Contents
What is urge incontinence
Urge incontinence or urgency incontinence, is the involuntary loss of urine preceded by a sudden and severe desire to pass urine 1. Urge incontinence is sometimes called an unstable or overactive bladder, which is where the bladder muscle is more active than usual. As well as sometimes causing urge incontinence, overactive bladder syndrome can also mean you need to pass urine very frequently and you may need to get up several times during the night to urinate.
In a properly functioning bladder, the bladder muscle (detrusor) remains relaxed as the bladder gradually fills up. As the bladder gradually stretches, you get a feeling of wanting to pass urine when the bladder is about half full. Most people can hold on after this initial feeling until a convenient time to go to the toilet arises. However, if you are experiencing an overactive bladder and urge incontinence, the bladder may feel fuller than it actually is. This means that the bladder contracts too early when it is not very full, and not when you want it to. This can make you suddenly need the toilet and perhaps leak some urine before you get there.
With urge incontinence, you leak urine because your bladder muscles squeeze, or contract, at the wrong times. These contractions often occur no matter how much urine is in the bladder. People with urge incontinence feel like their bladder is fuller than it actually is and they feel a sudden and very intense need to pass urine and they’re unable to delay going to the toilet. There’s often only a few seconds between the need to urinate and the release of urine. They may need to urinate very often, including during the night. Their bladder contractions may be stimulated by a change in body position (from lying down to upright) or with sensory stimulation (the sound of running water, hand washing, cold weather). You may also pass urine during sex, particularly when you reach orgasm. The pathophysiology of urge incontinence is uninhibited bladder contractions caused by irritation or loss of neurologic control of bladder contractions.
