Contents
What is vasopressin
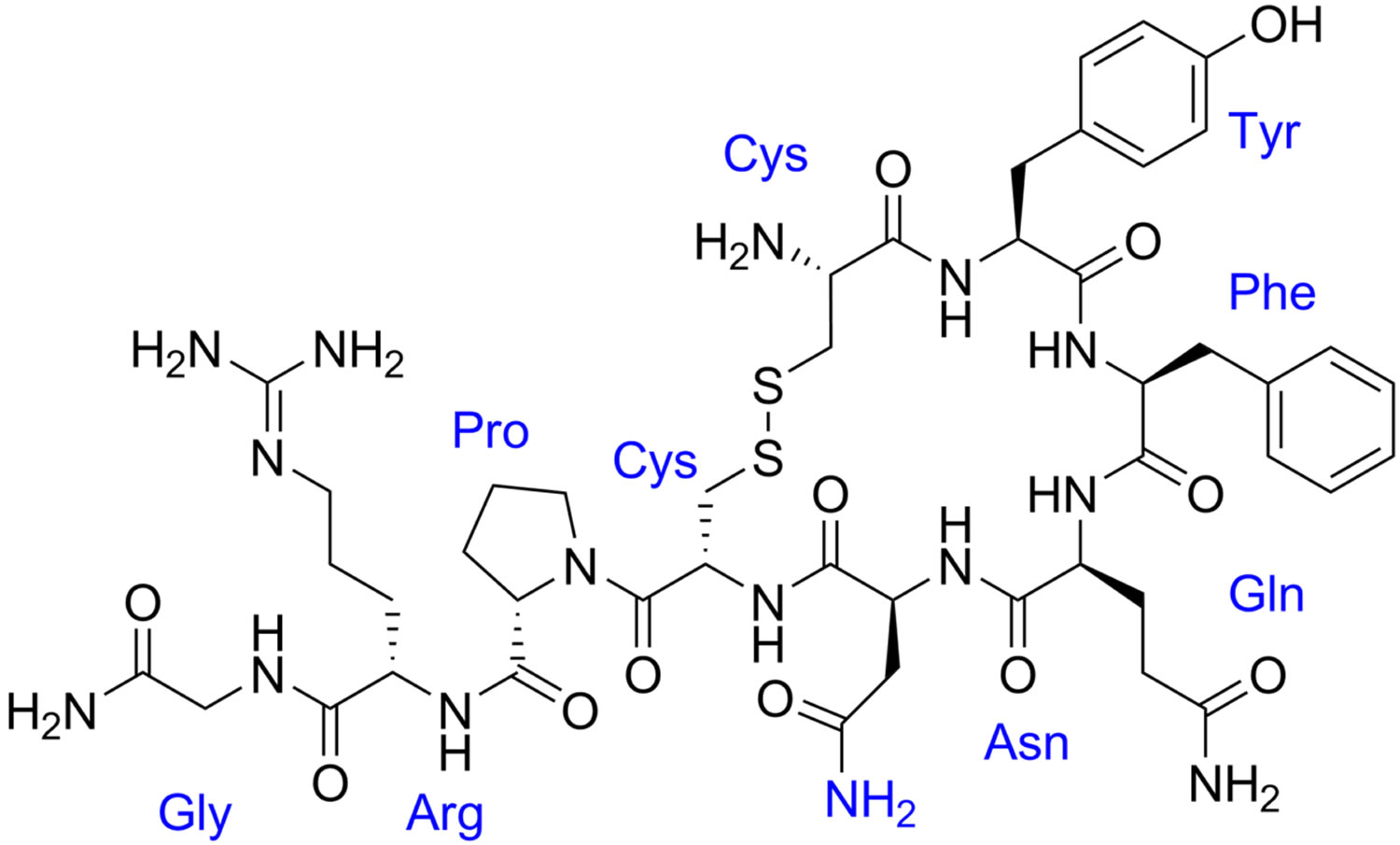
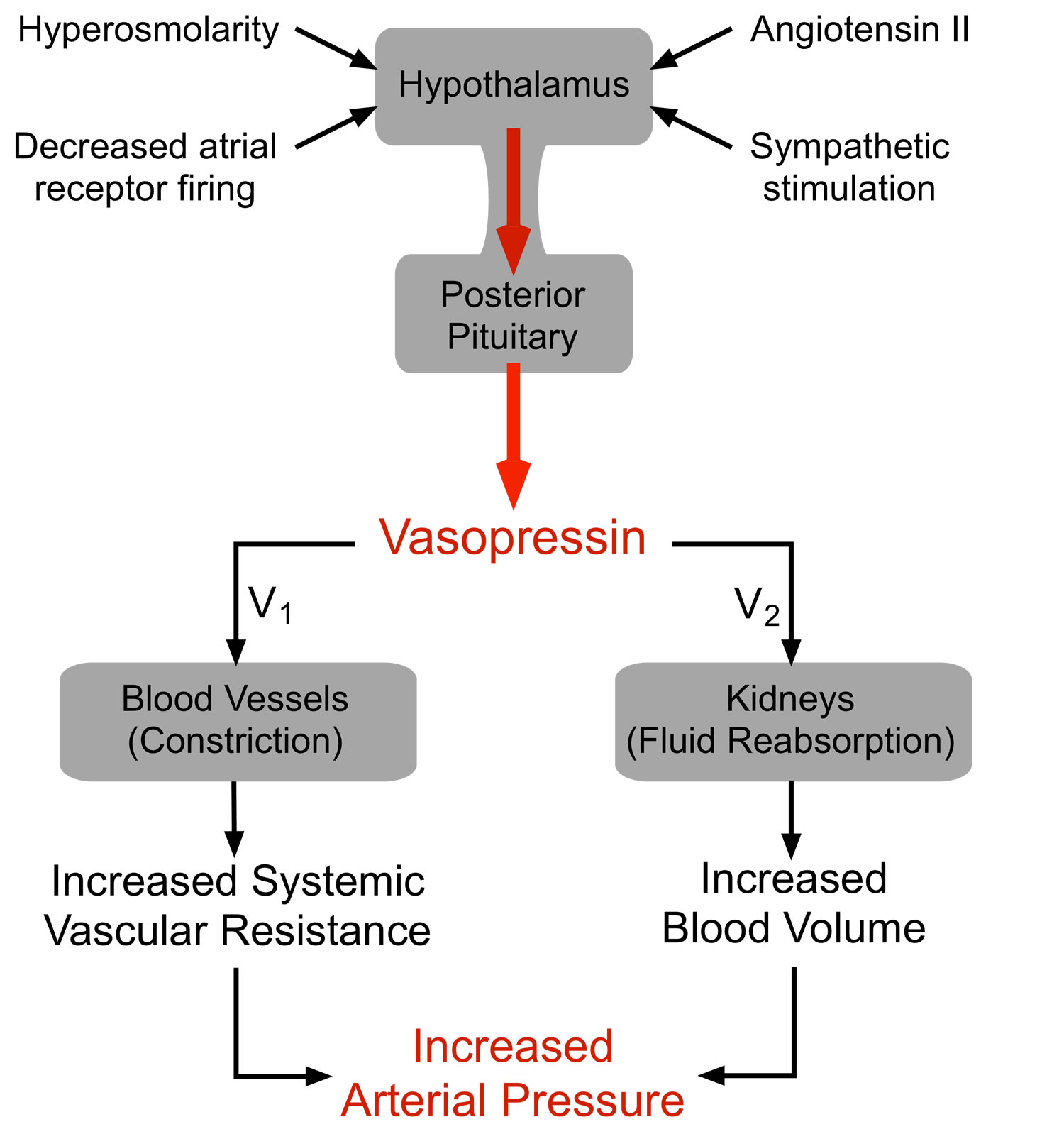
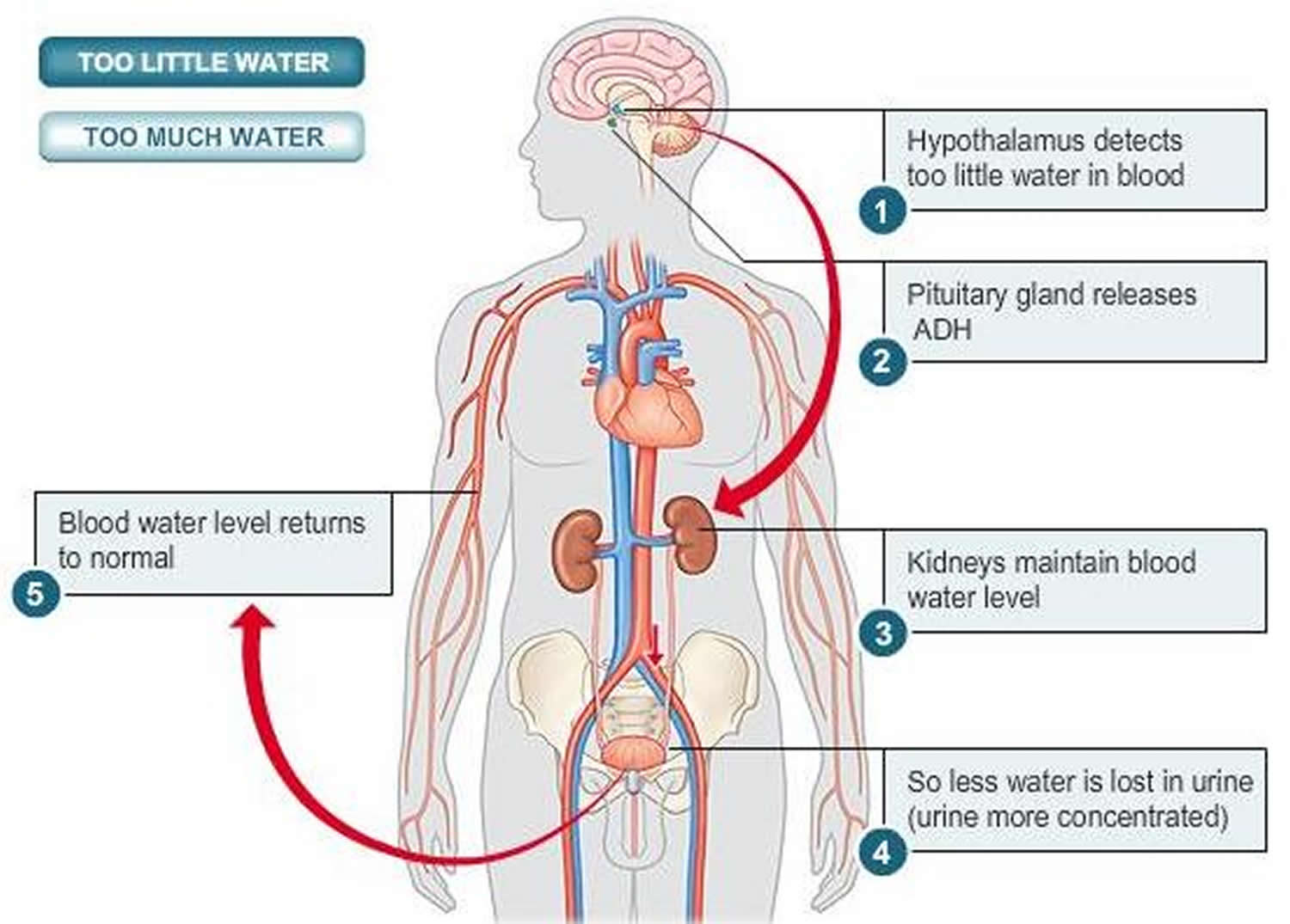
Vasopressin also called arginine vasopressin is a man-made form of a hormone called anti-diuretic hormone (ADH). Vasopressin is produced by the hypothalamus and stored in the posterior pituitary gland until needed. Vasopressin is a nonapeptide containing an arginine at residue 8 and two disulfide-linked cysteines at residues of 1 and 6 1 and is synthesized by the magnocellular neurons of the hypothalamus 2. The hypothalamus is an area of the brain that controls mood and appetite. The pituitary gland is located below your brain, behind the bridge of your nose. Vasopressin acts on your kidneys and blood vessels. Vasopressin regulates the level of water in your body by controlling the amount of urine your kidneys produce. When the level of water in your body decreases, your posterior pituitary gland releases vasopressin to conserve water by helping your kidneys reabsorb water into your body and stop the production of urine preventing loss of water from your body (antidiuretic effect). Vasopressin also raises blood pressure by narrowing blood vessels (vasopressor effect) 3. The antidiuretic effect of vasopressin has been exploited clinically for over half a century to treat diabetes insipidus, which is caused by a lack of a naturally occurring pituitary hormone in the body. In diabetes insipidus, vasopressin fails to properly regulate your body’s level of water, and allows too much urine to be produced and passed from your body 4. Only recently has vasopressin emerged as a therapy for shock states, renewing interest in the cardiovascular effects of vasopressin. Vasopressin is also used to treat or prevent certain conditions of the stomach after surgery or during abdominal x-rays.
