Contents
What is tarsal tunnel syndrome
Tarsal tunnel syndrome is a compression or squeezing on the posterior tibial nerve in the tarsal tunnel that produces symptoms anywhere along the path of the nerve running from the inside of the ankle into the foot. The posterior tibial nerve is the nerve in the ankle and foot and it provides sensation to the bottom of the foot. Tarsal tunnel syndrome can lead to numbness, tingling, weakness, or muscle damage mainly in the bottom of the foot.
When the tibial nerve is compressed inside the tarsal tunnel, the resulting condition is called tarsal tunnel syndrome. Tarsal tunnel syndrome has also been called posterior tibial neuralgia.
Tarsal tunnel syndrome is similar to carpal tunnel syndrome, which occurs in the wrist. Both disorders arise from the compression of a nerve in a confined space.
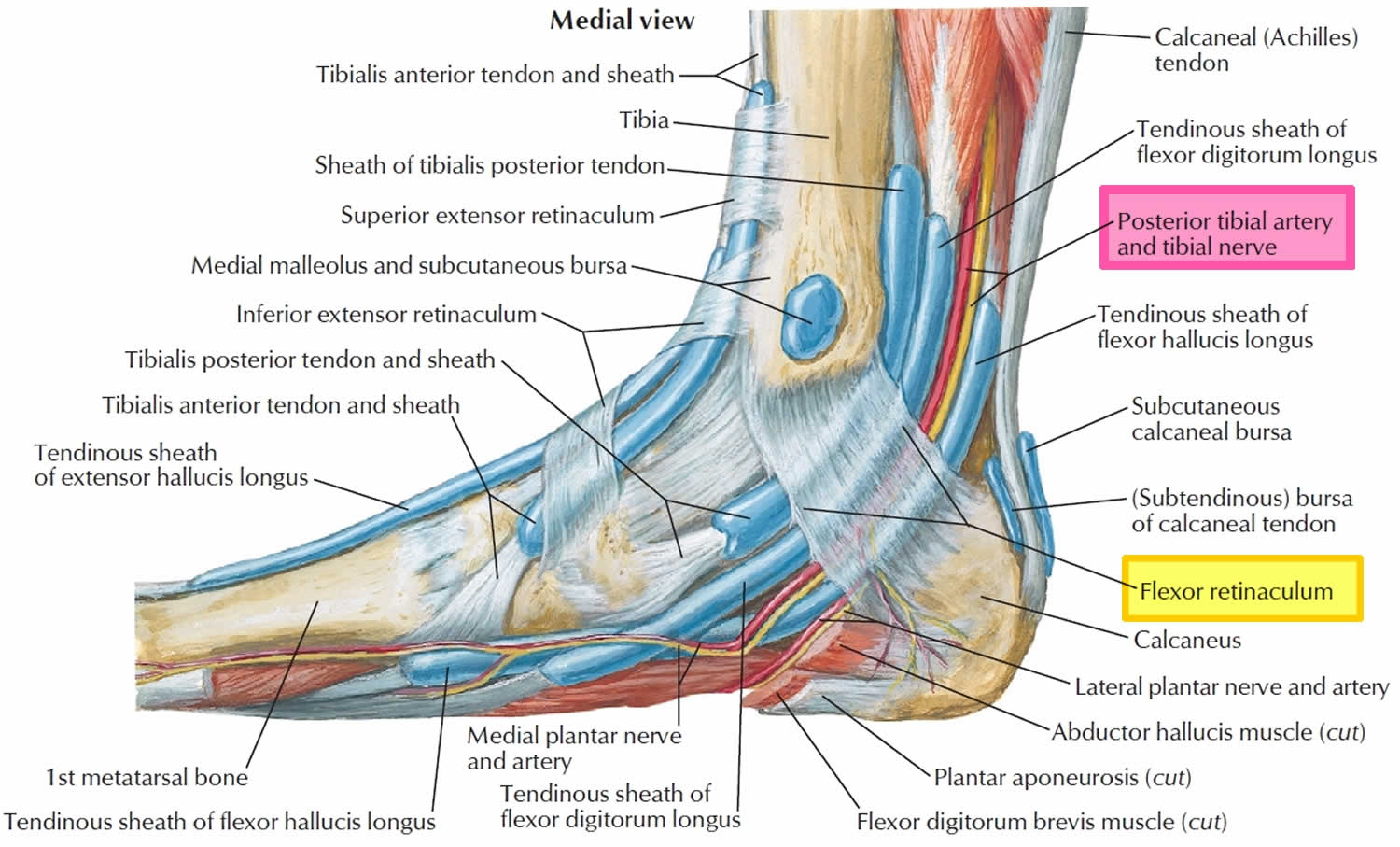
The tarsal tunnel is a narrow fibro-osseous tunnel, formed between the medial malleolus (part of the ankle bone, this is the bump on the inside of the ankle) and the flexor retinaculum (a band of ligaments that stretches across the foot), that lies on the inside of the ankle next to the ankle bones. The tunnel is covered with a thick ligament (the flexor retinaculum) that protects and maintains the structures contained within the tunnel—arteries, veins, tendons and nerves. One of these structures is the posterior tibial nerve, which is the focus of tarsal tunnel syndrome.
