Contents
What is endoscopy
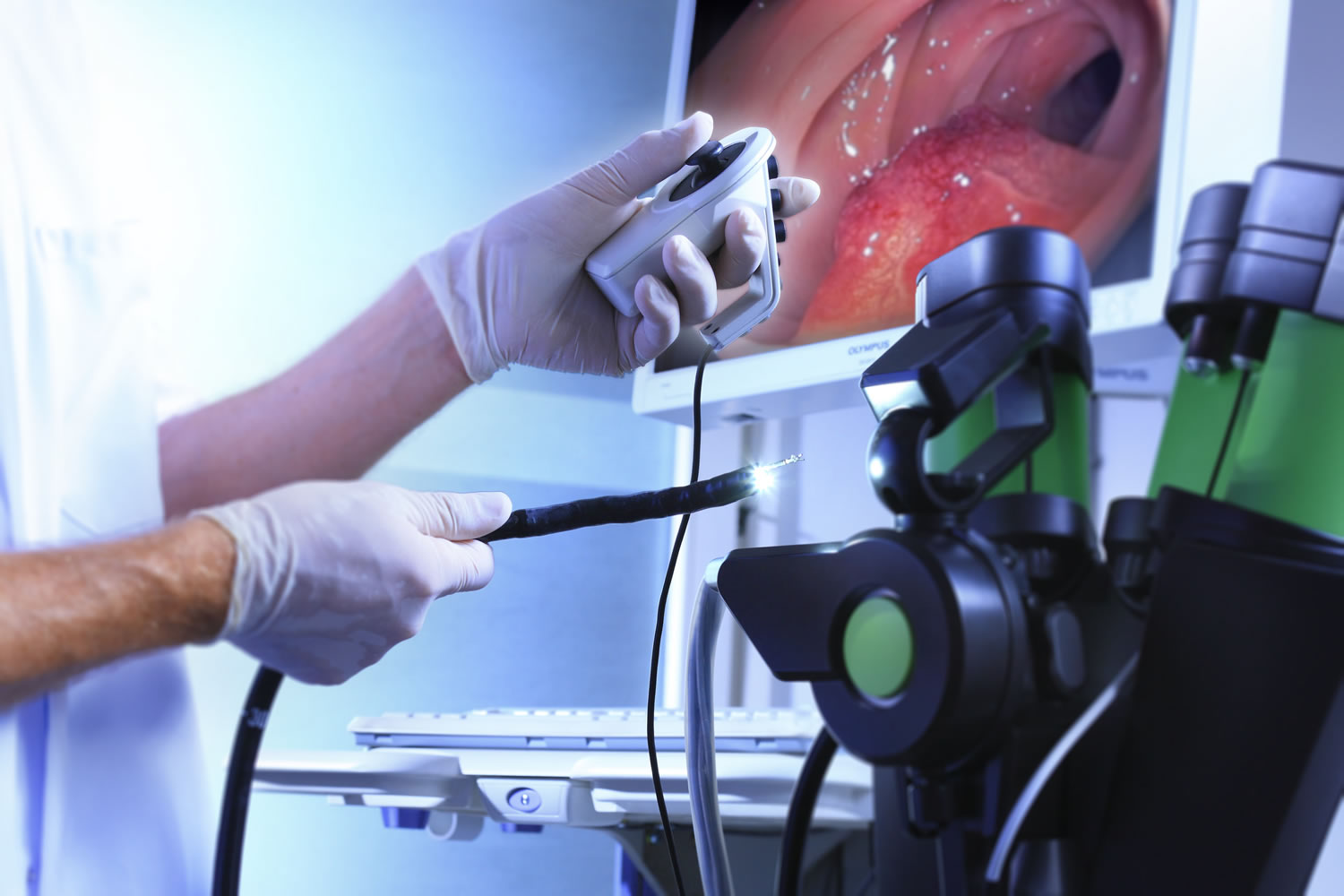
Endoscopy is a medical procedure where a doctor puts a tube-like instrument (an endoscope) into your body to look inside. There are many types of endoscopy, each type is specially designed for looking at a certain part of the body and is sometimes used for certain kinds of surgery or procedure.
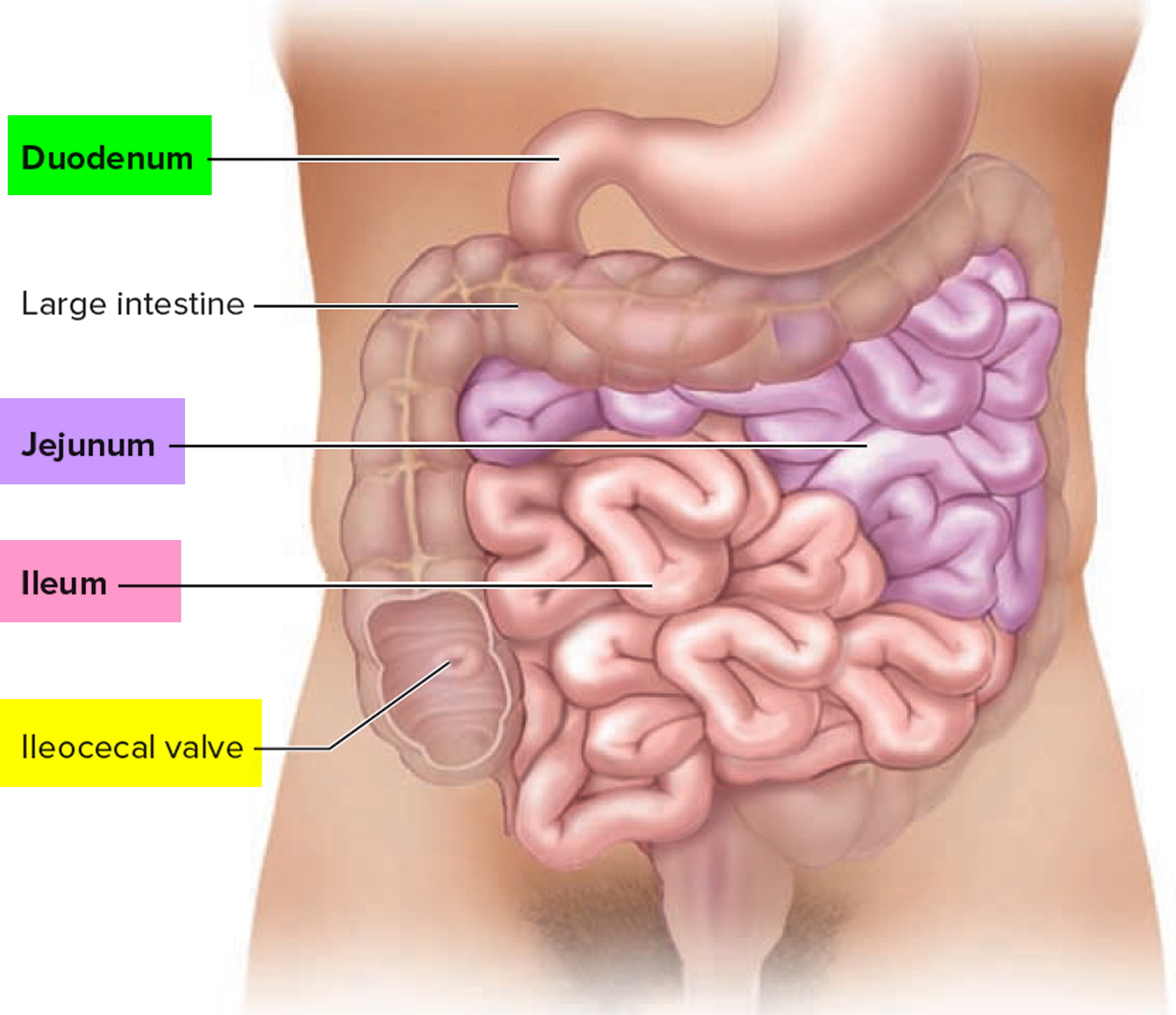
There are many different kinds of endoscopes, or “scopes.” Most are like thin, hollow tubes that a doctor uses to look right into the body. Most are lighted, and some have a small video camera on the end that puts pictures on a computer screen. Endoscopes are different lengths and shapes. Some are stiff, while others are flexible. There’s a new one called capsule endoscopy, which is small enough to be swallowed, which can send images wirelessly. Capsule endoscopy is often used to help your doctor see inside your small intestine. Your small intestine, which is composed of three sections, runs from your stomach to your colon (see Figure 3).
Depending on the area of the body being looked at, the endoscope may be put in the mouth, anus, or urethra (the tube that carries urine out of the bladder). Sometimes, it’s put through a small incision (cut) made in the skin.
Table 1. Some types of endoscopes and the areas of the body they view
| Type of endoscope | Put in through | Body part or area(s) looked at | Name(s) of procedure |
| Arthroscope | Cuts in the skin | Joints | Arthroscopy |
| Bronchoscope | Mouth or nose | Trachea (windpipe) and bronchi (tubes going to the lungs) | Bronchoscopy, flexible bronchoscopy |
| Colonoscope | Anus | Colon and large intestine | Colonoscopy, lower endoscopy |
| Cystoscope | Urethra | Bladder | Cystoscopy, cystourethroscopy |
| Enteroscope | Mouth or anus | Small intestine | Enteroscopy |
| Esophagogastro-duodenoscope | Mouth | Esophagus (swallowing tube), stomach, and duodenum (first part of small intestine) | Esophagogastro-duodenoscopy (EGD), upper endoscopy, panendoscopy, gastroscopy |
| Hysteroscope | Vagina | Inside of uterus | Hysteroscopy |
| Laparoscope | Cut(s) in the abdomen (belly) | Space inside abdomen and pelvis | Laparoscopy, peritoneal endoscopy |
| Laryngoscope | Mouth or nose | Larynx (voice box) | Laryngoscopy |
| Mediastinoscope | Cut(s) above the sternum (breastbone) | Mediastinum (space between the lungs) | Mediastinoscopy |
| Sigmoidoscope, flexible sigmoidoscope | Anus | Rectum and sigmoid colon (lower part of large intestine) | Sigmoidoscopy, flexible sigmoidoscopy, proctosigmoidoscopy |
| Thoracoscope | Cut(s) in the chest | Space between lungs and chest wall | Thoracoscopy, pleuroscopy |
When is endoscopy used?
