Contents
- What is amniotic fluid
- Amniotic fluid test
- Low amniotic fluid
- Too much amniotic fluid
- Amniotic fluid embolism
What is amniotic fluid
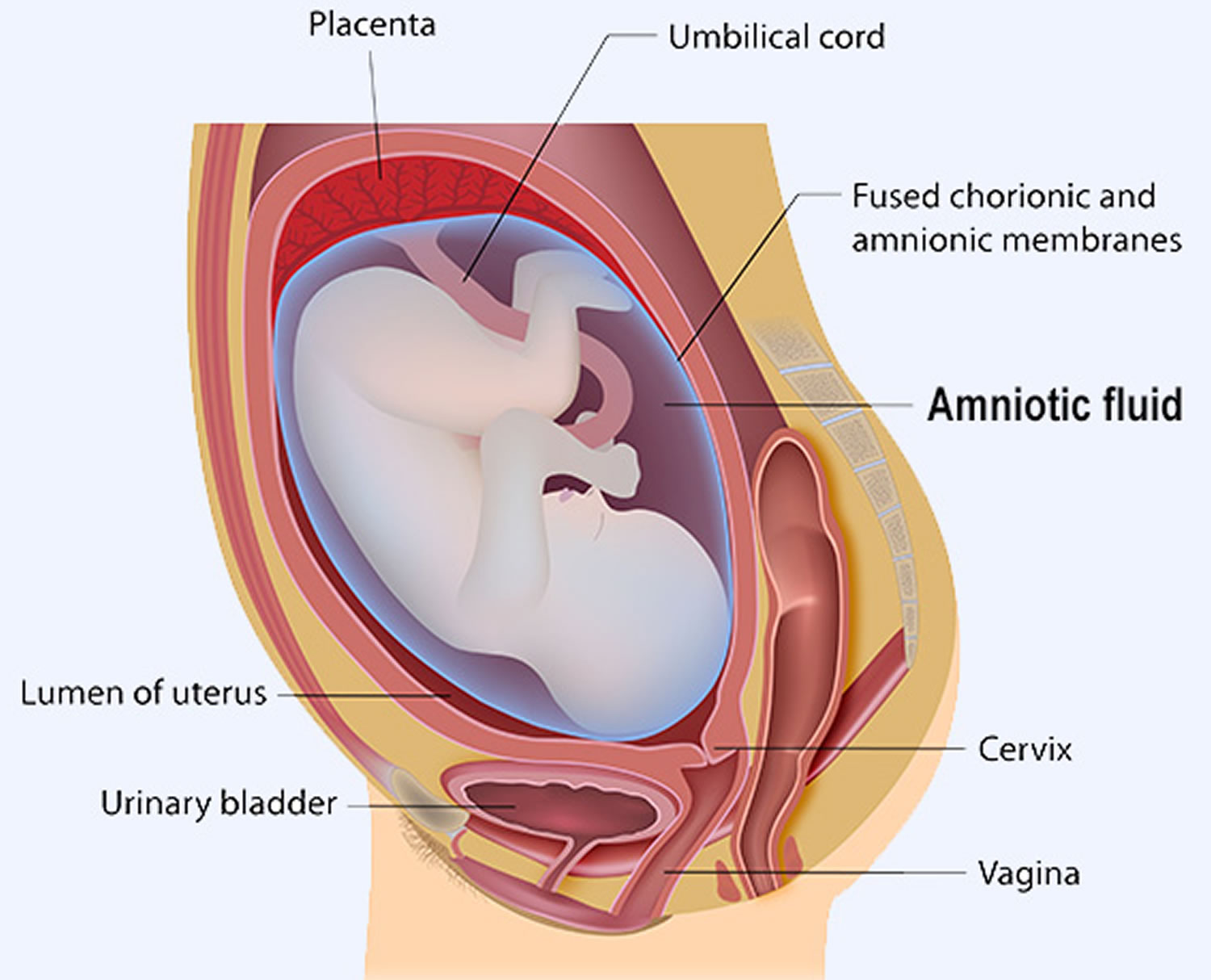
Amniotic fluid is is a clear, slightly yellowish liquid that surrounds, protects and nourishes a growing baby in the uterus during pregnancy. Amniotic fluid allows a fetus to move relatively freely within the uterus, keeps the umbilical cord from being compressed, and helps maintain a stable temperature. Amniotic fluid is contained within the amniotic sac and is normally a clear to pale yellow liquid that contains proteins, nutrients, hormones, fetal cells, fetal urine and antibodies.
Amniotic fluid begins forming one to two weeks after conception and increases in volume until there is about a quart (800 mL) at 36 weeks of pregnancy. Amniotic fluid is absorbed and continually renewed. The amniotic fluid constantly moves (circulates) as the baby swallows and “inhales” the fluid, and then releases it.
The fetus swallows and inhales amniotic fluid and releases it as urine. The amount of amniotic fluid increases over time and is constantly being absorbed and renewed. During this circulation process, cells from various parts of the fetus’s body slough off into the fluid, and chemicals produced by the fetus are present as well. This is why samples of the amniotic fluid can be tested to evaluate fetal health. Several laboratory tests may be performed on the amniotic fluid to help identify various conditions and diseases.
