What are wisdom teeth
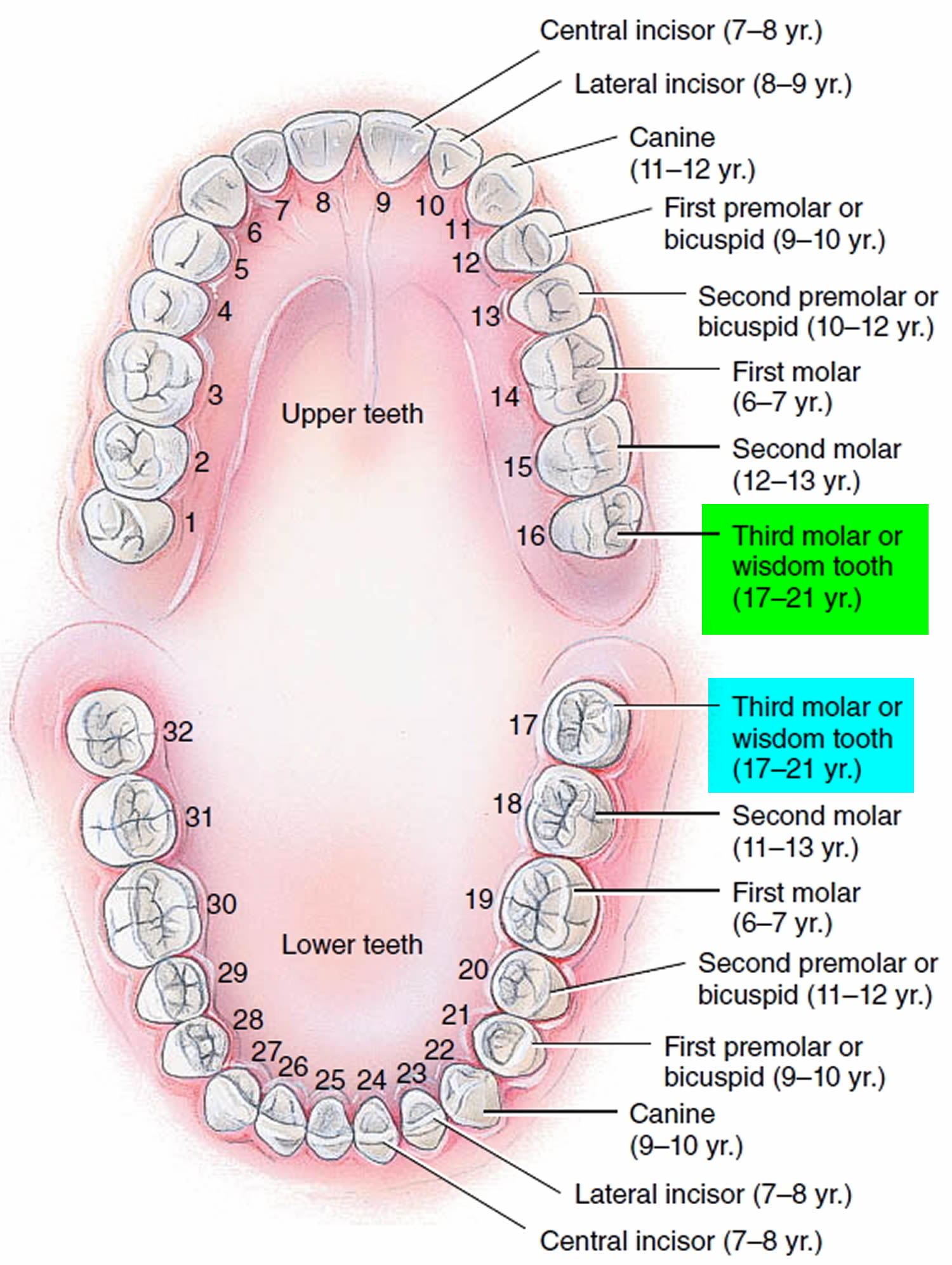
Humans have two dentitions, or sets of teeth: deciduous and permanent. The first of these—the deciduous teeth (decidu- = falling out), also called primary teeth, milk teeth, or baby teeth—begin to erupt at about 6 months of age, and approximately two teeth appear each month thereafter, until all 20 are present. All of the deciduous teeth are lost—generally between ages 6 and 12 years—and are replaced by the permanent (secondary) teeth (Figure 1).