Vasopressin can cause contraction of smooth muscle of the gastrointestinal tract and of all parts of the vascular bed, especially the capillaries, small arterioles and venules with less effect on the smooth musculature of the large veins. The direct effect on the contractile elements is neither antagonized by adrenergic blocking agents nor prevented by vascular denervation.
Figure 1. Vasopressin mechanism of action
Shock states (hypotension and hypovolemia) induce an increase in vasopressin levels from 20- to 200-fold 5. These supraphysiologic arginine vasopressin levels cause profound vasoconstriction and help to maintain end-organ perfusion 6. Prolonged shock is associated with a fall in vasopressin levels 7, probably due to depletion of vasopressin stores 8 and may contribute to the refractory hypotension (low blood pressure) that is seen in advanced shock states. Paradoxically, vasopressin has also been demonstrated to cause vasodilation (dilate blood vessels) in some vascular beds 9, distinguishing arginine vasopressin hormone from other vasoconstrictor agents.
The majority of a dose of vasopressin is metabolized and rapidly destroyed in the liver and kidneys. Vasopressin has a plasma half-life of about 10 to 20 minutes. Approximately 5% of a subcutaneous dose of Vasopressin is excreted in urine unchanged after 4 hours.
Oxytocin and vasopressin
Oxytocin differs from vasopressin by only one amino acid (80% homology), they have clearly divergent physiologic activity. Vasopressin is involved in osmotic and cardiovascular homeostasis, whereas oxytocin is important in parturition, lactation, and sexual behavior. Oxytocin and vasopressin are synthesized and stored in the pituitary gland, where these peptides are thought to remain in vesicles until released as the nine amino acid forms. However, these molecules also may be released from axons within the brain and spinal cord (central nervous system) 10, as well as from the neuronal soma and dendrites or by diffusion within the brain 11. In addition, oxytocin and vasopressin are made throughout the body with local effects on diverse tissues, including the uterus, testes, digestive system, kidney, and thymus 12.
Oxytocin and vasopressin are genetic and biochemical siblings 13. Both originated from a single ancestral gene that produced vasotocin 14. Vasotocin is found in reptiles and other vertebrates and can be measured in the mammalian fetus. Oxytocin and vasopressin differ from vasotocin by one amino acid and from each other by two amino acids. It is estimated that the ancestral peptides arose over 500 million years ago, that vasopressin evolved approximately 200 million years ago and oxytocin approximately 100 million years ago, originally through gene duplication 15. The genes for oxytocin and vasopressin reside near each other on human chromosome 20, lying in opposite transcriptional orientations 16.
Compared with oxytocin, vasopressin is the more primitive molecule and closer in function to vasotocin 16. However, other oxytocin-like peptides, including mesotocin and isotocin, have functions that resemble those of oxytocin. Animals that evolved from reptiles, including mammals and birds may be particularly dependent on selective social behaviors and oxytocin-like peptides for reproduction and survival.
