What is AST test
AST is short for aspartate aminotransferase is also called SGOT (Serum Glutamic-Oxaloacetic Transaminase) or GOT (Glutamic-Oxaloacetic Transaminase), which is an enzyme found throughout your body but mostly in your heart and liver and to a lesser extent, in the kidneys and muscles. In healthy individuals, levels of AST (aspartate aminotransferase) in the blood are low. When liver or muscle cells are injured, they release AST into the blood. This makes AST a useful test for detecting or monitoring liver damage. Normal AST is less than 42U/L [units per liter] (range 8 to 48 U/L). This result is typical for adult men. Normal results vary from laboratory to laboratory and might be slightly different for women and children. Hemolysis during collection or refrigeration of unseparated blood may cause an artefactual increase in AST.
A number of conditions can cause injury to liver cells (hepatocytes) and may cause increases in AST. The AST test is most useful in detecting liver damage due to hepatitis, drugs toxic to the liver, cirrhosis, or alcoholism. AST (aspartate aminotransferase), however, is not specific for the liver and may be increased in conditions affecting other parts of the body. Although AST levels are increased with cardiac and skeletal muscle disease, more specific tests are available in these situations.
An AST test is often performed along with an alanine aminotransferase (ALT) test. Both are enzymes found in the liver that become elevated in the blood when the liver is damaged. A calculated AST/ALT ratio is useful for differentiating between different causes of liver injury and in recognizing when the increased levels may be coming from another source, such as heart or muscle injury. The AST/ALT ratio is typically > 1 in alcoholic liver disease and AST/ALT < 1 in non-alcoholic liver disease.