The permanent dentition contains 32 teeth that erupt between age 6 and adulthood. The pattern resembles the deciduous dentition, with the following exceptions. The deciduous molars are replaced by the first and second premolars (bicuspids), which have two cusps and one root and are used for crushing and grinding. The permanent molars, which erupt into the mouth posterior to the premolars, do not replace any deciduous teeth and erupt as the jaw grows to accommodate them—the first permanent molars at age 6 (six-year molars), the second permanent molars at age 12 (twelve-year molars), and the third permanent molars (wisdom teeth) after age 17 or not at all. Wisdom teeth usually don’t develop fully until the ages of 18 to 24 1.
Wisdom teeth are the last molars to develop. They are located on each side of the jaw in the very back of your mouth. Most people have four wisdom teeth – one in each corner. By the time you are between 16-19 years old, you should be able to see them with the other 28 adult teeth that are usually already in place, so there isn’t always enough room in the mouth for the wisdom teeth to grow properly. Because of the lack of space, the wisdom teeth can sometimes emerge at an angle or get stuck and only partially emerge. Wisdom teeth that grow through like this are known as impacted. You may not even realize that you have wisdom teeth if they are impacted meaning they haven’t broken through the gums. There is a small percentage of lucky people who are born with at least one wisdom tooth missing or their wisdom teeth (third molars) may be dwarfed in size. Some people don’t have any wisdom tooth at all!
Wisdom teeth are thought to date back to our distant ancestors who had larger jaws and more teeth. Nowadays, most people’s jaws are too small for these “extra” teeth. For a while they were almost always pulled, but because they don’t always cause problems, and removing them can have side effects, dentists are now a bit more hesitant.
Wisdom teeth — the third molars in the very back of your mouth — may not need to be removed if they are:
- Healthy
- Grown in completely (fully erupted)
- Positioned correctly and biting properly with their opposing teeth
- Able to be cleaned as part of daily hygiene practices
Wisdom teeth often stay inside the gum, or only partially break through the gum, although they have stopped growing. In most cases, though, wisdom teeth that don’t break through don’t cause any trouble.
The same is true if wisdom teeth break through: Sometimes they have enough space. But they may push against other teeth, come in crooked, and cause inflammations or other complications.
Many times, however, wisdom teeth don’t have room to grow properly and can cause problems. Erupting wisdom teeth can grow at various angles in the jaw, sometimes even horizontally. Problems can include wisdom teeth that:
- Wisdom teeth may emerge partially through the gums. Because this area is hard to see and clean, wisdom teeth that partially emerge create a passageway that can become a magnet for bacteria that cause gum disease and oral infection.
- Wisdom teeth may also crowd nearby teeth. If wisdom teeth don’t have enough room to come in properly, they may crowd or damage nearby teeth.
Regular dental visits are an important part of keeping your wisdom teeth healthy and stable – and helping your dentist make an appropriately timed recommendation for their removal, should that be necessary.
You should make an appointment to see your dentist if you’re experiencing severe pain or discomfort from your wisdom teeth. Your dentist will check your teeth and advise you on whether they need to be removed.
If your dentist thinks you may need your wisdom teeth removed, they’ll usually carry out an X-ray of your mouth. This gives them a clearer view of the position of your teeth.
As with any teeth problems, it’s important to see your dentist as soon as possible, rather than waiting for your regular dental check-up.
Diagnosis of wisdom teeth
If you are worried about your wisdom teeth it is best to talk to your dentist. They will first ask you about your symptoms and examine your mouth and jaw. An x-ray is taken to see the position of the teeth. This thorough examination can help to predict whether the wisdom teeth will cause problems or will come in normally.
Impacted wisdom tooth
Often your jaw does not have enough room behind the second molars to accommodate the eruption of the wisdom teeth (third molars). In this case, the wisdom teeth (third molars) remain embedded in the alveolar bone and completely hidden within the gums. If wisdom teeth aren’t able to emerge normally, wisdom teeth are said to be impacted (trapped) within your jaw. Wisdom teeth become partially or completely impacted owing to lack of space, obstruction, or abnormal position. Impacted wisdom teeth may be diagnosed because of symptoms such as pressure, pain, or swelling; by physical examination with probing or direct visualisation; or incidentally by routine dental radiography.
