Contents
What is ureaplasma
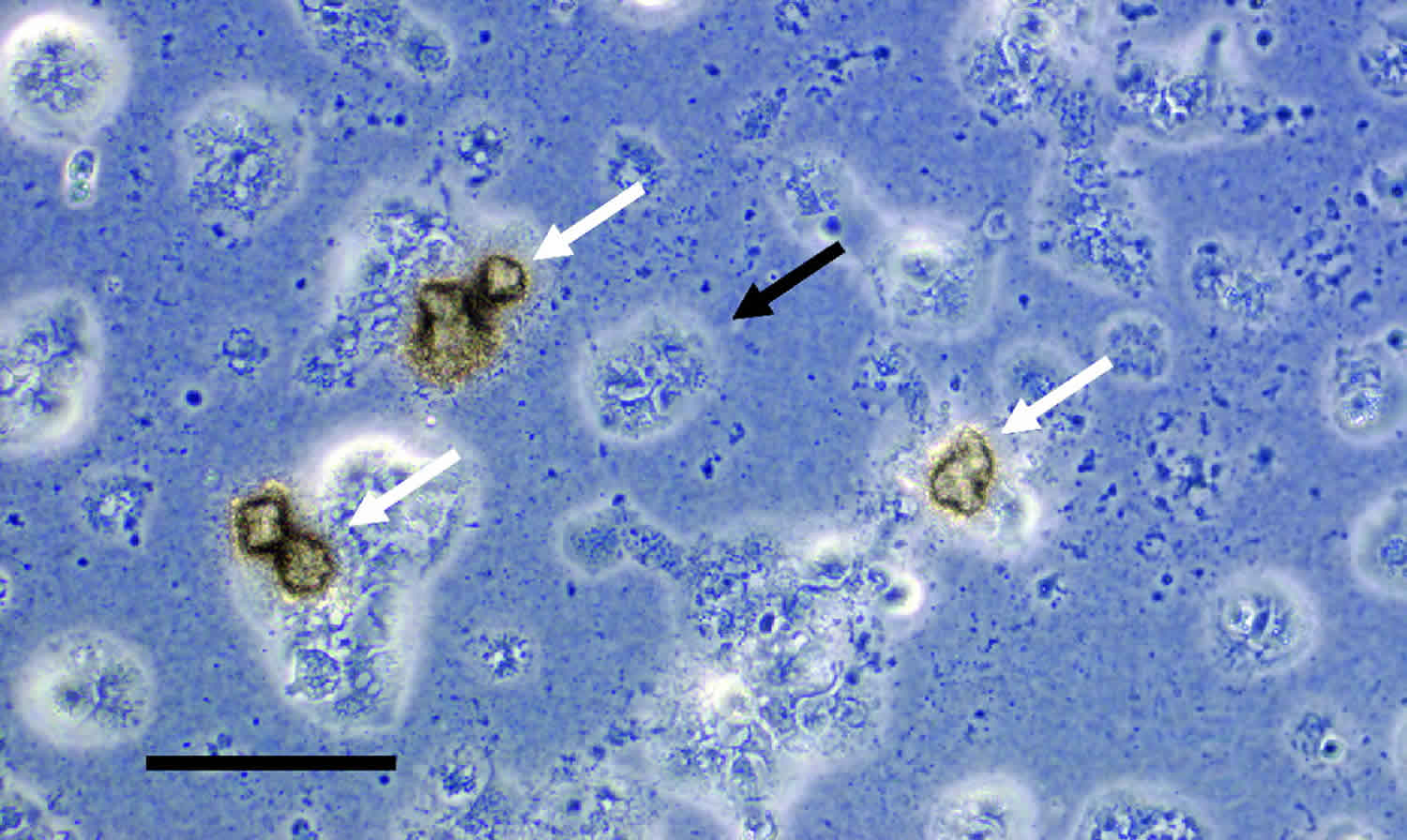
The human Ureaplasma species were first discovered in 1954 in agar cultures of urethral exudates from male patients with nongonococcal urethritis 1, 2 . Due to their small colony size (5 to 20 μm) and their resemblance to the human Mycoplasma species, Ureaplasma species were initially identified as tiny-form pleuropneuomonia-like organisms and referred to as T-mycoplasmas 1. However, Ureaplasma can be distinguished from Mycoplasma species 3 by the presence of a urease enzyme, which hydrolyzes urea to produce 95% of its energy requirements. The hydrolysis of urea produces ammonia, which leads to an increase in proton electrochemical potential and de novo ATP synthesis 4. The production of ammonia is a distinguishing feature for the identification of Ureaplasma species in culture, and these tiny bacteria are detected not by turbidity within broth but by an alkaline shift and pH indicator color change in both broth and agar culture media 5. Due to this distinctive urease activity, the Ureaplasma species were reclassified into their own genus within the Mycoplasmataceae family in 1974 3. As members of the class Mollicutes, Ureaplasma species do not possess a cell wall and are surrounded only by a plasma membrane. Due to this lack of structural integrity, the Ureaplasma species are pleomorphic, and individual organisms can range in size from 100 nm to 1 μm 6. As such, the Ureaplasma species are considered to be among the smallest self-replicating microorganisms.
The human Ureaplasma species are divided into two species, which contain at least 14 serovars: Ureaplasma parvum (serovars 1, 3, 6, and 14) and Ureaplasma urealyticum (serovars 2, 4, 5, and 7 to 13) 7, 8. Ureaplasma parvum possesses a smaller genome (0.75 to 0.78 Mbp) than Ureaplasma urealyticum (0.84 to 0.95 Mbp) 9, and these two species can also be distinguished based on restriction fragment length polymorphisms, DNA-DNA hybridization, multilocus sequence typing, and sequences of 16S rRNA, multiple-banded antigen (mba), and urease genes 10. While this taxonomic classification was formally accepted in 2002, it has not been universally adopted within the literature, and often the 14 serovars are still erroneously referred to as Ureaplasma urealyticum.