Endoscopes were first developed to look at parts of the body that couldn’t be seen any other way. This is still a common reason to use them, but endoscopy now has many other uses too. It’s often used in the prevention, early detection, diagnosis, staging, and treatment of cancer.
To prevent and screen for cancer
Some types of endoscopes are used to look for cancer in people who have no symptoms. For example, colonoscopy and sigmoidoscopy are used to screen for colon and rectal cancer. These procedures can also help prevent cancer because they let doctors find and remove polyps (growths) that might become cancer if left alone.
To find cancer early
Endoscopy can sometimes be used to find cancer early, before it has had a chance to grow or spread.
Looking for causes of symptoms
When people go to the doctor with certain symptoms, endoscopy can sometimes be used to help find a cause. For instance:
- Laryngoscopy to look at the vocal cords in people with long-term hoarseness
- Upper endoscopy in people having trouble swallowing
- Colonoscopy in people with anemia (low red blood cell counts) with an unknown cause
- Colonoscopy in people with blood in their stool
Looking at problems found on imaging tests
Imaging tests such as x-rays and CT scans can sometimes show physical changes within the body. But these tests may only give information about the size, shape, and location of the problem. Doctors use endoscopes to see more details, like color and surface texture, when trying to find out what’s going on. Newer methods of endoscopy that include high magnification are being tested to find out whether they are more useful in detecting cancer and other abnormal cells on the inner surfaces of the body.
To diagnose and find out the stage (extent) of cancer
To get a tissue sample
Going one step further, most types of endoscopes have tools on the end that the doctor can use to take out small tissue samples. This procedure is called a biopsy. Samples can be taken from suspicious areas and then looked at under a microscope or tested in other ways to see if cancer is there. A biopsy is usually the best way to find out if a growth or change is cancer or something else.
Getting a closer look
In some cases endoscopes are used to help find out how far a cancer has spread. Thoracoscopy and laparoscopy can be very useful in finding out if cancer has spread into the thorax (chest) or abdomen (belly). The surgeon can look into these places making only a small incision (cut) in the skin.
To get better pictures
Endoscopes can get pictures of the body parts they can get to. But some types of endoscopy can also be used to help get better, more detailed ultrasounds and x-rays in areas the scopes can’t quite reach. This can be especially useful when trying to find how much cancer is in the body (in other words, staging the cancer).
- Endoscopic ultrasound: Ultrasound is an imaging test in which a wand-like instrument (called a transducer) is moved over the skin. The transducer sends sound waves into the body. The waves bounce back in a pattern a computer uses to make a picture. Endoscopic ultrasound is a procedure in which a small transducer on the tip of an endoscope is put in through either the mouth or rectum. By putting the transducer on the tip of the endoscope, it can get closer to an organ or tumor to take more detailed ultrasound pictures. Endoscopic ultrasound is used to get information about problems in the digestive tract and nearby organs. It can be used to see how deep a tumor might have grown into the rectum or esophagus, or into a nearby organ like the pancreas. It can also help show if lymph nodes are swollen, which could mean they have cancer in them. Endoscopic ultrasound is proving useful in staging some lung, digestive tract (esophagus, stomach, pancreas, etc.), and other cancers. Endoscopic ultrasound can also help a doctor guide a needle to take a biopsy.
- Endoscopic retrograde cholangiopancreatography (ERCP): Endoscopic retrograde cholangiopancreatography (ERCP) is a complex procedure that helps doctors diagnose problems in the ducts of the pancreas, gall bladder, or liver. In this procedure, an endoscope is passed down the throat, through the stomach, and into the first part of the small intestine. The doctor then guides a tiny tube at the end of the endoscope into the common bile duct, which connects the intestine with the pancreas. A small amount of contrast material (dye) is pushed in, and x-rays are taken. The dye helps outline the bile ducts and pancreatic duct. The x-rays can show whether the ducts are narrowed or blocked, which could be caused by a gallstone or a cancer. The doctor doing this test can also put a small brush through the tube to take out some cells for biopsy.
To treat cancer
Destroying or removing cancer cells
Endoscopes can be used to take out or destroy small cancers. Small instruments passed through an endoscope can be used to cut out small growths. Doctors also can use tools like a cautery or laser through the tips of some endoscopes to burn or vaporize growths.
Surgery to take out cancer
Many types of endoscopic tools have been developed to let doctors perform minimally invasive surgery. This is sometimes called keyhole surgery. When it’s used for the abdomen (belly), it is called laparoscopic surgery. Instead of making one long surgical incision (cut), several small cuts are made in the skin, usually in the chest or abdomen. Long, thin instruments are then put through the cuts or holes to reach the inside of the body. A video endoscope – a thoracoscope or laparoscope – is put through one of the holes so that the surgeon can see inside during the operation.
This type of surgery is sometimes used to treat small lung cancers. This is called video-assisted thoracoscopic surgery It can also be used for the colon (called laparoscopic colectomy), prostate (called laparoscopic radical prostatectomy), and some other organs, but not all doctors agree keyhole surgery is better than open surgery.
- There are some benefits to keyhole surgery: Generally, less blood is lost during the operation and patients often recover faster and with less pain because the cuts are small. Some forms of keyhole surgery use robotic arms, which a surgeon controls from a console. This better magnifies the area so more precise work can be done with tiny, delicate surgical instruments.
- Keyhole surgery also has some drawbacks: It usually means more time in the operating room and more drugs to keep the patient asleep (more time under anesthesia). It also takes away the surgeon’s ability to feel organs for problems that they may not be able to see.
Most studies have not found keyhole surgery to be any less effective than open surgery, at least in the short term. But as of yet there are no studies to show that the long-term outcomes are the same.
If you are thinking about some type of minimally invasive or keyhole surgery, it’s important to understand the known benefits and risks. It’s also important to find out what’s not yet known about the procedure. If you decide on keyhole surgery, be sure your doctor has a lot of experience with the procedure and is skilled with the technique.
To relieve symptoms of advanced cancer
Endoscopes can also be used for palliative treatment (treatment given to reduce or control symptoms) in some cancers that can’t be cured by surgery. For example, instruments passed through endoscopes can be used to remove blockages in the lungs or digestive tract. If a tumor is narrowing an airway by pressing on its outside, endoscopy can be used to place a stent (a small, rigid tube) inside the airway to keep it open.
What is an endoscopy procedure like?
There are many different types of endoscopy procedures, and the experience of having one can vary a lot from one type to the next.
It’s important to keep in mind that some procedures might be done in more than one way. For example, bronchoscopy and laryngoscopy can be done with either a flexible or rigid scope. Local anesthesia (numbing the area) is generally used for flexible scopes, while rigid scopes often require general anesthesia (where you are given drugs to put you into a deep sleep).
People’s experiences may also vary depending on their health and what needs to be done, such as whether biopsy samples are going to be taken.
If you are going to have an endoscopy, your medical team will explain to you what will be done and what to expect before, during, and after the test. They will also tell you what you need to do to prepare for the procedure. The preparation could mean that you must fast (not eat anything) for a certain amount of time, follow a liquid diet for a certain amount of time, and/or use laxatives or enemas.
Table 2 shows some of the key facts of the more common forms of endoscopy.
Table 2. Common endoscopy and their procedures
| Type of endoscopy | Special preparation* (usually starting the night before) | Is it usually done in an operating room? | Usual type of anesthesia† | How long it takes (estimate) |
| Arthroscopy | Fasting | Yes | Local and sedation | 30 to 45 minutes |
| Bronchoscopy | Fasting | No | Local and sedation or general | 30 min to 2 hours |
| Enteroscopy | Fasting, liquid diet and laxative/ enema if using anal entry | No | Sedation or general | 45 to 90 minutes |
| Laryngoscopy | Fasting | No | Local or general | 15 min to 1 hour |
| Upper endoscopy | Fasting | No | Local and sedation | 15 to 30 min |
| Flexible sigmoidoscopy | Liquid diet, laxative/enema | No | Usually none | 15 to 30 min |
| Colonoscopy | Liquid diet, laxative/enema | No | Mild sedation | 30 to 60 min |
| Cystoscopy | Fasting | Sometimes | Local or general | 15 to 30 min |
| Mediastinoscopy | Fasting | Yes | General | 1 to 2 hours |
| Thoracoscopy | Fasting | Yes | General | 2 to 3 hours |
| Laparoscopy | Fasting | Yes | General | 20 min to 1 hour |
Notes:
* Fasting means not eating for a certain amount of time before the procedure
† Anesthesia is the use of drugs to make you not feel pain during a procedure. There are different kinds of anesthesia:
- Local means the area the scope is passed through is numbed but you are awake.
- Sedation means you are awake, but drugs are used to make you sleepy and relaxed.
- General means drugs are used to put you into a deep sleep.
Nasal endoscopy
A nasal endoscopy is also called rhinoscopy, where a long, thin, flexible tube attached to a light source is inserted into your nose to examine the inside of your nose and sinuses to check for problems.
Why is nasal endoscopy performed
You may have a nasal endoscopy to figure out what is causing problems in your nose and sinuses.