Wisdom tooth impaction may be more common now than in the past, as modern diet tends to be softer.
Although some people never have any trouble with them, impacted wisdom teeth can cause problems 1. An impacted wisdom tooth can sometimes trap food, plaque, and other debris in the soft tissue around it, leading to swelling, gum tenderness, cavities, and bad breath. Sometimes this can result in infection or can cause a cyst that can damage other teeth roots or bone support. And in this situation your dentist may recommend their removal.
You should see your dentist or oral surgeon to find out if your tooth is impacted. Dentists or oral surgeons often remove impacted wisdom teeth because they may damage other teeth or cause pain or infection.
During a regular check-up, your dentist will take an x-ray to find out where your wisdom teeth are located and if they are impacted. Make an appointment earlier if you have:
- Trouble opening your jaw
- Pain when you bite or chew
- Swollen gums at the back of your mouth or near the side of your jaw
- Irritation or pain when you open your mouth
Why are wisdom teeth removed?
Your wisdom teeth don’t usually need to be removed if they’re impacted but aren’t causing any problems. This is because there’s no proven benefit of doing this and it carries the risk of complications.
Sometimes, wisdom teeth that have become impacted or haven’t fully broken through the surface of the gum can cause dental problems. Food and bacteria can get trapped around the edge of the wisdom teeth, causing a build-up of plaque, which can lead to:
- tooth decay (dental caries) – this develops when plaque begins to break down the surface of your tooth. When tooth decay becomes more advanced, it leaves holes (cavities) in the tooth, which can affect the surrounding teeth.
- gum disease (also called gingivitis or periodontal disease) – this occurs when plaque releases toxins that irritate your gums, making them red, swollen and painful. Gum disease can also affect the surrounding teeth and the bone around the wisdom teeth.
- pericoronitis – when plaque causes an infection of the soft tissue that surrounds the tooth.
- cellulitis – a bacterial infection in the cheek, tongue or throat.
- abscess – when pus collects in your wisdom teeth or the surrounding tissue due to a bacterial infection.
- cysts and benign growths – very rarely, a wisdom tooth that hasn’t cut through the gum develops a cyst (a fluid-filled swelling).
Many of these problems can be treated with treatment such as antibiotics and antiseptic mouthwash, so removing your wisdom teeth is only recommended when other treatment hasn’t worked.
Figure 1. Teeth and their time of eruption
Wisdom teeth symptoms
In addition to problematic impacted wisdom teeth, partially erupted wisdom teeth (poking through the gums a little bit) may need to be removed. Bits of food and bacteria get trapped in the pockets between the partially erupted tooth and gum, and can cause infections and gum disease, not to mention discomfort. As there is always some risk of nerve damage to the lower jaw when removing wisdom teeth, your dentist will evaluate the risks and benefits of tooth removal in your individual circumstance and will consult with you on management or removal.
Most people who are having problems with their wisdom teeth experience pain in cycles. When the pain goes away for a while, they often decide it’s not a big enough problem to worry about. These pain cycles can continue for years. However, it’s better to remove the offending tooth early, as both the surgery and the healing afterward tend to be much easier when the jawbones are younger and spongier.
Wisdom tooth extraction
Some dentists recommend removing wisdom teeth if they don’t fully emerge. Many dentists believe it’s better to remove wisdom teeth at a younger age, before the roots and bone are fully formed, and when recovery is generally faster after surgery. This is why some young adults have their wisdom teeth pulled before the teeth cause problems. But nowadays this is usually only recommended if the teeth are causing problems or it is thought they will.
According to the American Dental Association, wisdom teeth removal may be necessary if you experience changes in the area of those teeth, such as:
- Pain
- Repeated infection of soft tissue behind the lower last tooth
- Fluid-filled sacs (cysts)
- Tumors
- Damage to nearby teeth
- Gum disease
- Extensive tooth decay or cavities that cannot be restored
The decision to remove wisdom teeth isn’t always clear. Talk to your dentist or an oral surgeon about the position and health of your wisdom teeth and what’s best for your situation.
Wisdom teeth surgery
If your dentist recommends removing your wisdom teeth, they’ll take an X-ray of your mouth to help them determine who should carry out the procedure.
Your dentist may remove your wisdom teeth or they may refer you to a specialist surgeon for hospital treatment.
