Contents
Swollen uvula causes
Swollen uvula is also called an uvulitis, which is inflammation of the uvula, the small tongue-shaped piece of tissue that hangs from the top of the back part of the mouth. Swollen uvula is usually associated with inflammation or infection involving other mouth parts, such as the palate, tonsils, or throat (pharynx). Acute painful swelling of uvula is an uncommon infectious condition 1. Swollen uvula frequently accompanies pharyngitis or epiglottitis 2. The classic reports of swollen uvula highlight the association of uvulitis with epiglittitis, a lifethreatening
condition 3. Some authors associate swollen uvula with allergic angioedema 4. Current reports of swollen uvula link uvulitis with group A streptococcal pharyngitis 2 or Haemophilia influenzae type b epiglottitis 5. These reports highlighted the importance of diagnosing the underlying epiglottitis, which may become an emergency 3.
Uvulitis and epiglottitis can have similar presenting symptoms such as fever, sore throat, and painful swallowing (odynophagia). Lateral neck radiography looking for an enlarged epiglottis (“thumb” sign) is recommended, given the similarities in presentation to uvulitis and the seriousness of epiglottitis if missed. If there are signs of airway obstruction, laryngoscopy should be performed in a controlled setting such as the intensive care unit, as it may precipitate sudden airway obstruction. Close observation in the intensive care unit is recommended in adults presenting with epiglottitis because of the risk of rapid deterioration and the need to secure the airway. Empirical therapy with intravenous antibiotics (e.g., a third-generation cephalosporin or a beta-lactamase inhibitor combination) to cover the common pathogens mentioned above is recommended and should then be tailored according to the results of blood culture testing.
Swollen uvula can also be caused by mechanical trauma, chemical or thermal injury 6. Allergic edema of uvula (Quincke’s edema) has been described wherein uvula is grossly enlarged but not erythematus. Fever and pain will be absent. Swollen uvula can also occur following general anesthesia with laryngeal mask airway and endotracheal tube even in the absence of direct trauma 7.
Uvulitis has not been previously described as a clinical entity occurring in the absence of pharyngitis or epiglottitis, except by Karl Li et al. 8, who reported two cases of isolated uvulitis (one case of 3.5-year-old boy and another 7-month-old child, the causative organism was Haemophilus influenzae type b).
Lathadevi et al. 1 presented five cases of uvulitis associated with neither tonsillopharyngitis nor epiglottitis. All cases presented with sudden onset of throat pain, choking, odynophagia, mild fever, and severely congested uvula. Laboratory investigations were normal except mild neutrophilia.
In the first and the last cases, the culture showed coagulase positive streptococci. Other cases showed sterile culture perhaps because of the fact that antibiotics were given before culture swab was taken (patients were admitted at midnight).
From these case reports, it is apparent that the focus of infection is uvula, occurring in adults with acute onset and respond to penicillin immediately. The organisms may be the same as bacteria-causing upper respiratory tract infection. In Karl L. Li’s 8 two cases, Haemophilus influenzae type b was the causative organism.
What is epiglottitis
Epiglottitis is inflammation of the epiglottis. Epiglottitis is a potentially life-threatening condition that occurs when the epiglottis — a small cartilage “lid” that covers your windpipe (trachea) — swells, blocking the flow of air into your lungs.
A number of factors can cause the epiglottis to swell — burns from hot liquids, direct injury to your throat and various infections. The most common cause of epiglottitis in children in the past was infection with Haemophilus influenzae type b (Hib), the same bacterium that causes pneumonia, meningitis and infections in the bloodstream. Epiglottitis can occur at any age.
Routine haemophilus influenzae type b (Hib) vaccination for infants has made epiglottitis rare, but the condition remains a concern. If you suspect that you or someone in your family has epiglottitis, seek emergency help immediately. Prompt treatment can prevent life-threatening complications.
Epiglottitis is a medical emergency. If you or someone you know suddenly has trouble breathing and swallowing, call your local emergency number for an ambulance or go to the nearest hospital emergency department. Try to keep the person quiet and upright, because this position may make it easier to breathe. Don’t try to examine the person’s throat yourself. This can make matters worse.
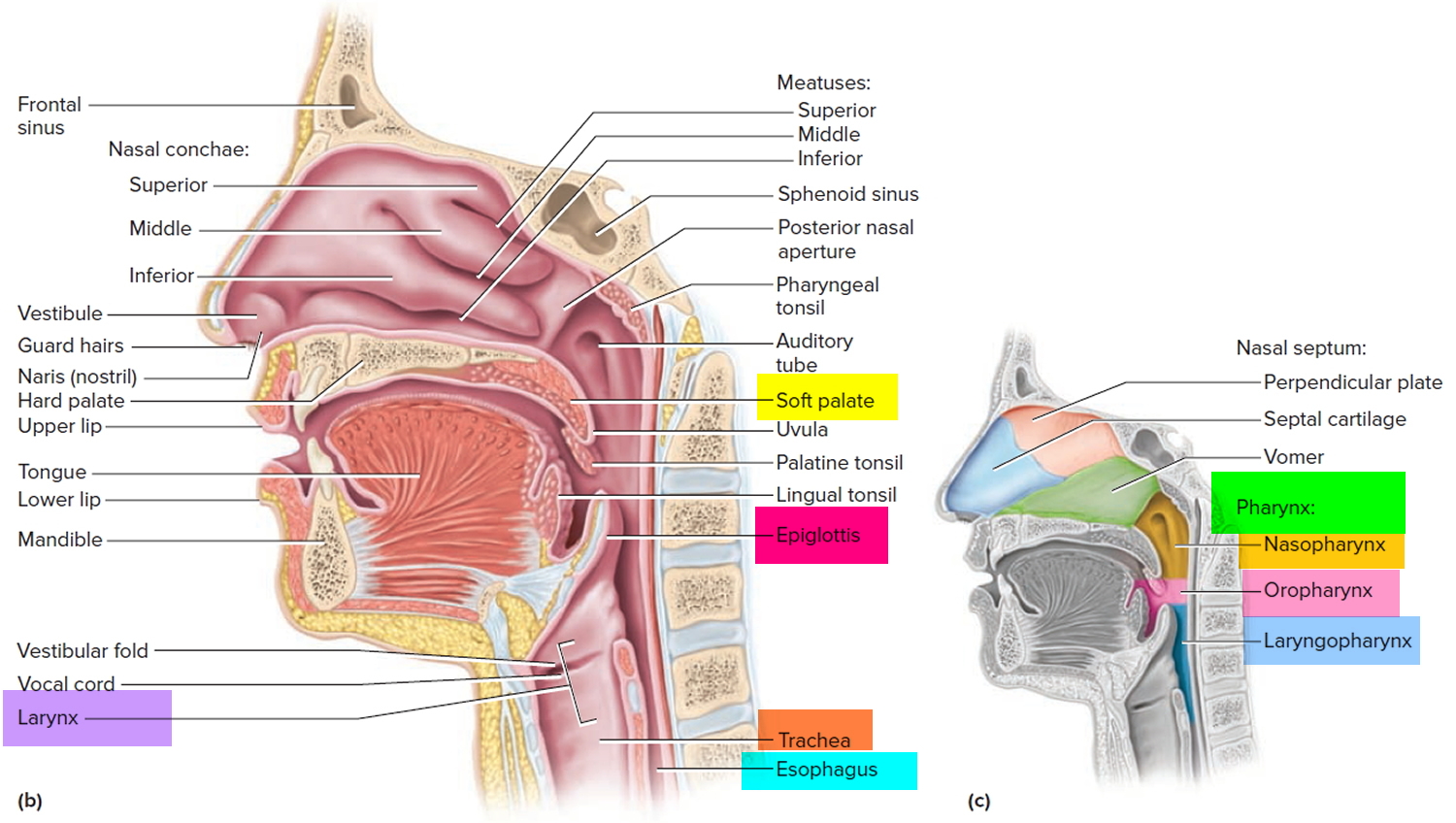
Figure 1. Larynx and pharynx anatomy
Epiglottitis complications
Epiglottitis can cause a number of complications, including:
- Respiratory failure. The epiglottis is a small, movable “lid” just above the larynx that prevents food and drink from entering your windpipe. But if the epiglottis becomes swollen — either from infection or from injury — the airway narrows and may become completely blocked. This can lead to respiratory failure — a life-threatening condition in which the level of oxygen in the blood drops dangerously low or the level of carbon dioxide becomes excessively high.
