Contents
What is rotavirus
Rotavirus is a highly contagious virus that can cause gastroenteritis (inflammation of the stomach and intestines) and is spread in feces (poop). Rotavirus is most often spread when someone who is infected does not wash their hands properly after going to the toilet. The gastroenteritis it causes usually begins with the symptoms of severe watery diarrhea and is sometimes accompanied by vomiting, fever, and abdominal pain. Infants and young children are most likely to get rotavirus disease and can lead to serious dehydration (loss of body fluid) in the very young. They can become severely dehydrated and need to be hospitalized and can even die if the dehydration is not treated. Very young children have the highest risk of severe complications, which can result from extreme dehydration. A very small number of children die from rotavirus infection each year.
Almost all children in the U.S. are likely to be infected with rotavirus before their 5th birthday 1. The child may develop a tummy ache and they may also have a fever (high temperature) of 100.4ºF (38ºC) or above.
The symptoms of diarrhea usually pass within three to eight days. Most diarrhea symptoms in children will not last more than two weeks.
Rotavirus infections happen most often in the winter and spring. It is very easy for children with rotavirus infection to spread it to other children and sometimes to adults. Once a child gets rotavirus, it takes about two days to become sick.
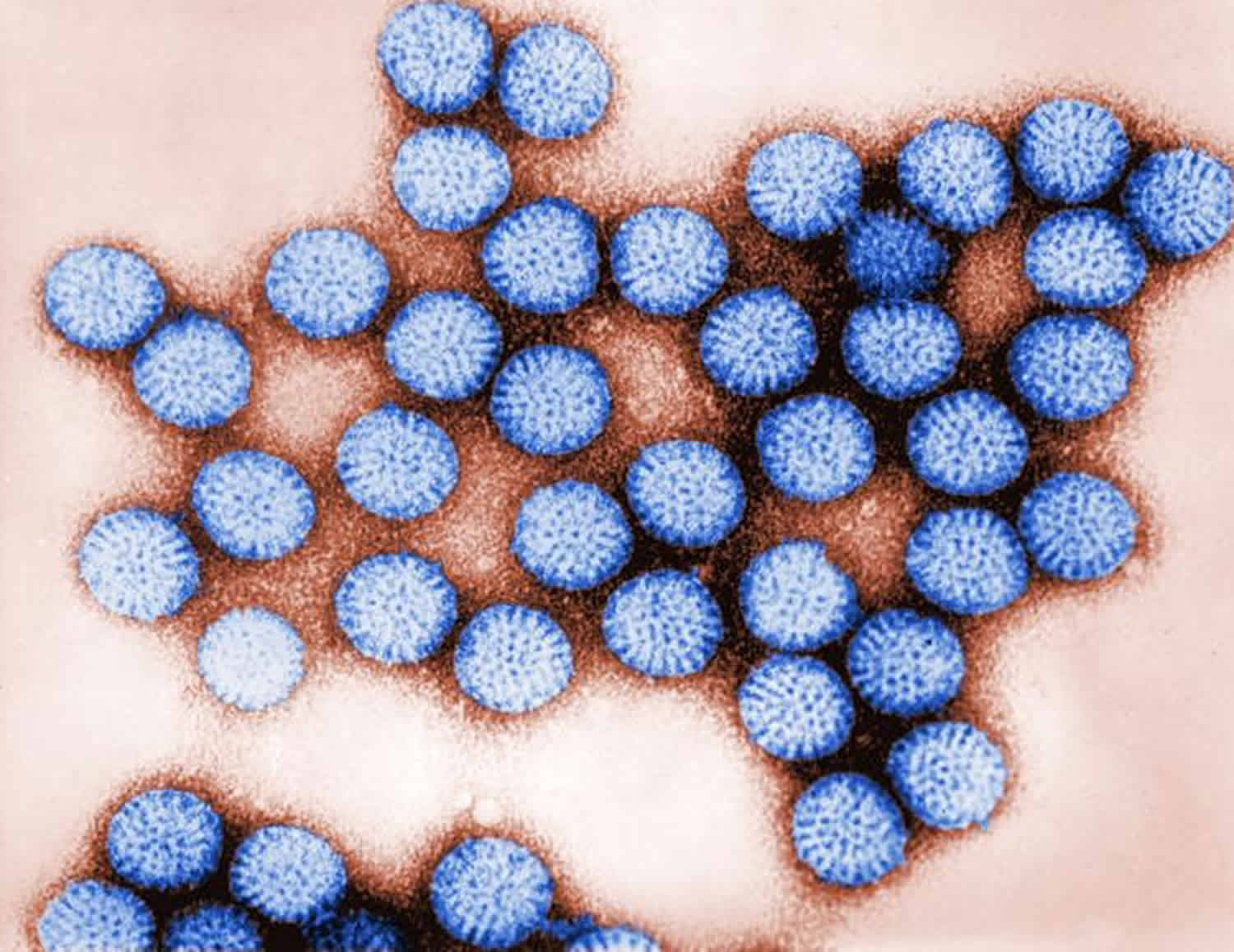
Rotavirus has a characteristic wheel-like appearance when viewed by an electron microscope. The name rotavirus is derived from the Latin word rota, meaning “wheel.” Rotaviruses are non-enveloped, double-shelled viruses. The genome is composed of 11 segments of double-stranded RNA, which code for six structural and five nonstructural proteins. The virus is stable in the environment.
