Contents
Sacroiliac joint pain
Sacroiliac joint pain is a common cause of buttock and lower back pain 1. Studies have shown that 10% to 27% of mechanical low back pain is secondary to sacroiliac joint pain. Sacroiliac joint pain can occur with or without lower extremity pain. Dysfunction of the sacroiliac joint occurs with degenerative conditions or with an imbalance between the sacroiliac joints. Patient with true and apparent leg length discrepancy, advanced age, inflammatory arthritis, pregnancy, trauma, and previous spine surgery are at increased risk of sacroiliac joint pain. Classically, sacroiliac joint pain is often reported as pain below L5, and certain physical exam maneuvers such as FABER, Gaenslen’s, and compression tests can elicit pain stemming from sacroiliac joint dysfunction. If sacroiliac joint pain is bilateral and symmetric, then a suspicion for inflammatory causes such as ankylosing spondylitis should be raised.
Sacroiliac joint is relatively immobile, and its main function is to transfer weight to and from the lower and axial appendicular skeleton. Also, the synovial articulation does allow for minimal rotation and gliding. The sacroiliac joint experiences the most movement during pregnancy when the ligaments become lax from the effects of the sex hormones 2. After the fifth decade of life, the sacroiliac joint does fuse.
The posterior sacral ramus innervates the sacroiliac joint and when compressed or inflamed, it is a source of significant pain 2. The majority of individuals affected by sacroiliac joint pain are adults. Sacroiliac joint pain is most common in individuals who lead a sedentary lifestyle. Overall, obese patients are more commonly affected by sacroiliac joint pain. Sacroiliac joint pain is seen in both genders and people of all races.
Because the sacroiliac joints transfer forces from the upper body to the lower extremities, they are subject to trauma and chronic degenerative changes. The most common cause of sacroiliac joint pain is osteoarthritis. Sacroiliac joint pain is also common in pregnancy. During pregnancy, hormones, such as relaxin, are increased leading to ligamentous laxity and joint hypermobility. Hypermobile sacroiliac joints in conjunction with the increased anterior weight of pregnancy and altered gait lead to sacroiliac joint pain. Leg length discrepancy is also a cause of sacroiliac joint pain. Leg lengths should be measured in all patients with suspected sacroiliac joint dysfunction.