- Spreading infection. Sometimes the bacteria that cause epiglottitis cause infections elsewhere in the body, such as pneumonia, meningitis or a blood infection (sepsis).
Epiglottitis can lead to airway loss and death. Epiglottic abscess has been found to occur in up to 24% of patients 9. The abscesses can often be detected using a computed tomography scan, while a magnetic resonance imaging shows obliteration of the surrounding fat planes. These scans require the patient to be in a supine position, and with this condition, respiratory distress can be greater when the patient is supine. If computed tomography or magnetic resonance imaging is felt to be necessary in a complicated patient, consideration should be given to securing the airway before placing these patients in the supine position in an imaging department. Likewise, naso-fiberoptic exam can also assess edema and abscesses even when performed on an intubated patient. Patients with epiglottic abscess often require drainage of the abscess in addition to intravenous antibiotics. Descending necrotizing mediastinitis has also been reported in cases of epiglottitis 10. These patients often require drainage of the mediastinum in addition to drainage of the primary abscess and airway management via tracheotomy. Immunocompromised patients are at a higher risk of these complications, and physicians must therefore use broad-spectrum antibiotics as well as debridement, as needed.
Epiglottitis causes
Epiglottitis is can be caused by an infection or an injury.
Infection
In the past, a common cause of swelling and inflammation of the epiglottis and surrounding tissues was infection with Haemophilus influenzae type b (Hib) bacteria. Haemophilus influenzae type b (Hib) is responsible for a number of serious conditions, the most common of which is meningitis. This is now much less common in developed countries due to Haemophilus influenzae type b (Hib) immunization in children.
Haemophilus influenzae type b (Hib) spreads through infected droplets coughed or sneezed into the air. It’s possible to harbor Hib in your nose and throat without becoming sick — though you still have the potential to spread the bacteria to others.
In adults, other bacteria and viruses also can cause inflammation of the epiglottis, including:
- Streptococcus pneumoniae (pneumococcus), another bacterium that can cause meningitis, pneumonia, ear infections and blood infection (septicemia)
- Streptococcus A, B and C, a group of bacteria that also can cause diseases ranging from strep throat to blood infections
- Staphylococcus aureus, a bacterium that causes skin infections and other diseases including pneumonia and toxic shock syndrome
Injury
Physical injury, such as a direct blow to the throat, can cause epiglottitis. So can burns from drinking very hot or caustic liquids.
You also may develop signs and symptoms similar to those of epiglottitis if you:
- Swallow a chemical that burns your throat
- Swallow a foreign object
- Smoke drugs, such as crack cocaine
Risk factors for epiglottitis
Certain factors increase the risk of developing epiglottitis, including:
- Being male. Epiglottitis affects more males than females.
- Having a weakened immune system. If your immune system has been weakened by illness or medication, you’re more susceptible to the bacterial infections that may cause epiglottitis.
- Lacking adequate vaccination. Delayed or skipped immunizations can leave a child vulnerable to Hib and increases the risk of epiglottitis.
Epiglottitis prevention
Haemophilus influenzae type b (Hib) vaccine
The most effective way to prevent your child getting epiglottitis is to make sure their vaccinations are up to date.
Children are particularly vulnerable to a Hib infection, because they have an underdeveloped immune system.
Children should receive their Hib as part of the 5 in 1 DTaP/IPV/Hib vaccine, which also protects against diphtheria, tetanus, whooping cough and polio.
Immunization with the Hib vaccine is an effective way to prevent epiglottitis caused by Hib. Children should receive three doses of the vaccine: one at two months, one when they are three months and one when they are four months old. This is followed by an additional Hib/Men C “booster” vaccine at 12 months.
In the United States, children usually receive the vaccine in three or four doses:
- At 2 months
- At 4 months
- At 6 months if your child is being given the four-dose vaccine
- At 12 to 15 months
The Hib vaccine is generally not given to children older than age 5 or to adults because they’re less likely to develop Hib infection. But the Centers for Disease Control and Prevention recommends the vaccine for older children and adults whose immune systems have been weakened by:
- Sickle cell disease
- HIV/AIDS
- Spleen removal
- Chemotherapy
- Medications to prevent rejection of organ or bone marrow transplants
Haemophilus influenzae type b (Hib) vaccine side effects
- Allergic reaction. Seek immediate medical help if you have an allergic reaction. Though rare, an allergic reaction may cause difficulty breathing, wheezing, hives, weakness, a rapid heartbeat or dizziness within minutes or a few hours after the shot.