Your ear, nose and throat (ENT) doctor may recommend nasal endoscopy if you are having:
- A lot of sinus infections
- Lots of drainage from your nose
- Face pain or pressure
- Sinus headaches
- A hard time breathing through your nose
- Nose bleeds
- Loss of sense of smell
During the nasal endoscopy procedure, your ear, nose and throat (ENT) doctor may:
- Look at the inside of your nose and sinuses
- Take a sample of tissue for a biopsy
- Do small surgeries to remove polyps, excess mucus, or other masses
Nasal endoscopy risks
There is very little risk with a nasal endoscopy for most people.
- If you have a bleeding disorder or take blood-thinning medicine, let your provider know so they are extra careful to decrease bleeding.
- If you have heart disease, there is a small risk that you could feel lightheaded or faint.
Nasal endoscopy prep
You do NOT need to do anything to prepare for the nasal endoscopy test.
How nasal endoscopy will feel
Nasal endoscopy test does not hurt.
- You may feel discomfort or pressure as the tube is put into your nose.
- The spray numbs your nose. It can numb your mouth and throat, and you may feel like you cannot swallow. This numbness goes away in 20 to 30 minutes.
- You might sneeze during the nasal endoscopy test. If you feel a sneeze coming on, let your provider know.
What is the procedure for a nasal endoscopy – what you can expect
How nasal endoscopy is performed
The test takes about 5 to 10 minutes. Your health care provider will:
- Spray your nose with a medicine to reduce swelling and numb the area.
- Insert the nasal endoscope into your nose. This is a long flexible or rigid tube with a camera at the end to look inside the nose and sinuses. Pictures may be projected onto a screen.
- Examine the inside of your nose and sinuses.
- Remove polyps, mucus, or other masses from the nose or sinuses.
Nasal endoscopy results
Normal Results
- The inside of the nose and bones look normal.
What Abnormal Results Mean
Nasal endoscopy helps with the diagnosis of:
- Polyps
- Blockages
- Sinusitis
- Swollen and runny nose that will not go away
- Nasal masses or tumors
- A foreign object (like a marble) in the nose or sinus
- Deviated septum (many insurance plans require a nasal endoscopy prior to surgery to correct it)
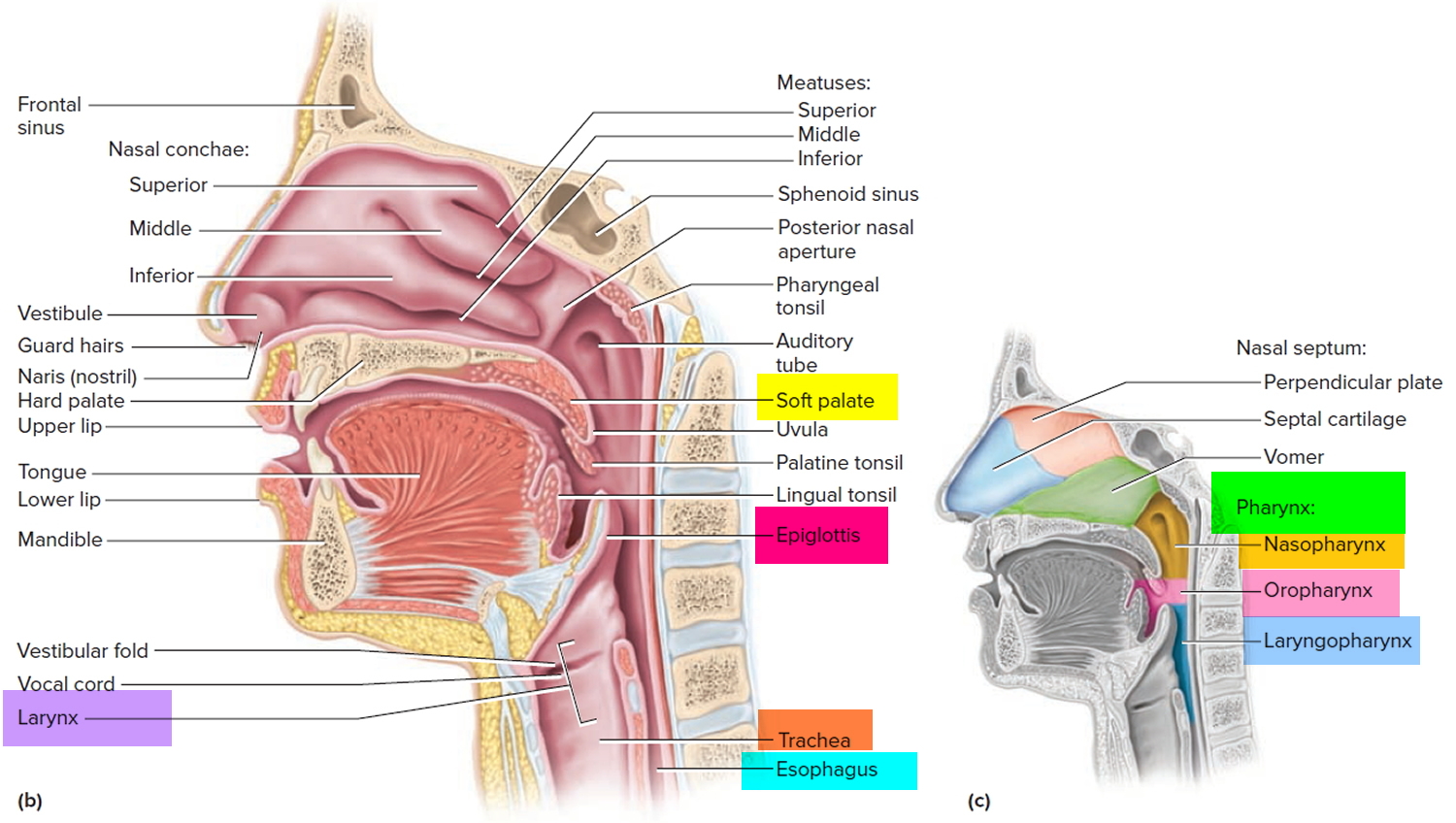
Figure 1. Pharynx and larynx anatomy
Upper endoscopy
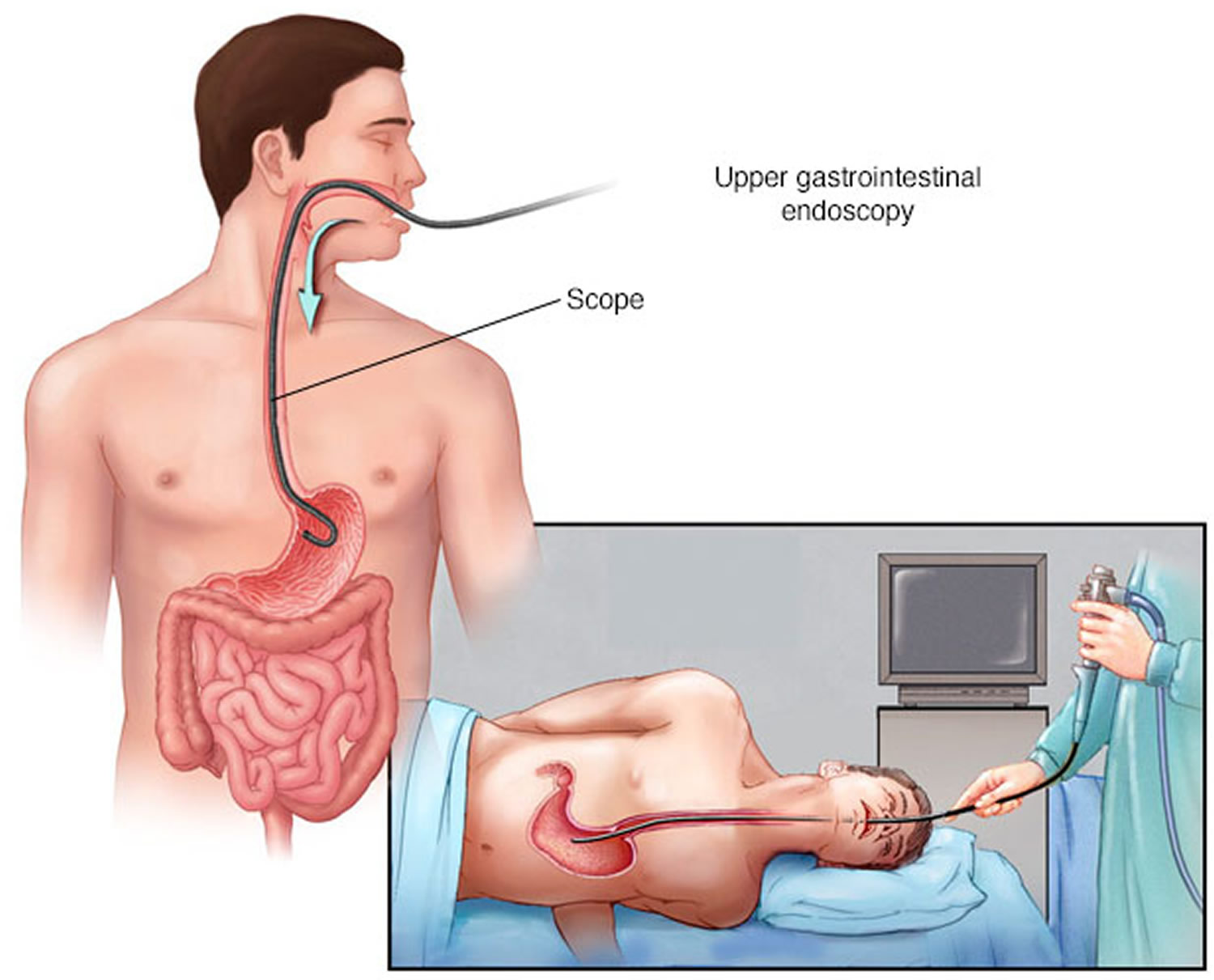
An upper endoscopy is a procedure used to visually examine your upper digestive system with a tiny camera on the end of a long, flexible tube. A specialist in diseases of the digestive system (gastroenterologist) uses an endoscopy to diagnose and sometimes, treat conditions that affect the esophagus, stomach and beginning of the small intestine (duodenum).
