Contents
- Vitamin B1
- What does vitamin B1 (Thiamine) do?
- What are some effects of vitamin B1 on health?
- How much vitamin B1 do I need?
- What foods provide vitamin B1?
- Vitamin B1 (Thiamine) Supplements
- Thiamine (Vitamin B1) Deficiency
Vitamin B1
Vitamin B1 also known as thiamin or thiamine, is one of the water-soluble B vitamins. Vitamin B1 or thiamine is naturally present in some foods, added to some food products, and available as a dietary supplement. Vitamin B1 or thiamine plays a critical role in energy metabolism and, therefore, in the growth, development, and function of cells 1. Foods rich in vitamin B1 or thiamine include whole grains, brown rice, lean pork, poultry, eggs, fish, soybean, nuts, dried beans, peas, and fortified or enriched grain products such as cereals, infant formulas, and bread 2, 3, 4. Multivitamins will provide an additional 1.5 mg of thiamine on top of a diet rich in thiamine 5.
Ingested vitamin B1 or thiamine from food and dietary supplements is absorbed by the small intestine through active transport at nutritional doses and by passive diffusion at pharmacologic doses 6, 1. Most dietary vitamin B1 or thiamine is in phosphorylated forms, and intestinal enzyme phosphatase hydrolyzes them to free thiamin before the vitamin is absorbed by the small intestine 1. The remaining dietary vitamin B1 or thiamine is in free (absorbable) form 1, 7. Thiamine, a water-soluble vitamin, cannot be stored in appreciable amounts 8. Humans store vitamin B1 or thiamine primarily in the liver, but in very small amounts (approximately 30 mg) 9. Vitamin B1 or thiamine has a short half‐life of 14 to 18 days and body stores are limited, so people require a continuous supply of thiamine from the diet 10, 6, 11.
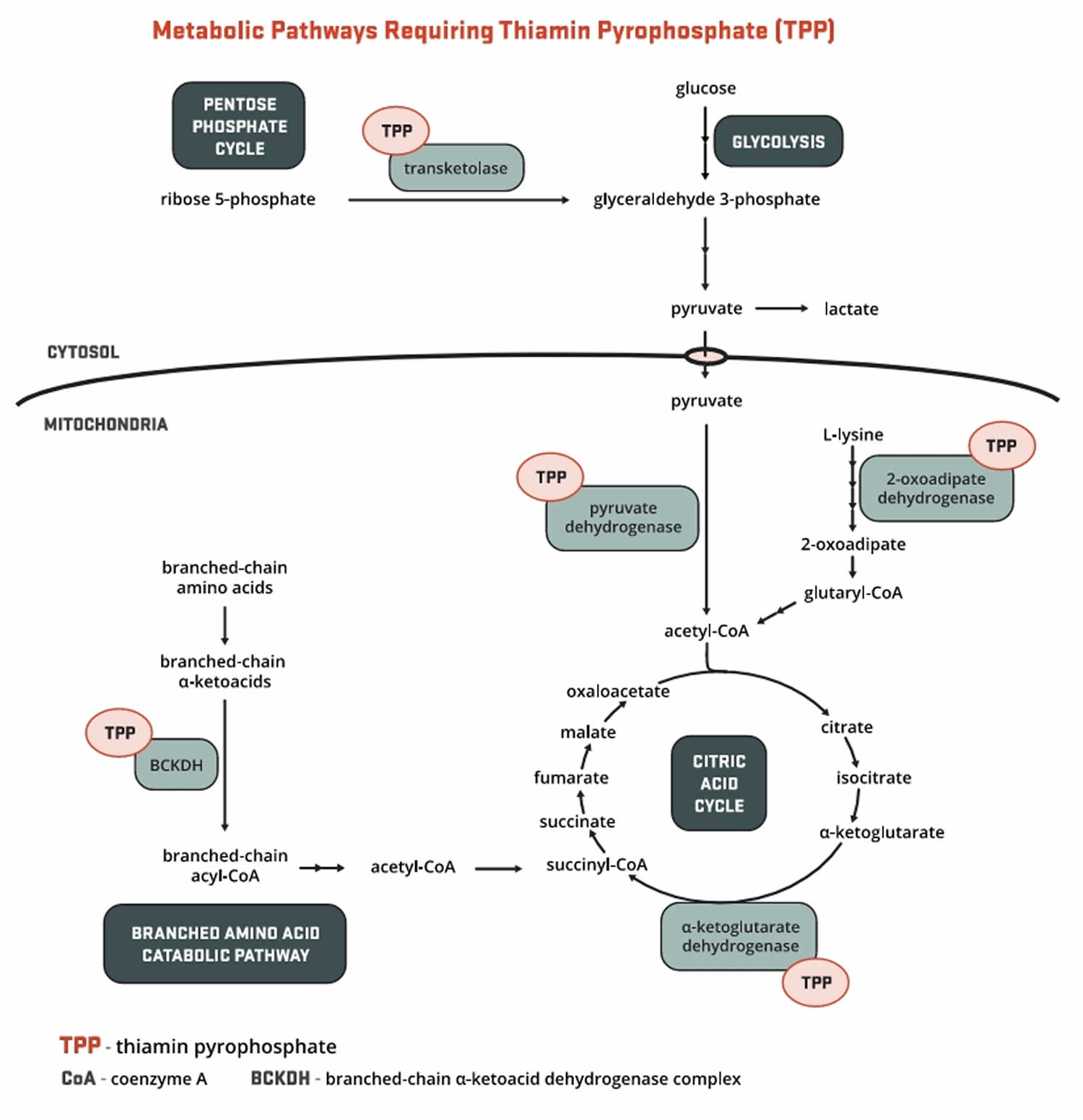
Vitamin B1 or thiamine is present in the body as free thiamine, as well as in several phosphorylated forms: thiamine monophosphate (TMP), thiamine diphosphate (TDP also known as thiamin pyrophosphate (TPP)), and thiamine triphosphate (TTP) 12, 13, 14. About 80% of the approximately 25–30 mg of vitamin B1 or thiamine in the adult human body is in the form of thiamin pyrophosphate (TPP) also known as thiamin diphosphate (TDP), the main metabolically active form of vitamin B1 or thiamine. Bacteria in the large intestine also synthesize free thiamin and thiamin pyrophosphate (TPP), but their contribution, if any, to thiamin nutrition is currently unknown 15. Thiamin pyrophosphate (TPP) serves as an essential cofactor for five enzymes involved in glucose, amino acid (proteins), and fatty acids (lipids) metabolism (Figure 1) 16, 1, 9.
Levels of vitamin B1 or thiamine in the blood are not reliable indicators of thiamin status. Thiamine status is often measured indirectly by assaying the activity of the transketolase enzyme, which depends on thiamin pyrophosphate (TPP), in red blood cell hemolysates in the presence and absence of added thiamin pyrophosphate (TPP) 9. The result, known as the “TPP effect,” reflects the extent of unsaturation of transketolase with TPP. The result is typically 0%–15% in healthy people, 15%–25% in those with marginal deficiency, and higher than 25% in people with thiamine deficiency. Another commonly used measure of vitamin B1 or thiamine status is urinary thiamine excretion, which provides data on dietary intakes but not tissue stores 17. For adults, excretion of less than 100 mcg/day vitamin B1 or thiamine in urine suggests insufficient thiamine intake, and less than 40 mcg/day indicates an extremely low intake 18.
Figure 1. Vitamin B1 (thiamine) function
Footnote: Major biochemical reactions requiring vitamin B1 or thiamine as a cofactor (a compound that is essential for the activity of an enzyme).
[Source 19 ]What does vitamin B1 (Thiamine) do?
Vitamin B1 or thiamine helps turn the food you eat into the energy you need. Thiamine is important for the growth, development, and function of the cells in your body.
About 80% of the approximately 25–30 mg of vitamin B1 or thiamine in the adult human body is in the form of thiamin pyrophosphate (TPP) also known as thiamin diphosphate (TDP), the main metabolically active form of vitamin B1 or thiamine. The synthesis of thiamin pyrophosphate (TPP) from free thiamine requires magnesium, adenosine triphosphate (ATP), and the enzyme, thiamin pyrophosphokinase 19. In humans, thiamin pyrophosphate (TPP) serves as an essential cofactor for five enzymes involved in glucose, amino acid (proteins), and fatty acids (lipids) metabolism (Figure 1) 16, 1, 9. Forms of thiamine are also needed for ribose synthesis and for α-oxidation of 3-methyl-branched fatty acids 19.
Pyruvate dehydrogenase, α-ketoglutarate dehydrogenase, 2-oxoadipate dehydrogenase, and branched-chain α-ketoacid dehydrogenase (BCKDH) each comprise a different enzyme complex found within cellular organelles called mitochondria 19. They catalyze the decarboxylation of pyruvate, α-ketoglutarate, 2-oxoadipate, and branched-chain amino acids (BCAAs) to form acetyl-coenzyme A (CoA), succinyl-CoA, glutaryl-CoA, and derivatives of branched-chain amino acid (BCAA), respectively (Figure 1). All products play critical roles in the production of energy from food through their connection to the citric acid (Krebs) cycle 20. Branched-chain amino acid (BCAA), including leucine, isoleucine, and valine, are eventually degraded into acetyl-CoA and succinyl-CoA to fuel the citric acid cycle. The catabolism of the three branched-chain amino acids (BCAAs) also contributes to the production of cholesterol and donates nitrogen for the synthesis of the neurotransmitters, glutamate and g-aminobutyric acid (GABA) 21. In addition to the thiamin coenzyme (thiamin pyrophosphate), each dehydrogenase complex requires a niacin-containing coenzyme (NAD), a riboflavin-containing coenzyme (FAD), and lipoic acid.
Transketolase catalyzes critical reactions in another metabolic pathway occurring in the cytosol, known as the pentose phosphate pathway 19. One of the most important intermediates of this pathway is ribose-5-phosphate, a phosphorylated 5-carbon sugar required for the synthesis of the high-energy ribonucleotides, such as ATP and guanosine triphosphate (GTP). Nucleotides are the building blocks of nucleic acids, DNA, and RNA 19. The pentose phosphate pathway also supplies various anabolic pathways, including fatty acid synthesis, with the niacin-containing coenzyme NADPH 22, 23. Because transketolase decreases early in thiamine deficiency and, unlike most thiamine-dependent enzymes, is present in red blood cells, measurement of its activity in red blood cells has been used to assess thiamine nutritional status 20, 24, 25.
2-Hydroxyacyl-CoA lyase is a thiamin pyrophosphate-dependent enzyme in peroxisomes that catalyzes the catabolism of 3-methyl-branched fatty acids through the process of α-oxidation, the oxidative removal of a single carbon atom from fatty acids like phytanic acid 26.
What are some effects of vitamin B1 on health?
Scientists are studying vitamin B1 or thiamine to better understand how it affects health. Here are some examples of what this research has shown.
Cataracts
A cross-sectional study of 2,900 Australian men and women, 49 years of age and older, found that those in the highest quintile of thiamin intake were 40% less likely to have nuclear cataracts than those in the lowest quintile 27. In addition, a study in 408 US women found that higher dietary intakes of vitamin B1 or thiamine were inversely associated with five-year change in lens opacification 28. However, these cross-sectional associations have yet to be elucidated by studies of causation.
Diabetes
People with diabetes have been reported to have low plasma concentrations and high renal clearance of thiamine, suggesting that individuals with type 1 or type 2 diabetes are at increased risk for thiamine deficiency 29, 30. Two thiamin transporters, thiamin transporter-1 (THTR-1) and thiamin transporter-2 (THTR-2), are involved in thiamine uptake by enterocytes in the small intestine and re-uptake in the proximal tubules of the kidneys. One study suggested that high blood sugar level (hyperglycemia) in patients with diabetes could affect thiamine re-uptake by decreasing the expression of thiamin transporters in the kidneys 31. Conversely, thiamine deficiency appears to impair the normal endocrine function of the pancreas and worsens hyperglycemia. Early studies showed that insulin synthesis and secretion were altered in the endocrine pancreatic cells of thiamine-deficient rats 32, 33. In humans, thiamine deficiency caused by recessive mutations in the gene encoding thiamin transporter-1 (THTR-1) leads to diabetes mellitus in the thiamine-responsive megaloblastic anemia syndrome 19.
The proportion of people with type 1 or type 2 diabetes who have poor thiamine status based on erythrocyte transketolase activity ranges from 17% to 79% in studies conducted to date 34. In a study of 76 consecutive patients with type 1 or type 2 diabetes, for example, 8% had mild thiamine deficiency and 32% had moderate thiamine deficiency based on assays of the transketolase enzyme 35.
Some small studies have shown that oral high-dose thiamine supplementation with 150–300 mg/day vitamin B1 or thiamine can decrease glucose levels in patients with type 2 diabetes or impaired glucose tolerance 36, 37. Vitamin B1 or thiamine supplementation prevented any further increase in fasting glucose and insulin concentrations compared with placebo treatment but did not reduce the hyperglycemia 37. One study suggested that vitamin B1 or thiamine supplementation might improve fasting glucose concentrations in in early stages of type 2 diabetes (i.e., pre-diabetes) 36. However, the authors of these studies did not assess the potential clinical significance of these findings 17.
A few small randomized studies have assessed the effects of benfotiamine (man made thiamine) supplements on diabetic neuropathy. Three studies found that, compared to placebo, 120–900 mg/day benfotiamine with or without other B-vitamins decreased the severity of neuropathy symptoms and lowered urinary albumin excretion (a marker of early-stage diabetic nephropathy) 38, 39, 40. However, another study found no effect of 900 mg/day benfotiamine on urinary excretion of albumin or kidney injury molecule-1, a marker of kidney injury 41.
Well-designed studies with larger sample sizes and longer durations are required to determine whether vitamin B1 or thiamine supplements can reduce glucose levels in patients with diabetes or decrease diabetic compications 17.
Heart failure
Severe thiamine deficiency (wet beriberi) can lead to impaired cardiac function and ultimately congestive heart failure 19. The rates of poor vitamin B1 or thiamine status in patients with congestive heart failure have ranged in studies from 21% to 98% 4. Explanations for this association include older age, comorbidities, insufficient dietary intake, treatment with diuretics, and frequent hospitalizations 42, 43, 44. Patients with congestive heart failure might also have altered thiamine metabolism, including reduced absorption of thiamine in the small intestine 45. A 2015 meta-analysis of nine observational studies found a 2.5 times higher risk of thiamine deficiency in patients with heart failure compared to control subjects 45. As in the general population, older patients with congestive heart failure were found to be at higher risk of thiamine deficiency than younger ones 46.
The authors of one study reported that 33% of 100 patients with chronic heart failure had thiamine deficiency compared to 12% of 50 healthy volunteers 43. Rates of thiamine deficiency were even higher when the investigators excluded those who used thiamine supplements. The different rates of thiamine deficiency in patients with heart failure in these and other studies are probably due to differences in nutrition status, comorbidities, medications and dietary supplements used, and techniques used to measure thiamine status 42.
An important measure of heart function in congestive heart failure is the left ventricular ejection fraction (LVEF), which can be assessed by echocardiogram. One study in 25 patients found that furosemide use at doses of 80 mg/day or greater was associated with a 98% prevalence of thiamine deficiency 47. In a randomized, double-blind study of 30 patients with congestive heart failure, all of whom had been taking furosemide (80 mg/day) for at least three months, intravenous (IV) thiamine therapy (200 mg/day) for seven days resulted in an improved left ventricular ejection fraction (LVEF) compared to IV placebo 48. When all 30 of the congestive heart failure patients in that study subsequently received six weeks of oral vitamin B1 or thiamine therapy (200 mg/day), the average left ventricular ejection fraction (LVEF) improved by 22%. This finding may be relevant because improvements in left ventricular ejection fraction (LVEF) have been associated with improved survival in congestive heart failure patients 49. However, clinical trials of oral vitamin B1 or thiamine supplementation in heart failure patients have not found any benefit. In a randomized, double-blind, placebo-controlled trial in 52 patients with systolic heart failure, 300 mg/day of supplemental thiamin for one month did not improve LVEF compared to placebo 50. A randomized, double-blind, placebo-controlled trial in 64 patients with heart failure reported that 200 mg/day or supplemental thiamin for six months did not improve LVEF 51.
The authors of a systematic literature review and meta-analysis found two randomized, double-blind, placebo-controlled trials of vitamin B1 or thiamine supplementation in people with heart failure that met their eligibility criteria 52. In these trials, vitamin B1 or thiamine supplements significantly improved net change in left ventricular ejection fraction (LVEF). However, the authors did not assess the clinical significance of this finding 17.
Although little evidence supports the routine use of supplemental vitamin B1 or thiamine in congestive heart failure patients and some authors suggest that it may be prudent to screen patients on long-term diuretic therapy for thiamine deficiency and treat accordingly 53.
In summary, more research is needed to determine whether vitamin B1 or thiamine supplements might benefit people with heart failure, even if they have normal thiamine status.
Alzheimer’s disease
Some older adults are at increased risk for developing subclinical thiamine deficiency secondary to poor dietary intake, reduced gastrointestinal absorption, and multiple medical conditions 54, 55. Since thiamine deficiency can result in a form of dementia called Wernicke-Korsakoff syndrome, its relationship to Alzheimer’s disease and other forms of dementia have been investigated. Alzheimer’s disease is characterized by a decline in cognitive function in elderly people, accompanied by pathologic features that include beta-amyloid plaque deposition and neurofibrillary tangles formed by hyperphosphorylated Tau protein 56.
Scientists are studying the possibility that thiamine deficiency could affect the dementia of Alzheimer’s disease. Whether thiamine supplements may help mental function in people with Alzheimer’s disease.
According to animal model studies, thiamine deficiency might play a role in the development of Alzheimer’s disease 57. For example, thiamine deficiency produces oxidative stress in neurons, death of neurons, loss of memory, plaque formation, and changes in glucose metabolism—all markers of Alzheimer’s disease. Autopsy studies have shown that transketolase and other thiamine-dependent enzymes have decreased activity in the brains of people with Alzheimer’s disease 58, 59.
Few studies have assessed the prevalence of thiamine deficiency in people with Alzheimer’s disease. One of these studies found that 13% of 150 patients with cognitive impairment and acute-onset behavioral disturbances were considered thiamine deficient based on plasma levels 60.
The authors of a 2001 Cochrane review assessed three double-blind, randomized trials (including two crossover trials) that compared the effects of 3 g/day oral thiamine to placebo on cognitive function in patients with Alzheimer’s type dementia 61. The three studies randomly assigned fewer than 20 patients each, and the two crossover studies did not include a washout period 62, 63, 64. The review authors stated that it was not possible to draw any conclusions from these three studies because they were small and the publications describing them did not provide enough detail to combine these data in a meta-analysis 61.
Larger, well-designed studies are needed to determine whether vitamin B1 or thiamine supplements are beneficial for Alzheimer’s disease.
Thiamine has not been shown to cause any harm.
Huntington’s disease
Huntington’s disease is an inherited neurodegenerative disorder characterized by selective degeneration of nerve cells known as striatal spiny neurons. Symptoms, such as movement disorders and impaired cognitive function, typically develop in the fourth decade of life and progressively deteriorate over time. A recent study found decreased levels of the thiamin transporter-2 (THTR-2) protein in the striatum and frontal cortex of patients with Huntington’s disease compared to age-and sex-matched healthy controls 65. Compared to control subjects, this study also found lower concentrations of thiamin pyrophosphate (TPP) in the striatum and lower concentrations of thiamin monophosphate (TMP) in the cerebrospinal fluid of patients with Huntington’s disease 65. Mutations in the SLC19A3 gene that encodes THTR-2 causes biotin-thiamin-responsive basal ganglia disease, which is treated with high-dose co-supplementation with biotin and thiamine for life. In a mouse model of Huntington’s disease, high-dose supplementation with both biotin and thiamine vitamins improved neuropathological and motor deficits but had no effect on lifespan 65. A phase 2, open-label clinical trial evaluating the effect of combined thiamine-biotin supplementation, at moderate (600 mg/day of thiamine and 150 mg/day of biotin) and high (1,200 mg/day of thiamine and 300 mg/day of biotin) dosages, in Huntington’s disease is currently underway 66.