- Possible mild side effects. These include redness, warmth, swelling or pain at the injection site, and a fever.
Commonsense precautions
Of course, the Hib vaccine doesn’t offer guarantees. Immunized children have been known to develop epiglottitis — and other germs can cause epiglottitis, too. That’s where commonsense precautions come in:
- Don’t share personal items.
- Wash your hands frequently.
- Use an alcohol-based hand sanitizer if soap and water aren’t available.
Epiglottitis symptoms
The symptoms of epiglottitis usually develop quickly and get rapidly worse, although they can develop over a few days in older children and adults.
The typical presentation in epiglottitis includes acute occurrence of high fever, severe sore throat and difficulty in swallowing with the sitting up and leaning forward position in order to enhance airflow. There is usually drooling because of difficulty and pain on swallowing. Acute epiglottitis usually leads to generalized toxemia. The most common differential diagnosis is croup and a foreign body in the airway. A late referral to an acute care setting with its serious consequences may result from difficulty in differentiation between acute epiglottitis and less urgent causes of a sore throat, shortness of breath and dysphagia. Antibiotic therapy is usually initiated without preceding bacterial culture, with the consequence of negative cultures at admission.
Epiglottitis symptoms include:
- a severe sore throat
- difficulty and pain when swallowing
- difficulty breathing, which may improve when leaning forwards
- breathing that sounds abnormal and high-pitched (stridor)
- a high temperature (fever) of 38 °C (100.4 °F) or above
- irritability and restlessness
- muffled or hoarse voice
- drooling
The main symptoms of epiglottitis in young children are breathing difficulties, stridor and a hoarse voice. In adults and older children, the main signs are a severe sore throat, swallowing difficulties and drooling.
Difficulty in breathing and stridor are common signs of epiglottitis in children, but are less frequent in adults. The most common presenting symptom in adults is odynophagia [painful swallowing] (100%), followed by dysphagia [difficulty in swallowing] (85%) and voice change (75%) 11. In adults, stridor is regarded as a warning sign for occlusion of the upper airway. Stridor, tachycardia, tachypnea, rapid onset of symptoms and a “thumb-sign” (see Figures 3 and 4 below) present in 79% of the cases on lateral X-rays of the neck are significant predictors for imminent airway compromise with rapid clinical deterioration 12.
Symptoms in children
In children, signs and symptoms of epiglottitis may develop within a matter of hours, including:
- Fever
- Severe sore throat
- Abnormal, high-pitched sound when breathing in (stridor)
- Difficult and painful swallowing
- Drooling
- Anxious, restless behavior
- Greater comfort when sitting up or leaning forward
Epiglottitis can cause a life-threatening airway emergency. Patients with epiglottitis usually present with a generalized toxemia, including high fevers, severe sore throat, and difficulty swallowing. Stridor, if present, is usually inspiratory. The patient may be sitting up and leaning forward in the sniffing position, breathing with an open mouth and a protruding tongue. The child frequently drools because of difficulty and pain on swallowing. This “tripod position” may not be present in the older child/adult presenting with epiglottitis. Findings may only include subtle signs of respiratory difficulties, such as the inability to lie flat, voice changes, and dysphagia. Epiglottitis patients tend to experience acute onset of symptoms. In one series, while both croup and epiglottitis were associated with acute stridor, croup was also associated with coughing and no drooling, while epiglottitis was associated with drooling and the lack of coughing.6
Symptoms in adults
For adults, signs and symptoms may develop more slowly, over days rather than hours. Signs and symptoms may include:
- Severe sore throat
- Fever
- A muffled or hoarse voice
- Abnormal, high-pitched sound when breathing in (stridor)
- Difficulty breathing
- Difficulty swallowing
- Drooling
Supraglottitis, or inflammation of the supraglottic larynx, seen in adults, has a different presentation than epiglottitis in children. Adults with supraglottitis have predominant symptoms of odynophagia, dysphagia, and voice changes out of proportion to pharyngeal inflammation. Childhood epiglottitis—muffled voice, drooling, dyspnea, stridor, and cough—occurs in less than 50% of adults 13. Adults may also experience fever, toxic appearance, cervical lymphadenopathy, and anterior neck and chest cellulitis. Guardiani et al. 14, based on a 10-yr study of 60 adults and 1 child, described odynophagia (painful swallowing) (100% of patients) as the most common symptom, followed by difficulty swallowing (85%) and voice changes (74%). The presentation of adult supraglottitis peaks at 42 to 48 yr of age, with a male predilection of 2.5:1 15. This “tripod position” may not be present in the older child/adult presenting with epiglottitis.
Epiglottitis diagnosis
If your doctor suspects epiglottitis, the first priority is to ensure that your or your child’s airway is open and that enough oxygen is getting through.
Initial test
A pulse oximeter is a device that estimates blood oxygen levels. This device:
- Clips onto a finger
- Measures an estimation of the saturation of oxygen in your blood
If oxygen saturation levels drop too low, you or your child may need help breathing.
Tests after stabilizing breathing
- Throat examination. Using a flexible fiber-optic-lighted tube, the doctor may look down your or your child’s throat to see what’s causing the symptoms. A local anesthetic can help relieve any discomfort. In case of the diagnosis of epiglottitis, a fibreoptic nasal intubation or rigid bronchoscopy using an endotracheal tube with substantially reduced diameter is preferred. Because of the risk of inducing laryngeal spasm and/or total airway obstruction, examination of the pharynx and larynx should be attempted only in an area with adequate equipment and staff prepared to intervene should upper airway obstruction develop, ideally, in the operating room.
- Chest or neck X-ray. Because of the danger of sudden breathing problems, children may have X-rays taken at their bedside rather than in the radiology department — but only after the airway is protected. With epiglottitis, the X-ray may reveal what looks like a thumbprint in the neck, an indication of an enlarged epiglottis.
- Ultrasonography has been described as a way to investigate the epiglottis by visualization of the “alphabet P sign” in a longitudinal view through the thyrohyoid membrane (Figure 5) 16.