Most sacroiliac joint pain gets better within a few weeks without treatment. Bed rest isn’t recommended. Over-the-counter pain medications often help reduce sacroiliac joint pain, as does the application of cold or heat to the painful area.
When indicated, the sacroiliac joint injection is used to aid the diagnosis and treat of sacroiliac joint pain. This procedure involves introducing a local anesthetic or a mixture of local anesthetic and corticosteroids into the sacroiliac joint. Once sustained and adequate pain relief is achieved, the patient can return to normal function or a physical therapy regiment can be implemented 3.
Schedule an office visit
Call your doctor if your back pain hasn’t improved after a week of home treatment or if your back pain:
- Is constant or intense, especially at night or when you lie down
- Spreads down one or both legs, especially if the pain extends below your knee
- Causes weakness, numbness or tingling in one or both legs
- Occurs with unintended weight loss
- Occurs with swelling or redness on your back
Seek emergency medical care
Call your local emergency services number or get emergency medical help or have someone drive you to the emergency room if your back pain:
- Occurs after a high-impact car crash, bad fall or sports injury
- Causes new bowel or bladder control problems
- Occurs with a fever
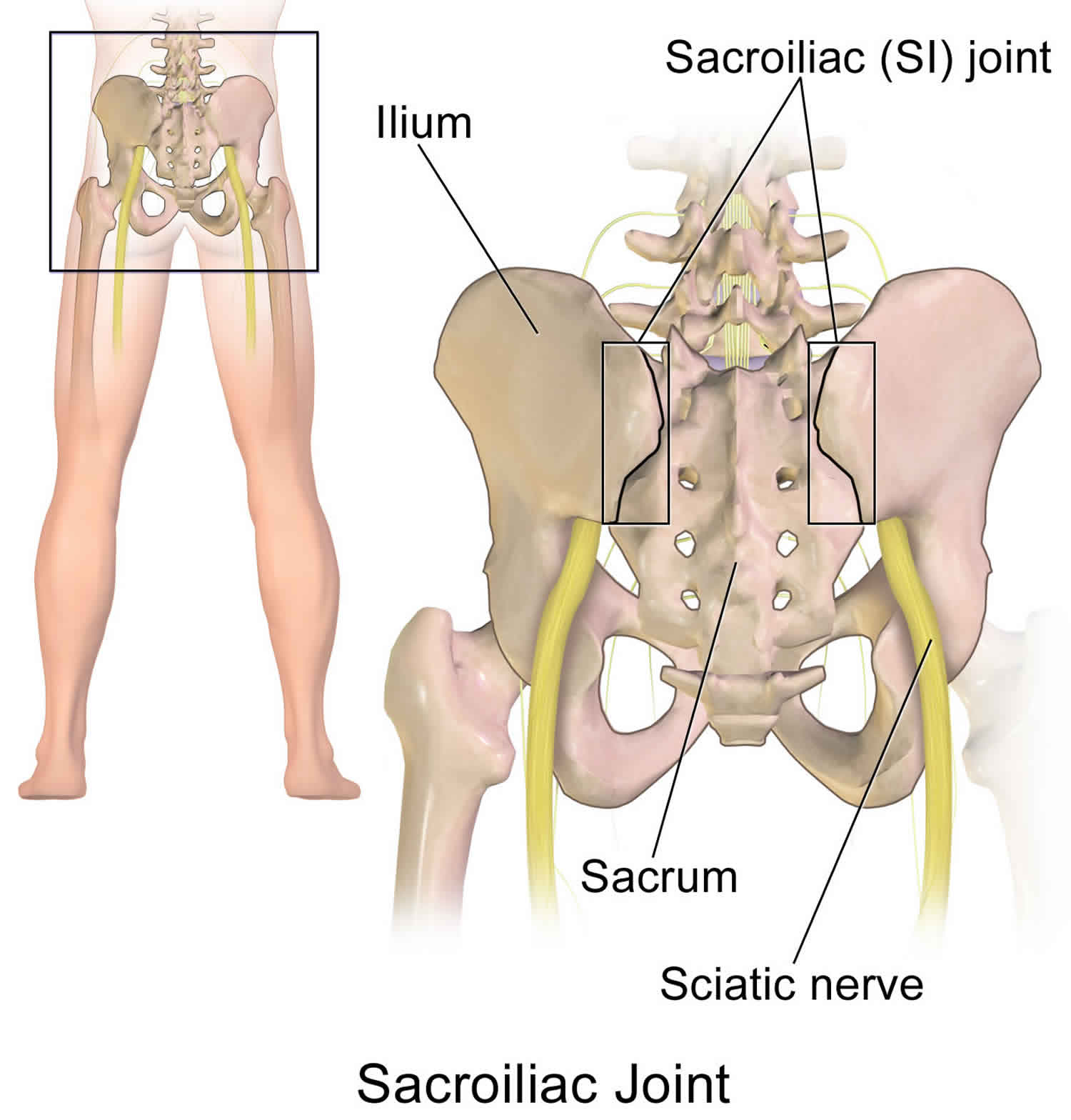
Sacroiliac joint anatomy
The sacroiliac joint is a synovial joint, which one of the largest joints in the body. The human body has two sacroiliac joints, connecting the bones of the ilium to the sacrum on each side of the body. The sacroiliac joint is auricular and has characteristics of both diarthrosis and synarthrosis joints. The ligaments form a capsule that follows its auricular margin, with an extracapsular articulation between the sacrum and ilia supported by the interosseous sacroiliac ligament. The symmetrical sacroiliac joint is located at S1 to S3 and has a slight oblique coronal orientation. During pregnancy, relaxin is released, and this can cause the ligaments to loosen. The sacroiliac joint innervation is complex, and conflicting information exists. According to some sources, the sensory fibers of the lateral branches of the posterior rami of L5 through S4, which serve as the pain generators for the joint.