Wernicke-Korsakoff syndrome
Wernicke-Korsakoff syndrome is caused by vitamin B1 or thiamine deficiency and is one of the most severe neuropsychiatric consequence of alcohol abuse primarily seen in alcoholics 67. Wernicke-Korsakoff syndrome patients classically present with a clinical triad of altered mental status (i.e., confusion or dementia), nystagmus (or ophthalmoplegia), and ataxia 68. However, less than a third of patients present with this complete triad 69, 70, 71.
The authors of a 2013 Cochrane review of thiamine to treat or prevent Wernicke-Korsakoff syndrome found only two studies that met their inclusion criteria, and one of these studies has not been published 67. These randomized, double-blind, placebo-controlled trials compared 5 mg/day by mouth for 2 weeks or daily intramuscular doses of 5 to 200 mg/day thiamine over 2 consecutive days in a total of 177 people with a history of chronic alcohol use. The Cochrane review authors concluded that the evidence from randomized clinical trials is insufficient to guide health care providers in selecting the appropriate dose, frequency, duration, or route of thiamine supplementation to treat or prevent Wernicke-Korsakoff syndrome in patients with alcohol abuse 67.
The authors of the European Federation of Neurological Societies guidelines for diagnosing, preventing, and treating Wernicke’s encephalopathy note that even high doses of oral vitamin B1 or thiamine supplements might not be effective in raising blood thiamin levels or curing Wernicke’s encephalopathy 72. They recommend 200 mg thiamine, preferably intravenously, three times daily (total of 600 mg/day) until the signs and symptoms stop, along with a balanced diet. In its guidelines for managing Wernicke’s encephalopathy in emergency departments, the Royal College of Physicians in London supports the administration of oral thiamin hydrochloride (100 mg three times a day) in patients with adequate dietary intakes of thiamin and no signs or symptoms of Wernicke’s encephalopathy 73. However, the authors recommend parenteral thiamin supplementation for patients at high risk, such as those with ataxia, confusion, and a history of chronic alcohol misuse, because oral supplementation is unlikely to produce adequate blood levels.
Cancer
Thiamine deficiency and Wernicke-Korsakoff syndrome have been observed in some cancer patients with rapidly growing tumors 74, 75. Research in cell culture and animal models indicates that rapidly dividing cancer cells have a high requirement for thiamine 76. All rapidly dividing cells require nucleic acids at an increased rate, and some cancer cells appear to rely heavily on the TPP-dependent enzyme, transketolase, to provide the ribose-5-phosphate necessary for nucleic acid synthesis. One study found that the levels of THTR-1, transketolase, and TPP mitochondrial transporters were increased in samples of human breast cancer tissue compared to normal tissue, suggesting an adaptation in thiamin homeostasis in support of cancer metabolism 77. Other studies have found that the gene encoding THTR-2 is downregulated in certain cancers 78. Moreover, use of the chemotherapeutic drug, 5-fluorouracil, inhibits phosphorylation of thiamin to thiamin pyrophosphate and may thus lead to thiamin deficiency 79, 80.
Vitamin B1 or thiamine supplementation in cancer patients is common to prevent thiamine deficiency, but Boros et al. 81 caution that too much thiamine may actually fuel the growth of some malignant tumors, suggesting that thiamin supplementation be reserved for those cancer patients who are actually deficient in thiamine. Presently, there is no evidence available from studies in humans to support or refute this theory. However, it would be prudent for individuals with cancer who are considering vitamin B1 or thiamine supplementation to discuss it with their clinician managing their cancer therapy. Intravenous, high-dose thiamine has been suggested as a treatment for cancer patients with confirmed Wernicke-Korsakoff syndrome 75.
Sepsis
Sepsis is a life-threatening medical emergency caused by the body’s extreme response to an infection 82. Sepsis happens when an infection you already have triggers a chain reaction throughout your body. Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract. Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death 82. Because thiamine deficiency is common among septic patients 83, several studies have investigated the treatment effect of intravenous thiamine – alone or in combination with other agents like vitamin C and hydrocortisone.
Observational studies examining the association of intravenous thiamine as a monotherapy have mainly looked at its association with lactic acidosis, which commonly occurs in both thiamine deficiency and sepsis, and with mortality. One retrospective study in 123 septic patients and 246 matched controls found that intravenous thiamin administration within 24 hours of hospital admission was linked to improvements in both lactate clearance and 28-day mortality 84. In a small retrospective study of 53 alcohol-use disorder patients presenting with septic shock, lower mortality was observed in the 34 patients who received intravenous thiamin compared to the 19 patients who did not 85.
A few randomized controlled trials have evaluated the effect of intravenous thiamine in the treatment of sepsis. A randomized, double-blind, placebo-controlled trial in 88 patients with sepsis and elevated blood concentrations of lactate reported that intravenous thiamine (200 mg twice daily for seven days or until discharge from the hospital) did not decrease lactate concentrations at 24 hours post initiation of treatment – the primary endpoint of the trial 86. No differences between the treatment and placebo groups were found for the secondary endpoints, which included survival 86. In a subsequent analysis of data from this trial, the septic patients that were given parenteral thiamin (n=31) had lower creatinine concentrations throughout the treatment and were less likely to need renal replacement therapy compared to placebo (n=39) 87.
A 2020 meta-analysis of four studies – one observational and three randomized controlled trials – found no benefit of intravenous thiamine for improving lactate concentrations, length of hospital stay in intensive care, or overall survival 88. Large-scale clinical trials are needed to determine whether parenteral administration of thiamin is beneficial in the treatment of sepsis. Administering thiamin in combination with vitamin C and corticosteroids may be more efficacious to treat sepsis 89; some clinical trials of such treatments are currently underway 19.
Metabolic diseases
Vitamin B1 or thiamine supplementation is included in the clinical management of genetic diseases that affect the metabolism of carbohydrates and branched-chain amino acids (BCAAs).
Thiamin-responsive pyruvate dehydrogenase deficiency
Pyruvate dehydrogenase deficiency is characterized by the buildup of a chemical called lactic acid (lactic acidosis) in the body and a variety of neurological problems 90. Signs and symptoms of pyruvate dehydrogenase deficiency usually first appear shortly after birth, and they can vary widely among affected individuals. The most common feature is a potentially life-threatening buildup of lactic acid (lactic acidosis), which can cause nausea, vomiting, severe breathing problems, and an abnormal heartbeat. People with pyruvate dehydrogenase deficiency usually have neurological problems as well. Most have delayed development of mental abilities and motor skills such as sitting and walking 90. Other neurological problems can include intellectual disability, seizures, weak muscle tone (hypotonia), poor coordination, and difficulty walking 90. Some affected individuals have abnormal brain structures, such as underdevelopment of the tissue connecting the left and right halves of the brain (corpus callosum), wasting away (atrophy) of the exterior part of the brain known as the cerebral cortex, or patches of damaged tissue (lesions) on some parts of the brain 90. Because of the severe health effects, many individuals with pyruvate dehydrogenase deficiency do not survive past childhood, although some may live into adolescence or adulthood 90.
The genes involved in pyruvate dehydrogenase deficiency each provide instructions for making a protein that is a component of a group of proteins called the pyruvate dehydrogenase complex. This complex plays an important role in the pathways that convert the energy from food into a form that cells can use. The pyruvate dehydrogenase complex converts a molecule called pyruvate, which is formed from the breakdown of carbohydrates, into another molecule called acetyl-CoA. This conversion is essential to begin the series of chemical reactions that produce energy for cells.
The pyruvate dehydrogenase complex is made up of multiple copies of several enzymes called E1, E2, and E3, each of which performs part of the chemical reaction that converts pyruvate to acetyl-CoA. In addition, other proteins included in the complex ensure its proper function. One of these proteins, E3 binding protein, attaches E3 to the complex and provides the correct structure for the complex to perform its function. Other associated proteins control the activity of the complex: pyruvate dehydrogenase phosphatase turns on (activates) the complex, while pyruvate dehydrogenase kinase turns off (inhibits) the complex.
The patients who respond to vitamin B1 or thiamine treatment (from a few mg/day to doses above 1,000 mg/day) exhibit pyruvate dehydrogenase complex (PDHC) deficiency due to the decreased affinity of pyruvate dehydrogenase complex (PDHC) deficiency for TPP 91, 92. Although vitamin B1 or thiamine supplementation can reduce lactate accumulation and improve the clinical features in thiamin-responsive patients, it does not constitute a cure 93.
Maple syrup urine disease
Maple syrup urine disease is an inherited disorder in which the body is unable to process branched-chain amino acid (BCAA) properly 94. Maple syrup urine disease gets its name from the distinctive sweet odor of affected infants’ urine. Alterations in the branched-chain amino acid (BCAA) catabolic pathway result in neurologic dysfunction caused by the accumulation of branched-chain amino acids (leucine, isoleucine, and valine) and their derivatives, branched-chain ketoacids (BCKA). Maple syrup urine disease is also characterized by poor feeding, vomiting, lack of energy (lethargy), abnormal movements, and delayed development. If untreated, maple syrup urine disease can lead to seizures, coma, and death 94.
Maple syrup urine disease is often classified by its pattern of signs and symptoms. The most common and severe form of the disease is the classic type, which becomes apparent soon after birth. Variant forms of the disorder become apparent later in infancy or childhood and are typically milder, but they still lead to delayed development and other health problems if not treated.
Mutations in the BCKDHA, BCKDHB, and DBT genes can cause maple syrup urine disease 94. The BCKDHA, BCKDHB, and DBT genes provide instructions for making proteins that work together as part of a complex. The protein complex is essential for breaking down the amino acids leucine, isoleucine, and valine, which are present in many kinds of food, particularly protein-rich foods such as milk, meat, and eggs.
Mutations in any of these three genes reduce or eliminate the function of the protein complex, preventing the normal breakdown of leucine, isoleucine, and valine. As a result, these amino acids and their byproducts build up in the body. Because high levels of these substances are toxic to the brain and other organs, their accumulation leads to the serious health problems associated with maple syrup urine disease.
Researchers are studying other genes related to the same protein complex that may also be associated with maple syrup urine disease.
The therapeutic approach includes a synthetic diet with reduced branched-chain amino acid (leucine, isoleucine, and valine) content, and thiamine (10-1,000 mg/day) is supplemented to patients with mutations in the E2 subunit of the BCKDH complex 95. In thiamine-responsive individuals, the supplementation has been proven effective to correct the phenotype without recourse to the branched-chain amino acid (BCAA) restriction diet.
Thiamine-responsive megaloblastic anemia
Mutations in the SLC19A2 gene that encodes THTR-1 impairs intestinal thiamine uptake and causes thiamine deficiency, leading to thiamine-responsive megaloblastic anemia 96. Thiamine-responsive megaloblastic anemia syndrome also called thiamin metabolism dysfunction syndrome-1, is characterized by megaloblastic anemia, diabetes mellitus, and deafness. A review of 30 cases reported additional neurologic, visual, and cardiac impairments 97. High-dose oral supplementation with thiamine (up to 300 mg/day) helps to maintain health and correct hyperglycemia in prepubescent children. A recent study in 32 individuals with found no additional benefit of oral doses above 150 mg/day 98. After puberty, a decline in pancreatic function results in the requirement of insulin together with thiamine to control the hyperglycemia. One study also reported that the treatment of a four-month-old girl with 100 mg/day of thiamin did not prevent hearing loss at 20 months of age 99. Early diagnosis of the thiamine-responsive megaloblastic anemia syndrome and early treatment with thiamin is important for a better prognosis 98.
Biotin-thiamin-responsive basal ganglia disease
Biotin-thiamin-responsive basal ganglia disease, also called biotin-responsive basal ganglia disease, thiamin transporter-2 deficiency, and thiamin metabolism dysfunction syndrome-2, is caused by an autosomal recessive mutation in the SLC19A3 gene that codes for THTR-2. The disease usually presents around 3 to 10 years of age 100, but an early infantile form of the disease exists with onset as early as one month of age 101. Clinical features include subacute encephalopathy (confusion, drowsiness, altered level of consciousness), ataxia, and seizures.
A retrospective study of 18 affected individuals from the same family or the same tribe in Saudi Arabia showed that biotin monotherapy (5-10 mg/kg/day) efficiently abolished the clinical manifestations of the disease, although one-third of the patients suffered from recurrent acute crises 102. Often associated with poor outcomes, acute crises were not observed for a five-year follow-up period following thiamin supplementation (300-400 mg/day) – early diagnosis and immediate treatment with biotin and thiamin led to positive outcomes 102. Recent studies have found supplemental thiamin to be important in treating the condition. In an open-label study of 20 pediatric patients with the disease, supplemental thiamin alone was as effective as combined biotin-thiamin supplementation when given for 30 months 103. Lifelong high-dose supplementation with a combination of biotin and thiamin is generally the treatment for biotin-thiamin-responsive basal ganglia disease 100. Early diagnosis and treatment is important to ensure a better prognosis 101, 104.
Other thiamine metabolism dysfunction syndromes
Supplemental thiamine has limited utility in treating other inborn errors of thiamin metabolism. Mutations in the SLC25A19 gene that codes for the mitochondrial TPP transporter can result in either thiamine metabolism dysfunction syndrome-3 (THMD3) or thiamine metabolism dysfunction syndrome-4 (THMD4). Of these rare syndromes, thiamine metabolism dysfunction syndrome-3 (THMD3), also called Amish-type microcephaly or Amish lethal microcephaly, has the more severe phenotype, resulting in a congenital microcephaly, elevated concentrations of α-ketoglutarate in urine, and usually death in infancy 105. Thiamine metabolism dysfunction syndrome-4 (THMD4) is characterized by episodic encephalopathy and weakness, which often presents following a viral infection or febrile illness in childhood. Some patients affected with THMD4 may respond to high-dose thiamin supplementation 106.
Mutations in the TPK1 gene result in thiamin pyrophosphokinase 1 deficiency and thiamine metabolism dysfunction syndrome-5 (THMD5), which usually manifests in early childhood. While the clinical presentation of THMD5 varies, affected individuals often experience episodic ataxia, dystonia, and lactic acidosis 107. Only a few cases of thiamine metabolism dysfunction syndrome-5 (THMD5) have been reported to date; two of these patients experienced limited improvement of symptoms upon supplementation with thiamin, in conjunction with adherence to a high-fat diet 108.
How much vitamin B1 do I need?
The amount of vitamin B1 or thiamine you need depends on your age and sex 109. Average daily recommended amounts are listed in Table 1 below in milligrams (mg). The Recommended Dietary Allowance (RDA) is average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals 110. Table 1 lists the current Recommended Dietary Allowance (RDA) for vitamin B1 or thiamine 110. For infants from birth to 12 months, the Food and Nutrition Board at the Institute of Medicine of the National Academies established an adequate intake (intake at this level is assumed to ensure nutritional adequacy; adequate intake is established when evidence is insufficient to develop an RDA). for vitamin B1 or thiamine that is equivalent to the mean intake of vitamin B1 or thiamine in healthy, breastfed infants 17.
Most people in the United States consume the recommended amounts of vitamin B1 or thiamine 17. An analysis of data from the 2003-2006 National Health and Nutrition Examination Survey showed that only 6% of the U.S. population has a usual intake below the estimated average requirement (average daily level of intake estimated to meet the requirements of 50% of healthy individuals. It is usually used to assess the adequacy of nutrient intakes in populations but not individuals) 3.
Among children and teens, the average daily vitamin B1 or thiamine intake from foods is 1.27 mg for ages 2–5 years, 1.54 mg for ages 6–11 years, and 1.68 mg for ages 12–19 years 111. In adults aged 20 and older, the average daily vitamin B1 or thiamine intake from foods is 1.95 mg in men and 1.39 mg in women. The average daily vitamin B1 or thiamine intake from foods and supplements in children and teens is 1.51 mg for ages 2–5 years, 1.76 mg for ages 6–11 years, and 1.95 mg for ages 12–19 years. In adults aged 20 and older, the average daily vitamin B1 or thiamine intake from foods and supplements is 4.89 mg in men and 4.90 mg in women 17.
No current data on rates of thiamine deficiency in the U.S. population are available 17.
Most people in the United States get enough vitamin B1 or thiamine from the foods they eat. Thiamine deficiency is rare in this country. However, certain groups of people are more likely than others to have trouble getting enough vitamin B1 or thiamine:
- People with alcohol dependence
- Older individuals
- People with HIV/AIDS
- People with diabetes
- People who have had weight loss surgery
Table 1. Recommended Dietary Allowances (RDAs) for vitamin B1 or thiamine
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 0.2 mg |
| Infants 7–12 months | 0.3 mg |
| Children 1–3 years | 0.5 mg |
| Children 4–8 years | 0.6 mg |
| Children 9–13 years | 0.9 mg |
| Teen boys 14–18 years | 1.2 mg |
| Teen girls 14–18 years | 1.0 mg |
| Men | 1.2 mg |
| Women | 1.1 mg |
| Pregnant teens and women | 1.4 mg |
| Breastfeeding teens and women | 1.4 mg |
What happens if I don’t get enough vitamin B1?
You can develop thiamine deficiency if you don’t get enough vitamin B1 or thiamine in the foods you eat or if your body eliminates too much or absorbs too little vitamin B1 or thiamine.
Thiamine deficiency can cause loss of weight and appetite, confusion, memory loss, muscle weakness, and heart problems. Severe thiamine deficiency leads to a disease called beriberi with the added symptoms of tingling and numbness in the feet and hands, loss of muscle, and poor reflexes. Beriberi is not common in the United States and other developed countries.
A more common example of thiamine deficiency in the United States is Wernicke-Korsakoff syndrome, which mostly affects people with alcoholism. It causes tingling and numbness in the hands and feet, severe memory loss, disorientation, and confusion.