- Throat culture and blood tests. For the culture, the epiglottis is wiped with a cotton swab and the tissue sample is checked for Hib. Blood cultures are usually taken because bacteremia — a severe bloodstream infection — may accompany epiglottitis.
In acute epiglottitis, the radiological “thumb sign” (Figures 3 and 4) is indicative of severe inflammation of the epiglottis with potential for irrevocable loss of the airway. The thumb sign in epiglottitis is a manifestation of swelling and enlarged epiglottis which is seen on lateral soft-tissue radiograph of the neck, and it suggests a diagnosis of acute infectious epiglottitis. This is the radiographic corollary of the omega sign 17.
Epiglottitis treatment
Patients with signs of an advancing upper airway obstruction, consistent with an acute epiglottitis, should be treated as a medical and an airway emergency. In the presence of respiratory distress, diagnostic procedures and radiography are not indicated, and securing the airway should be prioritized.
Treatment of epiglottitis involves first making sure you or your child can breathe, and then treating any identified infection.
Helping you breathe
The first priority in treating epiglottitis is ensuring that you or your child is receiving enough air. This may mean:
- Wearing a mask. The mask delivers oxygen to the lungs.
- Having a breathing tube placed into the windpipe through the nose or mouth (tracheal intubation). The tube must remain in place until the swelling in your or your child’s throat has decreased — sometimes for several days.
- Inserting a needle into the trachea (needle tracheostomy). In extreme cases or if more conservative measures fail, the doctor may need to create an emergency airway by inserting a needle directly into an area of cartilage in your or your child’s trachea. This procedure allows air into your lungs while bypassing the larynx.
Tracheal intubation of a patient with epiglottitis must be regarded as a potentially difficult procedure 18. It should be done in strict monitored conditions, i.e. in the operating room, while maintaining spontaneous ventilation. The readiness of a team capable of performing an immediate tracheotomy should be verified. The patient should be transferred to the operating room under the supervision of an experienced anesthesiologist and surgeon 18. The induction may be performed with the patient sitting upright. Forcing the child/patient into a supine position may precipitate acute airway obstruction. Anesthesia induction with achievement of a deep level of anesthesia and maintenance of spontaneous ventilation has been described as the method of choice. The amount of time necessary to produce deep anesthesia using an inhalation induction may be increased secondary to airway obstruction and may necessitate increasing gas concentration. Capnography with exhaled gas analysis is useful in determining anesthetic depth. Muscle relaxants are avoided and spontaneous ventilation should be maintained. The patient should be transferred sedated to an intensive care unit (ICU) after securing the airway. Intravenous sedation should ideally allow spontaneous ventilation. Tracheal extubation should be preceded by a cuff leak test with a deflated cuff and, usually, a second look by direct laryngoscopy with deep sedation or general anesthesia. Complications of acute epiglottitis may include deep neck space infection, recurrent illness and vocal granuloma 19. Dexamethasone treatment or budesonide aerosols could be used in an attempt to limit pharyngeal edema and thereby reduce the obstruction. The use of corticosteroids has been associated with shorter ICU and overall length of stay, with an average overall length of stay of 3.8 days in adults 20.
Once the airways have been secured and the person is able to breathe unrestricted, a more comfortable and convenient way of assisting breathing may be found. This is usually achieved by threading a tube through the nose and into the windpipe.
Fluids will be supplied through a drip into one of your veins, until the person is able to swallow.
Once this has been achieved and the situation is thought to be safe, some tests may be carried out, such as:
- a fibre-optic laryngoscopy – a flexible tube with a camera attached to one end (laryngoscope) is used to examine the throat
- a throat swab – to test for any bacteria or viruses
- blood tests – to check the number of white blood cells (a high number indicates there may an infection) and to identify any traces of bacteria or viruses in the blood
- an X-ray or a computerised tomography (CT) scan – sometimes used to check the level of swelling
The underlying infection will then be treated with a course of antibiotics, and most people with epiglottitis are well enough to leave hospital after five to seven days.
With prompt treatment, most people recover from epiglottitis after about a week and are usually well enough to leave hospital after five to seven days.
Treating infection
If your epiglottitis is related to an infection, intravenous antibiotics will be given once you or your child is getting enough air.
- Broad-spectrum antibiotic. Because of the need for quick treatment, rather than wait for the results of the blood and tissue cultures, you or your child is likely to be treated with a broad-spectrum drug.
- More-targeted antibiotic. The drug may be changed later, depending on what’s causing the epiglottitis.
What is angioedema
Angioedema is swelling underneath the skin caused by fluid leakage from blood vessels into the surrounding skin and tissue. Angioedema is usually a reaction to a trigger, such as a medication or something you’re allergic to. Angioedemais most often characterized by a sudden or come on gradually over a few hours of short-lived swelling of the skin and mucous membranes. Swelling caused by angioedema normally lasts a few days. All parts of your body may be affected but swelling most often occurs around the eyes, lips, mouth, tongue, extremities, and genitalia. In severe cases the internal lining of the upper respiratory tract and intestines may also be affected causing breathing difficulties, tummy (abdominal) pain and dizziness. The swelling may be accompanied by a raised, itchy rash called hives (urticaria), which are more superficial, while angioedema affects the deeper layers of skin.
Angioedema isn’t normally serious, but it can be a recurring problem for some people and can very occasionally be life-threatening if it affects your breathing.
Treatment can usually help keep the swelling under control.
See your doctor if you have episodes of swelling that affect your skin or lips and you’re not certain of the cause.
You may need to have some tests to determine the cause. Read more about tests for angioedema.
Dial your local emergency services number for an ambulance if you, or someone with you, has swelling and:
- sudden or worsening breathing problems
- feels faint or dizzy
- passes out or collapses
These are signs of a serious allergic reaction (anaphylaxis). If you, or the person who’s ill, have been prescribed an adrenaline auto-injector for this, use it while waiting for the ambulance to arrive.
