Contents
- What is urethritis
- Gonococcal urethritis
- Non-gonococcal urethritis
- Urethritis causes
- Urethritis prevention
- Urethritis symptoms
- Urethritis possible complications
- Urethritis diagnosis
- Urethritis treatment
- Urethritis prognosis
What is urethritis
Urethritis is inflammation of the urethra, the tube that carries urine from the bladder out of the body. Urethritis can be infectious or non-infectious 1. Infectious causes almost always sexually transmitted. Sexually transmitted urethritis is traditionally divided into 2 categories: gonococcal urethritis and non-gonococcal urethritis 2. Since almost all urethritis patients have penile discharge, gonococcal urethritis can easily be distinguished from non-gonococcal urethritis by looking for gram-negative diplococci on a gram stain. If diplococci are identified, the urethritis is gonococcal; if no diplococci are identified, the diagnosis is classified as non-gonococcal urethritis 3.
Important facts
- Urethritis is typically a sexually transmitted infection with most cases caused by gonorrhea, chlamydia, and mycoplasma 4.
- Typical presentation includes dysuria and penile discharge.
- Diagnosis is based on positive discharge on an exam or more than 2 white blood cells seen on microscopy or presence of leukocytes on urinalysis (or 10 white blood cells on first-void urine catch).
- Initial empiric treatment should be started at the time of diagnosis. Treatment for non-gonococcal urethritis when gonococcal infection can be rule out based on microscope examination includes azithromycin 1 g orally once or doxycycline 100 mg twice per day for 7 days. If a gonococcal infection cannot be ruled out treatment should add ceftriaxone 250 mg intramuscularly once to cover for gonococcal infection 4.
- Patients should be instructed to avoid sex for 1 week and until partners are treated 4.
- Partners should be tested and treated for urethritis 4.
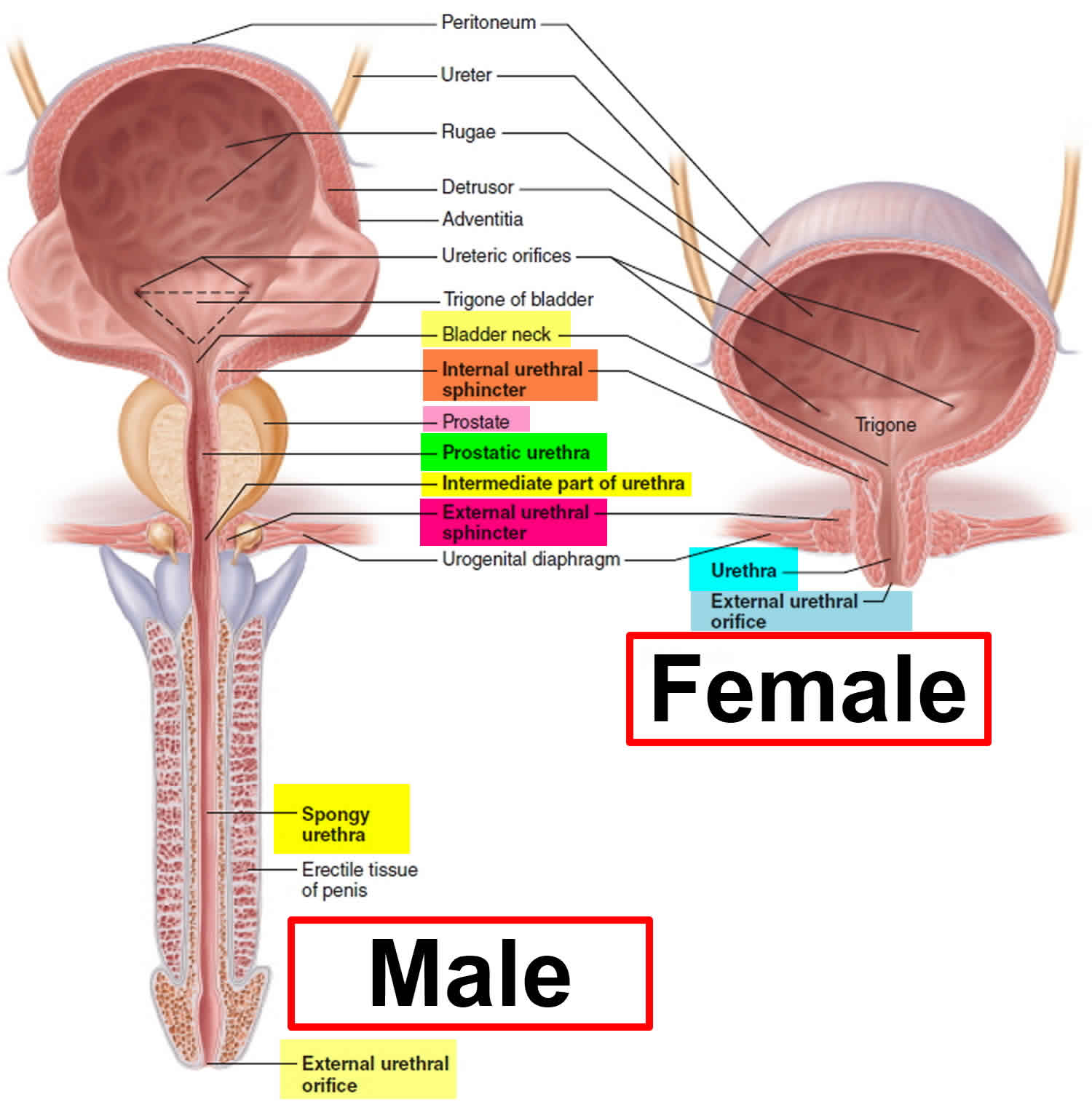
Figure 1. Male and Female Urethra
Gonococcal urethritis
Gonorrhea is a sexually transmitted infection (sexually transmitted disease) caused by bacteria called Neisseria gonorrhoeae or gonococcus. Gonorrhea used to be known as “the clap”. The Neisseria gonorrhoeae bacteria are mainly found in discharge from the penis and in vaginal fluid.
Gonorrhea is easily passed between people through:
- unprotected vaginal, oral or anal sex