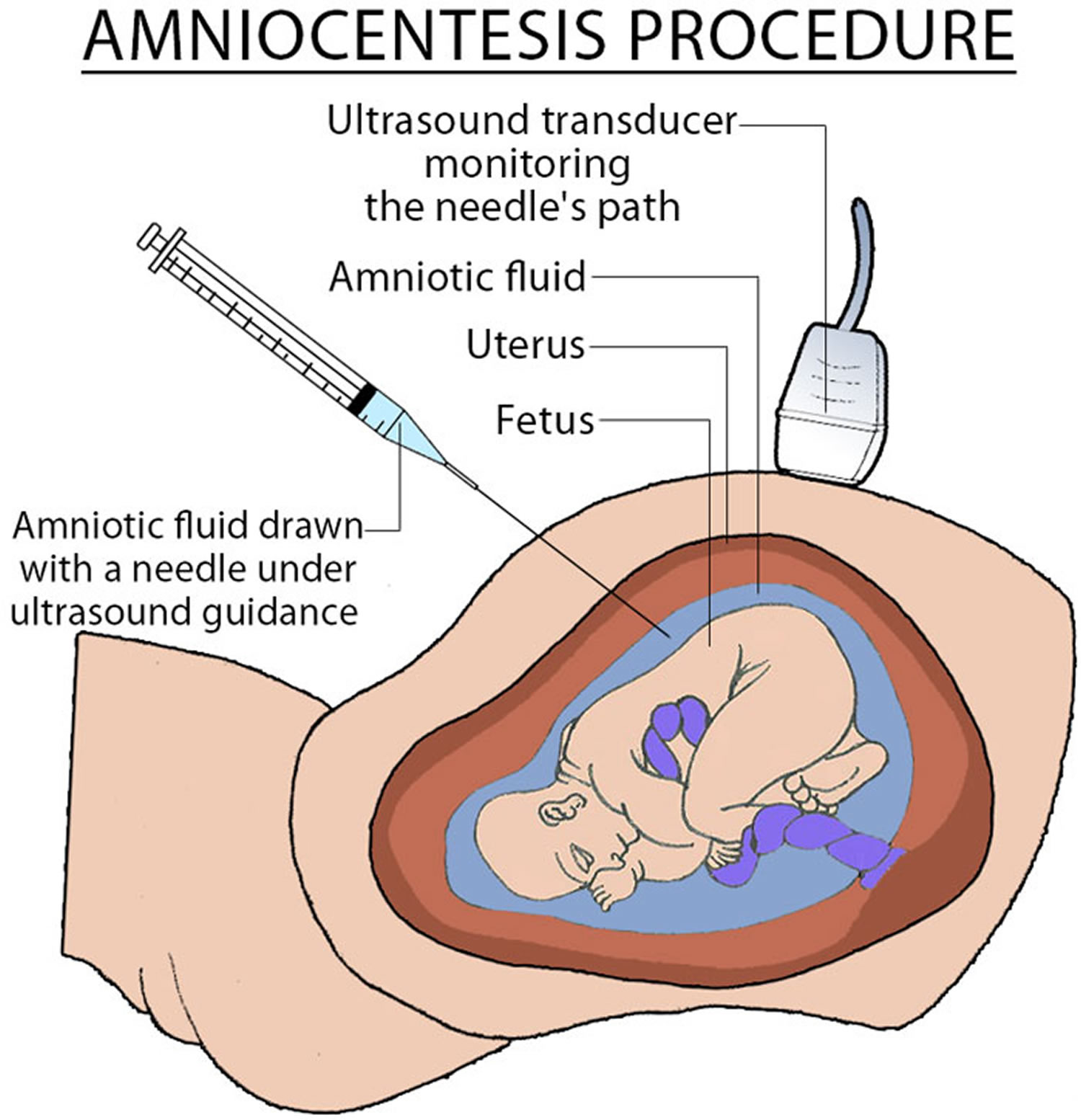
Amniocentesis is the removal of a small amount of fluid (about an ounce) from the sac that surrounds a developing fetus using a needle and syringe. Before the procedure, ultrasound is used to find the position of the fetus in the womb and is continuously used throughout the procedure to ensure that the needle remains safely away from the baby. Prior to inserting the needle, the skin on the mother’s abdomen is cleaned and sometimes a local anesthetic is applied to the surface of the skin or injected into the skin.
During the procedure, the needle is carefully inserted through the walls of the abdomen and the uterus so that it just enters the thin-walled sac of amniotic fluid that surrounds the developing fetus. A small amount of amniotic fluid is discarded to ensure that no maternal contamination is present within the needle, and then the fluid is drawn up into the syringe and sent to a laboratory for analysis. Depending on the specific tests being performed, results may be available within a few days to up to 4 weeks or, in the case of fetal lung maturity testing, within a few hours.
There is a slight risk with amniocentesis that the needle inserted into the amniotic sac might puncture the baby, cause a small amount of amniotic fluid leakage following the procedure, cause a uterine infection, or, in rare cases, cause a miscarriage. The risk for a miscarriage associated with this procedure is considered to be 1/300 to 1/500, which is much lower than a woman’s risk (at any age) to have a baby with a chromosomal abnormality.
Recently, advances in testing technology and improved prenatal screening options, specifically non-invasive prenatal screening, has led to a decrease in the use of diagnostic tests such as amniocentesis. Non-invasive prenatal screening screens a blood sample from a pregnant woman for fragments of cell-free DNA (cfDNA) produced by the placenta. It typically screens for certain chromosomal abnormalities, including Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and Patau syndrome (trisomy 13), and it can be performed as early as the 10th week of pregnancy. However, at this time, “invasive” diagnostic tests such as amniocentesis and chorionic villus sampling (CVS) are still needed to confirm the results of a positive prenatal screening test or to test for conditions not covered by the screening test.
Figure 1. Amniotic fluid
Figure 2. Amniocentesis
How does amniotic fluid keep your baby healthy?
During pregnancy, your uterus is filled with amniotic fluid. Here’s what the fluid does:
- Cushions and protects your baby from injury by cushioning sudden blows or movements
- Keeps a steady temperature around your baby, protecting from heat loss
- Helps your baby’s lungs grow and develop because your baby breathes in the fluid
- Helps your baby’s digestive system develop because your baby swallows the fluid
- Helps your baby’s muscles and bones develop because your baby can move around in the fluid
- Keeps the umbilical cord (the cord that carries food and oxygen from the placenta to your baby) from being squeezed
The amniotic sac (bag) inside the uterus holds your growing baby. It is filled with amniotic fluid. This sac forms about 12 days after getting pregnant.
In the early weeks of pregnancy, the amniotic fluid is mostly water that comes from your body. After about 20 weeks of pregnancy, your baby’s urine makes up most of the fluid. Amniotic fluid also contains nutrients, hormones (chemicals made by the body) and antibodies (cells in the body that fight off infection).
Amniotic fluid levels
The amount of amniotic fluid increases until about 36 weeks of pregnancy. At that time, it makes up about 1 quart (averages 800 mL). After that, the amount of amniotic fluid usually begins to decrease. About 600 mL of amniotic fluid surrounds the baby at full term (40 weeks gestation).
Amniotic fluid volume undergoes characteristic changes with gestation. It progressively rises.
- 10 weeks gestation it is about 10 to 20 mL
- at 16 weeks gestation ~250 mL
- at 33 weeks gestation ~800 mL
- at 38-39 weeks reaches a plateau of ~1000 mL
- finally decreases at 40 weeks to ~600-800 mL
Amniotic fluid rate of change
At 8 weeks the amniotic fluid volume increases by ~10 mL/week, at 13 weeks the amniotic fluid volume increases by 25 mL/week and reaches a maximum rate of 60 mL/week at 21 weeks gestation. The weekly volume increment then decreases and reaches zero at about 33 weeks of gestation at which point the mean amniotic fluid volume reaches its peak. After term the amniotic fluid volume declines at a rate of ~8% per week. During the first half of pregnancy, amniotic fluid volume is closely correlated with fetal weight. The ratio of amniotic fluid to fetal volume increases until about 36 weeks gestation and then appears to decline.
