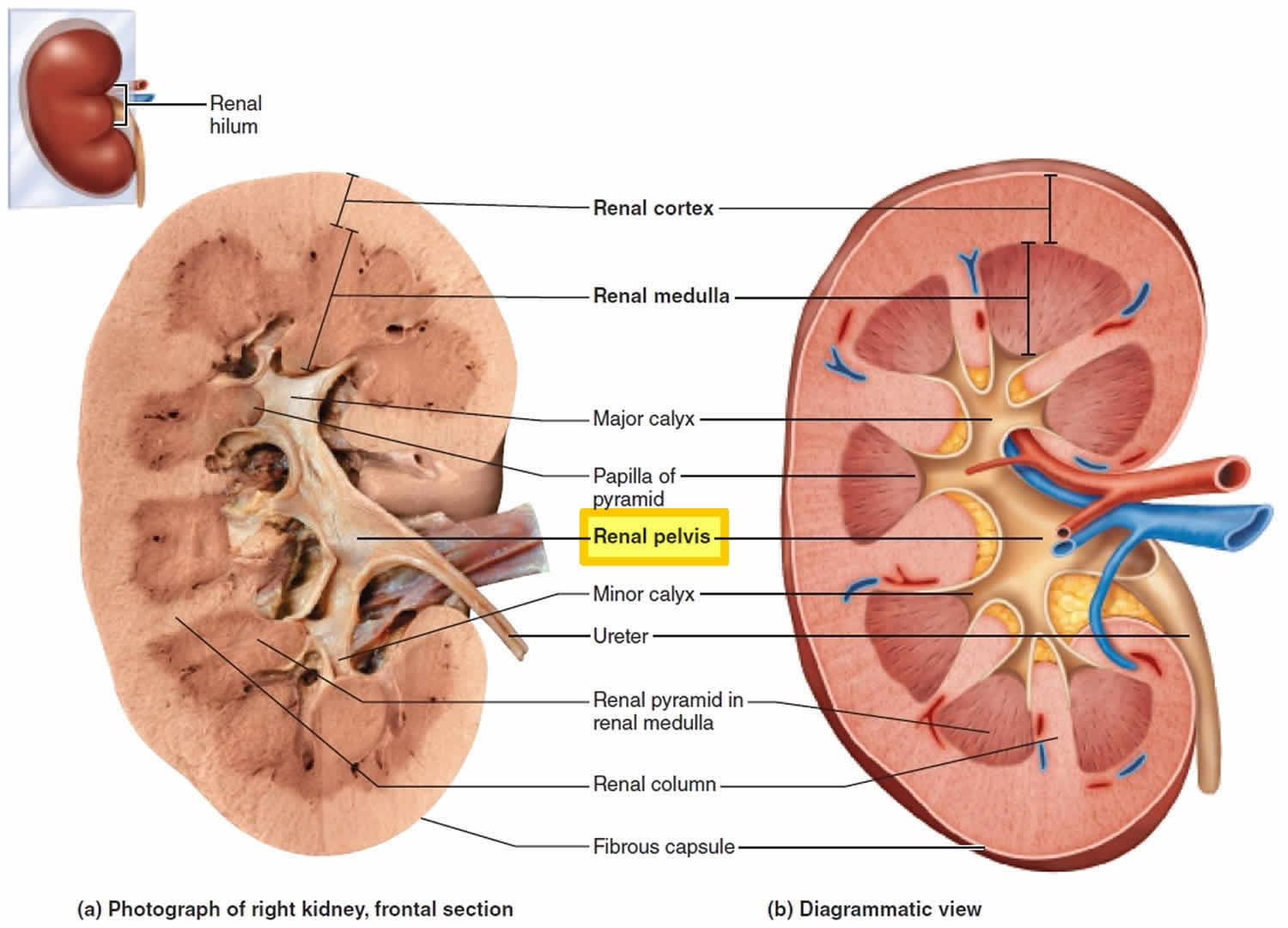
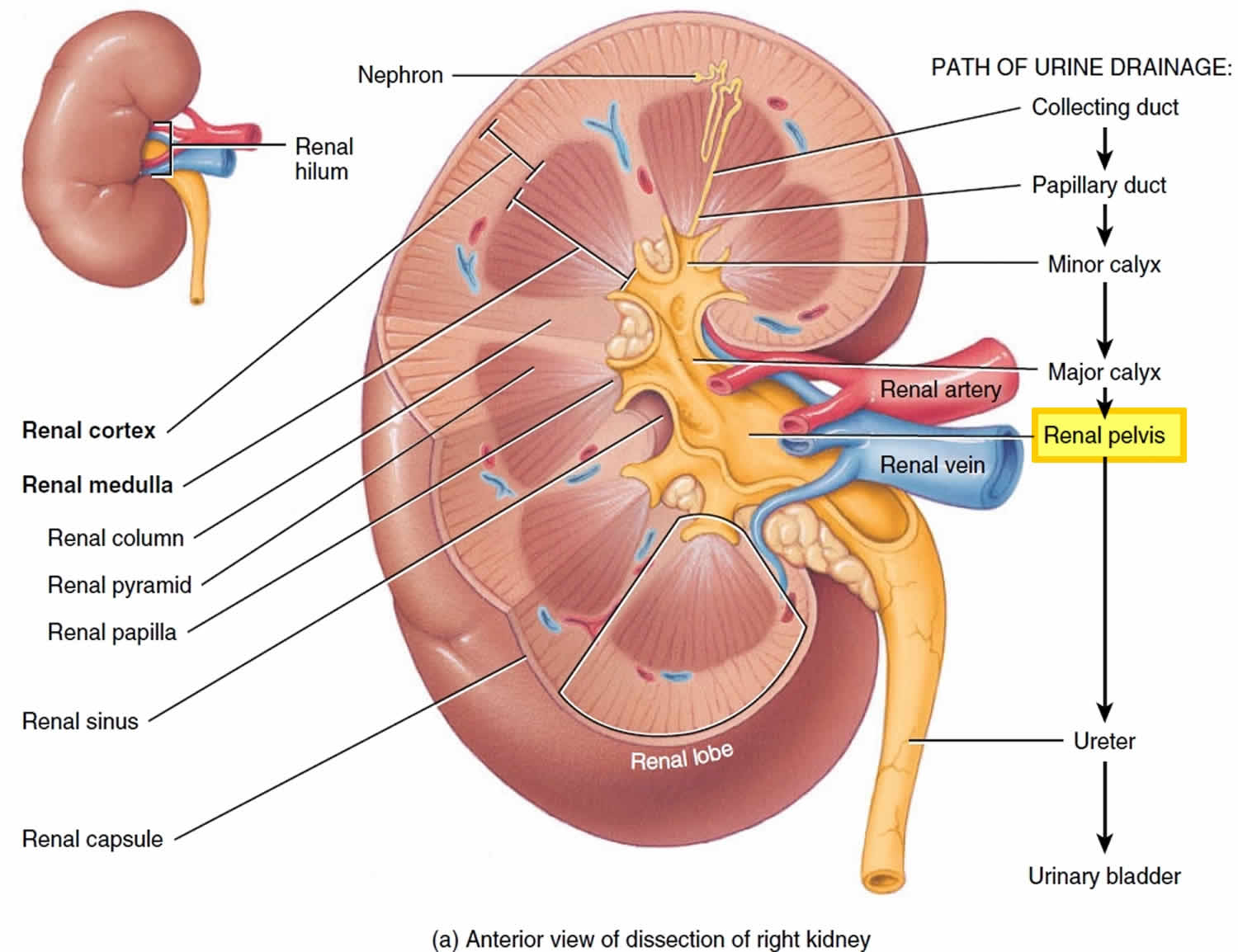
Renal pelvis is a flat, funnel-shaped urine-carrying tube and it is simply the expanded superior part of the ureter. Branching extensions of the renal pelvis form two or three major calices each of which divides to form several minor calices (calyx = cup), cup-shaped tubes that enclose the papillae of the pyramids. The calices collect urine draining from the papillae and empty it into the renal pelvis; the urine then flows through the renal pelvis and into the ureter, which transports it to the bladder for storage.
