Contents
What is wasting syndrome
Wasting syndrome also known as cachexia, is an involuntary loss of more than 10% of body weight (especially muscle mass), plus at least 30 days of either diarrhea or weakness and fever. HIV-associated wasting syndrome is defined as an AIDS-defining condition 1. Wasting syndrome also occurs in the last stages of many diseases including heart failure, chronic obstructive pulmonary disease (COPD), kidney disease, and cancer. Wasting syndrome causes extreme loss of fat and muscle, leading to dramatic weight loss. Wasting syndrome can lead to such weakness that even routine activities can become difficult. When a patient with one of these illnesses appears gaunt and emaciated, he or she may be suffering from cachexia.
Up to 50% of all cancer patients may have some degree of cancer cachexia. Wasting syndrome especially common in people with colorectal, gastrointestinal, lung, or pancreatic cancer. Wasting syndrome may be responsible for 20 to 30% of all deaths related to cancer.
It’s easy to assume that if someone with cancer is wasting away, it’s because they aren’t eating enough. Weight loss from eating too little is known as anorexia. It’s true that having cancer and going through treatment can make patients feel less hungry and want to eat less. But that’s not the reason for weight loss with wasting syndrome. Scientists think the tumors themselves are the source of the factors that cause fat and muscle wasting.
Lung cancer patients with wasting syndrome tend to die sooner than those without it. That’s largely because of its effect on their treatment options, not because it occurs during the late stages of disease as people once thought. Fat wasting, which occurs before muscle wasting, can occur even in early stages of disease before the cancer’s spread.
Patients with cancer wasting syndrome have really limited treatment options. A patient with early- stage lung cancer would normally have surgery if it’s possible because it’s a potentially curative treatment. But if they have wasting syndrome, they can’t have surgery. Plus, these patients are too weak to endure chemotherapy, and if they are strong enough for it, they don’t respond as well to it as a lung cancer patient who doesn’t have wasting syndrome.
This means that even these early-stage patients have already lost the opportunity to get the standard care of treatment. Plus, if a patient’s lost too much weight or has wasting syndrome-associated fat and muscle wasting, they won’t be eligible for advanced clinical trials. Again, they’ve lost out on the opportunity to have the most effective treatment modalities.
What patients with cancer wasting syndrome are left with is often radiation alone. A patient can be wasting away, but doctors can still treat the tumor. And hopefully by treating the cancer, doctors can slow down the wasting process.
Previously, most researchers focused on how to reverse muscle loss from wasting syndrome. But research teams have fundamentally shift their emphasis of wasting syndrome to the fat changes and losses. With other types of disease, wasting syndrome is thought to be related to the immune system. But with cancer wasting syndrome, the cause seems to be something in the tumor. The tumor needs nutrition as a fuel support, and it doesn’t have the normal means of generating fuel that a noncachectic tumor has. So, it breaks down fat to use as its fuel.
Working with mice that have a cancer wasting syndrome, scientists have tried several things to suppress the tumor’s ability to cause fat and muscle loss. For instance, they’ve tried:
- Feeding the mice a high-fat diet, thinking that such a diet might limit the tumor’s “need” to break down fat. The results are promising.
- Giving mice a chemical that removes all their body fat before injecting cancer cells that cause wasting syndrome. Their thinking was that the tumors won’t grow as much without their fuel source, fat. And they don’t.
- Genetically altering the mice to remove a molecule that a tumor needs to be able to break down fat. This resulted in the tumor growing half as big as the tumor in mice who weren’t genetically altered.
- Using the anti-diabetic drug pioglitazone, which is known to affect fat storage, to see how it reprograms fat. The research team also wanted to know if this drug could block the tumor’s ability to break down fat. Scientists found that it limited the growth of the tumor, preserved the fat mass, and promoted the mice’s overall survival.
Scientists have definitely found ways to manipulate the tumors to make it less beneficial for them to break down fat. But they’re still early in the evolution of their understanding of this wasting syndrome, but they certainly have identified molecules and factors in a patient’s blood that can actually help them determine whether a patient will be heading toward wasting syndrome.
AIDS wasting syndrome / HIV wasting syndrome
HIV wasting syndrome has been defined by the Centers for Disease Control and Prevention (CDC) an AIDS-defining condition, an involuntary weight loss greater than 10% of baseline weight associated with either chronic diarrhea for at least 30 days or chronic weakness or documented fever for at least 30 days in the absence of a concurrent illness or condition other than HIV infection that could explain findings (e.g., tuberculosis, cryptosporidiosis, or other specific enteritis) 1. Because HIV-associated wasting and weight loss can occur without diarrhea, fever, or weakness—it may be argued that unintentional weight loss in the absence of fever or diarrhea is more troubling—other definitions of wasting in HIV have been crafted 2. The CDC definition of HIV-associated wasting further assumed that baseline weight, which may have been reported and not measured, represented the patient’s usual or ideal weight. This premise is challenged when considering that HIV-infected patients are seen at varying stages of HIV infection and that “baseline” values may be less meaningful. Additionally, the CDC definition does not take into account the rate of weight loss, which may provide valuable information for the assessment of the need for intervention.
Because of these concerns, 3 definitions for wasting or weight loss of concern were used in the the Nutrition for Healthy Living (NFHL) study: (1) unintentional loss of >10% body weight since study entry, (2) a body mass index (BMI; calculated as weight in kilograms divided by the square of height in meters) decreasing to <20, or (3) unintentional loss of >5% body weight in 6 months (between 2 study visits) that persisted for at least 1 year 3. These definitions attempted to include significant weight loss (>10%), weight loss that was progressive and advanced (BMI, <20), and a rapid rate of weight loss (>5% in 6 months). These definitions may better capture medically important weight loss and provide clinical reference points. Other investigators have attempted to provide cutoff points for lean body mass (LBM) that correlate to wasting parameters, but there are fewer data to support this definition, so it was not used in the Nutrition for Healthy Living study. It is important to clarify terms that have been used in the literature of HIV-associated wasting and weight loss. “Cachexia” describes a preferential loss of lean body mass, which implies metabolic derangement rather than a nutrient deficiency 4. “Wasting” is a less precise term that suggests weight loss due to inadequate nutrient intake 5. The term has also been used for severe weight loss, but the exact point at which progressive weight loss becomes wasting is problematic. Because of the increasing mean BMI in the HIV-infected population, the Nutrition for Healthy Living study used a BMI of <20, even though this BMI is on the low side of normal. Whatever the initial BMI may be, unintentional weight loss may be of concern if it is rapid or substantial, even if the BMI remains within the normal range. The cutoff point for wasting is arbitrary.