The sacroiliac joint capsule is relatively thin and often develops defects that enable fluid, such as joint effusion or pus, to leak out onto the surrounding structures 4. As surrounding muscles and structures are affected different presentations of sacroiliac joint pain can present because different nerve roots innervate these structures. Common distributions of pain are L4-L5 dermatomes, but distributions can certainly present in dermatomes as high as L2 and as low as S3. The asymmetric motion of the pelvis can cause mechanical dysfunction, leading to degeneration and significant pain.
While the main purpose of sacroiliac joint is to supply stability and to decrease the forces transmitted from the lower extremities, the sacroiliac joint does have limited motion, with an average range of 2 degrees in both planes, according to one analysis. The sacroiliac joint motions include anterior and posterior innominate tilt of the pelvis on the sacrum. There is also the motion of nutation, where the sacrum moves anteriorly and inferiorly while the coccyx moves posteriorly relative to the ilium, and counternutation, where the sacrum moves posteriorly and superiorly while the coccyx moves anteriorly relative to the sacrum.
Figure 1. Sacroiliac joint
Sacroiliac joint pain causes
A problem in any part of your spine can cause back pain. A common cause of sacroiliac joint pain is injury to a muscle (strain) or ligament (sprain). Strains and sprains can occur for many reasons, including improper lifting, poor posture and lack of regular exercise. Being overweight might increase your risk of strains and sprains affecting your back.
Sacroiliac joint pain can also result from arthritis and other age-related changes in your spine, from more-serious injuries, such as a vertebral fracture or ruptured disk, and from certain infections.
Possible causes of sacroiliac joint pain include:
- Degenerative arthritis (e.g., osteoarthritis)
- Endometriosis
- Fibromyalgia
- Herniated disk
- High energy trauma (e.g. motor vehicle accident, falls) — can lead to pelvic ring injuries with a spectrum of injury to the sacroiliac joint ligaments.
- Ligament strain and/or stress or occult fractures
- Infection is rare cause of sacroiliac joint pain
- Inflammatory arthropathy (i.e. sacroiliitis):
- Spondyloarthropathies such as:
- Aankylosing spondylitis,
- Reactive arthritis,
- Psoriatic arthritis, and inflammatory bowel disease (Crohn disease and Ulcerative colitis) should be considered with sacroiliac joint pain especially those with systemic manifestations
- Spondyloarthropathies such as:
- Kidney infection (pyelonephritis)
- Kidney stones
- Obesity
- Osteoarthritis (disease causing the breakdown of joints)
- Osteomyelitis (a bone infection)
- Osteoporosis
- Poor posture
- Pregnancy
- Rheumatoid arthritis (inflammatory joint disease)
- Sacroiliitis
- Sciatica
- Scoliosis
- Secondary conditions:
- secondary to previous spinal fusion procedures
- secondary to scoliosis and/or leg length discrepancy
- Spinal fractures
- Spinal stenosis
- Sprains
Various conditions result in the inflammation of the sacroiliac joint, leading to significant pain. Sacroiliac joint pain often is due to chronic degenerative causes yet relatively uncommon. Sacroiliac joint pain can be secondary to rheumatic disease, infections, drug-related, or oncologic sources. Some specific examples of non-degenerative conditions that can lead to sacroiliac joint pain are ankylosing spondylitis, psoriatic arthropathy, Bechet disease, hyperparathyroidism, and various pyogenic sources 5.
Osteoarthritis can cause degeneration of the sacroiliac joint resulting in pathologic articulation and motion leading to this condition. Spondyloarthropathies themselves can cause significant inflammation of the sacroiliac joint itself. Pregnancy is another cause of the inflammation due to the hormone relaxin leading to the relaxation, stretching, and possible widening of the sacroiliac joint(s). The increased weight of pregnancy also causes extra mechanical stress on the sacroiliac joint, leading to further wear and tear. Trauma can cause direct or indirect stress and damage to the sacroiliac joint. Pyogenic sacroiliitis is the most frequently reported cause of acute sacroiliac joint pain. Sacroiliac joint pain can originate from the synovial joint but can also originate from the posterior sacral ligaments 6.
