Contents
What is telogen effluvium
Telogen effluvium is the name for temporary hair loss on all parts of your body, but, generally, only loss of scalp hair is symptomatic due to shedding of resting or telogen hair after some shock to your system. New hair continues to grow. Telogen hair has a bulb or club-shaped tip. Telogen effluvium should be distinguished from anagen effluvium, in which the hair shedding is due to interruption of active or anagen hair growth by drugs, toxins or inflammation (e.g. alopecia areata).
It is normal to shed approximately 30-150 hairs from your scalp daily as part of our hair cycle, but this can vary depending on washing and brushing routines. Hair regrows automatically so that the total number of hairs on your head remains constant. Telogen effluvium occurs when there is a marked increase in hairs shed each day. An increased proportion of hairs shift from the growing phase (anagen) to the shedding phase (telogen). Anagen hair has a pointed or tapered tip. Normally only 10% of your scalp hair is in the telogen phase, but in telogen effluvium this increases to 30% or more. This usually happens suddenly and can occur approximately 3 months after a trigger.
In most people, 5-15% of the hair on the scalp is in telogen at any given time. Telogen effluvium is triggered when a physiologic stress or hormonal change causes a large number of hairs to enter telogen at one time. Shedding does not occur until the new anagen hairs begin to grow. The emerging hairs help to force the resting hairs out of the follicle. Evidence suggests that the mechanism of shedding of a telogen hair is an active process that may occur independent of the emerging anagen hair. The interval between the inciting event in telogen effluvium and the onset of shedding corresponds to the length of the telogen phase, between 1 and 6 months (average 3 months).
Common triggers of telogen effluvium include childbirth, severe trauma or illness, a stressful or major life event (such as losing a loved one), marked weight loss and extreme dieting, a severe skin problem affecting the scalp, a new medication or withdrawal of a hormone treatment. No cause is found in around a third of people diagnosed with telogen effluvium.
Hair shedding in telogen effluvium is usually from all over the scalp. Hair thickness decreases in the early stages resulting in thinness of hair volume.
Telogen effluvium is a form of nonscarring alopecia (hair loss) characterized by diffuse hair shedding, often with an acute onset 1. A chronic telogen effluvium with a more insidious onset and a longer duration also exists 2. Telogen effluvium is a reactive process caused by a metabolic or hormonal stress or by medications. Generally, recovery is spontaneous and occurs within 6 months, unless a background of pattern alopecia is present 3.
Telogen effluvium treatment tips
Telogen effluvium is self-correcting. It is really not influenced by any treatment that can be given. However, gentle handling of the hair, avoiding over-vigorous combing, brushing and any type of scalp massage are important.
You should also ensure a nutritious diet, with plenty of protein, fruit and vegetables.
The doctor may check your thyroid function, and levels of iron, vitamin B12 and folic acid, as any deficiency in these can slow hair growth.
You should also consider stopping smoking as heavy metals in cigarette smoke may worsen your hair loss.
What if the scalp starts to become visible because of thinning of the hair?
This can happen in severe cases of telogen effluvium, but various options for helping disguise the hair loss can be discussed with your doctor. It is very unusual for hair thinning in patients with telogen effluvium to be severe enough to require the use of a wig.
Hair Growth Cycle
Hair follicles extend deep into the dermis, often projecting into the underlying subcutaneous layer. The epithelium at the follicle base surrounds a small hair papilla, a peg of connective tissue containing capillaries and nerves. The hair bulb consists of epithelial cells that surround the papilla.
Hair production involves a specialized keratinization process. The hair matrix is the epithelial layer involved in hair production. When the superficial basal cells divide, they produce daughter cells that are pushed toward the surface as part of the developing hair. Most hairs have an inner medulla and an outer cortex. The medulla contains relatively soft and flexible soft keratin. Matrix cells closer to the edge of the developing hair form the relatively hard cortex. The cortex contains
hard keratin, which gives hair its stiffness. A single layer of dead, keratinized cells at the outer surface of the hair overlap and form the cuticle that coats the hair.