Worldwide, rotavirus is the most common cause of viral gastroenteritis in children, who are usually infected when they put their fingers or other objects contaminated with rotavirus into their mouths. The rotavirus infection is most severe in infants and young children. Adults infected with rotavirus may not have symptoms, but can still spread the illness — of particular concern in institutional settings because infected adults unknowingly can pass the virus to others. A vaccine against rotavirus gastroenteritis is available in some countries, including the United States, and appears to be effective in preventing the infection. Two oral rotavirus vaccines are available for young infants — RotaTeq® (RV5) and Rotarix® (RV1).
There is no medicine to treat rotavirus infection. Antibiotics aren’t effective against viruses, and overusing them can contribute to the development of antibiotic-resistant strains of bacteria. The most important treatment for gastroenteritis is to drink fluids. To prevent dehydration, have your child drink plenty of liquids. Your health care provider may recommend oral rehydration drinks. Some children need to go to the hospital for IV fluids.
The dehydration caused by the symptoms of rotavirus gastroenteritis can be treated with rehydration solutions available from pharmacies. These are the best fluids to use in cases of gastroenteritis, especially for children. Frequent sips are easier for young children than a large amount all at once. Keep drinking regularly even if you are vomiting.
- If you have a baby or young child with gastroenteritis, it’s a good idea to have them checked by a doctor for dehydration.
If you can’t get any rehydration solutions, or your child refuses to drink it, giving diluted fruit juice (one part juice to four parts of water) is reasonable. You could try a cube of ice or an iceblock if your child won’t drink. Avoid milk and other dairy products and do not give juice, sodas, sports drinks or other soft drinks as the sugar may make the diarrhea worse. It is fine to eat once you feel like it.
Babies can continue milk feeds throughout the illness, with rehydration fluid between feeds. Medication for nausea or diarrhea can be useful for adults, but may not be safe for kids.
If you are very sick with gastroenteritis, you may need to go to hospital where you may be put on a drip.
Is rotavirus just a kids’ illness?
Adults can be infected with rotavirus, but they tend to have milder cases. Young children between the ages of six months and 24 months are at greatest risk for severe rotavirus disease. There’s no reliable way to predict how rotavirus will affect your child. New and expecting parents should speak with their child’s doctor at or before their first well baby visit.
Rotavirus complications
The main complication of rotavirus gastroenteritis is dehydration — a severe loss of water and essential salts and minerals. If you’re healthy and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn’t be a problem.
Infants, older adults and people with suppressed immune systems may become severely dehydrated when they lose more fluids than they can replace. Hospitalization might be needed so that lost fluids can be replaced intravenously. Dehydration can be fatal, but rarely.
Why can dehydration be serious for infants and small children?
The rapid loss of fluids that accompanies vomiting and diarrhea can lead to dehydration, during which the body does not have the water and salts (or electrolytes) it needs. Babies under one year of age, and especially those who have a fever, become dehydrated most easily because of their smaller body weights. It is sometimes necessary for children to be rehydrated using intravenous fluids. In the most severe cases of dehydration, a child may even develop convulsions or go into shock, which in rare cases can be life threatening.
What should I do if I think my child is experiencing rotavirus symptoms?
If you think your child is experiencing rotavirus you should see your child’s doctor. Rotavirus in young children and babies can be very upsetting for parents as well as for the child, so quick recognition of its symptoms is very important. In a severe case, a child could have as many as 20 diarrheal stools or vomiting episodes in a 24-hour period.