Differential diagnosis includes leg-length discrepancies, unilateral weaker limb or gluteal muscles, tight or strained surrounding muscles structures, or hip osteoarthritis 7.
Sacroiliac joint pain pathophysiology
Sacroiliac joint dysfunction or sacroiliitis are common terms used to describe sacroiliac joint pain. It is usually caused by abnormal motion (i.e. hyper- or hypo-mobile) or malalignment of the sacroiliac joint. The sacroiliac joint can be hyper or hypo-mobile which can cause pain. Pain is usually localized over the buttock. Patients usually describe the pain as sharp, dull, achy, stabbing, or shooting pain directly over the affected joint. Patient’s can often complain of sharp, stabbing, and/or shooting pain which extends down the posterior thigh usually not past the knee. Pain can frequently mimic and be misdiagnosed as radicular pain. Patients will frequently complain of pain while sitting down, lying on the ipsilateral side of pain, or climbing stairs.
Sacroiliac joint pain symptoms
Sacroiliac joint pain can be particularly difficult to diagnose because its symptoms are similar to many other common sources of back pain. Sacroiliac joint pain often is overlooked as a source of back or buttock pain.
Common symptoms of sacroiliac joint pain include pain that:
- Occurs in the lower back, buttock, hip, or thigh
- Gets worse after long periods of sitting or standing, or getting out of a chair
- Worsens after rotating your hips
- Feels sharp or stabbing, or dull and achy
Sacroiliac joint pain diagnosis
The diagnosis of sacroiliac joint pain is quite difficult as there are many other causes of pain around the hip and lower back. Some of the provocative tests that may help make the diagnosis include the yeoman test, gilet test, FABER (Flexion, Abduction, and External Rotation) test, Laguerre’s, and sacroiliac tests. There are no specific signs or symptoms asides from the pain. The laboratory investigations are not revealing.
Patrick’s test or FABER (flexion, abduction, and external rotation) is a physical exam finding of hip or sacroiliac joint pathology. FABER is performed with the patient supine on the exam table. The hip is flexed, knee flexed to 90 degrees, thigh abducted, and hip is externally rotated. Pain elicited over contralateral sacroiliac joint is considered a positive test for sacroiliac joint pathology. Pain in the groin on ipsilateral side is considered positive for hip pathology. The examiner should also perform the Gaenslen’s test when sacroiliac joint dysfunction is considered. The test is performed with the patient supine on the exam table. One hip is flexed to the patient’s chest while the opposite leg is allowed to drop off of the table. The examiner should provide a force to the anterior knee of the flexed hip on the ipsilateral side while the contralateral knee off the table is forced downward toward the ground.
Your doctor will ask you about your medical history, including any previous inflammatory disorders or conditions. Other diagnostic tests include:
- Physical exam, movement tests – During the physical exam, the spine is examined for proper alignment and rotation. During various physical movement tests, you are positioned or asked to move in specific directions. In some of these tests, the doctor applies pressure to your sacroiliac joint, spine, hip, or leg.
- Blood work – Blood work looks for signs of inflammation.
- Imaging tests – X-rays, CT scans, and/or MRI scans may be ordered if the doctor suspects an injury as the source of pain or to look for changes in the sacroiliac joint.
- Steroid injection – An injection of steroids into the sacroiliac joint is both a diagnostic test – if it relieves pain – and a treatment. This procedure is performed using x-ray to guide the spinal needle to the appropriate location for the injection.
Imaging studies are recommended to help rule out other possible sources of pain. Radiographs are often less than ideal as the sigmoid shape and oblique orientation limits visualization. CT and MRI are more helpful in ruling out other causes of pain — these include but are not limited to arthritis (of the hips or lumbar spine), multiple myeloma, spinal stenosis, ankylosing spondylitis, piriformis syndrome, trochanteric bursitis, tendinopathies, hip fracture, and disc herniations.
Ultrasound guided injections are an invaluable tool in the diagnosis (and therapeutic management) of sacroiliac joint pathology. Some authors advocate that patients presenting with 3 or more provocative examination maneuvers for sacroiliac joint pathology, or in patients with isolated and localized sacroiliac joint pain be considered the ideal candidates for diagnostic injections 8.