During the highly active antiretroviral therapy (HAART) era, HIV infection has become a chronic, manageable disease 2. Nutrition-related complications remain a challenging issue for HIV-infected patients and for those involved in their care. Involuntary weight loss is associated with disease progression and death, even where access to HAART is not limited 6. HIV-associated weight loss and wasting were among the most frequently occurring AIDS-defining conditions during the pre-HAART era, but the expectation was that viral control with therapy and prophylaxis for opportunistic infections would eliminate nutritional concerns in HIV-infected individuals 7.
Although the wasting syndrome has declined since the introduction of highly active antiretroviral therapy (HAART) 8, weight loss still remains a common cause of morbidity and mortality in HIV-infected patients receiving HAART 9.
The pathophysiological mechanisms underlying the HIV wasting syndrome are related to three major factors including inadequate nutrient intake, nutrient malabsorption, and disturbances in metabolism 10.
Figure 1. HIV wasting syndrome

Footnote: A 32-year-old HIV-1-infected Nigerian woman was admitted to a tertiary hospital with a 6-month history of progressive lethargy, anorexia, recurrent fever, vomiting, watery non-bloody diarrhoea, and progressive weight loss. She went from 50 kg to 21 kg in 5 months, a 42% weight loss. She was unemployed and had no source of regular income to care for herself or her 3 children. Hence, her meals before and during her illness were irregular and consisted mainly of carbohydrate diet.
On examination, she was conscious, prostrated, severely wasted with generalised wasting of muscle groups, loss of subcutaneous fat, and prominence of bones. There was no evidence of localised subcutaneous fat atrophy or fat redistribution. Her body mass index was 10.2 kg/m², and the mid-upper arm circumference was 10 cm. She had hypoproteinemic hair and skin changes, dehydration, fever (37.8°C), pallor, and oropharyngeal candidiasis but no lymphadenopathy. Chest, cardiovascular, and abdominal examinations were normal.
She was rehydrated, and diarrhoea was controlled with an antimotility agent (tablets loperamide) after empiric treatment for infectious diarrhoea using tablets albendazole 400 mg daily for 3 days, intravenous ciprofloxacin 500 mg twice daily for one week, and tablets tinidazole 2 g start. Oral fluconazole 200 mg daily for oral thrush, prohylactic septrin 960 mg daily, multivitamins, and haematinics were also given.
She had intensive nutritional rehabilitation with locally available high protein and high energy diet as well as fruits and vegetables. Specifically, “kwashiokor pap” or “kwashi pap”, a high protein local diet made up of a mixture of ground guinea corn, ground soya bean, and ground crayfish, ground dried fish, roasted ground groundnuts, and boiled water was given orally three to five times per day, along with variety of other local foods.
Additional adherence counselling was given, and ART was switched to Emtricitabine/Tenofovir and Nevirapine on account of anaemia.
All symptoms gradually resolved and she gradually regained her physical strength with improved physical activity. At the end of 6 weeks, her weight increased by about 8 kg and she was thereafter discharged to the social welfare, nutritional, and adherence counselling unit.
[Source 11 ]HIV wasting syndrome causes
The cause of HIV-associated wasting syndreome is multifactorial, and causes may include socioeconomic status, access to care, cultural practices, psychological factors, and medical complications of and therapies for HIV infection, which can be categorized these into 2 main categories: decreased nutrient intake and altered nutrient metabolism.
Inadequate nutrient intake
- Oral and upper gastrointestinal
- Anorexia
- Psyshosocial-economic
- Malabsorption
Altered nutrient metabolism
- Uncontrolled HIV infection
- Metabolic demands of HAART
- Opportunistic infections or malignancies (AIDS defining conditions)
- Hormonal deficiencies (testosterone or thyroid)
- Cytokine dysregulation
Hypogonadism, represented by low levels androgen such as testosterone, may accompany HIV infection in men 12, and it may be as a result of the suppressive effects of cytokines on testicular steroidogenesis, as well as due to functional disorder of the hypothalamus and/or primary testicular failure 13. Androgen deficiency inhibits protein synthesis and this may favour a greater loss of muscle mass relative to fat mass in men. In women, testosterone levels are normally low and although androgen deficiency has been reported in some women with weight loss, their contribution to weight loss in women is less understood 14.
Abnormalities in Nutrient Intake
Dietary intake
The diet of patients with HIV infection has evolved with changes in their health status. Dietary studies in HIV infection have provided conflicting results regarding the relationship between disease state and nutritional intake. To clarify some of those issues, 3-day food records of 516 participants from the Nutrition for Healthy Living cohort were analyzed stratified by CD4+ cell-count categories (<200, 200–499, and >500 cells/mm³) 15). BMI and weight were significantly lower in the low CD4+ cell count stratum than in the high CD4+ cell count stratum. In the high CD4+ cell count stratum, BMI and weight did not differ from those of the general population 16. Men in the lowest CD4+ cell count stratum required the highest caloric intake (in kilocalories per kilogram of body weight) to maintain a lower BMI. However, the energy intake per day (in kilocalories per day) did not significantly differ from National Health and Nutrition Examination Survey III data for the same age and sex groups in any CD4+ cell count stratum. Women in the Nutrition for Healthy Living cohort seemed to be particularly vulnerable to inadequate dietary intake, which may be explained by their lower socioeconomic status and the large proportion who were former or current intravenous drug users. White men had a significantly higher energy intake than did nonwhite men; white and nonwhite women had comparable energy intakes. The study determined that the intake of micronutrients was also higher at decreased CD4+ cell counts. Many participants, particularly women, consumed amounts of micronutrients that were less than the dietary reference intakes, despite adequate median intake of micronutrients. More than 25% of woman had inadequate dietary intake of vitamins A, C, E, and B6.