Figure 2. Angioedema eyes
Figure 3. Angioedema lips
Angioedema symptoms
Symptoms and signs of angioedema may vary slightly between the different types of angioedema but in general the main symptom of angioedema is swelling that develops below the skin’s surface:
- Marked swelling, usually around the eyes and mouth (lips and tongue)
- Throat, tongue, hands, feet and/or genitals may be affected too
- Skin may appear normal, i.e. no hives or other rash
- Swellings may or may not be itchy
- Swellings may be painful, tender or burning
- In severe angioedema swelling of the throat and/or tongue may make it difficult to breath
- Swelling of the lining of the intestinal tracts may cause gastrointestinal pain and cramps
Many people also have a raised, itchy rash called urticaria (hives). The rash will usually settle in a few days. Otherwise, the skin over the swelling may feel tight and painful but look normal.
Less common symptoms of angioedema include:
- difficulty breathing
- red, irritated eyes (conjunctivitis)
- tummy (abdominal) pain
- feeling sick
- diarrhea
- dizziness
- fainting
Some features specific to the different types of angioedema are listed below.
| Angioedema type | Clinical features |
|---|---|
| Acute allergic angioedema |
|
| Non-allergic drug reaction angioedema (drug-induced angioedema) |
|
| Idiopathic/chronic angioedema |
|
| Hereditary angioedema |
|
What causes angioedema
There are several different types of angioedema, each of which has a different cause. Angioedema can be classified into at least four types, acute allergic angioedema, non-allergic drug reactions, idiopathic angioedema, hereditary angioedema and acquired C1 inhibitor deficiency.
Whatever the cause of angioedema, the actual mechanism behind the swelling is the same in all cases. Small blood vessels in the subcutaneous and/or submucosal tissues leak watery liquid through their walls and cause swelling. This same mechanism occurs in urticaria but just closer to the skin surface.
| Angioedema type | Causes |
|---|---|
| Acute allergic angioedema (almost always occurs with urticaria within 1-2 hours of exposure to the allergen) |
|
| Non-allergic drug reaction (drug-induced angioedema) (onset may be days to months after first taking the medication) |
|
| Idiopathic angioedema (frequently chronic and relapsing and usually occurs with urticaria) |
|
| Hereditary angioedema (very rare autosomal dominant inherited disease) |
|
| Acquired C1 inhibitor deficiency |
|
Allergic angioedema
Allergic angioedema is often the result of an allergic reaction.
This is where the body mistakes a harmless substance, such as a certain food, for something dangerous. It releases chemicals into the body to attack the substance, which cause the skin to swell.
Angioedema can be triggered by an allergic reaction to:
- certain types of food – particularly nuts, shellfish, milk and eggs
- some types of medication – including some antibiotics, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- insect bites and stings – particularly wasp and bee stings
- latex – a type of rubber used to make medical gloves, balloons and condoms
Drug-induced angioedema
Some medicines can cause angioedema – even if you’re not allergic to the medication.
The swelling may occur soon after you start taking a new medication, or possibly months or even years later.
Medications that can cause angioedema include:
- angiotensin-converting enzyme (ACE) inhibitors, such as enalapril, lisinopril, perindopril and ramipril, which are used to treat high blood pressure
- ibuprofen and other types of NSAID painkillers
- angiotensin-2 receptor blockers (ARBs), such as andesartan, irbesartan, losartan, valsartan and olmesartan – another medication used to treat high blood pressure
Hereditary angioedema
Rarely, angioedema occurs because of a genetic fault that you inherit from your parents. If you have hereditary angioedema, you have a 50% chance of passing it on to your children.
The fault affects the gene responsible for the production of a substance called C1 esterase inhibitor. If you don’t have enough of this, the immune system can occasionally “misfire” and cause angioedema.
Symptoms of hereditary angioedema typically begin in childhood and worsen during puberty. On average, untreated individuals have an attack every 1 to 2 weeks, and most episodes last for about 3 to 4 days. The frequency and duration of attacks vary greatly among people with hereditary angioedema, even among people in the same family.
There are three types of hereditary angioedema, called types I, II, and III, which can be distinguished by their underlying causes and levels of a protein called C1 inhibitor in the blood 21. The different types have similar signs and symptoms. Type III was originally thought to occur only in women, but families with affected males have been identified.
Hereditary angioedema is estimated to affect 1 in 50,000 people. Type I is the most common, accounting for 85 percent of cases. Type II occurs in 15 percent of cases, and type III is very rare 21.
Hereditary angioedema causes
Mutations in the SERPING1 gene cause hereditary angioedema type I and type II. The SERPING1 gene provides instructions for making the C1 inhibitor protein, which is important for controlling inflammation. C1 inhibitor blocks the activity of certain proteins that promote inflammation. Mutations that cause hereditary angioedema type I lead to reduced levels of C1 inhibitor in the blood, while mutations that cause type II result in the production of a C1 inhibitor that functions abnormally. Without the proper levels of functional C1 inhibitor, excessive amounts of a protein fragment (peptide) called bradykinin are generated. Bradykinin promotes inflammation by increasing the leakage of fluid through the walls of blood vessels into body tissues. Excessive accumulation of fluids in body tissues causes the episodes of swelling seen in individuals with hereditary angioedema type I and type II.
Mutations in the F12 gene are associated with some cases of hereditary angioedema type III. This gene provides instructions for making a protein called coagulation factor XII. In addition to playing a critical role in blood clotting (coagulation), factor XII is also an important stimulator of inflammation and is involved in the production of bradykinin. Certain mutations in the F12 gene result in the production of factor XII with increased activity. As a result, more bradykinin is generated and blood vessel walls become more leaky, which leads to episodes of swelling in people with hereditary angioedema type III.
The cause of other cases of hereditary angioedema type III remains unknown. Mutations in one or more as-yet unidentified genes may be responsible for the disorder in these cases.
Inheritance Pattern
This condition is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
In some cases, an affected person inherits the mutation from one affected parent. Other cases result from new mutations in the gene and occur in people with no history of the disorder in their family.
Hereditary angioedema symptoms
The swelling may happen randomly, or it may be triggered by:
- an injury or infection
- surgery and dental treatment
- stress
- pregnancy
- certain medications, such as the contraceptive pill
How often the swelling occurs can vary. Some people experience it every week, while in others it may occur less than once a year.
Idiopathic angioedema
Angioedema without a clear cause is known as idiopathic angioedema.
One theory is that an unknown problem with the immune system might cause it to occasionally misfire.