Sacroiliac joint pain treatment
Most people with sacroiliac joint pain benefit from physical therapy. This treatment helps strengthen and stabilize the muscles surrounding your sacroiliac joints. Physical therapy also makes it easier for you to move your sacroiliac joints through full range of motion.
In some cases, doctors prescribe medications like nonsteroidal anti-inflammatory drugs (NSAIDs) (Advil®) to help manage sacroiliac joint pain.
How to relieve sacroiliac joint pain
Assuming your sacroiliac joint pain is simple back strain (and unless you develop other symptoms, you can safely assume it is), the following advice can help you achieve sacroiliac joint pain relief:
- Try to stay active. Prolonged bed rest (more than four days) has the potential for weakening muscles and prolonging the pain.
- Exercise in moderation. Start with a few minutes of daily walking, swimming or stationary cycling and build up to 20 or 30 minutes at a stretch once pain subsides. If the exercise causes too much pain, try another. Avoid aggravating activities. Jogging, golf or tennis are out until pain subsides.
- You can continue your daily work routine if your job does not consist of strenuous manual labor.
- Use medications. Acetaminophen or an over-the-counter nonsteroidal anti-inflammatory drug such as ibuprofen can offer low back pain relief and keep you mobile. Prescription muscle relaxants, sometimes prescribed for back pain, may do little to help your pain and may cause unwanted side effects, including dizziness, drowsiness or dry mouth.
- Use hot and cold treatments. An ice pack or hot water bottle applied to your lower back can be soothing.
- Practice proper lifting techniques. Lift objects close to your body at navel level and avoid twisting, bending and reaching while lifting.
- Avoid prolonged sitting. If you work at a desk, change positions often. Placing a support at the small of your back, using armrests to help support your body weight, and reclining your chair back slightly may make sitting more comfortable.
By following this simple advice and being patient, you’ll find low back pain relief shortly – most people do.