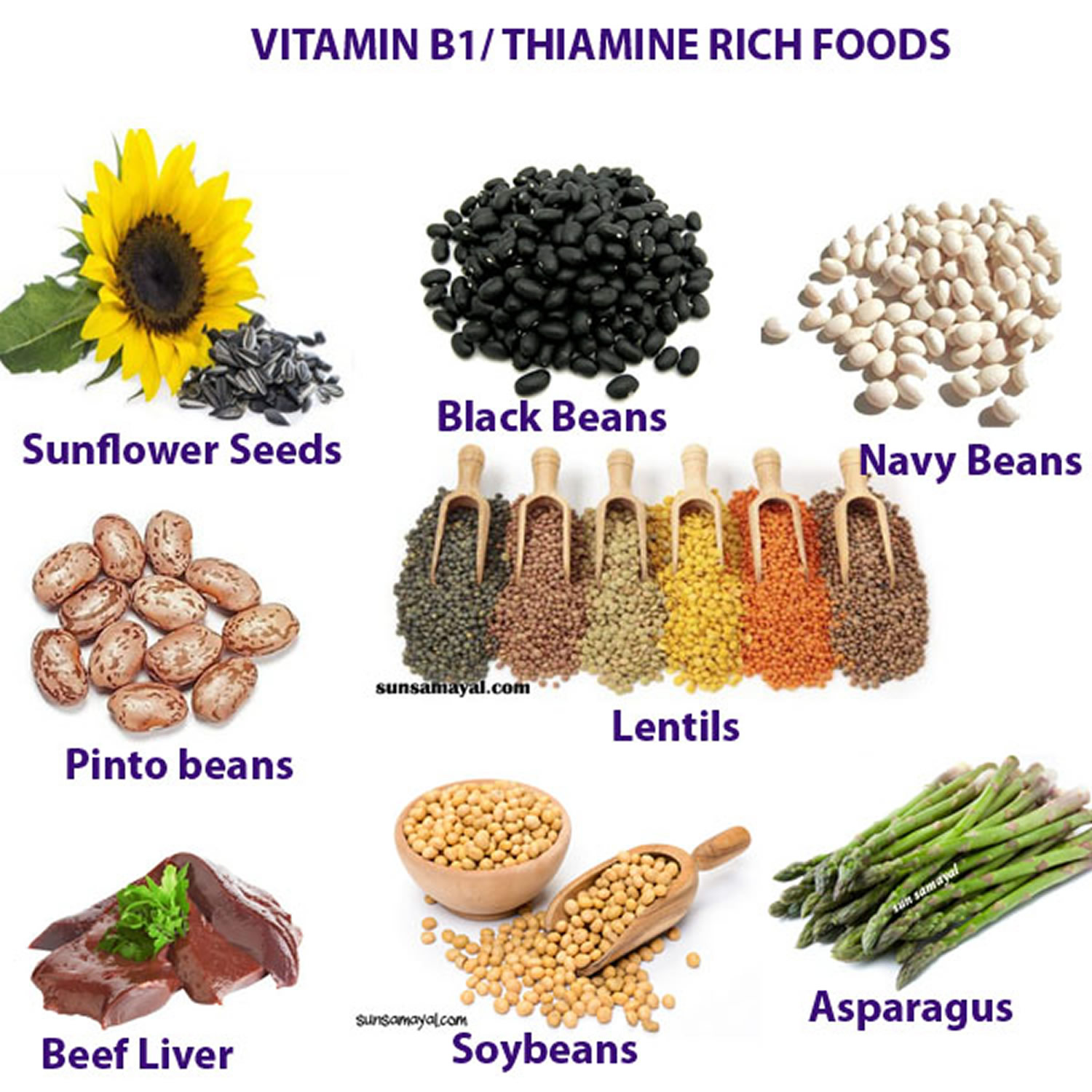
What foods provide vitamin B1?
Vitamin B1 or thiamine is found naturally in many foods and is added to some fortified foods. You can get recommended amounts of vitamin B1 or thiamine by eating a variety of foods, including the following 7:
- Whole grains and fortified bread, cereal, pasta, and rice
- Meat (especially pork) and fish
- Legumes (such as black beans and soybeans), seeds, and nuts
Breads, cereals, and infant formulas in the United States and many other countries are fortified with thiamine 7. The most common sources of vitamin B1 or thiamine in the U.S. diet are cereals and bread 2. Pork is another major source of the vitamin. Dairy products and most fruits contain little vitamin B1 or thiamine 9. About half of the vitamin B1 or thiamine in the U.S. diet comes from foods that naturally contain thiamin; the remainder comes from foods to which thiamine has been added 3.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central website (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides a comprehensive list of foods containing vitamin B1 or thiamine arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/Thiamin-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/Thiamin-Food.pdf).
Heating foods containing vitamin B1 or thiamine can reduce their thiamin content. For example, bread has 20%–30% less vitamin B1 or thiamine than its raw ingredients, and milk pasteurization reduces thiamin content (which is very small to begin with) in milk by up to 20% 9. Because vitamin B1 or thiamine dissolves in water, a significant amount of the vitamin is lost when cooking water is thrown out 9. Processing also alters vitamin B1 or thiamine levels in foods; for example, unless white rice is enriched with thiamin, it has one tenth the amount of thiamin in unenriched brown rice 112.
Data on the bioavailability of vitamin B1 or thiamine from food are very limited 113. Some studies do show, however, that thiamin absorption increases when intakes are low 1.
Several food sources of thiamine are listed in Table 2.
Table 2. Vitamin B1 (thiamine) food sources
| Food | Milligrams (mg) per serving | Percent Daily Value (DV*) |
|---|---|---|
| Breakfast cereals, fortified with 100% of the Daily Value (DV) for thiamine, 1 serving | 1.2 | 100 |
| Egg noodles, enriched, cooked, 1 cup | 0.5 | 42 |
| Pork chop, bone-in, broiled, 3 ounces | 0.4 | 33 |
| Trout, cooked, dry heat, 3 ounces | 0.4 | 33 |
| Black beans, boiled, ½ cup | 0.4 | 33 |
| English muffin, plain, enriched, 1 muffin | 0.3 | 25 |
| Mussels, blue, cooked, moist heat, 3 ounces | 0.3 | 25 |
| Tuna, Bluefin, cooked, dry heat, 3 ounces | 0.2 | 17 |
| Macaroni, whole wheat, cooked, 1 cup | 0.2 | 17 |
| Acorn squash, cubed, baked, ½ cup | 0.2 | 17 |
| Rice, brown, long grain, not enriched, cooked, ½ cup | 0.2 | 17 |
| Rice, white, long grain, enriched, cooked, ½ cup | 0.1 | 8 |
| Bread, whole wheat, 1 slice | 0.1 | 8 |
| Orange juice, prepared from concentrate, 1 cup | 0.1 | 8 |
| Sunflower seeds, toasted, 1 ounce | 0.1 | 8 |
| Beef steak, bottom round, trimmed of fat, braised, 3 ounces | 0.1 | 8 |
| Yogurt, plain, low fat, 1 cup | 0.1 | 8 |
| Oatmeal, regular and quick, unenriched, cooked with water, ½ cup | 0.1 | 8 |
| Corn, yellow, boiled, 1 medium ear | 0.1 | 8 |
| Milk, 2%, 1 cup | 0.1 | 8 |
| Barley, pearled, cooked, 1 cup | 0.1 | 8 |
| Cheddar cheese, 1½ ounces | 0 | 0 |
| Chicken, meat and skin, roasted, 3 ounces | 0 | 0 |
| Apple, sliced, 1 cup | 0 | 0 |
Footnote: *DV = Daily Value. Daily Values were developed by the U.S. Food and Drug Administration (FDA) to help consumers compare the nutrient contents of products within the context of a total diet. The DV for thiamine is 1.5 mg for adults and children age 4 and older. Foods providing 20% or more of the Daily Value are considered to be high sources of a nutrient.
[Source 114 ]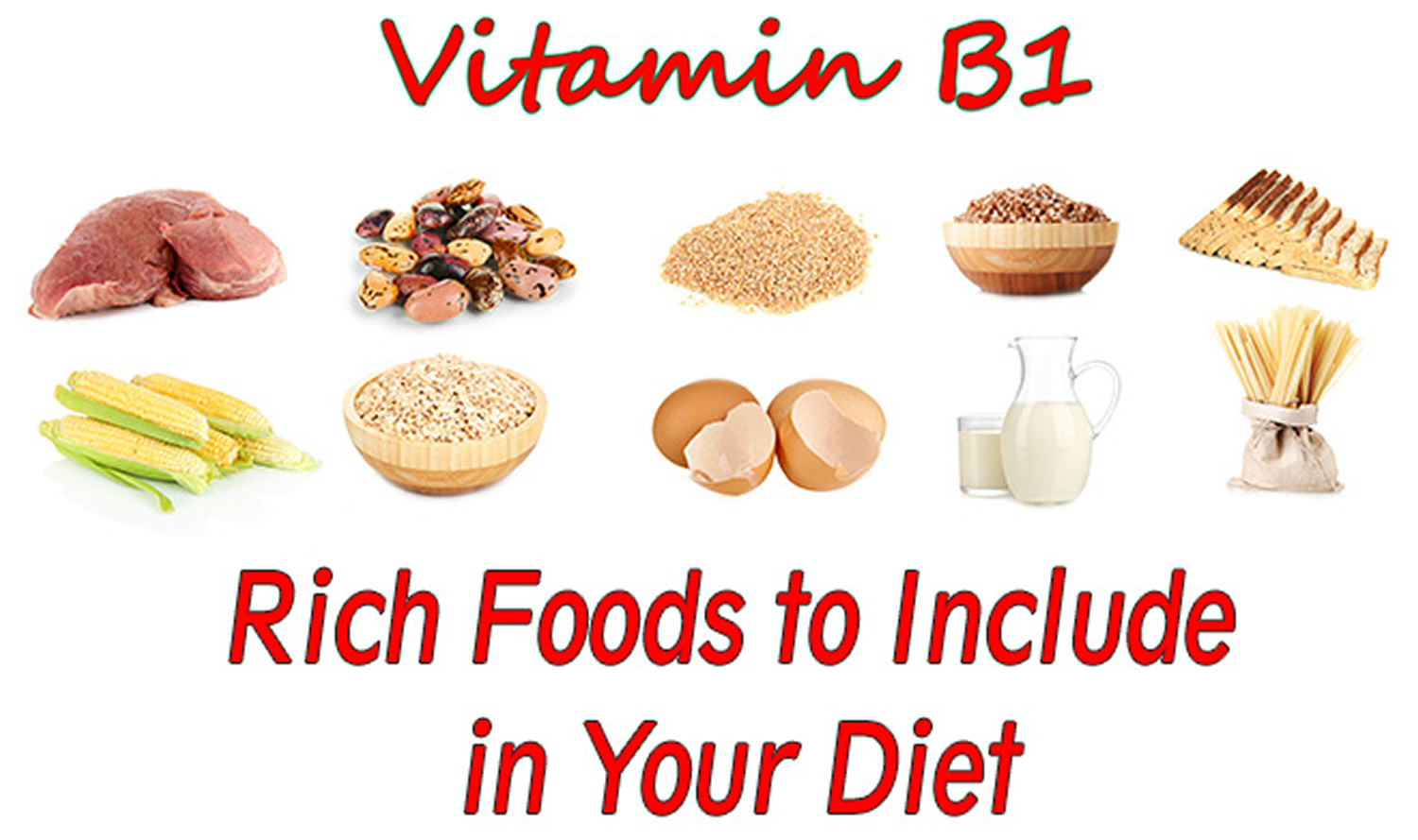
Vitamin B1 (Thiamine) Supplements
Vitamin B1 or thiamine is also available in many dietary supplements. Multivitamin or multimineral supplements with vitamin B1 or thiamine typically provide about 1.5 mg thiamine (100% of the Daily Value) and sometimes more 115. Supplements containing B-complex vitamins (including thiamin) or thiamine only are also available. The most commonly used forms of vitamin B1 or thiamine in supplements are thiamine mononitrate and thiamin hydrochloride, which are stable and water soluble 1, 115.
Benfotiamine is a synthetic thiamine derivative that is used in some dietary supplements. Benfotiamine is not water soluble and is converted to thiamine in the body 116.
Thiamine (Vitamin B1) Deficiency
Thiamine deficiency, also called vitamin B1 deficiency, is a rare disorder that occurs if the recommended daily intake of vitamin B1 or thiamine is not maintained 117, 118. Populations and cultures that rely heavily upon rice based diets are at increased risk of thiamine deficiency 119. Thiamine deficiency may also occur due to impaired intestinal absorption or high excretion rates, such as in people with alcohol dependency, acquired immunodeficiency syndrome (AIDS), and malnutrition 120, 121. Individuals with certain medical and non-medical conditions are more susceptible to vitamin B1 deficiency, e.g., alcohol dependency, older age, diabetes, post-weight loss surgery, cancers that have spread throughout the body, cancer chemotherapy with poor dietary intake, gastrointestinal disease, pregnancy with hyperemesis gravidarum (severe nausea and vomiting during pregnancy), lactation, fasting, starvation, use of unbalanced diets, malnourished patients with intestinal obstruction or malabsorption syndromes, hyperthyroidism (overactive thyroid), kidney failure on hemodialysis, and systemic infections 122, 123, 119.
Thiamine is important for the growth, development, and function of the cells in your body. In the human body, thiamine or vitamin B1 exists mainly in the form of thiamin pyrophosphate (TPP). This is the main active form of thiamine and serves as a cofactor for many enzymes during the metabolism of glucose, branched-chain amino acids (protein), and fatty acids (lipids) (see Figure 1 above) 16. Thiamine or vitamin B1 deficiency can lead to severe (or even fatal) cardiovascular, muscular, gastrointestinal, and central and peripheral nervous systems complications, including heart failure, neuropathy leading to ataxia and paralysis, confusion, or delirium 124, 21.
- Thiamin deficiency causes degeneration of peripheral nerves, thalamus, mammillary bodies, and cerebellum. Cerebral blood flow is markedly reduced, and vascular resistance is increased.
- The heart may become dilated; muscle fibers become swollen, fragmented, and vacuolized, with interstitial spaces dilated by fluid. Vasodilation occurs and can result in edema in the feet and legs. Arteriovenous shunting of blood increases. Eventually, high-output heart failure may occur.
Most people have no symptoms and signs of thiamine deficiency or vitamin B1 deficiency; therefore, it must be suspected in the appropriate clinical setting 125. Thiamine deficiency or vitamin B1 deficiency early symptoms and signs are often nonspecific and vague, such as fatigue. However, early symptoms mainly arise from neurological, heart and gastrointestinal systems, where patients may experience weight loss, anorexia, confusion, short-term amnesia, malaise, muscle weakness, and heart symptoms due to heart failure 126.
Generally, heart effects are referred to as “wet beriberi”, the peripheral neurological signs and symptoms are called “dry beriberi”, and delirium, mental confusion and abnormal eye movements (due to ophthalmoplegia, which is paralysis or weakness of the eye muscles), stance and gait ataxia are termed “cerebral beriberi” or Wernicke’s encephalopathy 127, 23, 19. “Gastrointestinal beriberi” is caused by lactic acidosis, a condition resulting from the accumulation of lactate and is often associated with nausea, vomiting, and severe abdominal pain 128.
Beriberi is the classic diet related thiamine deficiency which can present as wet or dry types. “Wet beriberi” presents as a right sided high-output heart failure with signs of peripheral swelling (edema), an enlarged heart, warm extremities, rapid heart rate (tachycardia), and respiratory distress 126. “Dry beriberi” is predominantly a neurological complication involving the peripheral nervous system and presents with painful peripheral neuropathy, malaise, muscle weakness, seizures, or brisk tendon reflexes 123. Infants and children are susceptible to vitamin B1 deficiency too, presenting as infantile or childhood beriberi. Usually, infants present with swelling (edema), ill-looking appearance, pallor, anorexia, coffee ground vomiting, and diarrhea 126. Neurological signs include a hoarse cry due to vocal cord paralysis, head lag, seizures, coma, and sudden infant death syndrome. “Juvenile beriberi” is uncommon and often misdiagnosed due to overlapping symptoms of meningitis 16.
If thiamine deficiency or vitamin B1 deficiency is prolonged or left untreated, an individual is at risk of advanced-stage symptoms due to irreversible neurological damage called Wernicke-Korsakoff syndrome 129, 130. Wernicke-Korsakoff syndrome is more common in the United States and 8 to 10 times more common among people with chronic alcohol consumption/misuse, severe gastrointestinal disorders, cancers, drug use, and AIDS 126. Wernicke-Korsakoff syndrome presents in two phases. Wernicke’s encephalopathy occurs early and presents with polyneuropathy, ataxia, abnormal eye movements due to ophthalmoplegia (paralysis or weakness of the eye muscles), and gait abnormalities. Korsakoff’s syndrome also called Korsakoff psychosis, Korsakoff’s dementia, Korsakoff’s amnesia, or amnestic confabulatory syndrome, is a residual syndrome in patients who suffered from a Wernicke encephalopathy, but did not receive immediate and adequate treatment with thiamine or vitamin B1 replacement therapy 130, 131, 132, 133. The most conspicuous symptom of Korsakoff’s syndrome is global short-term amnesia, which can be very profound. In combination with other cognitive and behavioral deficits such as disorientation, confabulation, and hallucinations, which may have far-reaching effects on daily life 134, 135, 136. Wernicke encephalopathy is acute and often reversible while Korsakoff syndrome is chronic and may be irreversible 137. The most common cause of Korsakoff syndrome is chronic alcohol abuse 138. Alcohol interferes with gastrointestinal tract absorption of thiamine as well as interfering with the liver’s ability to store thiamine. Additionally, accompanying malnutrition often compounds the effects of alcoholism leading to further thiamine deficiency. Other causes of Korsakoff syndrome include eating disorders, chronic vomiting (including hyperemesis gravidarum), psychiatric disorders, chemotherapy, and cancer 139, 140. As Korsakoff syndrome is advanced-stage symptoms of thiamine deficiency, parenteral thiamine treatment does not lead to recovery in about one-quarter of patients 136.
To treat mild thiamine deficiency, the World Health Organization (WHO) recommends daily oral doses of 10 mg thiamine for a week, followed by 3–5 mg/daily for at least 6 weeks 141. For patients at risk of thiamine deficiency or with confirmed thiamine deficiency, parenteral (intravenously or intramuscularly) thiamine of 100 mg and 200 mg 3 times a day has been used, respectively, in clinical practice 72. The recommended treatment for severe thiamine deficiency consists of 25–30 mg intravenously in infants and 50–100 mg in adults, then 10 mg daily administered intramuscularly for approximately one week, followed by 3–5 mg/day oral thiamine for at least 6 weeks 17.
Thiamine (Vitamin B1) Deficiency causes
Thiamine deficiency or vitamin B1 deficiency may result from inadequate dietary thiamine intake, administration of total parenteral nutrition without adequate thiamine replacement, increased physiological requirements for thiamine, excessive loss of thiamine from the body, impaired intestinal absorption, small intestinal bacterial overgrowth (SIBO), consumption of anti-thiamine factors (ATF) in food, antacids, sulfites, or sodium bicarbonate food preservatives or a combination of these factors 142, 143, 144, 19.
The maximum body store of thiamine is 30 mg, which is rapidly depleted within 2 weeks of beginning a thiamine-deficient diet 8. Risk factors for decreased thiamine intake include protracted vomiting, weight loss surgery or gastrointestinal surgery, malnutrition, extreme nausea and vomiting during pregnancy (hyperemesis gravidarum), anorexia, and alcoholism 42.
Other conditions that may cause thiamine deficiency or vitamin B1 deficiency include:
- HIV/AIDS
- Cancers that have spread throughout the body
- Extreme nausea and vomiting during pregnancy (hyperemesis gravidarum)
- Heart failure (when treated with long-term diuretic therapy)
- Long periods of intravenous (IV) nutrition without receiving thiamine supplements
- Long-term dialysis
- Taking high doses of diuretics (water pills)
- Very high thyroid hormone levels (thyrotoxicosis)
- Breastfed infants whose mother is lacking in thiamine
- Infants fed unusual formulas that don’t have enough thiamine.
In rare cases, thiamine deficiency or vitamin B1 deficiency can be a genetic metabolic disease 145, 146. This condition is passed down through families. People with this condition lose the ability to absorb thiamine from foods. This can happen slowly over time. The symptoms occur when the person is an adult. However, this diagnosis is often missed. This is because health care providers may not consider thiamine deficiency in nonalcoholics 146.
Inadequate dietary thiamine or vitamin B1 intake
Inadequate consumption of thiamine or vitamin B1 is the main cause of thiamine deficiency in developing countries 20. Thiamine deficiency is common in low-income populations whose diets are high in carbohydrate and low in thiamine. Examples of foods that can lead to inadequate thiamine intake upon prolonged consumption include sago, cassava flour, unfortified white bread, or highly refined cereals such as polished white rice 8. The consumption of a diet composed mainly of refined carbohydrates or one that includes high alcohol intake also reduces body thiamine stores 8.