- sharing vibrators or other sex toys that have not been washed or covered with a new condom each time they’re used
The bacteria can infect the entrance to the womb (cervix), the tube that passes urine out of the body (urethra), the rectum and, less commonly, the throat or eyes.
The infection can also be passed from a pregnant woman to her baby. If you’re pregnant and may have gonorrhea, it’s important to get tested and treated before your baby is born.
Without treatment, gonorrhea can cause permanent blindness in a newborn baby.
Gonorrhea is not spread by kissing, hugging, swimming pools, toilet seats, or sharing baths, towels, cups, plates or cutlery. The bacteria cannot survive outside the human body for long.
It’s important to be tested for gonorrhea if you think there’s a chance you’re infected, even if you have no obvious symptoms or the symptoms have gone away on their own.
If gonorrhea is left undiagnosed and untreated, you can continue to spread the infection and there’s a risk of potentially serious complications, including infertility.
Symptoms of gonorrhea
Typical symptoms of gonorrhea include a thick green or yellow discharge from the vagina or penis, pain when urinating and, in women, bleeding between periods. However, around 1 in 10 infected men and 5 in 10 infected women do not experience any symptoms, which means the condition can go untreated for some time.
Symptoms of gonorrhea usually develop within about 2 weeks of being infected, although they sometimes do not appear until many months later.
Gonorrhea symptoms in women
In women, symptoms of gonorrhea can include:
- an unusual vaginal discharge, which may be thin or watery and green or yellow in color
- pain or a burning sensation when passing urine
- pain or tenderness in the lower abdominal area – this is less common
- bleeding between periods, heavier periods and bleeding after sex – this is less common
Gonorrhea symptoms in men
In men, symptoms of gonorrhea can include:
- an unusual discharge from the tip of the penis, which may be white, yellow or green
- pain or a burning sensation when urinating
- inflammation (swelling) of the foreskin
- pain or tenderness in the testicles – this is rare
Infection in the rectum, throat or eyes
Both men and women can develop an infection in the rectum, throat or eyes by having unprotected anal or oral sex.
If infected semen or vaginal fluid comes into contact with the eyes, you can also develop conjunctivitis.
