Contents
- What is progesterone
- Menstruation cycle
- Progesterone test
- Progesterone in pregnancy
- In women presenting with a clinical diagnosis of threatened miscarriage
- In women with a history of unexplained recurrent miscarriage
- Role of luteal phase progestogen support in assisted reproductive technologies (ART)
- Progesterone use in the second and third trimester of pregnancy for the prevention of preterm birth
- Conclusion
- What are the management considerations for patients with a history of spontaneous preterm birth?
- What are the management considerations for asymptomatic women with a short cervix at 18-24 weeks?
- What other indications should be considered when using Progesterone to prevent preterm birth?
- What is the ideal route of administration and the correct dosage?
- Progesterone Medications
What is progesterone
Progesterone is a female hormone produced by the ovaries that is important for the regulation of ovulation and menstruation. Progesterone, along with estrogen, prepares the uterus (womb) for a possible pregnancy each month and supports the fertilized egg if conception occurs. Progesterone also helps prepare the breasts for milk production and breastfeeding.
Progesterone is used to cause menstrual periods in women who have not yet reached menopause but are not having periods due to a lack of progesterone in the body. Progesterone is also used to prevent overgrowth in the lining of the uterus in postmenopausal women who are receiving estrogen hormone replacement therapy (HRT). Progesterone (in the synthetic form progestin) is often used in hormone replacement therapy (HRT) for menopausal women who still have their uterus and is used in some contraceptive pills.