Sometimes you can have too little or too much amniotic fluid. Too little fluid is called oligohydramnios. Too much fluid is called polyhydramnios. Either one can cause problems for a pregnant woman and her baby. Even with these conditions, though, most babies are born healthy.
Abnormal amounts of amniotic fluid may cause your health care provider to watch your pregnancy more carefully. Removing a sample of the fluid through amniocentesis can provide information about the sex, health, and development of the fetus.
What does amniotic fluid look like
Normal amniotic fluid is clear or tinted yellow.
Amniotic fluid that looks green or brown usually means that the baby has passed his first bowel movement (meconium) while in the womb. (Usually, the baby has his first bowel movement after birth.)
If the baby passes meconium in the womb, it can get into his lungs through the amniotic fluid. This can cause serious breathing problems, called meconium aspiration syndrome, especially if the amniotic fluid is thick.
Some babies with meconium in the amniotic fluid may need treatment right away after birth to prevent breathing problems. Babies who appear healthy at birth may not need treatment, even if the amniotic fluid has meconium.
Amniotic fluid test
Amniotic fluid analysis involves a variety of tests that can be performed to evaluate the health of a fetus.
Amniotic fluid analysis may be used for several different purposes and the specific testing that is done depends on the reason for testing. The following list includes some of the more common ways that this analysis may be used for prenatal diagnosis:
To detect chromosomal abnormalities or genetic disorders
The American College of Obstetricians and Gynecologists recommends that all pregnant women should be given the option of having amniocentesis performed to detect chromosome abnormalities. A healthcare practitioner can help a pregnant woman weigh the pros and cons.
- Chromosome analysis—performed as either a cytogenetics test that can also be called karyotyping or as a chromosomal microarray analysis. Both methods detect chromosome abnormalities associated with a variety of chromosome disorders. The testing evaluates the 22 paired chromosomes and the sex chromosomes (X, Y) in cells from the sample of amniotic fluid and can be used to diagnose a variety of disorders, including:
- Down syndrome (Trisomy 21), caused by an extra chromosome 21 in all or most cells of the body
- Edwards syndrome (Trisomy 18), caused by an extra chromosome 18
- Patau syndrome (Trisomy 13), caused by an extra chromosome 13
- Klinefelter syndrome, the most common sex chromosome abnormality in males; caused by an extra X chromosome
- Turner syndrome, caused by missing one X chromosome in females
- Due to the nature of this type of testing, chromosome analysis can also definitively determine the sex of a fetus.
- Genetic testing, also called molecular testing, evaluates fetal DNA to look for specific gene mutations that are associated with specific genetic disorders. Molecular testing may be offered because of a family history of a specific inherited disorder or because of specific fetal ultrasound abnormalities that are known to have a genetic cause.
To detect open neural tube defects, such as spina bifida or anencephaly, or open abdominal wall defects
For example:
- AFP (alpha-fetoprotein) is elevated in amniotic fluid with neural tube defects.
- Acetylcholinesterase is increased with neural tube defects and other anatomic abnormalities.
To detect Rh and other blood type incompatibilities
When a mother has been previously exposed through prior pregnancies or blood transfusions to “foreign” red blood cells (RBCs), she may develop antibodies to the proteins present on the outer layer of the foreign red cells (antigens). If the antigens are present on the red blood cells of the fetus (inherited from the father), then the mother’s red blood cell antibodies can cross the placenta and bind to and destroy the fetus’s red blood cells, causing hemolytic anemia. An affected fetus can develop hemolytic disease of the newborn. One of the most commonly encountered incompatibilities are due to ABO and Rh group differences, but there are many other blood types that may also cause this problem.
Typically, if a fetus has been tested and is known to have Rh or blood type incompatibility with the mother, the fetus is monitored non-invasively using imaging scans. However, if the fetus shows signs that a blood transfusion is needed, then tests for bilirubin (also known as delta OD450) may be performed to help evaluate the severity of the hemolytic anemia. This is an invasive test and is not performed routinely. Bilirubin is an orange-yellow pigment, a waste product primarily produced by the normal breakdown of heme. Heme is a component of hemoglobin, which is found in red blood cells (RBCs).
To detect fetal infections
There are a few tests that can be performed on amniotic fluid to detect infections that are passed from mother to baby during pregnancy (congenital infections). Some of these infections may have serious consequences for the developing fetus. A few examples include tests for:
- TORCH: toxoplasmosis, rubella, cytomegalovirus (CMV), herpes simplex virus (HSV)
- Parvovirus B19
- Cultures for bacterial infections
To evaluate fetal lung maturity
Recent guidelines from American College of Obstetricians and Gynecologists no longer recommends routine use of fetal lung maturity in clinical decision-making. However, testing to evaluate fetal lung maturity may be performed in select situations, for example, if a woman is very unsure of her dates and is at an increased risk for premature delivery or there is a sudden medical need for a preterm delivery. Various substances are measured in amniotic fluid (lamellar body count, phosphatidylglycerol, lecithin/sphingomyelin (L/S) ratio). The goal of the testing is to determine the risk of a life-threatening condition called neonatal respiratory distress syndrome.
When is amniotic fluid test ordered?
Genetic amniotic fluid analysis may be offered as part of second trimester prenatal testing and is performed primarily between 15 and 20 weeks of pregnancy. In particular, testing is recommended when:
- A woman has an abnormality on a first trimester Down syndrome screen, non-invasive prenatal screening (NIPS) using cell-free DNA, or second trimester maternal serum screen
- A woman had a previous child or pregnancy with a chromosomal abnormality or genetic disorder
- A parent has an inherited disorder or both parents have a known gene for an inherited disorder
- An abnormality has been detected on a fetal ultrasound
Testing may be ordered to monitor bilirubin levels when there is a known Rh or blood type incompatibility between the fetus and mother and monitoring of the fetus indicates a blood transfusion may be needed.
An amniotic fluid analysis may be performed in late pregnancy to diagnose a fetal infection.
Fetal lung maturity amniotic fluid testing may be ordered woman is unsure of her dates and is at an increased risk for premature delivery or there is a sudden medical need for a preterm delivery.
What does amniotic fluid test result mean?
Genetic tests, chromosome analysis and testing for neural tube defects
Because these results can be complex, women should discuss their test results not only with their healthcare practitioner but also ideally with someone who has expertise in genetics, such as a genetic counselor or maternal-fetal medicine specialist.