An infection of the renal pelvis and calices is called pyelitis (inflammation of the renal pelvis). When the infection spreads to involve the rest of the kidney as well, the result is called pyelonephritis (nephros = kidney). Although it usually results from the spread of the fecal bacterium Escherichia coli from the anal region superiorly through the urinary tract, pyelonephritis also occurs when bloodborne bacteria lodge in the kidneys and proliferate there. In severe cases, the kidney swells and scars, abscesses form, and the renal pelvis fills with pus. Left untreated, the infected kidneys may be severely damaged, but timely administration of antibiotics usually achieves a total cure.
Figure 1. Renal pelvis
What is the function of the renal pelvis?
Renal pelvis is a flat, funnel-shaped urine-carrying tube and it is simply the expanded superior part of the ureter.
Healthy kidneys work like clockwork to clean your blood. These 2 bean-shaped organs are found near the middle of the back below the rib cage. They filter about 200 quarts of blood daily. Every day, the kidneys remove about 2 quarts of water and waste products in the form of urine. The urine then moves into the kidney’s collecting system, the renal pelvis. It then flows through the ureters to the bladder, where it is stored until it is pushed out of the urethra.
Renal pelvis cancer
Cancers of the upper urinary tract are relatively rare. In 2015, about 3,100 Americans will be diagnosed with this cancer. The most common of all upper urinary tract cancers are those found in the renal pelvis and renal calyces. Malignant tumors arising from the renal pelvis include transitional cell carcinoma (85–90 %), squamous cell carcinoma (10–15 %), and adenocarcinoma (<1 %) 1. Adenocarcinomas of the renal pelvis are rare and are classified as tubulovillous, mucinous, or papillary non-intestinal 2. Primary mucinous adenocarcinoma of the renal pelvis, first described in 1960 by Hasebe et al. 3, is especially rare. Till date, only ~100 cases have been reported 4, most from Asian countries 5. Unfortunately, it is difficult to diagnose preoperatively because there are no characteristic symptoms or laboratory and radiological findings.
Tumors of the renal calyces, renal pelvis and ureters start in the layer of tissue that lines the bladder and the upper urinary tract, called the urothelium. Cancer that starts in the urothelium is called urothelial (or transitional cell) cancer. This is the most common type of cancer found in the bladder, as well. Because many of the organs in the urinary system share common cells, cancers found in these organs often look and act alike.
The urothelium is special in the way that it swells and shrinks to push urine through the urinary tract. Because it is in direct contact with the urine, this lining is exposed to chemicals (carcinogens) filtered out of the blood by the kidneys. These chemicals can cause cells to change and grow out of control as cancer.
Because the bladder stores urine, it may be at greater risk for cancer than other parts of the upper tract. Its cells are exposed to harmful substances for a longer time. When urine has a high percent of harmful chemicals, cancer may also grow in the kidney or ureters.
Renal pelvis cancer causes
Since the exact cause of renal pelvis cancer is not known, it is difficult to prevent. Still, there are certain risk factors that are known to affect cancer development.
Gender
Upper urinary tract cancer is diagnosed in men 2 times more than in women. But women have a 50% greater chance of dying of this cancer.
Race
Experts are trying to understand the role of race in upper tract cancers. Like bladder cancer, upper urinary tract cancer is less common in African-Americans than whites, but it is more deadly.
Age
As with bladder cancer, upper tract cancer occurs most often in people older than age 70. It is rare in those younger than age 40.
Smoking
There is a strong link between renal pelvis and ureteral cancers and tobacco use. If you have been a smoker, your risk level is tied to the number of years you smoked. Unlike lung and esophageal cancer, the risk of upper urinary tract or bladder cancer will remain high for decades. Likewise, nonsmokers have a much lower level of risk for these cancers.
Chemicals in the workplace
Exposure, over time, to chemicals used to make plastics, textiles, leather and rubber, can cause cancer.
Risk factors for renal pelvis cancer
- Longtime use of large amounts of painkillers
- Certain herbs used to help you lose weight
- Previous bladder cancer
- Previous urothelial cancer treatment in smokers
Genetics
There isn’t a lot of proof connecting upper urinary tract cancers to family history. However, in a small number of cases, there are clear genetic factors. So if you have urothelial cancer, your family members could be at higher risk. Family members should avoid risks such as smoking.
Renal pelvis cancer symptoms
Hematuria (blood in the urine)
Blood in the urine is the most common sign of upper urinary tract cancer. As a rule it is painless. But since it can happen with a variety of urinary tract problems, your health care team should check for all likely sources of any blood found in your urine.
Pain
You may have no symptoms if the tumor is growing slowly. An X-ray or ultrasound may be the only way to see whether a slow-growing tumor is present. If the tumor is fast-growing, it could cause pain by blocking the kidney’s collecting system. This could cause nausea and sharp pain in your lower back, side or stomach. Since these are also signs of kidney stones, you should see a urologist right away.
Less Common Complaints
Weight loss, anorexia, and bone pain may be signs of advanced disease. A mass in your side or abdomen can also be signs of advanced disease.
Renal pelvis cancer diagnosis
Medical history and physical exam
If your primary care doctor feels that you should see an expert, you will be referred to a urologist. The urologist will ask a variety of questions about your health history and will check your body with a variety of tests. He or she will feel your belly, sides and back for lumps, and will order blood tests.
A microscopic exam of cells in the urine (cytology) can help find an upper urinary tract cancer. Sometimes normal urine from the other kidney can water down a sample, making cancerous cells hard to find. If your doctor suspects cancer or cannot find the source of blood in the urine, he or she may order imaging tests.
