Contents
Temporal lobe
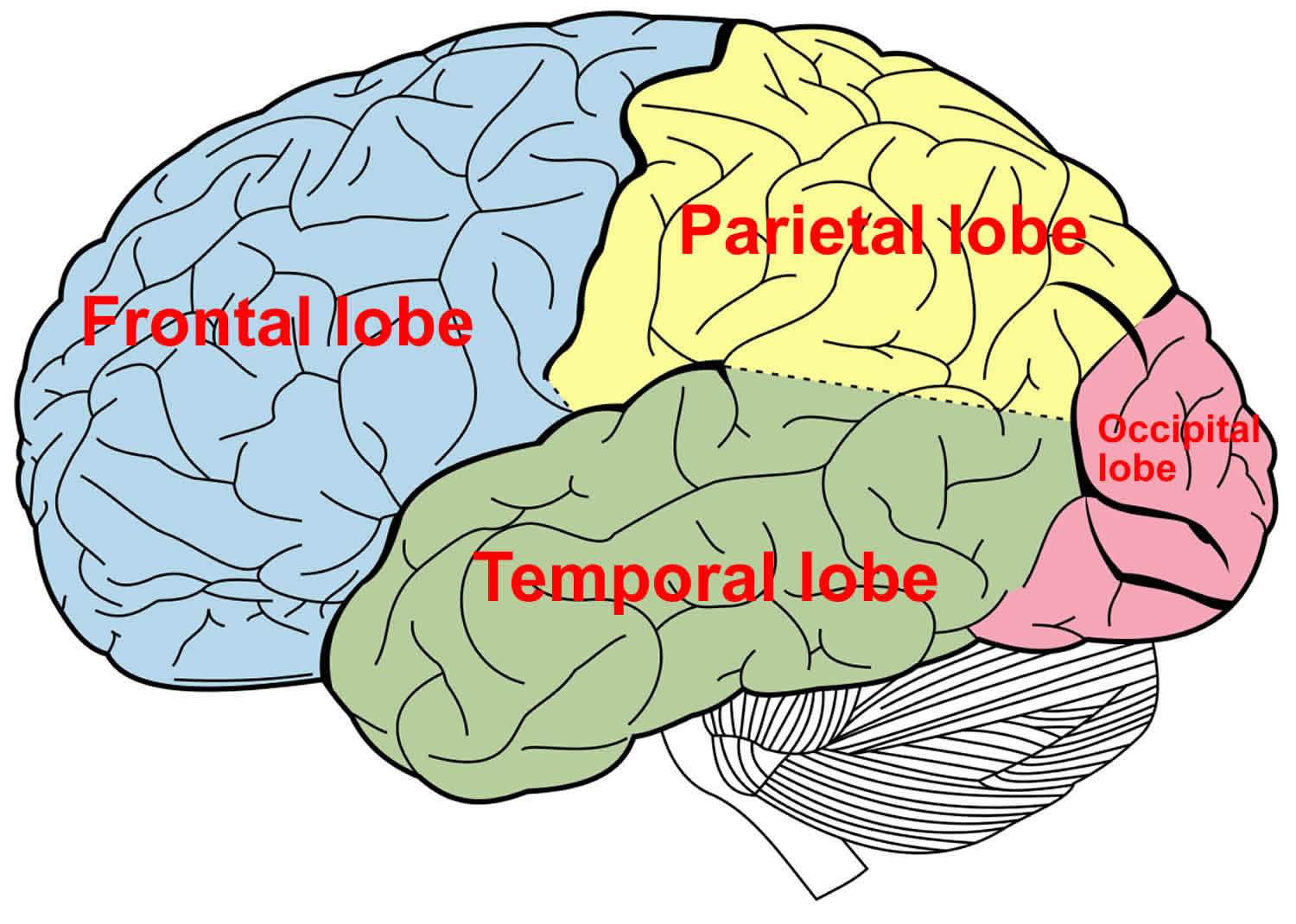
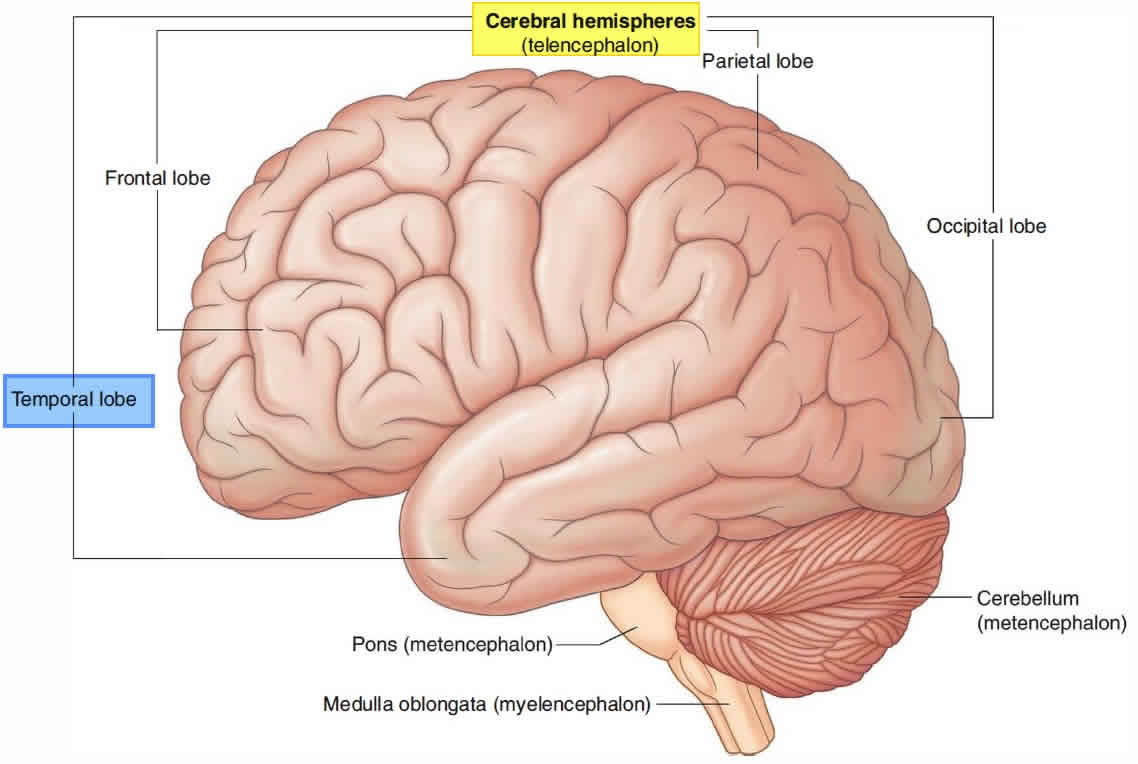
The temporal lobe of the brain is often referred to as the neocortex. The temporal lobe forms the cerebral cortex in conjunction with the occipital lobe, the parietal lobe, and the frontal lobe. Approximately 17% of the volume of the human cerebral cortex, 16% in the right and 17% in the left hemisphere, forms the surfaces of the temporal lobes 1. The temporal lobe subdivides further into the superior temporal lobe, the middle temporal lobe, and the inferior temporal lobe. The temporal lobe contains the auditory cortex and the olfactory cortex. The temporal lobe also functions in the recognition of objects, words, and faces; in language comprehension; and in emotional response and memory 2. In addition to temporal lobe cortex, the temporal lobe contains white matter, part of the lateral ventricle, the tail of the caudate nucleus, the stria terminalis, the hippocampal formation, and the amygdala. The medial side of the temporal lobe includes regions concerned with olfaction (the uncus and nearby cortex) and semantic memory (the hippocampal formation). The nearby amygdala generates responses to perceived sensory stimuli that have been partly analyzed elsewhere in the brain. Such responses include largely involuntary ones, mediated by the autonomic and somatic motor systems, and mental functions, especially those called feelings or emotions, that motivate decision and voluntary actions 3.
The temporal lobe, on the lateral side of the hemisphere, lies in the middle cranial fossa deep to the temporal bone. The temporal lobe is separated from the overlying parietal and frontal lobes by the deep lateral sulcus.
The temporal lobe is crucial in many essential activities such as processing of memory, language, and emotion.
The dominant temporal lobe, which is the left side in most people, is involved in understanding language and learning and remembering verbal information. The non-dominant lobe, which is typically the right temporal lobe, is involved in learning and remembering non-verbal information (e.g. visuo-spatial material and music).
The temporal lobe is involved in:
- Hearing (auditory cortex and association area)
- Smell (olfactory cortex)
- Object identification (posterior association area)
- Emotional response, memory (limbic association area)
The primary auditory cortex is located on the superior edge of the temporal lobe, primarily inside the lateral sulcus, functions in conscious awareness of sound. When sound waves excite the sound receptors of the inner ear, impulses are transmitted to the primary auditory cortex, where this information is related to loudness, rhythm, and pitch (high and low notes). The auditory association area lies just posterior and lateral to the primary auditory area. This area permits the evaluation of a sound as, say, a screech, thunder, or music.