The hair root anchors the hair into the skin. The root begins at the hair bulb and extends distally to the point where the internal organization of the hair is complete, about halfway to the skin surface. The hair shaft extends from this halfway point to the skin surface, where we see the exposed hair tip.
The size, shape, and color of the hair shaft are highly variable.
Growth and Replacement of Hair
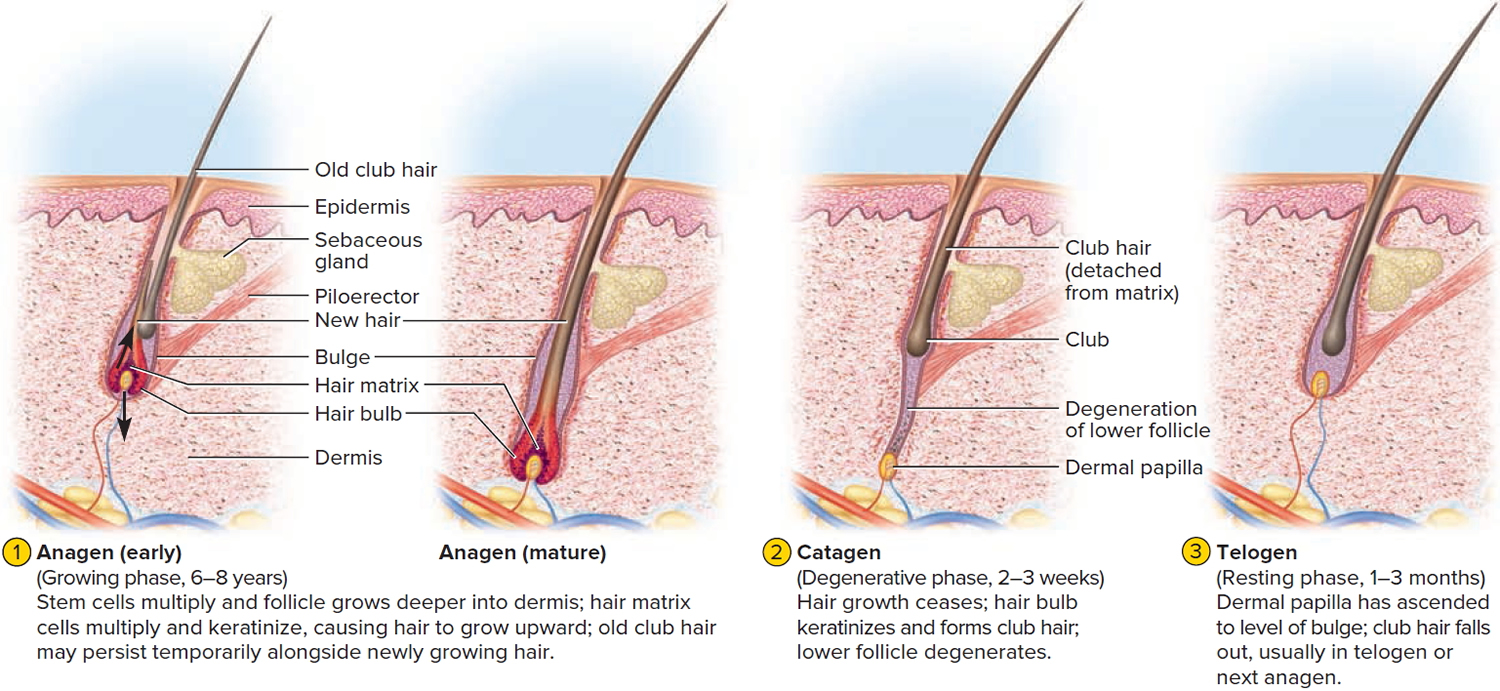
A hair in the scalp grows for two to five years, at a rate of around 0.33 mm/day (about 1/64 inch). Variations in hair growth rate and the duration of the hair growth cycle account for individual differences in uncut hair length. A given hair goes through a hair cycle consisting of three developmental stages (see Figure 1):
- Anagen.