Certain triggers may lead to swelling, such as:
- anxiety or stress
- minor infections
- hot or cold temperatures
- strenuous exercise
In very rare cases, the swelling may be associated with other medical conditions, such as lupus or lymphoma (cancer of the lymphatic system).
Angioedema diagnosis
If you have experienced angioedema for the first time, your doctor will try to work out what may have caused it.
There are several different causes of angioedema. It’s important to know what’s causing your symptoms, as this affects the treatment you’ll need.
There’s no single test to determine the cause of angioedema. Some of the checks and tests you may have are outlined below.
A detailed medical history is invaluable in diagnosing angioedema.
- Keep a diary of exposure to possible irritants
- Tell your doctor about all medications you take, including over-the-counter (OTC) drugs and herbal remedies (even if taking them irregularly)
- Any family history of skin rash, allergies
Skin prick testing may be performed to try and identify any allergens. If hereditary angioedema is suspected, blood tests to check for levels and function of specific complement blood proteins may be done.
Allergy tests
If your doctor thinks your symptoms may have been caused by an allergy, they may refer you to a specialist allergy or immunology clinic for further testing.
Tests you may have include:
- a skin prick test – your skin is pricked with a tiny amount of the suspected allergen to see whether there’s a reaction
- a blood test – a sample of your blood is tested to determine whether your immune system reacts to a suspected allergen
Blood test
If your doctor thinks your symptoms may be caused by a genetic fault (hereditary angioedema) you’ve inherited from your parents, they may refer you for a blood test.
The test checks the level of a substance called C1 esterase inhibitor in your blood. This substance is important in regulating the immune system.
A very low level of C1 esterase inhibitor would suggest you have hereditary angioedema affecting how much of this substance your body is able to produce.
Angioedema treatment
The swelling will usually get better by itself in a few days, but there are treatments that can help it settle faster and reduce the risk of it happening again.
Treatment of angioedema depends on the severity of the condition. Angioedema can usually be treated at home, although severe cases may need to be treated in hospital. In cases where the respiratory tract is involved the first priority is to secure the airway. Patients may need emergency hospital care and require intubation (placement of a tube in the throat to keep the airway open).
Allergic and idiopathic angioedema
Allergic angioedema and idiopathic angioedema are usually treated in a similar way as acute urticaria.
In many cases the swelling is self-limiting and resolves spontaneously after a few hours or days. In more severe cases where there is persistent swelling, itchiness or pain the following medications may be used:
- Subcutaneous adrenaline (epinephrine)
- Oral or intravenous corticosteroids
- Oral or injected antihistamines
Antihistamines and steroid medication
Your doctor may suggest taking antihistamines to reduce swelling when it occurs.
Antihistamines work by blocking the effects of histamine, one of the chemicals responsible for the swelling. Some types can be bought in pharmacies and supermarkets without a prescription.
Some antihistamines can make you feel drowsy, so it’s best to take non-drowsy medications such as cetirizine and loratadine if your symptoms occur during the day.
Some antihistamines can make you feel drowsy. Avoid driving, drinking alcohol or operating dangerous machinery if you experience this.
Other side effects of antihistamines can include:
- headaches
- a dry mouth
- a dry nose
If the swelling is severe, your doctor may prescribe a short course of steroid medication. This is a powerful medication that’s only used for short periods because it can have troublesome side effects.
Adrenaline auto-injectors
If you have a particularly serious allergy, you may be given adrenaline auto-injectors to use if you experience a severe allergic reaction (anaphylaxis).
There are several types of auto-injector, which are used in slightly different ways.
Chronic angioedema with chronic autoimmune or chronic idiopathic urticaria
Chronic angioedema with chronic autoimmune or chronic idiopathic urticaria is often difficult to treat and response to medication variable. The following treatment steps are recommended. Each step is added to the previous one if inadequate response is obtained.
- Step 1: non-sedating antihistamines, eg, cetirizine
- Step 2: sedating antihistamines, e.g., diphenhydramine
- Step 3: a) oral corticosteroids, e.g., prednisone
- b) immunosuppressants eg, ciclosporin or methotrexate
Omalizumab, an anti-IgE monoclonal antibody, has been reported to be effective in some refractory cases of angioedema.
The goal of treatment for chronic angioedema is to reduce itch, swelling, tenderness and pain to a tolerable level to maintain function (e.g, at work, school, and during sleep).
Avoiding triggers
The best way to prevent an allergic reaction is to avoid the substance that you’re allergic to, may help reduce your chances of experiencing swelling, although this isn’t always easy or practical.
For example, if you’re allergic to a certain type of food, it can help to check the ingredients in food you buy and be careful when eating out.
Below is some practical advice that should help you avoid the most common allergens.
Food allergies
By law, food manufacturers must clearly label any foods that contain something that’s known to cause allergic reactions in some people. By carefully checking the label for the list of ingredients, you should be able to avoid an allergic reaction.
People with food allergies most often experience an allergic reaction while eating out at a restaurant. You can avoid this by:
- not relying on the menu description alone (remember, many sauces or dressings could contain allergens)
- communicating clearly with the waiting staff and asking for their advice
- avoiding places where there’s a chance that different types of food could come into contact with each other, such as buffets or bakeries
- let restaurant staff you know your dietary requirements, including how severe your food allergy or intolerance is
- always check what allergens are in the dish even if you have eaten it before, as recipes and ingredients can change
Remember, simple dishes are less likely to contain “hidden” ingredients. If you’re not sure about a dish, don’t risk it
House dust mites
One of the biggest causes of allergies are dust mites, which are tiny insects found in household dust. You can limit the number of mites in your home by:
- choosing wood or hard vinyl floor coverings instead of a carpet
- fitting roller blinds that can be easily wiped clean
- choosing leather, plastic or vinyl furniture instead of upholstered furniture
- cleaning cushions, soft toys, curtains and upholstered furniture regularly, either by washing (at a high temperature) or vacuuming
- using tested allergy-proof covers on mattresses, duvets and pillows
- using a vacuum cleaner fitted with a HEPA (high efficiency particulate air) filter, because it can trap more dust mites than ordinary vacuum cleaners
- regularly wiping surfaces with a damp, clean cloth – avoid dry dusting, as this can spread dust into the air
Concentrate your efforts of controlling dust mites in the areas of your home where you spend the most time, such as the bedroom and living room.
Pets
It’s not the pet fur that causes an allergic reaction. Instead, it’s flakes of their dead skin, saliva and dried urine.