The primary olfactory cortex lies on the medial aspect of the temporal lobe in a small region called the piriform cortex (“pearshaped”), which is dominated by the hooklike uncus. The olfactory nerves from the nasal cavity transmit impulses that ultimately are relayed to the olfactory cortex, resulting in conscious awareness of smells. The olfactory cortex is part of a brain area called the rhinencephalon (“nose brain”), which includes all parts of the cerebrum that directly receive olfactory signals: the piriform cortex, the olfactory tract, the olfactory bulb, and some nearby structures.
The hippocampal formation, located in the temporal lobe, consists of the hippocampus (“sea horse”) and the parahippocampal gyrus. These regions encode, consolidate, and later retrieve memories of facts and events. The hippocampal formation receives information to be remembered from the rest of the cerebral cortex; it processes these data and returns them to the cortex, where they are stored as long-term memories.
The temporal lobe can be damaged by infection, trauma, ischemia, and neoplasia. Lesions in the temporal lobe can stimulate or inhibit the functions mentioned above. The syndrome of Kluver and Bucy 4 provided an extreme example of changed behavior following bilateral temporal lobectomy in monkeys. The animals became unnaturally docile, exhibited excessive and abnormal sexual behavior, lost the ability to be trained, and had a condition that the authors termed “psychic blindness,” in which tactile exploration of objects with the mouth replaced their visual recognition. The equivalent human syndrome is rare and usually associated with pathology extending beyond the temporal lobes 5. Fragments of the classical syndrome, such as visual field defects, visual agnosia, and inability to consolidate new memories, occur more frequently, with destructive lesions in parts of one or both temporal lobes.