Relationship between gastrointestinal symptoms and acute weight loss. According to data derived from phone contacts in between formal study visits, 24% of Nutrition for Healthy Living participants described at least 1 episode of acute weight loss (⩾5% of weight) 17. Episodes of acute weight loss were associated with oral symptoms and difficulty swallowing but not with anorexia. Among participants without diarrhea, the use of HAART protected against weight loss. Among those with diarrhea, HAART was not associated with weight loss, which suggests that HAART itself may be associated with diarrhea. Even in the absence of opportunistic infections, many patients with HIV infection may have HIV- or therapy-related reasons to have gastrointestinal symptoms, which may predispose them to weight loss.
Malabsorption and gastrointestinal dysfunction
The severe opportunistic diarrheal illnesses that contributed to HIV-associated wasting in the early days of the epidemic have rarely been seen since the beginning of the HAART era. However, gastrointestinal dysfunction may still play a role in weight loss during HIV infection. A striking 88% of the Nutrition for Healthy Living cohort had at least 1 abnormality in gastrointestinal function 18; 47.7% of participants had abnormal D-xylose absorption, which may serve as a surrogate marker of intestinal absorption, and 38.9% reported at least 1 episode of diarrhea within the preceding month. Significantly more men then women had diarrhea. Fat malabsorption was observed in 12.8% of subjects. However, there was no association of diarrhea with any measure of absorption, which suggests that the diarrhea is not primarily caused by malabsorption. These analyses suggest the continued frequency of gastrointestinal dysfunction.
Correlates of reduced intake
Groups at risk for adverse clinical outcomes are likely to have reduced dietary intakes. In a cross-sectional analysis of 633 Nutrition for Healthy Living participants, it was found that, as illness progressed, men “engaged in compensatory eating behaviors,” whereas women did not 19. When rates were adjusted for dieting, 38.4% of women reported inadequate caloric intake. The absence of a caregiver and the use of injection drugs correlated with a lower protein intake in men. This analysis further showed that the inability to meet recommended dietary allowances was largely the result of socioeconomic rather than clinical factors. Approximately 11.3% of participants had inadequate protein intake. A striking 36.1% of participants were classified as “food insecure” (defined as being unsure where meals in the subsequent 3 days will be obtained). Nearly 8% of the cohort classified themselves as hungry—that is, having insufficient access to intake to satisfy hunger. Analysis therefore concluded that, in HIV disease, “dietary intake reflects the confluence of attitudinal, economic, and lifestyle factors” 20.
Altered Metabolism
Relationship between HIV load and body weight. The precise relationship between the level of or changes in viral load and nutritional status in HIV infection has been unclear. In 38 Nutrition for Healthy Living participants who were receiving their first protease inhibitor therapy, those who achieved a decrease in viral load had a significantly greater weight gain per month than did those whose viral load did not decrease 21. The association between changes in viral load and HIV-associated weight loss was examined in 318 Nutrition for Healthy Living participants with 1886 study visits 22. It was found that, for participants who were not receiving HAART, each log10 increase in HIV RNA load resulted in a 0.92-kg decrease in body weight. Change in weight was independent of the viral load. The relationship between viral load and weight did not hold in participants receiving a stable HAART regimen; a 0.35-kg decrease in body weight was seen with every 100-cell/mm3 decrease in CD4+ cell count. For those individuals who stopped or started receiving HAART, changes in viral load were inversely associated with changes in weight. Changes in both viral load and severity of disease (as measured by CD4+ cell counts) contribute to changes in weight.
Increased resting energy expenditure
In a study to determine the effect of viral load and HAART use on resting energy expenditure, 372 Nutrition for Healthy Living participants were found to have a 90-kJ/day increase in resting energy expenditure per 1-log10 copy/mL increase in HIV RNA load and a 339-kJ/day higher resting energy expenditure if they were receiving HAART, compared with those who were not receiving HAART 23. These results suggest that HIV load and HAART have independent effects on resting energy expenditure and that HAART itself may increase resting energy expenditure. This finding was later confirmed in patients who developed lipodystrophy 24. Higher metabolic rates may partially account for the continued weight loss and wasting observed in HIV infection during the HAART era and may be associated with the metabolic and body-shape abnormalities seen during the present era 25.
Role of AIDS defining conditions
It was long assumed that weight loss in HIV-infected patients was directly associated with episodes of opportunistic infections or malignancies 26. A longitudinal analysis of 669 Nutrition for Healthy Living participants suggested that the increased energy requirements of AIDS defining conditions contribute in a small way to weight loss 27. Having had a diagnosis of 1 historical ADC in the past did not predict wasting-related outcomes, but having had >1 historical ADC predicted a 30% increase in developing a BMI of <20. The risk of a 10% weight loss increased 20% with each additional historical AIDS defining condition. If an AIDS defining condition occurred in the 6 months preceding a study visit, the risk of weight loss increased to 2.5–8.0 fold. No difference was detected in individuals who met the definition of wasting among those whose conditions progressed to AIDS on the basis of the ADC definition, compared with those whose conditions progressed on the basis of the definition of a CD4+ cell count of >200 cells/mm3. During the HAART era, AIDS defining conditions were increasingly rare among Nutrition for Healthy Living participants and were associated with a relatively small risk of developing weight loss or wasting; thus, we are not able to explain the majority of the weight loss seen at present in HIV-infected individuals.
Inflammatory cytokines and wasting
Disturbances in the production of inflammatory cytokines have been postulated to influence HIV-associated weight loss. A study of 172 men in the Nutrition for Healthy Living cohort assessed how catabolic cytokines and testosterone affect lean body mass 28. This analysis found that TNF-α and IL-1β from stimulated peripheral blood mononuclear cells independently predicted loss of lean body mass and changes in resting energy expenditure but that the level of free testosterone did not. In the present study, catabolic cytokines—not decreased dietary intake or hypogonadism—resulted in a loss of lean body mass. In a smaller group of 24 Nutrition for Healthy Living participants, cytokines produced by stimulated peripheral blood mononuclear cells were more associated with nutritional and metabolic abnormalities than were plasma cytokines 28. IL-1β, IL-6, and TNF-α levels in PBMCs were best able to discriminate between participants with and without HIV-associated wasting according to the CDC definition. IL-6 and TNF-α from plasma were increased in participants with wasting, but these could not reliably distinguish between participants with and without wasting.