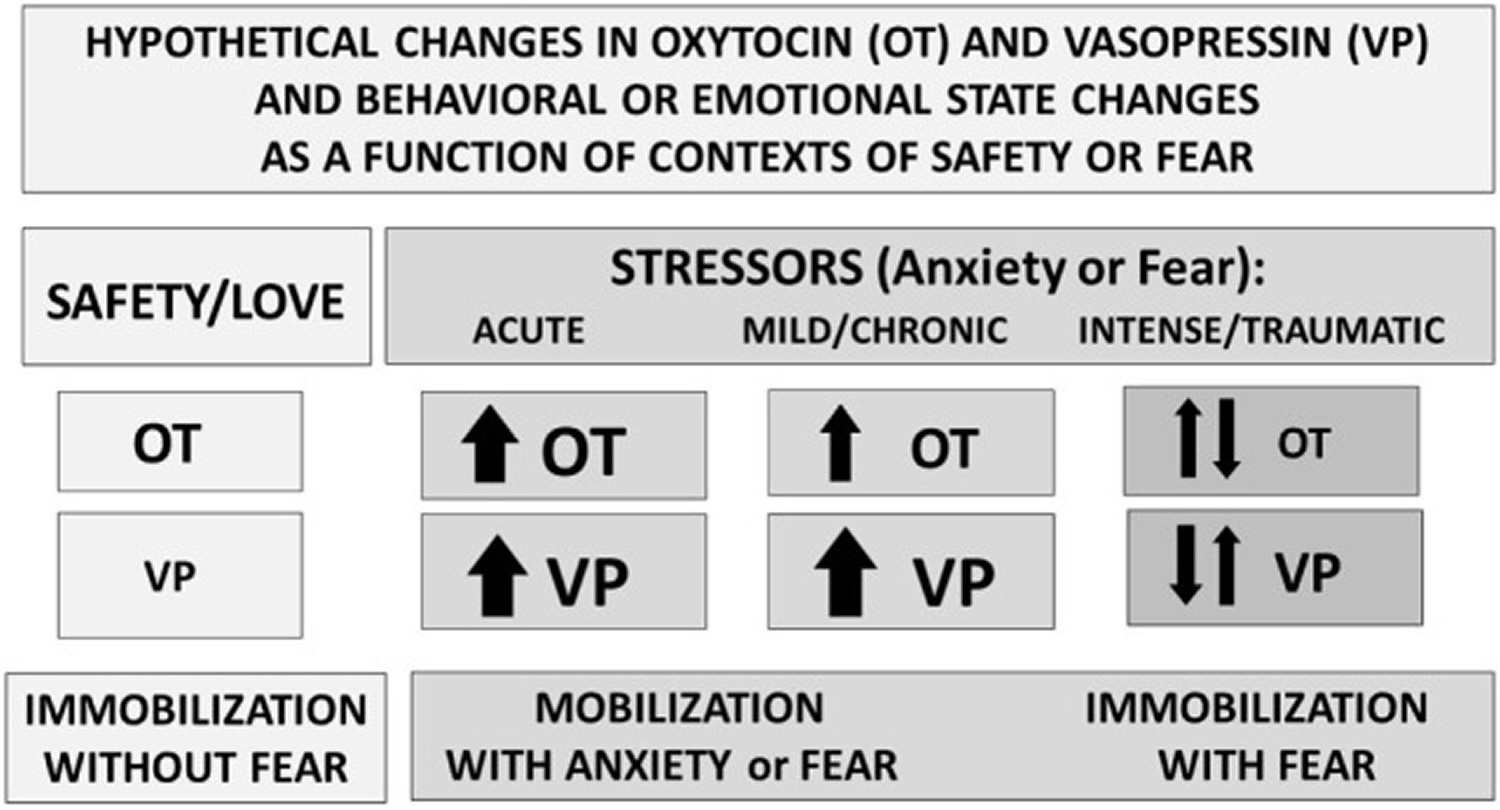
Vasopressin-like molecules are critical to adaptation and water balance under difficult environmental conditions. Vasopressin can support sympathetic arousal, mobilization (flight–flight responses) or in more extreme cases a metabolically conservative, shutdown response 17. Thus, under conditions of extreme stress or trauma, vasopressin may take precedent over oxytocin and over survival strategies that are more prosocial or mobilized (Figure 2). However, the benefits of either sociality or oxytocin also may be most easily detected in the presence of a stressor or of vasopressin 18.
Oxytocin and vasopressin are small peptides that are similar in structure. Both consist of nine amino acids in a six amino acid ring, formed by cysteine bonds, and a three amino acid tail with a terminal amine group. The precursors for oxytocin and vasopressin consist of 12 amino acids and are synthesized and released in conjunction with carrier proteins (neurophysin 1 and 2, respectively). The precursors are later cleaved into the “mature” forms of these peptides. It is also possible that precursors and fragments of oxytocin and vasopressin have unidentified functions 19; although not well studied, it is likely that these forms and the binding of oxytocin and vasopressin in blood and other tissues play a role in the functional interactions of oxytocin and vasopressin 20.
Oxytocin and arginine vasopressin are primarily synthesized in brain regions that are critical to behavioral and physiological homeostasis. Different cells in specific brain regions produce these two peptides, including the supraoptic nucleus (SON) and paraventricular nucleus (PVN) of the hypothalamus 10. Anatomical studies in rodents indicate that oxytocin and vasopressin are synthesized in discrete areas and in separate cells within the paraventricular nucleus (PVN) and supraoptic nucleus (SON); these cells also produce a network of neural projections reaching throughout the brain and spinal cord 11.
Research using brain slices 21 indicates that in other brain regions, including the amygdala and the bed nucleus of the stria terminalis, both oxytocin and vasopressin containing cells and projections lie adjacent to each other. These oxytocin–vasopressin associations form local functional units, capable of rapid and often opposite interactions—for example, in brain regions associated with fear versus fear reduction. Fear responses are mediated by V1aRs in the amygdala, while oxytocin may act to inhibit fear, depending on context (Figure 2) and gender 22.
Figure 2. Oxytocin and vasopressin hypothetical functions
Footnotes: Perceived context and the intensity of challenge can regulate the release or effects of oxytocin (OT) and vasopressin (VP). Under conditions of safety, the actions of oxytocin (OT) may dominate, supporting high levels of sociality. In response to an acute stressor, both oxytocin (OT) and vasopressin (VP) increase, supporting mobilization and escape, followed in some cases by increases in social behavior especially toward “safe” conspecifics. Following intense or traumatic stressors, initial responses would include mobilization and anxiety. However, following a traumatic experience, individuals may vacillate between mobilization and immobilization with fear or revert to the more primitive response of shutting down. These patterns differ between males and females and as a function of individual life histories.