The temporal lobe receives oxygenated blood via two primary sources, the internal carotid system and the vertebrobasilar artery. The internal carotid system contains the anterior choroidal artery and the middle cerebral artery. The blood flow from the anterior choroidal artery supplies the uncus, amygdala, and the anterior parahippocampal gyrus. The middle cerebral artery branches into the temporopolar artery, anterior temporal artery, middle temporal artery, and posterior temporal artery. It supplies the temporal pole as well as the superior and inferior portions of the temporal gyri. Blood flow from the vertebrobasilar system supplies the inferior surface of the temporal lobe from the temper-occipital artery.
Blood is drained from the temporal lobe by veins via two major routes. One route involves blood passing from the temporal lobe anteriorly to superficial middle cerebral vein. From there, it moves into the inferior anastomotic vein, known as the vein of Labbe, which goes on to join the transverse sinus. The other route involves blood flowing from the interior temporal lobe into the posterior choroidal vein. This vessel then pairs up with the thalamostriate vein from behind the interventricular foramen to form the internal cerebral vein. The internal cerebral vein then joins the basal veins to create the great cerebral vein.[1]
Figure 1. Temporal lobe
Figure 2. Coronal section through the temporal lobe
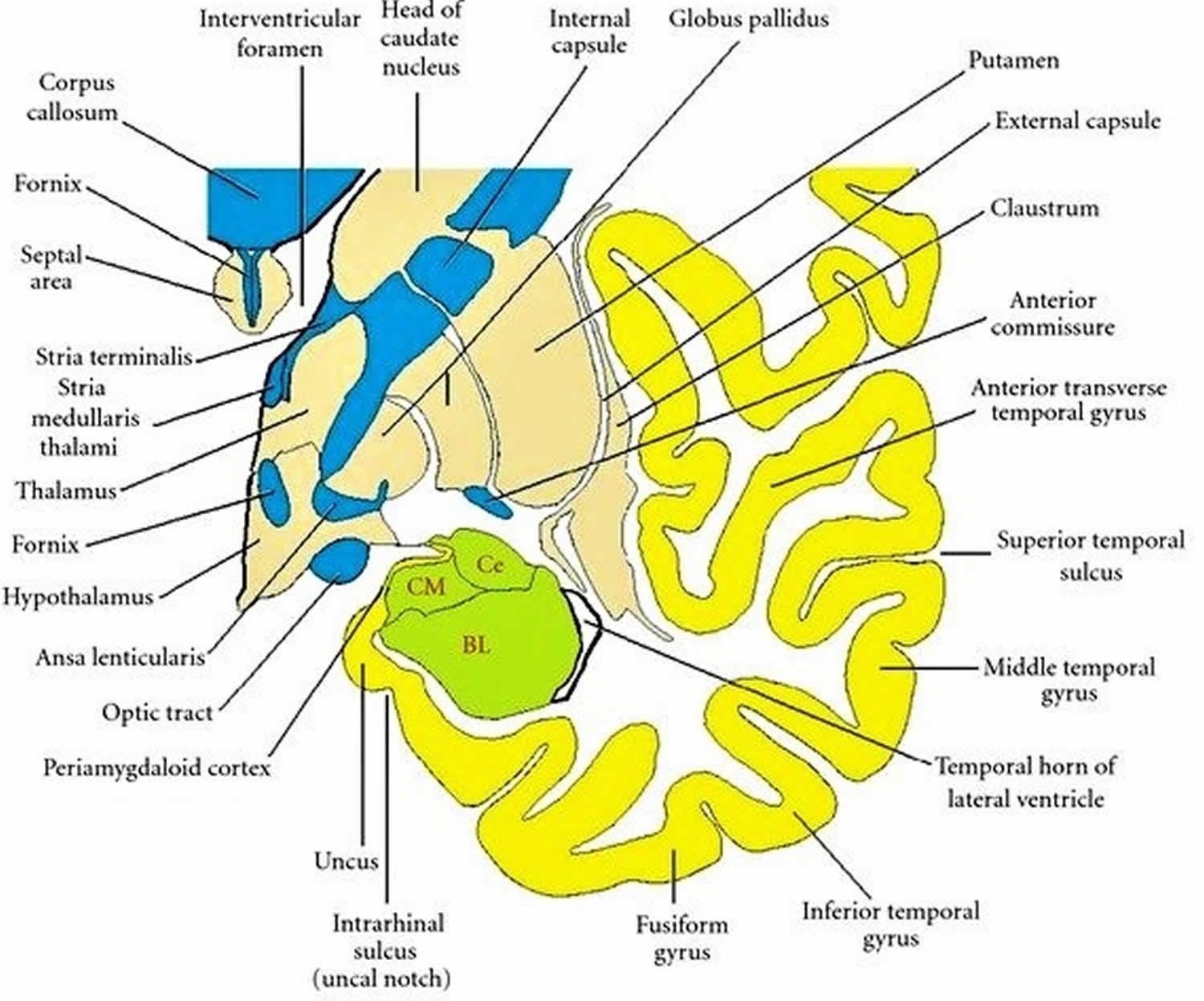 Footnote: Drawing of a coronal section through the temporal lobe and adjacent structures, at a level anterior to the hippocampal head. The amygdala is coloured green, with the positions of its three nuclear groups indicated: corticomedial (CM), basolateral (BL), and central (Ce). Selected bodies of white matter are coloured blue. [Source 2 ]
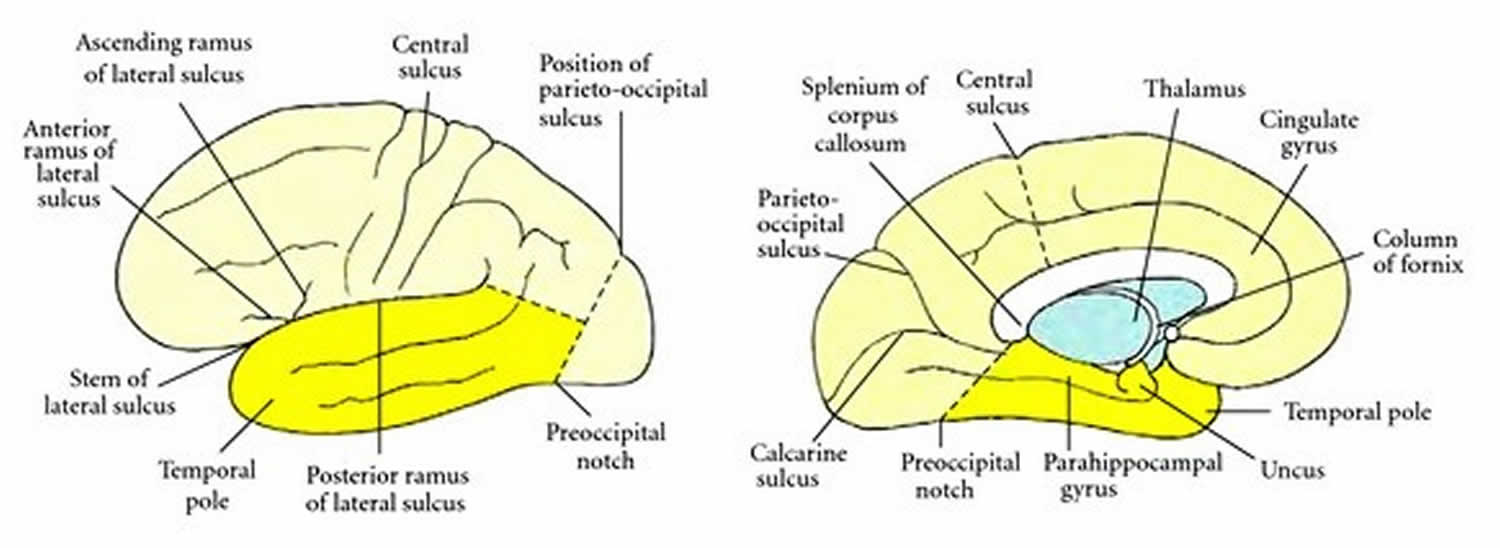
Footnote: Drawing of a coronal section through the temporal lobe and adjacent structures, at a level anterior to the hippocampal head. The amygdala is coloured green, with the positions of its three nuclear groups indicated: corticomedial (CM), basolateral (BL), and central (Ce). Selected bodies of white matter are coloured blue. [Source 2 ]Figure 3. Boundaries of the temporal lobe
Footnote: Boundaries of the temporal lobe and positions of major sulci and gyri and other anatomical landmarks of the lateral and medial surfaces of the left cerebral hemisphere.