To attain maximal erythrocyte transketolase activity, at least 0.6 mg of thiamine per 1000 kcal of carbohydrate is required 8. Most humans will develop symptoms of thiamine deficiency when intake is below 0.2 mg of thiamine per 1000 kcal. Whole wheat flour contains 0.55 mg of thiamine per 100 g, brown rice 0.33 mg per 100 g, and highly milled white rice only 0.08 mg per 100 g 8. Adding baking powder (sodium bicarbonate) to wholemeal flour when baking bread reduces the thiamine content 8. Washing white rice in water prior to cooking reduces the thiamine content by half. Thiamine is heat labile, chlorine sensitive, and water soluble, so discarding the rice water after cooking or using chlorinated water for cooking or washing rice contributes to thiamine loss from the diet 142. Parboiling (partly cook food by boiling) of rice was originally developed in India but is not practiced in Southeast Asia or Japan, where milled white rice is preferred. Rice parboiling distributes the thiamine content from the bran and aluerone layer to the endosperm prior to milling. This is why beriberi is rare in India, where parboiled rice is the primary form of rice consumed 142.
After 1878, mechanical roller milling of wheat and polishing of rice became widespread 147. Consumption of mass-produced, polished white rice as the staple diet in East Asian countries led to epidemics of thiamine deficiency (beriberi) in the 1800s and 1900s 148, 147. Polished rice and milled wheat were also popular because removal of the oil-rich bran layer from rice or the wheat bran from wheat grains prolonged storage times, minimized rancidity, and reduced the susceptibility to weevils. Mandatory fortification of wheat flour with the thiamine mononitrate vitamer was introduced in Australia in 1991. Since then, Wernicke-Korsakoff syndrome has become very uncommon in Australia. The thiamine mononitrate vitamer is used because it is non-hygroscopic and more stable than thiamine hydrochloride 149. Mandatory fortification of bread with iodine and folate was commenced in Australia in 2009. Folate deficiency may indirectly contribute to thiamine deficiency, as folate is required for the regeneration of reduced nicotinamide adenine dinucleotide (NADH) by dihydrofolate reductase. NADH is necessary for the regeneration of TPP 150. Vitamin C may protect against the development of symptoms of thiamine deficiency 142.
Breast-fed infants whose mothers are thiamine deficient are vulnerable to developing infantile beriberi. Alcoholism, which is associated with low intake of thiamine among other nutrients, is the primary cause of thiamine deficiency in industrialized countries. Some of the non-alcoholic conditions associated with Wernicke-Korsakoff syndrome include anorexia nervosa, bariatric surgery (weight-loss surgery), gastrointestinal malignancies, and malabsorption syndromes 151, 152, 153, 154. Obese individuals may also be at heightened risk of thiamine deficiency 155, 156. Moreover, cases of Wernicke’s encephalopathy have been linked with hyperemesis gravidarum (severe nausea and vomiting during pregnancy) 157, 158, and with parenteral nutrition lacking vitamin supplementation 159, 160.
Increased thiamine or vitamin B1 requirement
Conditions resulting in an increased requirement for thiamine or vitamin B1 include strenuous physical exertion, fever, severe infection or sepsis, hyperthyroidism, pregnancy, breast-feeding, adolescent growth, major surgery, refeeding syndrome, or rapid growth of cancers 6, 161, 162, 74, 163, 164, 165, 166, 167. Such conditions place individuals with marginal thiamine intake at risk for developing symptomatic thiamine deficiency.
Fever can critically increase the requirement for thiamine, as a rise in core body temperature of 1°C will increase the basal metabolic rate by 10% 168. Consumption of a high-fat or a high-carbohydrate diet results in increased metabolic consumption of thiamine 150. This is particularly relevant in individuals with preexisting thiamine deficiency, such as refugees, prisoners of war, persons with alcoholism, oncology patients, and postoperative bariatric surgery or gastrectomy patients. Administering oral, enteral, or parenteral nutrition to these patients without concomitant thiamine supplementation can result in fulminant beriberi or acute refeeding syndrome 142, 169, 170, 171, 172.
Malaria patients in Southeast Asia were found to be thiamine deficient more frequently than non-infected individuals 173, 174. Malarial infection leads to a large increase in the metabolic demand for glucose. Because thiamine is required for enzymes involved in glucose metabolism, the stresses induced by malarial infection could exacerbate thiamin deficiency in predisposed individuals. HIV-infected individuals, whether or not they had developed AIDS, were also found to be at increased risk for thiamine deficiency 175. Furthermore, chronic alcohol abuse impairs intestinal absorption and utilization of thiamine 23; therefore, alcoholics have increased requirements for thiamine or vitamin B1. Thiamine deficiency is also observed as a complication of the refeeding syndrome: the introduction of carbohydrates in severely starved individuals leads to an increased demand for thiamine in glycolysis and the citric acid cycle that precipitates thiamine deficiency 176.
Anti-thiamin factors
The presence of anti-thiamin factors (ATF) in foods contributes to the risk of thiamin deficiency. Certain plants contain anti-thiamin factors (ATF), which react with thiamine to form an oxidized, inactive product. Consuming very large amounts of tea or coffee (including decaffeinated), as well as chewing tea leaves and betel nuts, might lower thiamin status due to the presence of anti-thiamin factors (ATF) 177, 178. Anti-thiamin factors (ATF) include mycotoxins (molds), thiaminases that break down thiamin in food, thiamine antagonists, and hemin 8. Individuals who habitually eat certain raw fresh-water fish, raw shellfish, or ferns are at higher risk of thiamine deficiency because these foods contain thiaminase that normally is inactivated by heat in cooking 23, 24, 179, 180, 181. In Nigeria, an acute, neurologic syndrome (seasonal ataxia) has been associated with thiamine deficiency precipitated by a thiaminase in African silkworms (Anaphe species), a traditional, high-protein food for some Nigerians 182.
Thiamine antagonists are found in tea and betel nuts (tannic acid), coffee (chlorogenic acid, caffeic acid), bracken fern (caffeic acid), and pigmented polyphenol-containing foods such as red cabbage, blueberries, red currants, and red beets 8. These cause oxidation of the thiazole ring of thiamine, forming nonabsorbable thiamine disulfide 142. For example, consumption of 1 g of dry tea leaves boiled in 100 mL of water for 5 minutes caused thiamine loss of 0.21 mg per hour 183. Vitamin C and cysteine can protect thiamine from degradation caused by organic acids and polyphenols 184. Outbreaks of beriberi in the wet season in some countries may be related to low availability of food, importation of poor-quality rice or milled white rice, seasonal variations in plant tannin levels, or the mycotoxin citreoviridin, produced by rice mold 185, 162, 186.
Food additives and thiamine
Thiamine is unstable under alkaline conditions produced by food additives such as preservatives and antacids (eg, sodium bicarbonate), which cause disruption of the thiamine methylene bridge 8. Sulfite-type food preservatives include sulfur dioxide, sodium sulfite, sodium and potassium bisulfite, and sodium and potassium metabisulfite 8. These are used extensively in the production and preservation of foods and beverages, including dried fruit, ready-to-eat salad vegetables, frozen fried potatoes, wine, beer, soft drinks, packaged fruit juices, shellfish, and pickled and pureed foods. Sulfites possess antioxidant and antimicrobial activities, which inhibit the enzymatic and nonenzymatic (browning) spoiling of food. This preserves the color, freshness, flavor, and crispness of food but substantially reduces the available thiamine. For example, respective thiamine loss from cabbage blanched with sulfite-treated water versus untreated water was 45% vs 15% 142. The use of sulfiting agents in foods recognized as important sources of thiamine is prohibited by the US Food and Drug Administration 187, 188, 189, 190.
Excessive loss of thiamine caused by thiamine-drug interactions
Excessive loss of thiamine may precipitate thiamine deficiency. Increased losses of ingested thiamine can be caused by drug-related polyuria or diarrhea, drug interactions, or chronic excessive alcohol consumption 8. Thiamine is a polar, water-soluble vitamin and is not protein bound, which allows it to be easily dialyzed or filtered in the glomerulus. Increased urine flow, loop diuretics, or dialysis can all cause thiamine deficiency. Thiamine deficiency is associated with drugs such as omeprazole, phenytoin, 5-fluorouracil, metformin, alcohol, antibiotics, furosemide, and thiazide diuretics 42. By increasing urinary flow, diuretics may prevent reabsorption of thiamine by the kidneys and increase its excretion in the urine 191, 192. The risk of thiamine deficiency is increased in diuretic-treated patients with marginal thiamine intake 193 and in individuals receiving long-term, diuretic therapy 47. Patients with congestive heart failure who receive chronic therapy with furosemide or thiazide diuretics can also develop thiamine deficiency. The prevalence of thiamine deficiency in this patient population varies from 21% to 98% 8. Supplementation with thiamine has been shown to improve left ventricular ejection fraction by 22%, New York Heart Association Functional Classification, and TPP effect (from 11.7% to 5.4%) in these patients 48. Mechanisms for exacerbation of heart failure by diuretics include increased thiamine loss in urine, furosemide-related inhibition of cardiac myocyte thiamine uptake, furosemide-induced anorexia, furosemide inhibition of intestinal absorption or cellular uptake of thiamine, and hypomagnesemia 42. Unrecognized thiamine deficiency in heart failure patients treated with long-term diuretic therapy may result in Shoshin beriberi 194.
Individuals with kidney failure requiring hemodialysis lose thiamine at an increased rate and are at risk for thiamine deficiency 195. Alcoholics who maintain a high fluid intake and high urine flow rate may also experience increased loss of thiamine, exacerbating the effects of low thiamine intake 196.
Omeprazole a proton pump inhibitor because of its azole analogue molecular structure may cause inactivation of pyruvate decarboxylase and human erythrocyte transketolase, resulting in antagonism of thiamine 197. Omeprazole may inhibit gastric proton pumps by competing with thiamine for binding to hydrogen/potassium adenosine triphosphatase 145, 197. Proton pump inhibitor drugs or Roux-en-Y gastric bypass surgery may also worsen subclinical thiamine deficiency by promoting small intestinal bacterial overgrowth, which alters luminal thiamine levels 198, 144. Hypomagnesemia induced by proton pump inhibitors can contribute to functional thiamine deficiency, as magnesium is a required cofactor for the formation of TPP and acetyl coenzyme A 198. 5-Fluorouracil decreases hepatic thiamine levels and thiamine-dependent transketolase activity. This is associated with an increase in the TPP effect in vitro and in whole blood 199. 5-Fluorouracil is catabolized to fluoroacetate, which blocks the Krebs cycle and ATP production, leading to neurotoxicity, ammonia formation, and encephalopathy 200, 201, 202. Metformin, a substrate and inhibitor of the human thiamine transporter 2, reduces both intestinal absorption of thiamine and levels of thiamine in tissues and liver 203, 204, 205. Alcohol decreases carrier-mediated thiamine transport in the brush border and basolateral membrane of enterocytes in the jejunum (thiamine transporter 1) and potentially decreases thiamine production by intestinal flora in the lumen 206
Small intestinal bacterial overgrowth can be treated specifically with certain oral antibiotics such as rifaximin, neomycin, and metronidazole, which can improve postoperative thiamine deficiency in Roux-en-y gastric bypass patients 207, 143, 144. The use of broad-spectrum antibiotics (penicillins, cephalosporins, aminoglycosides, tetracyclines, fluoroquinolones, sulfonamides, trimethoprim), however, can potentially cause thiamine deficit in some patients by reducing counts of normal intestinal bacteria that produce thiamine (eg, Escherichia coli, bifidobacteria, Lactobacillus spp) and by promoting the growth of pathogenic flora such as Clostridium spp, which produce thiaminases 208, 42. Metronidazole, a thiazole, has been shown to be a substrate for thiaminase 1. Formation of thiamine antimetabolites from metronidazole, which can occur particularly with high cumulative doses or prolonged use of metronidazole, can inhibit thiamine pyrophosphokinase, leading to irreversible, painful, peripheral neuropathy 184.
Table 3. Effects of drugs and antithiamine agents on thiamine
| Drug family/antithiamine agent | Drug | Effect on thiamine |
|---|---|---|
| Alcohol | Ethanol | Decreased intestinal thiamine transport |
| Antibiotic | Metronidazole | Production of thiamine antimetabolites |
| Antibiotics | β-lactams, aminoglycosides, trimethoprim, quinolones | Decreased production of thiamine by intestinal microbiota |
| Chemotherapy | 5-fluorouracil | Decreased production of hepatic thiamine, decreased TKT activity |
| Polyphenols (coffee, tea) | Caffeic acid, tannic acid | Oxidation of thiazole ring |
| Diuretics | Furosemide, thiazides | Increased renal excretion, decreased intestinal absorption |
| Flavonoids | Quercetin, rutin | Oxidation to thiamine disulfide |
| Food preservatives | Sulfites | Disruption of thiamine methylene bridge |
| Oral hypoglycemics (biguanide) | Metformin | THTR2 inhibitor, prevents active transport of thiamine |
| Proton pump inhibitors | Omeprazole | Inactivation of PDH, erythrocyte transketolase, and H/K ATPase |
Abbreviations: H/K ATPase = hydrogen/potassium adenosine triphosphatase; PDH = pyruvate dehydrogenase; TKT = transketolase; THTR2 = thiamine transporter 2.
[Source 8 ]Groups at risk of thiamine deficiency
The following groups are among those most likely to have inadequate thiamine status 17.
People with alcohol dependence
In highly industrialized countries, chronic alcohol use disorders appear to be the most common cause of thiamine deficiency 1. Up to 80% of people with chronic alcoholism develop thiamine deficiency because ethanol reduces gastrointestinal absorption of thiamine, thiamine stores in the liver, and thiamine phosphorylation 9, 132. Also, people with alcoholism tend to have inadequate intakes of essential nutrients, including thiamine.
Older adults
Up to 20%–30% of older adults have laboratory indicators that suggest some degree of thiamine deficiency 7, 113. Possible reasons include low dietary intakes, a combination of chronic diseases, concomitant use of multiple medications, and low absorption of thiamin as a natural result of aging 209, 46. Some small studies have found that the risk of deficiency is particularly high in elderly people who reside in an institution 54, 60.
People with HIV/AIDS
People with HIV infection have an increased risk of thiamin deficiency and its sequelae, including beriberi and Wernicke-Korsakoff syndrome 1, 210. Autopsies of 380 people with AIDS found that almost 10% had Wernicke’s encephalopathy 211, and some experts believe that thiamin deficiency is underdiagnosed in this population 212. The association between thiamin deficiency and HIV/AIDS is probably due to malnutrition as a result of the catabolic state associated with AIDS 17.
People with diabetes
Some small studies have found that thiamine levels in plasma are up to 76% lower in people with type 1 diabetes than in healthy volunteers and 50%–75% lower in people with type 2 diabetes 213, 30. Other studies have shown a higher risk of thiamine deficiency in people with type 1 and/or type 2 diabetes based on tests of erythrocyte transketolase activity 35, 214. These lower thiamine levels might be due to increases in clearance of thiamin by the kidneys. The relevance of these effects to clinical prognosis or outcomes is not known.
People who have undergone weight loss surgery
Weight loss surgery also called bariatric surgery for weight loss is associated with some risks, including severe thiamine deficiency due to malabsorption that can lead to beriberi or Wernicke’s encephalopathy 17. A 2008 literature review identified 84 cases of Wernicke’s encephalopathy after bariatric surgery (primarily gastric bypass surgery) between 1991 and 2008 215. About half of these patients experienced long-lasting neurologic impairments. Micronutrient supplements that include thiamine are almost always recommended for patients following weight loss surgery to avoid deficiencies 216.
Thiamine deficiency prevention
Eating a proper diet that is rich in vitamins will prevent thiamine deficiency. Nursing mothers should make sure that their diet contains all vitamins. If your infant is not breastfed, make sure that the infant formula contains thiamine.
If you drink alcohol, try to cut down or quit. Also, take B vitamins to make sure your body is properly absorbing and storing thiamine.
Thiamine deficiency symptoms
Most people have no symptoms and signs of thiamine deficiency or vitamin B1 deficiency; therefore, it must be suspected in the appropriate clinical setting 125. Thiamine deficiency or vitamin B1 deficiency early symptoms and signs are often nonspecific and vague, such as fatigue. However, early symptoms mainly arise from neurological, heart and gastrointestinal systems, where patients may experience weight loss, anorexia, confusion, short-term amnesia, malaise, muscle weakness, and heart symptoms due to heart failure 126.
Generally, heart effects of thiamine deficiency are referred to as “wet beriberi”, the peripheral neurological signs and symptoms of thiamine deficiency are called “dry beriberi”, and delirium, mental confusion and abnormal eye movements (due to ophthalmoplegia, which is paralysis or weakness of the eye muscles), stance and gait ataxia are termed “cerebral beriberi” or Wernicke’s encephalopathy 127, 23, 19. “Gastrointestinal beriberi” is caused by lactic acidosis, a condition resulting from the accumulation of lactate and is often associated with nausea, vomiting, and severe abdominal pain 128.
Thiamine deficiency cardiovascular signs and symptoms are as follows:
- Fast heart rate (tachycardia)
- Chest pain
- Wide pulse pressure
- Heart failure (orthopnea with or without edema, warm skin due to vasodilation) 217
- Hypotension, shock
Thiamine deficiency gastroenterologic signs and symptoms are as follows:
- Anorexia
- Abdominal discomfort
- Constipation
- Difficulty swallowing (dysphagia) 218
Thiamine deficiency neurologic signs and symptoms of thiamine deficiency are as follows 219:
- Poor memory, irritability, sleep disturbance
- Wernicke encephalopathy and/or Korsakoff syndrome 220
- Bilateral, symmetrical lower extremity paresthesias, burning pain
- Muscle cramps
- Decreased vibratory position sensation
- Absent knee and ankle jerk
- Muscle atrophy
- Foot drop (late stage)
- Abnormal eye movement (back and forth movements called nystagmus) – most common (early sign) 221
Thiamine deficiency infantile beriberi signs and symptoms are as follows 222:
- Congestive heart failure
- Loss of voice (aphonia)
- Absent deep tendon reflex.
A study by Mifsud et al 221 described the characteristics of 56 cases of thiamine deficiency that were seen at a French tertiary hospital. A history of alcohol abuse was found in 45 patients (80%), and while neurologic symptoms were the basis for diagnosis in the majority of individuals, there were frequent instances of nonspecific and digestive symptoms. Moreover, the criteria for malnutrition were fulfilled in 34% of patients. Of the 54% of patients in whom brain magnetic resonance imaging (MRI) scans were performed, abnormal scans were found in 63% of cases 221.
A study by Isenberg-Grzeda et al 223 indicated that thiamine deficiency may be a frequent occurrence among inpatients with cancer, even in those who are of normal weight or overweight, lack other vitamin deficiencies, and are receiving multivitamin supplements. The single-center study found thiamine deficiency in 55.3% of 217 patients, with risk factors for the deficiency including active cancer treatment and fluorouracil-based chemotherapy 223.
A literature review by Jain et al 45 comparing the incidence of thiamine deficiency in patients with heart failure to that in controls reported an odds ratio of 2.53, with possible reasons for the deficiency in heart failure including diuretic use, dietary changes, and alterations in the absorption and metabolism of thiamine. The literature also indicated that thiamine supplementation may improve symptoms and ejection fraction in patients with heart failure 45.
Beriberi signs and symptoms
Beriberi is a disease in which the body does not have enough thiamine or vitamin B1.
There are two major types of beriberi:
- Wet beriberi: Thiamine deficiency with cardiovascular system involvement is termed wet beriberi. The chronic form of wet beriberi consists of 3 stages. In the first stage, peripheral vasodilation occurs, leading to a high cardiac output state. This leads to salt and water retention mediated through the renin-angiotensin-aldosterone system in the kidneys. As the vasodilation progresses, the kidneys detect a relative loss of volume and respond by conserving salt. With the salt retention, fluid is also absorbed into the circulatory system. The resulting fluid overload leads to edema of the dependent extremities.
- Dry beriberi: Thiamine deficiency with nervous system involvement is termed dry beriberi. This presentation usually occurs when poor caloric intake and relative physical inactivity are present. The neurologic findings can be peripheral neuropathy characterized by symmetrical impairment of sensory, motor, and reflex functions of the extremities, especially in the distal lower limbs. Histologic analysis has shown that the lesions arise from a degeneration of the myelin in the muscular sheaths without inflammation 224.