Dehydration is one of the most significant potential complications for infected children. An infant or toddler may need to be treated with intravenous (IV) fluids in a hospital.
Home care therapy can be used to help manage uncomplicated cases of diarrhea. The child is typically given fluids, such as oral electrolyte solutions, to replace those lost through diarrhea and vomiting. Severe vomiting, however, can make such oral rehydration fluid therapy difficult.
Rotavirus transmission
The primary mode of transmission is the fecal-oral route, usually through direct contact between people. Because the virus is stable in the environment, transmission also can occur through ingestion of contaminated water or food and contact with contaminated surfaces or objects.
People who are infected with rotavirus shed the virus in their stool (poop). This is how rotavirus gets into the environment and can infect other people. People shed rotavirus the most, and are more likely to infect others, when they have symptoms and during the first 3 days after they recover. People with rotavirus can also infect others before they have symptoms.
In the United States and other countries with a temperate climate, the disease has a winter and spring seasonal pattern, with annual epidemics occurring from December through June. The highest rates of illness occur among infants and young children, and most children are infected by age 5 . Adults can also be infected, though disease tends to be milder.
If you get rotavirus particles in your mouth, you can get sick. This can happen if you:
- put your unwashed hands that are contaminated with poop into your mouth
- touch contaminated objects or surfaces then put your fingers in your mouth
- eat contaminated food
Rotavirus spreads easily among infants and young children. They can spread rotavirus to family members and other people with whom they have close contact. Good hygiene like handwashing and cleanliness are important, but are not enough to control the spread of the disease. Rotavirus vaccination is the best way to protect your child from rotavirus disease.
Children are most likely to get rotavirus in the winter and spring (November through June).
How do you get rotavirus?
Rotavirus can be spread both before and after children show signs of being sick. Children can catch a rotavirus infection if they put their fingers in their mouths after touching something that has been contaminated by the stool of an infected person. Usually this happens when children forget to wash their hands often enough, especially before eating and after using the toilet.
People who care for children can also spread the virus, especially if they do not wash their hands after changing diapers. Rotavirus is resistant to most disinfectant cleaners, including anti-bacterial products. The virus can survive for a few hours on human hands and for days on hard and dry surfaces. As a result, rotavirus can be easily spread in families, and outbreaks can occur in childcare centers, playgroups, and hospitals.
Can I keep my child from being exposed to rotavirus?
It is difficult to keep a child from being exposed to rotavirus. Better hygiene and sanitation have not been very good at reducing rotavirus disease. Because the virus is so widespread, even the cleanest environments can be infected. Children who have previously had rotavirus may be infected again, but repeat infections tend to be less severe.
Rotavirus incubation period
Rotavirus incubation period is 1 to 3 days 2. Following the incubation period, the illness often begins abruptly, and vomiting often precedes the onset of diarrhea. Gastrointestinal symptoms generally resolve in 3–7 days. Up to one-third of patients have a temperature of >102°F (>39°C). Severe, dehydrating rotavirus infection occurs primarily among unvaccinated children 3–35 months of age 3.
How long does rotavirus last?
The symptoms of diarrhea usually pass within three to eight days. Most diarrhea symptoms in children will not last more than two weeks.
People who are infected with rotavirus shed the virus in their stool (poop). This is how rotavirus gets into the environment and can infect other people.
Rotavirus symptoms
Rotavirus disease is most common in infants and young children. However, older children and adults also can get sick from rotavirus. Once a person has been exposed to rotavirus, it takes about 2 days for symptoms to appear.
Children who get infected may have severe watery diarrhea, vomiting, fever, or abdominal pain. Vomiting and watery diarrhea can last 3 to 8 days. Additional symptoms may include loss of appetite and dehydration (loss of body fluids), which can be especially dangerous for infants and young children.
Rotavirus often begins with a mild fever and is followed by vomiting and an upset stomach, as well as increased amounts of watery diarrhea many times a day. Anyone caring for small children should know the symptoms of rotavirus, including:
- Frequent, watery diarrhea (often foul-smelling, green or brown)
- Frequent vomiting
- Fever
- Abdominal pain
The following are signs and symptoms of dehydration:
- Decreased urination or less frequent urination
- Dry or sticky mouth and throat
- Feeling dizzy when standing up
- Crying with few or no tears and
- Unusual sleepiness or fussiness.