Ureaplasma can be isolated from the mucosal surfaces of the vagina or cervix from 40 to 80% of sexually active females 11. Furthermore, the human Ureaplasma species are the most frequently isolated microorganisms from the amniotic fluid and placentae of women who deliver preterm and are also associated with spontaneous abortions or miscarriages, neonatal respiratory diseases, and chorioamnionitis (inflammation of the fetal membranes, which comprise the chorion and amnion) 12. Despite the fact that Ureaplasma have been habitually found within placentae of pregnancies with chorioamnionitis, the role of Ureaplasma species as a causative agent has not been satisfactorily explained 12. There is also controversy surrounding Ureaplasma role in disease, particularly as not all women infected with Ureaplasma speciss develop chorioamnionitis 12.
Clinical studies have shown that women intra-amniotically infected with Ureaplasma species exhibit a more intense inflammatory response than those infected with other microorganisms 13. Moreover, the earlier the gestational age, the greater the intensity of the intra-amniotic inflammatory response induced by Ureaplasma species 14. However, not all women intra-amniotically infected with Ureaplasma species deliver preterm 15. This finding is consistent with animal studies in which the intra-amniotic administration of Ureaplasma species does not always lead to preterm birth. Initial studies using an established model of chronically catheterized rhesus macaques 16 showed that intra-amniotic inoculation with Ureaplasma parvum or Mycoplasma hominis induces preterm labor, intra-amniotic inflammation, inflammation of the placenta (e.g., acute chorioamnionitis), and a systemic fetal inflammatory response 17. However, the ultrasound-guided intra-amniotic injection of Ureaplasma parvum in rhesus macaques does not induce preterm labor or a severe fetal inflammatory response but causes intra-amniotic and uterine inflammation 18. The difference between the two macaque models could be explained by the distinct methodologies utilized. In mice, surgical intra-amniotic infection with Ureaplasma species does not cause preterm birth 19. Therefore, scientists hypothesized that there is diversity in the Ureaplasma species found in the amniotic cavity of women with intra-amniotic infection, which differentially modulate the host immune responses of the mother and the fetus and may dictate pregnancy outcomes 20.
Ureaplasma parvum is isolated more frequently from the lower genital tract of females than Ureaplasma urealyticum 21, and serovar 3 is the most common serovar isolated from females in the United States and Australia 22. Ureaplasma colonization of the female lower genital tract has been associated with numerous factors, including ethnicity (particularly African-American, Central/West African, and Indigenous Australian women) 23, age (most prevalent in the 14- to 25-year age group; carriage declines with increasing age) 24, the number of recent sexual partners 25, the use of nonbarrier contraceptives 25, level of education 23, age of first sexual intercourse 25, and intrauterine devices 26. Ureaplasma urealyticum (serovars 2, 4, 5, 7–13) and the separate species Ureaplasma parvum (serovars 1, 3, 6, 14) are generally regarded to be commensal organisms (part of the normal flora) within the female lower genital tract due to (i) their high prevalence and (ii) studies demonstrating no differences in the rates of endocervical Ureaplasma colonization between women of reproductive age with and those without symptoms of genital infection 24. However, others have reported that Ureaplasma species can cause lower urogenital tract infections, such as symptomatic vaginitis 27, cervicitis 28, bacterial vaginosis 29, pelvic infections 30, and urinary tract infections 31.
In pregnant women, however, upper genital tract infection with Ureaplasma species (spp.) has been associated with chorioamnionitis, adverse pregnancy outcome and preterm birth (i.e., delivery <37 weeks of gestation), especially at gestational ages <30 weeks 32. Even in moderate preterm infants (i.e., birth between 32 and 36 weeks of gestation) Ureaplasma species are one of the most commonly recovered organisms in case of histologically confirmed chorioamnionitis 33. With upper genital tract infections often being polymicrobial and with genital tract colonization occurring both among mothers with preterm birth and among mothers with full-term delivery, nevertheless, the role of Ureaplasma in disease manifestation in pregnancy remains controversial 34.
Ureaplasma causes
Lower genital tract Ureaplasma colonization association with chorioamnionitis and adverse pregnancy outcomes
It has been proposed that the presence of Ureaplasma species in the female lower genital tract may be a risk factor for chorioamnionitis and adverse pregnancy outcomes, such as preterm birth 35. A prospective study of 2,471 women attending an antenatal clinic demonstrated that Ureaplasma species were isolated from vaginal swabs from 52/97 women (53.6%) who delivered preterm and that vaginal Ureaplasma colonization was an independent risk factor for preterm birth. Despite this statistical association, it should be noted that, in the same study, Ureaplasma was also isolated from the lower genital tract of 783/1,891 women (41.1%) who delivered at term. Similarly, Kataoka et al. 36 demonstrated that Ureaplasma parvum was detected in 16/21 women (76.2%) who delivered preterm and also in 440/856 women (51.4%) who delivered at term. Other authors have reported equally high carriage rates in women who deliver at term, and the majority of studies conclude that lower genital tract Ureaplasma colonization is not a significant predictor of preterm birth or chorioamnionitis 37.
Ureaplasma can cause ascending asymptomatic infections of the upper genital tract
Although Ureaplasma species are (in most instances) considered to be commensals within the lower genital tract, these microorganisms are capable of causing ascending asymptomatic infections of the upper genital tract. A recent study of fertile and infertile women undergoing diagnostic laparoscopy (who had no symptoms of genital tract infection) demonstrated that lower genital tract Ureaplasma colonization can lead to asymptomatic infection of the pouch of Douglas 38. Furthermore, Ureaplasma species have been isolated from the endometrium and Fallopian tubes of nonpregnant women in the absence of clinical symptoms or abnormal pathology 39. While it was historically thought that the Ureaplasma species were of low virulence and that their presence in the upper genital tract might be of little consequence, there is now increasing evidence that these microorganisms are not simply innocent bystanders. The presence of Ureaplasma species in the upper genital tract of nonpregnant women suggests that these microorganisms may infect the embryo at the time of implantation 11. Moreover, they are capable of inducing chorioamnionitis, which can adversely affect the health of the pregnancy and neonate.