Urge incontinence often gets worse as you age, and can be triggered by stress or by drinking caffeine in tea, coffee and fizzy drinks or alcohol. Urge incontinence is also linked to stroke, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, or stroke and other health conditions that interfere in the messages sent between the bladder and the brain.
If steps you can take at home do not work to improve your urge incontinence, your doctor may suggest one or more of the following treatments:
- Medicines. Medicines to treat urge incontinence help relax the bladder muscle and increase the amount of urine your bladder can hold. Common side effects of these medicines include constipation and dry eyes and mouth.
- Bladder retraining.
- Pelvic floor muscle training.
- Botox. Botox injections in the bladder can help if other treatments don’t work. Botox helps relax the bladder and increases the amount of urine your bladder can hold. You may need to get Botox treatments about once every 3 months.
- Nerve stimulation. This treatment uses mild electric pulses to stimulate nerves in the bladder. The pulses may increase blood flow to the bladder and strengthen the muscles that help control the bladder. Talk to your doctor about the different types of nerve stimulation.
- Biofeedback. Biofeedback helps you see how your bladder responds on a screen. A therapist puts an electrical patch on the skin over your bladder and urethral muscles. A wire connected to the patch is linked to a screen. You and your therapist watch the screen to see when these muscles contract so you can learn to control them.
- Surgery. If you have severe urge incontinence, your doctor may recommend surgery to help increase the amount of urine your bladder can hold or to remove your bladder. Removing your bladder is a serious surgery and is an option only when no other treatments work and the quality of your life is seriously affected.
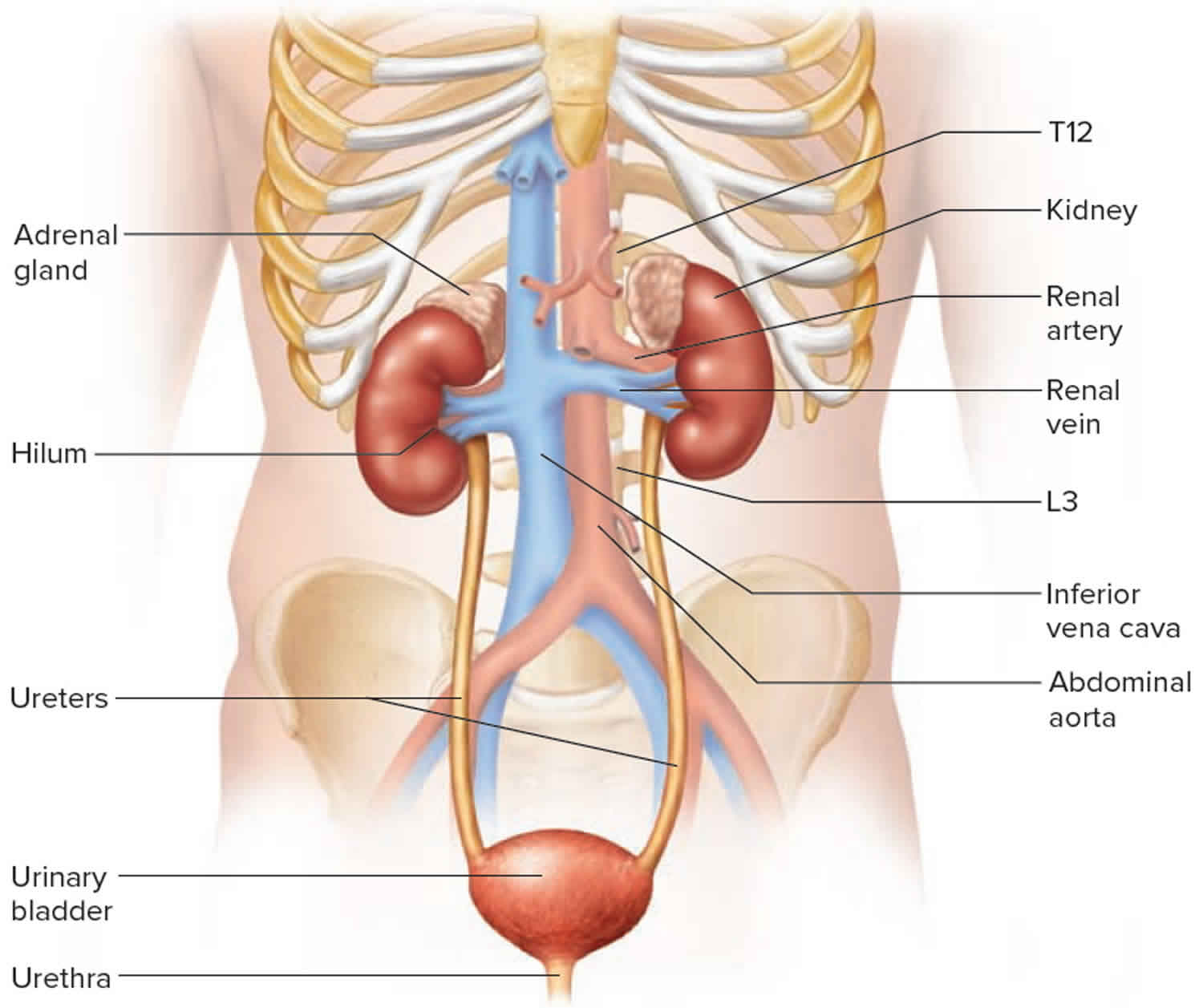
Figure 1. Urinary system anatomy
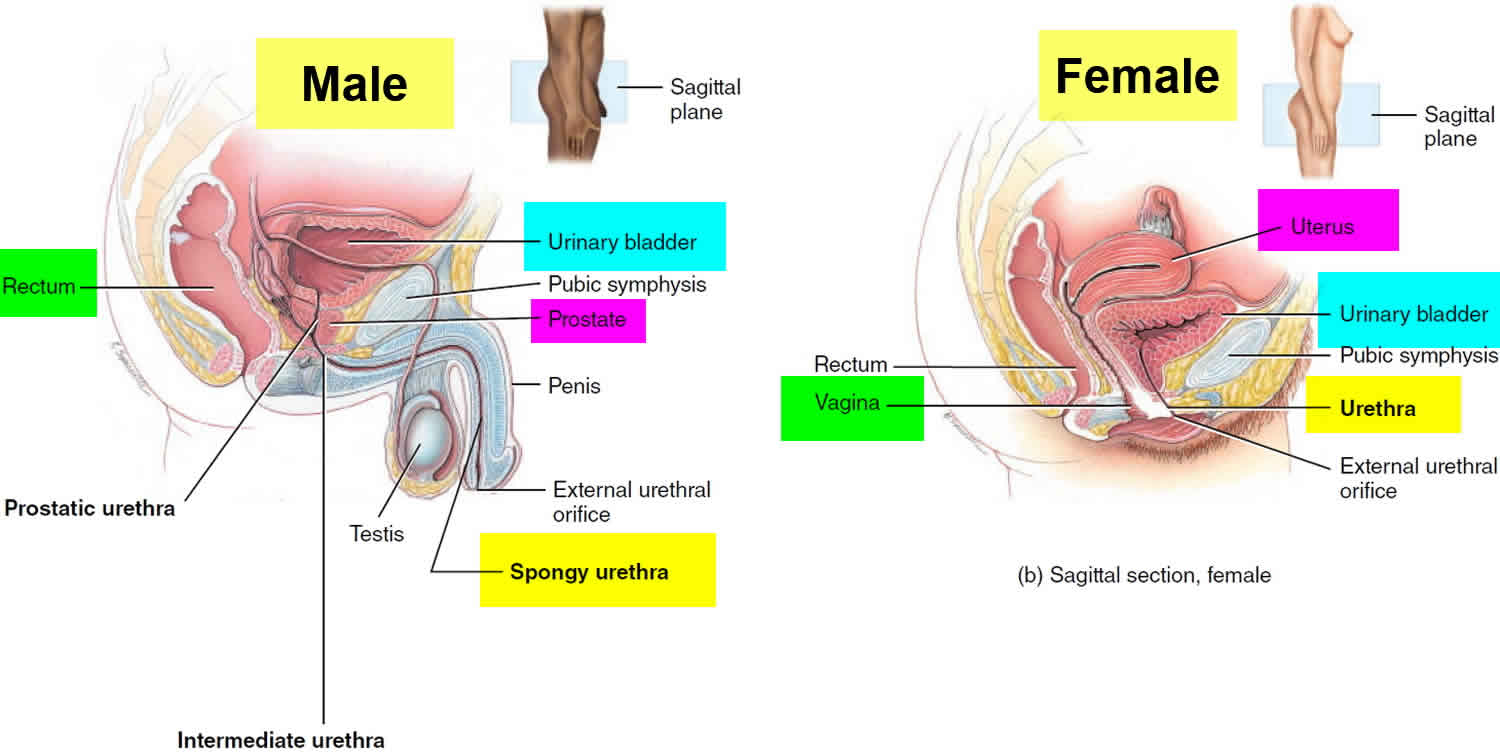
Figure 2. Urinary bladder anatomy
Figure 3. Pelvic floor female
Should I drink less water or other fluids if I have urinary incontinence?