- Catagen.
- Telogen.
At any given time, about 90% of the scalp follicles are in the anagen stage. In this stage, stem cells from the bulge in the follicle multiply and travel downward, pushing the dermal papilla deeper into the skin and forming the epithelial root sheath. Root sheath cells directly above the papilla form the hair matrix. Here, sheath cells transform into hair cells, which synthesize keratin and then die as they are pushed upward away from the papilla. The new hair grows up the follicle, often alongside an old club hair left from the previous cycle.
In the catagen stage, mitosis in the hair matrix ceases and sheath cells below the bulge die. The follicle shrinks and the dermal papilla draws up toward the bulge. The base of the hair keratinizes into a hard club and the hair, now known as a club hair, loses its anchorage. Club hairs are easily pulled out by brushing the hair, and the hard club can be felt at the hair’s end. When the papilla reaches the bulge, the hair goes into a resting period called the telogen stage. Eventually, anagen begins anew and the cycle repeats itself. A club hair may fall out during catagen or telogen, or as it is pushed out by the new hair in the next anagen phase.
You lose about 50 to 100 scalp hairs daily. In a young adult, scalp follicles typically spend 6 to 8 years in anagen, 2 to 3 weeks in catagen, and 1 to 3 months in telogen. Scalp hairs grow at a rate of about 1 mm per 3 days (10–18 cm/yr) in the anagen phase.
Hair grows fastest from adolescence until the 40s. After that, an increasing percentage of follicles are in the catagen and telogen phases rather than the growing anagen phase. Hair follicles also shrink and begin producing wispy vellus hairs instead of thicker terminal hairs. Thinning of the hair, or baldness, is called alopecia. It occurs to some degree in both sexes and may be worsened by disease, poor nutrition, fever, emotional stress, radiation, or chemotherapy. In the great majority of cases, however, it is simply a matter of aging.
Pattern baldness is the condition in which hair is lost unevenly across the scalp rather than thinning uniformly. It results from a combination of genetic and hormonal influences. The relevant gene has two alleles: one for uniform hair growth and a baldness allele for patchy hair growth. The baldness allele is dominant in males and is expressed only in the presence of the high level of testosterone characteristic of men. In men who are either heterozygous or homozygous for the baldness allele, testosterone causes terminal hair to be replaced by vellus hair, beginning on top of the head and later the sides. In women, the baldness allele is recessive. Homozygous dominant and heterozygous women show normal hair distribution; only homozygous recessive women are at risk of pattern baldness. Even then, they exhibit the trait only if their testosterone levels are abnormally high for a woman (for example, because of a tumor of the adrenal gland, a woman’s principal source of testosterone). Such characteristics in which an allele is dominant in one sex and recessive in the other are called sex-influenced traits.
Excessive or undesirable hairiness in areas that are not usually hairy, especially in women and children, is called hirsutism. It tends to run in families and usually results from either masculinizing ovarian tumors or hypersecretion of testosterone by the adrenal cortex. It is often associated with menopause.
Contrary to popular misconceptions, hair and nails do not continue to grow after a person dies, cutting hair does not make it grow faster or thicker, and emotional stress cannot make the hair turn white overnight.
Figure 1. Hair growth cycle
How long does telogen effluvium last?
Generally, telogen effluvium recovery is spontaneous and occurs within 6 months, unless a background of pattern alopecia is present 3.
Can telogen effluvium be cured?
Telogen effluvium usually resolves completely without any intervention as the normal length of telogen is approximately 100 days (3 to 6 months) after which period the hair starts growing again (anagen phase). However, depending on the length of the hair, it may take many months for the overall hair volume to gradually return to normal. Telogen effluvium can return, especially if the underlying cause is not treated or recurs, and would be called chronic telogen effluvium if lasting more than 6 months.
