Contents
What is urodynamic testing
Urodynamic testing is generally used as a collective term for all tests of bladder and urethral function. Urodynamic testing is widely used to direct decisions about treatment and provide prognostic information.
Urodynamic testing is any procedure that looks at how well the bladder, sphincters, and urethra are storing and releasing urine. Most urodynamic tests focus on the bladder’s ability to hold urine and empty steadily and completely. Urodynamic tests can also show whether the bladder is having involuntary contractions that cause urine leakage. A health care provider may recommend urodynamic tests if symptoms suggest problems with the lower urinary tract. Lower urinary tract symptoms include:
- urine leakage
- frequent urination
- painful urination
- sudden, strong urges to urinate
- problems starting a urine stream
- problems emptying the bladder completely
- recurrent urinary tract infections
Urodynamic tests range from simple observation to precise measurements using sophisticated instruments. For simple observation, a health care provider may record:
- the length of time it takes a person to produce a urinary stream
- the volume of urine produced
- ability or inability to stop the urine flow in midstream
For precise measurements, imaging equipment takes pictures of the bladder filling and emptying, pressure monitors record the pressures inside the bladder, and sensors record muscle and nerve activity. The health care provider will decide the type of urodynamic test based on the person’s health information, physical exam, and lower urinary tract symptoms. The urodynamic test results help diagnose the cause and nature of a lower urinary tract problem.
Most urodynamic tests do not involve special preparations, though some tests may require a person to make a change in fluid intake or to stop taking certain medications. Depending on the test, a person may be instructed to arrive for testing with a full bladder.
Urodynamic testing include:
- uroflowmetry
- postvoid residual measurement
- cystometric test
- leak point pressure measurement
- pressure flow study
- electromyography
- video urodynamic tests
After having urodynamic tests, a person may feel mild discomfort for a few hours when urinating. Drinking an 8-ounce glass of water every half-hour for 2 hours may help to reduce the discomfort. Your health care provider may recommend taking a warm bath or holding a warm, damp washcloth over the urethral opening to relieve the discomfort.
An antibiotic may be prescribed for 1 or 2 days to prevent infection, but not always. People with signs of infection—including pain, chills, or fever—should call their health care provider immediately.
Why would I need urodynamics?
Urodynamics help find the cause of problems related to:
- Urine leaks/controlling your urine
- Bladder not emptying all the way
- The need to go too often
- The need to go suddenly
- Weak urine flow
- Urine flow stopping and starting (“intermittent”)
- Getting urinary tract infections often
Your health care provider will talk with you about your symptoms. Then the provider should give you a physical exam, and start with simple urine tests.
If more information is needed, your doctor may suggest urodynamic testing and possibly x-rays. Your urologist will create a treatment plan based on what they learn. Additional tests will help to clarify the problem.
To prevent infection, you will often be given an antibiotic before and/or after your test. You will also be asked to arrive with a full bladder.
Urodynamics procedure
Uroflowmetry
Uroflowmetry is the measurement of urine speed and volume. Special equipment automatically measures the amount of urine and the flow rate—how fast the urine comes out. Uroflowmetry equipment includes a device for catching and measuring urine and a computer to record the data. During a uroflowmetry test, the person urinates privately into a special toilet or funnel that has a container for collecting the urine and a scale. The equipment creates a graph that shows changes in flow rate from second to second so the health care provider can see when the flow rate is the highest and how many seconds it takes to get there. Results of this test will be abnormal if the bladder muscles are weak or urine flow is blocked. Another approach to measuring flow rate is to record the time it takes to urinate into a special container that accurately measures the volume of urine. Uroflowmetry measurements are performed in a health care provider’s office; no anesthesia is needed.