Anesthesia
Before having your wisdom teeth removed, you’ll be given an injection of local anesthetic to numb the tooth and surrounding area.
If you’re particularly anxious about the procedure, your dentist or surgeon may give you a sedative to help you relax. This usually involves an injection into your arm.
General anesthetic is rarely necessary. When it’s needed, your wisdom tooth will be removed in hospital, although you should still be able to go home on the same day as the procedure.
Removing the wisdom tooth
If the tooth hasn’t come through the gum, a small cut (incision) will be made in the gum to access it. A small piece of the bone covering the tooth may also need to be removed.
The tooth may be cut into smaller parts to make it easier to remove through the opening. There’s less need to make an incision if the tooth has broken through the gum.
You’ll feel some pressure just before the tooth is removed. This is because your dentist or oral surgeon needs to widen the tooth socket by rocking the tooth back and forth before taking it out.
Surgery to remove wisdom teeth shouldn’t be painful, because the area will be numb. However, if you feel pain during the procedure, tell your dentist or oral surgeon so they can give you more anesthetic.
How long it takes to remove the tooth will vary. Simple procedures can take a few minutes, but it can take longer than 20 minutes if it’s more complicated.
After your wisdom teeth have been removed, you may experience swelling and discomfort, both on the inside and outside of your mouth. This is usually worse for the first three days, but it can last for up to two weeks.
After wisdom tooth surgery
If an incision has been made, dissolving stitches are used to seal the gum. Your dentist will tell you how long the stitches take to dissolve (usually 7 to 10 days).
Your dentist may place gauze over the site of the extraction and ask you to keep pressure on it by biting your jaws together for up to an hour. This is to allow a blood clot to form in the empty tooth socket. Blood clots are part of the healing process, so try not to dislodge them.
In some cases, antibiotics may be prescribed if you have an ongoing infection.
For the 24 hours after removing your wisdom tooth, you should avoid:
- rinsing your mouth out with liquid
- drinking alcohol and smoking
- drinking hot liquids such as tea or soup
- strenuous physical activity
Wisdom teeth removal recovery
After your wisdom teeth extraction, you should be able to go home the same day.
Depending on the difficulty of the procedure and the risk of infection, you may be given antibiotics.
During this time, you may experience:
- swelling (inflammation) of your mouth and cheeks – this will be worse for the first few days, but gradually improves; gently pressing a cold cloth to your face helps to reduce the swelling
- a stiff, sore jaw – this should wear off within 7 to 10 days; the skin around your jaw may also be bruised for up to two weeks
- pain – this is worse if the extraction was complicated
- an unpleasant taste in your mouth
- tingling or numbness of your face, lips or tongue (although this is uncommon)
You should report any excess bleeding, severe pain or any other unusual symptoms to your dentist or oral surgeon immediately.
You may need to take up to a week off work. You should be able to return to normal activities within a week.
It can take up to two weeks to fully recover after having your wisdom teeth removed.
You may be instructed to modify your diet following surgery and later progress to more normal foods.
Most people make a full recovery.
After wisdom teeth removal self-care advice
To reduce pain and aid your recovery, it can be helpful to:
- use painkillers such as paracetamol or ibuprofen (always read and follow the manufacturer’s dosage instructions) – there’s some evidence to suggest that ibuprofen is the best painkiller to take after having wisdom teeth removed
- avoid strenuous activity and exercise for a few days
- use an extra pillow to support your head at night
- for 24 hours, avoid rinsing, spitting, hot drinks or anything else that may dislodge the blood clots that form in the empty tooth socket, as they help the healing process
- avoid drinking alcohol and smoking
- eat soft or liquid food for a few days and chew with your other teeth
- gently rinse the extraction site with antiseptic mouthwash after 24 hours, and repeat this regularly over the next few days – you can also use warm water with a teaspoon of salt as mouthwash, to reduce gum soreness and inflammation
Working and driving
It’s usually recommended that you take a day or two off work after having a wisdom tooth removed.
You can drive immediately after the procedure if local anesthetic was used, but you should avoid driving for at least 24 hours if a sedative was used, or 48 hours if the procedure was carried out under general anesthetic.
Returning to normal
After your wisdom teeth have been removed and any swelling and bruising has disappeared, your mouth and face should return to normal.