Infection in the rectum can cause discomfort, pain or discharge. Infection in the eyes can cause irritation, pain, swelling and discharge, and infection in the throat usually causes no symptoms.
Gonorrhea in babies
Gonorrhea can be passed from a mother to her baby during childbirth. Newborn babies normally show symptoms in their eyes during the first 2 weeks. The eyes become red and swollen, and have a thick, pus-like discharge.
Gonorrhea can be treated with antibiotics when you’re pregnant or when you’re breastfeeding. The antibiotics won’t harm your baby.
Gonorrhea prevention
Gonorrhea and other sexually transmitted infections can be successfully prevented by using appropriate contraception and taking other precautions, such as:
- using male condoms or female condoms every time you have vaginal sex, or male condoms during anal sex
- using a condom to cover the penis or a latex or plastic square (dam) to cover the female genitals if you have oral sex
- not sharing sex toys, or washing them and covering them with a new condom before anyone else uses them
Gonorrhea complications
If treated early, gonorrhea is unlikely to lead to any complications or long-term problems. However, without treatment, it can spread to other parts of your body and cause serious problems.
The more times you have gonorrhea, the more likely you are to have complications.
In women, gonorrhea can spread to the reproductive organs and cause pelvic inflammatory disease (PID). This is estimated to occur in 10 to 20% cases of untreated gonorrhea. Pelvic inflammatory disease can lead to long-term pelvic pain, ectopic pregnancy and infertility.
During pregnancy, gonorrhea can cause:
- miscarriage
- premature labor
- the baby being born with conjunctivitis
If the baby is not promptly treated with antibiotics, there’s a risk of progressive and permanent vision damage.
In men, gonorrhea can cause a painful infection in the testicles and prostate gland, which may lead to reduced fertility in a small number of cases.
In rare cases, when gonorrhea has been left untreated, it can spread through the bloodstream and cause life-threatening infections in other parts of the body (sepsis).
Gonorrhea diagnosis
The only way to find out if you have gonorrhea is to be tested. If you suspect gonorrhea or any other sexually transmitted infection (STI), it’s important not to delay getting tested.
It’s possible to be tested within a few days of having sex, but you may be advised to wait up to a week. You can be tested even if you do not have any symptoms.
Early diagnosis and treatment of gonorrhea reduces the risk of complications developing, such as pelvic inflammatory disease (PID) or infection in the testicles. Complications that arise from long-term infection are much more difficult to treat.
Testing for gonorrhea
There are a number of different ways to test for gonorrhea. In many cases, a swab will be used to remove a sample for testing, although men may only be asked to provide a urine sample.
A swab looks a bit like a cotton bud, but it’s smaller and rounded. It’s wiped over parts of the body that may be infected to pick up samples of discharge. This only takes a few seconds and is not painful, although it may be a little uncomfortable.
Testing for women
For women, a doctor or nurse will usually take a swab to collect a sample from the vagina or cervix (entrance to the womb) during an internal examination. In some cases, a sample may also be taken from the urethra (the tube that carries urine out of the body).
Sometimes, you may be asked to use a swab or tampon to collect a sample from inside your vagina yourself.
Women are not usually asked to provide a urine sample to check for gonorrhea because this is a less-accurate test for women.
Testing for men
Men will normally be asked to provide a urine sample or a swab may be used to pick up a sample of discharge from the end of the penis.
If you’re asked to provide a urine sample, it’s important not to urinate for about 2 hours beforehand because this can wash the bacteria away and affect the results of the test.
Infections of the rectum, throat and eyes
If there’s a possibility that your rectum or throat is infected, the doctor or nurse may need to use a swab to collect a sample from these areas.
If you have symptoms of conjunctivitis, such as red, inflamed eyes with discharge, a sample of the discharge may be collected from your eye.
Who should get tested for gonorrhea
It’s recommended you get tested if:
- you or your partner think you have symptoms of gonorrhea
- you’ve had unprotected sex with a new partner
- you or your partner have had unprotected sex with other people
- you have another sexually transmitted infection (sexually transmitted disease)
- a sexual partner tells you they have an sexually transmitted infection (sexually transmitted disease)
- during a vaginal examination, your nurse or doctor tells you the cells of your cervix are inflamed or there’s discharge
- you’re pregnant or planning a pregnancy
Treating gonorrhea
Gonorrhea is usually treated with a single antibiotic injection (usually in the buttocks or thigh) followed by 1 antibiotic tablet. It’s sometimes possible to have another antibiotic tablet instead of an injection, if you prefer. With effective treatment, most of your symptoms should improve within a few days, although it may take up to 2 weeks for any pain in your pelvis or testicles to disappear completely.