- Lethargy (child won’t focus on you, is less responsive to touch or words)
- Dry, cool skin
- Sunken eyes or sunken soft spot on top of the head
- Extreme thirst
Adults who get rotavirus disease tend to have milder symptoms.
Children, even those who are vaccinated, may get infected and sick from rotavirus more than once. That is because neither natural infection with rotavirus nor vaccination provides full protection from future infections. Children who are not vaccinated usually have more severe symptoms the first time they get rotavirus disease. Vaccinated children are less likely to get sick from rotavirus.
Rotavirus causes
You’re most likely to contract rotavirus gastroenteritis when you eat or drink contaminated food or water, or if you share utensils, towels or food with someone who’s infected.
Worldwide, rotavirus is the most common cause of viral gastroenteritis in children, who are usually infected when they put their fingers or other objects contaminated with rotavirus into their mouths. The rotavirus infection is most severe in infants and young children. Adults infected with rotavirus may not have symptoms, but can still spread the illness — of particular concern in institutional settings because infected adults unknowingly can pass the virus to others. A vaccine against rotavirus gastroenteritis is available in some countries, including the United States, and appears to be effective in preventing the infection.
Risk factors for getting rotavirus
Rotavirus gastroenteritis occurs all over the world, affecting people of every age, race and background.
People who may be more susceptible to rotavirus gastroenteritis include:
- Young children. Children in child care centers or elementary schools may be especially vulnerable because it takes time for a child’s immune system to mature.
- Older adults. Adult immune systems tend to become less efficient later in life. Older adults in nursing homes, in particular, are vulnerable because their immune systems weaken and they live in close contact with others who may pass along germs.
- Schoolchildren, churchgoers or dormitory residents. Anywhere that groups of people come together in close quarters can be an environment for an intestinal infection to get passed.
- Anyone with a weakened immune system. If your resistance to infection is low — for instance, if your immune system is compromised by HIV/AIDS, chemotherapy or another medical condition — you may be especially at risk.
If you live in the Northern Hemisphere, for instance, you’re more likely to have rotavirus infections between November and June.
Rotavirus prevention
To reduce your risk of catching or spreading rotavirus, wash your hands well after using the bathroom or changing nappies, and before preparing or eating food.
If you have rotavirus gastroenteritis, it’s important to stay home (away from work, school or childcare) until the symptoms have been gone for at least 24 hours. If your work involves handling food or looking after children, the elderly, or patients, do not return to work until 48 hours after the symptoms have stopped.
Rotavirus spreads easily among infants and young children. Rotavirus can cause severe watery diarrhea, vomiting, fever, and abdominal pain. Children who get rotavirus disease can become dehydrated and may need to be hospitalized.
The best way to prevent the spread of rotavirus infections is to follow these precautions:
- Get your child vaccinated. A vaccine against gastroenteritis caused by the rotavirus is available in some countries, including the United States. Given to children in the first year of life, the vaccine appears to be effective in preventing severe rotavirus symptoms.
- Wash your hands thoroughly. And make sure your children do, too. If your children are older, teach them to wash their hands, especially after using the toilet. It’s best to use warm water and soap and to rub hands vigorously for at least 20 seconds, remembering to wash around cuticles, beneath fingernails and in the creases of the hands. Then rinse thoroughly. Carry towelettes and hand sanitizer for times when soap and water aren’t available.
- Use separate personal items around your home. Avoid sharing eating utensils, glasses and plates. Use separate towels in the bathroom.
- Keep your distance. Avoid close contact with anyone who has rotavirus, if possible.
- Disinfect hard surfaces. If someone in your home has rotavirus gastroenteritis, disinfect hard surfaces, such as counters, faucets and doorknobs, with a mixture of two cups of bleach to one gallon of water.
- Check out your child care center. Make sure the center has separate rooms for changing diapers and preparing or serving food. The room with the diaper-changing table should have a sink as well as a sanitary way to dispose of diapers.
Rotavirus precautions when traveling
When you’re traveling in other countries, you can become sick from contaminated food or water. You may be able to reduce your risk by following these tips:
- Drink only well-sealed bottled or carbonated water.
- Avoid ice cubes, because they may be made from contaminated water.
- Use bottled water to brush your teeth.
- Avoid raw food — including peeled fruits, raw vegetables and salads — that has been touched by human hands.
- Avoid undercooked meat and fish.