No. Many people with urinary incontinence think they need to drink less to reduce how much urine leaks out. But you need fluids, especially water, for good health. (But alcohol and caffeine can irritate or stress the bladder and make urinary incontinence worse.)
Women need 91 ounces (about 11 cups) of fluids a day from food and drinks 2. Getting enough fluids helps keep your kidneys and bladder healthy, prevents urinary tract infections, and prevents constipation, which may make urinary incontinence worse.
After age 60, people are less likely to get enough water, putting them at risk for dehydration and conditions that make urinary incontinence worse 3.
- Drinking enough water will help keep odors away.
- Drink a little bit of fluid at a time throughout the day, so your bladder does not need to handle a large amount of urine at one time. Drink less than 8 ounces (240 milliliters) at one time.
- Do not drink large amounts of fluids with meals.
- Sip small amounts of fluids between meals.
- Stop drinking fluids about 2 hours before bedtime.
- Avoid carbonated drinks.
It also may help to stop eating foods that may irritate the bladder, such as:
- Caffeine
- Highly acidic foods, such as citrus fruits and juices
- Spicy foods
- Artificial sweeteners
How can I prevent urinary incontinence?
Although you can’t always prevent urinary incontinence, you can take steps to lower your risk:
- Practice Kegel exercises daily (see pelvic floor exercises below), especially during pregnancy and after talking to your doctor, nurse, or midwife.
- Reach or stay at a healthy weight.
- Eat foods with fiber to help prevent constipation.
Kegel exercises, also called Kegels or pelvic floor muscle training, are exercises for your pelvic floor muscles to help prevent or reduce stress urinary incontinence. Your pelvic floor muscles support your uterus, bladder, small intestine, and rectum.
Four in 10 women improved their symptoms after trying Kegels 4. Kegels can be done daily and may be especially helpful during pregnancy. They can help prevent the weakening of pelvic floor muscles, which often happens during pregnancy and childbirth. Your pelvic floor muscles may also weaken with age and less physical activity.
Some women have urinary symptoms because the pelvic floor muscles are always tightened. In this situation, Kegel exercises will not help your urinary symptoms and may cause more problems. Talk to your doctor or nurse about your urinary symptoms before doing Kegel exercises.
Urge incontinence vs Stress incontinence
Stress incontinence occurs when urine leaks as pressure is put on the bladder, for example, during exercise, coughing, sneezing, laughing, or lifting heavy objects. Stress incontinence is the most common type of bladder control problem in younger and middle-age women. Stress incontinence may begin around the time of menopause. Stress incontinence is not related to psychological stress. Stress incontinence happens because increased pressure inside the tummy presses down on the bladder.
Stress incontinence is more common in women around the time of childbirth or after menopause. Stress incontinence can also happen in people who have diabetes, a chronic cough (due to asthma, smoking or bronchitis), constipation or obesity.
Stress incontinence differs from urge incontinence, which is the unintentional loss of urine caused by the bladder muscle contracting, usually associated with a sense of urgency. Stress incontinence is much more common in women than men.
If you have stress incontinence, you may feel embarrassed, isolate yourself, or limit your work and social life, especially exercise and leisure activities. With treatment, you’ll likely be able to manage stress incontinence and improve your overall well-being.
Stress incontinence symptoms
If you have stress incontinence, you may experience urine leakage when you:
- Cough
- Sneeze
- Laugh
- Stand up
- Get out of a car
- Lift something heavy
- Exercise
- Have sex
You may not experience incontinence every time you do one of these things, but any pressure-increasing activity can make you more vulnerable to unintentional urine loss, particularly when your bladder is full.
Stress incontinence causes
Stress incontinence occurs when the muscles and other tissues that support the bladder (pelvic floor muscles) and the muscles that regulate the release of urine (urinary sphincter) weaken.