HIV wasting syndrome treatment
Both micronutrient and macronutrient malabsorption have been observed in the wasting syndrome, and nutrient malabsorption may occur with or without diarrhoea 29. Chronic diarrhoea leading to malabsorption may either be due to the HIV virus itself (i.e., AIDS enteropathy) or due to occult opportunistic infections (e.g., Cytomegalovirus, Clostridium difficile, and Mycobacterium avium intracellular bacteria, among others) 30. In AIDS enteropathy, no specific pathogen can be isolated from the gut, and the chronic diarrhoea, motility disturbances, and mucosal atrophy accompanying this condition have been attributed to the direct effects of HIV, especially as viral proteins have been found in the gut mucosa 31. AIDS enteropathy is a diagnosis of exclusion; however, complete exclusion of all opportunistic causes of diarrhoea in HIV-infected patients is a challenging task sometimes requiring invasive techniques 32. Consequently, the WHO recommends the use of empiric antimicrobials and constipating drugs such as loperamide, for treatment of chronic HIV-related diarrhoea in resource poor settings 33.
Intensive nutritional rehabilitation to prevent or reverse weight loss remains the cornerstone of management of the wasting syndrome 29. The aims are to improve appetite and nutrient absorption by addressing all immediate causes of anorexia and malabsorption, such as oral sores and diarrhoea, to improve intake of adequate calories made up of high-protein and low-fat meals in addition to micronutrients supplementation, and to correct psychosocial issues that affect nutrient intake such as poverty and depression, by providing social and psychological support. In view of the principal role of HIV in the pathogenesis of the wasting syndrome, effective HAART aimed at reducing viral load to undetectable levels and sustaining immune restoration as reflected in improving CD4 cell count is indispensable 34.
In combination with adequate caloric intake, fitness training by progressive resistance exercises (e.g., lift of light weights and body building exercises) increases muscle function and strength, as well as lean body mass and weight 35. Conversely, aerobic exercises (e.g., walking, jogging, and running) may result in little or no increase in body mass or weight.
Pharmacological treatments are usually reserved for patients who fail nutritional therapy. Appetite stimulants (e.g., Megestrol acetate), recombinant human growth hormone (Serostim), and androgenic steroids (e.g., testosterone) in men with hypogonadism have all been approved for the treatment of the wasting syndrome 34. Cytokine modulators (such as thalidomide) have been investigated for treatment of wasting syndrome, but their success rates have been variable 34. Thus, they are not yet approved for the management of the wasting syndrome, until convincing evidence of their efficacy is established in future studies.
Cerebral salt wasting syndrome
Cerebral salt-wasting syndrome is defined by the development of extracellular volume depletion due to a kidney sodium transport abnormality in patients with intracranial disease and normal adrenal and thyroid function 36. As such, cerebral salt-wasting syndrome may be more appropriately termed renal salt wasting syndrome. Complications of cerebral salt-wasting syndrome include symptomatic hyponatremia and dehydration 37.
A study by Kalita et al. 38 suggested that cerebral salt wasting is the most frequent cause of stroke-related hyponatremia. The study, of 100 patients with stroke, including 47% with ischemic stroke and 53% with intracerebral hemorrhage, found that 43% of the stroke patients had hyponatremia. Of these, 19 (44.2%) had cerebral salt wasting, while 3 (7.0%) had syndrome of inappropriate antidiuretic hormone secretion (SIADH), 14 (32.6%) had miscellaneous causes of hyponatremia, and 7 (16.3%) had indeterminate causes of the condition. The investigators 38 also found that length of hospital stay independently predicted the development of cerebral salt wasting and hyponatremia.
A study by Misra et al. 39 suggested that in patients with tuberculous meningitis, hypovolemia associated with cerebral salt wasting may play a role in the occurrence of stroke. The report included 81 individuals with tuberculous meningitis, 39.5% of whom suffered ischemic stroke; 50% of these stroke patients had cerebral salt wasting.
Differentiation of cerebral salt-wasting syndrome from the syndrome of inappropriate antidiuretic hormone secretion (SIADH), a common cause of hyponatremia, can be difficult because both can present with hyponatremia and concentrated urine with natriuresis 37. However, distinguishing between the 2 disorders is important because treatment options differ. Failure to distinguish cerebral salt-wasting syndrome from SIADH in a patient with hyponatremia who has brain injury could lead to inappropriate therapy with fluid restriction.
The exact incidence of renal salt-wasting syndrome without cerebral disease is also unknown. Cerebral salt-wasting syndrome can occur at any age. Published reports include patients aged 6 months to 65 years. Exact incidence data for cerebral salt-wasting syndrome are not available. Approximately 60% of children with brain injuries or tumors develop hyponatremia during their hospital course. Some experts suggest that cerebral salt-wasting syndrome (renal salt wasting) is responsible for hyponatremia at least as often as syndrome of inappropriate antidiuretic hormone secretion (SIADH) is, particularly in neurosurgical patients. Other studies indicate that this syndrome explains the development of hyponatremia in no more than 6% of patients with acute brain injuries 40. A literature review by Leonard et al found the incidence of cerebral salt-wasting syndrome reported in traumatic brain injury to vary between 0.8-34.6%, with the studies determining these incidences differing with respect to the populations evaluated and the definitions used for hyponatremia and cerebral salt wasting syndrome 41.
Although the diagnosis of cerebral salt-wasting syndrome is thought to be controversial by some 42, it should be considered a discrete clinical entity and may be more common than perceived 43. It should also be considered in patients without cerebral disease 42. Possible mechanisms for cerebral salt-wasting syndrome are shown in the chart below.