What is rotavirus vaccine
The best way to protect against rotavirus in children is to have them vaccinated. Doctors recommend all children get the rotavirus vaccine. Most children (about 9 out of 10) who get the vaccine will be protected from severe rotavirus disease. About 7 out of 10 children will be protected from rotavirus disease of any severity.
Prior to rotavirus vaccine introduction in the United States, about 1 out of 70 children would be infected with rotavirus disease requiring hospitalization for intravenous fluids before their fifth birthday.
There are two brands of rotavirus vaccine: RotaTeq® (RV5) and Rotarix® (RV1). They are both given by mouth, not by a shot.
Two rotavirus vaccines are currently licensed for infants in the United States:
- RotaTeq® (RV5) is given in 3 doses at ages 2 months, 4 months, and 6 months
- Rotarix® (RV1) is given in 2 doses at ages 2 months and 4 months
Both vaccines are given by putting drops in the child’s mouth. Each requires multiple doses.
The first dose of either vaccine should be given before a child is 15 weeks of age. Children should receive all doses of rotavirus vaccine before they turn 8 months old.
There is a very small risk that babies may develop a bowel problem called intussusception after receiving the rotavirus vaccine.
Why should my child get the rotavirus vaccine?
The rotavirus vaccine:
- Protects your child from rotavirus, a potentially serious disease.
- Prevents your child from developing diarrhea, vomiting, and stomach pain caused by rotavirus.
- Keeps your child from missing school or child care (and keeps you from missing work to care for your sick child).
For about the first year of an infant’s life, rotavirus vaccine provided 85% to 98% protection against severe rotavirus illness and against hospitalization from rotavirus illness, and 74% to 87% protection against rotavirus illness of any severity 4.
Is rotavirus vaccine safe?
Both rotavirus vaccines (RotaTeq and Rotarix) are very safe and effective at preventing rotavirus disease. Millions of babies in the United States have gotten the vaccine safely.
What are the side effects of rotavirus vaccine?
Most babies who get rotavirus vaccine do not have any side effects. However, some babies can have side effects that are usually mild and go away on their own. Serious side effects are possible but rare.
Side effects are rare, usually mild, and may include fussiness, diarrhea, and vomiting.
Side effects or problems that have been associated with rotavirus vaccine include:
- Mild problems: Being irritable, or having mild, temporary diarrhea or vomiting after getting a dose of rotavirus vaccine.
- Serious problems: There is a small risk of intussusception, a type of bowel blockage that is treated in a hospital, and could require surgery. Intussusception happens in some babies every year in the United States, and usually there is no known reason for it. Intussusception from rotavirus vaccination usually occurs within a week of receiving a dose of vaccine. The risk of intussusception from rotavirus vaccination is estimated to range from about 1 in 20,000 to 1 in 100,000 US infants who get rotavirus vaccine. Your doctor can give you more information.
- Problems that could happen after any vaccine: Any medication can cause a severe allergic reaction. Such reactions from a vaccine are very rare, estimated at less than 1 in a million doses, and usually happen within a few minutes to a few hours after the vaccination. As with any medicine, there is a very remote chance of a vaccine causing a serious injury or death.
Some studies have shown a small rise in cases of intussusception within a week after the first or second dose of rotavirus vaccine. Intussusception is a type of bowel blockage that is treated in a hospital. Some babies might need surgery. Studies estimate a risk ranging from about 1 intussusception case in every 20,000 infants to 1 intussusception case in every 100,000 infants after vaccination 5, 6.
Who should NOT get Rotavirus vaccine?
Your healthcare provider is the best source of information on the benefits and risks of vaccines. Before your child receives any vaccine, discuss with your healthcare provider:
- health problems that your child may have
- medications that your child is currently taking
- concerns you might have about vaccination
Infants should NOT get rotavirus vaccine if they have any of the following:
- a severe (life-threatening) allergic reaction to an earlier dose of rotavirus vaccine,
- a severe (life threatening) allergy to any component of rotavirus vaccine. Tell your doctor if your baby has any severe allergies that you know of, including a severe allergy to latex,
- severe combined immunodeficiency (SCID), a condition in which a child’s immune system cannot fight infections, or
- a previous episode of a type of bowel blockage called intussusception.
Infants who are moderately or severely ill should wait to get the vaccine until they recover. This includes infants with moderate or severe diarrhea or vomiting. Babies who are mildly ill can get the vaccine.