The bladder expands as it fills with urine. Normally, valve-like muscles in the urethra — the short tube that carries urine out of your body — stay closed as the bladder expands, preventing urine leakage until you reach a bathroom. But when those muscles weaken, anything that exerts force on the abdominal and pelvic muscles — sneezing, bending over, lifting, laughing hard, for instance — can put pressure on your bladder and cause urine leakage.
Your pelvic floor muscles and urinary sphincter may lose strength because of:
- Childbirth. In women, poor function of pelvic floor muscles or the sphincter may occur because of tissue or nerve damage during delivery of a child. Stress incontinence from this damage may begin soon after delivery or occur years later.
- Prostate surgery. In men, the most common factor leading to stress incontinence is the surgical removal of the prostate gland (prostatectomy) to treat prostate cancer. Because the sphincter lies directly below the prostate gland and encircles the urethra, a prostatectomy may result in a weakened sphincter.
Contributing factors
Other factors that may worsen stress incontinence include:
- Illnesses that cause chronic coughing or sneezing
- Obesity
- Smoking, which can cause frequent coughing
- High-impact activities, such as running and jumping, over many years
Risk factors for developing stress incontinence
Factors that increase the risk of developing stress incontinence include:
- Age. Although stress incontinence isn’t a normal part of aging, physical changes associated with aging, such as the weakening of muscles, may make you more susceptible to stress incontinence. However, occasional stress incontinence can occur at any age.
- Type of childbirth delivery. Women who’ve had a vaginal delivery are more likely to develop urinary incontinence than women who’ve delivered via a cesarean section. Women who’ve had a forceps delivery to more rapidly deliver a healthy baby may also have a greater risk of stress incontinence. Women who’ve had a vacuum-assisted delivery don’t appear to have a higher risk for stress incontinence.
- Body weight. People who are overweight or obese have a much higher risk of stress incontinence. Excess weight increases pressure on the abdominal and pelvic organs.
- Previous pelvic surgery. Hysterectomy in women and particularly surgery for prostate cancer in men can alter the function and support of the bladder and urethra, making it much more likely for a person to develop stress incontinence.
Stress incontinence treatment
If steps you can take at home do not work to improve your stress incontinence, your doctor may talk to you about other options:
- Medicine. After menopause, applying vaginal creams, rings, or patches with estrogen (called topical estrogen) can help strengthen the muscles and tissues in the urethra and vaginal areas. A stronger urethra will help with bladder control. Learn more about menopause treatments.
- Vaginal pessary. A reusable pessary is a small plastic or silicone device (shaped like a ring or small donut) that you put into your vagina. The pessary pushes up against the wall of the vagina and the urethra to support the pelvic floor muscles and help reduce stress incontinence. Pessaries come in different sizes, so your doctor or nurse must write a prescription for the size that will fit you. Another type of pessary looks like a tampon and is used once and then thrown away. You can get this type of pessary at a store that also sells feminine hygiene products.
- Bulking agents. Your doctor can inject a bulking agent, such as collagen, into tissues around the bladder and urethra to cause them to thicken. This helps keep the bladder opening closed and reduces the amount of urine that can leak out.
- Surgery. Surgery for urinary incontinence is not recommended if you plan to get pregnant in the future. Pregnancy and childbirth can cause leakage to happen again. The two most common types of surgery for urinary incontinence are 5:
- Sling procedures. The mid-urethral sling is the most common type of surgery to treat stress incontinence. The sling is either a narrow piece of synthetic (man-made) mesh or a piece of tissue from your own body that your doctor places under your urethra. The sling acts like a hammock to support the urethra and hold the bladder in place. Serious complications from the sling procedure include pain, infection, pain during sex, and damage to nearby organs, such as the bladder. The Food and Drug Administration (FDA) reports that in 1 out of every 50 patients who have synthetic mesh for urinary incontinence, the mesh moves after surgery and stick outs, into the vagina, causing pain 6. The FDA recommends discussing treatment options with your doctor before surgery, and asking specific questions about side effects.
- Colposuspension. This surgery also helps hold the bladder in place with stitches on either side of the urethra. This is often referred to as a Burch procedure.
Urge incontinence causes
Normal bladder function
The kidneys produce urine, which drains into your bladder. When you urinate, urine passes from your bladder through an opening at the bottom and flows out a tube called the urethra. As your bladder fills with urine from the kidneys, it stretches to make room for the urine. You should feel the first urge to urinate when there is a bit less than 1 cup (240 milliliters) of urine in your bladder. Most people can hold more than 2 cups (480 milliliters) of urine in the bladder.
As your bladder fills, nerve signals sent to your brain eventually trigger the need to urinate. When you urinate, nerve signals coordinate the relaxation of the pelvic floor muscles and the muscles of the urethra (urinary sphincter muscles). The muscles of the bladder tighten (contract), pushing the urine out.
Two muscles help prevent the flow of urine:
- The sphincter is a muscle around the opening of the bladder. It squeezes to prevent urine from leaking into the urethra. This is the tube that urine passes through from your bladder to the outside.