Progesterone should not be used to prevent heart disease or dementia, because progesterone may actually increase your risk of developing these conditions.
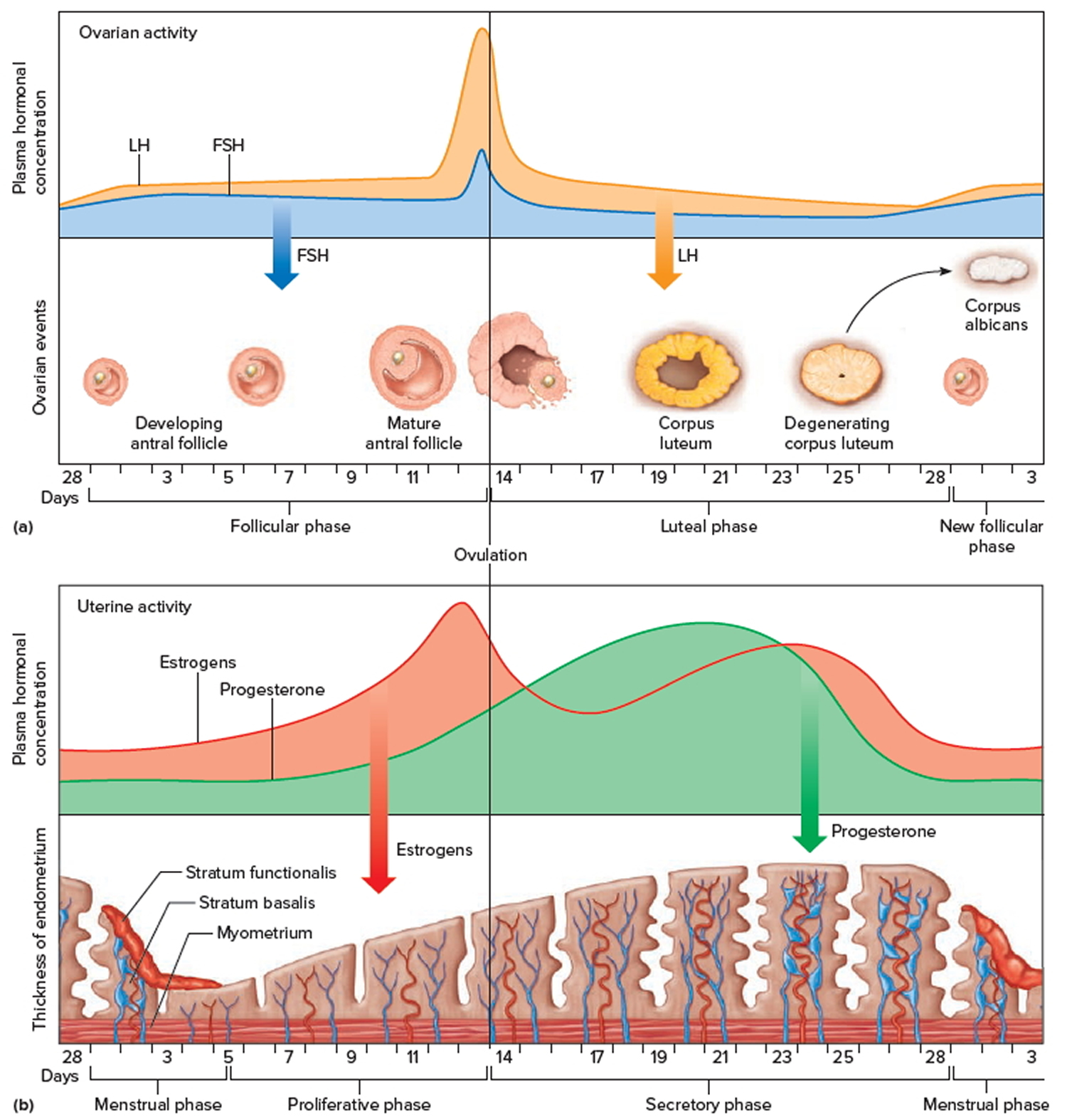
On a monthly basis, the hormone estrogen causes the lining of the uterus, the endometrium, to grow and replenish itself, while a surge in luteinizing hormone (LH) leads to the release of an egg from one of two ovaries. A corpus luteum then forms in the ovary at the site where the egg was released and begins to produce progesterone. This progesterone, supplemented by small amounts produced by the adrenal glands, stops endometrial growth and readies the uterus for the possible implantation of a fertilized egg.
If fertilization does not occur, the corpus luteum degenerates, progesterone levels drop, and menstrual bleeding begins. If a fertilized egg is implanted in the uterus, the corpus luteum continues to produce progesterone, with the egg forming a trophoblast that produces human chorionic gonadotropin (hCG). After several weeks, the placenta replaces the corpus luteum as the main source of progesterone, producing relatively large amounts of the hormone throughout the rest of a normal pregnancy.
Progesterone is also produced in males but at a much lower level. Its function involves the development of sperm.
Menstruation cycle
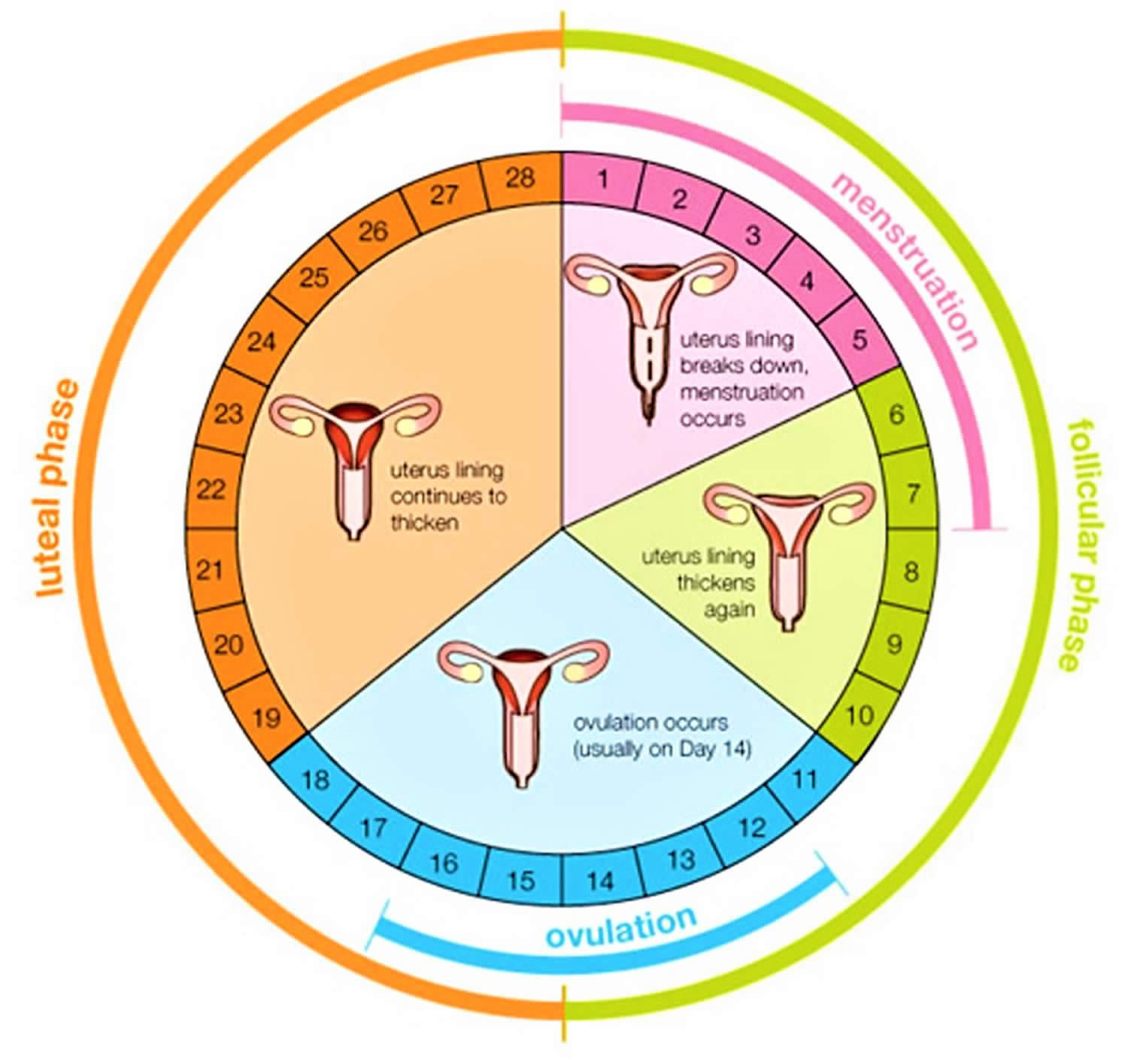