Check with your doctor before vaccinating if your baby’s immune system is weakened because of:
- HIV/AIDS, or any other disease that affects the immune system
- Treatment with drugs such as steroids
- Cancer, or cancer treatment with x-rays or drugs
Can Rotavirus vaccine be given with other vaccines?
Rotavirus vaccine can be safely given during the same doctor’s visit with DTaP vaccine, Hib vaccine, polio vaccine, hepatitis B vaccine, and pneumococcal conjugate vaccine.
Rotavirus diagnosis
It is not possible to diagnose rotavirus infection by clinical presentation because the clinical features of rotavirus gastroenteritis do not differ from those of gastroenteritis caused by other pathogens. Confirmation of rotavirus infection by laboratory testing is necessary for reliable rotavirus surveillance and can be useful in clinical settings to avoid inappropriate use of antimicrobial therapy 2.
Diagnosis may be made by rapid detection of rotavirus antigen in stool specimens. Strains may be further characterized by enzyme immunoassay or reverse transcriptase polymerase chain reaction, but such testing is not commonly done.
Rotavirus is shed in high concentration in the stool of children with gastroenteritis and a fecal specimen is the preferred specimen for diagnosis 2. The most widely available method for detection of rotavirus antigen in stool is an enzyme immunoassay (EIA) directed at an antigen common to all group A rotaviruses 2. Several commercial EIA kits are available that are inexpensive, easy to use, rapid, and highly sensitive (approximately 90–100%), making them suitable for rotavirus surveillance and clinical diagnosis.[50]; Polyacrylamide gel electrophoresis and silver staining is about as sensitive as EIA but is very labor intensive 7. Latex agglutination is less sensitive and specific than EIA but is still used in some settings 8. Other techniques, including electron microscopy, reverse transcription polymerase chain reaction (RT-PCR), nucleic acid hybridization, sequence analysis, and culture are used primarily in research settings.
Rotavirus treatment
There is no specific medicine to treat rotavirus infection, but your doctor may recommend medicine to treat the symptoms. Antibiotics will not help because they fight bacteria not viruses. For people with healthy immune systems, rotavirus disease is self-limited, lasting for only a few days (3 to 8 days). Treatment is nonspecific and consists primarily of oral rehydration therapy to prevent dehydration.
Since rotavirus disease can cause severe vomiting and diarrhea, it can lead to dehydration (loss of body fluids). Infants and young children, older adults, and people with other illnesses are most at risk of dehydration.
Symptoms of dehydration include:
- decreased urination
- dry mouth and throat
- feeling dizzy when standing up
- crying with few or no tears and
- unusual sleepiness or fussiness.
The best way to protect against dehydration is to drink plenty of liquids. You can get oral rehydration solutions over the counter in U.S. food and drug stores; these are most helpful for mild dehydration. Severe dehydration may require hospitalization for treatment with intravenous (IV) fluids, which are given to patients directly through their veins. If you or someone you are caring for is severely dehydrated, contact your doctor.
How to treat diarrhea and vomiting yourself
You can usually treat yourself or your child at home.
The most important thing is to have plenty of fluids to avoid dehydration.
DO
- stay at home and get plenty of rest
- drink lots of fluids, such as water and squash – take small sips if you feel sick
- carry on giving breast or bottle feeds to your baby – if they’re being sick, try giving small feeds more often than usual
- for babies on formula or solid foods, give small sips of water between feeds
- eat when you feel able to – you don’t need to have or avoid any specific foods
- take paracetamol if you’re in discomfort – check the leaflet before giving them to your child
DON’T
- have fruit juice or fizzy drinks – they can make diarrhea worse
- make baby formula weaker – use it at its usual strength
- give young children medicine to stop diarrhea
- give aspirin to children under 16
How to treat diarrhea and vomiting in children
The main treatment is to give enough fluids to prevent your child becoming dehydrated. Babies and children below 3 years old are most at risk and may need to be checked by a doctor. Give small amounts of fluids frequently as they can usually tolerate this better than large volumes at a time. You should continue to give fluids even if they are vomiting. Many common medicines to reduce vomiting or diarrhea are often not helpful and may instead be harmful in children. Antibiotic treatment is also unnecessary and unhelpful in most cases because the infection is usually caused by viruses which do not respond to this treatment.
If you’re breast-feeding, let your baby nurse. If your baby is bottle-fed, offer a small amount of an Oral Rehydration Solutions (ORS) or regular formula.
Consider acetaminophen (Tylenol, others) for relief of discomfort, unless your child has liver disease. Don’t give your child aspirin.