Chronic telogen effluvium
In some patients, hair shedding continues to be intermittently or continuously greater than normal for long periods of time, sometimes for years. The hair cycle appears to be reset so that the anagen period is shortened.
Chronic telogen effluvium often presents in women that actually continue to have quite thick and moderately long hair – this is because they notice the shed hair more than those with finer or shorter hair. Telogen effluvium does not cause complete baldness, although it may unmask a genetic tendency to genetic balding i.e. female pattern hair loss , or in men, male pattern hair loss.
Is telogen effluvium hereditary?
Telogen effluvium is not inherited, and it can affect all age groups and both genders equally.
Telogen effluvium causes
In a normal healthy person’s scalp about 85% of the hair follicles are actively growing hair (anagen hair) and 15% are resting hair (telogen hair). A hair follicle usually grows anagen hair for 4 years or so, then rests for about 4 months. The resting or telogen hair has a club or bulb at the tip. A new anagen hair begins to grow under the resting telogen hair and pushes it out.
Thus, it is normal to lose up to about 100 hairs a day on one’s comb, brush, in the basin or on the pillow, as a result of the normal scalp hair cycle.
If there is some shock to the system, as many as 70% of the anagen hairs can be precipitated into telogen, thus reversing the usual ratio. Typical precipitants include:
- Acute illness such as febrile illness, severe infection, major surgery, and severe trauma
- Chronic illness such as malignancy, particularly lymphoproliferative malignancy; and any chronic debilitating illness, such as systemic lupus erythematosus, end-stage renal disease, or liver disease
- Surgical operation
- Accident
- Hormonal changes such as pregnancy and delivery (can affect both mother and child), hypothyroidism, and discontinuation of estrogen-containing medications 4
- Childbirth
- Nervous shock
- Weight loss or unusual diet. Changes in diet like crash dieting, anorexia, low protein intake, and chronic iron deficiency 5: A study by Olsen et al. 6 sought to determine if iron deficiency played a role in female pattern hair loss. Results indicated that iron deficiency is common in women but is not significantly increased in patients with female patterns of hair loss or chronic telogen effluvium when compared with control subjects.
- Heavy metals such as selenium, arsenic, and thallium
- Medications, of which the most frequency cited are beta-blockers, anticoagulants, retinoids (including excess vitamin A), propylthiouracil (induces hypothyroidism), carbamazepine, and immunizations 7
- Allergic contact dermatitis of the scalp 8
- Psychological stress 5
- Discontinuing the contraceptive pill
- Overseas travel resulting in jetlag
- Excessive sun exposure
The resting scalp hairs, now in the form of club hairs, remain firmly attached to the hair follicles at first. It is only about 2 months after the shock that the new hairs coming up through the scalp push out the “dead” club hairs and increased hair fall is noticed.
Thus, paradoxically, with this type of hair loss, hair fall is a sign of hair regrowth. As the new hair first comes up through the scalp and pushes out the dead hair a fine fringe of new hair is often evident along the forehead hairline. At first the fall of club hairs is profuse and a general thinning of the scalp hair may become evident but after several months a peak is reached and hair fall begins to lessen, gradually tapering back to normal over 6-9 months. As the hair fall tapers off the scalp thickens back up to normal, but recovery may be incomplete in some cases.
Because nail and hair growth are under the same influences, an arrest in hair growth is often mirrored in the nails by a groove across them coinciding with the time of the shock to the system. This is called a Beau’s line. The time of the shock can be estimated from the fact that a finger nail takes 5 months to grow from the posterior nail fold to the free edge. So if the groove in the nail is half way down the nail then the shock must have been 2 1/2 months ago.