In preterm and term neonates, Ureaplasma species have been described as pathogens of invasive diseases, such as pneumonia, sepsis, and meningitis 40. Moreover, epidemiologic and experimental studies indicate an association of prenatal and perinatal Ureaplasma infection with fetal inflammatory response and neonatal short and long-term morbidity 41. Ureaplasma spp. have been reported to be the most common organisms isolated from the amniotic fluid, cord blood, respiratory tract and the cerebrospinal fluid of preterm infants who develop bronchopulmonary dysplasia 41. However, while respiratory tract colonization has been associated with bronchopulmonary dysplasia by several investigations 41, multivariable analysis did not confirm this relationship in other studies 42.
Vertical transmission rates of Ureaplasma spp. in pregnancy are highly variable, ranging from 15 to 88%, and seem to be inversely related to gestational age 43. Detection rates in initial tracheal aspirates or nasopharyngeal secretions range from 10 to 50% in term newborns 44 and 24–52% in preterm infants <32 weeks 45. Preterm colonization seems to be inversely proportional to gestational age, with 65% of preterm infants <26 weeks being colonized vs. 31% of preterm infants with a gestational age between 26 and 32 weeks 46. Of note, in preterm infants <32 weeks of gestation, up to 23% of infants may have positive blood cultures for Ureaplasma spp. and positive PCR results in venous blood and/or cerebrospinal fluid samples 47. The clinical relevance of detecting Ureaplasma spp. in microbiological specimen remains subject of discussion. For reasons of low pathogenicity in children and adults and the very common isolation from genitourinary samples, controversy remains concerning the impact of Ureaplasma colonization on infection and inflammation-related morbidities 32.
In pregnancy, intrauterine detection of Ureaplasma spp. has been linked to choriodecidual and amniotic inflammation 48. Invasive diseases in preterm and term neonates have been associated with increased peripheral leukocyte counts, increased numbers of neutrophils in airways secretions, and characteristic changes in cerebrospinal fluid profiles 40. Clinical studies in preterm infants suggest an association of Ureaplasma respiratory tract colonization with bronchopulmonary inflammation and altered lung development 49. As far as systemic inflammation is concerned, some studies in preterm infants indicate inflammatory cytokine responses upon neonatal Ureaplasma infection 50, while others failed to correlate detection of Ureaplasma spp. with systemic inflammation 42.
Ureaplasma symptoms
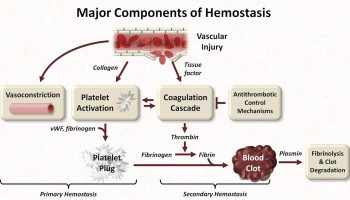
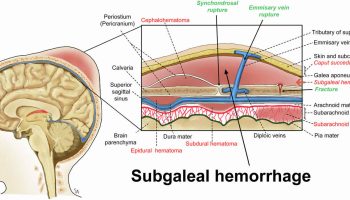
Chorioamnionitis presents as a febrile illness associated with an elevated white blood cell (WBC) count, uterine tenderness, abdominal pain, foul-smelling vaginal discharge, and fetal and maternal tachycardia. Diagnosing clinical chorioamnionitis includes a fever of at least 38 °C (100.4 °F) and one of the clinical symptoms or between 38 °C (100.4 °F) and 39 °C (102.2 °F) within 30 minutes. The majority of women presenting with chorioamnionitis are in labor or have ruptured membranes when it presents. Clinical chorioamnionitis and histological chorioamnionitis affect 1 to 4% and 23.6% of term births (37 to 42 weeks of gestation), respectively 51. However, it has been well established that the frequency and severity of chorioamnionitis are inversely related to gestational age at the time of delivery. In a study of 7,505 placentae from singleton pregnancies, Russell 52 reported that the frequency of chorioamnionitis in patients who delivered between 21 and 24 weeks of gestation was 94.4% (17/18 patients). More recently, Stoll et al. 53 demonstrated that histological chorioamnionitis was present in 70% (295/421) of pregnancies that delivered at 22 weeks of gestation. The frequency of histological chorioamnionitis was significantly higher in women who delivered after the spontaneous onset of labor than in those who had induction of labor at term or delivered via Caesarean section in the absence of labor 54. Furthermore, the frequency of histological chorioamnionitis increases in patients with prolonged duration of labor 55 and premature rupture of membranes 56. Additional risk factors for chorioamnionitis include multiple digital examinations, nulliparity, bacterial vaginosis, alcohol and tobacco use, group B Streptococcus colonization, meconium-stained amniotic fluid, and epidural anesthesia 56.
The diagnosis of chorioamnionitis is currently based on clinical signs coupled with histological and microbiological analysis of the placenta after delivery of the newborn. Histologic grading of the placenta is considered the gold standard for the diagnosis of chorioamnionitis; however, this retrospective diagnosis is not useful in informing patient management throughout pregnancy, especially in the absence of clinical signs. Several studies have investigated the diagnostic value of amniotic fluid and maternal serum biomarkers for the detection of chorioamnionitis in pregnant women undergoing amniocentesis. Elevated inflammatory markers such as interleukin 6 (IL-6), IL-8, matrix metalloproteinase 8 (MMP-8), MMP-9, and monocyte chemotactic proteins within amniotic fluid are positive predictors of intra-amniotic inflammation and/or clinical chorioamnionitis 57; however, these markers may have poor positive predictive values for the detection of subclinical, histologic chorioamnionitis and may be variably expressed within the amniotic fluid and fetal membranes during chorioamnionitis 58. Recently, Liu et al. 59 reported that surface-enhanced laser desorption ionization–time of flight mass spectrometry (SELDI-TOF-MS) for the detection of human neutrophil defensin 1 (HNP-1) and HNP-2 and calgranulins A and C within amniotic fluid was highly accurate for the diagnosis of subclinical chorioamnionitis, but further studies with larger patient cohorts are required to validate these findings. Noninflammatory markers such as amniotic fluid lactate dehydrogenase and glucose were also recently investigated for the detection of histologic chorioamnionitis 60, but the diagnostic accuracy of these assays was low, suggesting that additional amniotic fluid biomarkers should be investigated for the diagnosis of chorioamnionitis.