What fluids to use
The best fluids to use are Oral Rehydration Solutions (ORS), e.g., CeraLyte, Enfalyte, Pedialyte, Hydralyte, Gastrolyte, Repalyte etc., which are available from your local chemist. They contain glucose and different salts which tend to be lost from the body during vomiting or diarrhea. Make them up EXACTLY as it says on the packet. Breast fed babies should continue to be breastfed but may need to be fed more frequently. Oral Rehydration Solutions (ORS) or water (boiled if the baby is less than 6 months old) may be offered to babies in addition to breast feeds. Bottle fed babies may need to have both Oral Rehydration Solutions (ORS) and their formula at normal strength.
What can I do if my child refuse to take the oral rehydration solution?
Chilling the fluids or making them into iceblocks may help your child to take them. Some children may still refuse to drink. In this situation water or other fluids such as diluted juice or soft drinks may be given, although they are not as good as Oral Rehydration Solutions (ORS) because they don’t have all the extra salts in the right amounts and have sugars which are not as well absorbed.
DO NOT GIVE UNDILUTED juice, sodas, sports drinks or other soft drinks as they have too much sugar and may make the diarrhea worse. Chicken broth is also not recommended as it has too much salt and no sugar.
How much fluid does my child need?
This depends on the age and size of the child and also how dehydrated they are.
The minimum daily requirements in children are:
- 3-10kg (1-12months): 100ml/kg
- 10-20kg (1-5yrs): 1000ml + 50ml/kg for each kg over 10kg
- >20kg: 1500ml + 20ml/kg for each kg over 20kg
You may also need to give an extra 2ml/kg for every vomit and 10ml/kg for each diarrheal stool in addition to the maintenance amount of fluids required.
Give small volumes frequently, e.g. 5ml (1tsp) every 5 minutes, is better tolerated than 60ml all at once every hour.
What about eating food?
Doctors no longer recommend restricting food intake during gastroenteritis. Your child may not feel like eating initially but should be allowed to eat once they feel hungry. Gradually introduce bland, easy-to-digest foods, such as toast, rice, bananas and potatoes. Avoid giving your child full-fat dairy products, such as whole milk and ice cream, and sugary foods, such as sodas and candy. These can make diarrhea worse.
Bottle fed babies on infant formula should be given their formula at normal strength and not diluted down. The only foods to avoid are those with high sugar content such as undiluted juice, cordials, soft drinks, jelly, jam, sweets, chocolate etc. as they may make the diarrhea worse.
Lactose intolerance is uncommon in young American children but may occur temporarily after a bout of gastroenteritis. This may be suspected if their diarrhea worsens and is watery, frothy and explosive after drinking milk or formula. If this occurs, then a lactose free or soy formula may be used for a few weeks until the gut recovers.
- Frequently Asked Questions About Rotavirus. http://www.nfid.org/idinfo/rotavirus/faqs.html[↩]
- Chapter 13: Rotavirus. Manual for the Surveillance of Vaccine-Preventable Diseases (6th Edition, 2017). https://www.cdc.gov/vaccines/pubs/surv-manual/chpt13-rotavirus.html[↩][↩][↩][↩]
- CDC. Prevention of rotavirus gastroenteritis among infants and children: recommendation of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2009; 58(RR-2):1–25. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5802a1.htm[↩]
- Rotavirus. https://www.cdc.gov/rotavirus/clinical.html[↩]
- Weintraub ES, Baggs J, Duffy J, et al. Risk of intussusception after monovalent rotavirus vaccination. N Engl J Med 2014;370(6):513–9. doi: 10.1056/NEJMoa1311738[↩]
- Shui IM, Baggs J, Patel M, et al. Risk of intussusception following administration of a pentavalent rotavirus vaccine in U.S. infants. JAMA 2012;307(6):598–604. doi:10.1001/jama.2012.97[↩]
- Payne DC, Sulemana I, Parashar UD. Evaluation of effectiveness of mixed rotavirus vaccine course for severe rotavirus gastroenteritis. JAMA Pediatr, 2016;170(7):708–10. doi:10.1001/jamapediatrics.2016.0014[↩]
- Immergluck LC, Parker TC, Jain S, et al. Sustained effectiveness of monovalent and pentavalent rotavirus vaccines in children. J Pediatr 2016;172:116-20. doi: 10.1016/j.jpeds.2016.01.042[↩]