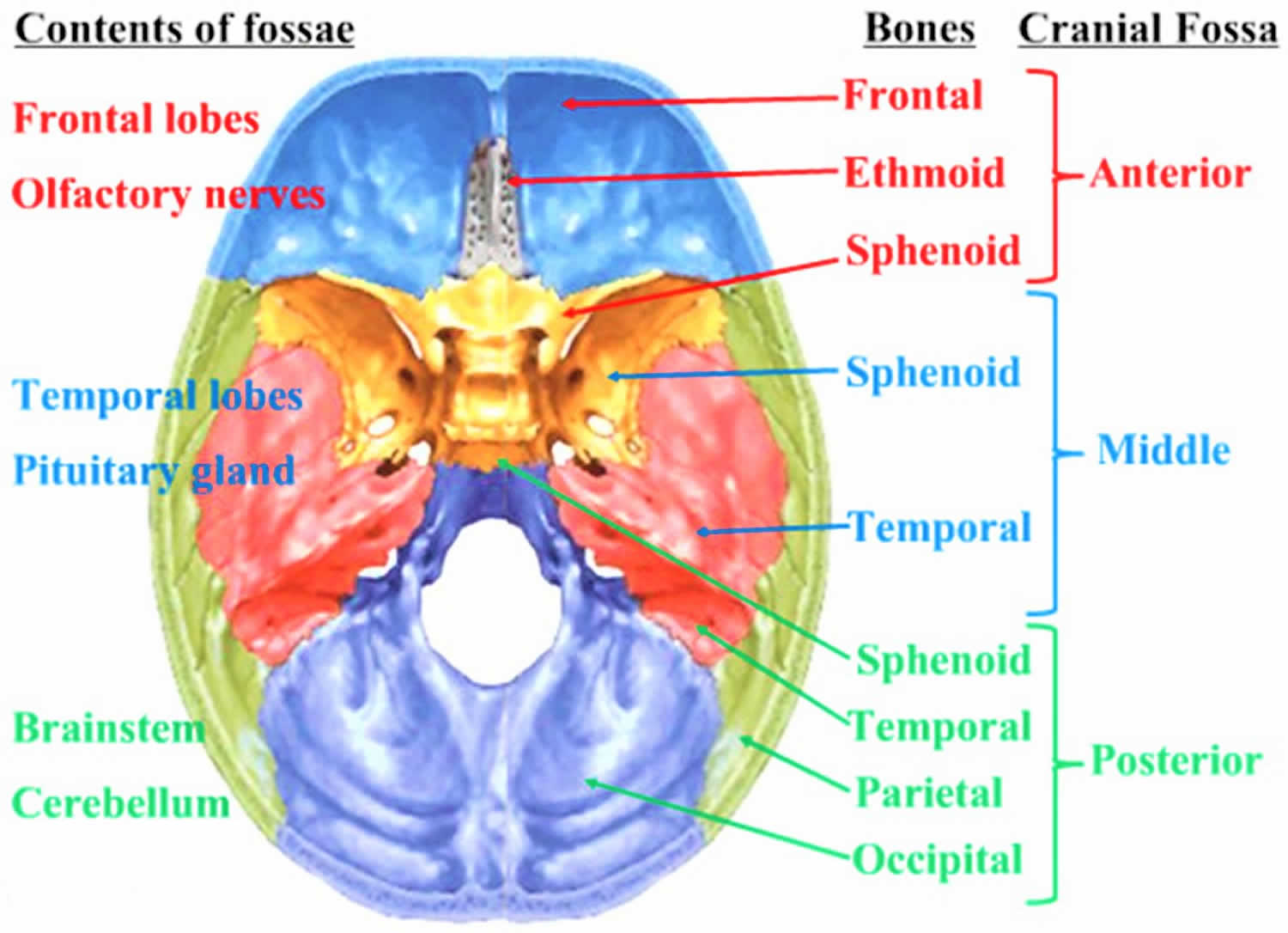
[Source 2 ]Figure 4. Middle cranial fossa
Where is the temporal lobe located?