Imaging
Ultrasound and CT (computerized tomography) scans are painless, nonsurgical ways to check the urinary tract. But while CT scans can show stones in the kidney and ureter, they are less useful in showing tumors. To see tumors more clearly, the doctor may use a contrast dye with the CT scan. To check whether the cancer has spread to other organs, MRI (magnetic resonance imaging) may also be helpful. Adding a retrograde X-ray (X-ray using a special dye) may be needed if you have poor kidney function.
Cystoscopy
If the source of bleeding is still in doubt, your doctor may order cystoscopy. A cystoscope uses a special fiber optic tool (like a camera lens) to look through the urethra into the bladder and urinary tract.
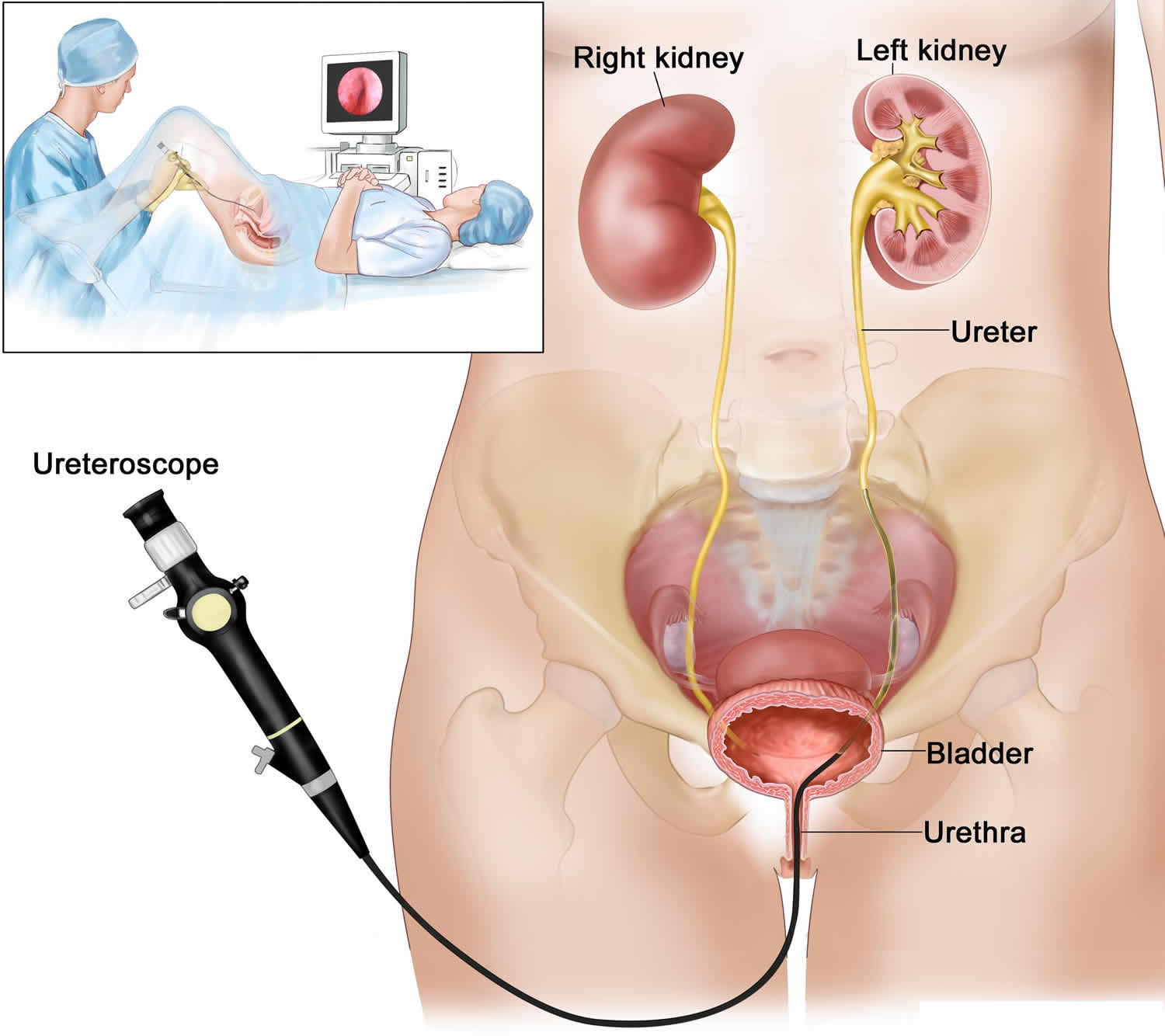
Endoscopy/Ureteroscopy
If the urologist needs more information, he or she may do a direct visual inspection of your upper urinary tract. This is usually done while you are under anesthesia. An endoscope (a scope with a light attached) is inserted through the urethra into the bladder. It is then moved up to see inside the ureter and renal pelvis. If needed, the doctor will remove a sample of tissue to help in the diagnosis (a biopsy).
Figure 2. Ureteroscopy
Imaging for Metastases
If the urologist has a confirmed cancer diagnosis, he or she will check to see if it has spread. If urinary tract cancer cells are found in other sites, it is called metastatic cancer.
Tests to see if the cancer has spread to common sites include:
- CT scan (of the abdomen, pelvis, and nearby lymph nodes and organs)
- MRI
- Chest X-ray (to look at the lungs)
- Bone scan (to look at the skeleton)
Grading and Staging
If cancer cells are found, your doctor will need to know the tumor grade and stage. Understanding these will help your health care team develop your treatment plan.
Grading
The grade tells how fast the tumor is likely to grow. The most widely used grading systems group tumors into 2 main grades: low and high.
- Low-grade tumors grow more slowly. They often come back after treatment, but rarely get into the upper urinary tract wall. They also don’t tend to spread to other parts of the body.
- High-grade tumors grow more quickly. They often come back after treatment and are more likely to spread to other parts of the body.
Staging
Your doctor must also learn how deeply the tumor has gone into the collecting system wall. This is called “staging.” Your doctor also wants to find out if the tumor has spread to other parts of the body (metastasis). In general, the higher the stage number, the more serious the cancer. Often the stage is not clearly defined until the tumor is removed and studied by a pathologist (an expert who looks for cancer cells in tissue samples).
The following stages are used for transitional cell cancer of the renal pelvis and/or ureter:
- Stage 0 (Noninvasive Papillary Carcinoma and Carcinoma in Situ):
- In stage 0, abnormal cells are found in tissue lining the inside of the renal pelvis or ureter. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is divided into stages 0a and 0is, depending on the type of tumor:
- Stage 0a is also called noninvasive papillary carcinoma, which may look like long, thin growths that grow out from the tissue lining the inside of the renal pelvis or ureter.
- Stage 0is is also called carcinoma in situ, which is a flat tumor on the tissue lining the inside of the renal pelvis or ureter.
- In stage 0, abnormal cells are found in tissue lining the inside of the renal pelvis or ureter. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is divided into stages 0a and 0is, depending on the type of tumor:
- Stage I: In stage 1, cancer has formed and has spread from the tissue lining the inside of the renal pelvis or ureter to the connective tissue layer.