Telogen effluvium symptoms
Most people become aware of losing hair in increased amounts. This is most noticeable after washing or brushing with more hair being found in the plug hole or on the hair brush or comb. Some people will notice increased hair on the pillow in the morning or around the house. Usually there are no symptoms, but occasionally telogen effluvium can be accompanied by tenderness and altered sensations in the scalp known as trichodynia.
Acute telogen effluvium is defined as hair shedding lasting less than 6 months. Patients with acute telogen effluvium usually complain of relatively sudden onset of hair loss. Careful questioning usually reveals a metabolic or physiologic stress 1-6 months before the start of the hair shedding. Physiologic stresses that can induce telogen effluvium include febrile illness, major injury, change in diet, pregnancy and delivery, and starting a new medication. Immunizations also have been reported to cause acute hair shedding. Papulosquamous diseases of the scalp, such as psoriasis and seborrheic dermatitis, can produce telogen effluvium.
Chronic telogen effluvium is hair shedding lasting longer than 6 months. The onset is often insidious, and it can be difficult to identify an inciting event. Because of the duration of the hair shedding, patients are more likely to complain of decreased scalp hair density, or they may note that their hair appears thin and lifeless. Visual analog scales can help patients to assess the severity of hair shedding 9.
How is telogen effluvium diagnosed?
The diagnosis is usually based on appearance and the history of the hair shedding. The hair may be gently pulled to see if an increased quantity of hair is shed (although this test may be falsely negative if the hair has been washed within 48 hours beforehand) and occasionally hairs are plucked from the scalp so that they can be examined under the microscope. Very rarely a skin biopsy may be required.
If a biopsy is performed, some authors advocate taking three 4-mm punch biopsy specimens, all imbedded horizontally. This method provides a generous sample for determining anagen-to-telogen and terminal-to-vellus ratios and leads to greater diagnostic accuracy 10.
Chronic telogen effluvium may have a metabolic cause. Testing should be directed toward causes that are common and correctable. If any sign or symptom of hypothyroidism is present, a thyrotropin test is warranted. Iron deficiency is common in premenopausal women. Evaluation of complete blood count (CBC) count, serum iron, iron saturation, and ferritin may be warranted. Note that CBC count results may be completely normal in women with mild iron deficiency and hair loss, particularly in women older than 40 years. Blood is more essential than hair, and the body will shed hair before red cell indices become microcytic. Also, note that ferritin behaves as an acute phase reactant. Inflammation can produce normal ferritin levels in an individual who is iron deficient. Although a low ferritin is proof of iron deficiency, a normal ferritin level does not exclude iron deficiency. Some experts in the field regard iron saturation as the most sensitive indicator of iron deficiency.
Occasionally, screening for renal and hepatic enzymes may detect a systemic cause of hair shedding. If syphilis is considered as a cause of hair loss, a rapid plasma reagin or Venereal Disease Research Laboratory test should be preformed.
Other tests
If a patient is unwilling to undergo a scalp biopsy but would like confirmation of the diagnosis, serial hair collections may be obtained. This process can educate the patient in the normal hair cycle and can confirm the spontaneous resolution of the process.
The patient should be instructed to collect all hairs shed in a 24-hour period. The patient should not shampoo the hair during the day of collection. This process should be repeated every week or every other week, for a total of 3 or 4 collections.
Collections totaling 100 hairs or more in a given 24-hour period are indicative of ongoing telogen effluvium. If the collections are performed over several weeks while the telogen effluvium is resolving, the number of hairs collected each time should decrease. This finding can be very comforting to the patient.
An alternate method of hair collection has been proposed by Rebora et al. 11. According to this method, the patient collects hair during shampooing and the physician both counts and measures the length of these hairs. This method has the advantage of being able to detect and differentiate between telogen effluvium and androgenetic alopecia, even when the 2 conditions occur in the same individual. The disadvantage to this method is that it cannot be used in patients who have short hair (< 3 cm). Additionally, the counting and measuring procedure is very labor intensive, which limits its practicality in normal clinical practice.