- The bladder wall muscle relaxes so the bladder can expand and hold urine.
When you urinate, the bladder wall muscle squeezes to force urine out of the bladder. As this happens, the sphincter muscle relaxes to allow the urine to pass through.
All of these systems must work together to control urination:
- Your bladder muscles and other parts of your urinary tract
- The nerves controlling your urinary system
- Your ability to feel and respond to the urge to urinate
The bladder may contract too often from nervous system problems or bladder irritation.
Involuntary bladder contractions
With urge incontinence, you leak urine because the bladder muscles squeeze, or contract, at the wrong times. These contractions often occur no matter how much urine is in the bladder.
Overactive bladder occurs because the muscles of the bladder start to contract involuntarily even when the volume of urine in your bladder is low. This involuntary contraction creates the urgent need to urinate.
Several conditions may contribute to signs and symptoms of overactive bladder. Urge incontinence may result from:
- Bladder cancer
- Bladder inflammation
- Factors that obstruct bladder outflow — enlarged prostate, constipation or previous operations to treat other forms of incontinence
- Bladder stones
- Acute urinary tract infections that can cause symptoms similar to an overactive bladder
- Brain or nerve problems, such as multiple sclerosis or stroke
- Nerve injury, such as from a spinal cord injury
- Neurological disorders, such as stroke and multiple sclerosis
- Diabetes
- Medications that cause a rapid increase in urine production or require that you take them with lots of fluids
- Excess consumption of caffeine or alcohol
- Declining cognitive function due to aging, which may make it more difficult for your bladder to understand the signals it receives from your brain
- Difficulty walking, which can lead to bladder urgency if you’re unable to get to the bathroom quickly
- Incomplete bladder emptying, which may lead to symptoms of overactive bladder, as you have little urine storage space left
In men, urge incontinence also may be due to:
- Bladder changes caused by an enlarged prostate, called benign prostatic hyperplasia (BPH)
- An enlarged prostate blocking urine from flowing from the bladder
In most cases of urge incontinence, no cause can be found.
Although urge incontinence may occur in anyone at any age, it is more common in women and older adults.
Risk factors for developing urge incontinence
As you age, you’re at increased risk of developing overactive bladder. You’re also at higher risk of diseases and disorders, such as enlarged prostate and diabetes, which can contribute to other problems with bladder function.
Many people with cognitive decline — for instance, after a stroke or with Alzheimer’s disease — develop an overactive bladder. Incontinence that results from situations like this can be managed with fluid schedules, timed and prompted voiding, absorbent garments, and bowel programs.
Some people with an overactive bladder also have bowel control problems; tell your doctor if this is a problem for you.
Urge incontinence prevention
These healthy lifestyle choices may reduce your risk of overactive bladder:
- Maintain a healthy weight.
- Get regular, daily physical activity and exercise.
- Limit consumption of caffeine and alcohol.
- Quit smoking.
- Manage chronic conditions, such as diabetes, that might contribute to overactive bladder symptoms.
- Learn where your pelvic floor muscles are and then strengthen them by doing Kegel exercises — tighten (contract) muscles, hold the contraction for two seconds and relax muscles for three seconds. Work up to holding the contraction for five seconds and then 10 seconds at a time. Do three sets of 10 repetitions each day.
Urge incontinence symptoms
Urge incontinence symptoms include:
- Not being able to control when you pass urine
- Having to urinate often during the day and night
- Needing to urinate suddenly and urgently
- Feel a sudden urge to urinate that’s difficult to control
- Experience urge incontinence — the involuntary loss of urine immediately following an urgent need to urinate
- Urinate frequently, usually eight or more times in 24 hours
- Awaken two or more times in the night to urinate (nocturia)
Although you may be able to get to the toilet in time when you sense an urge to urinate, unexpected frequent urination and nighttime urination can disrupt your life.
Urge incontinence complications
Complications of urge incontinence may include:
- Personal distress, anxiety or depression. If you experience urge incontinence with your daily activities, you may feel embarrassed and distressed by the condition. It can disrupt your work, social activities, relationships and even your sex life. Some people are embarrassed that they need pads or incontinence garments.
- Sleep disturbances and interrupted sleep cycles.
- Issues with sexuality.
- Mixed urinary incontinence. Mixed incontinence is common and means that you have both stress incontinence and urge incontinence — the loss of urine resulting from an involuntary contraction of bladder muscles (overactive bladder).
Some women also may have a disorder called mixed incontinence, when both urge and stress incontinence occur. Stress incontinence is the loss of urine when you exert physical stress or pressure on your bladder, such as during activities that include running or jumping. Treatment of the stress incontinence is not likely to help the overactive bladder symptoms.
Older people may have a common combination of bladder storage problems and bladder-emptying issues. The bladder may cause a lot of urgency and even incontinence, but it doesn’t empty well. A specialist may be able to help you with this combination of bladder problems.
Urge incontinence diagnosis
If you have an abnormal urge to urinate, your doctor will check to make sure that you don’t have an infection or blood in your urine. Your doctor may also want to make sure that you’re emptying your bladder completely when you urinate.