The medical term for an upper endoscopy is esophago-gastroduodenoscopy or upper GI (gastrointestinal) endoscopy. You may have an upper endoscopy done in your doctor’s office, an outpatient surgery center or a hospital.
Why is upper endoscopy done
An upper endoscopy is used to diagnose and, sometimes, treat conditions that affect the upper part of your digestive system, including the esophagus, stomach and beginning of the small intestine (duodenum).
Upper GI endoscopy can help find the cause of unexplained symptoms, such as:
- persistent heartburn
- bleeding
- nausea and vomiting
- pain
- problems swallowing
- unexplained weight loss
Upper GI endoscopy can be used to identify many different diseases:
- gastroesophageal reflux disease (GERD)
- ulcers
- cancer
- inflammation, or swelling
- precancerous abnormalities such as Barrett’s esophagus
- celiac disease
- strictures or narrowing of the esophagus
- blockages
Upper GI endoscopy can check for damage after a person eats or drinks harmful chemicals.
During upper GI endoscopy, a doctor obtains biopsies by passing an instrument through the endoscope to obtain a small piece of tissue for testing. Biopsies are needed to diagnose conditions such as:
- cancer
- celiac disease
- gastritis
Your doctor may recommend an upper GI endoscopy procedure to:
- Investigate symptoms. An upper endoscopy may help your doctor determine what’s causing digestive signs and symptoms, such as nausea, vomiting, abdominal pain, difficulty swallowing and gastrointestinal bleeding.
- Diagnose. Your doctor may use an upper endoscopy to collect tissue samples (biopsy) to test for diseases and conditions, such as anemia, bleeding, inflammation, diarrhea or cancers of the digestive system.
- Treat. Your doctor can pass special tools through the endoscope to treat problems in your digestive system, such as burning a bleeding vessel to stop bleeding, widening a narrow esophagus, clipping off a polyp or removing a foreign object.
- treat conditions such as bleeding from ulcers, esophageal varices, or other conditions
- dilate or open up strictures with a small balloon passed through the endoscope
- remove objects, including food, that may be stuck in the upper GI tract
- remove polyps or other growths
- place feeding tubes or drainage tubes
An upper endoscopy is sometimes combined with other procedures, such as an ultrasound. An ultrasound probe may be attached to the endoscope to create specialized images of the wall of your esophagus or stomach. An endoscopic ultrasound (EUS) may also help your doctor create images of hard-to-reach organs, such as your pancreas. Newer endoscopes use high-definition video to provide clearer images.
Many endoscopes allow your doctor to use technology called narrow band imaging, which uses special light to help better detect precancerous conditions, such as Barrett’s esophagus.
Doctors are also starting to use upper GI endoscopy to perform weight loss procedures for some people with obesity.
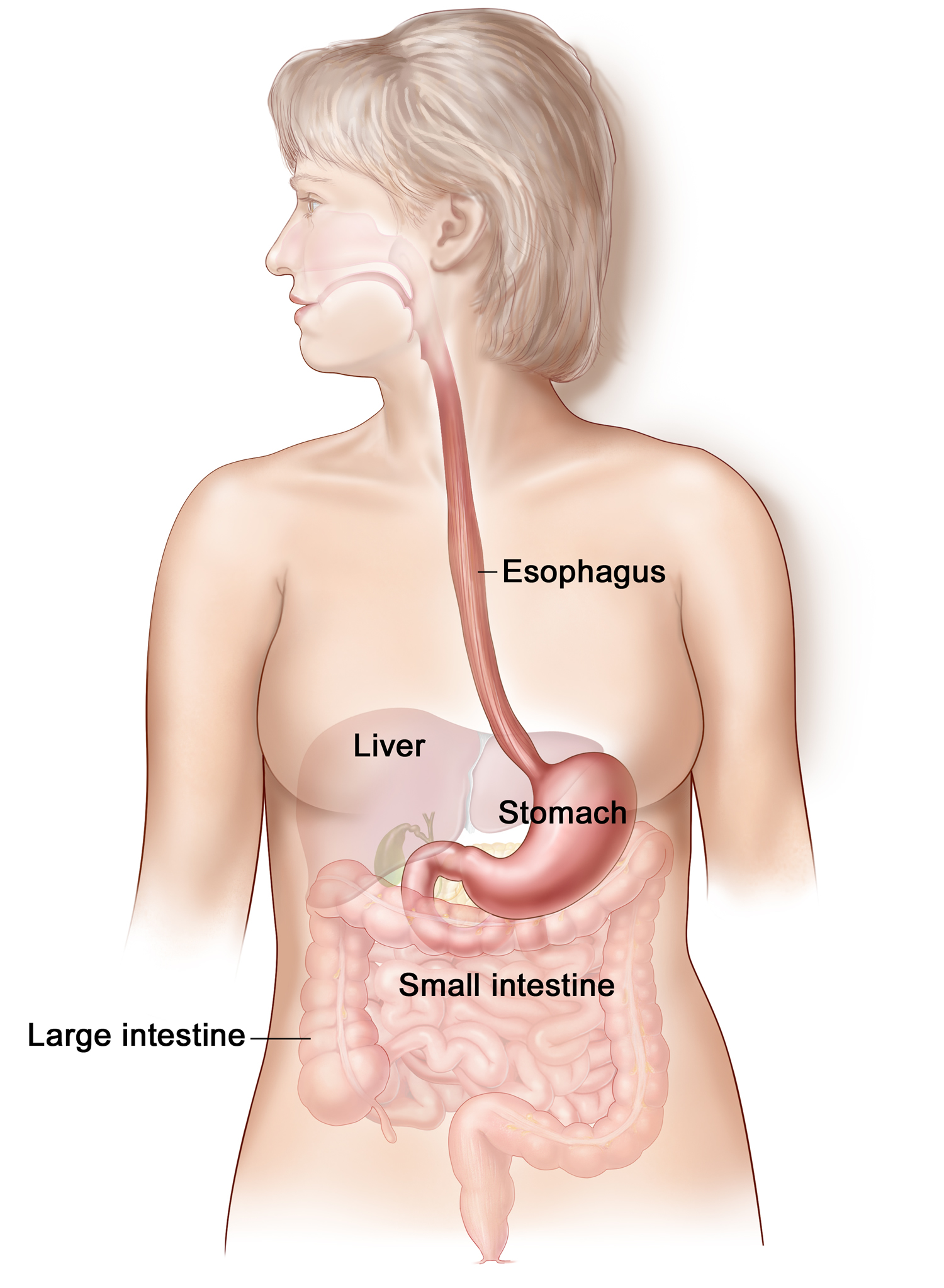
Figure 2. Esophagus
Notes: Upper endoscopy involves inserting a long, flexible tube (endoscope) down your throat and into your esophagus. A tiny camera on the end of the endoscope lets your doctor examine your esophagus, stomach and the beginning of your small intestine (duodenum).
Upper endoscopy risks
An upper endoscopy is a very safe procedure. Rare complications include:
- Bleeding. Your risk of bleeding complications after an endoscopy is increased if the procedure involves removing a piece of tissue for testing (biopsy) or treating a digestive system problem. In rare cases, such bleeding may require a blood transfusion.
- Infection. Most upper endoscopies consist of an examination and biopsy, and risk of infection is low. The risk of infection increases when additional procedures are performed as part of your endoscopy. Most infections are minor and can be treated with antibiotics. Your doctor may give you preventive antibiotics before your procedure if you are at higher risk of infection.
- Tearing of the gastrointestinal tract. A tear in your esophagus or another part of your upper digestive tract may require hospitalization, and sometimes surgery to repair it. The risk of this complication is very low — it occurs in an estimated 1 of every 2,500 to 11,000 diagnostic upper endoscopies. The risk increases if additional procedures, such as dilation to widen your esophagus, are performed.
Bleeding caused by the procedure often is minor and stops without treatment. Serious complications such as perforation are uncommon. Your doctor may need to perform surgery to treat some complications. Your doctor can also treat an abnormal reaction to a sedative with medicines or IV fluids during or after the procedure.
You can reduce your risk of complications by carefully following your doctor’s instructions for preparing for an endoscopy, such as fasting and stopping certain medications.
Signs and symptoms that could indicate a complication – Seek Care Right Away!
Signs and symptoms to watch for after your upper endoscopy include:
- Fever
- Chest pain
- Shortness of breath
- Bloody, black or very dark colored stool
- Difficulty swallowing
- Severe or persistent abdominal pain
- Vomiting, especially if your vomit is bloody or looks like coffee grounds
Call your doctor immediately or go to an emergency room if you experience any of these signs or symptoms.
Upper endoscopy prep
Your doctor will give you specific instructions to prepare for your upper endoscopy. In some cases your doctor may ask that you:
- Fast before the upper endoscopy. You will need to stop drinking and eating four to eight hours before your upper endoscopy to ensure your stomach is empty for the procedure.
- Stop taking certain medications. You will need to stop taking certain blood-thinning medications in the days before your upper endoscopy. Blood thinners may increase your risk of bleeding if certain procedures are performed during the upper endoscopy. If you have chronic conditions, such as diabetes, heart disease or high blood pressure, your doctor will give you specific instructions regarding your medications.