Chorioamnionitis: a major predictor of preterm birth
Preterm birth, defined as delivery at <37 weeks of gestation, is the leading cause of neonatal death worldwide 61. In addition, complications arising from preterm birth are a leading cause of death in children under the age of 5, second only to pneumonia 62. Microbiological studies have demonstrated that intrauterine infection may be responsible for 25 to 40% of preterm births 63; however, this is likely to be underreported due to difficulties in detecting fastidious microorganisms using conventional culture methods. Histological chorioamnionitis complicates 40 to 70% of all preterm births 64, suggesting that chorioamnionitis may be an important, and potentially preventable, antecedent of preterm birth.
Due to the difficulties associated with identifying and diagnosing Ureaplasma infections and chorioamnionitis, additional research should be undertaken to identify biomarkers for the rapid diagnosis of Ureaplasma in order to detect subclinical infections and clinically silent chorioamnionitis.
Ureaplasma treatment
The major difficulty in treating chorioamnionitis is that a large proportion of cases are clinically asymptomatic and therefore are not diagnosed until retrospective analysis of the placenta and fetal membranes. This is particularly problematic for the human Ureaplasma species, which can cause chronic, asymptomatic intrauterine infections that modulate the host immune response to prevent significant pathological events but are still associated with adverse outcomes. While antibiotics are recommended for women with preterm prelabor rupture of membranes 65 to prevent ascending invasive infections from the lower genital tract, the timing of administration may be too late to have beneficial effects against chronic Ureaplasma infections that were established in early/midgestation. It has been suggested that the administration of appropriate antibiotics before 22 weeks of gestation (or before inflammation and maternal-fetal damage occur) could significantly decrease the incidence of preterm birth 66. This is supported by a meta-analysis which demonstrated that the administration of macrolides and clindamycin during the second trimester of pregnancy was associated with a reduced risk of preterm delivery 67. However, due to concern about antibiotic resistance, widespread antimicrobial treatment is not recommended unless there is evidence of intra-amniotic infection. Culture and/or PCR detection of Ureaplasma species within amniotic fluid remains the gold standard for diagnosis; however, amniocentesis is an invasive procedure that is not routinely performed, and it is likely that high numbers of Ureaplasma infections during pregnancy remain undetected and therefore untreated.
An additional complicating factor for the treatment of Ureaplasma chorioamnionitis includes the often polymicrobial nature of this disease, which suggests that more than one antimicrobial agent may be required to successfully eradicate infection. Furthermore, treatment options for pregnant women are limited due to potential teratogenic and harmful effects associated with the use of some antimicrobials during pregnancy. Even fewer options are available for the treatment of intrauterine Ureaplasma infections, as these microorganisms are inherently resistant to beta-lactam and glycopeptide antibiotics (due to their lack of a cell wall), as well as trimethoprim and sulfonamides (as Ureaplasma species do not synthesize folic acid) 68. Antimicrobials that are potentially active against Ureaplasma include the tetracyclines, fluoroquinolones, and macrolides; however, resistance to these antimicrobial classes has also been well described 69.
Erythromycin, a 14-membered lactone ring macrolide, is the most common antibiotic used for the treatment of neonatal Ureaplasma infections and is routinely used in clinical obstetrics. Large randomized controls and meta-analyses have demonstrated that erythromycin administration for preterm prelabor rupture of membranes can reduce the risk of chorioamnionitis and neonatal morbidity and delay preterm birth 70. However, it is less clear if maternal erythromycin can eradicate existing human intrauterine infections due to conflicting reports within the literature 71. In pregnant sheep, maternal intramuscular erythromycin treatment (30 mg/kg of body weight/day for 4 days) failed to eradicate an erythromycin-susceptible strain of Ureaplasma parvum from the amniotic fluid, chorioamnion, and fetal lung 72, presumably due to poor transplacental passage 72. In a follow-up study, it was again demonstrated that intra-amniotic Ureaplasma infection was not eradicated following (i) single intra-amniotic and repeated maternal intramuscular erythromycin or (ii) single maternal intramuscular and repeated intra-amniotic erythromycin injections 73. These data suggest that erythromycin may not be beneficial for the treatment of intrauterine Ureaplasma infections.
Azithromycin is a 15-membered semisynthetic macrolide with superior tissue penetration, a prolonged half-life, and broader antimicrobial coverage than erythromycin 74. Azithromycin is well tolerated during pregnancy and achieves peak concentrations of 151 ± 46 ng/ml within human amniotic fluid and 2,130 ± 340 ng/ml within human placentae at 6 h postinjection, before rapidly declining 74. In pregnant sheep, a single intra-amniotic injection of azithromycin achieved therapeutic concentrations that were sustained for 48 h; however, there was poor maternal-fetal transfer 75. Despite this, a single maternal intravenous azithromycin injection or a single maternal intravenous azithromycin injection combined with an intra-amniotic azithromycin injection completely eradicated an established Ureaplasma parvum infection from the amniotic fluid, chorioamnion, and fetal lung in pregnant sheep 76. Similarly, studies in rhesus macaques demonstrated that maternal intravenous azithromycin (25 mg/kg/day for 10 days) administered 6 to 8 days after intra-amniotic Ureaplasma parvum inoculation successfully eradicated Ureaplasma from the amniotic fluid 77. It should be noted that in both of these sheep 76 and monkey 77 studies, histological evidence of chorioamnionitis was still observed at the time of delivery, suggesting that azithromycin treatment alone is not sufficient to reduce/eliminate inflammation within the fetal membranes.
Recent research efforts have evaluated a new, broad-spectrum fluoroketolide, solithromycin, in pregnant sheep and demonstrated that a single maternal dose can deliver therapeutic concentrations to both the fetus and the amniotic fluid 78. The transplacental transfer of solithromycin was significantly higher than that reported for other macrolides, including azithromycin, and a maternal intravenous infusion resulted in sustained therapeutic concentrations within maternal plasma, fetal plasma, and amniotic fluid for >12 h 78. In vitro, solithromycin has potent activity against human clinical Ureaplasma isolates 79, in addition to a range of other important pathogens 80. Both maternal intravenous solithromycin and maternal intravenous solithromycin combined with intra-amniotic solithromycin effectively eradicated Ureaplasma parvum from the amniotic cavity of pregnant sheep but, similarly to azithromycin, failed to reduce inflammation of the chorioamnion and fetal lung 76. These findings suggest that solithromycin may not accumulate in high-enough concentrations to exert anti-inflammatory effects and that coadministration of immune modulators should be investigated. To date, solithromycin is the most potent antimicrobial for the treatment of genital mycoplasmas and has several pharmacokinetic advantages over older macrolides, suggesting that it may be useful for the treatment of intrauterine infections. Human studies are required to further examine the effectiveness and safety of solithromycin in pregnancy and chorioamnionitis.