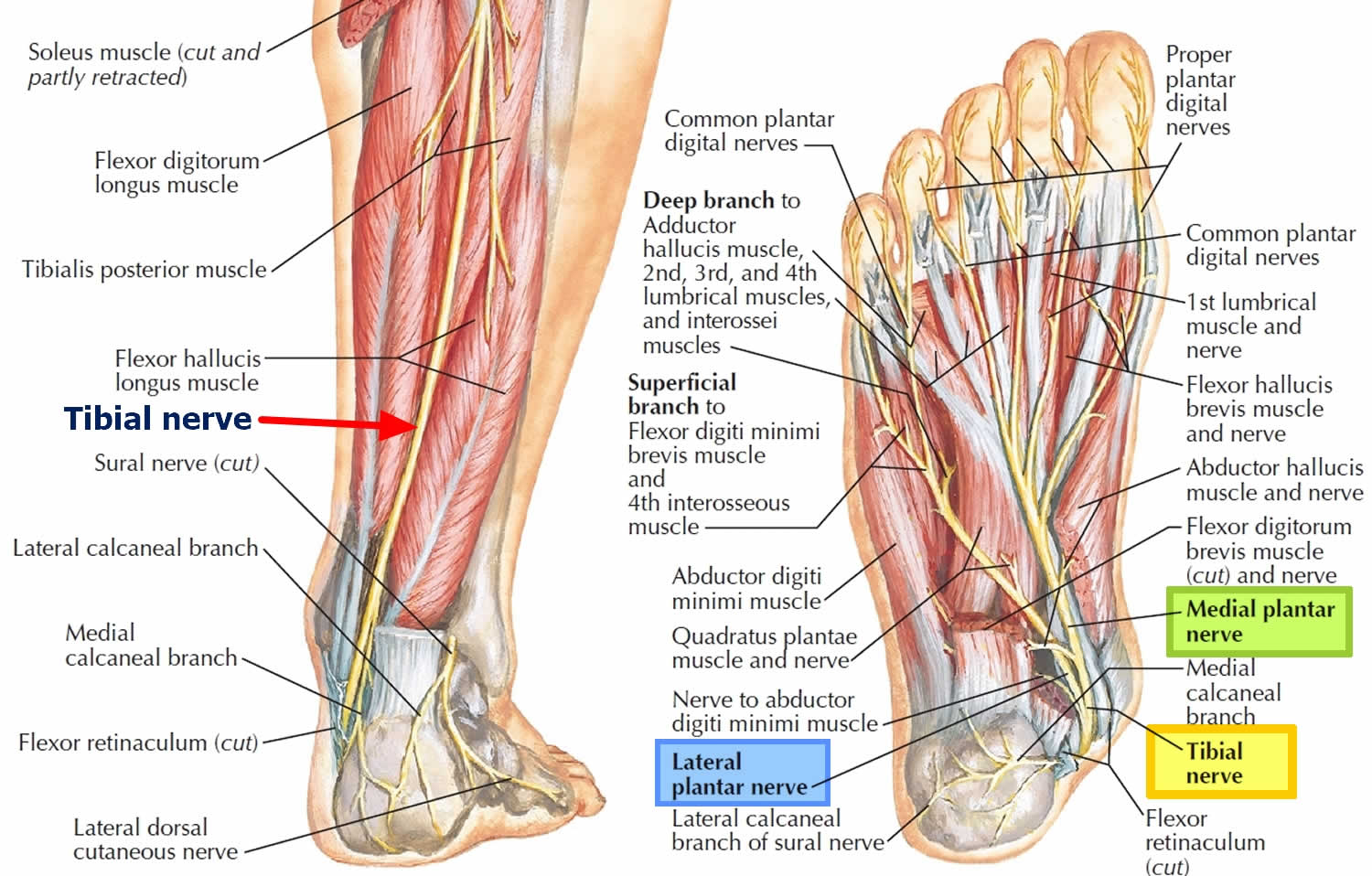
The tarsal tunnel is a fibro-osseous tunnel through which the distal posterior tibial nerve and its branches (the calcaneal nerve and the medial and lateral plantar nerves) pass as they curve around the medial malleolus into the foot 1. Entrapment of these nerves at this point results in the tarsal tunnel syndrome. The symptoms may vary according to the nerves affected 2: the calcaneal nerves are purely sensory and supply the heel; the medial plantar nerve innervates the medial aspect of the sole and the medial 3 or 4 toes and their associated muscles; and the lateral plantar nerve supplies the remainder of the skin on the plantar aspect of the sole and toes, and the small muscles that control the lateral toes (see Figure 2). The muscles responsible for ankle movements are unaffected.
Tarsal tunnel syndrome may be treated conservatively with physical therapy to strengthen the muscles, custom orthotics and ultrasound guided cortisone injections. In severe cases, surgical intervention is required. In such cases the surgeon would decompress the nerve and relieve it of any impingements that may cause compression.
Tarsal tunnel syndrome complications
Untreated, tarsal tunnel syndrome may lead to the following:
- Deformity of the foot (mild to severe)
- Movement loss in the toes (partial or complete)
- Repeated or unnoticed injury to the leg
- Sensation loss in the toes or foot (partial or complete)