Tell your doctor about all the medications and supplements you’re taking before your upper GI endoscopy.
Plan ahead for your recovery
Most people undergoing an upper endoscopy will receive a sedative to relax them and make them more comfortable during the procedure. Plan ahead for your recovery while the sedative wears off. You may feel mentally alert, but your memory, reaction times and judgment may be impaired. Find someone to drive you home. You may also need to take the day off from work. Don’t make any important personal or financial decisions for 24 hours.
What is the procedure for an upper endoscopy – what you can expect
During an upper endoscopy
During an upper endoscopy procedure, you’ll be asked to lie down on a table on your back or on your side. As the procedure gets underway:
- Monitors often will be attached to your body. This will allow your health care team to monitor your breathing, blood pressure and heart rate.
- You may receive a sedative medication. This medication, given through a vein in your forearm, helps you relax during the upper endoscopy.
- Your doctor may spray an anesthetic in your mouth. This medication will numb your throat in preparation for insertion of the long, flexible tube (endoscope). You may be asked to wear a plastic mouth guard to hold your mouth open.
- Then the endoscope is inserted in your mouth. Your doctor may ask you to swallow as the scope passes down your throat. You may feel some pressure in your throat, but you shouldn’t feel pain.
You can’t talk after the endoscope passes down your throat, though you can make noises. The endoscope doesn’t interfere with your breathing.
As your doctor passes the endoscope down your esophagus:
- A tiny camera at the tip transmits images to a video monitor in the exam room. Your doctor watches this monitor to look for abnormalities in your upper digestive tract. If abnormalities are found in your digestive tract, your doctor may record images for later examination.
- Gentle air pressure may be fed into your esophagus to inflate your digestive tract. This allows the endoscope to move freely. And it allows your doctor to more easily examine the folds of your digestive tract. You may feel pressure or fullness from the added air.
- Your doctor will pass special surgical tools through the endoscope to collect a tissue sample or remove a polyp. Your doctor watches the video monitor to guide the tools.
When your doctor has finished the exam, the endoscope is slowly retracted through your mouth. An upper endoscopy typically takes 15 to 30 minutes, depending on your situation.
After the upper endoscopy
You’ll be taken to a recovery area to sit or lie quietly after your upper endoscopy. You may stay for an hour or so. This allows your health care team to monitor you as the sedative begins to wear off.
Once you’re at home, you may experience some mildly uncomfortable signs and symptoms after upper endoscopy, such as:
- Bloating and gas for a short time after the procedure
- Cramping
- Sore throat for 1 to 2 days
These signs and symptoms will improve with time. If you’re concerned or quite uncomfortable, call your doctor.
Take it easy for the rest of the day after your upper endoscopy. After receiving a sedative, you may feel alert, but your reaction times are affected and judgment is delayed.
A friend or family member who is with you if you’re still groggy—will receive instructions on how to care for yourself when you are home. You should follow all instructions.
You can go back to your normal diet once your swallowing returns to normal.
Upper endoscopy results
When you receive the results of your upper endoscopy will depend on your situation. If, for instance, your doctor performed the upper endoscopy to look for an ulcer, you may learn the findings right after your procedure. If he or she collected a tissue sample (biopsy), you may need to wait a few days to get results from the testing laboratory. Ask your doctor when you can expect the results of your upper GI endoscopy.
Capsule endoscopy
Doctors can see a lot of the digestive tract using upper endoscopy or colonoscopy. But it’s harder for the 20 feet or so of small intestine to be seen this way, although enteroscopy can be used. Cancers in this area of the small intestine are rare, but tumors and other problems such as ulcers can develop here.
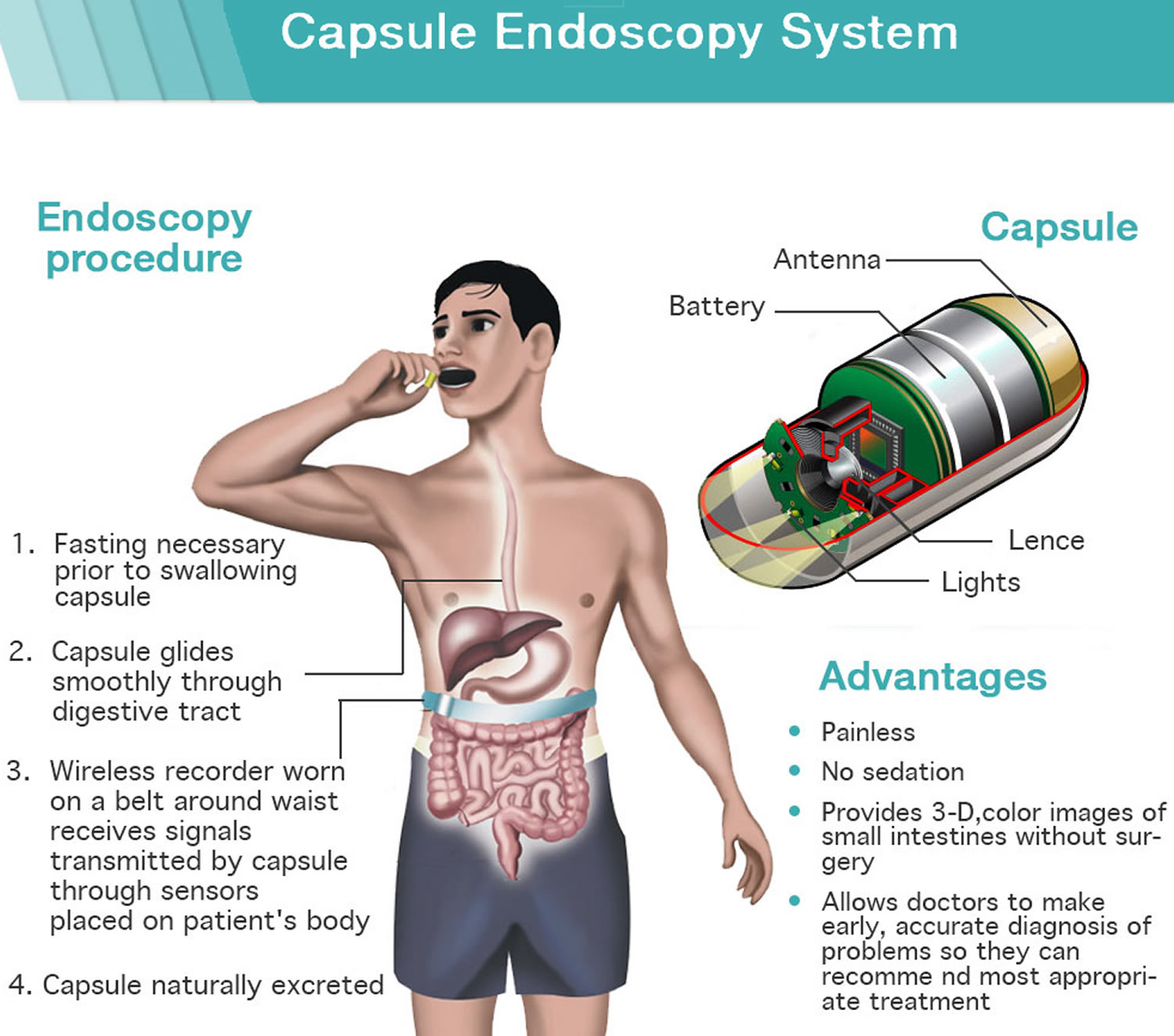
One way to look at this area is to use capsule endoscopy. Capsule endoscopy is a procedure that uses a tiny wireless camera that sits inside a vitamin-size capsule (it’s about the size of a large vitamin pill) you swallow to take pictures of your digestive tract.
To do this, a person swallows a capsule that contains a light source and a tiny camera. Like any other pill, the capsule goes through the stomach and into the small intestine. It travels through the small intestine, which usually takes about 8 hours, and takes thousands of pictures. These pictures are transmitted to a recorder worn around the person’s waist, while he or she goes on with normal daily activities. The pictures can then be downloaded onto a computer, where the doctor can look at them as a video. The camera capsule passes out of the body during a normal bowel movement and is flushed away.
Capsule endoscopy helps doctors see inside your small intestine — an area that isn’t easily reached with more-traditional endoscopy procedures. Capsule endoscopy may help find the source of bleeding, pain, or other symptoms that may be coming from the small intestine. But it’s not useful for looking closely at the colon or other parts of the body. Capsule endoscopy costs a lot, so you will need to find out if your insurance company will cover it before having it.
Traditional endoscopy involves passing a long, flexible tube equipped with a video camera down your throat or through your rectum.
Capsule endoscopy has also been approved for the screening of the colon for colon polyps for those for whom a colonoscopy couldn’t be completed. But how and on whom it will be used is still being determined because better alternatives are available. As technology improves, capsule endoscopy of the colon may be used more in the future.
Capsule endoscopy has also been approved to evaluate the muscular tube that connects your mouth and your stomach (esophagus) to look for abnormal, enlarged veins (varices). It’s rarely used because experience with it is limited and traditional upper endoscopy is widely available.
Figure 4. Capsule endoscopy
Notes: During a capsule endoscopy procedure, you swallow a tiny camera that’s about the size of a large vitamin pill. The capsule contains lights to illuminate your digestive system, a camera to take images and an antenna that sends those images to a recorder you wear on a belt.
Why is capsule endoscopy done
Your doctor might recommend a capsule endoscopy procedure to:
- Find the cause of gastrointestinal bleeding. If you have unexplained bleeding in your digestive tract, capsule endoscopy can help find the cause.
- Diagnose inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis. Capsule endoscopy can reveal areas of inflammation in the small intestine.
- Diagnose cancer. Capsule endoscopy can show tumors in the small intestine or other parts of the digestive tract.