- Stage II: In stage 2, cancer has spread to the muscle layer of the renal pelvis or ureter.
- Stage III: In stage 3, cancer has spread:
- from the muscle layer of the renal pelvis to fat around the renal pelvis or to tissue in the kidney; or
- from the muscle layer of the ureter to fat around the ureter.
- Stage IV: In stage 4, cancer has spread to at least one of the following:
- a nearby organ.
- the layer of fat around the kidney.
- lymph nodes.
- other parts of the body, such as the lung, liver, or bone.
Transitional cell cancer of the renal pelvis and ureter is also described as localized, regional, or metastatic:
- Localized: The cancer is found only in the kidney.
- Regional: The cancer has spread to tissues around the kidney and to nearby lymph nodes and blood vessels in the pelvis.
- Metastatic: The cancer has spread to other parts of the body.
Renal pelvis cancer treatment
What you and your doctor choose depends on many issues, such as:
- tumor grade (how aggressive the tumor is)
- tumor size, location and extent
- your age
- medical history
- overall health
- kidney collecting system anatomy
Options include:
- surgery
- chemotherapy
- radiation
Surgery – Removal of Kidney and Ureter
The majority of upper urinary tract cancers are treated with nephroureterectomy (surgery to remove the kidney and an entire ureter). The “radical” form involves removing nearby lymph nodes and tissue as well. Since you will only have 1 kidney, your doctor will closely watch your overall kidney function. You would not need dialysis unless you already have serious kidney problems.
The type of surgery you are offered will depend on surgeon preference, tumor size, tumor location and tumor aggressivenes. Options include:
- traditional: a 10-inch cut into the abdomen is made to remove the tumor(s)
- laparoscopy: tube-like instruments are inserted into the abdomen through small “key-hole” cuts.
Kidney Sparing Surgery
In kidney sparing surgery your doctor will try to keep the remaining kidney and ureter on the side with the tumor. This is an option if you already:
- lost a kidney to cancer
- lost a kidney because of stones, infection or trauma
- have kidney problems because of diabetes, high blood pressure or glomerulonephritis
If your doctor decides to spare the kidney, the tumor can be managed with segmental resection or endoscopic removal.
- Segmental resection: removing the cancerous part of the urinary tract and then reattaching it so the kidney is still joined to the bladder. This is done if the cancer hasn’t spread past the surface.
- Endoscopic removal: removing the tumor through a small scope called a ureteroscope. The ureteroscope is inserted through the bladder into the upper urinary tract. Then the tumor can be destroyed with a laser. This is done if the growth is small and low-grade.
- Percutaneous tumor removal: a scope is placed directly into the kidney’s collecting system through a small puncture in the back.
Protecting your kidney after surgery
If the surgery leaves you with only 1 kidney, you should avoid a few things, for example, major contact sports (e.g., football, karate or boxing), or NSAIDs (nonsteroidal anti-inflammatory drugs, e.g., aspirin and ibuprofen). In rare cases these drugs can cause kidney damage. Depending on how well the remaining kidney functions, you may need to avoid the dyes used in some imaging tests. You may also want to limit the salt and protein in your diet.
Treating problems like high blood pressure, diabetes, high cholesterol, and obesity can help prevent future kidney damage.
Chemotherapy
Topical chemotherapy and immunotherapy
In bladder cancer, drugs can be inserted in the bladder to prevent cancer from coming back. But they are not often used for renal pelvis or ureteral cancer. The bladder holds fluid for hours, so the tissue has plenty of exposure to the drugs. But the upper urinary tract doesn’t hold as much fluid as the bladder or for as long. Still, your doctor may use drugs in addition to surgery.
Systemic chemotherapy
Chemotherapy uses drugs to kill cancer cells. It may be used to treat upper urinary tract cancer before or after the kidney and ureter are removed.
You may receive chemotherapy in different ways:
- By mouth: Some drugs are pills that you can swallow. They may be given before or after surgery.
- Into a vein (intravenous): The drugs enter the bloodstream and travel throughout your body. Chemotherapy may be given before or after surgery.
You may have your treatment in an outpatient part of the hospital, at the doctor’s office, or at home. Rarely, you may need to stay in the hospital.
Chemotherapy is usually given in cycles. Each cycle has a treatment period followed by a rest period.
If the drugs are given by vein or taken by mouth, the side effects depend mainly on which drugs are given and how much. Chemotherapy kills fast-growing cancer cells, but the drugs can also harm normal cells that divide rapidly:
- Blood cells: When drugs lower the levels of healthy blood cells, you’re more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. If your levels are low, your health care team may stop the chemotherapy for a while or reduce the dose of the drug. There are also medicines that can help your body make new blood cells.
- Cells in hair roots: Chemotherapy may cause hair loss. If you lose your hair, it will grow back after treatment, but the color and texture may be changed.
- Cells that line the digestive system: Chemotherapy can cause a poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your health care provider can give you medicines and suggest other ways to help with these problems. They usually go away when treatment ends.
Some drugs used for upper urinary tract cancer may also cause tingling or numbness in your hands and feet. Your health care team can suggest ways to control many of these side effects.
Radiation
High-energy radiation is used to destroy cancer cells with minimal damage to nearby organs. Radiation is rarely used for urothelial tumors since the area to be treated is so small and hard to target. Your doctor will only use radiation if he or she can avoid damaging nearby tissue.
Renal pelvis cancer prognosis
When an upper urinary tract cancer is caught early, the chances of surgical cure are good. Overall the outlook depends on 2 factors:
- How aggressive the cancer cells are. Low-grade disease is less aggressive and has a lower chance of spreading to other organs. High-grade disease is more aggressive with a higher chance of spreading.
- How far the tumor has spread. If the tumor does not involve nearby lymph nodes or other tissue, there is a high likelihood of cure. Additional treatments would not be needed. But if the cancer has spread to nearby lymph nodes, your doctor will probably recommend additional systemic chemotherapy.
Recovery and Follow-up
Your recovery depends on your treatment. A minimally invasive approach will lead to a quicker recovery than traditional open surgery. The best treatment option is often the one that offers the best long-term outcome. If your surgeon has removed 1 kidney and the remaining kidney works well, your quality of life and future health should not be seriously affected. One good kidney can usually do the work of 2.
After treatment you will need continued check-ups to watch for regrowth of cancer. Upper urinary tract cancer is more likely to occur in multiple places than other cancers. For the first few years after treatment, your doctor will perform cystoscopy and other exams. These visits should continue at least yearly throughout your life.
Recurrence
Urothelial tumors often come back in new places in the urinary tract, even if the initial growth was on the surface of the urinary tract. New tumors develop lower in the ureter or the bladder in about 30 out of every 100 patients who have had upper tract tumors removed. If the lower ureter on the side of the cancer was not removed, it should be checked regularly with retrograde X-rays or a scope. For patients with upper tract tumors, it is rare for cancer to come back in the opposite upper urinary tract (less than 3 to 5 out of 100 patients).