- Cerebral beriberi also known as Wernicke-Korsakoff syndrome that affects the nervous system 225.
Symptoms of “dry beriberi” include:
- Difficulty walking
- Loss of feeling (sensation) in hands and feet
- Loss of muscle function or paralysis of the lower legs
- Mental confusion
- Pain
- Speech difficulties
- Strange eye movements (nystagmus)
- Tingling
- Vomiting
Symptoms of “wet beriberi” include:
- Awakening at night short of breath
- Increased heart rate
- Shortness of breath with activity
- Swelling of the lower legs
Wernicke-Korsakoff syndrome signs and symptoms
Wernicke encephalopathy and Korsakoff syndrome are often thought to be on a spectrum with one another as they are both due to thiamine or vitamin B1 deficiency. Wernicke’s encephalopathy causes brain damage in lower parts of the brain called the thalamus and hypothalamus 226. Korsakoff’s psychosis results from permanent damage to areas of the brain involved with memory 226. Therefore, clinicians should screen for them together. Wernicke encephalopathy classically presents with the triad of altered mental status, ophthalmoplegia, and ataxia. In reality, less than 20% of patients will present with all three of these findings 129. Korsakoff syndrome or Korsakoff’s psychosis is a neuropsychiatric disorder associated with memory disturbances in which there are significant deficits in anterograde and retrograde memory. Immediate memory is maintained, but short-term memory is diminished with intact sensorium. The disorder is associated with patients fabricating stories in the setting of clear consciousness. Confabulations can be spontaneous or provoked with provoked confabulation commonly seen in chronic Korsakoff syndrome and spontaneous confabulation usually noted in the acute Wernicke’s encephalopathy 227, 228.
The following signs and symptoms should cause suspicion for Wernicke-Korsakoff syndrome 129:
- Altered mental status (up to 82% of patients) – amnesia, disorientation, confabulations
- Oculomotor findings – most often horizontal nystagmus, retinal hemorrhage, ophthalmoplegia, cranial nerve IV palsy, conjugate gaze
- Loss of muscular coordination (ataxia) – wide-based gait. Ataxia is likely to be a combination of polyneuropathy, cerebellar damage, and vestibular paresis. Vestibular dysfunction, usually without hearing loss, is universally impaired in the acute stages of Wernicke encephalopathy.
The cognitive impairments specific to Korsakoff syndrome vs. Wernicke encephalopathy include anterograde amnesia, profoundly limiting one’s learning capacity, retrograde amnesia, as well as executive deficits, resulting in decreased inhibition and difficulties with judgment, planning and problem-solving 229. Anterograde amnesia can result in the classic symptom of confabulations, replacing one’s gap in memory with untrue information 230.
Symptoms of Wernicke encephalopathy include:
- Confusion and loss of mental activity that can progress to coma and death
- Loss of muscle coordination (ataxia) that can cause leg tremor
- Vision changes such as abnormal eye movements (back and forth movements called nystagmus), double vision, eyelid drooping
- Alcohol withdrawal
Symptoms of Korsakoff syndrome include:
- Inability to form new memories
- Loss of memory, can be severe
- Making up stories (confabulation)
- Seeing or hearing things that are not really there (hallucinations)
Thiamine deficiency complications
Thiamine deficiency complications may include:
- Coma
- Congestive heart failure
- Death
- Psychosis
Thiamine deficiency diagnosis
A physical examination may show signs of congestive heart failure, including:
- Difficulty breathing, with neck veins that stick out
- Enlarged heart
- Fluid in the lungs
- Rapid heartbeat
- Swelling in both lower legs
A person with late-stage beriberi may be confused or have memory loss and delusions. The person may be less able to sense vibrations. The person may appear poorly nourished.
A physical examination of the nervous and muscular system may show signs of damage to many nerve systems:
- Changes in walking
- Coordination problems
- Abnormal eye movement
- Drooping of the eyelids
- Decreased or abnormal reflexes
- Fast pulse (heart rate)
- Low blood pressure
- Low body temperature
- Muscle weakness and atrophy (loss of tissue mass)
- Problems with walk (gait) and coordination.
For practical reasons, replacing thiamine as an initial test may be most feasible 231. If the patient responds to thiamine administration, it is safe to assume that a measure of thiamine deficiency was responsible for the signs and symptoms 231. Thiamine is not toxic in high levels, which means that this route carries little risk. In addition, time is saved in treating the patient and money is saved in testing. However, although observation of a patient’s clinical response to thiamine administration remains the easiest, least expensive form of testing, clinicians usually miss the subclinical forms of thiamine deficiency 231.
The diagnosis of Wernicke’s encephalopathy is a histopathological diagnosis, made after a postmortem examination of the brain 232, 233, 234.
The Caine criteria have been described to have a sensitivity or 85% and specificity of 100% for Wernicke encephalopathy, in the alcoholic population 235, 129. Because of the strong overlap, the Caine criteria can be used to help screen for Korsakoff syndrome as well.
Caine criteria for the diagnosis of Wernicke encephalopathy in chronic alcoholics 235. When 2 out of these 4 criteria apply, the clinical diagnosis of Wernicke encephalopathy is made 129, 235:
- Dietary deficiencies
- Undernutrition (body mass index <2 SD below normal)
- A history of grossly impaired dietary intake
- An abnormal thiamine status
- Oculomotor abnormalities
- Ophthalmoplegia
- Nystagmus
- Gaze palsy
- Cerebellar dysfunction
- Unsteadiness or ataxia
- Abnormalities of past pointing
- Dysdiadokokinesia
- Impaired heel-shin testing
- Either an altered mental state OR mild memory impairment
- Altered mental status
- Disorientation in two of three fields
- Confused
- An abnormal digit span
- Comatose
- Mild memory impairment
- Failure to remember two or more words in the four-item memory test
- Impairment on more elaborate neuropsychological tests of memory function
- Altered mental status
The following tests are used to check a person’s nutrition level:
- Serum albumin (relates to person’s general nutrition)
- Transketolase activity in red blood cells (reduced in people with thiamine deficiency). The serum level of thiamin is not a reliable indicator of thiamin status. However, thiamin function can be measured by red blood cells transketolase activity (erythrocytes transketolase activity or ETKA). Red blood cells transketolase activity (EKTA) of 0 to 15% is considered adequate, 15 to 25% is considered a moderate risk, and 25% or higher is considered high risk for thiamin deficiency 236, 237.
- Serum vitamin B1 or thiamine levels. Direct measurement of erythrocyte thiamin pyrophosphate (TPP) can be done using whole-blood testing and has more sensitivity, specificity, precision, and robustness 236. The concentration of TPP in the whole blood ranges from 70 to 180 nmol/L 123.
- Urine tests to see if thiamine is passing through the urine. Urinary thiamine excretion can be used to measure adequate dietary intake. However, it does not reflect the thiamine stores in the body. In adults, urinary thiamine excretion of <100 mcg/day suggests inadequate intake, and less than 40 mcg/day suggests thiamin deficiency 18.
- Liver enzymes may be high in people with a history of long-term alcohol abuse.
A brain MRI may show changes in the tissue of the brain. But if Wernicke-Korsakoff syndrome is suspected, treatment should start immediately. Usually a brain MRI exam is not needed.
Thiamine deficiency treatment
In suspected cases of thiamine deficiency, prompt administration of parenteral (intravenously or intramuscularly) thiamine is indicated.
To treat mild thiamine deficiency, the World Health Organization (WHO) recommends daily oral doses of 10 mg thiamine for a week, followed by 3–5 mg/daily for at least 6 weeks 141. For patients at risk of thiamine deficiency or with confirmed thiamine deficiency, parenteral (intravenously or intramuscularly) thiamine of 100 mg and 200 mg 3 times a day has been used, respectively, in clinical practice 72. The recommended treatment for severe thiamine deficiency consists of 25–30 mg intravenously in infants and 50–100 mg in adults, then 10 mg daily administered intramuscularly for approximately one week, followed by 3–5 mg/day oral thiamine for at least 6 weeks 17.
The preferred dose of thiamine treatment for Wernicke encephalopathy may be as high as 500 mg intravenous thiamine given three times daily for 3 to 5 days, followed by intravenous thiamine, 250 mg/day for 3 to 5 days or until the symptoms disappear, and then further treatment with oral thiamine, 100 mg/day 238, 225. The rationale for using three times daily dosing of intravenous thiamine in acute presentations is based on the short half-life of intravenous thiamine (96 minutes) and the slow, carrier mediated process of thiamine transport across the blood–brain barrier 8. A single intravenous dose of thiamine is less likely to achieve sufficient brain tissue levels, and the bioavailability of oral thiamine hydrochloride is only 3.7% to 5.3% 238.
All malnourished patient may need higher doses of thiamine 225. Thiamine is generally administered before or together with glucose solutions because the glucose oxidation can decrease thiamine levels thereby exacerbating the neurological symptoms of Wernicke encephalopathy 225. Patients with magnesium deficiency should also be treated as this can result in reduced recovery from Wernicke encephalopathy especially in patients with alcoholism 239, 230, 240. Following a review of 19 papers, it has been recommended not to delay in correcting hypoglycemia 241. There are suggestions that prolonged and not acute replacement of glucose without thiamine supplementation increased the risk of Wernicke encephalopathy.
For Korsakoff syndrome high dose thiamine at 500 mg to 1500 mg, IV, three times daily for at least 3 days 129. Electrolyte abnormalities should be corrected and fluids replaced. In particular, magnesium requires replacement, as thiamine-dependent enzymes cannot operate in a magnesium-deficient state. Many patients will present needing glucose replacement as well, and traditionally it was thought that replacing glucose before thiamine could exacerbate the patient’s symptoms 138.
Thiamine, even at high concentrations, is not toxic in a person with normal kidney function 242. No cases of thiamine toxicity have been reported from the use of thiamine at the dosages indicated, even in patients in critical condition 242.
Once clinical symptoms improve, thiamine supplementation can switch to the oral route with a dose range of 50 to 100 mg per day 6. It is equally important in individuals with thiamine deficiency to require other nutrient supplementation such as magnesium, vitamin B2 (riboflavin), vitamin B3 (nicotinamide), vitamin B6 (pyridoxine), vitamin B12, vitamin C, potassium, and phosphate 17.
Support for cardiac function is necessary in cases of wet beriberi, because lack of cardiac support leads to low-output cardiac failure when the thiamine deficiency is corrected 242.
Follow-up care until delivery of current pregnancy, intensive care for advanced cardiomyopathy, definitive care for hyperthyroidism, or further workup of intestinal derangement may be warranted in patients with thiamine deficiency 242.
Blood tests may be repeated after the treatment is started. These tests will show how well you are responding to the medicine.
After the acute phase of vitamin and electrolyte replacement, there is mounting evidence that memory rehabilitation is beneficial in Korsakoff syndrome. Declarative memory (“knowing what”) seems to be most affected in Korsakoff syndrome, leading to many patients requiring lifelong care. Because procedural learning (“knowing how”) seems to remain somewhat maintained in Korsakoff syndrome, memory rehabilitation focussed in this area has shown promising outcomes. There has been some success in small Korsakoff syndrome patient populations in learning procedures and improving their autonomy 229.
Thiamine deficiency recovery time
Beriberi can be quickly fatal or can slowly rob an individual of almost all energy for even the simplest of daily activities. However, beriberi is one of the most easily treatable thiamine deficiency, with a remarkable recovery being possible even in severe cases 243. Therefore, the patient prognosis for beriberi is usually good, unless patients have established Korsakoff syndrome. While thiamine can induce partial improvement, the neuropsychological deficits persist in many cases. The confusional state usually improves when IV thiamine is administered but the learning and memory deficits only improve partially. A small number of patients fail to have any improvement and may develop Korsakoff psychosis or Korsakoff syndrome, which often requires institutionalization. Very few individuals recover at this point.
In cases of wet beriberi, clinical improvement can be observed within 12 hours of treatment, with normalization of heart function and size occurring in 1 or 2 days 243. The recovery is so dramatic that treatment with thiamine is a diagnostic test, which can be used in cases of acute heart failure and insidious peripheral neuropathy 243.
A retrospective study by Harel et al 244 indicated that thiamine deficiency in infancy can lead to long-term motor function problems. The study looked at children aged 5-6 years who, during the first 2 years of life, had been fed a faulty milk substitute that was deficient in thiamine, comparing them with age-matched controls. The Movement Assessment Battery for Children and the Zuk Assessment indicated that motor function difficulties existed in 56% and 59%, respectively, of the thiamine-deficient formula group, compared with 10% and 3%, respectively, of the control group. The results suggested that infantile thiamine deficiency affects gross and fine motor function, as well as balance skills 244.
Thiamine deficiency prognosis
Untreated, beriberi can be fatal. With treatment, symptoms usually improve quickly. Heart damage is usually reversible. A full recovery is expected in these cases. However, if acute heart failure has already occurred, the outlook is poor.
Nervous system damage is also reversible, if caught early. High suspicion for Wernicke’s encephalopathy is key to improving patient prognosis. Classically, the thinking was that once Korsakoff syndrome has set in, memory loss (amnesia) was generally irreversible, even with treatment 245, 246, 138. Several case studies and eight double-blind trials have been published, where Korsakoff syndrome patients were treated with clonidine, fluvoxamine, reboxetine, or rivastigmine. Together, these studies did not produce any consistent evidence for the efficacy of any of these interventions 247. Therefore, until this date, no effective pharmacological treatment for Korsakoff syndrome is available 130. More recent research has shown promise in memory rehabilitation including memory compensation techniques and error-less learning strategies 130. If a person with Wernicke encephalopathy receives thiamine replacement, language problems, unusual eye movements, and walking difficulties may go away. However, Korsakoff syndrome or Korsakoff psychosis tends to develop as Wernicke symptoms go away.
Regarding neuroimaging, associations with cortical lesions have shown to correlate with a worse prognosis 129.