How is the sample collected for testing?
A blood sample is drawn by needle from a vein in the arm.
Is any test preparation needed to ensure the quality of the sample?
No test preparation is needed.
The Liver
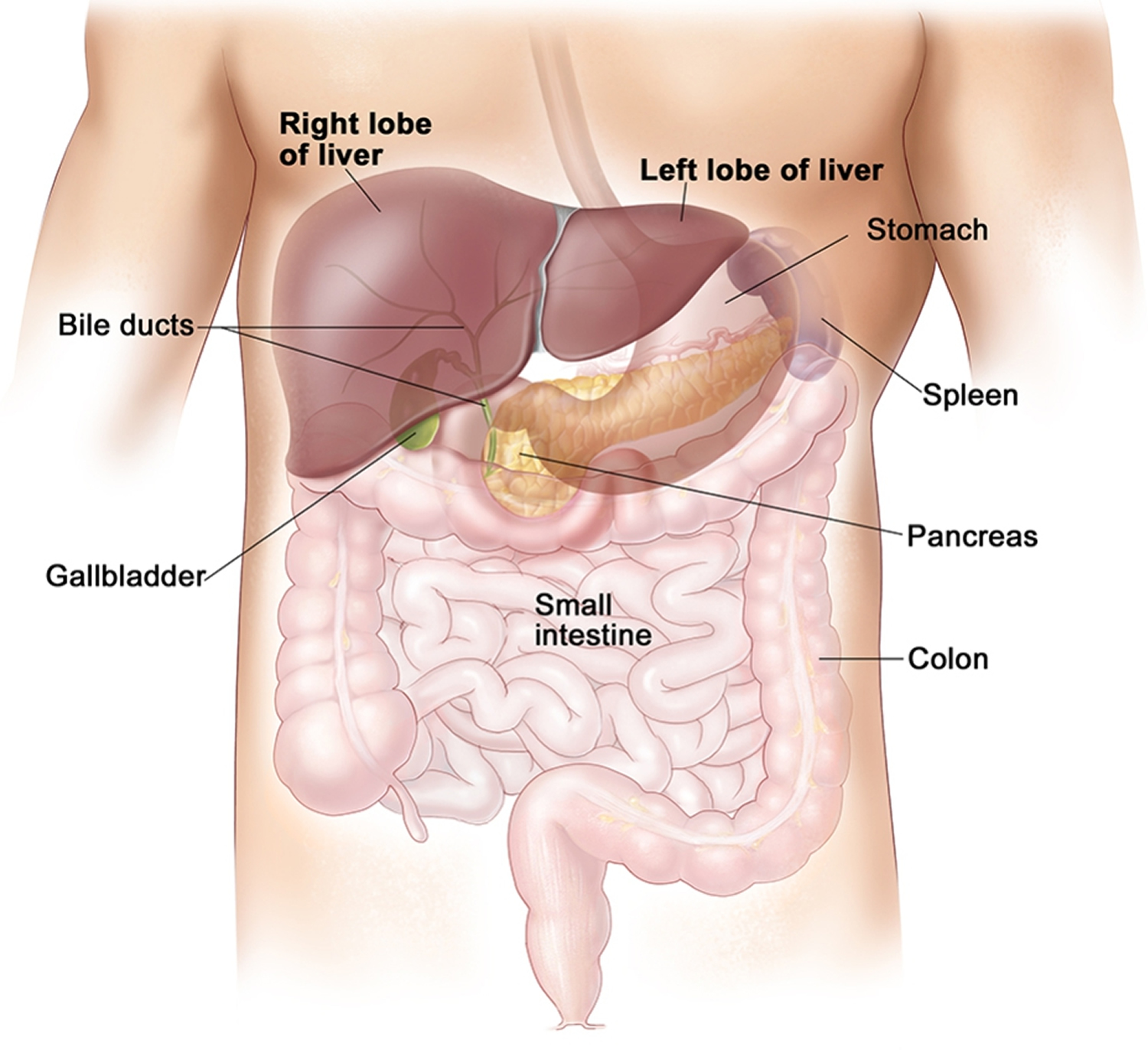
Your liver is the largest organ inside your body, weighing about 1.4 kg (3 pounds) in an average adult. Your liver is a vital organ located in the upper right-hand side of the abdominal cavity, just inferior to the diaphragm in the right superior part of the abdominal cavity and under your right ribs just beneath your right lung – filling much of the right hypochondriac and epigastric regions and extending into the left hypochondriac region.
Your liver is partially surrounded by the ribs, and extends from the level of the fifth intercostal space to the lower margin of the right rib cage, which protects this highly vascular organ from blows that could rupture it. Your liver is shaped like a wedge, the wide base of which faces right and the narrow apex of which lies just inferior to the level of the left nipple. The reddish-brown liver is well supplied with blood vessels.
Your liver is involved in many important functions in the body. Your liver helps to process your body’s nutrients, manufactures bile to help digest fats, produces many important proteins such as blood clotting factors, and breaks down potentially toxic substances into harmless ones that the body can use or excrete.
Figure 1. Location of the human liver
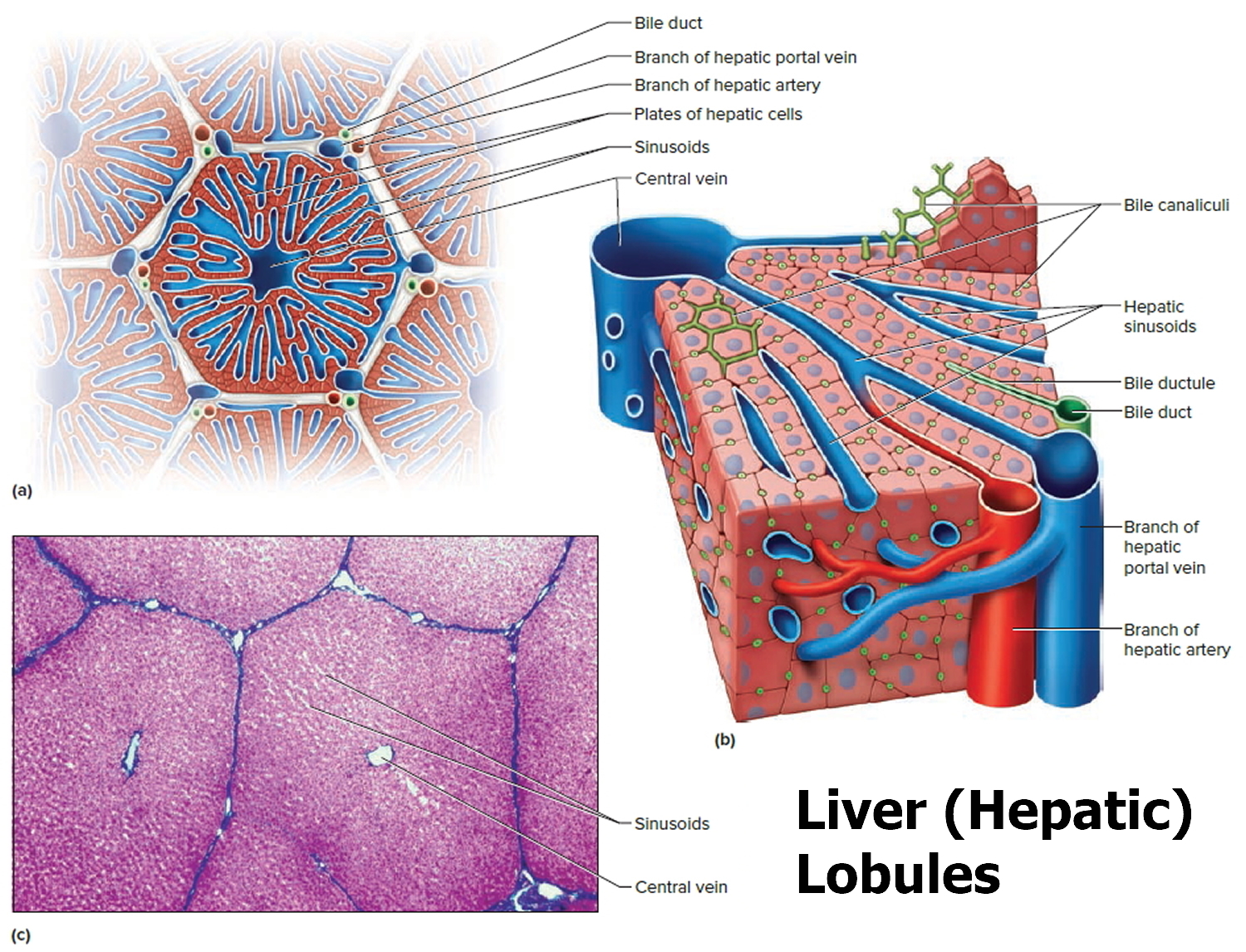
Figure 2. Liver lobule
Footnote: (a) Cross section of a hepatic lobule. (b) Enlarged longitudinal section of a hepatic lobule. (c) Light micrograph of hepatic lobules in cross section.
Liver functions