Renal pelvis obstruction
Renal pelvis obstruction or ureteropelvic junction obstruction is when part of the renal pelvis blocked. The blockage slows or stops the flow of urine out of the kidney. Urine can then build up and damage the kidney. Sometimes surgery is needed to improve the flow of urine and other times the problem will improve on its own.
Renal pelvis obstruction causes
Most often renal pelvis obstruction (ureteropelvic junction) is congenital. This means that children are born with this health issue. It is not known how to prevent it. One in 1,500 children are born with renal pelvis obstruction (ureteropelvic junction). The blockage occurs as the kidney is forming. Today most cases are found using ultrasound before birth. Though it occurs less often in adults, renal pelvis obstruction (ureteropelvic junction) may happen after kidney stones, surgery or upper urinary tract swelling.
In renal pelvis obstruction (ureteropelvic junction), the kidney makes urine faster than it can be drained through the renal pelvis into the ureter. This causes urine to pool in the kidney, which leads to kidney swelling (hydronephrosis). Often, only 1 kidney is affected. The enlarged kidney is easily seen on ultrasound. For this reason, a doctor can often predict renal pelvis obstruction (ureteropelvic junction) before a baby is born.
Renal pelvis obstruction symptoms
With the use of ultrasound, most cases of renal pelvis obstruction (ureteropelvic junction) are found long before birth. After birth, signs in infants and children are:
- abdominal mass
- urinary tract infection with fever
- flank pain (pain in the upper abdomen or back, mostly with fluid intake)
- kidney stones
- bloody urine
- vomiting
- poor growth in infants
Renal pelvis obstruction (ureteropelvic junction) may also cause pain without an infection.
Some cases of renal pelvis obstruction (ureteropelvic junction) are not clear. Urine may drain normally at times, and at other times be blocked. This causes pain that comes and goes. The general belief is that most children are not in pain unless the urine becomes infected or the blockage gets worse.
Renal pelvis obstruction diagnosis
While ultrasound helps your doctor see the kidneys, more tests are needed to confirm renal pelvis obstruction (ureteropelvic junction). To make a proper diagnosis, your urologist must see how well urine is produced and drained. There are several tests that can be done.
Blood samples and urine samples may be taken. The BUN (blood urea nitrogen) and creatinine tests find if the kidney is working well as it filters the blood.
An intravenous pyelogram (IVP) was often used in the past. In this test, a dye is injected into the bloodstream. An X-ray is used to see the kidneys remove the dye from the blood. As the dye passes through urine, your doctor can see if the kidney, renal pelvis and ureter look normal.
A nuclear renal scan is similar to an IVP but is more modern. This test uses radioactive material instead of dye. The material can be seen with a special camera. This test gives the doctor good information about how the kidney is working and how much blockage there is.
CT scans are sometimes used in the emergency room to find out why children are having severe pain. A CT scan can easily show the obstructed kidney if that is the cause of the pain. Magnetic resonance imaging (MRI) is also used to look at the kidneys, ureters and the bladder. But MRI is expensive and not used everywhere.
Siblings need screening for renal pelvis obstruction (ureteropelvic junction) only if they show signs. There have been some cases in which several members of a family have renal pelvis obstruction (ureteropelvic junction), but the majority of cases are individual.
Renal pelvis obstruction treatment
Treatment is not always necessary, and experts have different opinions. It is important to know that poor drainage in infants and children younger than 18 months may be temporary. Many infants with good kidney function and poor drainage at first will have much improvement after a few months. On the other hand, in some infants the obstruction won’t improve it will get worse.
Young patients with an enlarged kidney are first followed with repeat ultrasounds and, if there is any concern, repeat nuclear scans. Sudden improvement can occur. If so, it often occurs in the first 18 months of life. If urine flow does not improve for an infant and obstruction remains, then surgery is needed. Adults may find treatment in other ways.
Open surgery
The classic treatment for infants is an operation called pyeloplasty. In this surgery the ureteropelvic junction is removed, and the ureter is reattached to the renal pelvis to create a wide opening. This lets the urine drain quickly and easily. It also relieves symptoms and the risk of infection. The surgeon’s cut is usually 2 to 3 inches long, just below the ribs. This process usually takes a few hours with a great success rate (95% success). The patient may have to stay in the hospital for a day or 2 after surgery. Drainage tubes can be used to promote healing.
Minimally Invasive Surgery
Newer surgical options are less invasive, such as:
- laparoscopic pyeloplasty with or without a surgical robot, or
- internal incision of the ureteropelvic junction using a camera and scope inserted through the bladder
Laparoscopic Pyeloplasty
In this method the surgeon works through a small cut in the abdominal wall. A surgical robot can help guide the tools. The clear advantages of this method are less pain and nausea, especially in older children and adults. But scarring in the abdomen can result. This treatment has led to very successful results.
Internal Incision
With this option a wire is inserted through the ureter. This wire is used to cut the tight and narrow ureteropelvic junction from the inside. A special ureteral drain is left in for a few weeks and then removed. The ureteropelvic junction heals in a more open manner but the surgery may need to be repeated. The success rates are lower than with open or minimally invasive surgery. But the advantages also include less pain and nausea.
After Treatment
Patients usually recover quickly. After surgery the ureter may be swollen for a while. Some have pain for a few days after surgery. Kidney drainage can also remain poor, but often gets better as the area heals. The doctor uses ultrasound a few weeks after surgery to check for hydronephrosis (swollen kidney).
Sometimes a drainage tube is left in place to help drain the kidney while it heals. The appearance of the kidney will improve with time, though it will not look normal.
If the other kidney is normal, children can participate in sports or other activities when the blocked kidney responds well to treatment. Once the UPJ obstruction is fixed, it almost never comes back.
Note that patients who have had renal pelvis obstruction (ureteropelvic junction) may have a slightly greater risk of future kidney stones or infection. This is because the kidneys may still contain some pooled urine, even though overall drainage is improved. Sometimes a child who had some obstruction as an infant, which improved naturally, will later have signs of obstruction that call for surgery.
Renal pelvis stone
Urine contains many dissolved minerals and salts. When your urine has high levels of these minerals and salts, stones can form. The scientific name for a kidney stone is renal calculus or nephrolith. You may hear health care professionals call this condition nephrolithiasis, urolithiasis, or urinary stones. Kidney stones can start small but can grow larger in size. They can even fill the inner hollow structures of the kidney. Some stones stay in the kidney, and often do not cause any symptoms and can go undiagnosed. Others can travel down the ureter (the tube between the kidney and the bladder). If the stone reaches the bladder, it can be passed out through urine. If the stone becomes lodged in the ureter, it blocks the urine flow. This is often very painful. When the stone blocks the flow of urine, it can cause the kidney to swell (hydronephrosis). If a stone leaves the kidney and gets stuck in the ureter, it is called a ureteral stone.