The menstrual cycle is the monthly process in which female hormones stimulate an ovary to release an egg, thicken the lining of the uterus to support a pregnancy, and then cause the uterus to shed this lining (through menstruation) if there is no pregnancy. The average menstrual cycle is 28 days, but this varies between women and from month to month. In teens, the menstrual cycle can range from 21 to 45 days, but for most women, it is 21 to 35 days 1.
The menstrual cycle is characterized by regular, recurring changes in the endometrium, which culminate in menstrual bleeding (menses). Such cycles usually begin around age thirteen and continue into the early fifties, then cease.
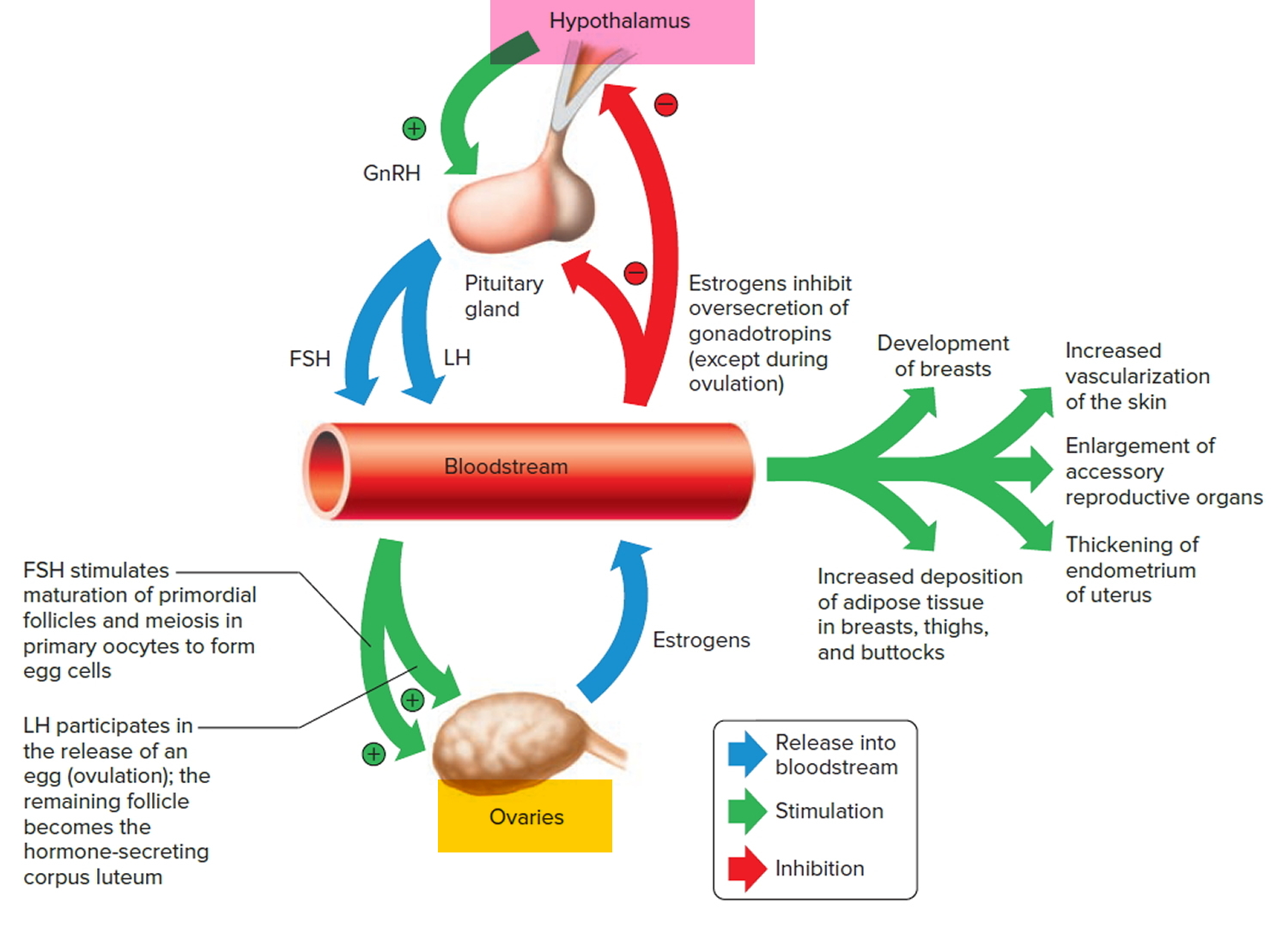
A female’s first menstrual cycle, called menarche, occurs after the ovaries and other organs of the reproductive control system mature and begin responding
to certain hormones. Then, the hypothalamic secretion of gonadotropin-releasing hormone (GnRH) stimulates the anterior pituitary to release threshold levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Follicle-stimulating hormone (FSH) stimulates the final maturation of an ovarian follicle. The follicular cells produce increasing amounts of estrogens and some progesterone. Luteinizing hormone (LH) stimulates certain ovarian cells to secrete precursor molecules (such as testosterone), also used to produce estrogens.
In a young female, estrogens stimulate the development of secondary sex characteristics. Estrogens secreted during subsequent menstrual cycles continue the development and maintenance of these characteristics.