If a chromosomal abnormality or a genetic disorder is detected by diagnostic testing, then the baby likely will have the associated condition. However, many chromosomal disorders have a range of severity, and simply knowing a diagnosis does not help predict the condition’s severity or prognosis. It should also be noted that not every genetic disorder or chromosomal abnormality will be detected with this testing.
If an increased alpha fetoprotein (AFP) suggests an abnormality, such as an open neural tube defect or abdominal wall defect, then additional testing and imaging may be performed to determine the severity of the condition and the best course of action.
Rh or other blood type incompatibility
Increasing bilirubin levels in the amniotic fluid in the case of fetal-maternal blood type incompatibility indicate increasing destruction of red blood cells and the likelihood that the fetus will have hemolytic disease of the newborn, requiring treatment before or after birth, depending on the severity.
Fetal infections
Results of cultures of the amniotic fluid as well as tests for various viruses will indicate whether an infection is present.
Fetal lung maturity
Although rarely used these days, if testing indicates that the a fetus’s lungs have not yet matured, then a healthcare practitioner may take measures to attempt delaying delivery, use medications to promote lung maturity, or when necessary to begin treating the baby immediately after birth.
Maternal or fetal blood contamination and stool from the fetus (meconium) in the amniotic fluid can affect some chemical test results.
An alternative to amniotic fluid analysis for chromosomal analysis and genetic testing is chorionic villus sampling (CVS), which can be performed earlier, between 10 and 12 weeks of pregnancy. This first trimester procedure collects a small placenta tissue sample at the site of implantation and carries about the same risks as amniocentesis when performed by an experienced practitioner. CVS cannot, however, detect neural tube defects or abdominal wall defects, and occasionally may provide a chromosomal result that is representative of the placenta, but not the fetus (confined placental mosaicism).
Can disorders detected through amniotic fluid analysis be prevented?
- Genetic and chromosomal abnormalities cannot be prevented, only diagnosed.
- The risk for open neural tube birth defects can be minimized by a woman getting plenty of folic acid prior to and during pregnancy.
- The number of women with Rh sensitization has greatly decreased since injections of Rh immune globulin to prevent the formation of Rh antibodies became routine in prenatal and postnatal care.
Should every pregnant woman have amniotic fluid analysis?
This is a highly personal decision, and one best made by a woman and her healthcare provider working together. The American College of Obstetricians and Gynecologists recommends that all pregnant women be given the option of having amniocentesis performed. Although the associated risk is low, it must be weighed against the desire for information that would be gained by testing. Speaking with a genetic counselor may also be helpful in learning more about the various types of testing available and what to expect from the information that can be learned through them.
Low amniotic fluid
Too little amniotic fluid is also called oligohydramnios, which is described as decreased amniotic fluid volume relative to gestational age. Too little amniotic fluid (oligohydramnios) occurs in approximately 11% of all pregnancies. Too little amniotic fluid (oligohydramnios) can happen at any time during pregnancy, but it’s most common in the last trimester (last 3 months). It happens in about 12 out of 100 (12 percent) women whose pregnancies last about 2 weeks past their due dates. This is because the amount of amniotic fluid usually decreases by that time.
Low amniotic fluid is most commonly caused by leaking of amniotic fluid due to a tear in the amniotic sac (premature rupture of the membranes), but it can also be caused by an abnormality of the fetal kidneys and/or urinary tract. If the fetal kidneys are not functioning normally, they will not produce enough urine to replace what the fetus swallows, and if there is a blockage of the urinary tract, it can prevent the urine from cycling back out to the amniotic fluid sac. Pregnancies affected by oligohydramnios are at higher risk for adverse fetal outcomes and should be monitored with care.
If you notice that you are leaking fluid from your vagina, tell your health care provider. It may be a sign of oligohydramnios. Your provider watches out for other signs, such as if you’re not gaining enough weight or if the baby isn’t growing as fast as he should.
Your health care provider uses ultrasound to measure the amount of amniotic fluid.
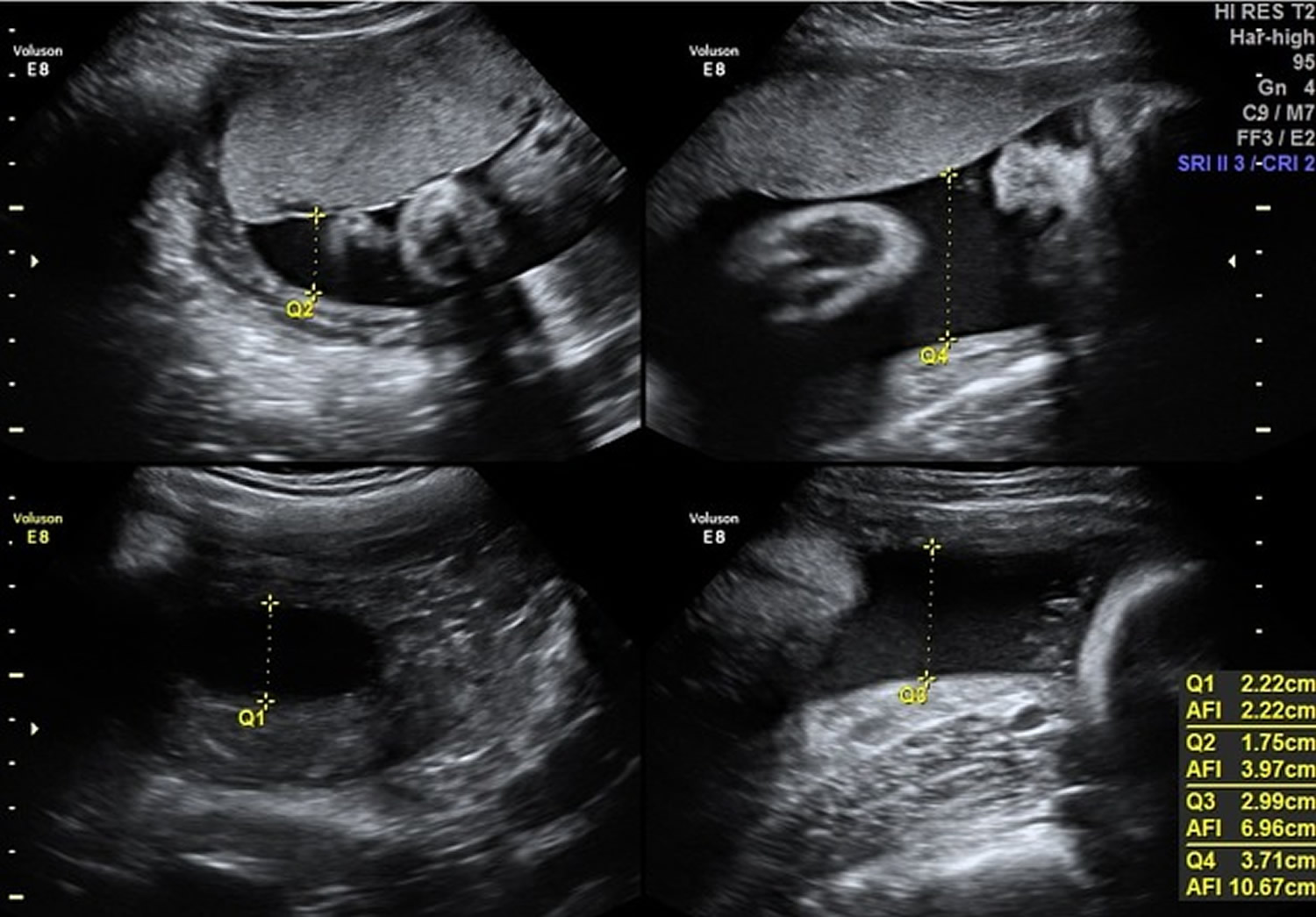
There are two ways to measure the amniotic fluid: amniotic fluid index (AFI) and maximum vertical pocket (MPV).