- Said HM. Thiamin. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:748-53.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Sharma S, Sheehy T, Kolonel LN. Ethnic differences in grains consumption and their contribution to intake of B-vitamins: results of the Multiethnic Cohort Study. Nutr J. 2013 May 20;12:65. doi: 10.1186/1475-2891-12-65[↩][↩]
- Fulgoni VL 3rd, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J Nutr. 2011 Oct;141(10):1847-54. doi: 10.3945/jn.111.142257[↩][↩][↩]
- Wooley, J.A. (2008), Characteristics of Thiamin and Its Relevance to the Management of Heart Failure. Nutr Clin Pract, 23: 487-493. https://doi.org/10.1177/0884533608323430[↩][↩]
- Saldanha LG, Dwyer JT, Bailen RA. Modernization of the National Institutes of Health Dietary Supplement Label Database. J Food Compost Anal. 2021 Sep;102:104058. doi: 10.1016/j.jfca.2021.104058[↩]
- Sriram, K., Manzanares, W. and Joseph, K. (2012), Thiamine in Nutrition Therapy. Nutrition in Clinical Practice, 27: 41-50. https://doi.org/10.1177/0884533611426149[↩][↩][↩][↩]
- Bettendorff L. Thiamin. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:261-79.[↩][↩][↩][↩]
- Wilson RB. Pathophysiology, prevention, and treatment of beriberi after gastric surgery. Nutr Rev. 2020 Dec 1;78(12):1015-1029. doi: 10.1093/nutrit/nuaa004[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bemeur C, Butterworth RF. Thiamin. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:317-24.[↩][↩][↩][↩][↩][↩][↩][↩]
- Thiamine. Monograph. Altern Med Rev. 2003 Feb;8(1):59-62.[↩]
- Tallaksen CM, Sande A, Bøhmer T, Bell H, Karlsen J. Kinetics of thiamin and thiamin phosphate esters in human blood, plasma and urine after 50 mg intravenously or orally. Eur J Clin Pharmacol. 1993;44(1):73-8. doi: 10.1007/BF00315284[↩]
- Lonsdale D. A review of the biochemistry, metabolism and clinical benefits of thiamin(e) and its derivatives. Evid Based Complement Alternat Med. 2006 Mar;3(1):49-59. doi: 10.1093/ecam/nek009[↩]
- Bettendorff, L. and Wins, P. (2009), Thiamin diphosphate in biological chemistry: new aspects of thiamin metabolism, especially triphosphate derivatives acting other than as cofactors. The FEBS Journal, 276: 2917-2925. https://doi.org/10.1111/j.1742-4658.2009.07019.x[↩]
- Manzetti S, Zhang J, van der Spoel D. Thiamin function, metabolism, uptake, and transport. Biochemistry. 2014 Feb 11;53(5):821-35. doi: 10.1021/bi401618y[↩]
- Nabokina SM, Said HM. A high-affinity and specific carrier-mediated mechanism for uptake of thiamine pyrophosphate by human colonic epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2012 Aug 1;303(3):G389-95. doi: 10.1152/ajpgi.00151.2012[↩]
- Lonsdale D. Thiamin. Adv Food Nutr Res. 2018;83:1-56. doi: 10.1016/bs.afnr.2017.11.001[↩][↩][↩][↩]
- Thiamin. https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Gibson GE, Blass JP. Thiamine-dependent processes and treatment strategies in neurodegeneration. Antioxid Redox Signal. 2007 Oct;9(10):1605-19. doi: 10.1089/ars.2007.1766[↩][↩]
- Thiamin. https://lpi.oregonstate.edu/mic/vitamins/thiamin[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Rindi G. Thiamin. In: Ziegler E, Filer L, eds. Present Knowledge in Nutrition. Washington D.C.: ILSI Press; 1996:160-166.[↩][↩][↩]
- Hutson SM, Sweatt AJ, Lanoue KF. Branched-chain [corrected] amino acid metabolism: implications for establishing safe intakes. J Nutr. 2005 Jun;135(6 Suppl):1557S-64S. doi: 10.1093/jn/135.6.1557S. Erratum in: J Nutr. 2005 Aug;135(8):2009.[↩][↩]
- Brody T. Nutritional Biochemistry. 2nd ed. San Diego: Academic Press; 1999.[↩]
- Tanphaichitr V. Thiamin. In: Shils M, ed. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins; 1999:381-389.[↩][↩][↩][↩][↩]
- Bettendorff L. Thiamin. In: Erdman Jr. JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Ames: Wiley-Blackwell; 2012:261-279.[↩][↩]
- Whitfield KC, Bourassa MW, Adamolekun B, Bergeron G, Bettendorff L, Brown KH, Cox L, Fattal-Valevski A, Fischer PR, Frank EL, Hiffler L, Hlaing LM, Jefferds ME, Kapner H, Kounnavong S, Mousavi MPS, Roth DE, Tsaloglou MN, Wieringa F, Combs GF Jr. Thiamine deficiency disorders: diagnosis, prevalence, and a roadmap for global control programs. Ann N Y Acad Sci. 2018 Oct;1430(1):3-43. doi: 10.1111/nyas.13919[↩]
- Foulon V, Antonenkov VD, Croes K, Waelkens E, Mannaerts GP, Van Veldhoven PP, Casteels M. Purification, molecular cloning, and expression of 2-hydroxyphytanoyl-CoA lyase, a peroxisomal thiamine pyrophosphate-dependent enzyme that catalyzes the carbon-carbon bond cleavage during alpha-oxidation of 3-methyl-branched fatty acids. Proc Natl Acad Sci U S A. 1999 Aug 31;96(18):10039-44. doi: 10.1073/pnas.96.18.10039[↩]
- Cumming RG, Mitchell P, Smith W. Diet and cataract: the Blue Mountains Eye Study. Ophthalmology. 2000 Mar;107(3):450-6. doi: 10.1016/s0161-6420(99)00024-x[↩]
- Jacques PF, Taylor A, Moeller S, Hankinson SE, Rogers G, Tung W, Ludovico J, Willett WC, Chylack LT Jr. Long-term nutrient intake and 5-year change in nuclear lens opacities. Arch Ophthalmol. 2005 Apr;123(4):517-26. doi: 10.1001/archopht.123.4.517[↩]
- Rosner EA, Strezlecki KD, Clark JA, Lieh-Lai M. Low thiamine levels in children with type 1 diabetes and diabetic ketoacidosis: a pilot study. Pediatr Crit Care Med. 2015 Feb;16(2):114-8. doi: 10.1097/PCC.0000000000000302[↩]
- Thornalley PJ, Babaei-Jadidi R, Al Ali H, Rabbani N, Antonysunil A, Larkin J, Ahmed A, Rayman G, Bodmer CW. High prevalence of low plasma thiamine concentration in diabetes linked to a marker of vascular disease. Diabetologia. 2007 Oct;50(10):2164-70. doi: 10.1007/s00125-007-0771-4[↩][↩]
- Larkin JR, Zhang F, Godfrey L, Molostvov G, Zehnder D, Rabbani N, Thornalley PJ. Glucose-induced down regulation of thiamine transporters in the kidney proximal tubular epithelium produces thiamine insufficiency in diabetes. PLoS One. 2012;7(12):e53175. doi: 10.1371/journal.pone.0053175[↩]
- Rathanaswami P, Sundaresan R. Effects of thiamine deficiency on the biosynthesis of insulin in rats. Biochem Int. 1991 Aug;24(6):1057-62.[↩]
- Rathanaswami P, Pourany A, Sundaresan R. Effects of thiamine deficiency on the secretion of insulin and the metabolism of glucose in isolated rat pancreatic islets. Biochem Int. 1991 Oct;25(3):577-83.[↩]
- Page GL, Laight D, Cummings MH. Thiamine deficiency in diabetes mellitus and the impact of thiamine replacement on glucose metabolism and vascular disease. Int J Clin Pract. 2011 Jun;65(6):684-90. doi: 10.1111/j.1742-1241.2011.02680.x[↩]
- Jermendy G. Evaluating thiamine deficiency in patients with diabetes. Diab Vasc Dis Res. 2006 Sep;3(2):120-1. doi: 10.3132/dvdr.2006.014[↩][↩]
- González-Ortiz M, Martínez-Abundis E, Robles-Cervantes JA, Ramírez-Ramírez V, Ramos-Zavala MG. Effect of thiamine administration on metabolic profile, cytokines and inflammatory markers in drug-naïve patients with type 2 diabetes. Eur J Nutr. 2011 Mar;50(2):145-9. doi: 10.1007/s00394-010-0123-x[↩][↩]
- Alaei Shahmiri F, Soares MJ, Zhao Y, Sherriff J. High-dose thiamine supplementation improves glucose tolerance in hyperglycemic individuals: a randomized, double-blind cross-over trial. Eur J Nutr. 2013 Oct;52(7):1821-4. doi: 10.1007/s00394-013-0534-6[↩][↩]
- Stracke H, Gaus W, Achenbach U, Federlin K, Bretzel RG. Benfotiamine in diabetic polyneuropathy (BENDIP): results of a randomised, double blind, placebo-controlled clinical study. Exp Clin Endocrinol Diabetes. 2008 Nov;116(10):600-5. doi: 10.1055/s-2008-1065351[↩]
- Carpenter KJ. The discovery of thiamin. Ann Nutr Metab. 2012;61(3):219-23. doi: 10.1159/000343109[↩]
- Rabbani N, Alam SS, Riaz S, Larkin JR, Akhtar MW, Shafi T, Thornalley PJ. High-dose thiamine therapy for patients with type 2 diabetes and microalbuminuria: a randomised, double-blind placebo-controlled pilot study. Diabetologia. 2009 Feb;52(2):208-12. doi: 10.1007/s00125-008-1224-4[↩]
- Alkhalaf A, Klooster A, van Oeveren W, Achenbach U, Kleefstra N, Slingerland RJ, Mijnhout GS, Bilo HJ, Gans RO, Navis GJ, Bakker SJ. A double-blind, randomized, placebo-controlled clinical trial on benfotiamine treatment in patients with diabetic nephropathy. Diabetes Care. 2010 Jul;33(7):1598-601. doi: 10.2337/dc09-2241[↩]
- DiNicolantonio, J.J., Niazi, A.K., Lavie, C.J., O’Keefe, J.H. and Ventura, H.O. (2013), Thiamine Supplementation for the Treatment of Heart Failure: A Review of the Literature. Congest Heart Fail, 19: 214-222. https://doi.org/10.1111/chf.12037[↩][↩][↩][↩][↩][↩]
- Hanninen SA, Darling PB, Sole MJ, Barr A, Keith ME. The prevalence of thiamin deficiency in hospitalized patients with congestive heart failure. J Am Coll Cardiol. 2006 Jan 17;47(2):354-61. doi: 10.1016/j.jacc.2005.08.060[↩][↩]
- Katta N, Balla S, Alpert MA. Does Long-Term Furosemide Therapy Cause Thiamine Deficiency in Patients with Heart Failure? A Focused Review. Am J Med. 2016 Jul;129(7):753.e7-753.e11. doi: 10.1016/j.amjmed.2016.01.037[↩]
- Jain A, Mehta R, Al-Ani M, Hill JA, Winchester DE. Determining the Role of Thiamine Deficiency in Systolic Heart Failure: A Meta-Analysis and Systematic Review. J Card Fail. 2015 Dec;21(12):1000-7. doi: 10.1016/j.cardfail.2015.10.005[↩][↩][↩][↩]
- T J Wilkinson, H C Hanger, P M George, R Sainsbury, Is thiamine deficiency in elderly people related to age or co-morbidity?, Age and Ageing, Volume 29, Issue 2, March 2000, Pages 111–116, https://doi.org/10.1093/ageing/29.2.111[↩][↩]
- Zenuk C, Healey J, Donnelly J, Vaillancourt R, Almalki Y, Smith S. Thiamine deficiency in congestive heart failure patients receiving long term furosemide therapy. Can J Clin Pharmacol. 2003 Winter;10(4):184-8.[↩][↩]
- Shimon I, Almog S, Vered Z, Seligmann H, Shefi M, Peleg E, Rosenthal T, Motro M, Halkin H, Ezra D. Improved left ventricular function after thiamine supplementation in patients with congestive heart failure receiving long-term furosemide therapy. Am J Med. 1995 May;98(5):485-90. doi: 10.1016/s0002-9343(99)80349-0[↩][↩]
- Leslie D, Gheorghiade M. Is there a role for thiamine supplementation in the management of heart failure? Am Heart J. 1996 Jun;131(6):1248-50. doi: 10.1016/s0002-8703(96)90121-0[↩]
- Mousavi, Mehdi & S, Namazi & M, Avadi & Amirahmadi, Maryam. (2017). Thiamine Supplementation in Patients with Chronic Heart Failure Receiving Optimum Medical Treatment. Journal of Cardiology & Current Research. 9. 00316. 10.15406/jccr.2017.09.00316[↩]
- Keith M, Quach S, Ahmed M, Azizi-Namini P, Al-Hesayen A, Azevedo E, James R, Leong-Poi H, Ong G, Desjardins S, Lee PJ, Ravamehr-Lake D, Yan AT. Thiamin supplementation does not improve left ventricular ejection fraction in ambulatory heart failure patients: a randomized controlled trial. Am J Clin Nutr. 2019 Dec 1;110(6):1287-1295. doi: 10.1093/ajcn/nqz192[↩]
- Dinicolantonio JJ, Lavie CJ, Niazi AK, O’Keefe JH, Hu T. Effects of thiamine on cardiac function in patients with systolic heart failure: systematic review and metaanalysis of randomized, double-blind, placebo-controlled trials. Ochsner J. 2013 Winter;13(4):495-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865826[↩]
- Goel A, Kattoor AJ, Mehta JL. Thiamin therapy for chronic heart failure: is there any future for this vitamin? Am J Clin Nutr. 2019 Dec 1;110(6):1270-1271. doi: 10.1093/ajcn/nqz246[↩]
- Ito Y, Yamanaka K, Susaki H, Igata A. A cross-investigation between thiamin deficiency and the physical condition of elderly people who require nursing care. J Nutr Sci Vitaminol (Tokyo). 2012;58(3):210-6. doi: 10.3177/jnsv.58.210[↩][↩]
- Lee, D.C., Chu, J., Satz, W. and Silbergleit, R. (2000), Low Plasma Thiamine Levels in Elder Patients Admitted through the Emergency Department. Academic Emergency Medicine, 7: 1156-1159. https://doi.org/10.1111/j.1553-2712.2000.tb01268.x[↩]
- Prvulovic D, Hampel H. Amyloid β (Aβ) and phospho-tau (p-tau) as diagnostic biomarkers in Alzheimer’s disease. Clin Chem Lab Med. 2011 Mar;49(3):367-74. doi: 10.1515/CCLM.2011.087[↩]
- Gibson GE, Hirsch JA, Cirio RT, Jordan BD, Fonzetti P, Elder J. Abnormal thiamine-dependent processes in Alzheimer’s Disease. Lessons from diabetes. Mol Cell Neurosci. 2013 Jul;55:17-25. doi: 10.1016/j.mcn.2012.09.001[↩]
- Gibson GE, Sheu KF, Blass JP, Baker A, Carlson KC, Harding B, Perrino P. Reduced activities of thiamine-dependent enzymes in the brains and peripheral tissues of patients with Alzheimer’s disease. Arch Neurol. 1988 Aug;45(8):836-40. doi: 10.1001/archneur.1988.00520320022009[↩]
- Butterworth RF, Besnard AM. Thiamine-dependent enzyme changes in temporal cortex of patients with Alzheimer’s disease. Metab Brain Dis. 1990 Dec;5(4):179-84. doi: 10.1007/BF00997071[↩]
- NICHOLAS P. O’ROURKE, VALDA W. BUNKER, ANITA J. THOMAS, PAUL M. FINGLAS, ANGELA L. BAILEY, BARBARA E. CLAYTON, Thiamine Status of Healthy and Institutionalized Elderly Subjects: Analysis of Dietary Intake and Biochemical Indices, Age and Ageing, Volume 19, Issue 5, September 1990, Pages 325–329, https://doi.org/10.1093/ageing/19.5.325[↩][↩]
- Rodríguez-Martín JL, López-Arrieta JM, Qizilbash N. Thiamine for Alzheimer’s disease. Cochrane Database Syst Rev. 2000;(2):CD001498. doi: 10.1002/14651858.CD001498. Update in: Cochrane Database Syst Rev. 2001;(2):CD001498.[↩][↩]
- Blass JP, Gleason P, Brush D, DiPonte P, Thaler H. Thiamine and Alzheimer’s disease. A pilot study. Arch Neurol. 1988 Aug;45(8):833-5. doi: 10.1001/archneur.1988.00520320019008[↩]
- Nolan KA, Black RS, Sheu KF, Langberg J, Blass JP. A trial of thiamine in Alzheimer’s disease. Arch Neurol. 1991 Jan;48(1):81-3. doi: 10.1001/archneur.1991.00530130093025[↩]
- Meador K, Loring D, Nichols M, Zamrini E, Rivner M, Posas H, Thompson E, Moore E. Preliminary findings of high-dose thiamine in dementia of Alzheimer’s type. J Geriatr Psychiatry Neurol. 1993 Oct-Dec;6(4):222-9. doi: 10.1177/089198879300600408[↩]
- Picó S, Parras A, Santos-Galindo M, Pose-Utrilla J, Castro M, Fraga E, Hernández IH, Elorza A, Anta H, Wang N, Martí-Sánchez L, Belloc E, Garcia-Esparcia P, Garrido JJ, Ferrer I, Macías-García D, Mir P, Artuch R, Pérez B, Hernández F, Navarro P, López-Sendón JL, Iglesias T, Yang XW, Méndez R, Lucas JJ. CPEB alteration and aberrant transcriptome-polyadenylation lead to a treatable SLC19A3 deficiency in Huntington’s disease. Sci Transl Med. 2021 Sep 29;13(613):eabe7104. doi: 10.1126/scitranslmed.abe7104[↩][↩][↩]
- Trial of the Combined Use of Thiamine and Biotin in Patients With Huntington’s Disease (HUNTIAM). https://clinicaltrials.gov/ct2/show/NCT04478734[↩]
- Day E, Bentham PW, Callaghan R, Kuruvilla T, George S. Thiamine for prevention and treatment of Wernicke-Korsakoff Syndrome in people who abuse alcohol. Cochrane Database Syst Rev. 2013 Jul 1;2013(7):CD004033. doi: 10.1002/14651858.CD004033.pub3[↩][↩][↩]
- Akhouri S, Kuhn J, Newton EJ. Wernicke-Korsakoff Syndrome. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430729[↩]
- Gerridzen IJ, Joling KJ, Depla MF, Veenhuizen RB, Verschuur EML, Twisk JWR, Hertogh CMPM. Awareness and its relationships with neuropsychiatric symptoms in people with Korsakoff syndrome or other alcohol-related cognitive disorders living in specialized nursing homes. Int J Geriatr Psychiatry. 2019 Jun;34(6):836-845. doi: 10.1002/gps.5093[↩]
- Yoon C, Gedzior J, DePry D. Wernicke-Korsakoff syndrome: Focus on low-threshold diagnosis and prompt treatment in the primary care setting. Int J Psychiatry Med. 2019 May;54(3):172-180. doi: 10.1177/0091217419832771[↩]
- van Dongen LCM, Wingbermühle E, van der Veld WM, Vermeulen K, Bos-Roubos AG, Ockeloen CW, Kleefstra T, Egger JIM. Exploring the behavioral and cognitive phenotype of KBG syndrome. Genes Brain Behav. 2019 Apr;18(4):e12553. doi: 10.1111/gbb.12553[↩]
- Galvin, R., Bråthen, G., Ivashynka, A., Hillbom, M., Tanasescu, R. and Leone, M.A. (2010), EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. European Journal of Neurology, 17: 1408-1418. https://doi.org/10.1111/j.1468-1331.2010.03153.x[↩][↩][↩]
- Allan D. Thomson, Christopher C. H. Cook, Robin Touquet, John A. Henry, THE ROYAL COLLEGE OF PHYSICIANS REPORT ON ALCOHOL: GUIDELINES FOR MANAGING WERNICKE’S ENCEPHALOPATHY IN THE ACCIDENT AND EMERGENCY DEPARTMENT, Alcohol and Alcoholism, Volume 37, Issue 6, November 2002, Pages 513–521, https://doi.org/10.1093/alcalc/37.6.513[↩]
- Seligmann H, Levi R, Konijn AM, Prokocimer M. Thiamine deficiency in patients with B-chronic lymphocytic leukaemia: a pilot study. Postgrad Med J. 2001 Sep;77(911):582-5. doi: 10.1136/pmj.77.911.582[↩][↩]
- Isenberg-Grzeda E, Alici Y, Hatzoglou V, Nelson C, Breitbart W. Nonalcoholic Thiamine-Related Encephalopathy (Wernicke-Korsakoff Syndrome) Among Inpatients With Cancer: A Series of 18 Cases. Psychosomatics. 2016 Jan-Feb;57(1):71-81. doi: 10.1016/j.psym.2015.10.001[↩][↩]
- Comín-Anduix, B., Boren, J., Martinez, S., Moro, C., Centelles, J.J., Trebukhina, R., Petushok, N., Lee, W.-N.P., Boros, L.G. and Cascante, M. (2001), The effect of thiamine supplementation on tumour proliferation. European Journal of Biochemistry, 268: 4177-4182. https://doi.org/10.1046/j.1432-1327.2001.02329.x[↩]