If you can’t permanently remove a pet from the house, you could try:
- keeping pets outside as much as possible, or limiting them to a particular area of the house, preferably an area without carpet
- not allowing pets in bedrooms
- washing pets at least once a week
- regularly grooming pets outside
- regularly washing all bedding and soft furnishings on which a pet has lain
- using an air filter in rooms where you spend most of your time
- increase ventilation with fans, air-conditioning or by opening windows
If you’re visiting a friend or relative with a pet, ask them not to dust or vacuum on the day you’re visiting, as this will stir up the allergens into the air. Taking an antihistamine medicine about an hour before entering a pet-inhabited house can also help reduce your symptoms.
Mould spores
Tiny particles released by molds can cause an allergic reaction in some people.
You can help prevent this by:
- keeping your home dry and well-ventilated
- removing any indoor pot plants from your home
- not drying clothes indoors, store clothes in damp cupboards or packing clothes too tightly in wardrobes
- dealing with any damp and condensation in your home
- avoiding damp buildings, damp woods and rotten leaves, cut grass and compost heaps
Hay fever
Pollen allergies – more commonly known as hay fever – are caused when trees and grasses release pollen into the air. Doctors often call hay fever allergic rhinitis.
Different plants pollinate at different times of the year, so the months that you get hay fever will depend on what sort of pollen(s) you are allergic to. Typically, people are affected during spring (trees) and summer (grasses).
To help keep your hay fever under control, you can:
- check weather reports for the pollen count and stay indoors when it’s high, if possible
- avoid drying clothes and bedding outside when the pollen count is high
- wear wraparound sunglasses to protect your eyes
- keep doors and windows shut when possible
- shower and change your clothes after being outside
- avoid grassy areas, such as parks and fields – particularly in the early morning, evening or night, when the pollen count is highest
- if you have a lawn, try asking someone else to cut the grass for you
- Insect bites and stings
If you’ve ever suffered a bad reaction to an insect bite or sting, it’s important to take precautions to minimize your risk.
When you’re outdoors, particularly in the summer, you could:
- cover exposed skin
- wear shoes
- apply insect repellent
- avoid wearing strong perfumes or fragrances, as these can attract insects
Preventing severe allergies (anaphylaxis)
If you’re at risk of experiencing a severe allergic reaction (anaphylaxis), make sure you carry two adrenaline auto-injectors with you everywhere.
Wearing a MedicAlert or Medi-Tag medallion or bracelet can make others aware of your allergy in an emergency.
Consider telling your teachers, work colleagues and friends, so they can give you your adrenaline injection in an emergency, while waiting for an ambulance.
There are three types of auto-injector – EpiPen, Jext and Emerade – that are each slightly different.
It’s important to remember the following:
- carry an auto-injector at all times (if you have two, carry them both) – there should be no exceptions; you may also be advised to get an emergency card or bracelet with full details of your allergy and doctor’s contact details to alert others
- extremes of heat can make adrenaline less effective – so don’t leave your auto-injector in the fridge or your car’s glove compartment, for example
check the expiry date regularly – an out-of-date injector will offer limited protection - manufacturers offer a reminder service, where you can be contacted near the expiry date – check the information leaflet that comes with your medicine for more information
- don’t delay injecting yourself if you think you may be experiencing anaphylaxis, even if your initial symptoms are mild – it’s better to use adrenaline early and then find out it was a false alarm than delay treatment until you’re sure you’re experiencing severe anaphylaxis
If your child has an auto-injector, they will need to change over to an adult dose once they reach 30kg (approximately 4.5 stone).
Hereditary angioedema treatment
Hereditary angioedema can’t be cured, but medications can help prevent and treat the swelling.
Preventing swelling
Medications called danazol and oxandrolone can help reduce the chances of swelling occurring if you have hereditary angioedema.
These medicines boost the levels of C1 esterase inhibitor in your blood. Low levels of this substance are what causes the swelling.
Side effects of these medications can include:
- weight gain
- in women, excessive body or facial hair growth, deepening of the voice, irregular periods or absent periods
- depression
- high blood pressure
- liver problems
A medication called tranexamic acid may sometimes be used as an alternative, particularly in children and women. This causes fewer side effects, but may not be as effective in preventing swelling.
Treating swelling
Acute episodes of hereditary angioedema do not respond to adrenaline, antihistamine and corticosteroids. Most acute episodes of Type I and II hereditary angioedema are non life-threatening.
Two main treatments can be used to treat swelling caused by hereditary angioedema:
- icatibant – a medication given by injection that blocks the effects of some of the chemicals responsible for the swelling
- C1 esterase inhibitor replacement – a treatment given by injection that boosts the levels of C1 esterase inhibitor in your blood
Occasionally, C1 esterase inhibitor replacement may also be used shortly before surgery or dental treatment, as it can reduce the risk of these triggering swelling.
You may be given a supply of medication to keep at home and be taught how to give the injections yourself.
- The mainstay of emergency medical treatment is intravenous C1 inhibitor concentrate (a blood product).
- If this is unavailable, fresh frozen plasma can be infused, but this occasionally exacerbates the angioedema.
- Icatibant, a synthetic peptidomimetic drug and bradykinin B2 receptor antagonist, can be used in emergencies for the symptomatic treatment of acute attacks of hereditary angioedema in adults with C1-esterase-inhibitor deficiency. It was approved by the FDA in 2011. In New Zealand, it is available for home use on Special Authority application.
- Ecallantide is a potent and selective human plasma kallikrein inhibitor that is also indicated for the symptomatic treatment of hereditary angioedema, approved for use by the FDA in 2009. It is a protease that is responsible for liberating bradykinin from its precursor kininogen. Ecallantide has been reported to cause anaphylaxis in 4% of cases and thus has a black box warning in the USA.
The chance of an attack can be reduced with the following medications:
- C1 inhibitor concentrate infused an hour before a surgical procedure
- Anabolic steroids (stanazolol, oxandrolone and danazol) to increase circulating levels of normal functional C1 inhibitor. These have ‘male-like’ hormonal activity, so may cause weight gain, menstrual irregularities and virilism.
- Tranexamic acid has been used in pre-pubertal children and may be effective in Type III hereditary angioedema.