Postvoid residual measurement
This urodynamic test measures the amount of urine left in the bladder after urination. The remaining urine is called the postvoid residual. Postvoid residual can be measured with ultrasound equipment that uses harmless sound waves to create a picture of the bladder. Bladder ultrasounds are performed in a health care provider’s office, radiology center, or hospital by a specially trained technician and interpreted by a doctor, usually a radiologist. Anesthesia is not needed. Postvoid residual can also be measured using a catheter—a thin flexible tube. A health care provider inserts the catheter through the urethra up into the bladder to remove and measure the amount of remaining urine. A postvoid residual of 100 milliliters or more is a sign that the bladder is not emptying completely. Catheter measurements are performed in a health care provider’s office, clinic, or hospital with local anesthesia.
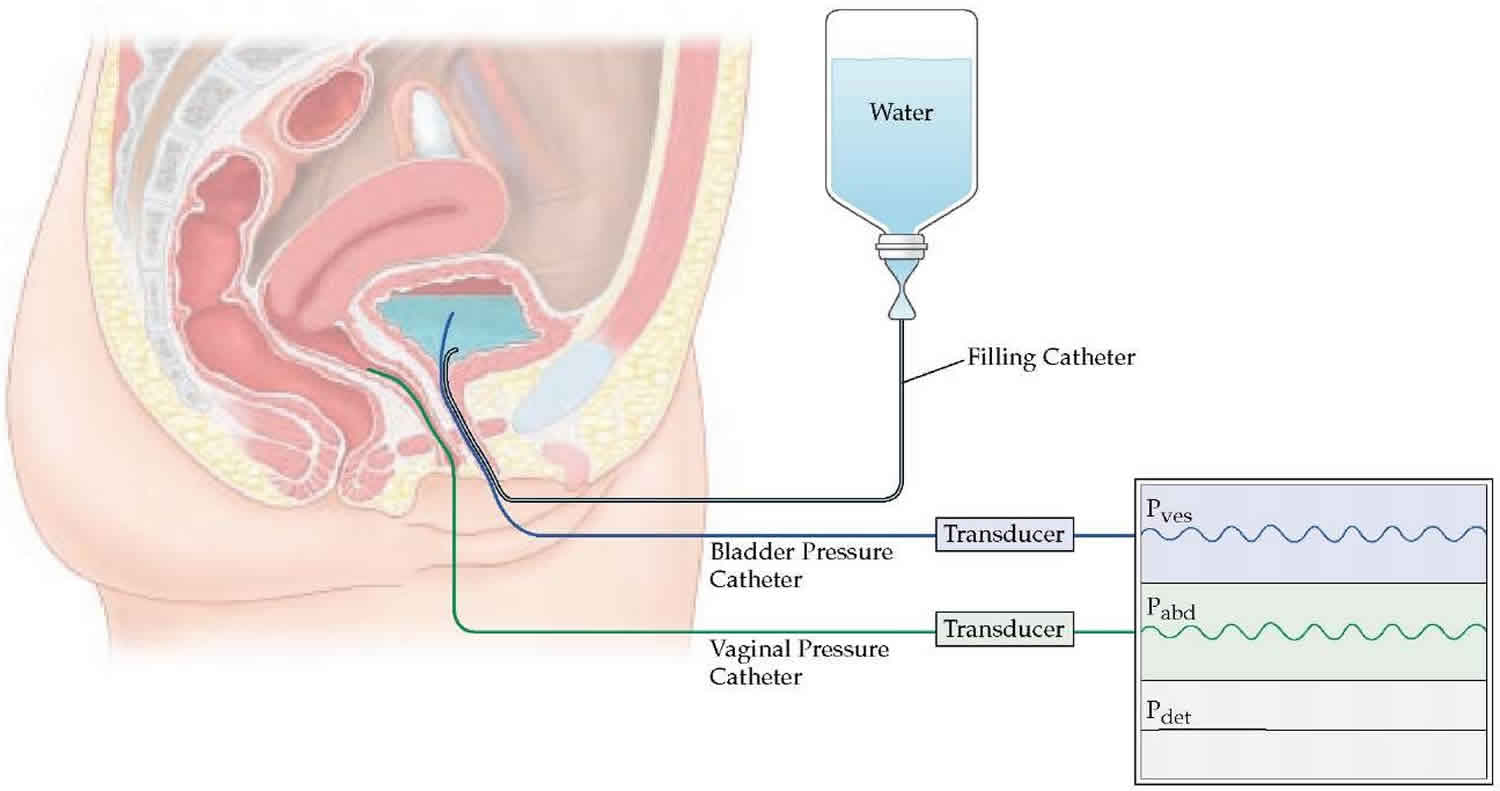
Cystometric test
A cystometric test measures how much urine the bladder can hold, how much pressure builds up inside the bladder as it stores urine, and how full it is when the urge to urinate begins. A catheter is used to empty the bladder completely. Then a special, smaller catheter is placed in the bladder. This catheter has a pressure-measuring device called a manometer. Another catheter may be placed in the rectum to record pressure there.