Bleeding between periods or heavy periods should improve by the time of your next period.
Antibiotics are usually recommended if:
- tests have shown you have gonorrhea
- there’s a high chance you have gonorrhea, even though your test results have not come back yet
- your partner has been diagnosed with gonorrhea
It’s usually recommended you attend a follow-up appointment a week or two after treatment so another test can be carried out to see if you’re clear of infection.
You should avoid having sex until you, and your partner, have been treated and given the all-clear, to prevent re-infection or passing the infection on to anyone else.
If your symptoms do not improve after treatment or you think you’ve been infected again, see your doctor or nurse. You may need repeat treatment or further tests to check for other problems.
Previous successful treatment for gonorrhea does not make you immune to catching it again.
It’s important that your current partner and any other recent sexual partners are tested and treated.
Treating babies with gonorrhea
Babies with signs of a gonorrhea infection at birth, or who have an increased risk of infection because their mother has gonorrhea, will usually be given antibiotics immediately after they’re born.
This does not harm the baby, and helps prevent blindness and other complications of gonorrhea.
Non-gonococcal urethritis
The term non-gonococcal urethritis is used when the urethritis isn’t caused by the sexually transmitted infection gonorrhea. Non-gonococcal urethritis is the most common sexually transmitted illness in men 1.
The most common cause of non-gonococcal urethritis is Chlamydia trachomatis, which accounts for 15% to 40% of non-gonococcal urethritis cases 3. The second most common cause is Mycoplasma genitalium, which accounts for 15% to 20% of non-gonococcal urethritis cases; although widespread testing for mycoplasma is not available 5. Less common causes of non-gonococcal urethritis include infection with Trichomonas vaginalis, herpes simplex virus, Epstein Barr virus, and Adenovirus. Enteric bacteria is an uncommon cause of non-gonococcal urethritis that is typically seen in males who practice insertive anal intercourse. In almost half of all cases of non-gonococcal urethritis, an etiology is not identified 3. Non-gonococcal urethritis is sometimes referred to as non-specific urethritis when no cause can be found.
Non-gonococcal urethritis causes
Non-gonococcal urethritis can have a number of possible causes, such as an infection, irritation or damage to the urethra.
There are also many cases where no cause is found – this is sometimes known as non-specific urethritis (NSU).
Sexually transmitted infections (STIs)
If urethritis is caused by gonorrhea, it is known as gonococcal urethritis (see above).
non-gonococcal urethritis can also be caused by other sexually transmitted infections (STIs), such as chlamydia. Chlamydia is spread during unprotected sex (sex without a condom), including anal and oral sex.
Urethritis is more common among people who are at risk of sexually transmitted infections. This includes people who:
- are sexually active
- have had unprotected sex
- have recently had a new sexual partner
Other infections
A number of other infections can cause non-gonococcal urethritis. These are caused by other bacteria that usually live harmlessly in the throat, mouth or rectum.
These bacteria can cause non-gonococcal urethritis if they get into the urethra, which is the tube that carries urine from the bladder to the outside of the body. This can occur during oral or anal sex.
Infections that can cause non-gonococcal urethritis include:
- Trichomonas vaginalis – an sexually transmitted infection caused by a tiny parasite
- Mycoplasma genitalium – tests for this condition have only recently been developed and are not available in all clinics yet; if you can’t be tested, you will be treated as though you might have it
- Urinary tract infection
- Herpes simplex virus (HSV) – this can also cause cold sores and genital herpes
- Adenovirus – usually causes a sore throat or an eye infection
Non-infectious causes
It’s possible for non-gonococcal urethritis to have a non-infectious cause. This is when something else leads to the urethra becoming inflamed.