The amniotic fluid index (AFI) checks how deep the amniotic fluid is in four areas of your uterus. These amounts are then added up. If your amniotic fluid index (AFI) is less than 5 centimeters, you have oligohydramnios.
The normal range for amniotic fluid volumes varies with gestational age. Typical values include:
- Amniotic fluid index (AFI) between 8-18 cm is considered normal; median AFI level is ~14 cm from week 20 to week 35, after which the amniotic fluid volume begins to reduce
- Amniotic fluid index (AFI) <5 cm is considered as oligohydramnios
value changes with age: the 5th percentile for gestational ages is most often taken as the cutoff value, and this around an AFI of 7 cm for second and third trimester pregnancies; and AFI of 5 cm is two standard deviations from the mean - Amniotic fluid index (AFI) >20-24 cm is considered as polyhydramnios
Amniotic fluid index (AFI) has been known to play significant role in obstetric management 1. AFI is calculated by adding the depth in centimeters of the largest vertical pocket in each of four equal uterine quadrants 2. Amniotic fluid index (AFI) less than or equal to 5 cm is defined as oligohydramnios 3. A borderline AFI has been defined as an AFI of 5.1 cm to 8 cm 3. The incidence of an AFI of 5.1 to 8 cm compared with a normal AFI (8.1 cm to 18 cm) in different studies varied from 6% to 44%, with the overall rate being 12% 4.
The maximum vertical pocket (MPV) measures the deepest area of your uterus to check the amniotic fluid level. If your MPV is less than 2 centimeters, you have oligohydramnios.
The deepest (maximal) vertical pocket (MPV) depth is considered a reliable method for assessing amniotic fluid volume on ultrasound 5. It is performed by assessing a pocket of maximal depth of amniotic fluid which is free of umbilical cord and fetal parts.
The usually accepted maximum vertical pocket (MPV) values are:
- <2 cm: indicative of oligohydramnios
- 2-8 cm: normal but should be taken in the context of subjective volume
- >8 cm: indicative of polyhydramnios (although some centers particularly in Australia, New Zealand and the United Kingdom use a cut off of >10 cm)
Ask your health provider if you have questions about these measurements.
Figure 3. Amniotic fluid index (AFI is normal = 10.67 cm)
What problems can low amniotic fluid cause?
If oligohydramnios happens in the first 2 trimesters (first 6 months) of pregnancy, it is more likely to cause serious problems than if it happens in the last trimester. These problems can be:
- Birth defects – Problems with a baby’s body that are present at birth
- Miscarriage – When a baby dies in the womb before 20 weeks of pregnancy
- Premature birth – Birth before 37 weeks of pregnancy
- Stillbirth – When a baby dies in the womb after 20 weeks of pregnancy
If oligohydramnios happens in the third trimester of pregnancy, it can cause:
- The baby to grow slowly
- Problems during labor and birth, such as the umbilical cord being squeezed. The umbilical cord carries food and oxygen from the placenta to the baby. If it’s squeezed, the baby doesn’t get enough food and oxygen.
- A greater chance of needing a cesarean section (when your baby is born through a cut the doctor makes in your belly and uterus)
Low amniotic fluid causes
The causes of oligohydramnios are many and sometimes the causes of oligohydramnios are not known.
Some known causes of low amniotic fluid can be simplified by using the mnemonic DRIPPC:
D: demise and drugs: e.g. prostaglandin inhibitors (indomethacin) or medicine to treat high blood pressure – If you have high blood pressure, talk to your provider before getting pregnant to make sure your blood pressure is under control.
R: renal abnormalities (from decreased urine output)
- renal agenesis
- renal dysplasia
- posterior urethral valves
- polycystic kidneys
- multicystic dysplastic kidney
- urethral atresia
I: IUGR (intra-uterine growth restriction): 80% may occur from decreased renal perfusion due to sparing effect
P: premature rupture of membranes
- premature rupture of membranes (PROM): when the amniotic sac breaks after 37 weeks of pregnancy but before labor starts. Estimated incidence is at 10% of pregnancies at term
- preterm premature rupture of membranes (PPROM): refers to rupture of membranes prior to 37 weeks of gestation. Estimated incidence is at 0.7%-2.0% of preterm pregnancies.
P: Post-term pregnancy – A pregnancy that goes 2 or more weeks past the due date. A full-term pregnancy is one that lasts 39 to 41 weeks.
C: chromosomal anomalies (especially if other anomalies are found)
- trisomy 18
- trisomy 13
- triploidy
How is low amniotic fluid treated?
If you have a healthy pregnancy and get oligohydramnios near the end of your pregnancy, you probably don’t need treatment. Your provider may want to see you more often. She may want to do ultrasounds weekly or more often to check the amount of amniotic fluid.
Sometimes amnioinfusion can help prevent problems in the baby. Amnioinfusion is when the provider puts a saline solution (salty water) into the uterus through your cervix (the opening to the uterus that sits at the top of your vagina). This treatment can help prevent some problems, such as the umbilical cord being squeezed. If the umbilical cord is squeezed, the baby doesn’t get enough food and oxygen.