Your doctor will look for clues that might also indicate contributing factors. The work-up will likely include a:
- Medical history
- Physical exam, focusing on your abdomen and genitals
- Urine sample to test for infection, traces of blood or other abnormalities
- Focused neurological exam that may identify sensory problems or abnormal reflexes
During a physical exam, your health care provider will look at your belly and rectum.
- Women will have a pelvic exam.
- Men will have a genital exam.
In most cases, the physical exam will not find any problems. If there are nervous system causes, other problems also may be found.
Tests include the following:
- Cystoscopy to view the inside of your bladder. Your doctor inserts a thin tube with a tiny camera into your urethra and bladder to look for damaged tissue. Depending on the type of cystoscopy you need, your doctor may use medicine to numb your skin and urinary organs while you are still awake, or you may be fully sedated.
- Pad test. You wear a pad or pads to collect all of your leaked urine. Then the pad is weighed to find out how much urine you lost.
- Pelvic or abdominal ultrasound. Your doctor will use an ultrasound wand on the outside of your abdomen to take pictures of the kidneys, bladder, and urethra. Your doctor will look for anything unusual that may be causing urinary incontinence.
- Measuring urine left in the bladder. This test is important if your bladder doesn’t empty completely when you urinate or experience urinary incontinence. Remaining urine (postvoid residual urine) may cause symptoms identical to an overactive bladder. To measure residual urine after you have voided, your doctor may request an ultrasound scan of your bladder or pass a thin tube (catheter) through the urethra and into your bladder to drain and measure the remaining urine.
- Measuring urine flow rate. To measure the volume and speed of your voiding, you may be asked to urinate into a uroflowmeter. This device translates the data into a graph of changes in your flow rate.
- Testing bladder pressures. Cystometry measures pressure in your bladder and in the surrounding region during bladder filling. During this test, your doctor uses a thin tube (catheter) to fill your bladder slowly with warm water. Another catheter with a pressure-measuring sensor is placed in your rectum or, if you’re a woman, in your vagina. This procedure can identify whether you have involuntary muscle contractions or a stiff bladder that’s not able to store urine under low pressure.
- Urinalysis to check for infection. After you urinate into a cup, the doctor or nurse will send your urine to a lab. At the lab, your urine will be checked for infection or other causes of incontinence.
- Urinary stress test (you stand with a full bladder and cough). During this test, you will cough or bear down as if pushing during childbirth as your doctor watches for loss of urine.
- Urine cytology to rule out bladder cancer.
- Urodynamic studies to measure pressure and urine flow. Your doctor inserts a thin tube into your bladder and fills your bladder with water. This allows your doctor to measure the pressure in your bladder to see how much fluid your bladder can hold.
- X-rays with contrast dye to look at your kidneys and bladder.
- Voiding diary to assess your fluid intake, urine output, and urination frequency. Your doctor or nurse may ask you to keep a diary for 2 to 3 days to track when you empty your bladder or leak urine. The diary may help your doctor or nurse see patterns in the incontinence that give clues about the possible cause and treatments that might work for you.
Urge incontinence treatment
Treatment depends on how bad your symptoms are and how they affect your life.
There are four main treatment approaches for urge incontinence:
- Bladder and pelvic floor muscle training
- Lifestyle changes
- Medicines
- Surgery
Bladder retraining
Managing urge incontinence most often begins with bladder retraining. This helps you become aware of when you lose urine because of bladder spasms. Then you relearn the skills you need to hold and release urine.
- You set a schedule of times when you should try to urinate. You try to avoid urination between these times.
- One method is to force yourself to wait 1 to 1 1/2 hours between trips to the bathroom, even if you have any leakage or an urge to urinate in between these times.
- As you become better at waiting, gradually increase the time by 1/2 hour until you are urinating every 3 to 4 hours.
Pelvic floor muscle training
Sometimes, Kegel exercises (pelvic floor exercises), biofeedback, or electrical stimulation may be used with bladder retraining. These methods help strengthen the muscles of your pelvic floor:
Kegel exercises (pelvic floor exercises)
To do Kegel exercises 7:
- Lie down. It may be easier to learn how to do Kegels correctly while lying down. You don’t have to lie down once you learn to do Kegels correctly.
- Squeeze the muscles in your genital area as if you were trying to stop the flow of urine or passing gas. Try not to squeeze the muscles in your belly or legs at the same time. Try to squeeze only the pelvic muscles. Be extra careful not to tighten your stomach, legs, or buttocks (because then you will not be using your pelvic floor muscles).
- Relax. Squeeze the muscles again and hold for 3 seconds. Then relax for 3 seconds.
- Repeat 10 times, 3 times a day (morning, afternoon, and night). Work up to 3 sets of 10 each day.