Non-infectious causes of non-gonococcal urethritis include:
- irritation from a product used in the genital area – such as soap, deodorant or spermicide
- damage to the urethra caused by vigorous sex or masturbation, or by frequently squeezing the urethra – some men may do this if they’re worried they have an infection
- damage to the urethra caused by inserting an object into it, such as a catheter – this can be done during an operation in hospital
Non-gonococcal urethritis prevention
As non-gonococcal urethritis is usually caused by an sexually transmitted infection, practising safer sex is the best way to reduce the chances of it developing.
Non-gonococcal urethritis symptoms
Patients present with complaints of dysuria, pruritus, penile burning, and urethral discharge. Urethral discharge can be purulent, mucoid or watery. Discharge in non-gonococcal urethritis is sometimes scant and only noted as crusting at the meatus or staining of the underwear.
Not all men with urethritis have symptoms, and over 40% of cases of all cases of non-gonococcal urethritis are asymptomatic 6.
Patients who present with regional lymphadenopathy, constitutional symptoms, or vesicles may have urethritis from HSV (herpes simplex virus) non-gonococcal urethritis.
Physical examination may reveal penile discharge. Differentiating between gonococcal and non-gonococcal urethritis is difficult based on clinical examination of discharge. non-gonococcal urethritis tends to be mucoid or clear, compared to gonococcal urethritis which is more commonly purulent; however, this generalization is not reliable.
Men with urethritis can also present with fever, testicular pain, testicular swelling, sore throat, rectal pain, or rectal discharge. Differential diagnoses of these symptoms would include other infectious processes such as epididymitis, pharyngitis, or prostatitis, and these should be considered accordingly.
Conjunctivitis can accompany urethritis caused by gonorrhea, chlamydia, or adenovirus.
Some patients with non-gonococcal urethritis can also present with reactive arthritis, which is characterized by urethritis, uveitis, and arthritis. This constellation of symptoms is typically associated with the HLA-B27 gene 2.
Symptoms of non-gonococcal urethritis in men
Symptoms of non-gonococcal urethritis in men include:
- a white or cloudy discharge from the tip of the penis
- a burning or painful sensation when you pee
- the tip of your penis feeling irritated and sore
Depending on the cause of non-gonococcal urethritis, symptoms may begin a few weeks or several months after an infection.
If non-gonococcal urethritis has a non-infectious cause, such as irritation to the urethra, symptoms may begin after a couple of days.
Symptoms that start a day or two after sex are not usually caused by an sexually transmitted infection, but testing for sexually transmitted infections is still recommended.
Symptoms of non-gonococcal urethritis in women
In women, non-gonococcal urethritis rarely causes any symptoms. However, the infections that cause non-gonococcal urethritis in men can spread to other parts of the female reproductive system – for example, the womb or fallopian tubes, which connect the ovaries to the womb.
If the infection does spread, a woman may develop pelvic inflammatory disease (PID).
Pelvic inflammatory disease is a serious health condition that can cause persistent pain. Repeated episodes of pelvic inflammatory disease are associated with an increased risk of infertility.
Some women with pelvic inflammatory disease (PID) don’t have symptoms. If there are symptoms, they include:
- pain around the pelvis or lower part of your stomach (abdomen)
- discomfort or pain during sexual intercourse that is felt deep inside the pelvis
- bleeding between periods and after sex
- pain when you urinate
- heavy or painful periods
- unusual vaginal discharge – especially if it is yellow or green
A few women with pelvic inflammatory disease (PID) become very ill with:
- severe lower abdominal pain
- a fever (high temperature) of 100.4 °F (38 °C) or above
- nausea and vomiting
Non-gonococcal urethritis complications
Complications for non-gonococcal urethritis in men are rare but include epididymitis, prostatitis, abscess formation, and reactive arthritis. One percent to 2% of males with non-gonococcal urethritis develop epididymitis. One percent to 2% develop conjunctivitis. Urethral stricture or stenosis is possible after non-gonococcal urethritis due to post inflammatory scar formation but is rare.
Complications in women are more common than in men (10% to 40%). Women with urethritis can potentially develop pelvic inflammatory disease, infertility, and ectopic pregnancy 7.
Children born to mothers with chlamydia urethritis can potentially develop complications including conjunctivitis, iritis, and pneumonia. Routine treatment of all newborns with antibiotic eye ointment has significantly decreased the incidence of these 8.
