Contents
What is tracheitis
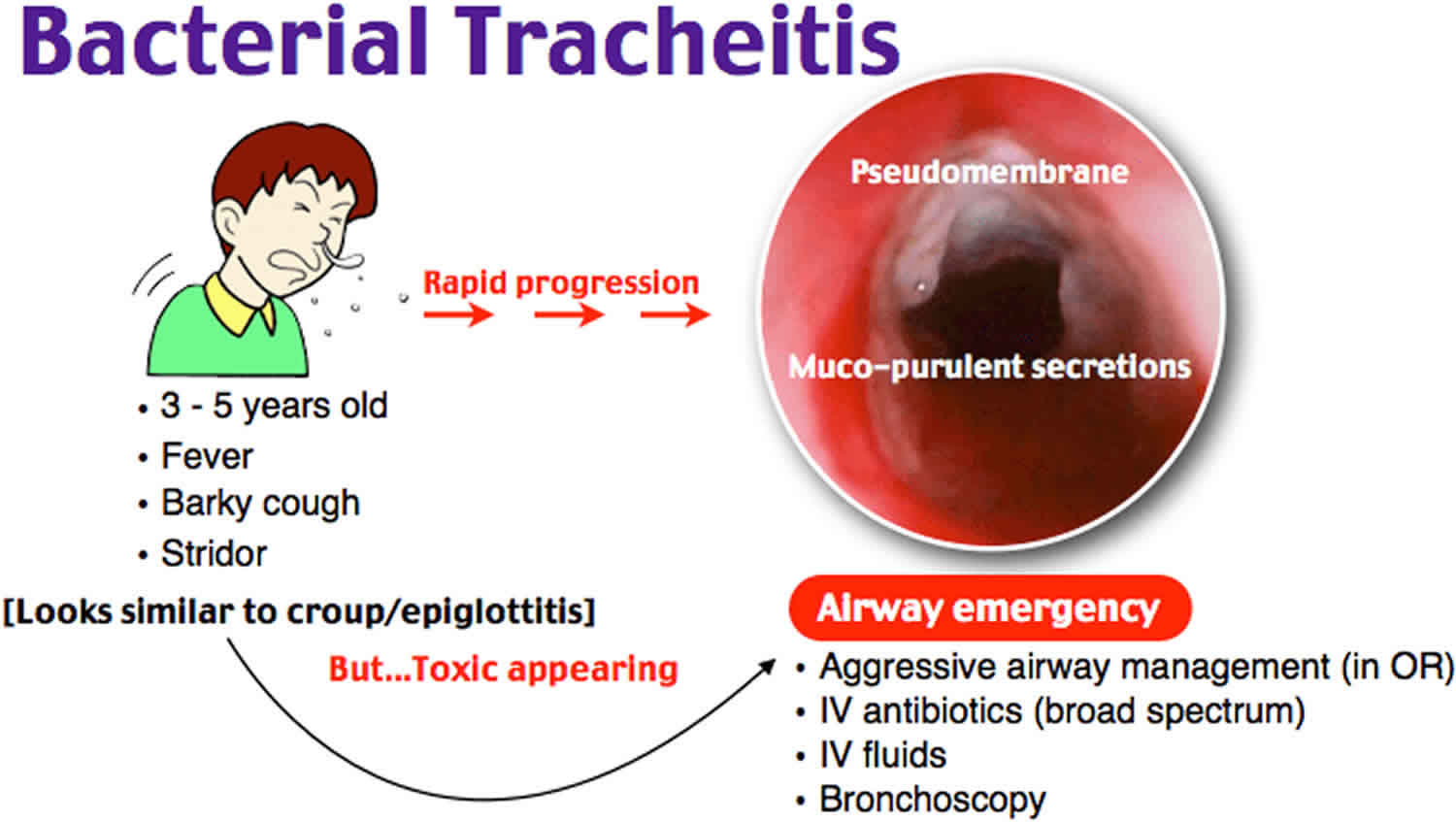
Tracheitis is a bacterial infection of the trachea or windpipe. Tracheitis is an emergency medical condition. Go to the emergency room right away if your child has had a recent upper respiratory infection and suddenly has a high fever, a cough that gets worse, or trouble breathing. Bacterial tracheitis also known as “bacterial croup,” “acute laryngotracheobronchitis,” or “membranous croup,” is due to a secondary bacterial infection of the trachea, resulting in the formation of mucopurulent exudates that may acutely obstruct the upper airway, resulting in a life-threatening condition 1. Bacterial tracheitisis often a secondary bacterial infection preceded by a viral infection affecting children most commonly under age six 2. This may be due to children’s tracheas being smaller and more easily blocked by swelling. Bacterial tracheitis is most often caused by the bacteria Staphylococcus aureus, although reports suggest Moraxella catarrhalis is becoming more common especially in younger children.