In some cases, doctors inject steroids into your sacroiliac joints to help decrease inflammation and pain. This procedure involves introducing a local anesthetic or a mixture of local anesthetic and corticosteroids into the sacroiliac joint. Once sustained and adequate pain relief is achieved, the patient can return to normal function or a physical therapy regiment can be implemented 3.
Radiofrequency ablation is considered only if pain relief is temporarily achieved after sacroiliac joint injection. This procedure uses radio waves to heat a small area of nerve tissue to stop it from sending pain signals, thereby reducing pain.
Sacroiliac joint pain exercises
Exercise is commonly advised as one of the best ways to help prevent and man age most back pain. The type of exercise you do does not matter as long as you do something and remain active. Some people find that swimming helps them, others swear by yoga, while many people enjoy walking or running. The choice of exercise is yours because if you enjoy what you are doing, you will be more likely to continue and see the benefits.
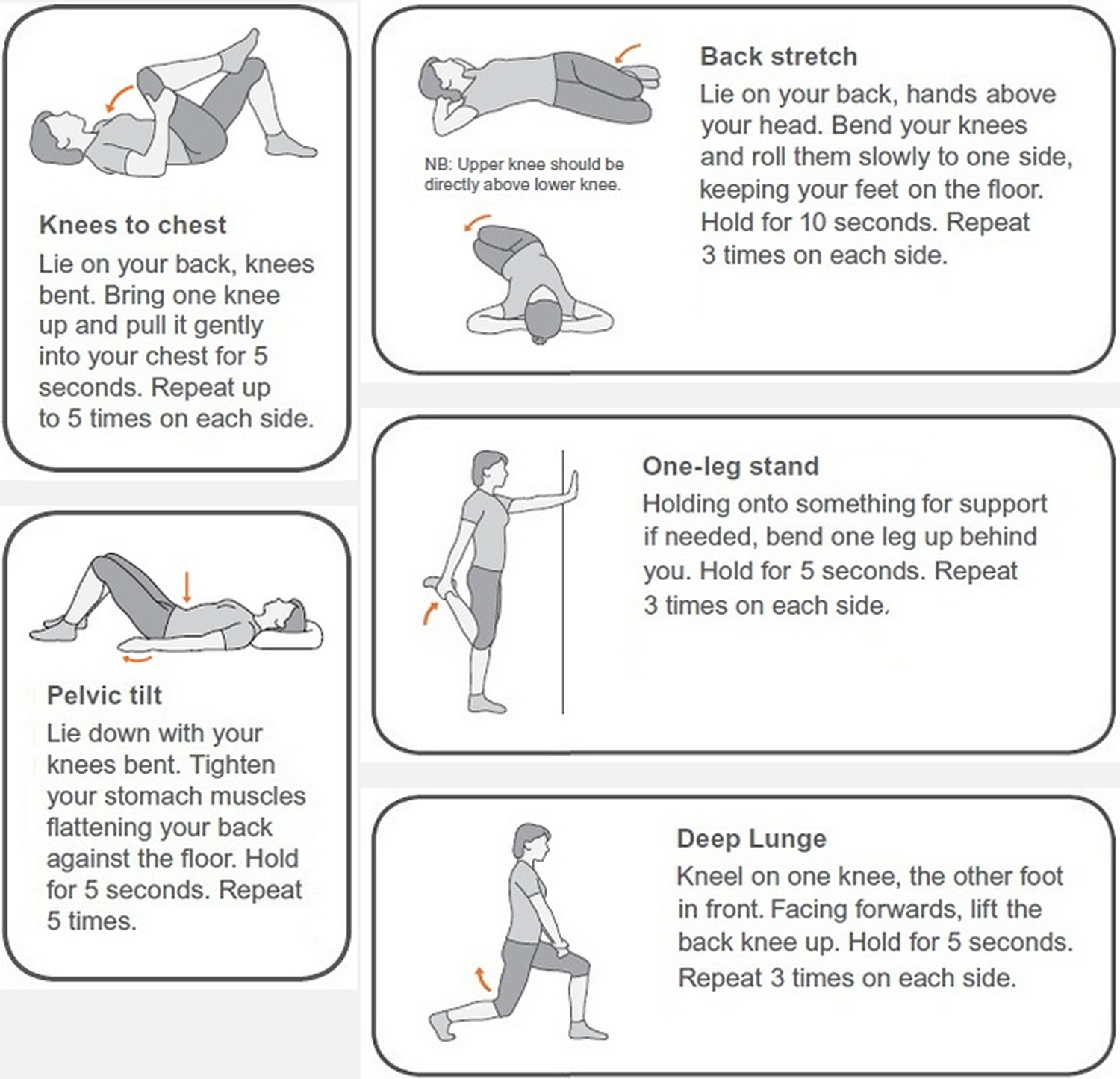
There are some simple back exercises and stretches you can do at home to help ease lower back pain and improve your strength and flexibility.
Common exercises beneficial for back pain:
- Swimming – the water environment takes the strain off joints and muscles while working out the entire body
- Yoga – strengthens core and back muscles and increases flexibility
- Pilates – strengthens muscles and the spinal column and promotes good posture
- Exercise programmes – provide a cardiovascular work out and all over body conditioning which includes the back and core muscles
There are many other exercises that you could do which would be helpful. Although structured exercises are extremely beneficial, there are also some exercises you can do on your own at home without specialist equipment that can help to strengthen your back and prevent and ease back pain. If you find that any of the exercises exacerbates your back pain, try another one or seek advice from your doctor or health professional. You should, however, expect some minor discomfort after starting an exercise programme, since your body may not be used to exercise.
Figure 2. Exercises for lower back pain
Aim to do these exercises every day, along with other activities like walking, swimming or yoga.
Your pain should start to ease within 2 weeks and will usually pass in about 4 to 6 weeks.