- The recovery of pleuropneumonia-like organisms from Negro men with and without nongonococcal urethritis. SHEPARD MC. Am J Syph Gonorrhea Vener Dis. 1954 Mar; 38(2):113-24.[↩][↩]
- SHEPARD MC. The recovery of pleuropneumonia-like organisms from Negro men with and without nongonococcal urethritis. Am J Syph Gonorrhea Vener Dis. 1954 Mar;38(2):113-24.[↩]
- Shepard MC, Lunceford CD, Ford DK, Purcell RH, Taylor-Robinson D, Razin S, Black FT. 1974. Ureaplasma urealyticum gen. nov., sp. nov.: proposed nomenclature for the human T (T-strain) mycoplasmas. Int J Syst Bacteriol 24:160–171. doi:10.1099/00207713-24-2-160[↩][↩]
- Hydrolysis of urea by Ureaplasma urealyticum generates a transmembrane potential with resultant ATP synthesis. Smith DG, Russell WC, Ingledew WJ, Thirkell D. J Bacteriol. 1993 Jun; 175(11):3253-8.[↩]
- Tully JG. 1983. Cloning and filtration techniques for mycoplasmas, p 173–177. In Razin S, editor. (ed), Methods in mycoplasmology, vol 1 Academic Press, Inc, New York, NY.[↩]
- Shepard MC, Masover GK. 1979. Special features of the ureaplasmas, p 452–494. In Barile MF, Razin S. (ed), The mycoplasmas, vol 1 Academic Press, Inc, New York, NY[↩]
- Robertson JA, Stemke GW, Davis JW Jr, Harasawa R, Thirkell D, Kong F, Shepard MC, Ford DK. 2002. Proposal of Ureaplasma parvum sp. nov. and emended description of Ureaplasma urealyticum (Shepard et al. 1974) Robertson et al. 2001. Int J Syst Evol Microbiol 52:587–597. doi: 10.1099/00207713-52-2-587[↩]
- Kim M, Kim G, Romero R, Shim SS, Kim EC, Yoon BH. 2003. Biovar diversity of Ureaplasma urealyticum in amniotic fluid: distribution, intrauterine inflammatory response and pregnancy outcomes. J Perinat Med 31:146–152. doi: 10.1515/JPM.2003.020[↩]
- Comparative genome analysis of 19 Ureaplasma urealyticum and Ureaplasma parvum strains. Paralanov V, Lu J, Duffy LB, Crabb DM, Shrivastava S, Methé BA, Inman J, Yooseph S, Xiao L, Cassell GH, Waites KB, Glass JI. BMC Microbiol. 2012 May 30; 12():88.[↩]
- The phylogeny of Ureaplasma urealyticum based on the mba gene fragment. Knox CL, Giffard P, Timms P. Int J Syst Bacteriol. 1998 Oct; 48 Pt 4():1323-31.[↩]
- Ureaplasma urealyticum intrauterine infection: role in prematurity and disease in newborns. Cassell GH, Waites KB, Watson HL, Crouse DT, Harasawa R. Clin Microbiol Rev. 1993 Jan; 6(1):69-87.[↩][↩]
- Sweeney EL, Dando SJ, Kallapur SG, Knox CL. The Human Ureaplasma Species as Causative Agents of Chorioamnionitis. Clin Microbiol Rev. 2016 Dec 14;30(1):349-379. doi: 10.1128/CMR.00091-16[↩][↩][↩]
- Oh KJ, Lee KA, Sohn YK, Park CW, Hong JS, Romero R, Yoon BH. 2010. Intraamniotic infection with genital mycoplasmas exhibits a more intense inflammatory response than intraamniotic infection with other microorganisms in patients with preterm premature rupture of membranes. Am J Obstet Gynecol 203:211.e1–211.e8. doi: 10.1016/j.ajog.2010.03.035[↩]
- Oh KJ, Romero R, Park JY, Hong JS, Yoon BH. 2019. The earlier the gestational age, the greater the intensity of the intra-amniotic inflammatory response in women with preterm premature rupture of membranes and amniotic fluid infection by Ureaplasma species. J Perinat Med 47:516–527. doi: 10.1515/jpm-2019-0003[↩]
- Gerber S, Vial Y, Hohlfeld P, Witkin SS. 2003. Detection of Ureaplasma urealyticum in second-trimester amniotic fluid by polymerase chain reaction correlates with subsequent preterm labor and delivery. J Infect Dis 187:518–521. doi: 10.1086/368205[↩]
- Gravett MG, Witkin SS, Haluska GJ, Edwards JL, Cook MJ, Novy MJ. 1994. An experimental model for intraamniotic infection and preterm labor in rhesus monkeys. Am J Obstet Gynecol 171:1660–1667. doi: 10.1016/0002-9378(94)90418-9[↩]
- Novy MJ, Duffy L, Axthelm MK, Sadowsky DW, Witkin SS, Gravett MG, Cassell GH, Waites KB. 2009. Ureaplasma parvum or Mycoplasma hominis as sole pathogens cause chorioamnionitis, preterm delivery, and fetal pneumonia in rhesus macaques. Reprod Sci 16:56–70. doi: 10.1177/1933719108325508[↩]
- Senthamaraikannan P, Presicce P, Rueda CM, Maneenil G, Schmidt AF, Miller LA, Waites KB, Jobe AH, Kallapur SG, Chougnet CA. 2016. Intra-amniotic Ureaplasma parvum-induced maternal and fetal inflammation and immune responses in rhesus macaques. J Infect Dis 214:1597–1604. doi: 10.1093/infdis/jiw408[↩]
- Normann E, Lacaze-Masmonteil T, Eaton F, Schwendimann L, Gressens P, Thébaud B. 2009. A novel mouse model of Ureaplasma-induced perinatal inflammation: effects on lung and brain injury. Pediatr Res 65:430–436. doi: 10.1203/PDR.0b013e31819984ce[↩]
- Motomura K, Romero R, Xu Y, Theis KR, Galaz J, Winters AD, Slutsky R, Garcia-Flores V, Zou C, Levenson D, Para R, Ahmad MM, Miller D, Hsu CD, Gomez-Lopez N. Intra-Amniotic Infection with Ureaplasma parvum Causes Preterm Birth and Neonatal Mortality That Are Prevented by Treatment with Clarithromycin. mBio. 2020 Jun 23;11(3):e00797-20. doi: 10.1128/mBio.00797-20[↩]