Increasing concentration of estrogens during the first week or so of a menstrual cycle changes the uterine lining, thickening the glandular endometrium (proliferative phase). Meanwhile, the follicle fully matures, and by around the fourteenth day of the cycle, the antral follicle appears on the ovary surface as a blisterlike bulge. Within the follicle, the follicular cells, which surround and connect the secondary oocyte to the inner wall, loosen. Follicular fluid accumulates.
While the follicle matures, it secretes estrogens that inhibit the release of luteinizing hormone (LH) from the anterior pituitary gland but allow luteinizing hormone (LH) to be stored in the gland. Estrogens also make anterior pituitary cells more sensitive to the action of gonadotropin-releasing hormone (GnRH), which is released from the hypothalamus in rhythmic pulses about ninety minutes apart.
Near the fourteenth day of follicular development, the anterior pituitary cells finally respond to the pulses of GnRH (gonadotropin-releasing hormone) and release the stored LH (luteinizing hormone). The resulting surge in LH concentration lasts about thirty-six hours. In response to the LH, the primary oocyte completes meiosis I. The LH (luteinizing hormone) also acts with FSH (follicle-stimulating hormone) inducing complex interactions with prostaglandins, progesterone, plasmin, and proteolytic enzymes, leading to the weakening and rupturing of the bulging follicular wall. This event sends the secondary oocyte and follicular fluid out of the ovary (ovulation).