In bacterial tracheitis, opportunistic bacteria invade damaged tracheal mucosa and stimulate local and systemic inflammatory responses. Local responses cause swelling, thick mucopurulent secretions, ulceration, and mucosal sloughing, which can predispose to subglottic narrowing. Systemic inflammation leading to sepsis is rare but can occur in immunocompromised children.
Concern for airway protection is the mainstay of treatment as thick, mucopurulent secretions can cause airway narrowing. Treatment is aimed at protection of the airway, assessing the need for endoscopy for therapeutic and/or diagnostic reasons, and antimicrobial therapy 3. Very ill children require endotracheal intubation. The tube keeps the airway from swelling shut. Antibiotics (such as cefuroxime or vancomycin) are given to treat the infection.
Is tracheitis contagious?
Yes. Tracheitis can be caused bacterial and/or viral infection of the trachea or windpipe. Bacterial tracheitis often preceded by a viral upper respiratory infection. Most common viruses implicated include Influenza A and B (with type A being the most common), respiratory syncytial virus (RSV), parainfluenza virus, measles virus, and enterovirus. These viruses cause airway mucosal damage via a local immune response which predisposes the trachea to the seeding of bacterial infections. Staphylococcus aureus has been the most commonly implicated pathogen in tracheitis.
Tracheitis how long does it last?
Mean duration of hospitalization is estimated to range from 3 to 12 days 2. One small case series of children with bacterial tracheitis reported a mean duration of hospitalization of 20.8 days 4. The authors speculated that this was due to complications associated with a protracted recovery in several patients 4. Most children recover without debilitating sequelae with the tracheal mucosa fully healing without permanent damage.
Bacterial tracheitis complications may include:
- Airway obstruction (can lead to death)
- Toxic shock syndrome if the condition was caused by the bacteria staphylococcus
Tracheitis causes
Bacterial tracheitis is a bacterial infection of the trachea often preceded by a viral upper respiratory infection. Most common viruses implicated include Influenza A and B (with type A being the most common), respiratory syncytial virus (RSV), parainfluenza virus, measles virus, and enterovirus. These viruses cause airway mucosal damage via a local immune response which predisposes the trachea to the seeding of bacterial infections. Children affected are usually healthy. However, at-risk populations including immunocompromised individuals are prone to severe sequelae. Implicated bacteria include Staphylococcus aureus (most common, including MRSA), Streptococcus pneumoniae, Streptococcus pyogenes, Moraxella catarrhalis, Haemophilus influenzae type B, and less commonly, Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumonia, and anaerobic organisms 5.
Bacterial tracheitis has a peak incidence between the ages of three to eight years, although it has been described less commonly in infants and adults. Males have a slight predominance over females with a 1.3:1 prevalence ratio. Annual incidence is rare with an estimated incidence of 0.1 cases per 100,000 children. Incidences are more common in fall and winter months than in summer or spring. This coincides with the typical seasonal viral epidemics of influenza, parainfluenza, and respiratory syncytial virus (RSV) 6.
Microscopic Gram stain analysis of tracheal secretions usually reveals neutrophilia and bacteria identification. Often, bacterial tracheitis is polymicrobial. Infection of the tracheal mucosa causes local inflammation, swelling, thick exudates, pseudomembranes, and necrosis of the larynx, trachea, and mainstem bronchi.
Tracheitis symptoms
Tracheitis symptoms include:
- Deep cough (similar to that caused by croup)
- Difficulty breathing
- High fever
- High-pitched breathing sound (stridor)
Presentation occurs in two primary ways including a more insidious development with prodromal symptoms that suggest a viral respiratory tract infection. These are present for 1 to 3 days until the more severe development of airway deterioration occurs due to an overlapping bacterial infection. Less commonly, fulminant respiratory distress with less than 24 hours of symptoms can occur. These children tend to be more toxic appearing. Signs and symptoms include stridor (inspiratory or expiratory), fever, exudative cough, and respiratory distress. Drooling and tripoding are less common and suggest an alternative diagnosis such as epiglottitis, as children with bacterial tracheitis do not have difficulty swallowing their oral secretions. Patients with severe subglottic obstruction may have cyanosis, appear lethargic or can be combative suggesting hypoxemia and/or hypercarbia.
