Contents
What is Sheehan syndrome
Sheehan syndrome also called postpartum hypopituitarism (the pituitary gland not producing enough pituitary hormones), is a rare complication of life-threatening amount of blood loss that may occur in a woman who has a severe uterine hemorrhage during childbirth. Severe blood loss during or after childbirth can deprive the body of oxygen and seriously damage your pituitary gland. This causes the pituitary gland to permanently lose its ability to function properly 1. Sheehan syndrome symptoms vary, from failure to lactate, to nonspecific symptoms like fatigue, to adrenal crisis (a life-threatening shortage of the hormone cortisol) 2.
Sheehan syndrome is rare in developed countries because of advanced obstetrical practices and more exposure to experienced medical providers and medical facilities. Unfortunately, it’s a major threat to women following childbirth in developing and low-income countries. Some studies have placed the incidence of Sheehan syndrome as high as five patients out of 100,000 births 3.
Sheehan’s syndrome treatment involves lifelong replacement of the hormones produced by the pituitary gland. The following may be recommended, depending on individual circumstances 2:
- Estrogen alone (if the uterus has been removed) or estrogen and progesterone in combination. This should be taken at least until the normal age of menopause.
- Levothyroxine to replace thyroid stimulating hormone. This will need to be taken throughout the lifetime.
- Corticosteroids to replace adrenal hormones. These must also be taken throughout the lifetime.
- Growth hormone may also be suggested, as this may help normalize the body’s muscle-to-fat ratio, maintain bone mass, lower cholesterol levels, and/or improve overall quality of life.
The levels of these hormones should be monitored on a regular basis and may need to be adjusted periodically based on factors such as stress level, illness, pregnancy, or changes in weight 2.
What causes Sheehan syndrome