Following ovulation, the space containing the follicular fluid fills with blood, which soon clots. Under the influence of LH (luteinizing hormone), the remnants of the follicle within the ovary form a temporary glandular structure in the ovary called a corpus luteum (“yellow body”).
Follicular cells secrete some progesterone during the first part of the menstrual cycle. During the second half of the cycle, cells of the corpus luteum secrete abundant progesterone and estrogens. Consequently, as a corpus luteum forms, the blood progesterone concentration sharply increases.
Progesterone causes the endometrium to become more vascular and glandular. It also stimulates the uterine glands to secrete more glycogen and lipids (secretory phase). The endometrial tissues fill with fluids containing nutrients and electrolytes, which provide a favorable environment for an embryo to develop.
High levels of estrogens and progesterone inhibit the anterior pituitary gland’s release of LH (luteinizing hormone) and FSH (follicle-stimulating hormone). Consequently, no other follicles are stimulated to complete development when the corpus luteum is active. However, if the secondary oocyte released at ovulation is not fertilized, the corpus luteum begins to degenerate (regress) on about the twenty-fourth day of the cycle. Eventually, connective tissue replaces it. The remnant of such a corpus luteum is called a corpus albicans, and is eventually absorbed.
When the corpus luteum ceases to function, concentrations of estrogens and progesterone rapidly decline, and in response, blood vessels in the endometrium constrict. This reduces the supply of oxygen and nutrients to the thickened endometrium (stratum functionalis and stratum basalis), and these lining tissues soon disintegrate and slough off. At the same time, blood leaves damaged capillaries, creating a flow of blood and cellular debris that passes through the vagina as the menstrual flow (menses). This flow usually begins about the twenty-eighth day of the cycle and continues for three to five days, while the concentrations of estrogens are relatively low. The beginning of the menstrual flow marks the end of a menstrual cycle and the beginning of the next cycle as a new developing antral follicle becomes available.
Low blood concentrations of estrogens and progesterone at the beginning of the menstrual cycle mean that the hypothalamus and anterior pituitary gland are no longer inhibited. Consequently, FSH (follicle-stimulating hormone) and LH (luteinizing hormone) concentrations soon increase, stimulating a new antral follicle to mature. As this follicle secretes estrogens, the uterine lining undergoes repair, and the endometrium begins to thicken again.
Day 1
The first day of bleeding is considered the first day of the menstrual cycle. After bleeding ends, usually around day 5, levels of the hormone estrogen begin to rise. The rise in estrogen causes the lining of the uterus to thicken as it prepares to hold a fertilized egg. At the same time, the changes in hormone levels cause follicles (the sacs in the ovary that contain eggs) to grow and mature, in preparation for one follicle to go through ovulation.
Ovulation
Around day 12 to 14 in an average 28-day cycle, the egg is released from a follicle on the ovary in a process called ovulation. Ovulation can occur anywhere between 10 and 21 days after the first day of a woman’s menstrual cycle. Ovulation is when the ovary releases an egg so it can be fertilized by a sperm to make a baby. A woman is most likely to get pregnant if she has sex without birth control in the three days before and up to the day of ovulation.
It may be difficult to know when you ovulate, but you can watch for signs. A few days before you ovulate, your vaginal mucus or discharge changes and becomes
more slippery and clear. A woman can also tell when she has begun ovulating using several methods, including at-home tests that measure levels of luteinizing hormone (LH) in the urine and keeping track of her body temperature, which typically rises slightly at ovulation. At mid-cycle, some women experience pain on one side of their pelvic area; this pain is called “Mittelschmerz” (meaning “middle pain,” because it occurs in the middle of the cycle) and may be a signal of ovulation 2.
More than 90 percent of women say they get symptoms of premenstrual syndrome (PMS) in the time after ovulation and before their period starts.
If a pregnancy does not occur, decreasing hormone levels signal for the lining of the uterus, called the endometrium, to be shed during menstruation.