The temporal lobe is located in the middle cranial fossa deep to the temporal bone. The middle cranial fossa consists of parts of the sphenoid and temporal bones. The floor in the midline of the middle cranial fossa is elevated and formed by the body of the sphenoid. Lateral to this are large depressions formed on either side by the greater wing of the sphenoid and the squamous part of the temporal bone. These depressions contain the temporal lobes of the brain.
What does the temporal lobe do?
The primary functions of the temporal lobe are to process sensory information and derive it into meaningful memories, language, and emotions 6. The temporal lobe is responsible primarily for declarative memory, which is memory that can be said out loud, and is subdivided into episodic (life events) and semantic (fact-like) memory. Located within the middle temporal lobe are the hippocampus and the amygdala. The hippocampus manages the formation of new memories and the conversion of short-term memories into long-term ones. The hippocampus communicates closely with the amygdala, which is responsible for the processing of emotions.
The temporal lobe also plays an essential role in processing sounds. It houses the primary auditory cortex and the superior temporal gyrus. The primary auditory cortex can process input from the ears into meaningful units like words and sentences. The sounds we hear first enter the brain in an area within the superior temporal gyrus traveling from the cochlea.
Parts of the temporal lobe aid in processing visual stimuli, primarily to allow us to recognize objects. The fusiform gyrus distinguishes faces, and the parahippocampal gyrus identifies locations and landscapes.
A specialized area of the temporal lobe, known as the Wernicke area, is found on the dominant hemisphere. It is responsible for processing written and spoken language.
Temporal lobe damage
Uncontrolled damage to the temporal lobe poses a significant threat to the quality of a patient’s life. A review of 56 localized lesions to the temporal lobe showed widespread effects on patient lives. The most common symptoms observed are mental disturbances generally categorized as a confused state. The secondary ailment of temporal lesions is personality changes, which ranges widely from slight emotional changes to homicidal tendencies. Of lesser frequency but still reported include symptoms of muscular pareses, somatic seizures, psychical seizures, autonomic seizures, visual field defects, and speech disorders 7.
Damage to the temporal lobes can result in:
- Difficulty in understanding spoken words (Receptive Aphasia)
- Disturbance with selective attention to what we see and hear
- Difficulty with identification and categorisation of objects
- Difficulty learning and retaining new information
- Impaired factual and long-term memory
- Persistent talking
- Difficulty in recognising faces (Prosopagnosia)
- Increased or decreased interest in sexual behaviour
- Emotional disturbance (e.g. Aggressive behaviour)
Wernicke aphasia is one clinical presentation of damage to the temporal lobe. It is seen often in patients who have suffered an ischemic stroke to the temporal lobe. Less frequently, it affects patients with infections, trauma, tumors, central nervous system infections, and other degenerative brain conditions. Wernicke aphasia, also known as receptive aphasia, impairs language function. Patients presenting with this aphasia can still speak with normal rate and tone but will often misuse words and form nonsensical sentences. This aphasia is in contrast to Broca aphasia in which patients cannot talk with normal fluency and tone.
Temporal lobe epilepsy
Temporal lobe epilepsy also called temporal lobe seizures, begin in the temporal lobes of your brain, which process emotions and are important for short-term memory. Some symptoms of a temporal lobe seizure may be related to these functions, including having odd feelings — such as euphoria, deja vu or fear.
Temporal lobe epilepsy are sometimes called focal epilepsy with impaired awareness. Some people remain aware of what’s happening, but during more-intense epilepsy, you might look awake but be unresponsive. Your lips and hands may make purposeless, repetitive movements.
Temporal lobe epilepsy may stem from an anatomical defect or scar in your temporal lobe, but the cause is often unknown. Temporal lobe epilepsy are treated with medication. For some people who don’t respond to medication, surgery may be an option.