Figure 2. Cerebral salt-wasting syndrome
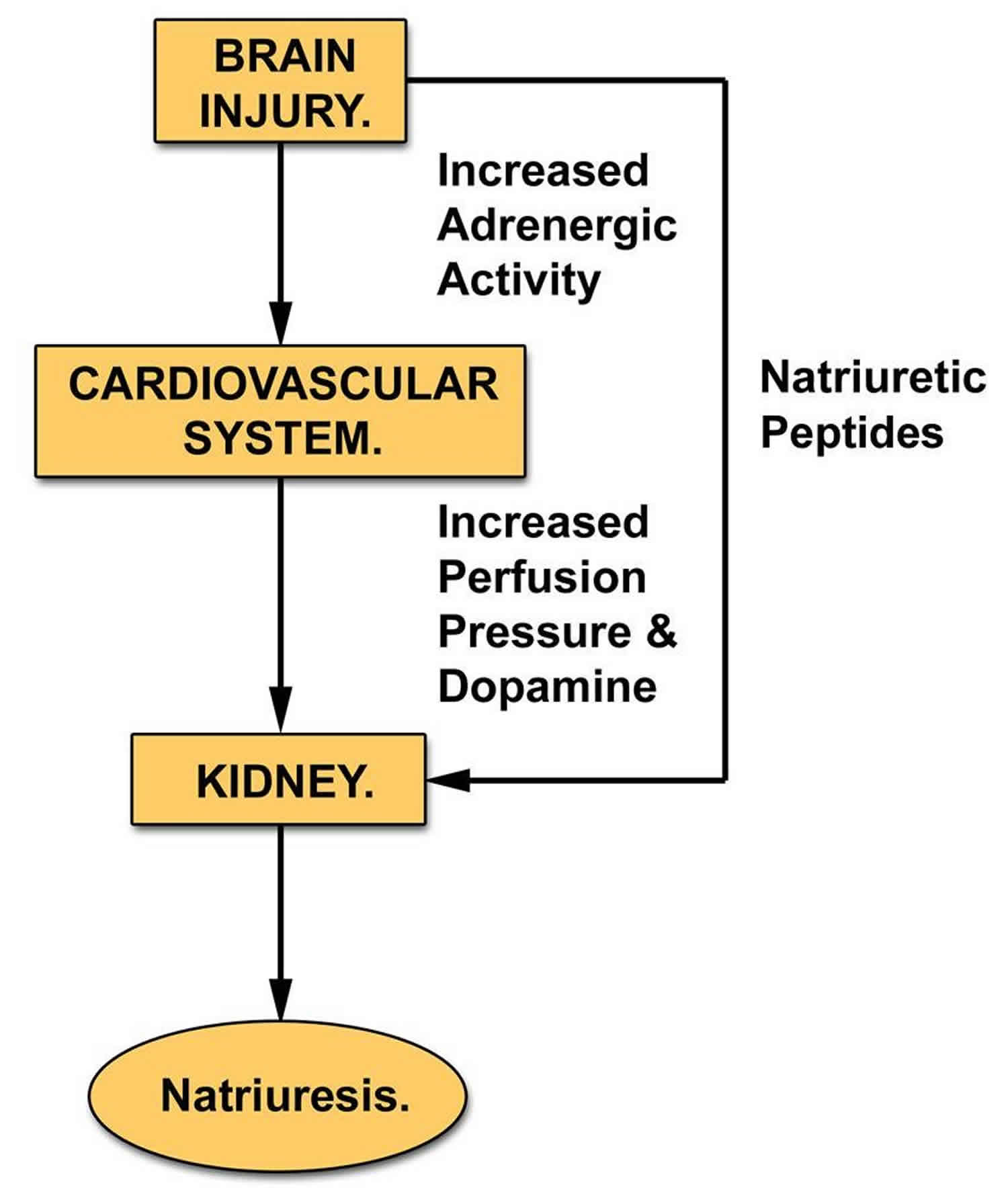
Footnote: Possible mechanisms for cerebral salt-wasting syndrome. The injured brain may release natriuretic proteins that act directly on the kidney. In addition, cerebral injury may increase sympathetic nervous system activity, elevating renal perfusion pressure and releasing dopamine.
[Source 37 ]Cerebral salt-wasting syndrome or renal salt wasting syndrome, may be more common than syndrome of inappropriate antidiuretic hormone secretion (SIADH) and may even occur in the absence of cerebral disease 43. Although the exact mechanism that underlies the development of cerebral salt-wasting syndrome is unclear, it is known that the initiating defect in renal sodium transport leads to extracellular volume depletion and that a cascade of compensatory changes occurs.
Abnormalities in the proximal tubule result in excessive sodium losses, which lead to decreased effective circulating volume. This activates baroreceptors, which increase antidiuretic hormone (ADH) secretion. This results in water conservation and a return to an equilibrated state. In contrast, SIADH primarily occurs due to an inappropriate euvolemic rise in ADH secretion.
The relationship among serum urate, fractional excretion of urate, and hyponatremia in cerebral salt-wasting syndrome is unclear. Fractional excretion of urate may remain elevated even after correction of hyponatremia in patients with cerebral salt-wasting syndrome. This is distinct from SIADH, in which the fractional excretion of urate returns to the reference range once the hyponatremia is corrected 44. The physiologic basis for this in cerebral salt-wasting syndrome may be related to the receptor-mediated processing of sodium and urate in the proximal tubule, which may be defective in this syndrome. The physiologic basis for hypouricemia in SIADH remains unclear.
The abnormalities in proximal tubular transport may be secondary to a plasma natriuretic factor that reduces proximal and, possibly, distal sodium transport in cerebral salt-wasting syndrome. It may also inhibit the tubular transport of urate, phosphate, and urea in addition to sodium 45.
Cerebral salt-wasting syndrome causes
The cause of cerebral salt wasting is not completely understood. Cerebral salt wasting is most commonly seen after a central nervous system (CNS) insult or disease 46. Conditions leading to cerebral salt-wasting syndrome include the following 37:
- Head injury
- Brain tumor
- Intracranial surgery
- Stroke
- Intracerebral hemorrhage 47
- Tuberculous meningitis
- Craniosynostosis repair
The most commonly described precipitating insult is aneurysmal subarachnoid hemorrhage 46. Why cerebral salt wasting syndrome occurs more frequently after aneurysmal subarachnoid hemorrhage versus traumatic subarachnoid hemorrhage or other CNS insult is not well defined 46. Why cerebral salt wasting syndrome is uncommon after other injuries or diseases is also not well defined 46.
Cerebral salt-wasting syndrome can also occur in the absence of cerebral disease 48.
The exact mechanism underlying cerebral salt-wasting syndrome remains unclear. In the setting of cerebral injury, one hypothesis is that an exaggerated renal pressure–natriuresis response caused by increased activity of the sympathetic nervous system and dopamine release is responsible for urinary sodium loss.