- Genital tract colonization with Ureaplasma spp. and its association with abnormal vaginal flora. Vancutsem E, Faron G, Foulon W, Naessens A. J Med Microbiol. 2015 Jun; 64(6):654-6.[↩]
- Ureaplasma parvum and Ureaplasma urealyticum are detected in semen after washing before assisted reproductive technology procedures. Knox CL, Allan JA, Allan JM, Edirisinghe WR, Stenzel D, Lawrence FA, Purdie DM, Timms P. Fertil Steril. 2003 Oct; 80(4):921-9.[↩]
- Vaginal and endocervical microorganisms in symptomatic and asymptomatic non-pregnant females: risk factors and rates of occurrence. Tibaldi C, Cappello N, Latino MA, Masuelli G, Marini S, Benedetto C. Clin Microbiol Infect. 2009 Jul; 15(7):670-9.[↩][↩]
- Ureaplasma parvum and Ureaplasma urealyticum detected with the same frequency among women with and without symptoms of urogenital tract infection. Marovt M, Keše D, Kotar T, Kmet N, Miljković J, Šoba B, Matičič M. Eur J Clin Microbiol Infect Dis. 2015 Jun; 34(6):1237-45.[↩][↩]
- The role of Ureaplasma urealyticum in adverse pregnancy outcome. Knox CL, Cave DG, Farrell DJ, Eastment HT, Timms P. Aust N Z J Obstet Gynaecol. 1997 Feb; 37(1):45-51.[↩][↩][↩]
- An intrauterine device as a possible cause of change in the microbial flora of the female genital system. Kaliterna V, Kučišec-Tepeš N, Pejković L, Zavorović S, Petrović S, Barišić Z. J Obstet Gynaecol Res. 2011 Aug; 37(8):1035-40.[↩]
- Detection of Ureaplasma biovars and polymerase chain reaction-based subtyping of Ureaplasma parvum in women with or without symptoms of genital infections. De Francesco MA, Negrini R, Pinsi G, Peroni L, Manca N. Eur J Clin Microbiol Infect Dis. 2009 Jun; 28(6):641-6.[↩]
- High bacterial loads of Ureaplasma may be associated with non-specific cervicitis. Liu L, Cao G, Zhao Z, Zhao F, Huang Y. Scand J Infect Dis. 2014 Sep; 46(9):637-41.[↩]
- Relationship of Ureaplasma urealyticum biovars to the presence or absence of bacterial vaginosis in pregnant women and to the time of delivery. Povlsen K, Thorsen P, Lind I. Eur J Clin Microbiol Infect Dis. 2001 Jan; 20(1):65-7.[↩]
- Isolation of genital mycoplasmas from the blood of neonates and women with pelvic infection using conventional SPS-free blood culture media. Kelly VN, Garland SM, Gilbert GL. Pathology. 1987 Jul; 19(3):277-80.[↩]
- Mycoplasma and ureaplasma colonisation in women with lower urinary tract symptoms. Latthe PM, Toozs-Hobson P, Gray J. J Obstet Gynaecol. 2008 Jul; 28(5):519-21.[↩]
- The Human Ureaplasma Species as Causative Agents of Chorioamnionitis. Sweeney EL, Dando SJ, Kallapur SG, Knox CL. Clin Microbiol Rev. 2017 Jan; 30(1):349-379.[↩][↩]
- Placental Infection With Ureaplasma species Is Associated With Histologic Chorioamnionitis and Adverse Outcomes in Moderately Preterm and Late-Preterm Infants. Sweeney EL, Kallapur SG, Gisslen T, Lambers DS, Chougnet CA, Stephenson SA, Jobe AH, Knox CL. J Infect Dis. 2016 Apr 15; 213(8):1340-7.[↩]
- Mycoplasma/Ureaplasma infection in pregnancy: to screen or not to screen. Donders GGG, Ruban K, Bellen G, Petricevic L. J Perinat Med. 2017 Jul 26; 45(5):505-515.[↩]
- Temporal and spatial variation of the human microbiota during pregnancy. DiGiulio DB, Callahan BJ, McMurdie PJ, Costello EK, Lyell DJ, Robaczewska A, Sun CL, Goltsman DS, Wong RJ, Shaw G, Stevenson DK, Holmes SP, Relman DA. Proc Natl Acad Sci U S A. 2015 Sep 1; 112(35):11060-5.[↩]
- Association between preterm birth and vaginal colonization by mycoplasmas in early pregnancy. Kataoka S, Yamada T, Chou K, Nishida R, Morikawa M, Minami M, Yamada H, Sakuragi N, Minakami H. J Clin Microbiol. 2006 Jan; 44(1):51-5.[↩]
- The prevalence of vaginal microorganisms in pregnant women with preterm labor and preterm birth. Choi SJ, Park SD, Jang IH, Uh Y, Lee A. Ann Lab Med. 2012 May; 32(3):194-200.[↩]
- Colonization of the lower urogenital tract with Ureaplasma parvum can cause asymptomatic infection of the upper reproductive system in women: a preliminary study. Kasprzykowska U, Elias J, Elias M, Mączyńska B, Sobieszczańska BM. Arch Gynecol Obstet. 2014 May; 289(5):1129-34.[↩]
- Difficulties experienced in defining the microbial cause of pelvic inflammatory disease. Taylor-Robinson D, Jensen JS, Svenstrup H, Stacey CM. Int J STD AIDS. 2012 Jan; 23(1):18-24.[↩]
- Neonatal CNS infection and inflammation caused by Ureaplasma species: rare or relevant? Glaser K, Speer CP. Expert Rev Anti Infect Ther. 2015 Feb; 13(2):233-48.[↩][↩]
- Association between pulmonary ureaplasma colonization and bronchopulmonary dysplasia in preterm infants: updated systematic review and meta-analysis. Lowe J, Watkins WJ, Edwards MO, Spiller OB, Jacqz-Aigrain E, Kotecha SJ, Kotecha S. Pediatr Infect Dis J. 2014 Jul; 33(7):697-702.[↩][↩][↩]