If the fluid gets too low or if your baby is having trouble staying healthy, your provider may recommend starting labor early to help prevent problems during labor and birth. However, with regular prenatal care, chances are that your baby will be born healthy.
What can you do if you have low amniotic fluid?
Drinking lots of water may help increase the amount of amniotic fluid. Your provider may recommend less physical activity or going on bed rest.
Leaking amniotic fluid
Premature rupture of membranes (PROM) refers to a rupture of the amniotic sac and chorion (membranes) occurring prior to the onset of uterine contractions. When this occurs prior to 37 weeks it is then termed a pre-term premature rupture of membranes (PPROM). By this definition, premature rupture of membranes (PROM) is classified as a rupture of membranes between 37 weeks and full term.
Prolonged rupture of membranes refers to a rupture of membranes lasting longer than 18-24 hours (i.e. between time of rupture and time of delivery) 6. This situation can occur in either the term or pre-term newborns where in the latter case it is also termed prolonged preterm rupture of membranes.
Leaking amniotic fluid signs and symptoms
- Slow leak or gushing of fluid from the vagina
- Wetness in underwear
Sometimes women mistake the leaking of amniotic fluid for urine, especially when it leaks slowly. If you notice any symptoms or think your membranes may have ruptured call your primary health care provider immediately.
You’ll be offered:
- antibiotics to take for a maximum of 10 days, or until labor starts – whichever is sooner
- tests for infection, which may include blood and urine tests
Pre-term premature rupture of membranes (PPROM) doesn’t definitely mean you’re going into labor. You may be able to go home if there’s no infection and you don’t go into labor within 48 hours. If you go home, you’ll be advised to tell your midwife immediately if:
- your temperature is raised (a raised temperature is usually over 37.5 °C (99.5 °F) but check with your midwife – they may need you to call before it gets to 37.5 °C). You should take your temperature every four hours when you’re awake
- any fluid coming from your vagina (called vaginal loss) is colored or smelly
- you bleed from your vagina
- your baby’s movements slow down or stop
Complications of premature rupture of membranes
- increased risk of neonatal sepsis
- increased risk of chorioamnionitis: an infection of the chorion and amnion during pregnancy
- pulmonary hypoplasia can develop when there is very long-standing rupture of membranes causing persistent oligohydramnios
- increased risk of cerebral palsy 7
Clinical presentation of chorionamnionitis
Clinically, chorionamnionitis can present with the following maternal signs and symptoms 8:
- fever
- abdominal pain / uterine tenderness
- raised white blood cell count (> 15 000 cells/mm3)
- purulent or foul vaginal discharge
- tachycardia
Pathology
Chorioamnionitis most frequently occurs due to an ascending bacterial infection from the lower genital tract (vagina and cervix) in the setting of prolonged rupture of membranes (PROM) 8. Other less common causes include introduction of an infection through invasive procedures such as amniocentesis and chorionic villus sampling 8.
Risk factors of ruptured membranes include
- Premature birth
- Infection
- Bleeding
- Early labor and preterm delivery
- Compression of the umbilical called (umbilical cord prolapse)
- Placental abruption
Premature labor and birth
Premature labor is labor that happens before the 37th week of pregnancy. About 8 out of 100 babies will be born prematurely.
If you think your labor might be starting and you’re less than 37 weeks pregnant, call your midwife or hospital straight away. They’ll need to check you and your baby to find out whether you’re in labor, and discuss your care choices with you.
They’ll offer checks, tests and monitoring to find out whether:
- your waters have broken
- you’re in labor
- you have an infection
These may include a vaginal examination, blood test, urine test and cardiotocography to record contractions and the baby’s heartbeat.
If you’re in premature labor
The midwife or doctor may offer:
- medicine to try to slow down or stop your labor (tocolysis)
- corticosteroid injections, which can help your baby’s lungs
Slowing down labor or stopping it isn’t appropriate in all circumstances – your midwife or doctor can discuss your situation with you. They will consider:
- how many weeks pregnant you are
- whether it might be safer for the baby to be born – for example, if you have an infection or you’re bleeding
- local neonatal (newborn) care facilities and whether you might need to be moved to another hospital
- your wishes
Corticosteroid injections can help your baby’s lungs get ready for breathing if they’re born prematurely. There are two injections, given 12 hours apart – your midwife or doctor will discuss the benefits and risks with you.
Corticosteroids probably won’t be offered after 36 weeks as your baby’s lungs are likely to be ready for breathing on their own.
If you’re in premature labor and you’re between 24 and 29 weeks pregnant you should be offered magnesium sulphate. This can help protect your baby’s brain development. You may also be offered it if you’re in labor between 30 and 34 weeks. This is to protect your baby against problems linked to being born too soon, such as cerebral palsy.
What are the risks to my baby of being born early?
Babies born before full term (before 37 weeks) are vulnerable to problems associated with being born premature. The earlier in the pregnancy a baby is born, the more vulnerable they are.
Babies are considered ‘viable’ at 24 weeks of pregnancy – this means it’s possible for them to survive being born at this stage.
Babies born this early need special care in a hospital with specialist facilities for premature babies. This is called a neonatal unit. They may have health and development problems because they haven’t fully developed in the womb.
If your baby is likely to be delivered early, you should be admitted to a hospital with a neonatal unit.
Not all hospitals have facilities for the care of very premature babies, so it may be necessary to transfer you and your baby to another unit, ideally before delivery (if time permits) or immediately afterwards.
Too much amniotic fluid
Too much amniotic fluid is also called polyhydramnios, which is the medical term for excessive accumulation of amniotic fluid — the fluid that surrounds the baby in the uterus during pregnancy. Too much amniotic fluid or polyhydramnios occurs in about 1 to 2 percent of pregnancies and while it typically is not associated with significant issues, it if is severe, it can affect the mother by causing shortness of breath, preterm labor, or severe post-delivery bleeding.
Most cases of too much amniotic fluid (polyhydramnios) are mild and result from a gradual buildup of amniotic fluid during the second half of pregnancy. Severe polyhydramnios may cause shortness of breath, preterm labor, or other signs and symptoms. In some cases, draining of excess fluid by amniocentesis may be required.
In approximately 20% of pregnancies with polyhydramnios, a fetal abnormality is identified, such as an incompletely formed esophagus that prevents the fetus from swallowing the amniotic fluid. However, a majority of the time, the cause is not clear.
If you’re diagnosed with polyhydramnios, your health care provider will carefully monitor your pregnancy to help prevent complications. Treatment depends on the severity of the condition. Mild polyhydramnios may go away on its own. Severe polyhydramnios may require closer monitoring.