You’ll usually be able to brush your teeth normally after a few days. Make sure you finish any course of antibiotics you’ve been given.
A check-up appointment may be arranged for about a week or so after the procedure. At this point, any remaining stitches may be removed.
Wisdom Teeth Removal Complications or Adverse Effects of Extraction 1
- Pain;
- Bleeding;
- Swelling;
- Nerve injury – this can cause temporary or permanent problems, such as pain and numbness;
- Prolonged or persistent trismus (spasm of the jaw muscles, causing the mouth to remain tightly closed);
- Persistent or excessive bleeding;
- Surgical-site infection with or without cellulitis or osteomyelitis. Infection – signs include a high temperature, yellow or white discharge;
- Disruption to regular activities of daily living (e.g., chewing, speaking, and missing work or education);
- Wound dehiscence;
- Wisdom teeth dry socket (alveolar osteitis);
- New or persistent periodontal defects on the adjacent teeth;
- Damage to adjacent teeth or restorations;
- Temporary, permanent, or prolonged symptoms related to inferior alveolar or lingual nerve injuries;
- Maxillary tuberosity fracture;
- Temporary or persistent oro-antral communication with or without sinusitis.
Wisdom teeth dry socket
Dry socket (alveolar osteitis) is one of the most common complications of wisdom tooth removal. It occurs when a blood clot fails to develop in the tooth socket, or if the blood clot becomes dislodged or disappears. This can happen three to five days after surgery.
The empty socket causes an ache or throbbing pain in your gum or jaw, which can be intense. There may also be an unpleasant smell or taste from the empty tooth socket. If you look into the socket, you might be able to see exposed bone rather than a blood clot.
You’re more at risk of developing dry socket if:
- you don’t follow your dentist’s instructions after the extraction
- you smoke
- you’ve had the condition before
- you’re over 25 years old
- the extraction was complicated
Contact your dentist or surgeon if you suspect you have dry socket. They can flush any debris out of the socket or cover it with a medicated dressing, which may be removed and replaced frequently until it heals.
Dry socket may occur as a complication secondary to the removal of any tooth. However, most dry socket cases develop in the third molar region. Dry socket is multifactorial in nature 2. Wisdom teeth dry socket or alveolar osteitis (dry socket) is a complication of dental extractions and occurs more commonly in extractions involving mandibular molar teeth 3. In a dry socket, blood clots dissolve 4. Dry socket is associated with severe pain developing 2 to 3 days post-operatively and in some patients there may be a complaint of halitosis. Dry socket may result from many factors including surgical trauma, infection, type of extraction, patient factors, and surgeon factors 5. Fibrinolytic activity is postulated to occur through plasminogen-mediated fibrinolysis, non-plasminogen-mediated fibrinolysis, and leucocyte-mediated fibrinolysis 6. Other reports have suggested explanations for the differential occurrence of dry socket in females, including menstrual cycle associations and the use of oral contraceptives 7. Poor oral hygiene and dislodgement of clot due to forceful spitting and sucking through straw have been suggested as predisposing factors 8.
Since dry socket is the most common post extraction complication, many researchers have attempted to find a successful method for its prevention. Systemic antibiotics, topical antibiotics, chlorhexidine, para-hydroxybenzoic acid, tranexemic acid, polylactic acid, steroids, eugenol containing dressings, lavage, 9-aminoacridine, etc., have been proposed to assist in the prevention of dry socket. However, this area remains controversial as no single method has gained universal acceptance 9.
The management of dry socket is as controversial as its etiology and prevention. Recommending any “treatment” is probably misleading as the condition cannot be treated as long as the etiology has not been firmly established. Most agree that the primary aim of dry socket management, as indicated by Fazakerlev and Field [10], is pain control until commencement of normal healing, and in the majority, local measures alone are satisfactory. In some instances, systemic analgesics or antibiotics may be necessary. The use of intra-alveolar dressing materials is widely suggested in the literature, although it is generally acknowledged that dressings delay healing of the extraction socket. Different medicaments and carrier systems are commercially available with little scientific evidence to guide a selection process for their use 9.
Management of dry socket was initially with anti-bacterial agents 8, lavage, anti-fibrinolytic agents, steroidal anti-inflammatory agents, analgesics and clot supportive agents 10. The concept of dry socket management is changing toward alternative interventions including plasma rich growth factors, platelet rich fibrin 11, low level laser therapy 12 and other treatments such as the use of honey. However, none of these modalities have proven 100% successful for prevention or for treatment 3.