- Microbial load of umbilical cord blood Ureaplasma species and Mycoplasma hominis in preterm prelabor rupture of membranes. Kacerovsky M, Pliskova L, Menon R, Kutova R, Musilova I, Maly J, Andrys C. J Matern Fetal Neonatal Med. 2014 Nov; 27(16):1627-32.[↩][↩]
- Maternal genital colonization with Ureaplasma urealyticum promotes preterm delivery: association of the respiratory colonization of premature infants with chronic lung disease and increased mortality. Kafetzis DA, Skevaki CL, Skouteri V, Gavrili S, Peppa K, Kostalos C, Petrochilou V, Michalas S. Clin Infect Dis. 2004 Oct 15; 39(8):1113-22.[↩]
- Mycoplasmas and ureaplasmas as neonatal pathogens. Waites KB, Katz B, Schelonka RL. Clin Microbiol Rev. 2005 Oct; 18(4):757-89.[↩]
- A quantitative analysis of Ureaplasma urealyticum and Ureaplasma parvum compared with host immune response in preterm neonates at risk of developing bronchopulmonary dysplasia. Payne MS, Goss KC, Connett GJ, Legg JP, Bruce KD, Chalker V. J Clin Microbiol. 2012 Mar; 50(3):909-14.[↩]
- Frequency of ureaplasma serovars in respiratory secretions of preterm infants at risk for bronchopulmonary dysplasia. Sung TJ, Xiao L, Duffy L, Waites KB, Chesko KL, Viscardi RM. Pediatr Infect Dis J. 2011 May; 30(5):379-83.[↩]
- The Alabama Preterm Birth Study: umbilical cord blood Ureaplasma urealyticum and Mycoplasma hominis cultures in very preterm newborn infants. Goldenberg RL, Andrews WW, Goepfert AR, Faye-Petersen O, Cliver SP, Carlo WA, Hauth JC. Am J Obstet Gynecol. 2008 Jan; 198(1):43.e1-5.[↩]
- The impact of the microbial load of genital mycoplasmas and gestational age on the intensity of intraamniotic inflammation. Kacerovsky M, Pliskova L, Bolehovska R, Skogstrand K, Hougaard DM, Tsiartas P, Jacobsson B. Am J Obstet Gynecol. 2012 Apr; 206(4):342.e1-8[↩]
- Antenatal Ureaplasma urealyticum respiratory tract infection stimulates proinflammatory, profibrotic responses in the preterm baboon lung. Viscardi RM, Atamas SP, Luzina IG, Hasday JD, He JR, Sime PJ, Coalson JJ, Yoder BA. Pediatr Res. 2006 Aug; 60(2):141-6.[↩]
- Ureaplasma species: role in neonatal morbidities and outcomes. Viscardi RM. Arch Dis Child Fetal Neonatal Ed. 2014 Jan; 99(1):F87-92.[↩]
- Tita AT, Andrews WW. 2010. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol 37:339–354. doi:10.1016/j.clp.2010.02.003.[↩]
- Russell P. 1979. Inflammatory lesions of the human placenta: clinical significance of acute chorioamnionitis. Am J Diagn Gynecol Obstet 2:127–137[↩]
- Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sanchez PJ, O’Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID III, Watterberg KL, Saha S, Das A, Higgins RD. 2010. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126:443–456. doi:10.1542/peds.2009-2959[↩]
- Park HS, Romero R, Lee SM, Park CW, Jun JK, Yoon BH. 2010. Histologic chorioamnionitis is more common after spontaneous labor than after induced labor at term. Placenta 31:792–795. doi:10.1016/j.placenta.2010.06.013[↩]
- Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. 2014. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol 124:57–67. doi:10.1097/AOG.0000000000000278[↩]
- Rickert VI, Wiemann CM, Hankins GD, McKee JM, Berenson AB. 1998. Prevalence and risk factors of chorioamnionitis among adolescents. Obstet Gynecol 92:254–257. doi:10.1016/S0029-7844(98)00135-5[↩][↩]
- Chaemsaithong P, Romero R, Korzeniewski SJ, Martinez-Varea A, Dong Z, Yoon BH, Hassan SS, Chaiworapongsa T, Yeo L. 2016. A point of care test for interleukin-6 in amniotic fluid in preterm prelabor rupture of membranes: a step toward the early treatment of acute intra-amniotic inflammation/infection. J Matern Fetal Neonatal Med 29:360–367. doi:10.3109/14767058.2015.1006621[↩]
- Bhat G, Peltier MR, Syed TA, Drobek CO, Saade G, Menon R. 2013. Fetal membrane biomarker network diversity and disease functions induced by intra-amniotic pathogens. Am J Reprod Immunol 69:124–133. doi:10.1111/aji.12047[↩]
- Liu Y, Liu Y, Du C, Zhang R, Feng Z, Zhang J. 2016. Diagnostic value of amniotic fluid inflammatory biomarkers for subclinical chorioamnionitis. Int J Gynaecol Obstet 134:160–164. doi:10.1016/j.ijgo.2016.01.007[↩]
- Myntti T, Rahkonen L, Tikkanen M, Patari-Sampo A, Paavonen J, Stefanovic V. 2016. Amniotic fluid rapid biomarkers are associated with intra-amniotic infection in preterm pregnancies regardless of the membrane status. J Perinatol 36:606–611. doi:10.1038/jp.2016.59[↩]
- Howson CP, Kinney MV, McDougall L, Lawn JE. 2013. Born too soon: preterm birth matters. Reprod Health 10(Suppl 1):S1. doi:10.1186/1742-4755-10-S1-S1.[↩]