Chlamydia urethritis can also cause lymphogranuloma venereum, a genital ulcer disease which presents as lymphadenitis or lymphangitis and can lead to lymphatic obstruction, strictures or fistulas 2.
Non-gonococcal urethritis diagnosis
The diagnosis of non-gonococcal urethritis requires the exclusion of gonorrheal infection. This can be achieved with a gram stain that lacks gram-negative diplococci or by any negative gonorrhea test (culture, nucleic acid testing, among others) 9.
In men at high risk for infection, if symptoms are present but none of these criteria are met, a presumptive diagnosis can be made, and empiric treatment started. These patients should be treated with a drug regimen for both chlamydia and gonorrhea 10.
Patients should also have a nucleic acid amplification test (NAAT) performed for chlamydia, gonorrhea, and trichomoniasis. In urethritis, NAAT testing is recommended over culture because of its high sensitivity and specificity. NAAT testing for M. genitalium exists but is not widely available 2.
Non-gonococcal urethritis treatment
Empiric treatment for urethritis should be started at the time of diagnosis, before results of testing for a specific cause. Treatment should be based on whether the gonococcal infection has been evaluated by microscope:
Presumptive Treatment of non-gonococcal urethritis with Microscope
Recommended Regimens
- Azithromycin 1 g orally in a single dose, or
- Doxycycline 100 mg orally twice a day for 7 days
Azithromycin and doxycycline are both highly effective for the treatment for chlamydial urethritis. Urethritis associated with M. genitalium responds better to azithromycin, although azithromycin resistance is increasing.
Presumptive Treatment of non-gonococcal urethritis without Microscope
When Gram stain is not available gonorrheal infection cannot be ruled out. These patients should be treated with a drug regimen effective against both chlamydia and gonorrhea.
Recommended Regimens
- Ceftriaxone 250 mg IM
PLUS
- Azithromycin 1 g orally in a single dose, or
- Doxycycline 100 mg orally twice a day for 7 days
Patient education
- Patients should abstain from sexual activity for 7 days, starting after the completion of therapy for the patient and all partners
- 2.
- Patients taking doxycycline should be advised to reduce sun exposure, as doxycycline can cause photosensitivity 11.
- Patients taking metronidazole should be advised to avoid alcoholic beverages.
Recurrent or Persistent non-gonococcal urethritis
Recurrent or persistent symptoms can be common following treatment for non-gonococcal urethritis with the recommended regimen. Patients should first be evaluated for adherence to prior treatment and re-exposure to disease. If they continue to have evidence of urethritis (discharge on exam, elevated WBC on a microscope, or leukocyte esterase on urinalysis) therapy should be directed towards M. genitalium. M. genitalium is the most common cause of persistent or recurrent non-gonococcal urethritis.
Recommended Regimens
- If azithromycin was not used for initial exposure: Azithromycin 1 g orally once
- If azithromycin was used for initial exposure: Moxifloxacin 400 mg orally daily for 7 days
- In either instance, metronidazole 2 g orally once should be given in areas where Trichomonas vaginalis is prevalent 2.
Informing partners
Partner management is recommended for patients with urethritis regardless of whether specific cause is identified. Sexual partners within 60 days should be referred for complete sexually transmitted infection (STI) evaluation and treatment with the same treatment regimen as the original patient 2.
It’s possible to pass on non-gonococcal urethritis during sex, so it’s wise to treat all cases of non-gonococcal urethritis as an sexually transmitted infection and ensure all recent partners have been treated.
You also shouldn’t have any kind of sex until you’re certain the condition has cleared up.
It’s suggested that you inform any person you’ve had sex with in the last three months, but this timeframe can vary.
Some people can feel angry, upset or embarrassed about discussing sexually transmitted infections with their current partner or previous partners.
However, don’t be afraid to discuss your concerns with your healthcare professionals or sexual health clinic. They can advise you about who to contact and the best way to contact them.
With your permission, the clinic can arrange for a “contact slip” to be given to your former partner or partners.
The slip explains that they may have been exposed to an sexually transmitted infection and advises them to have a check-up. It doesn’t have your name on it, and your details will remain totally confidential.