Figure 1. Tarsal tunnel anatomy
Figure 2. Tibial nerve (posterior tibial nerve and branches)
What is anterior tarsal tunnel syndrome?
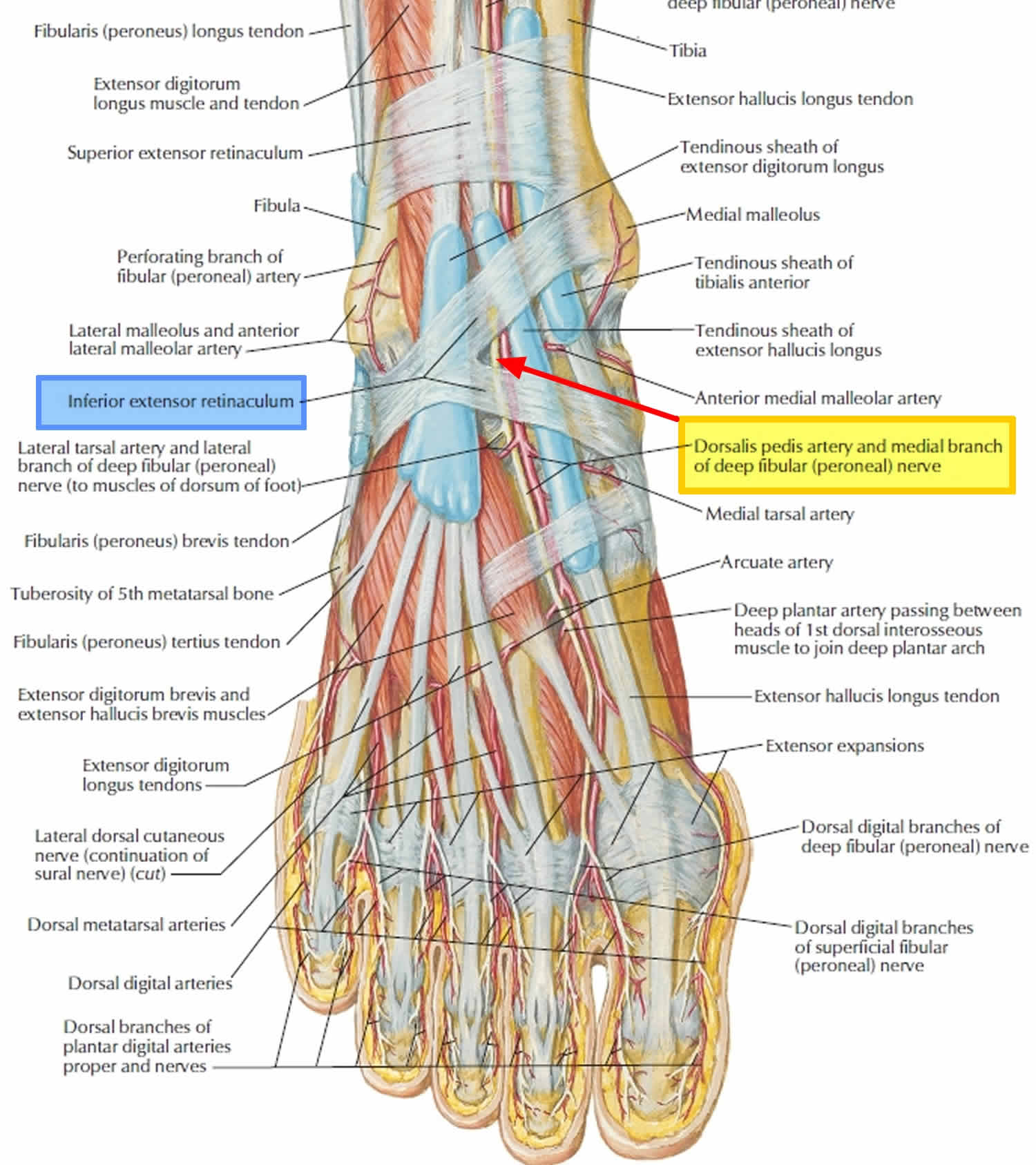
The anterior tarsal tunnel syndrome denotes the entrapment of the deep peroneal nerve under the inferior extensor retinaculum 3. The little space in the tunnel formed by the inferior extensor retinaculum and the close proximity of the structures make the nerve vulnerable to compressive neuropathy. In an already small space, any addition to the structure can cause pressure over the nearby structures. The usual complaints are dysesthesias (abnormal unpleasant sensation felt when touched) in the first web space and opposing sides of the adjacent toes with or without proximally radiating dysesthesias. Clinical findings are decreased touch and pinprick in the first web space. Tinel’s sign over the deep peroneal nerve beneath the inferior extensor retinaculum may be present and extensor digitorum brevis muscle may be atrophic. Anterior tarsal tunnel syndrome is mostly seen in runners 3. Anterior tarsal tunnel syndrome cause as described in literature can be due to tight shoes, high heeled shoes or ski boots, ganglion cyst, lipomas, dorsal osteophytes at the ankle, midtarsal or metatarsocuneiform articulation. In ballet dancers, stretching of the deep peroneal nerve due to extreme planter flexion was described by Borges 4. Cetinkal et al. 5 reported such a case in a missed talar fracture.
Figure 3. Anterior tarsal tunnel syndrome
How long does tarsal tunnel syndrome last?
A full recovery is possible if the cause of tarsal tunnel syndrome is found and successfully treated. Some people may have a partial or complete loss of movement or sensation. Nerve pain may be uncomfortable and last for a long time.
Properly performed decompression may yield satisfactory results. An initial marked decrease in pain and paresthesias may occur, followed by a reduction of symptoms to the extent that the patient may be able to tolerate the symptoms. Complete resolution of symptoms may not be possible because the disorder has numerous etiologies and because the likelihood of irreversible nerve damage exists. An increase in pain after decompression, however, is extremely rare.
Studies by Mann 6 demonstrated that approximately 75% of patients who undergo surgical decompression have appreciable pain relief, and 25% obtain little or no relief. Mann 6 also stated that a repeat surgical exploration of a previous tarsal canal release rarely causes appreciable benefit to the patient.
Gondring et al 7 did a prospective evaluation of 46 consecutive patients (56 feet) who underwent nonoperative and surgical treatment for tarsal tunnel syndrome and documented pain intensity before and after treatment with the Wong-Baker FACES Pain Rating Scale applied to the anatomic nerve regions of the plantar aspect of the foot.