Excess amniotic fluid symptoms
Polyhydramnios symptoms result from pressure being exerted within the uterus and on nearby organs.
Mild excess amniotic fluid may cause few — if any — signs or symptoms.
Severe excess amniotic fluid may cause:
- Shortness of breath or the inability to breathe
- Swelling in the lower extremities and abdominal wall
- Uterine discomfort or contractions
- Fetal malposition, such as breech presentation
Your health care provider may also suspect polyhydramnios if your uterus is excessively enlarged and he or she has trouble feeling the baby.
Too much amniotic fluid causes
Some of the known causes of polyhydramnios include:
- A birth defect that affects the baby’s gastrointestinal tract or central nervous system
- Maternal diabetes
- Twin-twin transfusion — a possible complication of identical twin pregnancies in which one twin receives too much blood and the other too little
- A lack of red blood cells in the baby (fetal anemia)
- Blood incompatibilities between mother and baby
- Infection during pregnancy
Often, however, the cause of too much amniotic fluid (polyhydramnios) isn’t clear.
Too much amniotic fluid complications
Polyhydramnios is associated with:
- Premature birth
- Premature rupture of membranes (PROM) — when your water breaks early
- Placental abruption — when the placenta peels away from the inner wall of the uterus before delivery
- Umbilical cord prolapse — when the umbilical cord drops into the vagina ahead of the baby
- Cesarean section delivery
- Stillbirth
- Heavy bleeding due to lack of uterine muscle tone after delivery
The earlier that polyhydramnios occurs in pregnancy and the greater the amount of excess amniotic fluid, the higher the risk of complications.
Too much amniotic fluid diagnosis
If your health care provider suspects polyhydramnios, he or she will do a fetal ultrasound. This test uses high-frequency sound waves to produce images of your baby on a monitor.
If the initial ultrasound shows evidence of polyhydramnios, your health care provider may do a more detailed ultrasound. He or she will estimate the amniotic fluid volume (AFV) by measuring the single largest, deepest pocket of fluid around your baby. An AFV value of 8 centimeters or more suggests polyhydramnios.
An alternative way of measuring amniotic fluid is measuring the largest pocket in four specific parts of your uterus. The sum of these measurements is the amniotic fluid index (AFI). An AFI of 25 centimeters or more indicates polyhydramnios. Your health care provider will also use a detailed ultrasound to diagnose or rule out birth defects and other complications.
Your health care provider may offer additional testing if you have a diagnosis of polyhydramnios. Testing will be based on your risk factors, exposure to infections and prior evaluations of your baby. Additional tests may include:
Blood tests. Blood tests for infectious diseases associated with polyhydramnios may be offered.
Amniocentesis. Amniocentesis is a procedure in which a sample of amniotic fluid — which contains fetal cells and various chemicals produced by the baby — is removed from the uterus for testing. Testing may include a karyotype analysis, used to screen the baby’s chromosomes for abnormalities.
If you’re diagnosed with polyhydramnios, your health care provider will closely monitor your pregnancy. Monitoring may include the following:
Nonstress test. This test checks how your baby’s heart rate reacts when your baby moves. During the test, you’ll wear a special device on your abdomen to measure the baby’s heart rate. You may be asked to eat or drink something to make the baby active. A buzzer-like device also may be used to wake the baby and encourage movement.
Biophysical profile. This test uses an ultrasound to provide more information about your baby’s breathing, tone and movement, as well as the volume of amniotic fluid in your uterus. It may be combined with a nonstress test.
Too much amniotic fluid treatment
Mild cases of polyhydramnios rarely require treatment and may go away on their own. Even cases that cause discomfort can usually be managed without intervention.
In other cases, treatment for an underlying condition — such as maternal diabetes — may help resolve polyhydramnios.
If you experience preterm labor, shortness of breath or abdominal pain, you may need treatment — potentially in the hospital. Treatment may include:
- Drainage of excess amniotic fluid. Your health care provider may use amniocentesis to drain excess amniotic fluid from your uterus. This procedure carries a small risk of complications, including preterm labor, placental abruption and premature rupture of the membranes.
- Medication. Your health care provider may prescribe the oral medication indomethacin (Indocin) to help reduce fetal urine production and amniotic fluid volume. Indomethacin isn’t recommended beyond 31 weeks of pregnancy. Due to the risk of fetal heart problems, your baby’s heart may need to be monitored with a fetal echocardiogram and Doppler ultrasound. Other side effects may include nausea, vomiting, acid reflux and inflammation of the lining of the stomach (gastritis).
After treatment, your doctor will still want to monitor your amniotic fluid level approximately every one to three weeks.
If you have mild to moderate polyhydramnios, you’ll likely be able to carry your baby to term, delivering at 39 or 40 weeks. If you have severe polyhydramnios, your health care provider will discuss the appropriate timing of delivery, to avoid complications for you and your baby.
Polyhydramnios can be a worrisome finding during pregnancy. Work with your pregnancy care provider to ensure that you and your baby receive the best possible care.
Amniotic fluid embolism
Amniotic fluid embolism is a rare but serious condition that occurs when amniotic fluid or fetal material, such as fetal cells, enters the mother’s bloodstream. Amniotic fluid embolism is most likely to occur during delivery or immediately afterward.
Amniotic fluid embolism is difficult to diagnose. If your doctor suspects you might have amniotic fluid embolism, you’ll need immediate treatment to prevent potentially life-threatening complications.
Amniotic fluid embolism signs and symptoms
Amniotic fluid embolism develops suddenly and rapidly.
Signs and symptoms of amniotic fluid embolism might include:
- Sudden shortness of breath
- Excess fluid in the lungs (pulmonary edema)
- Sudden low blood pressure
- Sudden failure of the heart to effectively pump blood (cardiovascular collapse)
- Life-threatening problems with blood clotting (disseminated intravascular coagulopathy)
- Altered mental status, such as anxiety
- Chills
- Rapid heart rate or disturbances in the rhythm of the heart rate
- Fetal distress, such as a slow heart rate
- Seizures
- Coma
- Sudden fetal heart rate abnormalities
- Bleeding from the uterus, incision or intravenous (IV) sites
Causes of amniotic fluid embolism
Amniotic fluid embolism occurs when amniotic fluid or fetal material enters the mother’s bloodstream. Why this happens isn’t well understood. A likely cause is a breakdown in the placental barrier, such as from trauma.
When this breakdown happens, the immune system responds by releasing products that cause an inflammatory reaction, activating abnormal clotting in the mother’s lungs and blood vessels that can result in a serious blood-clotting disorder known as disseminated intravascular coagulation (DIC).