Nobody can force you to tell any of your partners about your sexually transmitted infection, but it’s strongly recommended that you do. Without treatment, sexually transmitted infections such as chlamydia can have serious effects on a person’s health, particularly for women.
Complications of untreated chlamydia include:
- infection of the testicles in men
- infection of the neck of the womb (cervix) in women
- pelvic inflammatory disease (PID) – this can increase the risk of infertility and ectopic pregnancy
Urethritis causes
Both bacteria and viruses may cause urethritis. Urethritis is the most common sexually transmitted infection in men with gonorrhea (Neisseria gonorrhoeae) and chlamydia representing the primary pathogens 4.
The Center for Disease Control and Prevention (CDC) does not publish rates of urethritis as a syndrome. The CDC instead breaks down sexual infection rates down by cause. Chlamydia is the most commonly reported sexually transmitted infection in the United States with over 1,500,000 new cases in 2016. Rates of new diagnoses continue to rise annually with an estimated increase of 4.7% from 2015 to 2016 4. Trends show that rates of chlamydia in females are 2 times higher than that of males. Rates are highest among adolescents and young adults. Racial disparities exist, and blacks are 5.6 times more commonly affected with chlamydia when compared to whites. Gonorrhea cases are more commonly seen in males, and there were an estimated 468,000 new cases of gonorrhea in 2016. Like with chlamydia, infections rates are higher in adolescents and young adults; the African American race is also disproportionately affected.
The most common cause of non-gonococcal urethritis is chlamydia. Chlamydia trachomatis typically infects columnar epithelial cells at mucosal sites. It replicates in host cells eventually causing cell death 12. Other causes of non-gonococcal urethritis are less well described.
Some of the bacteria that can also cause urethritis include E-coli. Viral causes are herpes simplex virus and cytomegalovirus.
Other causes include:
- Injury
- Sensitivity to the chemicals used in spermicides, contraceptive jellies, or foams
Sometimes the cause is unknown.
Risks factors for urethritis
Risks factors for urethritis include:
- Being a female
- Being male, ages 20 to 35
- Having many sexual partners
- High-risk sexual behavior (such as men having penetrating anal sex without a condom)
- History of sexually transmitted diseases
Urethritis prevention
Things you can do to help avoid urethritis include:
- Keep the area around the opening of the urethra clean.
- Follow safer sex practices. Have one sexual partner only (monogamy) and use condoms.
Urethritis symptoms
Urethritis symptoms in men
- Blood in the urine or semen
- Burning pain while urinating (dysuria)
- Discharge from penis
- Fever (rare)
- Frequent or urgent urination
- Itching, tenderness, or swelling in penis
- Enlarged lymph nodes in the groin area
- Pain with intercourse or ejaculation
Urethritis symptoms in women
- Abdominal pain
- Burning pain while urinating
- Fever and chills
- Frequent or urgent urination
- Pelvic pain
- Pain with intercourse
- Vaginal discharge
Urethritis possible complications
Men with urethritis are at risk for the following:
- Bladder infection (cystitis)
- Epididymitis
- Infection in the testicles (orchitis)
- Prostate infection (prostatitis)
After a severe infection, the urethra may become scarred and then narrowed.
Women with urethritis are at risk for the following:
- Bladder infection (cystitis)
- Cervicitis
- Pelvic inflammatory disease (PID — an infection of the uterus lining, fallopian tubes, or ovaries)
Urethritis diagnosis
Your health care provider will examine you.
In men, the exam will include the abdomen, bladder area, penis, and scrotum. The physical exam may show:
- Discharge from the penis
- Tender and enlarged lymph nodes in the groin area
- Tender and swollen penis
A digital rectal exam will also be performed.
Women will have abdominal and pelvic exams. Your doctor will check for:
- Discharge from the urethra
- Tenderness of the lower abdomen
- Tenderness of the urethra
Your doctor may look into your bladder using a tube with a camera on the end. This is called cystoscopy.