Once the bladder is emptied completely, the bladder is filled slowly with warm water. During this time, the person is asked to describe how the bladder feels and indicate when the need to urinate arises. When the urge to urinate occurs, the volume of water and the bladder pressure are recorded. The person may be asked to cough or strain during this procedure to see if the bladder pressure changes. A cystometric test can also identify involuntary bladder contractions. Cystometric tests are performed in a health care provider’s office, clinic, or hospital with local anesthesia.
Leak point pressure measurement
This urodynamic test measures pressure at the point of leakage during a cystometric test. While the bladder is being filled for the cystometric test, it may suddenly contract and squeeze some water out without warning. The manometer measures the pressure inside the bladder when this leakage occurs. This reading may provide information about the kind of bladder problem that exists. The person may be asked to apply abdominal pressure to the bladder by coughing, shifting position, or trying to exhale while holding the nose and mouth. These actions help the health care provider evaluate the sphincters.
Pressure Flow Study
A pressure flow study measures the bladder pressure required to urinate and the flow rate a given pressure generates. After the cystometric test, the person empties the bladder, during which time a manometer is used to measure bladder pressure and flow rate. This pressure flow study helps identify bladder outlet blockage that men may experience with prostate enlargement. Bladder outlet blockage is less common in women but can occur with a cystocele or, rarely, after a surgical procedure for urinary incontinence. Pressure flow studies are performed in a health care provider’s office, clinic, or hospital with local anesthesia.
Electromyography
Electromyography uses special sensors to measure the electrical activity of the muscles and nerves in and around the bladder and the sphincters. If the health care provider thinks the urinary problem is related to nerve or muscle damage, the person may be given an electromyography. The sensors are placed on the skin near the urethra and rectum or on a urethral or rectal catheter. Muscle and nerve activity is recorded on a machine. The patterns of the nerve impulses show whether the messages sent to the bladder and sphincters are coordinated correctly. Electromyography is performed by a specially trained technician in a health care provider’s office, outpatient clinic, or hospital. Anesthesia is not needed if sensors are placed on the skin. Local anesthesia is needed if sensors are placed on a urethral or rectal catheter.
Video Urodynamic Tests
Video urodynamic tests take pictures and videos of the bladder during filling and emptying. The imaging equipment may use x-rays or ultrasound. If x-ray equipment is used, the bladder will be filled with a special fluid, called contrast medium, that shows up on x-rays. X-rays are performed by an x-ray technician in a health care provider’s office, outpatient facility, or hospital; anesthesia is not needed. If ultrasound equipment is used, the bladder is filled with warm water and harmless sound waves are used to create a picture of the bladder. The pictures and videos show the size and shape of the bladder and help the health care provider understand the problem. Bladder ultrasounds are performed in a health care provider’s office, radiology center, or hospital by a specially trained technician and interpreted by a doctor, usually a radiologist. Although anesthesia is not needed for the ultrasound, local anesthesia is needed to insert the catheter to fill the bladder.
Urodynamics test side effects
There is a small risk of urinary tract infection (less than 1%). Your urine will be tested on arrival to minimize this risk. An antibiotic may be prescribed for 1 or 2 days to prevent infection, but not always. People with signs of infection—including pain, chills, or fever—should call their health care provider immediately.
Dysuria (burning urination) for 24 hours.
Slight blood staining of the urine for 24 hours.