- Zastre JA, Hanberry BS, Sweet RL, McGinnis AC, Venuti KR, Bartlett MG, Govindarajan R. Up-regulation of vitamin B1 homeostasis genes in breast cancer. J Nutr Biochem. 2013 Sep;24(9):1616-24. doi: 10.1016/j.jnutbio.2013.02.002[↩]
- Lu’o’ng KV, Nguyễn LT. The role of thiamine in cancer: possible genetic and cellular signaling mechanisms. Cancer Genomics Proteomics. 2013 Jul-Aug;10(4):169-85. https://cgp.iiarjournals.org/content/10/4/169.long[↩]
- Aksoy M, Basu TK, Brient J, Dickerson JW. Thiamin status of patients treated with drug combinations containing 5-fluorouracil. Eur J Cancer (1965). 1980 Aug;16(8):1041-5. doi: 10.1016/0014-2964(80)90251-0[↩]
- Basu TK. Vitamins – cytotoxic drug interaction. Int J Vitam Nutr Res Suppl. 1983;24:225-33.[↩]
- Boros LG, Brandes JL, Lee WN, Cascante M, Puigjaner J, Revesz E, Bray TM, Schirmer WJ, Melvin WS. Thiamine supplementation to cancer patients: a double edged sword. Anticancer Res. 1998 Jan-Feb;18(1B):595-602.[↩]
- What is Sepsis? https://www.cdc.gov/sepsis/what-is-sepsis.html[↩][↩]
- Moskowitz A, Donnino MW. Thiamine (vitamin B1) in septic shock: a targeted therapy. J Thorac Dis. 2020 Feb;12(Suppl 1):S78-S83. doi: 10.21037/jtd.2019.12.82[↩]
- Woolum JA, Abner EL, Kelly A, Thompson Bastin ML, Morris PE, Flannery AH. Effect of Thiamine Administration on Lactate Clearance and Mortality in Patients With Septic Shock. Crit Care Med. 2018 Nov;46(11):1747-1752. doi: 10.1097/CCM.0000000000003311[↩]
- Holmberg MJ, Moskowitz A, Patel PV, Grossestreuer AV, Uber A, Stankovic N, Andersen LW, Donnino MW. Thiamine in septic shock patients with alcohol use disorders: An observational pilot study. J Crit Care. 2018 Feb;43:61-64. doi: 10.1016/j.jcrc.2017.08.022[↩]
- Donnino MW, Andersen LW, Chase M, Berg KM, Tidswell M, Giberson T, Wolfe R, Moskowitz A, Smithline H, Ngo L, Cocchi MN; Center for Resuscitation Science Research Group. Randomized, Double-Blind, Placebo-Controlled Trial of Thiamine as a Metabolic Resuscitator in Septic Shock: A Pilot Study. Crit Care Med. 2016 Feb;44(2):360-7. doi: 10.1097/CCM.0000000000001572[↩][↩]
- Moskowitz A, Andersen LW, Cocchi MN, Karlsson M, Patel PV, Donnino MW. Thiamine as a Renal Protective Agent in Septic Shock. A Secondary Analysis of a Randomized, Double-Blind, Placebo-controlled Trial. Ann Am Thorac Soc. 2017 May;14(5):737-741. doi: 10.1513/AnnalsATS.201608-656BC[↩]
- Qian X, Zhang Z, Li F, Wu L. Intravenous thiamine for septic shock: A meta-analysis of randomized controlled trials. Am J Emerg Med. 2020 Dec;38(12):2718-2722. doi: 10.1016/j.ajem.2020.08.050[↩]
- Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest. 2017 Jun;151(6):1229-1238. doi: 10.1016/j.chest.2016.11.036[↩]
- Pyruvate dehydrogenase deficiency. https://medlineplus.gov/genetics/condition/pyruvate-dehydrogenase-deficiency[↩][↩][↩][↩][↩]
- Naito E, Ito M, Yokota I, Saijo T, Ogawa Y, Kuroda Y. Diagnosis and molecular analysis of three male patients with thiamine-responsive pyruvate dehydrogenase complex deficiency. J Neurol Sci. 2002 Sep 15;201(1-2):33-7. doi: 10.1016/s0022-510x(02)00187-9[↩]
- Patel KP, O’Brien TW, Subramony SH, Shuster J, Stacpoole PW. The spectrum of pyruvate dehydrogenase complex deficiency: clinical, biochemical and genetic features in 371 patients. Mol Genet Metab. 2012 Jul;106(3):385-94. doi: 10.1016/j.ymgme.2012.03.017[↩]
- Lee EH, Ahn MS, Hwang JS, Ryu KH, Kim SJ, Kim SH. A Korean female patient with thiamine-responsive pyruvate dehydrogenase complex deficiency due to a novel point mutation (Y161C)in the PDHA1 gene. J Korean Med Sci. 2006 Oct;21(5):800-4. doi: 10.3346/jkms.2006.21.5.800[↩]
- Maple syrup urine disease. https://medlineplus.gov/genetics/condition/maple-syrup-urine-disease[↩][↩][↩]
- Chuang DT, Chuang JL, Wynn RM. Lessons from genetic disorders of branched-chain amino acid metabolism. J Nutr. 2006 Jan;136(1 Suppl):243S-9S. doi: 10.1093/jn/136.1.243S[↩]
- Labay V, Raz T, Baron D, Mandel H, Williams H, Barrett T, Szargel R, McDonald L, Shalata A, Nosaka K, Gregory S, Cohen N. Mutations in SLC19A2 cause thiamine-responsive megaloblastic anaemia associated with diabetes mellitus and deafness. Nat Genet. 1999 Jul;22(3):300-4. doi: 10.1038/10372[↩]
- Shaw-Smith, C, Flanagan, SE, Patch, A-M, Grulich-Henn, J, Habeb, AM, Hussain, K, Pomahacova, R, Matyka, K, Abdullah, M, Hattersley, AT, Ellard, S. Recessive SLC19A2 mutations are a cause of neonatal diabetes mellitus in thiamine-responsive megaloblastic anaemia. https://doi.org/10.1111/j.1399-5448.2012.00855.x[↩]
- Habeb AM, Flanagan SE, Zulali MA, Abdullah MA, Pomahačová R, Boyadzhiev V, Colindres LE, Godoy GV, Vasanthi T, Al Saif R, Setoodeh A, Haghighi A, Haghighi A, Shaalan Y; International Neonatal Diabetes Consortium; Hattersley AT, Ellard S, De Franco E. Pharmacogenomics in diabetes: outcomes of thiamine therapy in TRMA syndrome. Diabetologia. 2018 May;61(5):1027-1036. doi: 10.1007/s00125-018-4554-x[↩][↩]
- Akın L, Kurtoğlu S, Kendirci M, Akın MA, Karakükçü M. Does early treatment prevent deafness in thiamine-responsive megaloblastic anaemia syndrome? J Clin Res Pediatr Endocrinol. 2011;3(1):36-9. doi: 10.4274/jcrpe.v3i1.08[↩]
- Tabarki B, Al-Hashem A, Alfadhel M. Biotin-Thiamine-Responsive Basal Ganglia Disease. 2013 Nov 21 [Updated 2020 Aug 20]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK169615[↩][↩]
- Kılıç B, Topçu Y, Dursun Ş, Erol İ, Dolu MH, Taşdemir HA, Aydın K. Single gene, two diseases, and multiple clinical presentations: Biotin-thiamine-responsive basal ganglia disease. Brain Dev. 2020 Sep;42(8):572-580. doi: 10.1016/j.braindev.2020.05.008[↩][↩]
- Alfadhel M, Almuntashri M, Jadah RH, Bashiri FA, Al Rifai MT, Al Shalaan H, Al Balwi M, Al Rumayan A, Eyaid W, Al-Twaijri W. Biotin-responsive basal ganglia disease should be renamed biotin-thiamine-responsive basal ganglia disease: a retrospective review of the clinical, radiological and molecular findings of 18 new cases. Orphanet J Rare Dis. 2013 Jun 6;8:83. doi: 10.1186/1750-1172-8-83[↩][↩]
- Tabarki B, Alfadhel M, AlShahwan S, Hundallah K, AlShafi S, AlHashem A. Treatment of biotin-responsive basal ganglia disease: Open comparative study between the combination of biotin plus thiamine versus thiamine alone. Eur J Paediatr Neurol. 2015 Sep;19(5):547-52. doi: 10.1016/j.ejpn.2015.05.008[↩]
- Algahtani H, Ghamdi S, Shirah B, Alharbi B, Algahtani R, Bazaid A. Biotin-thiamine-responsive basal ganglia disease: catastrophic consequences of delay in diagnosis and treatment. Neurol Res. 2017 Feb;39(2):117-125. doi: 10.1080/01616412.2016.1263176[↩]
- Tabarki B, Thabet F, Alfadhel M. SLC25A19-Related Thiamine Metabolism Dysfunction. 2003 Sep 4 [Updated 2023 Mar 30]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1365[↩]
- Chen Y, Fang B, Hu X, Guo R, Guo J, Fang K, Ni J, Li W, Qian S, Hao C. Identification and functional analysis of novel SLC25A19 variants causing thiamine metabolism dysfunction syndrome 4. Orphanet J Rare Dis. 2021 Sep 29;16(1):403. doi: 10.1186/s13023-021-02028-4[↩]
- THIAMINE METABOLISM DYSFUNCTION SYNDROME 5 (EPISODIC ENCEPHALOPATHY TYPE); THMD5. https://omim.org/entry/614458[↩]
- Mayr JA, Freisinger P, Schlachter K, Rolinski B, Zimmermann FA, Scheffner T, Haack TB, Koch J, Ahting U, Prokisch H, Sperl W. Thiamine pyrophosphokinase deficiency in encephalopathic children with defects in the pyruvate oxidation pathway. Am J Hum Genet. 2011 Dec 9;89(6):806-12. doi: 10.1016/j.ajhg.2011.11.007[↩]
- Thiamin. https://ods.od.nih.gov/factsheets/Thiamin-Consumer[↩][↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998[↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. What We Eat in America, 2013-2014. 2012. https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweia-data-tables/[↩]
- The USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998.[↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 27. Nutrient Data Laboratory home page, 2014. https://ndb.nal.usda.gov/ndb/[↩]
- National Institutes of Health. Dietary Supplement Label Database. 2014.[↩][↩]
- Aguilar F, Charrondiere UR, Dusemund B, Galtier P, Gilbert J, Gott DM, et al. Benfotiamine, thiamine monophosphate chloride and thiamine pyrophosphate chloride, as sources of vitamin B1 added for nutritional purposes to food supplements: Scientific Opinion of the Panel on Food Additives and Nutrient Sources added to Food (ANS). EFSA J 2008;864:1-31.[↩]
- World Health Organization. Geneva: Department of Nutrition for Health and Development, WHO; 1999. Thiamine deficiency and its prevention and control in major emergencies. Report no: WHO/NHD/99.13.[↩]
- Fattal-Valevski A, Kesler A, Sela BA, Nitzan-Kaluski D, Rotstein M, Mesterman R, Toledano-Alhadef H, Stolovitch C, Hoffmann C, Globus O, Eshel G. Outbreak of life-threatening thiamine deficiency in infants in Israel caused by a defective soy-based formula. Pediatrics. 2005 Feb;115(2):e233-8. https://doi.org/10.1542/peds.2004-1255[↩]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Vitamin B. [Updated 2021 May 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548710[↩][↩]
- Thomson AD, Baker H, Leevy CM. Patterns of 35S-thiamine hydrochloride absorption in the malnourished alcoholic patient. J Lab Clin Med. 1970 Jul;76(1):34-45.[↩]
- Thomson AD, Jeyasingham MD, Pratt OE, Shaw GK. Nutrition and alcoholic encephalopathies. Acta Med Scand Suppl. 1987;717:55-65. doi: 10.1111/j.0954-6820.1987.tb13042.x[↩]
- Kumar N. Neurologic presentations of nutritional deficiencies. Neurol Clin. 2010 Feb;28(1):107-70. doi: 10.1016/j.ncl.2009.09.006[↩]
- Frank, L.L. (2015), Thiamin in Clinical Practice. Journal of Parenteral and Enteral Nutrition, 39: 503-520. https://doi.org/10.1177/0148607114565245[↩][↩][↩]
- Kerns JC, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015 Mar 13;6(2):147-53. doi: 10.3945/an.114.007526[↩]
- Beriberi (Thiamine Deficiency) Clinical Presentation. https://emedicine.medscape.com/article/116930-clinical[↩][↩]
- Martel JL, Kerndt CC, Doshi H, et al. Vitamin B1 (Thiamine) [Updated 2022 Aug 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482360[↩][↩][↩][↩][↩]
- Yamasaki H, Tada H, Kawano S, Aonuma K. Reversible pulmonary hypertension, lactic acidosis, and rapidly evolving multiple organ failure as manifestations of shoshin beriberi. Circ J. 2010 Sep;74(9):1983-5. doi: 10.1253/circj.cj-10-0202[↩][↩]
- Donnino M. Gastrointestinal beriberi: a previously unrecognized syndrome. Ann Intern Med. 2004 Dec 7;141(11):898-9. doi: 10.7326/0003-4819-141-11-200412070-00035[↩][↩]
- Sharp CS, Wilson MP, Nordstrom K. Psychiatric Emergencies for Clinicians: Emergency Department Management of Wernicke-Korsakoff Syndrome. J Emerg Med. 2016 Oct;51(4):401-404. doi: 10.1016/j.jemermed.2016.05.044[↩][↩][↩][↩][↩][↩][↩]
- Arts NJ, Walvoort SJ, Kessels RP. Korsakoff’s syndrome: a critical review. Neuropsychiatr Dis Treat. 2017 Nov 27;13:2875-2890. doi: 10.2147/NDT.S130078[↩][↩][↩][↩]
- Thomson AD, Guerrini I, Marshall EJ. The evolution and treatment of Korsakoff’s syndrome: out of sight, out of mind? Neuropsychol Rev. 2012 Jun;22(2):81-92. doi: 10.1007/s11065-012-9196-z[↩]
- ROBERTA AGABIO, THIAMINE ADMINISTRATION IN ALCOHOL-DEPENDENT PATIENTS, Alcohol and Alcoholism, Volume 40, Issue 2, March/April 2005, Pages 155–156, https://doi.org/10.1093/alcalc/agh106[↩][↩]
- ALLAN D. THOMSON, E. JANE MARSHALL, THE NATURAL HISTORY AND PATHOPHYSIOLOGY OF WERNICKE’S ENCEPHALOPATHY AND KORSAKOFF’S PSYCHOSIS, Alcohol and Alcoholism, Volume 41, Issue 2, March/April 2006, Pages 151–158, https://doi.org/10.1093/alcalc/agh249[↩]
- Talland G. Deranged Memory: A Psychonomic Study of the Amnesic Syndrome. New York: Academic Press; 1965.[↩]
- Kopelman MD. The Korsakoff syndrome. Br J Psychiatry. 1995 Feb;166(2):154-73. doi: 10.1192/bjp.166.2.154[↩]
- Michael D. Kopelman, Allan D. Thomson, Irene Guerrini, E. Jane Marshall, The Korsakoff Syndrome: Clinical Aspects, Psychology and Treatment, Alcohol and Alcoholism, Volume 44, Issue 2, March-April 2009, Pages 148–154, https://doi.org/10.1093/alcalc/agn118[↩][↩]
- Segal JB, Bouffard MA, Schlaug G. Characteristic Neuroimaging Abnormalities of Korsakoff Syndrome. JAMA Neurol. 2016;73(10):1248–1249. doi:10.1001/jamaneurol.2016.1843[↩]
- Covell T, Siddiqui W. Korsakoff Syndrome. [Updated 2023 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539854[↩][↩][↩]
- Nikolakaros G, Ilonen T, Kurki T, Paju J, Papageorgiou SG, Vataja R. Non-alcoholic Korsakoff syndrome in psychiatric patients with a history of undiagnosed Wernicke’s encephalopathy. J Neurol Sci. 2016 Nov 15;370:296-302. doi: 10.1016/j.jns.2016.09.025[↩]
- Isenberg-Grzeda E, Rahane S, DeRosa AP, Ellis J, Nicolson SE. Wernicke-Korsakoff syndrome in patients with cancer: a systematic review. Lancet Oncol. 2016 Apr;17(4):e142-e148. doi: 10.1016/S1470-2045(16)00037-1[↩]
- Thiamine deficiency and its prevention and control in major emergencies. 23 February 1999. https://www.who.int/publications/i/item/WHO-NHD-99.13[↩][↩]
- World Health Organization, United Nations High Commissioner for Refugees. Thiamine deficiency and its prevention and control in major emergencies. https://apps.who.int/iris/bitstream/handle/10665/66139/WHO_NHD_99.13.pdf[↩][↩][↩][↩][↩][↩][↩]
- Lakhani SV, Shah HN, Alexander K, Finelli FC, Kirkpatrick JR, Koch TR. Small intestinal bacterial overgrowth and thiamine deficiency after Roux-en-Y gastric bypass surgery in obese patients. Nutr Res. 2008 May;28(5):293-8. doi: 10.1016/j.nutres.2008.03.002[↩][↩]
- Shah HN, Bal BS, Finelli FC, Koch TR. Constipation in patients with thiamine deficiency after Roux-en-Y gastric bypass surgery. Digestion. 2013;88(2):119-24. doi: 10.1159/000353245[↩][↩][↩]
- Brown, G. (2014), Defects of thiamine transport and metabolism. J Inherit Metab Dis, 37: 577-585. https://doi.org/10.1007/s10545-014-9712-9[↩][↩]
- Beriberi. https://medlineplus.gov/ency/article/000339.htm[↩][↩]
- Arnold D. British India and the “beriberi problem”, 1798-1942. Med Hist. 2010 Jul;54(3):295-314. doi: 10.1017/s0025727300004622[↩][↩]
- Baeltz B. Ueber das Verhältniss der multiplen peripherischen Neuritis zur Beriberi (Panneuritis endemica) [in German]. Z Klin Med. 1882;4:616–617.[↩]
- Truswell, A.S. (2000), Australian experience with the Wernicke–Korsakoff syndrome. Addiction, 95: 829-832. https://doi.org/10.1046/j.1360-0443.2000.9568291.x[↩]
- Beriberi (Thiamine Deficiency). https://emedicine.medscape.com/article/116930-overview[↩][↩]
- Greenspon J, Perrone EE, Alaish SM. Shoshin beriberi mimicking central line sepsis in a child with short bowel syndrome. World J Pediatr. 2010 Nov;6(4):366-8. doi: 10.1007/s12519-010-0022-5[↩]
- Saad L, Silva LF, Banzato CE, Dantas CR, Garcia C Jr. Anorexia nervosa and Wernicke-Korsakoff syndrome: a case report. J Med Case Rep. 2010 Jul 20;4:217. doi: 10.1186/1752-1947-4-217[↩]
- Jung ES, Kwon O, Lee SH, Lee KB, Kim JH, Yoon SH, Kim GM, Jeung HC, Rha SY. Wernicke’s encephalopathy in advanced gastric cancer. Cancer Res Treat. 2010 Jun;42(2):77-81. doi: 10.4143/crt.2010.42.2.77[↩]
- Becker DA, Balcer LJ, Galetta SL. The Neurological Complications of Nutritional Deficiency following Bariatric Surgery. J Obes. 2012;2012:608534. doi: 10.1155/2012/608534[↩]
- Nath A, Tran T, Shope TR, Koch TR. Prevalence of clinical thiamine deficiency in individuals with medically complicated obesity. Nutr Res. 2017 Jan;37:29-36. doi: 10.1016/j.nutres.2016.11.012[↩]
- Polegato, B.F., Pereira, A.G., Azevedo, P.S., Costa, N.A., Zornoff, L.A.M., Paiva, S.A.R. and Minicucci, M.F. (2019), Role of Thiamin in Health and Disease. Nutrition in Clinical Practice, 34: 558-564. https://doi.org/10.1002/ncp.10234[↩]
- Oudman E, Wijnia JW, Oey M, van Dam M, Painter RC, Postma A. Wernicke’s encephalopathy in hyperemesis gravidarum: A systematic review. Eur J Obstet Gynecol Reprod Biol. 2019 May;236:84-93. doi: 10.1016/j.ejogrb.2019.03.006[↩]
- Meggs WJ, Lee SK, Parker-Cote JN. Wernicke encephalopathy associated with hyperemesis gravidarum. Am J Emerg Med. 2020 Mar;38(3):690.e3-690.e5. doi: 10.1016/j.ajem.2019.09.012[↩]
- Sequeira Lopes da Silva JT, Almaraz Velarde R, Olgado Ferrero F, Robles Marcos M, Pérez Civantos D, Ramírez Moreno JM, Luengo Pérez LM. Wernicke’s encephalopathy induced by total parental nutrition. Nutr Hosp. 2010 Nov-Dec;25(6):1034-6.[↩]
- Francini-Pesenti F, Brocadello F, Manara R, Santelli L, Laroni A, Caregaro L. Wernicke’s syndrome during parenteral feeding: not an unusual complication. Nutrition. 2009 Feb;25(2):142-6. doi: 10.1016/j.nut.2008.08.003[↩]
- Zastre JA, Sweet RL, Hanberry BS, Ye S. Linking vitamin B1 with cancer cell metabolism. Cancer Metab. 2013 Jul 24;1(1):16. doi: 10.1186/2049-3002-1-16[↩]
- Thurnham DI, Cathcart AE, Livingstone MB. A retrospective investigation of thiamin and energy intakes following an outbreak of beriberi in The Gambia. Nutrients. 2011 Jan;3(1):135-51. doi: 10.3390/nu3010135[↩][↩]
- Koike H, Misu K, Hattori N, Ito S, Ichimura M, Ito H, Hirayama M, Nagamatsu M, Sasaki I, Sobue G. Postgastrectomy polyneuropathy with thiamine deficiency. J Neurol Neurosurg Psychiatry. 2001 Sep;71(3):357-62. doi: 10.1136/jnnp.71.3.357[↩]