The following tests may be done:
- Complete blood count (CBC)
- C-reactive protein test
- Pelvic ultrasound (women only)
- Pregnancy test (women only)
- Urinalysis and urine cultures
- Tests for gonorrhea, chlamydia, and other sexually transmitted illnesses (STI)
- Urethral swab
Urethritis treatment
The goals of treatment are to:
- Get rid of the cause of infection
- Improve symptoms
- Prevent the spread of infection
If you have a bacterial infection, you will be given antibiotics. Treatment depends on the cause of the infection. However, identification of the organism causing urethritis can take days. Thus, doctors usually begin treatment with antibiotics that cure the most common causes. For sexually active men, treatment is usually with a ceftriaxone injection for gonorrhea plus oral azithromycin or oral doxycycline for chlamydia. If tests exclude the possibility of gonorrhea and chlamydia, trimethoprim/sulfamethoxazole or a fluoroquinolone antibiotic (such as ciprofloxacin) may be used. Women may be treated as if they had cystitis. An antiviral drug, such as acyclovir, may be needed for a herpes simplex infection. If the cause is suspected to be a sexually transmitted disease, the person’s sex partners should be evaluated for treatment. Men who receive a diagnosis of urethritis should be tested for HIV and syphilis.
You may take both pain relievers for general body pain and products for localized urinary tract pain, plus antibiotics.
People with urethritis who are being treated should avoid sex, or use condoms during sex. Your sexual partner must also be treated if the condition is caused by an infection.
Urethritis caused by trauma or chemical irritants is treated by avoiding the source of injury or irritation.
Urethritis that does not clear up after antibiotic treatment and lasts for at least 6 weeks is called chronic urethritis. Different antibiotics may be used to treat this problem.
Urethritis prognosis
With the correct diagnosis and treatment, urethritis most often clears up without further problems.
However, urethritis can lead to long-term damage to the urethra and scar tissue called urethral stricture. It can also cause damage to other urinary organs in both men and women. In women, the infection could lead to fertility problems if it spreads to the pelvis.
- Territo H, Ashurst JV. Nongonococcal Urethritis (NGU) [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535411[↩][↩]
- Workowski KA, Bolan GA., Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015 Jun 05;64(RR-03):1-137.[↩][↩][↩][↩][↩][↩][↩]
- Bradshaw CS, Tabrizi SN, Read TR, Garland SM, Hopkins CA, Moss LM, Fairley CK. Etiologies of nongonococcal urethritis: bacteria, viruses, and the association with orogenital exposure. J. Infect. Dis. 2006 Feb 01;193(3):336-45.[↩][↩][↩]
- Territo H, Ashurst JV. Nongonococcal Urethritis (NGU) [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535411[↩][↩][↩][↩][↩][↩]
- Ross JD, Jensen JS. Mycoplasma genitalium as a sexually transmitted infection: implications for screening, testing, and treatment. Sex Transm Infect. 2006 Aug;82(4):269-71.[↩]
- Shahmanesh M, Moi H, Lassau F, Janier M., IUSTI/WHO. 2009 European guideline on the management of male non-gonococcal urethritis. Int J STD AIDS. 2009 Jul;20(7):458-64.[↩]
- Scholes D, Satterwhite CL, Yu O, Fine D, Weinstock H, Berman S. Long-term trends in Chlamydia trachomatis infections and related outcomes in a U.S. managed care population. Sex Transm Dis. 2012 Feb;39(2):81-8.[↩]
- Numazaki K, Wainberg MA, McDonald J. Chlamydia trachomatis infections in infants. CMAJ. 1989 Mar 15;140(6):615-22.[↩]
- Centers for Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae–2014. MMWR Recomm Rep. 2014 Mar 14;63(RR-02):1-19.[↩]
- Geisler WM, Yu S, Hook EW. Chlamydial and gonococcal infection in men without polymorphonuclear leukocytes on gram stain: implications for diagnostic approach and management. Sex Transm Dis. 2005 Oct;32(10):630-4[↩]
- Goetze S, Hiernickel C, Elsner P. Phototoxicity of Doxycycline: A Systematic Review on Clinical Manifestations, Frequency, Cofactors, and Prevention. Skin Pharmacol Physiol. 2017;30(2):76-80.[↩]
- Ceovic R, Gulin SJ. Lymphogranuloma venereum: diagnostic and treatment challenges. Infect Drug Resist. 2015;8:39-47.[↩]