Seizures don’t usually result in serious injury, but if you have recurrent epilepsy, injury is a possibility. These steps can help you avoid injury during a seizure:
- Take care near water. Don’t swim alone or relax in a boat without someone nearby.
- Wear a helmet for protection during activities such as bike riding or sports participation.
- Take showers instead of baths, unless someone is near you.
- Modify your furnishings. Pad sharp corners, buy furniture with rounded edges and choose chairs that have arms to keep you from falling off the chair.
- Consider carpet with thick padding to protect you if you do fall.
- Display seizure first-aid tips in a place where people can easily see them. Include any important phone numbers there, too.
Seizure first aid
It’s helpful to know what to do if you witness someone having a seizure. If you’re at risk of having epilepsy in the future, pass this information along to family, friends and co-workers so that they know what to do if you have a seizure.
To help someone during a seizure:
- Carefully roll the person onto one side
- Place something soft under his or her head
- Loosen tight neckwear
- Avoid putting your fingers or other objects in the person’s mouth
- Don’t try to restrain someone having a seizure
- Clear away dangerous objects, if the person is moving
- Stay with the person until medical personnel arrive
- Observe the person closely so that you can provide details on what happened
- Time the seizure
- Stay calm
Temporal lobe epilepsy symptoms
An unusual sensation (aura) may precede a temporal lobe seizure, acting as a warning. Not everyone who has temporal lobe epilepsy has auras, and not everyone who has auras remembers them.
The aura is actually the first part of a focal seizure before consciousness is impaired. Examples of auras include:
- A sudden sense of unprovoked fear or joy
- A deja vu experience — a feeling that what’s happening has happened before
- A sudden or strange odor or taste
- A rising sensation in the abdomen, similar to being on a roller coaster
Sometimes temporal lobe epilepsy impair your ability to respond to others. This type of temporal lobe seizure usually lasts 30 seconds to two minutes.
Characteristic signs and symptoms include:
- Loss of awareness of surroundings
- Staring
- Lip smacking
- Repeated swallowing or chewing
- Unusual finger movements, such as picking motions
After a temporal lobe seizure, you may have:
- A period of confusion and difficulty speaking
- Inability to recall what occurred during the seizure
- Unawareness of having had a seizure
- Extreme sleepiness
In extreme cases, what starts as a temporal lobe seizure evolves into a generalized tonic-clonic (grand mal) seizure — featuring convulsions and loss of consciousness.
Temporal lobe epilepsy complications
Over time, repeated temporal lobe epilepsy can cause the part of the brain that’s responsible for learning and memory (hippocampus) to shrink. Brain cell loss in this area may cause memory problems.
Temporal lobe epilepsy causes
Often, the cause of temporal lobe epilepsy remains unknown. However, they can be a result of a number of factors, including:
- Traumatic brain injury
- Infections, such as encephalitis or meningitis, or a history of such infections
- A process that causes scarring (gliosis) in a part of the temporal lobe called the hippocampus
- Blood vessel malformations in the brain
- Stroke
- Brain tumors
- Genetic syndromes
During normal waking and sleeping, your brain cells produce varying electrical activity. If the electrical activity in many brain cells becomes abnormally synchronized, a convulsion or seizure may occur.
If this happens in just one area of the brain, the result is a focal seizure. A temporal lobe seizure is a focal seizure that originates in one of the temporal lobes.
Temporal lobe epilepsy diagnosis
After a seizure, your doctor will thoroughly review your symptoms and medical history. Your doctor may order several tests to determine the cause of your seizure and evaluate how likely it is that you’ll have another one.
Tests may include:
- Neurological exam. Your doctor may test your behavior, motor abilities and mental function to determine if you have a problem with your brain and nervous system.
- Blood tests. Your doctor may take a blood sample to check for signs of infections, genetic conditions, blood sugar levels or electrolyte imbalances.
- Electroencephalogram (EEG). Electrodes attached to your scalp record the electrical activity of your brain, which shows up as wavy lines on an EEG recording. The EEG may reveal a pattern that tells doctors whether a seizure is likely to occur again, or help rule out other conditions that mimic epilepsy.
- Computerized tomography (CT) scan. A CT scan uses X-rays to obtain cross-sectional images of your brain. CT scans can reveal abnormalities in your brain that might cause a seizure, such as tumors, bleeding and cysts.
- Magnetic resonance imaging (MRI). An MRI uses powerful magnets and radio waves to create a detailed view of your brain. Your doctor may be able to detect lesions or abnormalities in your brain that could lead to seizures.
- Positron emission tomography (PET). PET scans use a small amount of low-dose radioactive material that’s injected into a vein to help visualize active areas of the brain and detect abnormalities.