Another hypothesis involves the release of natriuretic factors, possibly including brain natriuretic peptide (C-type natriuretic peptide) or urodilatin by the injured brain. Kojima et al. 49 have described an animal model of cerebral salt-wasting syndrome that may allow better clarification of the cerebral salt-wasting syndrome cause.
Cerebral salt-wasting syndrome symptoms
The most common presenting story for cerebral salt wasting is hyponatremia after aneurysmal subarachnoid hemorrhage 50. As the decline in serum sodium concentration reduces serum osmolality, a tonicity gradient develops across the blood-brain barrier that causes cerebral edema. Symptoms include lethargy, agitation, headache, altered consciousness, seizures, and coma 51.
The severity of symptoms typically reflects the magnitude and rapidity of the decrease in serum sodium concentration.
Intravascular volume depletion
Historical features suggesting hypovolemia include thirst, abrupt weight loss, decreasing urinary frequency, and negative fluid balance.
Physical signs of cerebral salt-wasting syndrome (renal salt wasting) include those associated with severe hyponatremia or intravascular volume depletion.
Hyponatremia can be indicated by acute CNS dysfunction such as altered mental status, seizures, and coma.
The differentiation of SIADH from cerebral salt-wasting syndrome depends on an accurate estimation of extracellular volume. Unfortunately, no single physical finding can accurately and reproducibly measure effective circulating volume. Commonly used signs of hypovolemia include orthostatic tachycardia or hypotension, increased capillary refill time, increased skin turgor, dry mucous membranes, and a sunken anterior fontanel. These signs usually appear only when the degree of dehydration is moderate to severe. Central venous pressure may be an unreliable determinant of extracellular volume.
Cerebral salt-wasting syndrome diagnosis
Failure to distinguish cerebral salt-wasting syndrome (renal salt wasting) from SIADH as the cause of hyponatremia may lead to improper therapy (ie, fluid restriction), thereby exacerbating intravascular volume depletion and potentially jeopardizing cerebral perfusion.
The following lab studies may be indicated in patients with cerebral salt-wasting syndrome:
- Serum sodium concentration – Patients with untreated cerebral salt-wasting syndrome are often hyponatremic
- Serum osmolality – If measured serum osmolality exceeds twice the serum sodium concentration and azotemia is not present, suspect hyperglycemia or mannitol as the cause of hyponatremia
- Urinary output – Urine is relatively dilute and the flow rate is often high in cerebral salt-wasting syndrome; urine is usually very concentrated and the flow rate is low in SIADH
Urinary sodium concentrations
Urinary sodium concentrations are typically elevated in SIADH and in cerebral salt-wasting syndrome (>40 mEq/L). However, urinary sodium excretion (urinary sodium concentration [mEq/L] x urinary volume [L/24 h]) is substantially higher than sodium intake in cerebral salt-wasting syndrome but generally equals sodium intake in SIADH. Therefore, net sodium balance (intake minus output) is negative in cerebral salt-wasting syndrome.
Urinary sodium excretion and urinary volume
A retrospective study by Arieff et al indicated that in patients with cerebral lesions who exhibit hyponatremia, urinary sodium excretion and urinary volume can be used to differentiate cerebral salt-wasting syndrome from SIADH. In patients with cerebral salt-wasting syndrome, these values were 394 ± 369 mmol/24 h and 2603 ± 996 mL/24 h, respectively. In comparison, the values were significantly lower—51 ± 25 mmol/24 h and 745 ± 298 mL/24 h, respectively—in patients with SIADH 52.
Cerebral salt-wasting syndrome and central diabetes insipidus
A retrospective study by Wu et al. 53 found that distinctive features of combined central diabetes insipidus and cerebral salt-wasting syndrome following traumatic brain injury include massive polyuria (the most typical presentation) that responds to vasopressin plus cortisone acetate but not to vasopressin alone, low central venous pressure, a high level of brain natriuretic peptide precursor in the absence of cardiac dysfunction, high 24-hour urine sodium excretion and hypovolemia, and a much greater osmolarity for urine than for serum 53.
Fractional Excretion of Uric Acid and Phosphate
Uric acid
Fractional excretion of uric acid (FEUA) is defined as the percentage of urate filtered by glomeruli that is excreted in urine. It is calculated by dividing the product of (urinary uric acid [mg/mL] x serum creatinine [mg/mL]) by the product of (serum uric acid [mg/mL] x urinary creatinine [mg/mL]) and multiplying the result by 100%. Normal values are less than 10%.
Patients with either cerebral salt-wasting syndrome or SIADH can have hypouricemia and elevated FEUA. However, after correction of hyponatremia, hypouricemia and elevated FEUA may normalize in SIADH but persist in cerebral salt-wasting syndrome (renal salt wasting) 43.
Phosphate
Fractional excretion of phosphate (FEP) should be determined when evaluating patients with hyponatremia and hypouricemia. Elevated fractional excretion of phosphate suggests cerebral salt-wasting syndrome as opposed to SIADH 44.
Cerebral salt-wasting syndrome treatment
Evaluation and treatment of cerebral salt-wasting syndrome or renal salt wasting syndrome, typically occurs in the inpatient setting because most patients are seriously ill with acute CNS disease.
Management centers on correction of intravascular volume depletion and hyponatremia, as well as on replacement of ongoing urinary sodium loss, usually with intravenous (IV) hypertonic saline solutions 54. Some clinicians have reported a favorable response to mineralocorticoid therapy in cerebral salt-wasting syndrome. Mineralocorticoids, such as fludrocortisone, promote increased sodium reabsorption, as well as potassium loss, from the renal distal tubules. Once the patient is stabilized, enteral salt supplementation can be considered.
Ongoing monitoring of body weight, fluid balance, and serum sodium concentration is essential during the hospital course.
Long-term monitoring
Patients whose neurologic insult has improved and who demonstrate normal intravascular volume and serum sodium concentrations on enteral salt supplements, fludrocortisone, or both can be closely observed on an outpatient basis until cerebral salt-wasting syndrome resolves.
Cerebral salt-wasting syndrome prognosis
Cerebral salt-wasting syndrome usually develops in the first week following a brain insult. Its duration is usually brief (spontaneously resolves in 2-4 weeks), although it can last for several months. Death and complication rates for cerebral salt-wasting syndrome are not available 37.