- Practice Kegels anywhere. When your muscles get stronger, try doing Kegels while sitting or standing. You can do these exercises at any time, such as while sitting at your desk or in the car, waiting in line, or doing the dishes. Don’t do Kegel exercises at the same time you are urinating. This can weaken your pelvic floor muscles over time.
If you are uncomfortable or uncertain about doing Kegel exercises on your own, a doctor or nurse can also teach you how to do Kegels. A pelvic floor physical therapist or other specialist may also be available in your area to help teach you how to strengthen these muscles.
Breathe deeply and relax your body when you are doing these exercises. Make sure you are not tightening your stomach, thigh, buttock, or chest muscles.
After 4 to 6 weeks, you should feel better and have fewer symptoms. Keep doing the exercises, but do not increase how many you do. Overdoing it can lead to straining when you urinate or move your bowels.
Kegel exercises work differently for each person. Your symptoms may go away totally, you may notice an improvement in your symptoms but still have some leakage, or you may not see any improvement at all. But even if your symptoms don’t get better, Kegel exercises can help prevent your incontinence from getting worse.
You may need to continue doing Kegel exercises for the rest of your life. Even if your symptoms improve, urinary incontinence can come back if you stop doing the exercises.
Some notes of caution:
- Once you learn how to do them, do not practice Kegel exercises at the same time you are urinating more than twice a month. Doing the exercises while you are urinating can weaken your pelvic floor muscles over time or cause damage to bladder and kidneys.
- In women, doing Kegel exercises incorrectly or with too much force may cause vaginal muscles to tighten too much. This can cause pain during sexual intercourse.
- Incontinence will return if you stop doing these exercises. Once you start doing them, you may need to do them for the rest of your life.
- It may take several months for your incontinence to lessen once you start doing these exercises.
How to find the right muscles
A Kegel exercise is like pretending you have to urinate and then holding it. You relax and tighten the muscles that control urine flow. It is important to find the right muscles to tighten.
Next time you have to urinate, start to go and then stop. Feel the muscles in your vagina (for women), bladder, or anus get tight and move up. These are the pelvic floor muscles. If you feel them tighten, you have done the exercise right. Your thighs, buttock muscles, and abdomen should remain relaxed.
If you still are not sure you are tightening the right muscles:
- Imagine that you are trying to keep yourself from passing gas.
- Women: Insert a finger into your vagina. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down.
- Men: Insert a finger into your rectum. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down.
Vaginal cones
This is a weighted cone that is inserted into the vagina to strengthen the pelvic floor muscles.
- You place the cone into the vagina.
- Then you try to squeeze your pelvic floor muscles to hold the cone in place.
- You can wear the cone for up to 15 minutes at a time, 2 times a day.
Biofeedback
This method can help you learn to identify and control your pelvic floor muscles.
- Some therapists place a sensor in the vagina (for women) or the anus (for men) so they can tell when they are squeezing the pelvic floor muscles.
- A monitor will display a graph showing which muscles are squeezing and which are at rest.
- The therapist can help you find the right muscles for performing Kegel exercises.
Electrical nerve stimulation
This uses a gentle electrical current to contract your bladder muscles. The pulses may increase blood flow to the bladder and strengthen the muscles that help control the bladder. Talk to your doctor about the different types of nerve stimulation.
- The current is delivered using an anal or vaginal probe.
- This therapy may be done at your doctor’s office or at home.
- Treatment sessions usually last 20 minutes and may be done every 1 to 4 days.
Percutaneous tibial nerve stimulation
This treatment may help some people with overactive bladder.
- An acupuncture needle is placed behind the ankle, and electrical stimulation is used for 30 minutes.
- Most often, treatments will occur weekly for around 12 weeks, and perhaps monthly after that.
Lifestyle changes
Pay attention to how much water you drink and when you drink.
- Drinking enough water will help keep odors away.
- Drink a little bit of fluid at a time throughout the day, so your bladder does not need to handle a large amount of urine at one time. Drink less than 8 ounces (240 milliliters) at one time.
- Do not drink large amounts of fluids with meals.
- Sip small amounts of fluids between meals.
- Stop drinking fluids about 2 hours before bedtime.
- Avoid carbonated drinks.
It also may help to stop eating foods that may irritate the bladder, such as:
- Caffeine
- Highly acidic foods, such as citrus fruits and juices
- Spicy foods
- Artificial sweeteners
Avoid activities that irritate the urethra and bladder. This includes taking bubble baths or using harsh soaps.
Urge incontinence medication
Medicines used to treat urge incontinence relax bladder contractions and help improve bladder function. There are several types of medicines that may be used alone or together:
- Anticholinergic medicines help relax the muscles of the bladder. They include oxybutynin (Oxytrol, Ditropan), tolterodine (Detrol), darifenacin (Enablex), trospium (Sanctura), and solifenacin (VESIcare).
- Beta agonist drugs can also help relax the muscles of the bladder. The only medicine of this type currently is mirabegron (Myrbetriq).
- Flavoxate (Urispas) is a drug that calms muscle spasms. However, studies have shown that it is not always effective at controlling symptoms of urge incontinence.