However, amniotic fluid embolisms are rare — and it’s likely that some amniotic fluid commonly enters the mother’s bloodstream during delivery without causing problems. It’s not clear why in some cases this leads to amniotic fluid embolism.
Further research on what causes amniotic fluid embolisms is needed.
Amniotic fluid embolism risk factors
Amniotic fluid embolisms are rare, which makes it difficult to identify risk factors. It’s estimated that there are between 1 and 12 cases of amniotic fluid embolism for every 100,000 deliveries.
Research suggests that several factors might be linked to an increased risk of amniotic fluid embolism, however, including:
- Advanced maternal age. If you’re 35 or older at the time of your child’s birth, you might be at increased risk of amniotic fluid embolism.
- Placenta problems. If there are abnormalities in your placenta — the structure that develops in your uterus during pregnancy — you might be at increased risk of amniotic fluid embolism. Abnormalities might include the placenta partially or totally covering the cervix (placenta previa) or the placenta peeling away from the inner wall of the uterus before delivery (placental abruption). These conditions can disrupt the physical barriers between you and your baby.
- Preeclampsia. If you have preeclampsia — high blood pressure and excess protein in the urine after 20 weeks of pregnancy — you might be at increased risk of developing amniotic fluid embolism.
- Medically induced labor. Limited research suggests that certain labor induction methods are associated with an increased risk of amniotic fluid embolism. Research on this link, however, is conflicting.
- Operative delivery. Having a cesarean section, a forceps delivery or a vacuum extraction might increase your risk of amniotic fluid embolism. These procedures can disrupt the physical barriers between you and your baby. It’s not clear, however, whether operative deliveries are true risk factors for amniotic fluid embolisms or are used after the condition develops to ensure a rapid delivery.
- Polyhydramnios. Having too much amniotic fluid around your baby may put you at risk of amniotic fluid embolism.
Amniotic fluid embolism complications
Amniotic fluid embolism can cause serious complications for you and your baby.
If you have amniotic fluid embolism, you’re at increased risk of:
- Brain injury. Low blood oxygen can cause permanent, severe neurological damage or brain death.
- Lengthy hospital stay. Women who survive an amniotic fluid embolism often require treatment in the intensive care unit and — depending on the extent of their complications — might spend weeks or months in the hospital.
- Maternal death. The number of women who die of amniotic fluid embolism (mortality rate) is very high. The numbers vary, but as many as 20 percent of maternal deaths in developed countries may be due to amniotic fluid embolisms. However, prompt evaluation and treatment may save your life.
- Infant death. Your baby is at risk of brain injury or death. Prompt evaluation and delivery of your baby improves survival.
Amniotic fluid embolism diagnosis
The diagnosis of amniotic fluid embolism is based on a doctor’s evaluation. A diagnosis is typically made after other conditions have been ruled out. In some cases, a diagnosis is only made after maternal death. Your health care provider might order the following lab tests during your evaluation:
- Blood tests, including those that evaluate clotting, heart enzymes, electrolytes and blood type, as well as a complete blood count (CBC)
- Electrocardiogram (ECG or EKG) to evaluate your heart’s rhythm
- Pulse oximetry to check the amount of oxygen in your blood
- Chest X-ray to look for fluid around your heart
- Echocardiography to evaluate your heart’s function
Amniotic fluid embolism treatment
Amniotic fluid embolism requires rapid treatment to address low blood oxygen and low blood pressure.
Emergency treatments might include:
- Catheter placement. Your health care team places a thin, hollow tube into one of your arteries (arterial catheter) to monitor your blood pressure. You’ll also have another tube placed into a vein in your chest (central venous catheter), which can be used to give fluids, medications or transfusions, as well as draw blood.
- Oxygen. You might need to have a breathing tube inserted into your airway to help you breathe.
- Medications. Your doctor might give you medications to improve and support your heart function. Other medications might be used to decrease the pressure caused by fluid going into your heart and lungs.
- Transfusions. If you have uncontrollable bleeding, you’ll need transfusions of blood, blood products and replacement fluids.
If you have amniotic fluid embolism before delivering your baby, your doctor will treat you with the goal of safely delivering your baby as soon as possible. An emergency cesarean section might be needed.
Coping and support
Experiencing a life-threatening pregnancy condition can be frightening and stressful for you and your family. You and your baby might experience serious complications and require lengthy hospital stays.
Amniotic fluid embolism is a medical emergency, leaving you no time to prepare. If you’re concerned about your risk of amniotic fluid embolism, talk with your doctor. Keep in mind, however, that amniotic fluid embolisms are rare, unpredictable and unpreventable.
During this challenging time, lean on loved ones for support. Consider joining a survivors’ network. Also, work with your health care provider to determine how you can safely manage your recovery and your role as the mother of a newborn.
- [Maternal and perinatal outcomes in women with decreased amniotic fluid]. Souza AS, de Andrade LR, da Silva FL, Cavalcanti AN, Guerra GV. Rev Bras Ginecol Obstet. 2013 Aug; 35(8):342-8. https://www.ncbi.nlm.nih.gov/pubmed/24126352/[↩]
- Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, et al. Amniotic fluid. Williams Obstetrics. New York: McGraw Hill Education; 2014. pp. 460–76.[↩]
- Choi SR. Borderline amniotic fluid index and perinatal outcomes in the uncomplicated term pregnancy. J Matern Fetal Neonatal Med. 2016;29(3):457–60. https://www.ncbi.nlm.nih.gov/pubmed/25626056[↩][↩]
- Kwon J-Y, Kwon H-S, Kim Y-H, Park Y-W. Abnormal Doppler velocimetry is related to adverse perinatal outcome for borderline amniotic fluid index during third trimester. J Obstet Gynaecol Res. 2006;32(6):545–49. https://www.ncbi.nlm.nih.gov/pubmed/17100815[↩]
- Magann EF, Chauhan SP, Doherty DA et-al. The evidence for abandoning the amniotic fluid index in favor of the single deepest pocket. Am J Perinatol. 2007;24 (9): 549-55.[↩]
- Callahan TL, Caughey AB. Blueprints Obstetrics and Gynecology. Lippincott Williams & Wilkins. (2008) ISBN:078178249X[↩]
- Azziz R. Obstetrics and gynecology, cases, questions, and answers. McGraw-Hill Professional. (2006) ISBN:0071458204[↩]
- Czikk MJ, McCarthy FP, Murphy KE. Chorioamnionitis: from pathogenesis to treatment. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 17 (9): 1304-11. https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(14)61208-8/fulltext[↩][↩][↩]