Sheehan syndrome is caused by severe blood loss or extremely low blood pressure during or after childbirth. Blood loss at delivery can be particularly damaging to the pituitary gland, which enlarges during pregnancy. This damage destroys the hormone-producing tissue so that the gland cannot function properly. Women who are carrying multiples (twins, triplets, etc.) and those who have problems with the placenta have an increased risk for bleeding during childbirth and Sheehan syndrome.
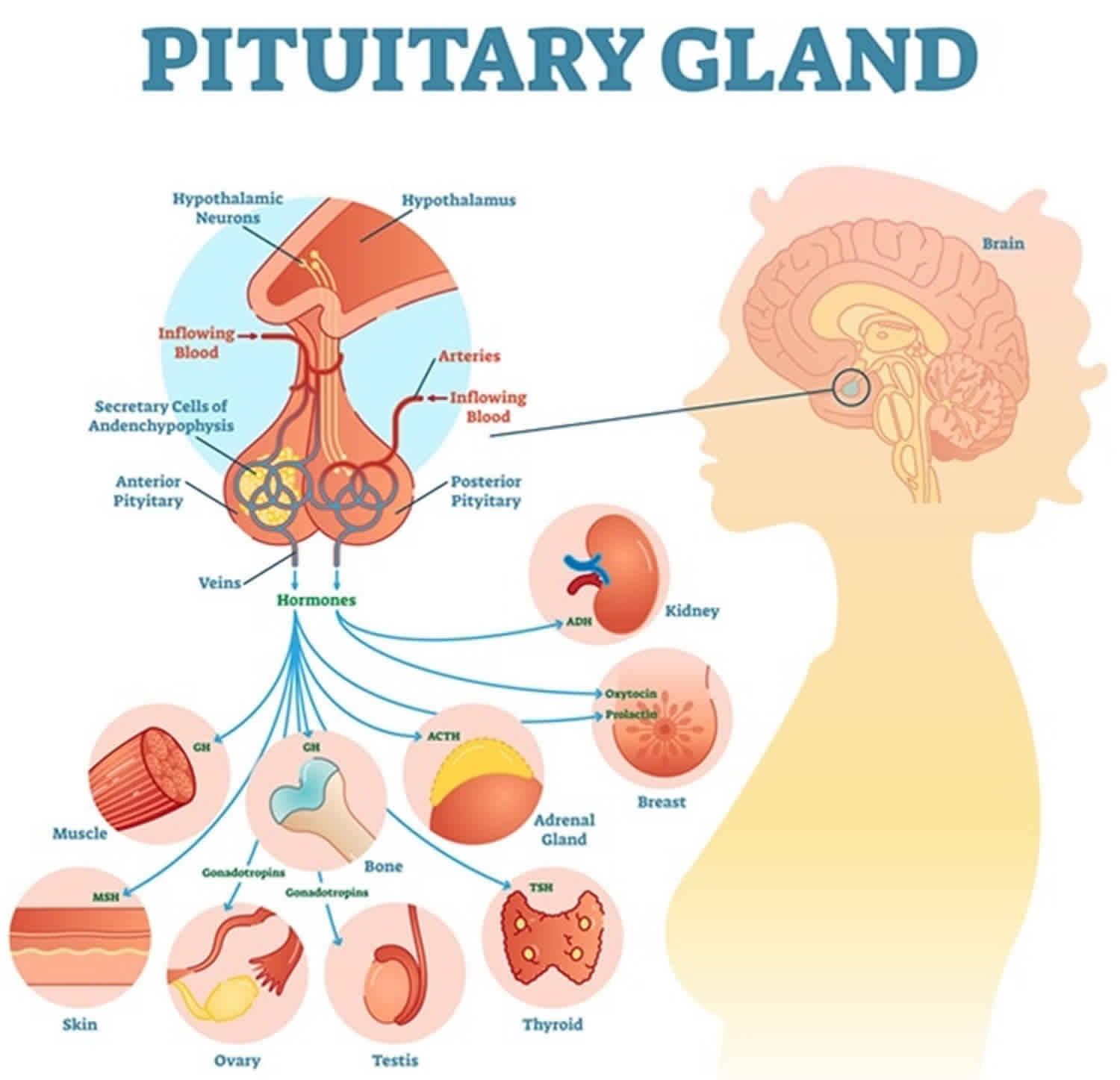
Pituitary hormones regulate the rest of your endocrine system, signaling other glands to increase or decrease production of the hormones that control metabolism, fertility, blood pressure, breast milk production and many other vital processes. A lack of any of these hormones can cause problems throughout your body.
Hormones from the front of your pituitary include:
- Growth hormone (GH). This hormone controls bone and tissue growth and maintains the right balance of muscle and fat tissue.
- Thyroid-stimulating hormone (TSH). This hormone stimulates your thyroid gland to produce key hormones that regulate your metabolism. Shortage of TSH results in an underactive thyroid gland (hypothyroidism).
- Luteinizing hormone (LH). In women, LH regulates estrogen.
- Follicle-stimulating hormone (FSH). Working with LH, FSH helps stimulate egg development and ovulation in women.
- Adrenocorticotropic hormone (ACTH). This hormone stimulates your adrenal glands to produce cortisol and other hormones. Cortisol helps your body deal with stress and influences many body functions, including blood pressure, heart function and your immune system. A low level of adrenal hormones caused by pituitary damage is called secondary adrenal insufficiency.
- Prolactin. This hormone regulates the development of female breasts, as well as the production of breast milk.
Risk factors for developing Sheehan syndrome
Any condition that increases the chance of severe blood loss (hemorrhage) or low blood pressure during childbirth, such as being pregnant with multiples or having a problem with the placenta, can increase your risk of Sheehan’s syndrome.
Hemorrhage is a rare childbirth complication, however, and Sheehan’s syndrome is even more uncommon. Both risks are greatly reduced with proper care and monitoring during labor and delivery.