Amazingly versatile, your liver performs over 500 functions. Its digestive function is to produce bile, a green alkaline liquid that is stored in the gallbladder and secreted into the duodenum. Bile salts emulsify fats in the small intestine; that is, they break up fatty nutrients into tiny particles, just as dish detergent breaks up a pool of fat drippings in a roasting pan. These smaller particles are more accessible to digestive enzymes from the pancreas. The liver also performs many metabolic functions and you cannot live without your liver:
- Picks up glucose from nutrient-rich blood returning from the alimentary canal and stores this carbohydrate as glycogen for subsequent use by the body.
- Processes fats and amino acids and stores certain vitamins.
- Detoxifies many poisons and drugs in the blood.
- Makes the blood proteins.
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It secretes bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Almost all of these functions are carried out by a type of cell called a hepatocyte or simply a liver cell.
The liver carries on many important metabolic activities. The liver plays a key role in carbohydrate metabolism by helping maintain concentration of blood glucose within the normal range. Liver cells responding to the hormone insulin lower the blood glucose level by polymerizing glucose to glycogen. Liver cells responding to the hormone glucagon raise the blood glucose level by breaking down glycogen to glucose or by converting noncarbohydrates into glucose.
The liver’s effects on lipid metabolism include oxidizing (breaking down) fatty acids at an especially high rate; synthesizing lipoproteins, phospholipids, and cholesterol; and converting excess portions of carbohydrate molecules into fat molecules. The blood transports fats synthesized in the liver to adipose tissue for storage.