In this study 7, patients who had successful nonoperative treatment experienced significantly reduced overall pain intensity in the medial calcaneal, medial plantar, and lateral plantar nerve regions. In patients who had ongoing symptoms despite nonoperative treatment, surgical treatment significantly reduced pain in the medial calcaneal and medial plantar nerve regions but not in the lateral plantar nerve area. Pretreatment motor nerve conduction latency was significantly greater in surgically treated patients than in those who had only nonoperative treatment. The authors concluded that anatomic pain intensity rating models may be useful in pretreatment and follow-up evaluation of tarsal tunnel syndrome.
Antoniadas et al 8 performed a literature review of posterior tarsal tunnel syndrome and found that accurate diagnosis required proper clinical, neurologic, and neurophysiologic examinations. Success rates of 44-91% were attained with operative treatment. The results were found to be better in idiopathic cases than in posttraumatic cases, and if surgery failed, reoperation was indicated only in patients with inadequate release.
McSweeney et al 9 conducted a rigorous review of tarsal tunnel syndrome that included the Cochrane Neuromuscular Group’s Specialized Register (Cochrane Library 2013), as well as EMBASE, AMED, MEDLINE, CINAHL, Physiotherapy Evidence Database (PEDro), Biomed Central, Science Direct, and Trip Database (1972-2015). They found that there was limited high-level robust evidence to guide and refine the clinical management of tarsal tunnel syndrome. Requirements for small-scaled randomized controlled trials in groups with homogenous etiology are needed to analyze the effectiveness of specific treatment modalities.
Tarsal tunnel syndrome causes
Tarsal tunnel syndrome may be caused by an injury, disease, or due to the natural shaping of the foot. Possible causes may include:
- Having flat feet or fallen arches, which can produce strain or compression on the tibial nerve. A person with flat feet is at risk for developing tarsal tunnel syndrome, because the outward tilting of the heel that occurs with fallen arches can produce strain and compression on the nerve.
- An injury, such as an ankle sprain, may produce inflammation and swelling in or near the tunnel, resulting in compression of the nerve.
- Diseases such as arthritis or diabetes which can cause swelling, thus resulting in nerve compression
- An enlarged or abnormal structure that occupies space within the tunnel can compress the nerve, such as a varicose vein, ganglion cyst, swollen tendon, or arthritic bone spur, that might compress the nerve
- Systemic diseases, such as diabetes or arthritis, can cause swelling, thus compressing the nerve.
Tarsal tunnel syndrome symptoms
Patients with tarsal tunnel syndrome experience one or more of the following symptoms:
- Shooting pain in the foot
- Numbness
- Tingling or burning sensation
- Pain and tingling around the ankle
- Swelling in the foot
- Pain radiating up into the leg or down into the ankle and foot
- Pins and needles feeling in the foot
Symptoms are typically felt on the inside of the ankle and/or on the bottom of the foot. In some people, a symptom may be isolated and occur in just one spot. In others, it may extend to the heel, arch, toes and even the calf.
Sometimes the symptoms of the syndrome appear suddenly. They are often brought on or aggravated by overuse of the foot, such as in prolonged standing, walking, exercising or beginning a new exercise program.
It is important to seek early treatment if any of the symptoms of tarsal tunnel syndrome occur. If left untreated, the condition progresses and may result in permanent nerve damage. In addition, because the symptoms of tarsal tunnel syndrome can be confused with other conditions, proper evaluation is essential so that a correct diagnosis can be made and appropriate treatment initiated.
Tarsal tunnel syndrome diagnosis
Proper diagnosis of a tarsal tunnel syndrome requires the expert attention of experienced foot and ankle surgeon.
During your medical examination, the surgeon will position your foot and tap on the nerve to see if the symptoms can be reproduced. He or she will also press on the area to help determine if a small mass is present.
Advanced imaging studies may be ordered if a mass is suspected or if initial treatment does not reduce the symptoms. Studies used to evaluate nerve problems—electromyography and nerve conduction velocity (EMG/nerve conduction study)—may be ordered if the condition shows no improvement with nonsurgical treatment.
Tarsal tunnel syndrome test will include:
- Electrical testing (EMG or nerve conduction study)
- Imaging (X-rays, CT, or MRI scans)
Diagnosis is necessary to determine the severity of the condition, so the appropriate treatment plan, including a surgical option, can be considered.