Sheehan syndrome pathophysiology
Pituitary gland volume and cell count increase in pregnant women in the weeks preceding delivery 4. This increase is caused principally by hyperplasia of prolactin producing cells (lactotrophs) and hyperplasia of other cells in the anterior pituitary gland. This hyperplasia leads to increased nutritional and metabolic demand by the anterior pituitary gland as a whole, but the blood supply that feeds the anterior pituitary does not increase 4. The blood supply that feeds the anterior pituitary gland is a relatively low-pressure system. It is theorized that this is the mechanism that makes the pituitary cells more susceptible to ischemia. Consequently, the cells of the anterior pituitary are more prone to necrosis in pregnancies complicated by significant postpartum hemorrhage. The posterior pituitary gland has its blood supply which functions under higher pressure than the anterior pituitary, so it is not usually affected by shock or hypovolemia 5.
Sheehan syndrome is the clinical manifestation of anterior pituitary cell necrosis and may present as pan-hypopituitarism or as selective loss of pituitary function. Pan-hypopituitarism is a result when many cells of the pituitary are affected, as opposed to only a few cells. Pan-hypopituitarism is far more common than the selective loss of pituitary function. Prolactin and growth hormone are the most common hormones affected by selective pituitary necrosis and hypofunction. The posterior pituitary function is usually not affected as stated above. However, diabetes insipidus can occur, but it is a rare manifestation of Sheehan syndrome 6.
Sheehan syndrome symptoms
Signs and symptoms of Sheehan’s syndrome typically appear slowly, after a period of months or even years. But sometimes problems appear right away, such as the inability to breast-feed.
Signs and symptoms of Sheehan’s syndrome occur because of having too little of the hormones the pituitary gland controls: thyroid, adrenal, breast milk production and menstrual function hormones. These include:
- Difficulty breast-feeding (breast milk never “comes in”) or an inability to breast-feed
- No menstrual periods (amenorrhea) or infrequent menstruation (oligomenorrhea)
- Inability to regrow shaved pubic hair
- Slowed mental function, weight gain and difficulty staying warm as a result of an underactive thyroid (hypothyroidism)
- Low blood pressure (hypotension)
- Low blood sugar (hypoglycemia)
- Fatigue
- Irregular heartbeat
- Breast shrinkage
- Loss of pubic and axillary hair
Note: Other than not being able to breast feed, symptoms may not develop for several years after the delivery.
For many women, Sheehan’s syndrome symptoms are nonspecific and often thought to be caused by other things. Fatigue, for instance, goes hand in hand with being a new mother. You might not realize you have Sheehan’s syndrome until you need treatment for thyroid or adrenal insufficiency.
It’s also possible to remain relatively symptom-free with Sheehan’s syndrome, depending on the extent of damage to the pituitary gland. Some women live for years not knowing their pituitary isn’t working properly. Then an extreme physical stressor, such as severe infection or surgery, triggers an adrenal crisis.
Sheehan syndrome possible complications
Because pituitary hormones control so many aspects of your metabolism, Sheehan’s syndrome can cause a number of problems, including:
- Adrenal crisis, a serious condition in which your adrenal glands produce too little of the hormone cortisol
- Low blood pressure
- Unintended weight loss
- Menstrual irregularities
Adrenal crisis: Life-threatening situation
The most serious complication is adrenal crisis, a sudden, life-threatening state that can lead to extremely low blood pressure, shock, coma and death.
Adrenal crisis usually occurs when your body is under marked stress — such as during surgery or a serious illness — and your adrenal glands produce too little cortisol, a powerful stress hormone.
Because of the potentially serious consequences of adrenal insufficiency, your doctor is likely to recommend that you wear a medical alert bracelet.
Sheehan syndrome diagnosis
Diagnosing Sheehan’s syndrome can be difficult. Many of the symptoms overlap with those of other conditions. To diagnose Sheehan’s, your doctor likely will:
- Collect a thorough medical history. It’s important to mention any childbirth complications you’ve had, no matter how long ago you gave birth. Also, be sure to tell your doctor if you didn’t produce breast milk or you failed to start menstruating after delivery — two key signs of Sheehan’s syndrome.
- Run blood tests. Blood tests will check your pituitary hormone levels.