- Single-photon emission computerized tomography (SPECT). A SPECT test uses a small amount of low-dose radioactive material that’s injected into a vein to create a detailed, 3-D map of the blood flow activity in your brain that happens during a seizure. Doctors may also conduct a form of a SPECT test called subtraction ictal SPECT coregistered to magnetic resonance imaging (SISCOM), which may provide even more-detailed results.
Temporal lobe epilepsy treatment
Not everyone who has one seizure will have another one. Because a seizure can be an isolated incident, your doctor may not decide to start treatment until you’ve had more than one.
The optimal goal in seizure treatment is to find the best possible therapy to stop epilepsy, with the fewest side effects.
Medications
Many medications are available to treat temporal lobe epilepsy. However, many people don’t achieve seizure control with medications alone, and side effects, including fatigue, weight gain and dizziness, are common.
Discuss possible side effects with your doctor when deciding about treatment options. Also ask what effect your seizure medications and other medications you take, such as oral contraceptives, may have on each other.
Surgical or other procedures
When anti-seizure medications aren’t effective, other treatments may be an option:
- Surgery. The goal of surgery is to stop epilepsy from happening. This is often done through a traditional surgery, where surgeons operate to remove the area of the brain where epilepsy begin. In certain people, surgeons may be able to use MRI-guided laser therapy as a less invasive way to destroy the area of damaged tissue that causes epilepsy. Surgery works best for people who have epilepsy that always originate in the same place in their brains. Surgery generally isn’t an option if your epilepsy come from more than one area of the brain, your seizure focus can’t be identified or your epilepsy come from a region of the brain that performs vital functions.
- Vagus nerve stimulation. A device implanted underneath the skin of your chest stimulates the vagus nerve in your neck, sending signals to your brain that inhibit epilepsy. With vagus nerve stimulation, you may still need to take medication, but you may be able to lower the dose.
- Responsive neurostimulation. During responsive neurostimulation, a device implanted on the surface of your brain or within brain tissue can detect seizure activity and deliver an electrical stimulation to the detected area to stop the seizure.
- Dietary therapy. Following a diet that’s high in fat and low in carbohydrates, known as a ketogenic diet, can improve seizure control. Variations on a high-fat, low-carbohydrate diet, such as the low glycemic index and modified Atkins diets, may be less effective. However, they aren’t as restrictive as the ketogenic diet and might provide some benefit.
Pregnancy and epilepsy
Women who’ve had previous epilepsy typically are able to have healthy pregnancies. Birth defects related to certain medications can sometimes occur.
In particular, valproic acid (Depakene) — one possible medication for generalized epilepsy — has been associated with cognitive deficits and neural tube defects, such as spina bifida. The American Academy of Neurology recommends that women avoid using valproic acid during pregnancy because of risks to the baby.
Discuss these risks with your doctor. Because of the risk of birth defects, and because pregnancy can alter medication levels, preconception planning is particularly important for women who’ve had epilepsy.
In some cases, it may be appropriate to change the dose of seizure medication before or during pregnancy. Medications may be switched in rare cases.
Contraception and anti-seizure medications
It’s also important to know that some anti-seizure medications can alter the effectiveness of oral contraceptives — a form of birth control — and some oral contraceptives can speed up the absorption of seizure medications. If contraception is a high priority, check with your doctor to evaluate whether your medication interacts with your oral contraceptive, and if other forms of contraception need to be considered.
- Mai JG, Paxinos G, Voss T. Atlas of the Human Brain. 3rd edition. Amsterdam, The Netherlands: Elsevier; 2008[↩]
- Kiernan JA. Anatomy of the temporal lobe. Epilepsy Res Treat. 2012;2012:176157. doi:10.1155/2012/176157 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3420617[↩][↩][↩]
- Baloh RW, Kerber KA. Neurophysiology of the Vestibular System. 4th edition. New York, NY, USA: Oxford University Press; 2011[↩]
- Kluver H, Bucy PC. Preliminary analysis of functions of temporal lobes in monkeys. Archives of Neurology and Psychiatry. 1939;42:979–1000[↩]
- Jha S, Patel R. Kluver-Bucy syndrome—an experience with six cases. Neurology India. 2004;52(3):369–371[↩]
- Patel A, Fowler JB. Neuroanatomy, Temporal Lobe. [Updated 2019 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519512[↩]
- WYKE BD. Surgical considerations of the temporal lobes; a clinical report based on a study of fifty-six verified localised lesions of the temporal lobes. Ann R Coll Surg Engl. 1958 Feb;22(2):117-38[↩]