- Diagnose Celiac disease. Capsule endoscopy is sometimes used in diagnosing and monitoring this immune reaction to eating gluten.
- Screen for polyps. People who have inherited syndromes that can cause polyps in the small intestine might occasionally undergo capsule endoscopy.
- Do follow-up testing after X-rays or other imaging tests. If results of an imaging test are unclear or inconclusive, your doctor might recommend a capsule endoscopy to get more information.
Figure 5. Small intestine
Capsule endoscopy risks
Capsule endoscopy is a safe procedure that carries few risks. However, it’s possible for a capsule to become lodged in the digestive tract rather than leaving your body in a bowel movement within several days.
The risk, which is small, might be higher in people who have a condition — such as a tumor, Crohn’s disease or previous surgery in the area — that causes a narrowing (stricture) in the digestive tract. If you have abdominal pain or are at risk of a narrowing of your intestine, your doctor likely will get a CT scan to look for a narrowing before using capsule endoscopy. Even if the imaging study is negative, there’s still a small chance that the capsule could get stuck.
If the capsule hasn’t passed in a bowel movement but isn’t causing signs and symptoms, your doctor might give the capsule more time to leave your body. However, a capsule causing signs and symptoms that indicate bowel obstruction must be removed, either by surgery or through a traditional endoscopy procedure, depending on where the capsule is stuck.
Capsule endoscopy prep
To prepare for your capsule endoscopy, your doctor is likely to ask that you:
- Stop eating and drinking at least 12 hours before the procedure. This will ensure that the camera captures clear images of your digestive tract.
- Stop or delay taking certain medications. To keep medication from interfering with the camera, your doctor might ask you not to take certain medications before the procedure. In other cases, your doctor will want you to take your medication two hours before or after you swallow the camera capsule that contains the camera.
- Plan to take it easy for the day. In most cases, you’ll be able to go about your day after you swallow the camera capsule. But you’ll likely be asked not to do strenuous exercise or heavy lifting. If you have an active job, ask your doctor whether you can go back to work the day of your capsule endoscopy.
In some cases, your doctor may ask you to take a laxative before your capsule endoscopy to flush out your small intestine. This has been shown to improve the quality of the pictures collected by the capsule’s camera.
Follow your doctor’s instructions in preparing for your capsule endoscopy. Failure to follow the directions may mean your capsule endoscopy may need to be rescheduled.
What is the procedure for an capsule endoscopy – what you can expect
During capsule endoscopy
On the day of your capsule endoscopy, your health care team will review the procedure. You might be asked to remove your shirt so that adhesive patches can be attached to your abdomen. Each patch contains an antenna with wires that connect to a recorder. Some devices don’t require the patches.
You wear the recorder on a special belt around your waist. The camera sends images to an antenna on your abdomen, which feeds the data to the recorder. The recorder collects and stores the images.
Once the recorder is connected and ready, you swallow the camera capsule with water. A slippery coating makes it easier to swallow. Once you swallow it, you shouldn’t be able to feel it.
You’ll then go about your day. You can drive, and you might be able to go to work, depending on your job. Your doctor will discuss restrictions, such as avoiding strenuous activity, such as running and jumping.
After the capsule endoscopy
Wait two hours after you swallow the capsule to resume drinking clear liquids. After four hours, you can have a light lunch or a snack unless your doctor tells you otherwise.
The capsule endoscopy procedure is complete after eight hours or when you see the camera capsule in the toilet after a bowel movement, whichever comes first. Remove the patches and the recorder from your body, pack them in a bag and follow your doctor’s instructions for returning the equipment. You can flush the camera capsule down the toilet.
Your body might expel the camera capsule within hours or after several days. Each person’s digestive system is different. If you don’t see the capsule in the toilet within two weeks, contact your doctor. Your doctor might order an X-ray to see if the capsule is still in your body.
Capsule endoscopy results
The camera used in capsule endoscopy takes thousands of color photos as it passes through your digestive tract. The images saved on the recorder are transferred to a computer with special software that strings the images together to create a video. Your doctor watches the video to look for abnormalities within your digestive tract.
It might take a few days to a week or longer to receive the results of your capsule endoscopy. Your doctor will then share the results with you.
Colonoscopy
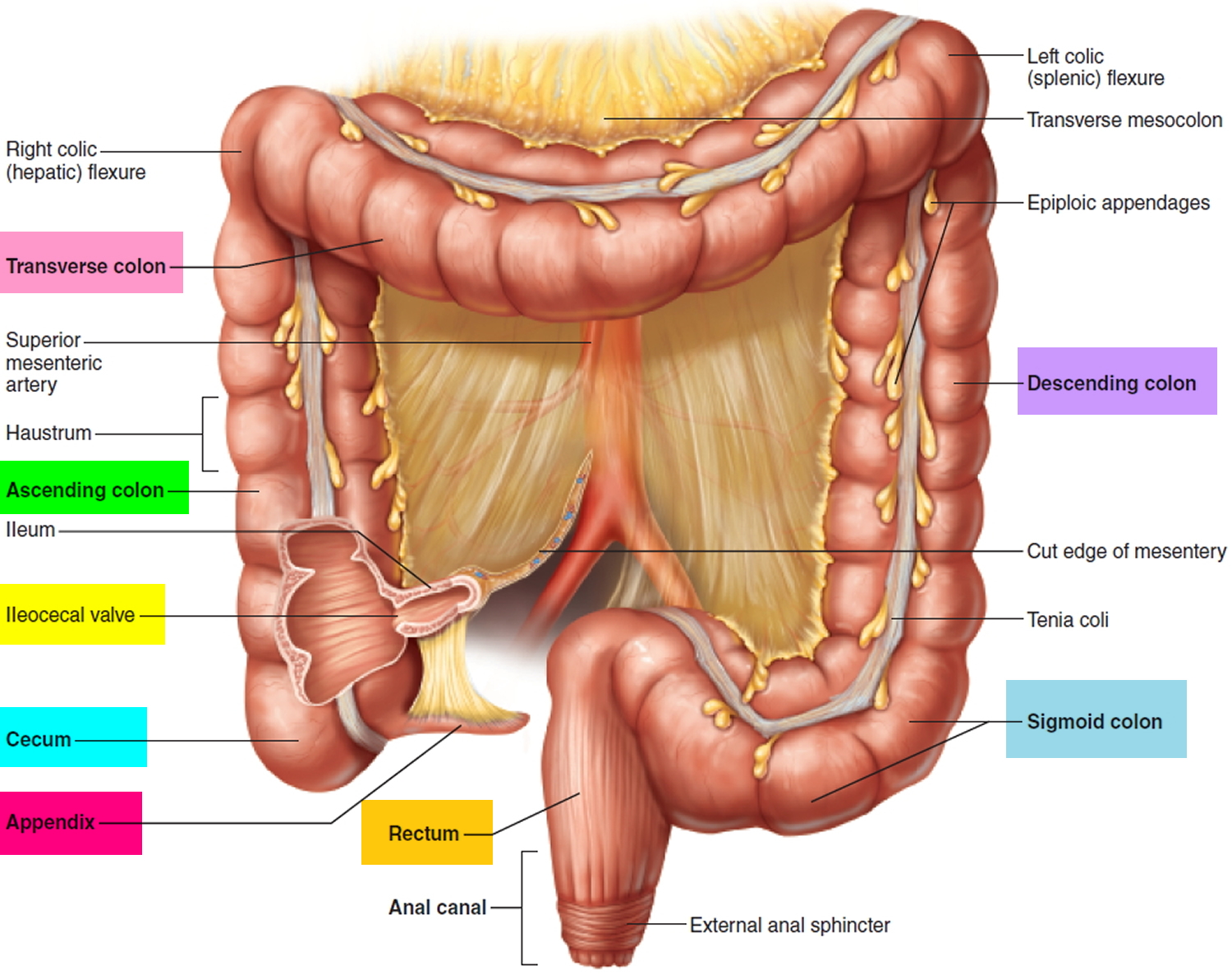
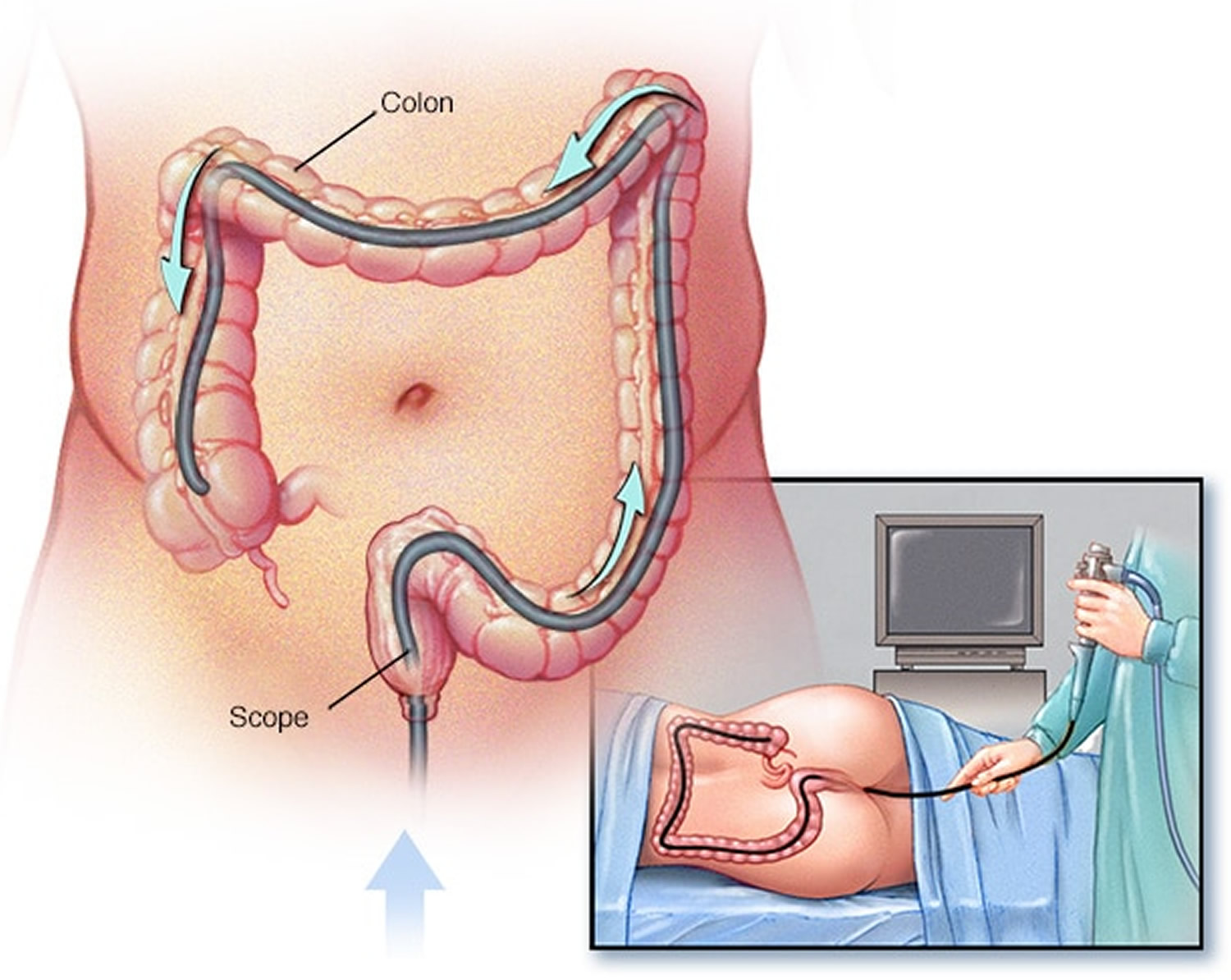
Colonoscopy is a procedure that lets your doctor look inside your entire large intestine (colon) to detect changes or abnormalities in the large intestine and rectum. Doctors (gastroenterologists) use an instrument called colonoscope that have a tiny video camera and light source attached to a long, thin flexible tube, so that the large intestine (colon) can be viewed in detail. During a colonoscopy, a long, flexible tube (colonoscope) is inserted into your rectum/anus. The colonoscope is flexible and can be turned around corners so it can travel along the length of the large bowel. The colonoscopy procedures let your doctor see things such as inflamed tissue, abnormal growths (e.g. polyps, cancers) and ulcers. And if necessary, polyps or other types of abnormal tissue can be removed through the colonoscope during a colonoscopy. Tissue samples (biopsies) can be taken during a colonoscopy as well.