- Tricyclic antidepressants (imipramine, doxepin) help “paralyze” the smooth muscle of the bladder.
- Botox injections are commonly used to treat overactive bladder. The medicine is injected into the bladder through a cystoscope. The procedure is most often done in the provider’s office.
These medicines may have side effects such as dizziness or dry eyes and dry mouth. Talk with your provider if you notice bothersome side effects.
Extended-release forms of these medications, including the skin patch or gel, may cause fewer side effects.
Your doctor may recommend that you suck on a piece of sugar-free candy or chew sugar-free gum to relieve dry mouth, and use eyedrops to keep your eyes moist. Over-the-counter preparations, such as Biotene products, can be helpful for long-term dry mouth. To avoid constipation, your doctor might recommend a fiber-rich diet or use of stool softeners.
If you have an infection, your provider will prescribe antibiotics. Be sure to take the entire amount as directed.
Bladder injections
OnabotulinumtoxinA, also called Botox (Botulinum neurotoxin), is a protein from the bacteria that cause botulism illness. Used in small doses directly injected into bladder tissues, this protein partially paralyzes muscles.
Clinical research shows that it may be useful for severe urge incontinence. The temporary effects generally last five months or more, but repeat injections are necessary.
About half of people had side effects from these injections, including 9 percent who had urinary retention. So, if you’re considering Botox treatments, you should be willing and able to catheterize yourself if urinary retention occurs.
Surgery
Surgery can help your bladder store more urine. It can also help relieve the pressure on your bladder. Surgery is only used for people who have too many spasms and are not able to store much urine. Surgery to treat overactive bladder is also reserved for people with severe symptoms who don’t respond to other treatments.
Augmentation cystoplasty is the surgery most often performed for severe urge incontinence. In this surgery, a part of the bowel is added to the bladder. This increases the bladder size and allows it to store more urine.
- Surgery to increase bladder capacity (augmentation cystoplasty). This procedure uses pieces of your bowel to replace a portion of your bladder. This surgery is used only in cases of severe urge incontinence that doesn’t respond to any other, more-conservative treatment measures. If you have this surgery, you may need to use a catheter intermittently for the rest of your life to empty your bladder.
- Bladder removal (cystectomy). This procedure is used as a last resort and involves removing the bladder and surgically constructing a replacement bladder (neobladder) or an opening in the body (stoma) to attach a bag on the skin to collect urine.
Possible complications include:
- Blood clots
- Bowel blockage
- Infection
- Pneumonia
- Slightly increased risk of tumors
- Not being able to empty your bladder
There is a risk of forming tube-like passages from the bladder to other organs or your skin. These are called urinary fistulae. They can lead to:
- Urine draining out in an unusual way, such as from your vagina
- Urinary tract infection
- Difficulty urinating
Sacral nerve stimulation
Regulating the nerve impulses to your bladder can improve overactive bladder symptoms. A small unit is implanted under your skin. This sends small electrical pulses to the sacral nerve (one of the nerves that comes out at the base of your spine). The electrical pulses can be adjusted to help relieve your symptoms.
This surgical procedure is often done with a trial of a temporary wire or as an advanced procedure in which the permanent electrode is implanted and a longer trial is performed prior to a surgical placement of the battery-powered pulse generator. Your doctor then uses a device connected to the wire to deliver electrical impulses to your bladder, similar to what a pacemaker does for the heart.
If this successfully reduces your symptoms, the wire is eventually connected to a small battery device that’s placed under your skin.
Urge incontinence prognosis
How well you do depends on your symptoms, diagnosis, and treatment. Many people must try different treatments (some at the same time) to reduce symptoms.
Getting better takes time, so try to be patient. A small number of people need surgery to control their symptoms.
Urinary incontinence is a long-term (chronic) problem. While treatments can cure your condition, you should still to see your doctor to make sure you are doing well and check for possible problems.
- Harris S, Riggs J. Mixed Urinary Incontinence. [Updated 2018 Nov 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534234[↩]
- Institute of Medicine. (2004). Dietary References Intakes: Water, Potassium, Sodium, Chloride, and Sulfate [↩]
- Rosinger, A. and Herrick, K. (2016). Daily water intake among U.S. men and women, 2009–2012. National Center for Health Statistics Data Brief; 242.[↩]
- Health Resources and Services Administration, Agency for Healthcare Research and Quality. (2012). Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness. Comparative Effectiveness Review; 36.[↩]
- American College of Obstetricians and Gynecologists. (2017). Surgery for Stress Urinary Incontinence https://www.acog.org/-/media/For-Patients/faq166.pdf?dmc=1&ts=20151007T1250145628[↩]
- Food and Drug Administration. (2018). Considerations about surgical mesh for SUI. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/UroGynSurgicalMesh/ucm345219.htm[↩]
- Kegel exercises – self-care. https://medlineplus.gov/ency/patientinstructions/000141.htm[↩]