The following may be signs of kidney stones that need a doctor’s help:
- Extreme pain in your back or side that will not go away
- Blood in your urine
- Fever and chills
- Vomiting
- Urine that smells bad or looks cloudy
- A burning feeling when you urinate
Your doctor will diagnose a kidney stone with urine, blood, and imaging tests.
Kidney stone disease is one of the most common problems of the urinary system. More than 1 million Americans will get a kidney stone this year. The number of people in the U.S. with stones is rising. In 1980, about 3 in every 100 people got a stone at some point in their life. In 1994, that number rose to about 5 in every 100 people. At this time, about 1 in 10 Americans will have a kidney stone during his or her lifetime (about 11 percent of men and 6 percent of women). Children getting kidney stones has also become more common in recent years.
Race, gender and ethnicity play a part in who may get kidney stones. Whites are more likely to get kidney stones than African-Americans or other races. Men get kidney stones more often than women. Still, the number of women getting kidney stones is rising.
If you have a family history of kidney stones, you are more likely to develop them. You are also more likely to develop kidney stones again if you’ve had them once.
You may also be more likely to develop a kidney stone if you don’t drink enough liquids.
Kidney stones are often very painful, and can keep happening in some people. Kidney stone attacks lead to over 2 million visits to the doctor and over 600,000 visits to the emergency room each year. People tend to get stones in midlife.
Who is more likely to develop kidney stones?
You are more likely to develop kidney stones if you have certain conditions, including:
- a blockage of the urinary tract
- chronic, or long-lasting, inflammation of the bowel
- cystic kidney diseases , which are disorders that cause fluid-filled sacs to form on the kidneys
- cystinuria
- digestive problems or a history of gastrointestinal tract surgery
- gout , a disorder that causes painful swelling of the joints
- hypercalciuria , a condition that runs in families in which urine contains unusually large amounts of calcium; this is the most common condition found in
- people who form calcium stones
- hyperoxaluria , a condition in which urine contains unusually large amounts of oxalate
- hyperparathyroidism, a condition in which the parathyroid glands release too much parathyroid hormone, causing extra calcium in the blood
- hyperuricosuria, a disorder in which too much uric acid is in the urine
- obesity
- repeated, or recurrent, urinary tract infections (UTIs)
- renal tubular acidosis, a disease that occurs when the kidneys fail to remove acids into the urine, which causes a person’s blood to remain too acidic
People who take certain medicines
You are more likely to develop kidney stones if you are taking one or more of the following medicines over a long period of time:
- diuretics, often called water pills, which help rid your body of water
- calcium-based antacids
- indinavir , a protease inhibitor used to treat HIV infection
- topiramate , an anti-seizure medication
Type of kidney stones
You probably have one of four main types of kidney stones. Treatment for kidney stones usually depends on their size, location, and what they are made of.
Calcium stones
Calcium stones, including calcium oxalate stones and calcium phosphate stones, are the most common types of kidney stones (80% of kidney stones). Calcium oxalate stones are more common than calcium phosphate stones.
Some people have too much calcium in their urine, raising their risk. Even with normal amounts of calcium in the urine, calcium stones may form for other reasons.
Calcium from food does not increase your chance of having calcium oxalate stones. Normally, extra calcium that isn’t used by your bones and muscles goes to your kidneys and is flushed out with urine. When this doesn’t happen, the calcium stays in the kidneys and joins with other waste products to form a kidney stone.
Uric acid stones
A uric acid stone (5 to 10% of kidney stones) may form when your urine contains too much acid. Eating a lot of fish, shellfish, and meat—especially organ meat—may increase uric acid in urine.
Uric acid crystals do not dissolve well in acidic urine. Instead it will form a uric acid stone.
Having acidic urine may come from:
- Being overweight
- Chronic diarrhea
- Type 2 diabetes (high blood sugar)
- Gout
- A diet that is high in animal protein and low in fruits and vegetables
Struvite stones
Struvite stones (10% of kidney stones) may form after you have a urinary tract infection (UTI). They can develop suddenly and become large quickly.
Some bacteria make the urine less acidic and more basic or alkaline. Magnesium ammonium phosphate (struvite) stones form in alkaline urine. Struvite stones are often large, with branches, and they often grow very fast. People who get chronic urinary tract infections (UTIs), such as those with long-term tubes in their kidneys or bladders, or people with poor bladder emptying due to neurologic disorders (paralysis, multiple sclerosis, and spina bifida) are at the highest risk for developing struvite stones.
Cystine stones
Cystine is an amino acid that is in certain foods. It is one of the building blocks of protein. Cystine stones (less than 1% of kidney stones) result from a disorder called cystinuria (too much cystine in the urine) that is passed down through families. Cystinuria is a rare, inherited metabolic disorder that causes the amino acid cystine to leak through your kidneys and into the urine. When high amounts of cystine are in the urine, it causes stones to form. Cystine stones often start to form in childhood.
Renal pelvis stone causes
Kidney stones are caused by high levels of calcium, oxalate, and phosphorus in the urine. These minerals are normally found in urine and do not cause problems at low levels.
Certain foods may increase the chances of having a kidney stone in people who are more likely to develop them.
Renal pelvis stone prevention
To help prevent future kidney stones, you also need to know what caused your previous kidney stones. Once you know what type of kidney stone you had, a health care professional can help you make changes to your eating, diet, and nutrition to prevent future kidney stones.
Drinking liquids
In most cases, drinking enough liquids each day is the best way to help prevent most types of kidney stones. Drinking enough liquids keeps your urine diluted and helps flush away minerals that might form stones.
Though water is best, other liquids such as citrus drinks may also help prevent kidney stones. Some studies show that citrus drinks, such as lemonade and orange juice, protect against kidney stones because they contain citrate, which stops crystals from turning into stones.
Unless you have kidney failure, you should drink six to eight, 8-ounce glasses a day. If you previously had cystine stones, you may need to drink even more. Talk with a health care professional if you can’t drink the recommended amount due to other health problems, such as urinary incontinence, urinary frequency, or kidney failure.
The amount of liquid you need to drink depends on the weather and your activity level. If you live, work, or exercise in hot weather, you may need more liquid to replace the fluid you lose through sweat. A health care professional may ask you to collect your urine for 24 hours to determine the amount of urine you produce a day. If the amount of urine is too low, the health care professional may advise you to increase your liquid intake.
Medicines
If you have had a kidney stone, a health care professional also may prescribe medicines to prevent future kidney stones. Depending on the type of kidney stone you had and what type of medicine the health care professional prescribes, you may have to take the medicine for a few weeks, several months, or longer.
For example, if you had struvite stones, you may have to take an oral antibiotic for 1 to 6 weeks, or possibly longer.
If you had another type of stone, you may have to take a potassium citrate tablet 1 to 3 times daily. You may have to take potassium citrate for months or even longer until a health care professional says you are no longer at risk for kidney stones.