See a doctor if:
- your pain doesn’t improve within a few weeks
- you experience severe pain while trying any of these exercises
Stretches for lower back pain
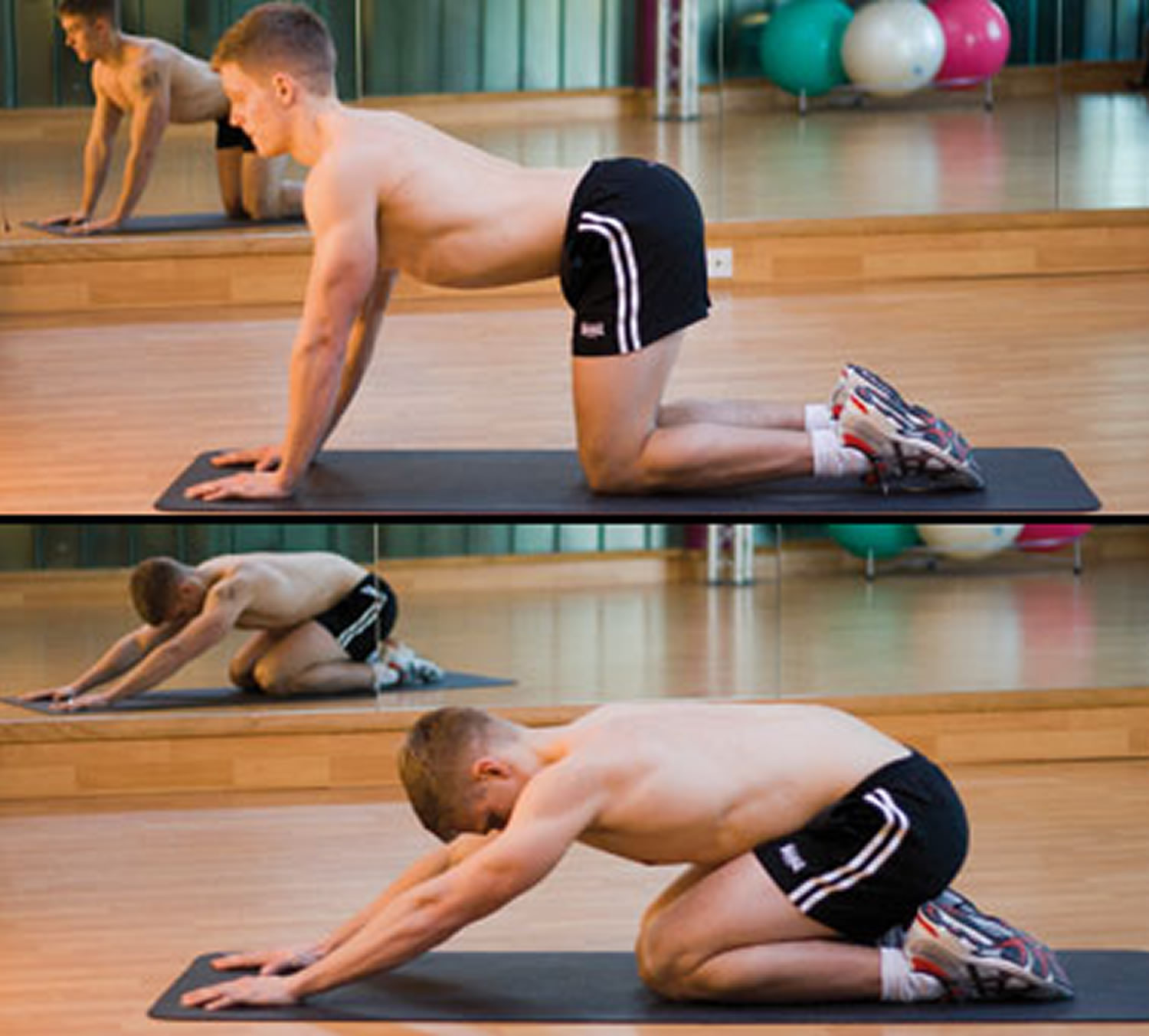
Bottom to heels stretch
Start position: Kneel on all fours, with your knees under your hips and hands under your shoulders. Try to keep your back and neck fairly straight, and don’t lock your elbows.
Action: Slowly move your bottom back towards your heels. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times.
Tips:
- avoid going right back onto your heels if you have a knee problem
- ensure correct positioning with the help of a mirror
- only stretch as far as feels comfortable
Figure 3. Bottom to heels stretch
Knee rolls
Start position: Lie on your back. Place a small flat cushion or book under your head. Keep your knees bent and together. Keep your upper body relaxed and your chin gently tucked in.