- 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992 Dec 18; 41(RR-17):1-19.[↩][↩]
- A. Mangili, D. H. Murman, A. M. Zampini, C. A. Wanke, Kenneth H. Mayer, Nutrition and HIV Infection: Review of Weight Loss and Wasting in the Era of Highly Active Antiretroviral Therapy from the Nutrition for Healthy Living Cohort, Clinical Infectious Diseases, Volume 42, Issue 6, 15 March 2006, Pages 836–842, https://doi.org/10.1086/500398[↩][↩]
- Wanke CA, Silva M, Knox TA, Forrester J, Speigelman D, Gorbach SL. Weight loss and wasting remain common complications in individuals infected with human immunodeficiency virus in the era of highly active antiretroviral therapy, Clin Infect Dis , 2000, vol. 31, pg. 803-4[↩]
- Nelson KA, Walsh D, Sheehan FA. The cancer anorexia-cachexia syndrome, J Clin Oncol , 1994, vol. 12, pg. 213-25[↩]
- Kotler D. Challenges to diagnosis of HIV-associated wasting, J Acquir Immune Defic Syndr , 2004, vol. 37, pg. S280-3[↩]
- Tang AM, Forrester J, Spiegelman D, Knox TA, Tchetgen E, Gorbach SL. Weight loss and survival in HIV-positive patients in the era of highly active antiretroviral therapy, J Acquir Immune Defic Syndr , 2002, vol. 31, pg. 230-6[↩]
- Jones JL, Hanson DL, Dworkin MS, et al. Surveillance for AIDS-defining opportunistic illnesses, 1992–1997, MMWR CDC Surveill Summ , 1999, vol. 48, pg. 1-22[↩]
- Smit E, Skolasky RL, Dobs AS, et al. Changes in the incidence and predictors of wasting syndrome related to human immunodeficiency virus infection, 1987–1999. American Journal of Epidemiology. 2002;156(3):211–218.[↩]
- Wanke CA, Silva M, Knox TA, Forrester J, Speigelman D, Gorbach SL. Weight loss and wasting remain common complications in individuals infected with human immunodeficiency virus in the era of highly active antiretroviral therapy. Clinical Infectious Diseases. 2000;31(3):803–805.[↩]
- Mangili A, Murman DH, Zampini AM, Wanke CA. Nutrition and HIV infection: review of weight loss and wasting in the era of highly active antiretroviral therapy from the nutrition for healthy living cohort. Clinical Infectious Diseases. 2006;42(6):836–842. https://www.ncbi.nlm.nih.gov/pubmed/16477562[↩]
- Ogoina D, Obiako RO, Muktar HM. HIV Wasting Syndrome in a Nigerian Failing Antiretroviral Therapy: A Case Report and Review of the Literature. Case Rep Med. 2010;2010:192060. doi:10.1155/2010/192060 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3014846[↩]
- Bhasin S, Storer TW, Javanbakht M, et al. Testosterone replacement and resistance exercise in HIV-infected men with weight loss and low testosterone levels. Journal of the American Medical Association. 2000;283(6):763–770.[↩]
- Grinspoon S. Mechanisms and treatment of androgen deficiency in HIV disease. Current Opinion in Endocrinology and Diabetes. 2000;7(6):332–336[↩]
- Grinspoon S, Corcoran C, Miller K, et al. Body composition and endocrine function in women with acquired immunodeficiency syndrome wasting. Journal of Clinical Endocrinology and Metabolism. 1997;82(5):1332–1337[↩]
- Woods MN, Spiegelman D, Knox TA, et al. Nutrient intake and body weight in a large HIV cohort that includes women and minorities, J Am Diet Assoc , 2002, vol. 102 (pg. 203-11[↩]
- US Department of Health and Human Services, National Center for Health StatisticsThird National Health and Nutrition Examination Survey, 1988–1994, NHANES III laboratory data file , 1996Hyattsville, MDCenters for Disease Control and Prevention[↩]
- Jacobson DL, Bica I, Knox TA, et al. Difficulty swallowing and lack of receipt of highly active antiretroviral therapy predict acute weight loss in human immunodeficiency virus disease, Clin Infect Dis , 2003, vol. 37, pg. 1349-56[↩]
- Knox TA, Spiegelman D, Skinner SC, Gorbach S. Diarrhea and abnormalities of gastrointestinal function in a cohort of men and women with HIV infection, Am J Gastroenterol , 2000, vol. 95, pg. 3482-9[↩]
- Kim JH, Spiegelman D, Rimm E, Gorbach SL. The correlates of dietary intake among HIV-positive adults, Am J Clin Nutr , 2001, vol. 74, pg. 852-61[↩]
- Kim JH, Spiegelman D, Rimm E, Gorbach SL. The correlates of dietary intake among HIV-positive adults, Am J Clin Nutr , 2001, vol. 74, pg. 860[↩]
- Silva M, Skolnik PR, Gorbach SL, et al. The effect of protease inhibitors on weight and body composition in HIV-infected patients, AIDS , 1998, vol. 12, pg. 1645-51[↩]
- Mwamburi DM, Wilson IB, Jacobson DL, et al. Understanding the role of HIV load in determining weight change in the era of highly active antiretroviral therapy, Clin Infect Dis , 2005, vol. 40, pg. 167-73[↩]
- Roubenoff R, Grinspoon S, Skolnik PR, et al. Role of cytokines and testosterone in regulating lean body mass and resting energy expenditure in HIV-infected men, Am J Physiol Endocrinol Metab , 2002, vol. 283, pg. E138-45[↩]
- Kosmiski L, Kuritzkes D, Hamilton J, et al. Fat distribution is altered in HIV-infected men without clinical evidence of the HIV lipodystrophy syndrome, HIV Med , 2003, vol. 4, pg. 235-40[↩]
- Dong KR, Hendricks KM. The role of nutrition in fat deposition and fat atrophy in patients with HIV, Nutr Clin Care , 2005, vol. 8, pg. 31-6[↩]