Trial with nebulized epinephrine and glucocorticoids will fail to show improvement in the patient’s clinical course 2.
Tracheitis possible complications
Tracheitis complications may include:
- Airway obstruction (can lead to death)
- Toxic shock syndrome if the condition was caused by the bacteria staphylococcus
The most frequent complication associated with the acute phase of tracheitis is pneumonia 1. Other less common complications include acute respiratory distress syndrome, septic shock, toxic shock syndrome, pulmonary edema, pneumothorax, and rarely, cardiorespiratory arrest 7.
Long-term morbidity associated with bacterial tracheitis is minimal. As treatment in the acute phase of the illness frequently requires insertion of an endotracheal tube into an inflamed airway, the potential for the subsequent development of subglottic stenosis is recognized. This complication, indeed, has been reported in two papers. Gallagher 8 reported that three of 18 patients had subglottic stenosis, and Kasian 9 reported one case in 14 patients.
Tracheitis diagnosis
The diagnosis of bacterial tracheitis is clinical with a thorough history and physical examination. Children may appear febrile, toxic-appearing, and in respiratory distress. Your health care provider will perform a physical exam and listen to the child’s lungs. The muscles between the ribs may pull in as the child tries to breathe. This is called intercostal retractions.
Diagnosis of bacterial tracheitis can be difficult given its rarity, in addition to more prevalent diseases with similar presentations. Epiglottitis can also present with fever, upper airway obstruction, and toxic appearance. However, these patients often present with drooling and preference for the tripod position which is uncommon in bacterial tracheitis. Croup can also present with stridor and similar radiographic presentation with subglottic narrowing (“steeple” sign). Bacterial tracheitis can be a complication of croup and should be suspected if therapeutic interventions such as nebulized racemic epinephrine or steroids do not improve the clinical course. Peritonsillar or retropharyngeal abscesses will demonstrate fever, drooling, muffled voice changes and pharyngeal pain with limited mobility of the neck. Other diseases that can mimic bacterial tracheitis include foreign body aspiration, diphtheria, and severe bacterial pneumonia.
Tests that may be done to diagnose this condition include:
- Blood oxygen level
- Nasopharyngeal culture to look for bacteria
- Tracheal culture to look for bacteria
- X-ray of the trachea
- Tracheoscopy or bronchoscopy
Definitive diagnosis is made by direct visualization, although is not necessary with strong clinical suspicion. Bronchoscopy allows visualization of the infected airway and will demonstrate a normal or mildly erythematous epiglottis and an erythematous, edematous trachea with thick mucopurulent exudates. Bronchoscopy is performed with either a rigid or flexible endoscope, with the former suggested for suctioning the exudations to provide transient relief of airway obstruction as well as obtain specimens for culture. The decision to undergo bronchoscopy is made on a clinical severity basis. More severe cases benefit from the therapeutic stripping of membranes or exudates to provide relief of secretion obstruction. Exudates can be thick secretions or pseudomembranous that adhere to the tracheal wall. Flexible bronchoscopy is an alternative for those patients with the less severe presentation. However, those patients without severe respiratory distress, hypoxia and with minimal tracheal abnormalities on radiograph can be managed without bronchoscopy. Exudative secretions can extend distally to the mainstem bronchi. If bronchoscopy is performed, specimens for gram stain and cultures should be obtained during this time. Less severe cases not requiring endoscopy or endotracheal intubation can obtain cultures via sputum sample.
Tracheitis treatment
Treatment of bacterial tracheitis includes a prompt assessment for airway compromise. The child often needs to have a tube placed into the airways to help with breathing. This is called an endotracheal tube.
The need for intubation is common and is required in an estimated 72% to 75% of patients 2. This procedure can be difficult secondary to airway edema, and it is recommended to be performed in the operating room or intensive care unit setting by the most experienced provider available. Hypoxia, respiratory muscle retractions, fatigue, altered mental status and decreased breath sounds are signs indicative of impending airway failure. Younger children with smaller airways are at higher risk for the need for airway stabilization. If intubation is indicated, endotracheal tubes one or two sizes smaller should be selected due to airway narrowing. Placement into the ICU after intubation should serve to provide close monitoring and frequent suctioning of the endotracheal tube. In one case series, average intubation duration was reportedly 3.2 days. Extubation should be considered in those with clinical improvement, reduced tracheal secretions, and development of an air leak around the endotracheal tube. Other treatments in less severe cases include supplemental humidified oxygen, racemic epinephrine trial, and avoiding patient agitation which can worsen an already compromised airway 10.