Talk with a health care professional about your health history prior to taking kidney stone medicines. Some kidney stone medicines have minor to serious side effects. Side effects are more likely to occur the longer you take the medicine and the higher the dose. Tell the health care professional about any side effects that occur when you take kidney stone medicine.
Table 1. Kidney stone medications
| Type of kidney stone | Possible medicines prescribed by your doctor |
|---|---|
| Calcium Stones |
|
| Uric Acid Stones |
|
| Struvite Stones |
|
| Cystine Stones |
|
Renal pelvis stone symptoms
Stones in the kidney often do not cause any symptoms and can go undiagnosed. When a stone leaves the kidney, it can travel to the bladder and may get stuck in the ureter. When the stone blocks the flow of urine, it can cause the kidney to swell (hydronephrosis), This is often very painful.
Symptoms of kidney stones include:
- Sharp cramping pains in your back, side, lower abdomen, or groin. The pain often moves to the lower abdomen or groin. Some women say the pain is worse than childbirth labor pains. The pain can start quickly and come in waves. It can come and go as the body tries to get rid of the stone.
- Pink, red, or brown blood in your urine, also called hematuria (urine that is dark or red due to blood)
- A feeling of intense need to urinate
- Nausea and vomiting
- Men may feel pain at the tip of their penis
- Going to the bathroom more often or having a burning feeling when you go
- Pain while urinating
- Inability to urinate or can only urinate a small amount
- Cloudy or bad-smelling urine
See a health care professional right away if you have any of these symptoms. These symptoms may mean you have a kidney stone or a more serious condition.
Your pain may last for a short or long time or may come and go in waves. Along with pain, you may have
- nausea
- vomiting
Other symptoms include
- fever
- chills
Renal pelvis stone complications
Complications of kidney stones are rare if you seek treatment from a health care professional before problems occur.
If kidney stones are not treated, they can cause
- hematuria, or blood in the urine
- severe pain
- UTIs, including kidney infections
- loss of kidney function
Renal pelvis stone diagnosis
Health care professionals use your medical history, a physical exam, and lab and imaging tests to diagnose kidney stones.
A health care professional will ask if you have a history of health conditions that make you more likely to develop kidney stones. The health care professional also may ask if you have a family history of kidney stones and about what you typically eat. During a physical exam, the health care professional usually examines your body. The health care professional will ask you about your symptoms.
Health care professionals may use lab or imaging tests to diagnose kidney stones.
Lab tests
Urine tests can show whether your urine contains high levels of minerals that form kidney stones. Urine and blood tests can also help a health care professional find out what type of kidney stones you have.
Urinalysis. Urinalysis involves a health care professional testing your urine sample. You will collect a urine sample at a doctor’s office or at a lab, and a health care professional will test the sample. Urinalysis can show whether your urine has blood in it and minerals that can form kidney stones. White blood cells and bacteria in the urine mean you may have a urinary tract infection.
Blood tests. A health care professional may take a blood sample from you and send the sample to a lab to test. The blood test can show if you have high levels of certain minerals in your blood that can lead to kidney stones.
Imaging tests
Health care professionals use imaging tests to find kidney stones. The tests may also show problems that caused a kidney stone to form, such as a blockage in the urinary tract or a birth defect. You do not need anesthesia for these imaging tests.
Abdominal x-ray. An abdominal x-ray is a picture of the abdomen that uses low levels of radiation and is recorded on film or on a computer. An x-ray technician takes an abdominal x-ray at a hospital or outpatient center, and a radiologist reads the images. During an abdominal x-ray, you will lie on a table or stand up. The x-ray technician will position the x-ray machine over or in front of your abdomen and ask you to hold your breath so the picture won’t be blurry. The x-ray technician then may ask you to change position for additional pictures. Abdominal x-rays can show the location of kidney stones in the urinary tract. Not all stones are visible on abdominal x-ray.
Computed tomography (CT) scans. CT scans use a combination of x-rays and computer technology to create images of your urinary tract. Although a CT scan without contrast medium is most commonly used to view your urinary tract, a health care professional may give you an injection of contrast medium. Contrast medium is a dye or other substance that makes structures inside your body easier to see during imaging tests. You’ll lie on a table that slides into a tunnel-shaped device that takes the x-rays. CT scans can show the size and location of a kidney stone, if the stone is blocking the urinary tract, and conditions that may have caused the kidney stone to form.
Renal pelvis stone treatment
Health care professionals usually treat kidney stones based on their size, location, and what type they are.
Small kidney stones may pass through your urinary tract without treatment. If you’re able to pass a kidney stone, a health care professional may ask you to catch the kidney stone in a special container. A health care professional will send the kidney stone to a lab to find out what type it is. A health care professional may advise you to drink plenty of liquids if you are able to help move a kidney stone along. The health care professional also may prescribe pain medicine.
Larger kidney stones or kidney stones that block your urinary tract or cause great pain may need urgent treatment. If you are vomiting and dehydrated, you may need to go to the hospital and get fluids through an IV.
People with hyperparathyroidism, a condition that results in too much calcium in the blood, sometimes develop calcium stones. Treatment for hyperparathyroidism may include surgery to remove the abnormal parathyroid gland. Removing the parathyroid gland cures hyperparathyroidism and can prevent kidney stones. Surgery sometimes causes complications, including infection.
Kidney stone removal
A urologist can remove the kidney stone or break it into small pieces with the following treatments:
Shock wave lithotripsy. The doctor can use shock wave lithotripsy to blast the kidney stone into small pieces. The smaller pieces of the kidney stone then pass through your urinary tract. A doctor can give you anesthesia during this outpatient procedure.
Cystoscopy and ureteroscopy. During cystoscopy, the doctor uses a cystoscope to look inside the urethra and bladder to find a stone in your urethra or bladder. During ureteroscopy, the doctor uses a ureteroscope, which is longer and thinner than a cystoscope, to see detailed images of the lining of the ureters and kidneys. The doctor inserts the cystoscope or ureteroscope through the urethra to see the rest of the urinary tract. Once the stone is found, the doctor can remove it or break it into smaller pieces. The doctor performs these procedures in the hospital with anesthesia. You can typically go home the same day.
Percutaneous nephrolithotomy. The doctor uses a thin viewing tool, called a nephroscope, to locate and remove the kidney stone. The doctor inserts the tool directly into your kidney through a small cut made in your back. For larger kidney stones, the doctor also may use a laser to break the kidney stones into smaller pieces. The doctor performs percutaneous nephrolithotomy in a hospital with anesthesia. You may have to stay in the hospital for several days after the procedure.
After these procedures, sometimes the urologist may leave a thin flexible tube, called a ureteral stent, in your urinary tract to help urine flow or a stone to pass. Once the kidney stone is removed, your doctor sends the kidney stone or its pieces to a lab to find out what type it is.
The health care professional also may ask you to collect your urine for 24 hours after the kidney stone has passed or been removed. The health care professional can then measure how much urine you produce in a day, along with mineral levels in your urine. You are more likely to form stones if you don’t make enough urine each day or have a problem with high mineral levels.