Other liver functions concern protein metabolism. They include deaminating amino acids; forming urea; synthesizing plasma proteins such as clotting factors; and converting certain amino acids into other amino acids.
The liver also stores many substances, including glycogen, iron, and vitamins A, D, and B12. In addition, macrophages in the liver help destroy damaged red blood cells and phagocytize foreign antigens. The liver also removes toxic substances such as alcohol and certain drugs from blood (detoxification).
Table 1. Major Functions of the Liver
| General Function | Specific Function |
| Carbohydrate metabolism | Polymerizes glucose to glycogen; breaks down glycogen to glucose; converts noncarbohydrates to glucose |
| Lipid metabolism | Oxidizes fatty acids; synthesizes lipoproteins, phospholipids, and cholesterol; converts excess portions of carbohydrate molecules into fats |
| Protein metabolism | Deaminates amino acids; forms urea; synthesizes plasma proteins; converts certain amino acids into other amino acids |
| Storage | Stores glycogen, iron, and vitamin A, vitamin D and vitamin B12 |
| Blood filtering | Removes damaged red blood cells and foreign substances by phagocytosis |
| Detoxification | Removes toxins from blood |
| Secretion | Produces and secretes bile |
The Bile
Bile is a yellowish-green liquid continuously secreted from hepatic cells. In addition to water, bile contains bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes. Of these, bile salts are the most abundant and are the only bile components that have a digestive function.
Bile pigments are breakdown products of hemoglobin from red blood cells and are normally secreted in the bile.
Jaundice, a yellowing of the skin and mucous membranes due to accumulation of bile pigment, has several causes. In obstructive jaundice bile ducts are blocked, perhaps by gallstones or tumors. In hepatocellular jaundice the liver is diseased, as in cirrhosis or hepatitis. In hemolytic jaundice red blood cells are destroyed too rapidly, as happens with an incompatible blood transfusion or a blood infection.
Regulation of Bile Release
Normally bile does not enter the duodenum until cholecystokinin stimulates the gallbladder to contract. The intestinal mucosa releases this hormone in response to proteins and fats in the small intestine. The hepatopancreatic sphincter usually remains contracted until a peristaltic wave in the duodenal wall approaches it. Then the sphincter relaxes, and bile is squirted into the duodenum.
Functions of Bile Salts
Bile salts aid digestive enzymes. Bile salts affect fat globules (clumped molecules of fats) much like a soap or detergent would affect them. That is, bile salts break fat globules into smaller droplets that are more soluble in water. This action, called emulsification, greatly increases the total surface area of the fatty substance. The resulting fat droplets disperse in water. Fat-splitting enzymes (lipases) can then digest the fat molecules more effectively. Bile salts also enhance absorption of fatty acids, cholesterol, and the fat-soluble vitamins A, D, E, and K.
Low levels of bile salts result in poor lipid absorption and vitamin deficiencies.
What does AST mean in a blood test
The AST blood test is usually used to detect liver damage. AST blood test is often ordered in conjunction with another liver enzyme, alanine aminotransferase (ALT), or as part of a liver panel or comprehensive metabolic panel to screen for and/or help diagnose liver disorders.
AST and ALT (alanine aminotransferase) are considered to be two of the most important tests to detect liver injury, although ALT (alanine aminotransferase) is more specific for the liver than is AST and is more commonly increased than is AST. Sometimes AST is compared directly to ALT and an AST/ALT ratio is calculated. This ratio may be used to distinguish between different causes of liver damage and to distinguish liver injury from damage to heart or muscle.
AST levels are often compared with results of other tests such as alkaline phosphatase (ALP), total protein, and bilirubin to help determine which form of liver disease is present.
AST is often measured to monitor treatment of persons with liver disease and may be ordered either by itself or along with other tests for this purpose.
Sometimes AST may be used to monitor people who are taking medications that are potentially toxic to the liver. If AST levels increase, then the person may be switched to another medication.
When is AST blood test ordered?