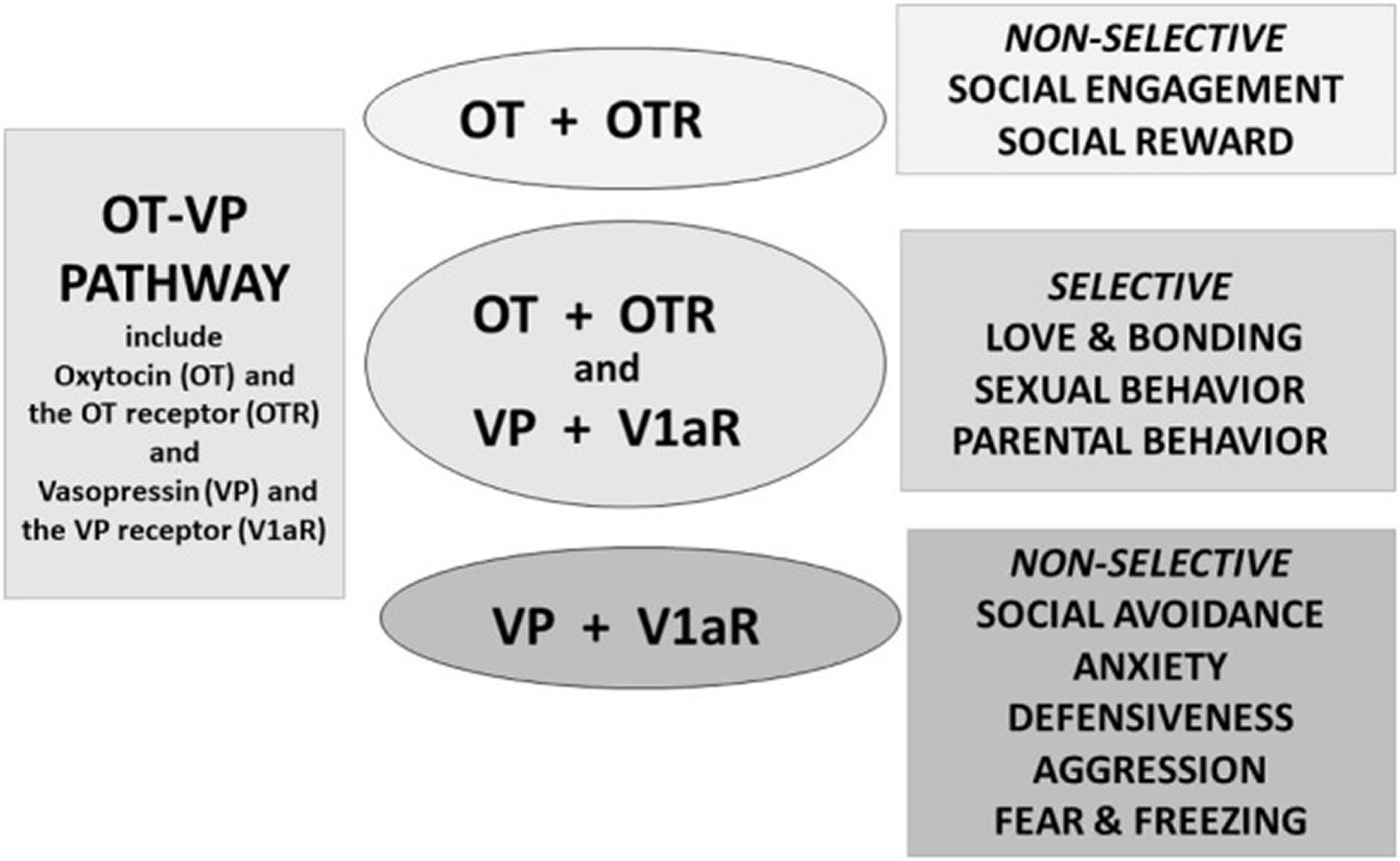
[Source 13]Combined actions of oxytocin and vasopressin
At the core of positive social behaviors are neurobiological systems that regulate fear and threats versus safety (Figures 2 and 3). Oxytocin typically supports immobilization without fear, necessary in interactions with family and friendly associates 23. Vasopressin supports mobilization, and in some cases defensive aggression and protection of social boundaries. By contrast, vasopressin, in conjunction with corticotropin-releasing hormone (CRH), dopamine and many other molecules, may support active and mobilized coping strategies 24. However, as with many features of the oxytocin–vasopressin pathway, exceptions exist—possibly because of the capacity of oxytocin and vasopressin to interact with each other’s receptors (Figure 3).
Increasing evidence suggests that the actions of oxytocin on the vasopressin 1a receptor (V1aR), versus the oxytocin receptor (OTR), vary depending on the behavior and context being examined 25 (Figure 3). In hamsters, fear-based or aggressive effects of oxytocin rely on the vasopressin 1a receptor (V1aR) and social reward on the oxytocin receptor (OTR) 26. The capacity of oxytocin and vasopressin to bind to each other’s receptors adds complexity to attempts to understand both peptides. However, oxytocin–vasopressin interactions also are adaptive, increasing the capacity for a small number of peptides and receptors to regulate various processes across different tissues.
Both oxytocin and vasopressin are responsive to environmental and social demands, although in somewhat different ways 27. These peptides—presumably via interactions with their receptors—may have diverse physiological and behavioral properties. Regional effects of oxytocin and vasopressin are expected and need to be investigated to fully understand the functional consequences for these peptides. Dynamic interactions either on specific receptors, due to brain region-specific actions, or due to relative availability of the peptides to a receptor 10 could help to explain the behavioral properties of these two molecules. In addition, refined behavioral studies are necessary, since the effects of oxytocin and vasopressin on various behaviors change across time and as behavioral context changes.