There is some evidence that rinsing with chlorhexidine (0.12% and 0.2%) or placing chlorhexidine gel (0.2%) in the sockets of extracted teeth, provides a benefit in preventing dry socket 3. However there have been reports in the UK of two cases of serious adverse events associated with irrigation of dry socket with chlorhexidine mouthrinse.
How to prevent dry socket
In a well conducted systematic Cochrane review of dry socket prevention, there is some evidence that rinsing both before and after tooth extraction with chlorhexidine gluconate rinse (at 0.12% and 0.2% strength) or placing chlorhexidine gel (0.2%) in the sockets of extracted teeth, provides a benefit in preventing dry socket 3. However, there was insufficient evidence to conclude whether any treatments relieved established dry socket or not 3.
Nerve injury
Although far less common than dry socket, injury to sections of a nerve called the trigeminal nerve is another possible complication of wisdom tooth removal. This can cause pain, a tingling sensation and numbness in the tongue, lower lip, chin, teeth and gums.
In most cases, the damage is temporary, lasting for a few weeks or months. However, it can be permanent if the nerve has been severely damaged.
A nerve injury can interfere with your daily activities, making things such as eating and drinking difficult and painful.
Every attempt will be made to minimize the possibility of nerve damage when your wisdom tooth is removed, and you should be informed about the risk of complications before the procedure.
- Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clinical Evidence. 2014;2014:1302. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4148832/[↩][↩][↩]
- Alveolar osteitis following surgical removal of mandibular third molars. Fridrich KL, Olson RA. Anesth Prog. 1990 Jan-Feb; 37(1):32-41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2163524/pdf/anesthprog00261-0038.pdf[↩]
- Daly B, Sharif MO, Newton T, Jones K, Worthington HV. Local interventions for the management of alveolar osteitis (dry socket). Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No.: CD006968. DOI: 10.1002/14651858.CD006968.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006968.pub2/full[↩][↩][↩][↩][↩]
- Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Blum IR. Int J Oral Maxillofac Surg. 2002 Jun; 31(3):309-17. https://www.ncbi.nlm.nih.gov/pubmed/12190139/[↩]
- Prevention of alveolar osteitis with chlorhexidine: a meta-analytic review. Caso A, Hung LK, Beirne OR. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005 Feb; 99(2):155-9. https://www.ncbi.nlm.nih.gov/pubmed/15660084/[↩]
- Dental extraction wound management: medicating postextraction sockets. Vezeau PJ. Oral Maxillofac Surg. 2000 May; 58(5):531-7. https://www.ncbi.nlm.nih.gov/pubmed/10800909/[↩]
- Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar? Garcia AG, Grana PM, Sampedro FG, Diago MP, Rey JM. Br Dent J. 2003 Apr 26; 194(8):453-5; discussion 445. https://www.ncbi.nlm.nih.gov/pubmed/12778101/[↩]
- Modern concepts in understanding and management of the “dry socket” syndrome: comprehensive review of the literature. Noroozi AR, Philbert RF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Jan; 107(1):30-5. https://www.ncbi.nlm.nih.gov/pubmed/18755610/[↩][↩]
- Alveolar osteitis: a comprehensive review of concepts and controversies. Kolokythas A, Olech E, Miloro M. Int J Dent. 2010; 2010():249073. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2905714/[↩][↩]
- Comparison of alvogyl, SaliCept patch, and low-level laser therapy in the management of alveolar osteitis. Kaya GŞ, Yapici G, Savaş Z, Güngörmüş M. J Oral Maxillofac Surg. 2011 Jun; 69(6):1571-7.[↩]
- Chakravarthi S. Platelet rich fibrin in the management of established dry socket. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2017;43(3):160-165. doi:10.5125/jkaoms.2017.43.3.160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5529189/[↩]
- [Assessment of the effectiveness of low level laser in the treatment of alveolar osteitis]. Jovanović G, Urić N, Krunić N, Tijanić M, Stojanović S. Vojnosanit Pregl. 2011 Jun; 68(6):506-10. https://www.ncbi.nlm.nih.gov/pubmed/21818918/[↩]