AST may be ordered as part of a comprehensive metabolic panel when someone has a routine health examination.
An AST test may be ordered along with several other tests when a person has signs and symptoms of a liver disorder. Some of these may include:
- Weakness, fatigue
- Loss of appetite
- Nausea, vomiting
- Abdominal swelling and/or pain
- Jaundice
- Dark urine, light-colored stool
- Itching (pruritus)
- Swelling in the legs and ankles
- Tendency to bruise easily
AST may also be ordered, either by itself or with other tests, for people who are at an increased risk for liver disease since many people with mild liver damage will have no signs or symptoms. Some examples include:
- Persons who might have been exposed to hepatitis viruses
- Persons who are heavy drinkers
- Persons who have a history of liver disease in their family
- Persons taking drugs that can damage the liver
- Persons who are overweight and/or have diabetes
When AST is used to monitor treatment of persons with liver disease, it may be ordered on a regular basis during the course of treatment to determine whether the therapy is effective.
AST liver test
AST blood test normal range: Normal AST is less than 42U/L [units per liter] (range 8 to 48 U/L). This result is typical for adult men. Normal results vary from laboratory to laboratory and might be slightly different for women and children. Hemolysis during collection or refrigeration of unseparated blood may cause an artefactual increase in AST.
Low levels of AST in the blood are expected and are normal.
AST blood test high
Very high levels of AST (more than 10 times normal) are usually due to acute hepatitis, sometimes due to a viral infection. With acute hepatitis, AST levels usually stay high for about 1-2 months but can take as long as 3-6 months to return to normal. Levels of AST may also be markedly elevated (often over 100 times normal) as a result of exposure to drugs or other substances that are toxic to the liver as well as in conditions that cause decreased blood flow (ischemia) to the liver.
Pregnancy, a shot or injection of medicine into muscle tissue, or even strenuous exercise may increase AST levels. Acute burns, surgery, and seizures may raise AST levels as well. In rare instances, some drugs can damage the liver or muscle, increasing AST levels. This is true of both prescription drugs and some “natural” health products. Be sure to tell your healthcare practitioner about all of the drugs and/or health supplements that you are taking.
With chronic hepatitis, AST levels are usually not as high, often less than 4 times normal, and are more likely to be normal than are ALT levels. AST often varies between normal and slightly increased with chronic hepatitis, so the test may be ordered frequently to determine the pattern. Such moderate increases may also be seen in other diseases of the liver, especially when the bile ducts are blocked, or with cirrhosis or certain cancers of the liver. AST may also increase after heart attacks and with muscle injury, usually to a much greater degree than ALT.
AST is often performed together with the ALT test or as part of a liver panel. For more about AST results in relation to other liver tests, see the Liver Panel article.
In most types of liver disease, the ALT level is higher than AST and the AST/ALT ratio will be low (less than 1). There are a few exceptions; the AST/ALT ratio is usually increased in alcoholic hepatitis, cirrhosis, hepatitis C virus-related chronic liver disease, and in the first day or two of acute hepatitis or injury from bile duct obstruction. With heart or muscle injury, AST is often much higher than ALT (often 3-5 times as high) and levels tend to stay higher than ALT for longer than with liver injury.
What conditions other than liver problems can cause increased AST?
Conditions that affect other organs, such as the heart and skeletal muscle, can cause elevations of AST. Mild to moderate increases may be seen with vigorous exercise and skeletal muscle injury or in conditions such as acute pancreatitis and heart attacks.
What other tests may be used to help determine the cause of liver damage?
After a thorough physical exam and evaluation of a person’s medical history, there are several other tests that may be performed as follow up depending on what is suspected to be the cause of liver damage. Some of these include:
- Tests for hepatitis A, hepatitis B, and hepatitis C
- Testing for exposure to drugs and other substances toxic to the liver (see Drug Abuse Testing and Emergency and Overdose Drug Testing)
- Ethanol level
- Copper and ceruloplasmin for Wilson disease
- Iron tests and genetic tests for hereditary hemochromatosis
A liver biopsy may be performed to help determine the cause of liver injury and to evaluate the extent of liver damage.