Figure 3. Oxytocin and vasopressin in human behavior
Footnotes: Oxytocin (OT) and vasopressin (VP) are components of an integrated pathway. Oxytocin (OT) and vasopressin (VP) interact dynamically with receptors [including the oxytocin receptor (OTR) or vasopressin 1a receptor (V1aR)] to influence social engagement and defensive behaviors. In many cases, oxytocin (OT) acts in conjunction with vasopressin (VP), via the V1aR or through effects on both the oxytocin receptor (OTR) and vasopressin 1a receptor (V1aR), thus regulating the capacity to form selective social behaviors. Oxytocin (OT) rarely acts alone but, especially under nonthreatening or “safe” conditions, may facilitate features of “love,” including social engagement, and social reward, and “immobility without fear”.
[Source 13]Summary
Across the lifespan, the effects of oxytocin and vasopressin dynamically interact to adjust to and influence the perception of fear and safety 13. Vasopressin is the evolutionarily older molecule with presumably the older receptors. Vasopressin is implicated in mobilized behaviors including defense of self and the family. Among the patterns of behavior for which both oxytocin and vasopressin may be necessary are sexual behavior 28, paternal behavior, and pair bonding 29. Oxytocin is of special relevance to adaptations that involve high levels of sociality, a sense of psychological safety within a family or familiar social group, as well as emotional regulation and higher levels of rational cognition 30. Furthermore, working together oxytocin and vasopressin, and their receptors, create a biological and genetic pathway that regulates attachment and bonding, which in turn may be protective against threats or other forms of challenge.
The nature of interactions of oxytocin and vasopressin at their receptors needs further study, especially in vivo and the epigenetic context of development 31. There is considerable interest in using oxytocin-like molecules as therapeutics. However, the evolved and dynamic features of the oxytocin–vasopressin pathway create difficulties for attempts to study oxytocin and vasopressin independently. These also pose challenges for the usefulness of drugs based on this system, including those commonly used around the time of birth, such as synthetic forms of oxytocin, which may affect both the oxytocin and vasopressin receptors 13.
Vasopressin uses
Vasopressin is used to control the symptoms of a certain type of diabetes insipidus (‘water diabetes’; condition in which the body produces an abnormally large amount of urine). Following subcutaneous or intramuscular administration of Vasopressin injection, the duration of antidiuretic activity is variable but effects are usually maintained for 2 to 8 hours. Vasopressin is also used for vasodilatory shock states and to treat hypotension, to increase blood pressure in patients with vasodilatory shock (e.g., post-cardiotomy or sepsis) who remain hypotensive despite fluids and catecholamines. Vasopressin is also used to control excessive thirst and the passage of an abnormally large amount of urine that may occur after a head injury or after certain types of surgery. Vasopressin is also used to treat or prevent certain conditions of the stomach after surgery or during abdominal x-rays.
How is vasopressin given?
Vasopressin is injected into a muscle or under the skin, or into a vein through an IV. A healthcare provider will give you this injection. Since this medication is given by a healthcare professional in a medical setting, an overdose is unlikely to occur.
Vasopressin is usually given as needed to help control your condition. The time interval between doses will depend on how your body responds to the medication.
To treat diabetes insipidus, vasopressin is sometimes given into the nose by nasal spray or medicine dropper, or insertion of a cotton pad that has been soaked in vasopressin.
When used for abdominal x-ray, vasopressin injections are usually given at 2 hours before and 30 minutes before your x-ray. Your doctor may also recommend you receive an enema before you receive your first dose of vasopressin.
Vasopressin can cause temporary side effects such as nausea, stomach pain, or “blanching” of your skin (pale spots when you press on the skin).
Drinking 1 or 2 glasses of water each time you receive an injection may help ease these side effects. If you are receiving this medicine in your vein through an IV, you may be told not to drink water for a certain period of time.
While using vasopressin, you may need frequent blood tests. Your heart function may also need to be checked using an electrocardiograph or ECG (sometimes called an EKG).
Follow your doctor’s instructions about the amount of liquids you should drink during your treatment with vasopressin. In some cases, drinking too much liquid can be as unsafe as not drinking enough.
Vasopressin dose
You should not be treated with vasopressin if you are allergic to it. To make sure vasopressin is safe for you, tell your doctor if you have:
- coronary artery disease (hardened arteries);
- congestive heart failure;
- kidney disease;
- asthma;
- migraine headaches; or
- epilepsy or other seizure disorder.
Tell your doctor if you are pregnant. Vasopressin can cause premature labor contractions if you receive vasopressin during the second or third trimester of pregnancy.
It is not known whether vasopressin passes into breast milk or if it could harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
Adult Dose for Hypotension
Post-Cardiotomy Shock:
- Initial dose: 0.03 units/min IV infusion
- If target blood pressure response is not achieved: titrate up by 0.005 units/min at 10 to 15 minute intervals
- Maximum dose: 0.1 units/min
Septic Shock:
- Initial dose: 0.01 units/min IV infusion
- If target blood pressure response is not achieved: titrate up by 0.005 units/min at 10 to 15 minute intervals
- Maximum dose: 0.07 units/min
Comments:
- After target blood pressure has been maintained for 8 hours without use of catecholamines, taper by 0.005 units/min every hour as tolerated to maintain target blood pressure.
- The goal of treatment is optimization of perfusion to critical organs, however, aggressive treatment can compromise perfusion of organs; titrate to the lowest dose compatible with a clinically acceptable response.
Use: To increase blood pressure in patients with vasodilatory shock (e.g., post-cardiotomy or sepsis) who remain hypotensive despite fluids and catecholamines.