Action: Roll your knees to one side, keeping both shoulders on the floor. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times, alternating sides.
Tips:
- only move as far as feels comfortable
- place a pillow between your knees for comfort
Figure 4. Knee rolls exercise
Back extensions
Start position: Lie on your front and rest on your forearms, with your elbows bent at your sides. Look towards the floor and keep your neck straight.
Action: Keeping your neck straight, arch your back up by pushing down on your hands. You should feel a gentle stretch in the stomach muscles. Breathe and hold for 5 to 10 seconds. Return to the starting position.
Repeat 8 to 10 times.
Tips:
- don’t bend your neck backwards
- keep your hips on the floor
Figure 5. Back extensions
Deep abdominal strengthening
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees, keeping your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: As you breathe out, gently tense the muscles in your pelvis and lower tummy so they’re pulled up towards your chest. Hold for 5 to 10 breaths and relax.
Repeat 5 times.
Tips:
- this is a slow, gentle exercise – don’t try to tense your muscles too quickly or too hard
- make sure you don’t tense up through the neck, shoulders or legs
Figure 6. Deep abdominal strengthening exercise
Pelvic tilts
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees, keeping your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: Gently flatten your lower back into the floor and tense your stomach muscles. Now tilt your pelvis towards your heels until you feel a gentle arch in your lower back and return to the starting position.
Repeat 10 to 15 times, tilting your pelvis back and forth in a slow rocking motion.
Tips:
- don’t press down through your neck, shoulders or feet
- place one hand on your stomach and the other under your lower back – if you’re doing the exercise correctly, you should feel the muscles working in these areas
Figure 7. Pelvic tilts exercise
Back pain pilates workout
A pilates-inspired exercise video suitable for people with chronic back pain.
This 29-minute class focuses on improving posture and improving the strength and flexibility of the muscles that support the back.
Regular pilates practice can help improve posture, muscle tone, balance and joint mobility, as well as relieve stress and tension.
- Wu L, Varacallo M. Sacroiliac Joint Injection. [Updated 2019 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513245[↩]
- Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299[↩][↩]
- Navani A, Manchikanti L, Albers SL, Latchaw RE, Sanapati J, Kaye AD, Atluri S, Jordan S, Gupta A, Cedeno D, Vallejo A, Fellows B, Knezevic NN, Pappolla M, Diwan S, Trescot AM, Soin A, Kaye AM, Aydin SM, Calodney AK, Candido KD, Bakshi S, Benyamin RM, Vallejo R, Watanabe A, Beall D, Stitik TP, Foye PM, Helander EM, Hirsch JA. Responsible, Safe, and Effective Use of Biologics in the Management of Low Back Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2019 Jan;22(1S):S1-S74.[↩][↩]
- Buchanan BK, Varacallo M. Sacroiliitis. [Updated 2019 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448141[↩]
- Gutierrez M, Rodriguez S, Soto-Fajardo C, Santos-Moreno P, Sandoval H, Bertolazzi C, Pineda C. Ultrasound of sacroiliac joints in spondyloarthritis: a systematic review. Rheumatol. Int. 2018 Oct;38(10):1791-1805[↩]
- Kocak O, Kocak AY, Sanal B, Kulan G. Bilateral Sacroiliitis Confirmed with Magnetic Resonance Imaging during Isotretinoin Treatment: Assessment of 11 Patients and a Review of the Literature. Acta Dermatovenerol Croat. 2017 Oct;25(3):228-233[↩]
- Poddubnyy D, Listing J, Haibel H, Knüppel S, Rudwaleit M, Sieper J. Functional relevance of radiographic spinal progression in axial spondyloarthritis: results from the GErman SPondyloarthritis Inception Cohort. Rheumatology (Oxford). 2018 Apr 01;57(4):703-711[↩]
- Rupert MP, Lee M, Manchikanti L, Datta S, Cohen SP. Evaluation of sacroiliac joint interventions: a systematic appraisal of the literature. Pain Physician. 2009 Mar-Apr;12(2):399-418.[↩]