How long does a colonoscopy take?
A colonoscopy typically takes about 30 to 60 minutes.
Why is colonoscopy done
Your doctor may recommend a colonoscopy:
- To look for early signs of cancer in the colon and rectum. It may be part of a routine colon cancer screening, which usually starts at age 50. If you’re age 50 or older and at average risk of colon cancer — you have no colon cancer risk factors other than age — your doctor may recommend a colonoscopy every 10 years or sometimes sooner to screen for colon cancer. Colonoscopy is one option for colon cancer screening. Talk with your doctor about your options.
- To look for causes of unexplained changes in bowel habits
- To evaluate symptoms like abdominal pain, rectal bleeding, and weight loss
- Investigate intestinal signs and symptoms. A colonoscopy can help your doctor explore possible causes of abdominal pain, rectal bleeding, chronic constipation, chronic diarrhea and other intestinal problems.
- Look for more colon polyps. If you have had colon polyps before, your doctor may recommend a follow-up colonoscopy to look for and remove any additional polyps. This is done to reduce your risk of colon cancer.
You will get written bowel prep instructions to follow at home before the colonoscopy procedure. The bowel prep cleans out your intestine so your doctor can see everything clearly. During a colonoscopy, you get medicines to keep you relaxed.
Afterwards, you may feel drowsy, and it is best to arrange somebody to help you get home.
Your doctor may give you a brief report on what they saw, but you probably won’t get full results and further advice until later at a follow up appointment.
Colonoscopy risks and side effects
A colonoscopy poses few risks. Rarely, complications of a colonoscopy may include:
- Adverse reaction to the sedative used during the colonoscopy, including breathing or heart problems
- Bleeding from the site where a tissue sample (biopsy) was taken or a polyp or other abnormal tissue was removed
- A tear in the colon or rectum wall (perforation)
- Severe pain in your abdomen
- Death, although this risk is rare
A study of screening colonoscopies found roughly 4 to 8 serious complications for every 10,000 procedures 1.
Bleeding and perforation are the most common complications from colonoscopy. Most cases of bleeding occur in patients who have polyps removed. The doctor can treat bleeding that happens during the colonoscopy right away.
You may have delayed bleeding up to 2 weeks after the procedure. The doctor can diagnose and treat delayed bleeding with a repeat colonoscopy. The doctor may need to treat perforation with surgery.
After discussing the risks of colonoscopy with you, your doctor will ask you to sign a consent form authorizing the procedure.
Seek Care Right Away
If you have any of the following symptoms after a colonoscopy, seek medical care right away:
- severe pain in your abdomen
- fever
- bloody bowel movements that do not get better
- bleeding from the anus that does not stop
- dizziness
- weakness
Colonoscopy prep
If you are having a colonoscopy, there are a number of steps that need to be followed to get the best result.
Before a colonoscopy, you’ll need to clean out (empty) your colon. Any fecal residue in your colon may obscure the view of your colon and rectum during the colonoscopy procedure.
The preparations vary between clinics but the aim is to clear the colon of feces so the doctor can get the best view on examination.
Arrange for a ride home
For safety reasons, you can’t drive for 24 hours after the procedure, as the sedatives or anesthesia need time to wear off. You will need to make plans for getting a ride home after the procedure.
Colonoscopy prep instructions
You should talk with your doctor about any health problems you have and all prescribed and over-the-counter medicines, vitamins, and supplements you take, including:
- arthritis medicines
- aspirin or medicines that contain aspirin
- blood thinners
- diabetes medicines
- nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen
- vitamins that contain iron or iron supplements
Colonoscopy Diet
Your doctor will give you written bowel prep instructions to follow at home before the procedure so that little or no stool remains in your intestine. A complete bowel prep lets you pass stool that is clear and liquid. Stool inside your intestine can prevent your doctor from clearly seeing the lining.
Follow a special diet the day before the exam. Typically, you won’t be able to eat solid food the day before the exam. Drinks may be limited to clear liquids — plain water, tea and coffee without milk or cream, broth, and carbonated beverages. Avoid red liquids, which can be confused with blood during the colonoscopy. You may not be able to eat or drink anything after midnight the night before the exam.
You may need to follow a clear liquid diet for 1 to 3 days before the procedure. You should avoid red and purple-colored drinks or gelatin. The instructions will include details about when to start and stop the clear liquid diet. In most cases, you may drink or eat the following:
- fat-free bouillon or broth
- gelatin in flavors such as lemon, lime, or orange
- plain coffee or tea, without cream or milk
- sports drinks in flavors such as lemon, lime, or orange
- strained fruit juice, such as apple or white grape—avoid orange juice
- water
To empty your colon
Different bowel preps may contain different combinations of laxatives—pills that you swallow or powders that you dissolve in water or clear liquids. Some people will need to drink a large amount, often a gallon, of liquid laxative over a scheduled amount of time—most often the night before and the morning of the procedure. Your doctor may also prescribe an enema.
The bowel prep will cause diarrhea, so you should stay close to a bathroom. You may find this part of the bowel prep hard; however, finishing the prep is very important. Call a health care professional if you have side effects that keep you from finishing the prep.
Your doctor will tell you how long before the procedure you should have nothing by mouth.
- The day before the colonoscopy, you may be asked to drink a bowel preparation, a laxative. This is a flavored powder that is mixed with water. It causes diarrhea to empty the colon. Your doctor will usually recommend you take a laxative, in either pill form or liquid form. You may be instructed to take the laxative the night before your colonoscopy, or you may be asked to use the laxative both the night before and the morning of the procedure. It’s best to do the bowel preparation at home. The area around your anus may become irritated from diarrhea. Showering, and using moist wipes instead of toilet paper, may ease this discomfort. It is important to drink only clear fluids on the day before, and not eat solid foods or dairy products like milk. You will be allowed to have fluids like water, clear fruit juice, clear carbonated drinks and clear soup. You will probably be told to have no fluids in the 6 hours before the colonoscopy.
- Use an enema kit. In some cases, you may need to use an over-the-counter enema kit — either the night before the exam or a few hours before the exam — to empty your colon. This is generally only effective in emptying the lower colon and is usually not recommended as a primary way of emptying your colon.
- If you take regular medication, talk to your doctor. Some medications should be taken and some can be delayed. It is particularly important to talk to your doctor if you take blood-thinning medications.
- Adjust your medications. Remind your doctor of your medications at least a week before the exam — especially if you have diabetes, high blood pressure or heart problems or if you take medications or supplements that contain iron.
- Also tell your doctor if you take aspirin or other medications that thin the blood, such as warfarin (Coumadin, Jantoven); newer anticoagulants, such as dabigatran (Pradaxa) or rivaroxaban (Xarelto), used to reduce risk of blot clots or stroke; or heart medications that affect platelets, such as clopidogrel (Plavix). You may need to adjust your dosages or stop taking the medications temporarily.