Adult Dose for Shock
Post-Cardiotomy Shock:
- Initial dose: 0.03 units/min IV infusion
- If target blood pressure response is not achieved: titrate up by 0.005 units/min at 10 to 15 minute intervals
- Maximum dose: 0.1 units/min
Septic Shock:
- Initial dose: 0.01 units/min IV infusion
- If target blood pressure response is not achieved: titrate up by 0.005 units/min at 10 to 15 minute intervals
- Maximum dose: 0.07 units/min
Comments:
- After target blood pressure has been maintained for 8 hours without use of catecholamines, taper by 0.005 units/min every hour as tolerated to maintain target blood pressure.
- The goal of treatment is optimization of perfusion to critical organs, however, aggressive treatment can compromise perfusion of organs; titrate to the lowest dose compatible with a clinically acceptable response.
Use: To increase blood pressure in patients with vasodilatory shock (e.g., post-cardiotomy or sepsis) who remain hypotensive despite fluids and catecholamines.
Adult Dose for Diabetes Insipidus
- 5 to 10 units (0.25 to 0.5 mL) IM or subcutaneously repeated 2 or 3 times a day as needed.
Comments:
- May be administered intranasally on cotton pledgets, by nasal spray, or by dropper as well; the dose and interval between treatments must be determined for each patient.
- This drug has not been found by the by the US FDA to be safe and effective and the labeling has not been approved by the US FDA.
Adult Dose for Abdominal Distension
- 5 units (0.25 mL) IM or subcutaneously initially; increase to 10 units (0.5 mL) at subsequent injections if necessary and repeated at 3 to 4 hour intervals as required
Comments:
- This drug has not been found by the by the US FDA to be safe and effective and the labeling has not been approved by the US FDA.
Adult Dose for Abdominal Radiological Procedure
- 2 injections of 10 units (0.5 mL) each IM or subcutaneously given 2 hours and one-half hour, respectively, before films are exposed
Comments:
- This drug has not been found by the by the US FDA to be safe and effective and the labeling has not been approved by the US FDA.
- Some radiologists advise giving an enema prior to the first injection.
Renal Dose Adjustments
- Data not available
Liver Dose Adjustments
- Data not available
Vasopressin side effects
Along with its needed effects, vasopressin may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking vasopressin:
- Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Tell your doctor right away if you have:
- chest pain or tight feeling;
- severe or pounding headache, severe drowsiness, feeling very weak;
- slow heart rate, weak pulse, fainting, slow breathing;
- loss of color in your lips or around your mouth;
- numbness or tingling in your hands or feet; or
- pain or loss of feeling anywhere in your body.
Common side effects may include:
- slow heartbeats;
- pale skin, numbness in your fingers or toes;
- stomach pain, gas, nausea, vomiting;
- dizziness, headache;
- sweating; or
- rash.
Side effects were reported on a voluntary basis from a population of uncertain size and it is therefore not possible to estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular
- Frequency not reported: Right heart failure, atrial fibrillation, bradycardia, myocardial ischemia, cardiac arrest, shock, circumoral pallor, arrhythmia, cardiac output decreased, angina, peripheral vasoconstriction, distal limb ischemia, chest pain, hypertension
Dermatologic
- Frequency not reported: Gangrene, sweating, cutaneous gangrene, ischemic lesions, urticaria
Gastrointestinal
- Frequency not reported: Mesenteric ischemia, abdominal cramps, nausea, vomiting, gas
Renal
- Frequency not reported: Acute renal insufficiency
Nervous system
- Frequency not reported: Tremor, head pounding
Respiratory
- Frequency not reported: Bronchial constriction, bronchospasm
Hematologic
- Frequency not reported: Hemorrhagic shock, platelets decreased, intractable bleeding
Immunologic
- Frequency not reported: Anaphylaxis, hypersensitivity
Musculoskeletal
- Frequency not reported: Rhabdomyolysis
Metabolic
- Frequency not reported: Water intoxication, hyponatremia, fluid retention
Hepatic
- Frequency not reported: Bilirubin increased
Other
- Frequency not reported: Vertigo
This is not a complete list of side effects and others may occur.
Drug Interactions
The following drugs may potentiate the antidiuretic effect of Vasopressin when used concurrently: carbamazepine; chlorpropamide; clofibrate; urea; fludrocortisone; tricyclic antidepressants.
The following drugs may decrease the antidiuretic effect of Vasopressin when used concurrently: demeclocycline; norepinephrine; lithium; heparin; alcohol.
Ganglionic blocking agents may produce a marked increase in sensitivity to the pressor effects of Vasopressin.