- Request a pituitary hormone stimulation test. You might need stimulation testing of the pituitary hormones, which involves injecting hormones and running repeated blood tests to see how your pituitary responds. This test is typically done after consulting a doctor who specializes in hormonal disorders (endocrinologist).
- Request imaging tests. You might also need imaging tests, such as an MRI scan or CT scan, to check the size of your pituitary and to look for other possible reasons for your symptoms, such as a pituitary tumor.
Evaluation of anterior pituitary gland function is done by obtaining blood when a high clinical suspicion is evident to diagnose Sheehan syndrome. The hormones that are manufactured in the anterior pituitary gland are:
- the gonadotropins such as follicle stimulating hormone (FSH) and luteinizing hormone (LH),
- growth hormone (GH),
- prolactin (PRL),
- adrenocorticotropic hormone (ACTH),
- thyroid stimulating hormone (TSH).
They are affected primarily in a certain order when necrosis occurs, growth hormone (GH) first, followed by prolactin (PRL), follicle stimulating hormone (FSH), luteinizing hormone (LH), adrenocorticotropic hormone (ACTH) and then thyroid stimulating hormone (TSH) last 3. Laboratory tests to order would include a complete blood count (CBC) with differenial, basic metabolic profile, thyroid function tests (TSH, FT3, FT4), FSH, LH, prolactin, estrogen, cortisol, and growth hormone 7. Finding a low basal hormone level along with a history and physical suggestive of Sheehan syndrome would help to make the diagnosis.
Other laboratory tests that may occur with Sheehan syndrome include a normocytic/normochromic anemia, thrombocytopenia, and/or pancytopenia. Hyponatremia and hypoglycemia may also be present as well. Other less common laboratory tests in the workup for Sheehan syndrome that may be abnormal include multiple thrombophilic genetic mutations, low PT and aPTT tests, anti-pituitary antibodies, and anti-hypothalamus antibodies 8. These tests may be considered after the primary tests to confirm the diagnosis. Also, a magnetic resonance imaging (MRI) evaluation of the pituitary can be done to confirm the diagnosis. An empty sella is present in about 70% of patients, and a partially empty sella is present in about 30% of patients on a later MRI 9. Acute Sheehan syndrome signs on an MRI may demonstrate acute central infarction without hemorrhage in an enlarged pituitary. As the disease progresses, the MRI may show pituitary gland atrophy and eventually a partial or empty sella 10.
Sheehan syndrome treatment
Treatment for Sheehan syndrome is lifelong hormone replacement therapy for the hormones you’re missing. Your doctor might recommend one or more of the following medications:
- Corticosteroids. These drugs, such as hydrocortisone or prednisone, replace the adrenal hormones that aren’t being produced because of an adrenocorticotropic hormone (ACTH) deficiency. You’ll need to adjust your medication if you become seriously ill or undergo major physical stress. During these times, your body would ordinarily produce extra cortisol — a stress hormone. The same kind of dosage fine-tuning may be necessary when you have the flu, diarrhea or vomiting, or have surgery or dental procedures. Adjustments in dosage might also be necessary during pregnancy or with marked weight gain or weight loss. Avoiding doses higher than you need can help avoid the side effects associated with high doses of corticosteroids.
- Levothyroxine (Levoxyl, Synthroid, others). This medication boosts deficient thyroid hormone levels caused by low or deficient thyroid-stimulating hormone (TSH) production. If you change brands, let your doctor know to ensure you’re still receiving the right dosage. Also, don’t skip doses or stop taking the drug because you’re feeling better. If you do, signs and symptoms will gradually return.
- Estrogen. This includes estrogen alone if you’ve had your uterus removed (hysterectomy) or a combination of estrogen and progesterone if you still have your uterus. Estrogen use has been linked to an increased risk of blood clots and stroke in women who still make their own estrogen. The risk should be less in women who are replacing missing estrogen. Preparations containing luteinizing hormone (LH) and follicle-stimulating hormone (FSH), also called gonadotropins, might make future pregnancies possible. These can be administered by injection to stimulate ovulation. After age 50, around the time of natural menopause, discuss the risks and benefits of continuing to take estrogen or estrogen and progesterone with your doctor.