Drug-induced angioedema
If a certain medication you’re taking is thought to be responsible for your angioedema, your doctor will usually advise stopping it.
They can prescribe a different medication for you to take instead.
This is usually all that needs to be done. Tell your doctor if your symptoms continue or come back after switching medication.
Swollen uvula treatment
The doctor may prescribe antibiotics for an infection. For an allergic reaction or angioedema, medicines called steroids or antihistamines may be given. Follow instructions when using any medicine. Empiric antibiotics directed against the most common infectious agents, Haemophilus and Streptococcus species were given with rapid improvement in symptoms over the next 24 hours 1.
Home care
To care for the condition at home:
- Gargle with warm salt water once an hour to help reduce swelling and relieve pain. Use 1 teaspoon of salt mixed in 1 cup of warm water.
- Try an over-the-counter throat spray to relieve throat pain.
- If medicines were prescribed, be sure they are taken as directed. They should be taken until they are gone or the healthcare provider says to stop them.
- If you were told that your angioedema was from a medicine that you are taking, you must stop taking this medicine. Contact your doctor for a prescription for a different medicine. Advise future medical providers that you are allergic to this medicine.
- Contact your healthcare provider before taking any over-the-counter medicines.
- Drink fluids. Pain when swallowing may make it harder to drink and lead to dehydration. To prevent this, sip fluids throughout the day. Children can be given frozen juice bars, milk, or other cold liquids. Watch for the signs of dehydration listed below.
- Drink plenty of fluids. Fluids may help soothe your throat. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
- Do not smoke or allow others to smoke around you. Smoking can make your throat problem worse. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Lathadevi HT, Karadi RN, Thobbi RV, Guggarigoudar SP, Kulkarni NH. Isolated uvulitis: An uncommon but not a rare clinical entity. Indian J Otolaryngol Head Neck Surg. 2005;57(2):139-40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3450958/pdf/12070_2008_Article_BF02907669.pdf[↩][↩][↩]
- Rapkin RH. Simultaneous uvulitis and epiglottitis, JAMI 1980;43:1843.[↩][↩]
- Gorjinkel HJ, Everett ED. Haemophilus influenzae infections in adults, Report of nine cases and a review of the literature, Medicine 1979;58:80-94.[↩][↩]
- Deweere DP, Saunders WH. Textbook of Otolaryngology, 6th Ed., St. Louis: CV Mosby; 1982. p. 53.[↩]
- Hirschmann KL, Wald ER. Uvulitis in children. Paediatr Infect Des 1983:2:392-3.[↩]
- Cohen M, Chhetri DK, Head C. Isolated uvulitis. ENT J. 2007;86(8):462–464.[↩]
- Ziahosseini K, Ali S, Simo R, Malhotra R. Uvulitis following general anaesthesia. BMJ Case Rep. 2014;2014:bcr2014205038. Published 2014 Sep 23. doi:10.1136/bcr-2014-205038 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4173138/[↩]
- Karl L. Li MD, Sharon, et al. Isolated uvulitis due to Haemophilus influenza type b, Paediatrics 1984;74:1054-7.[↩][↩]
- Ozanne, A, Marsot-Dupuch, K, Ducreux, D, Meyer, B, Lasjaunias, P Acute epiglottitis: MRI.. Neuroradiology. (2004). 46 153–5 https://www.ncbi.nlm.nih.gov/pubmed/14726983[↩]
- Huopio, M, Kokkonen, J, Heino, S, Valtonen, M, Hakala, T [Epiglottitis and necrotizing mediastinitis in a middle-aged man].. Duodecim. (2014). 130 503–6 https://www.ncbi.nlm.nih.gov/pubmed/24730202[↩]
- Guardiani E, Bliss M, Harley E. Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: Evolving principles in diagnosis and management. Laryngoscope. 2010;120:2183–8 https://www.ncbi.nlm.nih.gov/pubmed/20925091[↩]
- Chan KO, Pang YT, Tan KK. Acute epiglottitis in the tropics: Is it an adult disease? J Laryngol Otol. 2001;115:715–8. https://www.ncbi.nlm.nih.gov/pubmed/11564297[↩]
- Mayo-Smith, MF, Spinale, JW, Donskey, CJ, Yukawa, M, Li, RH, Schiffman, FJ Acute epiglottitis. An 18-year experience in Rhode Island.. Chest. (1995). 108 1640–7 http://journal.chestnet.org/article/S0012-3692(15)45122-0/fulltext[↩]
- Guardiani, E, Bliss, M, Harley, E Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: Evolving principles in diagnosis and management.. Laryngoscope. (2010). 120 2183–8 https://www.ncbi.nlm.nih.gov/pubmed/20925091[↩]
- Al-Qudah, M, Shetty, S, Alomari, M, Alqdah, M Acute adult supraglottitis: Current management and treatment.. South Med J. (2010). 103 800–4 https://www.ncbi.nlm.nih.gov/pubmed/20622745[↩]
- Hung TY, Li S, Chen PS, Wu LT, Yang YJ, Tseng LM, et al. Bedside ultrasonography as a safe and effective tool to diagnose acute epiglottitis. Am J Emerg Med. 2011;29:359.e1–3. Epub 2010 Aug 1. https://www.ncbi.nlm.nih.gov/pubmed/20674236[↩]
- Grover C. Images in clinical medicine. “Thumb sign” of epiglottitis. N. Engl. J. Med. 2011;365 (5): 447. doi:10.1056/NEJMicm1009990 http://www.nejm.org/doi/full/10.1056/NEJMicm1009990[↩]
- Abdallah C. Acute epiglottitis: Trends, diagnosis and management. Saudi Journal of Anaesthesia. 2012;6(3):279-281. doi:10.4103/1658-354X.101222. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498669/[↩][↩]
- Shah RK, Roberson DW, Jones DT. Epiglottitis in the Hemophilus influenzae type B vaccine era: Changing trends. Laryngoscope. 2004;114:557–60 https://www.ncbi.nlm.nih.gov/pubmed/15091234[↩]
- Guardiani E, Bliss M, Harley E. Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: Evolving principles in diagnosis and management. Laryngoscope. 2010;120:2183–8. https://www.ncbi.nlm.nih.gov/pubmed/20925091[↩]
- Hereditary angioedema. https://ghr.nlm.nih.gov/condition/hereditary-angioedema[↩][↩]