The child will receive antibiotics through a vein. Antibacterial management should be prompt and include broad coverage, including MRSA. Gram stain results, if obtained, can focus antibiotic selection but broad coverage should be initially chosen until culture results are obtained. Current guidelines recommend a 10-day to 14-day antibiotic course, although no formal studies have investigated the recommended time length of antimicrobial treatment. First-line treatment has been suggested to include ceftriaxone plus nafcillin or vancomycin or clindamycin plus a third-generation cephalosporin or ampicillin-sulbactam. For patients with beta-lactam antibiotic severe allergy, the recommended antibiotic treatment regimen includes vancomycin or clindamycin plus levofloxacin or ciprofloxacin. Glucocorticoids have not been shown to alter clinical course or patient outcomes. Antiviral therapy may be beneficial if a preceding viral cause is determined to be influenza and symptoms have been present for less than 48 hours.
Tracheitis prognosis
With prompt treatment, the child with tracheitis should recover. Mean duration of hospitalization is estimated to range from 3 to 12 days 2. The mortality rate due to bacterial tracheitis has decreased dramatically with time. In the early twentieth century, the mortality rate was 10% to 40% 11. This has declined slowly with time, and the most recent and largest case series reported no mortality associated with the illness 8. The improvement in mortality rate is likely due to the early recognition and improved treatment of the disorder with aggressive airway clearance techniques and early initiation of broad spectrum antibiotics.
Most children recover without debilitating complications with the tracheal mucosa fully healing without permanent damage. However, subglottic stenosis has been reported secondary to endotracheal intubation with an inflamed airway. Mortality has been estimated in 2% to 3% of patients due to primary respiratory failure with cardiac arrest, cerebral anoxia, acute respiratory distress syndrome (ARDS), pulmonary edema, pneumothorax, toxic shock syndrome, and septic shock 2. These incidences are rare with septic shock seen in 2% to 6%, cardiorespiratory arrest in 2% to 3%, ARDS (acute respiratory distress syndrome) in 1% to 3% and the remainder of complications listed in one percent or less of patients. Prevention is aimed at vaccination against viral syndromes (measles and influenza) and pneumococcus, especially in immunocompromised children.
- Al-Mutairi B, Kirk V. Bacterial tracheitis in children: Approach to diagnosis and treatment. Paediatr Child Health. 2004;9(1):25-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2719512/[↩][↩]
- Burton LV, Silberman M. Bacterial Tracheitis. [Updated 2018 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470240[↩][↩][↩][↩][↩][↩]
- Casazza G, Graham ME, Nelson D, Chaulk D, Sandweiss D, Meier J. Pediatric Bacterial Tracheitis-A Variable Entity: Case Series with Literature Review. Otolaryngol Head Neck Surg. 2019 Mar;160(3):546-549[↩]
- Bacterial tracheitis–an old disease rediscovered. Sofer S, Duncan P, Chernick V. Clin Pediatr (Phila). 1983 Jun; 22(6):407-11.[↩][↩]
- Martin-Loeches I, Coakley JD, Nseir S. Should We Treat Ventilator-Associated Tracheobronchitis with Antibiotics? Semin Respir Crit Care Med. 2017 Jun;38(3):264-270.[↩]
- Casazza G, Graham ME, Nelson D, Chaulk D, Sandweiss D, Meier J. Pediatric Bacterial Tracheitis-A Variable Entity: Case Series with Literature Review. Otolaryngol Head Neck Surg. 2019 Mar;160(3):546-549.[↩]
- Britto J, Habibi P, Walters S, Levin M, Nadel S. Systemic complications associated with bacterial tracheitis. Arch Dis Child. 1996;74:249–50[↩]
- Gallagher P. An approach to the diagnosis and treatment of membranous laryngotracheobronchitis in infants and children. Pediatr Emerg Care. 1991;7:337–42[↩][↩]
- Kasian G, Bingham W, Steingberg J, et al. Bacterial tracheitis in children. CMAJ. 1989;140:46–50.[↩]
- Russell CJ, Shiroishi MS, Siantz E, Wu BW, Patino CM. The use of inhaled antibiotic therapy in the treatment of ventilator-associated pneumonia and tracheobronchitis: a systematic review. BMC Pulm Med. 2016 Mar 08;16:40[↩]
- Donaldson J, Maltby C. Bacterial tracheitis in children. J Otolaryngol. 1989;18:101–4.[↩]