- Macallan DC. Wasting in HIV infection and AIDS, J Nutr , 1999, vol. 129 1 Suppl, pg. 238-42[↩]
- Wanke CA, Silva M, Ganda A, et al. Role of acquired immune deficiency syndrome-defining conditions in human immunodeficiency virus-associated wasting, Clin Infect Dis , 2003, vol. 37 Suppl 2, pg. S81-4[↩]
- Abad LW, Schmitz HR, Parker R, Roubenoff R. Cytokine responses differ by compartment and wasting status in patients with HIV infection and healthy controls, Cytokine , 2002, vol. 18, pg. 286-93[↩][↩]
- Mangili A, Murman DH, Zampini AM, Wanke CA. Nutrition and HIV infection: review of weight loss and wasting in the era of highly active antiretroviral therapy from the nutrition for healthy living cohort. Clinical Infectious Diseases. 2006;42(6):836–842.[↩][↩]
- HIV-Associated Wasting. http://hivinsite.ucsf.edu/InSite?page=kb-04-01-08[↩]
- Ullrich R, Zeitz M, Heise W, L’age M, Hoffken G, Riecken EO. Small intestinal structure and function in patients infected with human immunodeficiency virus (HIV): evidence for HIV-induced enteropathy. Annals of Internal Medicine. 1989;111(1):15–21[↩]
- Cello JP, Day LW. Idiopathic AIDS enteropathy and treatment of gastrointestinal opportunistic pathogens. Gastroenterology. 2009;136(6):1952–1965[↩]
- World health organisation. Guidelines for the clinical management of HIV infection in adults. 1991. Dec[↩]
- Polsky B, Kotler D, Steinhart C. Treatment guidelines for HIV-associated wasting. HIV Clinical Trials. 2004;5(1):50–61[↩][↩][↩]
- Spence DW, Galantino MLA, Mossberg KA, Zimmerman SO. Progressive resistance exercise: effect on muscle function and anthropometry of a select AIDS population. Archives of Physical Medicine and Rehabilitation. 1990;71(9):644–648[↩]
- Peters JP, Welt LG, Sims EA, et al. A salt-wasting syndrome associated with cerebral disease. Trans Assoc Am Physicians. 1950. 63:57-64.[↩]
- Cerebral salt-wasting syndrome. https://emedicine.medscape.com/article/919609-overview[↩][↩][↩][↩][↩]
- Kalita J, Singh RK, Misra UK. Cerebral Salt Wasting Is the Most Common Cause of Hyponatremia in Stroke. J Stroke Cerebrovasc Dis. 2017 Jan 16.[↩][↩]
- Misra UK, Kalita J, Kumar M, Neyaz Z. Hypovolemia due to cerebral salt wasting may contribute to stroke in tuberculous meningitis. QJM. 2018 Apr 9.[↩]
- Rivkees SA. Differentiating appropriate antidiuretic hormone secretion, inappropriate antidiuretic hormone secretion and cerebral salt wasting: the common, uncommon, and misnamed. Curr Opin Pediatr. 2008 Aug. 20(4):448-52.[↩]
- Leonard J, Garrett RE, Salottolo K, et al. Cerebral salt wasting after traumatic brain injury: a review of the literature. Scand J Trauma Resusc Emerg Med. 2015 Nov 11. 23:98.[↩]
- Bettinelli A, Longoni L, Tammaro F, Fare PB, Garzoni L, Bianchetti MG. Renal salt-wasting syndrome in children with intracranial disorders. Pediatr Nephrol. 2012 May. 27(5):733-9.[↩][↩]
- Moritz ML. Syndrome of inappropriate antidiuresis and cerebral salt wasting syndrome: are they different and does it matter?. Pediatr Nephrol. 2012 May. 27(5):689-93.[↩][↩][↩]
- Maesaka JK, Miyawaki N, Palaia T, Fishbane S, Durham JH. Renal salt wasting without cerebral disease: diagnostic value of urate determinations in hyponatremia. Kidney Int. 2007 Apr. 71(8):822-6.[↩][↩]
- Bitew S, Imbriano L, Miyawaki N, Fishbane S, Maesaka JK. More on renal salt wasting without cerebral disease: response to saline infusion. Clin J Am Soc Nephrol. 2009 Feb. 4(2):309-15.[↩]
- Tenny S, Thorell W. Cerebral Salt Wasting Syndrome. [Updated 2018 Nov 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534855[↩][↩][↩][↩]
- Kao L, Al-Lawati Z, Vavao J, Steinberg GK, Katznelson L. Prevalence and clinical demographics of cerebral salt wasting in patients with aneurysmal subarachnoid hemorrhage. Pituitary. 2009. 12(4):347-51.[↩]
- Maesaka JK, Imbriano LJ, Ali NM, Ilamathi E. Is it cerebral or renal salt wasting?. Kidney Int. 2009 Nov. 76(9):934-8[↩]
- Kojima J, Katayama Y, Moro N, et al. Cerebral salt wasting in subarachnoid hemorrhage rats: model, mechanism, and tool. Life Sci. 2005 Apr 1. 76(20):2361-70.[↩]
- Cerdà-Esteve M, Cuadrado-Godia E, Chillaron JJ, Pont-Sunyer C, Cucurella G, Fernández M, Goday A, Cano-Pérez JF, Rodríguez-Campello A, Roquer J. Cerebral salt wasting syndrome: review. Eur. J. Intern. Med. 2008 Jun;19(4):249-54[↩]
- Sherlock M, O’Sullivan E, Agha A, et al. Incidence and pathophysiology of severe hyponatraemia in neurosurgical patients. Postgrad Med J. 2009 Apr. 85(1002):171-5.[↩]
- Arieff AI, Gabbai R, Goldfine ID. Cerebral Salt-Wasting Syndrome: Diagnosis by Urine Sodium Excretion. Am J Med Sci. 2017 Oct. 354 (4):350-4.[↩]
- Wu X, Zhou X, Gao L, et al. Diagnosis and Management of Combined Central Diabetes Insipidus and Cerebral Salt Wasting Syndrome After Traumatic Brain Injury. World Neurosurg. 2016 Apr. 88:483-7.[↩][↩]
- [Guideline] Rahman M, Friedman WA. Hyponatremia in neurosurgical patients: clinical guidelines development. Neurosurgery. 2009 Nov. 65(5):925-35; discussion 935-6.[↩]