Tarsal tunnel syndrome treatment
Nonsurgical treatment for tarsal tunnel syndrome
Whenever possible, doctors will prescribe nonsurgical treatment options before surgery is recommended. Possible treatment options may include anti-inflammatory medications or steroid injections into the nerves in the tarsal tunnel to relieve pressure and swelling. Orthosis (e.g., braces, splints, orthotic devices) may be recommended to reduce pressure on the foot and limit movement that could cause compression on the nerve.
Many treatment options, often used in combination, are available to treat tarsal tunnel syndrome. These include:
- Rest. Staying off the foot prevents further injury and encourages healing.
- Ice. Apply an ice pack to the affected area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Immobilization. Restricting movement of the foot by wearing a cast is sometimes necessary to enable the nerve and surrounding tissue to heal.
- Physical therapy. Ultrasound therapy, exercises and other physical therapy modalities may be prescribed to reduce symptoms.
- Injection therapy. Injections of a local anesthetic provide pain relief, and an injected corticosteroid may be useful in treating the inflammation.
- Orthotic devices. Custom shoe inserts may be prescribed to help maintain the arch and limit excessive motion that can cause compression of the nerve.
- Shoes. Supportive shoes may be recommended.
- Bracing. Patients with flatfoot or those with severe symptoms and nerve damage may be fitted with a brace to reduce the amount of pressure on the foot.
Tarsal tunnel syndrome surgery
The foot and ankle surgeon will determine if surgery is necessary and will select the appropriate procedure or procedures based on the cause of the condition. Depending on the severity of the condition, one of several surgical options may be recommended, including tarsal tunnel release.
Complications are associated with tarsal tunnel decompression surgery may include nerve or artery laceration and plantar fasciitis 10. One small study reviewed the results of 30 patients who underwent decompression surgery for tarsal tunnel syndrome and reported a 13 percent complication rate 11. In this study, three individuals had wound infections and one person had a delay in wound healing.
- These boots weren’t made for walking: tarsal tunnel syndrome. CMAJ May 2007, 176 (10) 1415-1416; DOI: 10.1503/cmaj.061062[↩]
- Nagaoka M, Satou K. Tarsal tunnel syndrome caused by ganglia. J Bone Joint Surg Br 1999;81:607-10.[↩]
- Gani N, Khan HA, Kamal Y, Farooq M, Jeelani H, Shah AB. Anterior Tarsal Tunnel Syndrome With Thrombosed Dorsalis Pedis Artery: A Case Report. Archives of Trauma Research. 2015;4(1):e21738. doi:10.5812/atr.21738. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4460259/[↩][↩]
- The anterior tarsal tunnel syndrome. Report of two cases. Borges LF, Hallett M, Selkoe DJ, Welch K. J Neurosurg. 1981 Jan; 54(1):89-92. https://www.ncbi.nlm.nih.gov/pubmed/7463126/[↩]
- Anterior tarsal tunnel syndrome secondary to missed talus fracture: a case report. Cetinkal A, Topuz K, Kaya S, Colak A, Demircan MN. Turk Neurosurg. 2011; 21(2):259-63.[↩]
- Mann RA, DuVries HL, Inman VT, eds. Surgery of the Foot. 5th ed. St Louis, Mo: Mosby-Year Book; 1986. 205-7.[↩][↩]
- Gondring WH, Trepman E, Shields B. Tarsal tunnel syndrome: assessment of treatment outcome with an anatomic pain intensity scale. Foot Ankle Surg. 2009. 15(3):133-8.[↩][↩]
- Antoniadis G, Scheglmann K. Posterior tarsal tunnel syndrome: diagnosis and treatment. Dtsch Arztebl Int. 2008 Nov. 105(45):776-81.[↩]
- McSweeney SC, Cichero M. Tarsal tunnel syndrome-A narrative literature review. Foot (Edinb). 2015 Dec. 25 (4):244-50.[↩]
- Tarsal Tunnel Syndrome. https://emedicine.medscape.com/article/1236852-overview[↩]
- Pfeiffer WH, Cracchiolo A 3rd. Clinical results after tarsal tunnel decompression. J Bone Joint Surg Am. 1994;76:1222-1230[↩]