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE. 2012. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161. doi:10.1016/S0140-6736(12)60560-1[↩]
- Goldenberg RL, Hauth JC, Andrews WW. 2000. Intrauterine infection and preterm delivery. N Engl J Med 342:1500–1507. doi:10.1056/NEJM200005183422007[↩]
- Tita AT, Andrews WW. 2010. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol 37:339–354. doi:10.1016/j.clp.2010.02.003[↩]
- Yudin MH, van Schalkwyk J, Van Eyk N, Boucher M, Castillo E, Cormier B, Gruslin A, Money DM, Murphy K, Ogilvie G, Paquet C, Steenbeek A, Wong T, Gagnon R, Hudon L, Basso M, Bos H, Delisle MF, Farine D, Grabowska K, Menticoglou S, Mundle WR, Murphy-Kaulbeck LC, Ouellet A, Pressey T, Roggensack A. 2009. Antibiotic therapy in preterm premature rupture of the membranes. J Obstet Gynaecol Can 31:863–874. doi:10.1016/S1701-2163(16)34305-5[↩]
- Lamont RF, Jaggat AN. 2007. Emerging drug therapies for preventing spontaneous preterm labor and preterm birth. Expert Opin Invest Drugs 16:337–345. doi:10.1517/13543784.16.3.337[↩]
- Morency AM, Bujold E. 2007. The effect of second-trimester antibiotic therapy on the rate of preterm birth. J Obstet Gynaecol Can 29:35–44. doi:10.1016/S1701-2163(16)32350-7[↩]
- Waites KB, Katz B, Schelonka RL. 2005. Mycoplasmas and ureaplasmas as neonatal pathogens. Clin Microbiol Rev 18:757–789. doi:10.1128/CMR.18.4.757-789.2005[↩]
- Fernandez J, Karau MJ, Cunningham SA, Greenwood-Quaintance KE, Patel R. 2016. Antimicrobial susceptibility and clonality of clinical ureaplasma isolates in the United States. Antimicrob Agents Chemother 60:4793–4798. doi:10.1128/AAC.00671-16[↩]
- Kenyon S, Boulvain M, Neilson J. 2004. Antibiotics for preterm rupture of the membranes: a systematic review. Obstet Gynecol 104:1051–1057. doi:10.1097/01.AOG.0000143268.36682.21[↩]
- Gomez R, Romero R, Nien JK, Medina L, Carstens M, Kim YM, Espinoza J, Chaiworapongsa T, Gonzalez R, Iams JD, Rojas I. 2007. Antibiotic administration to patients with preterm premature rupture of membranes does not eradicate intra-amniotic infection. J Matern Fetal Neonatal Med 20:167–173. doi:10.1080/14767050601135485[↩]
- Dando SJ, Nitsos I, Newnham JP, Jobe AH, Moss TJ, Knox CL. 2010. Maternal administration of erythromycin fails to eradicate intrauterine ureaplasma infection in an ovine model. Biol Reprod 83:616–622. doi:10.1095/biolreprod.110.084954[↩][↩]
- Kemp MW, Miura Y, Payne MS, Watts R, Megharaj S, Jobe AH, Kallapur SG, Saito M, Spiller OB, Keelan JA, Newnham JP. 2014. Repeated maternal intramuscular or intraamniotic erythromycin incompletely resolves intrauterine Ureaplasma parvum infection in a sheep model of pregnancy. Am J Obstet Gynecol 211:134.e1–134.e9. doi:10.1016/j.ajog.2014.02.025[↩]
- Ramsey PS, Vaules MB, Vasdev GM, Andrews WW, Ramin KD. 2003. Maternal and transplacental pharmacokinetics of azithromycin. Am J Obstet Gynecol 188:714–718. doi:10.1067/mob.2003.141[↩][↩]
- Keelan JA, Nitsos I, Saito M, Musk GC, Kemp MW, Timmins M, Li S, Yaegashi N, Newnham JP. 2011. Maternal-amniotic-fetal distribution of macrolide antibiotics following intravenous, intramuscular, and intraamniotic administration in late pregnant sheep. Am J Obstet Gynecol 204:546.e10–546.e17. doi:10.1016/j.ajog.2011.02.035[↩]
- Miura Y, Payne MS, Keelan JA, Noe A, Carter S, Watts R, Spiller OB, Jobe AH, Kallapur SG, Saito M, Stock SJ, Newnham JP, Kemp MW. 2014. Maternal intravenous treatment with either azithromycin or solithromycin clears Ureaplasma parvum from the amniotic fluid in an ovine model of intrauterine infection. Antimicrob Agents Chemother 58:5413–5420. doi:10.1128/AAC.03187-14[↩][↩][↩]
- Grigsby PL, Novy MJ, Sadowsky DW, Morgan TK, Long M, Acosta E, Duffy LB, Waites KB. 2012. Maternal azithromycin therapy for ureaplasma intraamniotic infection delays preterm delivery and reduces fetal lung injury in a primate model. Am J Obstet Gynecol 207:475.e1–475.e14. doi:10.1016/j.ajog.2012.10.871[↩][↩]
- Keelan JA, Kemp MW, Payne MS, Johnson D, Stock SJ, Saito M, Fernandes P, Newnham JP. 2014. Maternal administration of solithromycin, a new, potent, broad-spectrum fluoroketolide antibiotic, achieves fetal and intra-amniotic antimicrobial protection in a pregnant sheep model. Antimicrob Agents Chemother 58:447–454. doi:10.1128/AAC.01743-13[↩][↩]
- Furfaro LL, Spiller OB, Keelan JA, Payne MS. 2015. In vitro activity of solithromycin and its metabolites, CEM-214 and N-acetyl-CEM-101, against 100 clinical Ureaplasma spp. isolates compared with azithromycin. Int J Antimicrob Agents 46:319–324. doi:10.1016/j.ijantimicag.2015.04.015[↩]
- Farrell DJ, Flamm RK, Sader HS, Jones RN. 2016. Results from the Solithromycin International Surveillance Program (2014). Antimicrob Agents Chemother 60:3662–3668. doi:10.1128/AAC.00185-16[↩]