Ross et al. 12 report on the successful use of videodermoscopy in the diagnosis of hair and scalp disorders. The color-transition sign has been used to differentiate alopecia areata from telogen effluvium 13.
Telogen effluvium treatments
There is normally no treatment required for telogen effluvium as the hair will start growing back once the trigger is removed. Medication does not speed up this process.
The doctor may check your thyroid function for over- or underactive thyroid and levels of iron, vitamin B12 and folic acid, as any deficiency in these can slow hair growth.
While topical minoxidil is not proven to promote recovery of hair in telogen effluvium, this medication has a theoretical benefit and is well tolerated. Patients who are eager to play an active role in their treatment may choose to use minoxidil.
While chronic telogen effluvium is less likely to resolve rapidly, reassurance is appropriate for these patients. Often, the knowledge that the hair loss will not progress to baldness is comforting to the patient. The patient should be encouraged to style the hair in a way that masks any perceived defects in hair density.
Telogen effluvium diet
You should also ensure a nutritious diet, with plenty of protein, fruit and vegetables.
- Poonia K, Thami GP, Bhalla M, Jaiswal S, Sandhu J. NonScarring Diffuse Hair Loss in Women: a Clinico-Etiological Study from tertiary care center in North-West India. J Cosmet Dermatol. 2018 May 17.[↩]
- Sinclair R. Chronic telogen effluvium: a study of 5 patients over 7 years. J Am Acad Dermatol. 2005 Feb. 52(2 Suppl 1):12-6.[↩]
- Perez-Mora N, Goren A, Velasco C, Bermudez F. Acute telogen effluvium onset event is associated with the presence of female androgenetic alopecia: potential therapeutic implications. Dermatol Ther. 2014 May-Jun. 27(3):159-62.[↩][↩]
- Freinkel RK, Freinkel N. Hair growth and alopecia in hypothyroidism. Arch Dermatol. 1972 Sep. 106(3):349-52.[↩]
- Malkud S. A Hospital-based Study to Determine Causes of Diffuse Hair Loss in Women. J Clin Diagn Res. 2015 Aug. 9 (8):WC01-4.[↩][↩]
- Olsen EA, Reed KB, Cacchio PB, Caudill L. Iron deficiency in female pattern hair loss, chronic telogen effluvium, and control groups. J Am Acad Dermatol. 2010 Dec. 63(6):991-9.[↩]
- Katz KA, Cotsarelis G, Gupta R, Seykora JT. Telogen effluvium associated with the dopamine agonist pramipexole in a 55-year-old woman with Parkinson’s disease. J Am Acad Dermatol. 2006 Nov. 55(5 Suppl):S103-4.[↩]
- Tosti A, Piraccini BM, van Neste DJ. Telogen effluvium after allergic contact dermatitis of the scalp. Arch Dermatol. 2001 Feb. 137(2):187-90.[↩]
- Martínez-Velasco MA, Vázquez-Herrera NE, Maddy AJ, Asz-Sigall D, Tosti A. The Hair Shedding Visual Scale: A Quick Tool to Assess Hair Loss in Women. Dermatol Ther (Heidelb). 2017 Mar. 7 (1):155-165.[↩]
- Sinclair R, Jolley D, Mallari R, Magee J. The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair loss in women. J Am Acad Dermatol. 2004 Aug. 51(2):189-99.[↩]
- Rebora A, Guarrera M, Baldari M, Vecchio F. Distinguishing androgenetic alopecia from chronic telogen effluvium when associated in the same patient: a simple noninvasive method. Arch Dermatol. 2005 Oct. 141(10):1243-5.[↩]
- Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol. 2006 Nov. 55(5):799-806.[↩]
- Kinoshita-Ise M, Fukuyama M, Ohyama M. Color-transition sign: A useful trichoscopic finding for differentiating alopecia areata incognita from telogen effluvium. J Dermatol. 2018 Mar 6.[↩]