- Structural bases of vasopressin/oxytocin receptor function. Barberis C, Mouillac B, Durroux T. J Endocrinol. 1998 Feb; 156(2):223-9. http://joe.endocrinology-journals.org/content/156/2/223.long[↩]
- Distribution of oxytocin and vasopressin in the rat supraoptic and paraventricular nucleus. Swaab DF, Nijveldt F, Pool CW. J Endocrinol. 1975 Dec; 67(3):461-2.[↩]
- Du Vigneaud V, Gash DT, Katsoyannis PG. A synthetic preparation possessing biological properties associated with argininevasopressin. J Am Chem Soc. 1954;76:4751–4752.[↩]
- Holmes CL, Landry DW, Granton JT. Science Review: Vasopressin and the cardiovascular system part 1 – receptor physiology. Critical Care. 2003;7(6):427-434. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC374366/[↩]
- The effects of hypotension and hypovolaemia on the liberation of vasopressin during haemorrhage in the unanaesthetized monkey (Macaca mulatta). Arnauld E, Czernichow P, Fumoux F, Vincent JD. Pflugers Arch. 1977 Nov 23; 371(3):193-200.[↩]
- Role of vasopressin in cardiovascular and blood pressure regulation. Abboud FM, Floras JS, Aylward PE, Guo GB, Gupta BN, Schmid PG. Blood Vessels. 1990; 27(2-5):106-15. https://www.ncbi.nlm.nih.gov/pubmed/2242439/[↩]
- Reversal by vasopressin of intractable hypotension in the late phase of hemorrhagic shock. Morales D, Madigan J, Cullinane S, Chen J, Heath M, Oz M, Oliver JA, Landry DW. Circulation. 1999 Jul 20; 100(3):226-9.[↩]
- The pathogenesis of vasodilatory shock. Landry DW, Oliver JA. N Engl J Med. 2001 Aug 23; 345(8):588-95.[↩]
- Mechanisms underlying arginine vasopressin-induced relaxation in monkey isolated coronary arteries. Okamura T, Ayajiki K, Fujioka H, Toda N. J Hypertens. 1999 May; 17(5):673-8.[↩]
- Chini B, Verhage M, Grinevich V. The action radius of oxytocin release in the mammalian CNS: from single vesicles to behavior. Trends Pharmacol Sci (2017) 38(11):982–91.10.1016/j.tips.2017.08.005[↩][↩][↩]
- Grinevich V, Knobloch-Bollmann HS, Eliava M, Busnelli M, Chini B. Assembling the puzzle: pathways of oxytocin signaling in the brain. Biol Psychiatry (2016) 79:155–64.10.1016/j.biopsych.2015.04.013[↩][↩]
- Geenen V. Thymus-dependent T cell tolerance of neuroendocrine functions: principles, reflections, and implications for tolerogenic/negative self-vaccination. Ann N Y Acad Sci (2006) 1088:284–96.10.1196/annals.1366.009[↩]
- Carter CS. The Oxytocin–Vasopressin Pathway in the Context of Love and Fear. Frontiers in Endocrinology. 2017;8:356. doi:10.3389/fendo.2017.00356. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5743651/[↩][↩][↩][↩][↩]
- Goodson JL, Kingsbury MA. What’s in a name? Considerations of homologies and nomenclature for vertebrate social behavior networks. Horm Behav (2013) 64:103–12.10.1016/j.yhbeh.2013.05.006[↩]
- Acher R, Chauvet J, Chauvet MT. Man and the chimaera. Selective versus neutral oxytocin evolution. Adv Exp Med Biol (1995) 395:615–27[↩]
- Gainer H. Cell-type specific expression of oxytocin and vasopressin genes: an experimental odyssey. J Neuroendocrinol (2012) 24:528–38.10.1111/j.1365-2826.2011.02236.x[↩][↩]
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication and Self-Regulation. New York, NY: WW Norton and Co; 2011[↩]
- Carter CS. Neuroendocrine perspectives on social attachment and love. Psychoneuroendocrinology (1998) 23:779–818.10.1016/S0306-4530(98)00055-9[↩]
- de Wied D, Elands J, Kovacs G. Interactive effects of neurohypophyseal neuropeptides with receptor antagonists on passive avoidance behavior: mediation by a cerebral neurohypophyseal hormone receptor? Proc Natl Acad Sci U S A (1991) 88:1494–8.10.1073/pnas.88.4.1494[↩]
- Yee JR, Kenkel WM, Frijling JL, Dodhia S, Onishi KG, Tovar S, et al. Oxytocin promotes functional coupling between paraventricular nucleus and both sympathetic and parasympathetic cardioregulatory nuclei. Horm Behav (2016) 80:82–91.10.1016/j.yhbeh.2016.01.010[↩]
- Stoop R, Hegoburu C, Van Den Burg E. New opportunities in vasopressin and oxytocin research: a perspective from the amygdala. Annu Rev Neurosci (2015) 38:369–88.10.1146/annurev-neuro-071714-033904[↩]
- Dumais KM, Veenema AH. Vasopressin and oxytocin receptor systems in the brain: sex differences and sex-specific regulation of social behavior. Front Neuroendocrinol (2016) 40:1–23.10.1016/j.yfrne.2015.04.003[↩]
- Porges SW. Love: an emergent property of the mammalian autonomic nervous system. Psychoneuroendocrinology (1998) 23:837–61.10.1016/S0306-4530(98)00057-2[↩]
- Herman JP, Tasker JG. Paraventricular hypothalamic mechanisms of chronic stress adaptation. Front Endocrinol (2016) 7:137.10.3389/fendo.2016.00137[↩]
- Albers HE. Species, sex and individual differences in the vasotocin/vasopressin system: relationship to neurochemical signaling in the social behavior neural network. Front Neuroendocrinol (2015) 36:49–71.10.1016/j.yfrne.2014.07.001[↩]
- Song Z, Larkin TE, Malley MO, Albers HE. Oxytocin (OT) and arginine-vasopressin (Avp) act on OT receptors and not Avp V1a receptors to enhance social recognition in adult Syrian hamsters (Mesocricetus auratus). Horm Behav (2016) 81:20–7.10.1016/j.yhbeh.2016.02.004[↩]
- Neumann ID, Slattery DA. Oxytocin in general anxiety and social fear: a translational approach. Biol Psychiatry (2016) 79:213–21.10.1016/j.biopsych.2015.06.004[↩]
- Carter CS. Oxytocin and sexual behavior. Neurosci Biobehav Rev (1992) 16:131–44.10.1016/S0149-7634(05)80176-9[↩]
- Carter CS. Oxytocin and human evolution. Curr Top Behav Neurosci (2017).10.1007/7854_2017_18[↩]
- Carter CS. Oxytocin pathways and the evolution of human behavior. Annu Rev Psychol (2014) 65:17–39.10.1146/annurev-psych-010213-115110[↩]
- Hammock EA. Developmental perspectives on oxytocin and vasopressin. Neuropsychopharmacology (2015) 40:24–42.10.1038/npp.2014.120[↩]