- Growth hormone. Some studies have shown that replacing growth hormone in women with Sheehan’s syndrome — as well as in adults with other forms of hypopituitarism — can help normalize the body’s muscle-to-fat ratio, maintain bone mass, lower cholesterol levels and improve overall quality of life. Side effects might include joint stiffness and fluid retention.
- For patients who develop diabetes insipidus, desmopressin nasal (DDAVP) is the recommended treatment of choice.
Referral to an endocrinologist who is familiar with hypopituitarism and the usage of growth hormone is recommended 11. Your endocrinologist is likely to test your blood regularly to make sure that you’re getting adequate — but not excessive — amounts of hormones. Generally, hormone levels are checked every few months at the beginning of treatment and then once a year thereafter.
Sheehan syndrome prognosis
Sheehan syndrome outlook with early diagnosis and treatment is excellent. Sheehan syndrome can be life threatening if not treated.
- Karaca Z, Laway BA, Dokmetas HS, Atmaca H, Kelestimur F. Sheehan syndrome. Nat Rev Dis Primers. 2016 Dec 22; 2:https://www.ncbi.nlm.nih.gov/pubmed/28004764[↩]
- Sheehan’s syndrome. https://www.mayoclinic.org/diseases-conditions/sheehans-syndrome/symptoms-causes/syc-20351847[↩][↩][↩]
- Karaca Z, Laway BA, Dokmetas HS, Atmaca H, Kelestimur F. Sheehan syndrome. Nat Rev Dis Primers. 2016 Dec 22;2:16092.[↩][↩]
- Schury MP, Adigun R. Sheehan Syndrome. [Updated 2019 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459166[↩][↩]
- Woodmansee WW. Pituitary Disorders in Pregnancy. Neurol Clin. 2019 Feb;37(1):63-83.[↩]
- Wang CZ, Guo LL, Han BY, Su X, Guo QH, Mu YM. Pituitary Stalk Interruption Syndrome: From Clinical Findings to Pathogenesis. J. Neuroendocrinol. 2017 Jan;29, 1[↩]
- Drummond JB, Ribeiro-Oliveira A, Soares BS. Non-Functioning Pituitary Adenomas. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, Hershman JM, Kaltsas G, Koch C, Kopp P, Korbonits M, McLachlan R, Morley JE, New M, Perreault L, Purnell J, Rebar R, Singer F, Trence DL, Vinik A, Wilson DP, editors. Endotext [Internet]. MDText.com, Inc.; South Dartmouth (MA): Nov 28, 2018[↩]
- Chiloiro S, Tartaglione T, Angelini F, Bianchi A, Arena V, Giampietro A, Mormando M, Sciandra M, Laino ME, De Marinis L. An Overview of Diagnosis of Primary Autoimmune Hypophysitis in a Prospective Single-Center Experience. Neuroendocrinology. 2017;104(3):280-290[↩]
- Kanekar S, Bennett S. Imaging of Neurologic Conditions in Pregnant Patients. Radiographics. 2016 Nov-Dec;36(7):2102-2122[↩]
- Miljic D, Pekic S, Popovic V. Empty Sella. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, Hershman JM, Kaltsas G, Koch C, Kopp P, Korbonits M, McLachlan R, Morley JE, New M, Perreault L, Purnell J, Rebar R, Singer F, Trence DL, Vinik A, Wilson DP, editors. Endotext [Internet]. MDText.com, Inc.; South Dartmouth (MA): Oct 1, 2018[↩]
- Matsuzaki S, Endo M, Ueda Y, Mimura K, Kakigano A, Egawa-Takata T, Kumasawa K, Yoshino K, Kimura T. A case of acute Sheehan’s syndrome and literature review: a rare but life-threatening complication of postpartum hemorrhage. BMC Pregnancy Childbirth. 2017 Jun 14;17(1):188[↩]