- Spinazzi M, Angelini C, Patrini C. Subacute sensory ataxia and optic neuropathy with thiamine deficiency. Nat Rev Neurol. 2010 May;6(5):288-93. doi: 10.1038/nrneurol.2010.16[↩]
- Sobue G, Li M, Terao S, Aoki S, Ichimura M, Ieda T, Doyu M, Yasuda T, Hashizume Y, Mitsuma T. Axonal pathology in Japanese Guillain-Barré syndrome: a study of 15 autopsied cases. Neurology. 1997 Jun;48(6):1694-700. doi: 10.1212/wnl.48.6.1694[↩]
- Ohnishi A, Tsuji S, Igisu H, Murai Y, Goto I, Kuroiwa Y, Tsujihata M, Takamori M. Beriberi neuropathy. Morphometric study of sural nerve. J Neurol Sci. 1980 Mar;45(2-3):177-90. doi: 10.1016/0022-510x(80)90164-1[↩]
- Koike, H., Iijima, M., Sugiura, M., Mori, K., Hattori, N., Ito, H., Hirayama, M. and Sobue, G. (2003), Alcoholic neuropathy is clinicopathologically distinct from thiamine-deficiency neuropathy. Ann Neurol., 54: 19-29. https://doi.org/10.1002/ana.10550[↩]
- Khounnorath S, Chamberlain K, Taylor AM, Soukaloun D, Mayxay M, Lee SJ, Phengdy B, Luangxay K, Sisouk K, Soumphonphakdy B, Latsavong K, Akkhavong K, White NJ, Newton PN. Clinically unapparent infantile thiamin deficiency in Vientiane, Laos. PLoS Negl Trop Dis. 2011 Feb 22;5(2):e969. doi: 10.1371/journal.pntd.0000969[↩]
- Chiappetta S, Stein J. Refeeding Syndrome: An Important Complication Following Obesity Surgery. Obes Facts. 2016;9(1):12-6. doi: 10.1159/000442534[↩]
- Boateng AA, Sriram K, Meguid MM, Crook M. Refeeding syndrome: treatment considerations based on collective analysis of literature case reports. Nutrition. 2010 Feb;26(2):156-67. doi: 10.1016/j.nut.2009.11.017[↩]
- Marinella MA. Refeeding syndrome: implications for the inpatient rehabilitation unit. Am J Phys Med Rehabil. 2004 Jan;83(1):65-8. doi: 10.1097/01.PHM.0000104666.88102.99[↩]
- Raziel A. Thiamine deficiency after bariatric surgery may lead to Wernicke encephalopathy. Isr Med Assoc J. 2012 Nov;14(11):692-4[↩]
- Krishna S, Taylor AM, Supanaranond W, Pukrittayakamee S, ter Kuile F, Tawfiq KM, Holloway PA, White NJ. Thiamine deficiency and malaria in adults from southeast Asia. Lancet. 1999 Feb 13;353(9152):546-9. doi: 10.1016/s0140-6736(98)06316-8[↩]
- Mayxay M, Taylor AM, Khanthavong M, Keola S, Pongvongsa T, Phompida S, Phetsouvanh R, White NJ, Newton PN. Thiamin deficiency and uncomplicated falciparum malaria in Laos. Trop Med Int Health. 2007 Mar;12(3):363-9. doi: 10.1111/j.1365-3156.2006.01804.x[↩]
- Müri RM, Von Overbeck J, Furrer J, Ballmer PE. Thiamin deficiency in HIV-positive patients: evaluation by erythrocyte transketolase activity and thiamin pyrophosphate effect. Clin Nutr. 1999 Dec;18(6):375-8. doi: 10.1016/s0261-5614(99)80019-3[↩]
- Stanga Z, Brunner A, Leuenberger M, Grimble RF, Shenkin A, Allison SP, Lobo DN. Nutrition in clinical practice-the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr. 2008 Jun;62(6):687-94. doi: 10.1038/sj.ejcn.1602854[↩]
- Vimokesant SL, Hilker DM, Nakornchai S, Rungruangsak K, Dhanamitta S. Effects of betel nut and fermented fish on the thiamin status of northeastern Thais. Am J Clin Nutr. 1975 Dec;28(12):1458-63. doi: 10.1093/ajcn/28.12.1458[↩]
- Ventura A, Mafe MC, Bourguet M, Tornero C. Wernicke’s encephalopathy secondary to hyperthyroidism and ingestion of thiaminase-rich products. Neurologia. 2013 May;28(4):257-9. English, Spanish. doi: 10.1016/j.nrl.2012.01.005[↩]
- Soukaloun D, Lee SJ, Chamberlain K, Taylor AM, Mayxay M, Sisouk K, Soumphonphakdy B, Latsavong K, Akkhavong K, Phommachanh D, Sengmeuang V, Luangxay K, McDonagh T, White NJ, Newton PN. Erythrocyte transketolase activity, markers of cardiac dysfunction and the diagnosis of infantile beriberi. PLoS Negl Trop Dis. 2011 Feb 22;5(2):e971. doi: 10.1371/journal.pntd.0000971[↩]
- Earl JW, McCleary BV. Mystery of the poisoned expedition. Nature. 1994 Apr 21;368(6473):683-4. doi: 10.1038/368683a0[↩]
- MATSUKAWA D, CHANG S, MISAWA H, FUJIMIYA M, KOBAYASHI N, HORIKAWA Y, TAKATO K. Studies on the thiamine deficiency due to bacterial thiaminase. I. Investigations on intestinal contents. J Vitaminol (Kyoto). 1954 Jul 10;1(1):43-8. doi: 10.5925/jnsv1954.1.43[↩]
- Nishimune T, Watanabe Y, Okazaki H, Akai H. Thiamin is decomposed due to Anaphe spp. entomophagy in seasonal ataxia patients in Nigeria. J Nutr. 2000 Jun;130(6):1625-8. doi: 10.1093/jn/130.6.1625[↩]
- Vimokesant, S., Kunjara, S., Rungruangsak, K., Nakornchai, S. and Panijpan, B. (1982), BERIBERI CAUSED BY ANTITHIAMIN FACTORS IN FOOD AND ITS PREVENTION. Annals of the New York Academy of Sciences, 378: 123-136. https://doi.org/10.1111/j.1749-6632.1982.tb31191.x[↩]
- Bender DA. Nutritional Biochemistry of the Vitamins. 1st ed. Cambridge, UK: Cambridge University Press; 2003.[↩][↩]
- Carvajal-Moreno M. Mycotoxins that affect the human cardiovascular system. J Biomol Res Ther. 2015;4:2.[↩]
- Rosa CA, Keller KM, Oliveira AA, Almeida TX, Keller LA, Marassi AC, Kruger CD, Deveza MV, Monteiro BS, Nunes LM, Astoreca A, Cavaglieri LR, Direito GM, Eifert EC, Lima TA, Modernell KG, Nunes FI, Garcia AM, Luz MS, Oliveira DC. Production of citreoviridin by Penicillium citreonigrum strains associated with rice consumption and beriberi cases in the Maranhão State, Brazil. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2010 Feb;27(2):241-8. doi: 10.1080/19440040903289712[↩]
- Sulfiting agents: affirmation of GRAS status. Fed Regis. 1988;53:51065–51084.[↩]
- Sulfites – USA. https://farrp.unl.edu/sulfites-usa[↩]
- https://www.fda.gov/media/80337/download[↩]
- https://www.fda.gov/media/136310/download[↩]
- Suter PM, Haller J, Hany A, Vetter W. Diuretic use: a risk for subclinical thiamine deficiency in elderly patients. J Nutr Health Aging. 2000;4(2):69-71.[↩]
- Rieck J, Halkin H, Almog S, Seligman H, Lubetsky A, Olchovsky D, Ezra D. Urinary loss of thiamine is increased by low doses of furosemide in healthy volunteers. J Lab Clin Med. 1999 Sep;134(3):238-43. doi: 10.1016/s0022-2143(99)90203-2[↩]
- Sica, D.A. (2007), Loop Diuretic Therapy, Thiamine Balance, and Heart Failure. Congestive Heart Failure, 13: 244-247. https://doi.org/10.1111/j.1527-5299.2007.06260.x[↩]
- Misumida N, Umeda H, Iwase M. Shoshin beriberi induced by long-term administration of diuretics: a case report. Case Rep Cardiol. 2014;2014:878915. doi: 10.1155/2014/878915[↩]
- Hung SC, Hung SH, Tarng DC, Yang WC, Chen TW, Huang TP. Thiamine deficiency and unexplained encephalopathy in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2001 Nov;38(5):941-7. doi: 10.1053/ajkd.2001.28578[↩]
- Wilcox CS. Do diuretics cause thiamine deficiency? J Lab Clin Med. 1999 Sep;134(3):192-3. doi: 10.1016/s0022-2143(99)90198-1[↩]
- Nixon PF, Diefenbach RJ, Duggleby RG. Inhibition of transketolase and pyruvate decarboxylase by omeprazole. Biochem Pharmacol. 1992 Jul 7;44(1):177-9. doi: 10.1016/0006-2952(92)90053-l[↩][↩]
- Toh JW, Ong E, Wilson R. Hypomagnesaemia associated with long-term use of proton pump inhibitors. Gastroenterol Rep (Oxf). 2015 Aug;3(3):243-53. doi: 10.1093/gastro/gou054[↩][↩]
- Basu TK, Aksoy M, Dickerson JW. Effects of 5-fluorouracil on the thiamin status of adult female rats. Chemotherapy. 1979;25(2):70-6. doi: 10.1159/000237825[↩]
- Cho KP, Lee JS, Seong JS, Woo YM, Cho YJ, Jeong BJ, Sohn JH, Kim SJ. [Two cases of Wernicke´s encephalopathy that developed during total parenteral nutrition in colon cancer patients treated with 5-fluorouracil-based chemotherapy]. Korean J Gastroenterol. 2014 Sep 25;64(3):158-63. Korean. doi: 10.4166/kjg.2014.64.3.158[↩]
- Koenig H, Patel A. Biochemical basis for fluorouracil neurotoxicity. The role of Krebs cycle inhibition by fluoroacetate. Arch Neurol. 1970 Aug;23(2):155-60. doi: 10.1001/archneur.1970.00480260061008[↩]
- Arellano M, Malet-Martino M, Martino R, Gires P. The anti-cancer drug 5-fluorouracil is metabolized by the isolated perfused rat liver and in rats into highly toxic fluoroacetate. Br J Cancer. 1998;77(1):79-86. doi: 10.1038/bjc.1998.12[↩]
- Schümann K. Interactions between drugs and vitamins at advanced age. Int J Vitam Nutr Res. 1999;69:173–178. doi:10.1024/0300-9831.69.3.173[↩]
- Chen L, Shu Y, Liang X, Chen EC, Yee SW, Zur AA, Li S, Xu L, Keshari KR, Lin MJ, Chien HC, Zhang Y, Morrissey KM, Liu J, Ostrem J, Younger NS, Kurhanewicz J, Shokat KM, Ashrafi K, Giacomini KM. OCT1 is a high-capacity thiamine transporter that regulates hepatic steatosis and is a target of metformin. Proc Natl Acad Sci U S A. 2014 Jul 8;111(27):9983-8. doi: 10.1073/pnas.1314939111[↩]
- Liang X, Chien HC, Yee SW, Giacomini MM, Chen EC, Piao M, Hao J, Twelves J, Lepist EI, Ray AS, Giacomini KM. Metformin Is a Substrate and Inhibitor of the Human Thiamine Transporter, THTR-2 (SLC19A3). Mol Pharm. 2015 Dec 7;12(12):4301-10. doi: 10.1021/acs.molpharmaceut.5b00501[↩]
- Subramanya SB, Subramanian VS, Said HM. Chronic alcohol consumption and intestinal thiamin absorption: effects on physiological and molecular parameters of the uptake process. Am J Physiol Gastrointest Liver Physiol. 2010 Jul;299(1):G23-31. doi: 10.1152/ajpgi.00132.2010[↩]
- Salem A, Roland BC. Small intestinal bacterial overgrowth (SIBO). J Gastroint Dig Syst. 2014;4:225.[↩]
- Pelton R, LaValle JB, Hawkins E, Krinsky DL, eds. Drug-Induced Nutrient Depletion Handbook. Hudson, OH: Wolters Kluwer Clinical Drug Information (Lexicomp; );1999:258.[↩]
- Vognar, L. and Stoukides, J. (2009), The Role of Low Plasma Thiamin Levels in Cognitively Impaired Elderly Patients Presenting with Acute Behavioral Disturbances. Journal of the American Geriatrics Society, 57: 2166-2168. https://doi.org/10.1111/j.1532-5415.2009.02542.x[↩]
- Lu’o’ng KV, Nguyễn LT. The role of thiamine in cancer: possible genetic and cellular signaling mechanisms. Cancer Genomics Proteomics. 2013 Jul-Aug;10(4):169-85.[↩]
- Boldorini R, Vago L, Lechi A, Tedeschi F, Trabattoni GR. Wernicke’s encephalopathy: occurrence and pathological aspects in a series of 400 AIDS patients. Acta Biomed Ateneo Parmense. 1992;63(1-2):43-9.[↩]
- Larsen TR, Dragu D, Williams M. Wernicke’s Encephalopathy: An Unusual Consequence of the Acquired Immune Deficiency Syndrome-Case Report and Literature Review. Case Rep Med. 2013;2013:709474. doi: 10.1155/2013/709474[↩]
- Al-Attas OS, Al-Daghri NM, Alfadda AA, Abd-Alrahman SH, Sabico S. Blood thiamine and its phosphate esters as measured by high-performance liquid chromatography: levels and associations in diabetes mellitus patients with varying degrees of microalbuminuria. J Endocrinol Invest. 2012 Dec;35(11):951-6. doi: 10.3275/8126[↩]
- Saito N, Kimura M, Kuchiba A, Itokawa Y. Blood thiamine levels in outpatients with diabetes mellitus. J Nutr Sci Vitaminol (Tokyo). 1987 Dec;33(6):421-30. doi: 10.3177/jnsv.33.421[↩]
- Aasheim ET. Wernicke encephalopathy after bariatric surgery: a systematic review. Ann Surg. 2008 Nov;248(5):714-20. doi: 10.1097/SLA.0b013e3181884308[↩]
- Xanthakos SA. Nutritional deficiencies in obesity and after bariatric surgery. Pediatr Clin North Am. 2009 Oct;56(5):1105-21. doi: 10.1016/j.pcl.2009.07.002[↩]
- Shenoy VV, Patil PV, Nagar VS, Deshpande AK, Shedge RT, Badiye AP, Saigaonkar R. Congestive cardiac failure and anemia in a 15-year-old boy. J Postgrad Med. 2005 Jul-Sep;51(3):225-7.[↩]
- Karaiskos I, Katsarolis I, Stefanis L. Severe dysphagia as the presenting symptom of Wernicke-Korsakoff syndrome in a non-alcoholic man. Neurol Sci. 2008 Feb;29(1):45-6. doi: 10.1007/s10072-008-0859-8[↩]
- Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Front Psychiatry. 2019 Apr 4;10:207. doi: 10.3389/fpsyt.2019.00207[↩]
- Zuccoli G, Gallucci M, Capellades J, Regnicolo L, Tumiati B, Giadás TC, Bottari W, Mandrioli J, Bertolini M. Wernicke encephalopathy: MR findings at clinical presentation in twenty-six alcoholic and nonalcoholic patients. AJNR Am J Neuroradiol. 2007 Aug;28(7):1328-31. doi: 10.3174/ajnr.A0544[↩]
- Mifsud F, Messager D, Jannot AS, Védie B, Balanant NA, Poghosyan T, Flamarion E, Carette C, Lucas-Martini L, Czernichow S, Rives-Lange C. Clinical diagnosis, outcomes and treatment of thiamine deficiency in a tertiary hospital. Clin Nutr. 2022 Jan;41(1):33-39. doi: 10.1016/j.clnu.2021.10.021[↩][↩][↩]
- S. Narasimha Rao, Shalini Mani, Karuna Madap, M. V. Kranthi Kumar, Lalji Singh, Giriraj Ratan Chandak, High Prevalence of Infantile Encephalitic Beriberi with Overlapping Features of Leigh’s Disease, Journal of Tropical Pediatrics, Volume 54, Issue 5, October 2008, Pages 328–332, https://doi.org/10.1093/tropej/fmn031[↩]
- Isenberg-Grzeda E, Shen MJ, Alici Y, Wills J, Nelson C, Breitbart W. High rate of thiamine deficiency among inpatients with cancer referred for psychiatric consultation: results of a single site prevalence study. Psychooncology. 2017 Sep;26(9):1384-1389. doi: 10.1002/pon.4155[↩][↩]
- Karuppagounder SS, Xu H, Pechman D, Chen LH, DeGiorgio LA, Gibson GE. Translocation of amyloid precursor protein C-terminal fragment(s) to the nucleus precedes neuronal death due to thiamine deficiency-induced mild impairment of oxidative metabolism. Neurochem Res. 2008 Jul;33(7):1365-72. doi: 10.1007/s11064-008-9594-z[↩]
- Vasan S, Kumar A. Wernicke Encephalopathy. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470344[↩][↩][↩][↩]
- Wernicke-Korsakoff syndrome. https://medlineplus.gov/ency/article/000771.htm[↩][↩]
- Karakonstantis S, Galani D, Korela D, Maragou S, Arna D, Basta M. Missing the early signs of thiamine deficiency. A case associated with a liquid-only diet. Nutr Neurosci. 2020 May;23(5):384-386. doi: 10.1080/1028415X.2018.1507964[↩]
- Oudman, E., Wijnia, J.W., Oey, M.J., van Dam, M.J. and Postma, A. (2018), Preventing Wernicke’s encephalopathy in anorexia nervosa: A systematic review. Psychiatry Clin. Neurosci., 72: 774-779. https://doi.org/10.1111/pcn.12735[↩]
- Oudman E, Nijboer TC, Postma A, Wijnia JW, Van der Stigchel S. Procedural Learning and Memory Rehabilitation in Korsakoff’s Syndrome – a Review of the Literature. Neuropsychol Rev. 2015 Jun;25(2):134-48. doi: 10.1007/s11065-015-9288-7[↩][↩]
- Johnson JM, Fox V. Beyond Thiamine: Treatment for Cognitive Impairment in Korsakoff’s Syndrome. Psychosomatics. 2018 Jul-Aug;59(4):311-317. doi: 10.1016/j.psym.2018.03.011[↩][↩]
- Beriberi (Thiamine Deficiency) Workup. https://emedicine.medscape.com/article/116930-workup[↩][↩][↩]
- Colmant H. Enzephalopathien Bei Chronischem Alkoholismus. Stuttgart: Enke; 1965.[↩]
- Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry. 1986 Apr;49(4):341-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1028756/pdf/jnnpsyc00096-0001.pdf[↩]
- Torvik A. Wernicke’s encephalopathy–prevalence and clinical spectrum. Alcohol Alcohol Suppl. 1991;1:381-4.[↩]
- Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997 Jan;62(1):51-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486695/pdf/jnnpsyc00001-0059.pdf[↩][↩][↩]
- Talwar D, Davidson H, Cooney J, St JO’Reilly D. Vitamin B(1) status assessed by direct measurement of thiamin pyrophosphate in erythrocytes or whole blood by HPLC: comparison with erythrocyte transketolase activation assay. Clin Chem. 2000 May;46(5):704-10.[↩][↩]
- Bates CJ. Vitamin analysis. Ann Clin Biochem. 1997 Nov;34 ( Pt 6):599-626. doi: 10.1177/000456329703400604[↩]
- Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: Micronutrients. Surg Obes Relat Dis. 2017 May;13(5):727-741. doi: 10.1016/j.soard.2016.12.018[↩][↩]
- Onishi H, Ishida M, Uchida N, Shintani D, Nishikawa T, Hasegawa K, Fujiwara K, Akechi T. Subclinical thiamine deficiency identified by preoperative evaluation in an ovarian cancer patient: Diagnosis and the need for preoperative thiamine measurement. Palliat Support Care. 2019 Oct;17(5):609-610. doi: 10.1017/S1478951518000615[↩]
- Oudman E, Wijnia JW, van Dam M, Biter LU, Postma A. Preventing Wernicke Encephalopathy After Bariatric Surgery. Obes Surg. 2018 Jul;28(7):2060-2068. doi: 10.1007/s11695-018-3262-4[↩]
- Schabelman E, Kuo D. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012 Apr;42(4):488-94. doi: 10.1016/j.jemermed.2011.05.076[↩]
- Beriberi (Thiamine Deficiency) Treatment & Management. https://emedicine.medscape.com/article/116930-treatment[↩][↩][↩][↩]
- Beriberi (Thiamine Deficiency). https://emedicine.medscape.com/article/116930-overview#a7[↩][↩][↩]
- Harel Y, Zuk L, Guindy M, Nakar O, Lotan D, Fattal-Valevski A. The effect of subclinical infantile thiamine deficiency on motor function in preschool children. Matern Child Nutr. 2017 Oct;13(4):e12397. doi: 10.1111/mcn.12397[↩][↩]
- Kessels R. Korsakoff syndrome. In: Weiner I, Craighead W, editors. The Corsini Encyclopedia of Psychology. New York: Wiley; 2010. pp. 902–904.[↩]
- Fujiwara E, Brand M, Borsutzky S, Steingass HP, Markowitsch HJ. Cognitive performance of detoxified alcoholic Korsakoff syndrome patients remains stable over two years. J Clin Exp Neuropsychol. 2008 Jul;30(5):576-87. doi: 10.1080/13803390701557271[↩]
- Arts N, Wiersma J. Psychofarmaca bij de behandeling van langetermijngevolgen van chronisch alcoholmisbruik. Psyfar. 2011;(3):54–57.[↩]