Split Dose Regimen for colonoscopy preparation
“Splitting” implies that roughly half of the bowel cleansing dose is given on the day of the colonoscopy. Overwhelmingly consistent data show superior efficacy with a split dose compared with the traditional regimen of administering the preparation the day before the procedure 2. Split dosing leads to higher adenoma detection rates 3. Four guidelines have endorsed split dosing of preparations for colonoscopy 4, 5, 6, 7.
To make bowel preparation more tolerable, many doctors recommend splitting the dose of bowel preparation. This regimen may not be possible if your colonoscopy is scheduled for early in the morning, because you should consume the morning dose four to six hours prior to the procedure.
If your procedure is scheduled at a time that allows you to split the dose, take the recommended amount of the bowel cleansing liquid the night before the exam, and the remainder in the morning before the test. Depending on the type of preparation, your doctor may recommend splitting the dose 1-to-1 or 3-to-1.
The biggest reason for poor colonoscopy preparation is people’s distaste for having to drink large quantities of bowel cleaning solution. The most common colonoscopy preparation calls for drinking 1 gallon (4 liters) of a polyethylene glycol solution. Some studies have shown that more than a third of people don’t complete the full preparation.
Studies have shown that the split-dose approach not only is more tolerable, but also does a better job of cleaning the colon. Better cleaning will lead to better results. One study found that doctors detected more benign tumors (adenomas) in people who prepared with split doses than in people who prepared with single doses.
Cleaning as much waste material as possible from your large intestine (colon) is crucial to a successful colonoscopy exam. Poor colonoscopy preparation can keep your doctor from finding polyps, tumors and other problems. It also increases the length of the exam and the risk of complications. In many cases, the exam has to be redone.
Ask your doctor about split-dose preparation for your next colonoscopy.
During the colonoscopy procedure
A doctor performs a colonoscopy in a hospital or an outpatient center. The colonoscopy procedure is painless and lasts about 30 to 60 minutes. Most people have a mild anesthetic/sedation and can remember nothing or very little. A health care professional will place an intravenous (IV) needle in a vein in your arm or hand to give you sedatives, anesthesia, or pain medicine, so you won’t be aware or feel pain during the procedure. The health care staff will check your vital signs and keep you as comfortable as possible.
During a colonoscopy, you’ll wear a gown, but likely nothing else. Sedation is usually recommended. Sometimes a mild sedative is given in pill form. In other cases, the sedative is combined with an intravenous pain medication to minimize any discomfort.
For the procedure, you’ll lie on your side on the exam table, usually with your knees drawn toward your chest while the doctor inserts a colonoscope through your anus and into your rectum and colon. The scope inflates your large intestine with air for a better view.
The colonoscope — which is long enough to reach the entire length of your colon — contains a light and a tube (channel) that allows the doctor to pump air or carbon dioxide into your colon. The air or carbon dioxide inflates the colon, which provides a better view of the lining of the colon.
When the colonoscope is moved or air is introduced, you may feel abdominal cramping or the urge to have a bowel movement.
The colonoscope also contains a tiny video camera at its tip. The camera sends images to an external monitor so that the doctor can study the inside of your colon.
The doctor can also insert instruments through the channel to take tissue samples (biopsies) or remove polyps or other areas of abnormal tissue.
The doctor may move you several times on the table to adjust the scope for better viewing. Once the colonoscope reaches the opening to your small intestine, the doctor slowly removes the colonoscope and examines the lining of your large intestine again.
During the procedure, the doctor may remove polyps and will send them to a lab for testing. You will not feel the polyp removal. Colon polyps are common in adults and are harmless in most cases. However, most colon cancer begins as a polyp, so removing polyps early helps to prevent cancer.
If your doctor finds abnormal tissue, he or she may perform a biopsy. You won’t feel the biopsy.
Colonoscopy recovery
After the colonoscopy procedure, it takes about an hour for you to begin to recover from the sedative. You’ll need someone to take you home because it can take up to a day for the full effects of the sedative to wear off. Don’t drive or make important decisions or go back to work for the rest of the day.
If your doctor removed a polyp during your colonoscopy, you may be advised to eat a special diet temporarily.
You may feel bloated or pass gas for a few hours after the exam, as you clear the air from your colon. Walking may help relieve any discomfort.
You may also notice a small amount of blood with your first bowel movement after the exam. Usually this isn’t cause for alarm. Consult your doctor if you continue to pass blood or blood clots or if you have persistent abdominal pain or a fever. While unlikely, this may occur immediately or in the first few days after the procedure, but may be delayed for up to one to two weeks.
Figure 6. Large intestine
Figure 7. Colonoscopy
What should I expect after a colonoscopy?
After a colonoscopy, you can expect the following:
- The anesthesia takes time to wear off completely. You’ll stay at the hospital or outpatient center for 1 to 2 hours after the procedure.
- You may feel cramping in your abdomen or bloating during the first hour after the procedure.
- After the procedure, you—or a friend or family member—will receive instructions on how to care for yourself after the procedure. You should follow all instructions.
- You’ll need your pre-arranged ride home, since you won’t be able to drive after the procedure.
- You should expect a full recovery and return to your normal diet by the next day.
After the sedatives or anesthesia wear off, your doctor may share what was found during the procedure with you or, if you choose, with a friend or family member.
If the doctor removed polyps or performed a biopsy, you may have light bleeding from your anus. This bleeding is normal. A pathologist will examine the biopsy tissue, and results take a few days or longer to come back. A health care professional will call you or schedule an appointment to go over the results.
Colonoscopy Results
Your doctor will review the results of the colonoscopy and then share the results with you.
Negative result
A colonoscopy is considered negative if the doctor doesn’t find any abnormalities in the colon.
Your doctor may recommend that you have another colonoscopy:
- In 10 years, if you’re at average risk of colon cancer — you have no colon cancer risk factors other than age
- In five years, if you have a history of polyps in previous colonoscopy procedures
- In one year, if there was residual stool in the colon that prevented complete examination of your colon
Positive result
A colonoscopy is considered positive if the doctor finds any polyps or abnormal tissue in the colon.
Most polyps aren’t cancerous, but some can be precancerous. Polyps removed during colonoscopy are sent to a laboratory for analysis to determine whether they are cancerous, precancerous or noncancerous.
Depending on the size and number of polyps, you may need to follow a more rigorous surveillance schedule in the future to look for more polyps.
If your doctor finds one or two polyps less than 0.4 inch (1 centimeter) in diameter, he or she may recommend a repeat colonoscopy in five to 10 years, depending on your other risk factors for colon cancer.
Your doctor will recommend another colonoscopy sooner if you have:
- More than two polyps
- A large polyp — larger than 0.4 inch (1 centimeter)
- Polyps and also residual stool in the colon that prevents complete examination of the colon
- Polyps with certain cell characteristics that indicate a higher risk of future cancer
- Cancerous polyps
If you have a polyp or other abnormal tissue that couldn’t be removed during the colonoscopy, your doctor may recommend a repeat exam with a gastroenterologist who has special expertise in removing large polyps, or surgery.
Problems with your exam
If your doctor is concerned about the quality of the view through the scope, he or she may recommend a repeat colonoscopy or a shorter time until your next colonoscopy. If your doctor wasn’t able to advance the scope through your entire colon, a barium enema or virtual colonoscopy may be recommended to examine the rest of your colon.
Virtual endoscopy
Virtual endoscopy is really an imaging test, not an endoscopy procedure per se. Virtual endoscopy uses a special CT scan to look at the inside surfaces of organs such as the lungs (virtual bronchoscopy) or colon (virtual colonoscopy or CT colonography).
Patients have this procedure just as they would any other CT scan — they lie still on a table while a large ring (the CT scanner) passes over the part of the body being imaged.
Unlike the usual CT scans, which make pictures in 2 dimensions, virtual endoscopy uses a computer to combine many images to create a 3-dimensional (3-D) picture. Doctors can even use the images to create a black and white “fly-through” view on the screen, which looks a lot like it would if they were doing an actual endoscopy.
Virtual endoscopy has some advantages over standard endoscopy — nothing is put into your body and no drugs are needed for the test. The doctor can change the angle or magnify the image, which can help with diagnosis.
But there are some disadvantages, too. Virtual endoscopy does show good detail, but it’s not quite as good at showing fine surface detail as standard endoscopy. For example, it can’t show color differences. Virtual endoscopy also exposes the patient to about the same amount of radiation as a standard CT. And because nothing is put into the body, the doctor can’t take biopsy samples or remove growths. This means that if something abnormal is found, the patient may still need a standard endoscopy. To get good pictures on a virtual colonoscopy, the patient must still take medicines (laxatives and/or enemas) to clean out the colon.
Virtual endoscopy is a fairly new procedure, and doctors aren’t yet sure how best to use it. It will likely be used more in the future as the technology improves.
- Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(23):2576–2594.[↩]
- Menard C, Barkun A, Martel M et al. A meta-analysis of colon cleansing with PEG compared to other bowel preparations. Gastrointest Endosc (2014). In press.[↩]
- Jover R, Zapater P, Polania E et al. Modifiable endoscopic factors that influence the adenoma detection rate in colorectal cancer screening colonoscopies. Gastrointest Endosc 2013;77:381–389.[↩]
- Wexner SD, Beck DE, Baron TH et al. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Gastrointest Endosc 2006;63:894–909.[↩]
- Lieberman DA, Rex DK, Winawer SJ et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844–857.[↩]
- Rex DK, Johnson DA, Anderson JC et al. American College of Gastroenterology guidelines for colorectal cancer screening 2008. Am J Gastroenterol 2009;104:739–750.[↩]
- Hassan C, Bretthauer M, Kaminski MF et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013;45:142–150.[↩]