Renal pelvis stone diet
Drinking enough liquid, mainly water, is the most important thing you can do to prevent kidney stones. Unless you have kidney failure, many health care professionals recommend that you drink six to eight, 8-ounce glasses a day. Talk with a health care professional about how much liquid you should drink.
Studies have shown that the Dietary Approaches to Stop Hypertension (DASH) diet can reduce the risk of kidney stones.
Studies have shown that being overweight increases your risk of kidney stones. A dietitian can help you plan meals to help you lose weight.
Does the type of kidney stone I had affect food choices I should make?
Yes. If you have already had kidney stones, ask your health care professional which type of kidney stone you had. Based on the type of kidney stone you had, you may be able to prevent kidney stones by making changes in how much sodium, animal protein, calcium, or oxalate is in the food you eat.
You may need to change what you eat and drink for these types of kidney stones:
- Calcium Oxalate Stones
- Calcium Phosphate Stones
- Uric Acid Stones
- Cystine Stones
A dietitian who specializes in kidney stone prevention can help you plan meals to prevent kidney stones. Find a dietitian who can help you.
Calcium Oxalate Stones
Reduce oxalate
If you’ve had calcium oxalate stones, you may want to avoid these foods to help reduce the amount of oxalate in your urine:
- nuts and nut products
- peanuts—which are legumes, not nuts, and are high in oxalate
- rhubarb
- spinach
- wheat bran
Talk with a health care professional about other food sources of oxalate and how much oxalate should be in what you eat.
Reduce sodium
Your chance of developing kidney stones increases when you eat more sodium. Sodium is a part of salt. Sodium is in many canned, packaged, and fast foods. It is also in many condiments, seasonings, and meats.
Talk with a health care professional about how much sodium should be in what you eat.
Limit animal protein
Eating animal protein may increase your chances of developing kidney stones.
A health care professional may tell you to limit eating animal protein, including:
- beef, chicken, and pork, especially organ meats
- eggs
- fish and shellfish
- milk, cheese, and other dairy products
Although you may need to limit how much animal protein you eat each day, you still need to make sure you get enough protein. Consider replacing some of the meat and animal protein you would typically eat with beans, dried peas, and lentils, which are plant-based foods that are high in protein and low in oxalate.
Talk with a health care professional about how much total protein you should eat and how much should come from animal or plant-based foods.
Get enough calcium from foods
Even though calcium sounds like it would be the cause of calcium stones, it’s not. In the right amounts, calcium can block other substances in the digestive tract that may cause stones. Talk with a health care professional about how much calcium you should eat to help prevent getting more calcium oxalate stones and to support strong bones. It may be best to get calcium from low-oxalate, plant-based foods such as calcium-fortified juices, cereals, breads, some kinds of vegetables, and some types of beans. Ask a dietitian or other health care professional which foods are the best sources of calcium for you.
Calcium Phosphate Stones
Reduce sodium
Your chance of developing kidney stones increases when you eat more sodium. Sodium is a part of salt. Sodium is in many canned, packaged, and fast foods. It is also in many condiments, seasonings, and meats.
Talk with a health care professional about how much sodium should be in what you eat.
Limit animal protein
Eating animal protein may increase your chances of developing kidney stones.
A health care professional may tell you to limit eating animal protein, including
- beef, chicken, and pork, especially organ meats
- eggs
- fish and shellfish
- milk, cheese, and other dairy products
Although you may need to limit how much animal protein you have each day, you still need to make sure you get enough protein. Consider replacing some of the meat and animal protein you would typically eat with some of these plant-based foods that are high in protein:
- legumes such as beans, dried peas, lentils, and peanuts
- soy foods, such as soy milk, soy nut butter, and tofu
- nuts and nut products, such as almonds and almond butter, cashews and cashew butter, walnuts, and pistachios
- sunflower seeds
Talk with a health care professional about how much total protein you should eat and how much should come from animal or plant-based foods.
Get enough calcium from foods
Even though calcium sounds like it would be the cause of calcium stones, it’s not. In the right amounts, calcium can block other substances in the digestive tract that may lead to stones. Talk with a health care professional about how much calcium you should eat to help prevent getting more calcium phosphate stones and to support strong bones. It may be best to get calcium from plant-based foods such as calcium-fortified juices, cereals, breads, some kinds of vegetables, and some types of beans. Ask a dietitian or other health care professional which foods are the best sources of calcium for you.
Uric Acid Stones
Limit animal protein
Eating animal protein may increase your chances of developing kidney stones.
A health care professional may tell you to limit eating animal protein, including
- beef, chicken, and pork, especially organ meats
- eggs
- fish and shellfish
- milk, cheese, and other dairy products
Although you may need to limit how much animal protein you have each day, you still need to make sure you get enough protein. Consider replacing some of the meat and animal protein you would typically eat with some of these plant-based foods that are high in protein:
- legumes such as beans, dried peas, lentils, and peanuts
- soy foods, such as soy milk, soy nut butter, and tofu
- nuts and nut products, such as almonds and almond butter, cashews and cashew butter, walnuts, and pistachios
- sunflower seeds
Talk with a health care professional about how much total protein you should eat and how much should come from animal or plant-based foods.
Losing weight if you are overweight is especially important for people who have had uric acid stones.
Cystine Stones
Drinking enough liquid, mainly water, is the most important lifestyle change you can make to prevent cystine stones. Talk with a health care professional about how much liquid you should drink.
- Han DS, Yuk SM, Youn CS, Park G, Sul HJ, Jang H. Primary mucinous cystadenocarcinoma of the renal pelvis misdiagnosed as ureteropelvic junction stenosis with renal pelvis stone: a case report and literature review. World J Surg Oncol. 2015;13:324. Published 2015 Nov 26. doi:10.1186/s12957-015-0739-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4662030[↩]
- Abbas M, Kramer MW, Spieker T, Herrman TR, Merseburger AS, Muller KM, Kuczyk MA, Becker JU, Kreipe HH. Primary mucinous adenocarcinoma of the renal pelvis with carcinoma in situ in the ureter. J Egypt Natl Canc Inst. 2014;26(1):51–54. doi: 10.1016/j.jnci.2013.11.002[↩]
- Hasebe M, Serizawa S, Chino S. On a case of papillary cystadenocarcinoma following malignant degeneration of a papillary adenoma in the kidney pelvis. Yokohama Med Bull. 1960;11:491–500[↩]
- Shah VB, Amonkar GP, Deshpande JR, Bhalekar H. Mucinous adenocarcinoma of the renal pelvis with pseudomyxoma peritonei. Indian J Pathol Microbiol. 2008;51(4):536–537. doi: 10.4103/0377-4929.43753[↩]
- Gangane N, Anshu, Shende N, Sharma SM. Mucinous cystadenoma arising from renal pelvis: a report of 2 cases. Urol J. 2008;5(3):197–199[↩]