The endometrium builds up and breaks down during the menstrual cycle. The endometrium is thickest halfway through the 28-day cycle. Then, if there is no pregnancy, it breaks down. This breakdown causes the bleeding of the menstrual phase. Figure 5 above illustrates an average 28-day cycle.
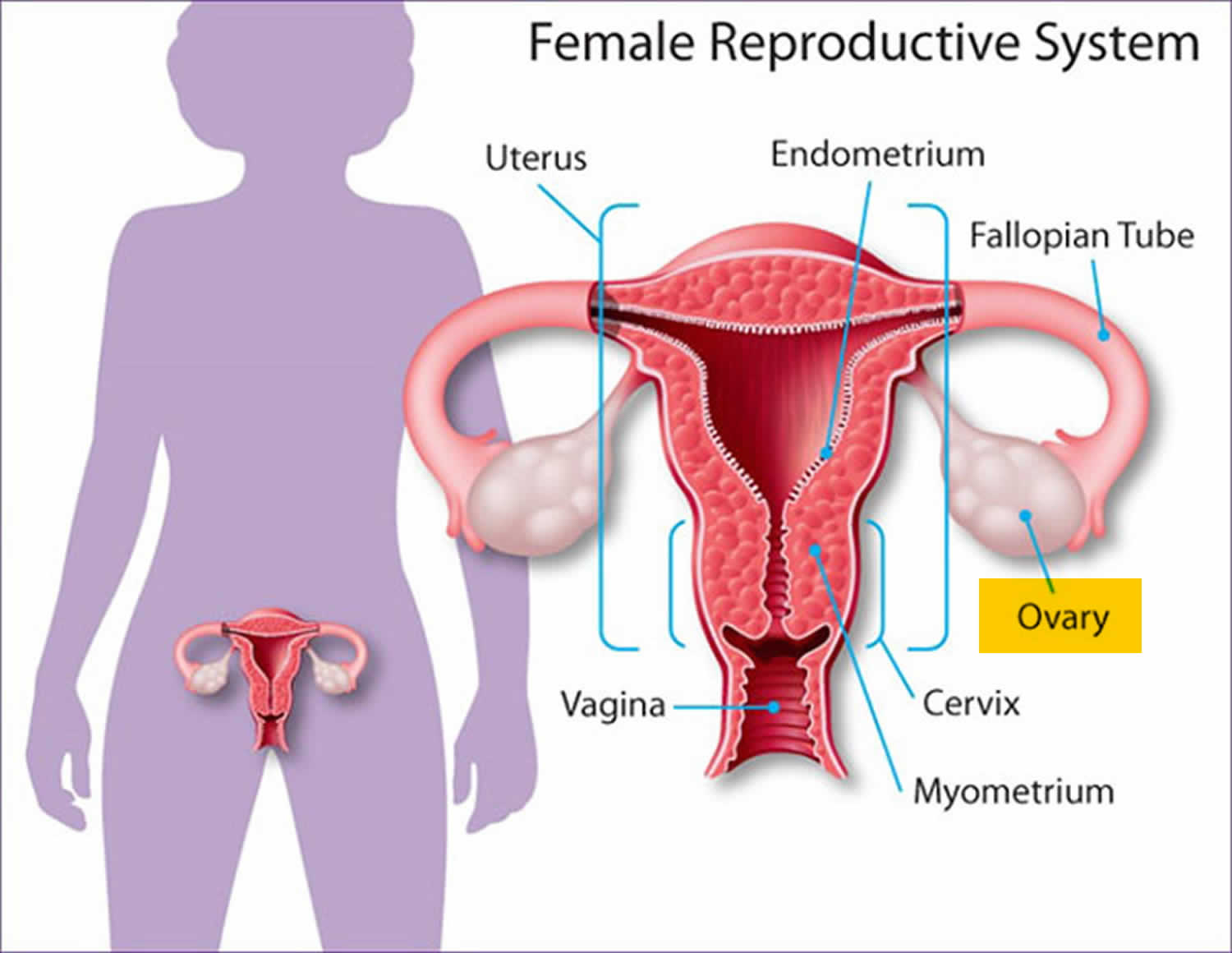
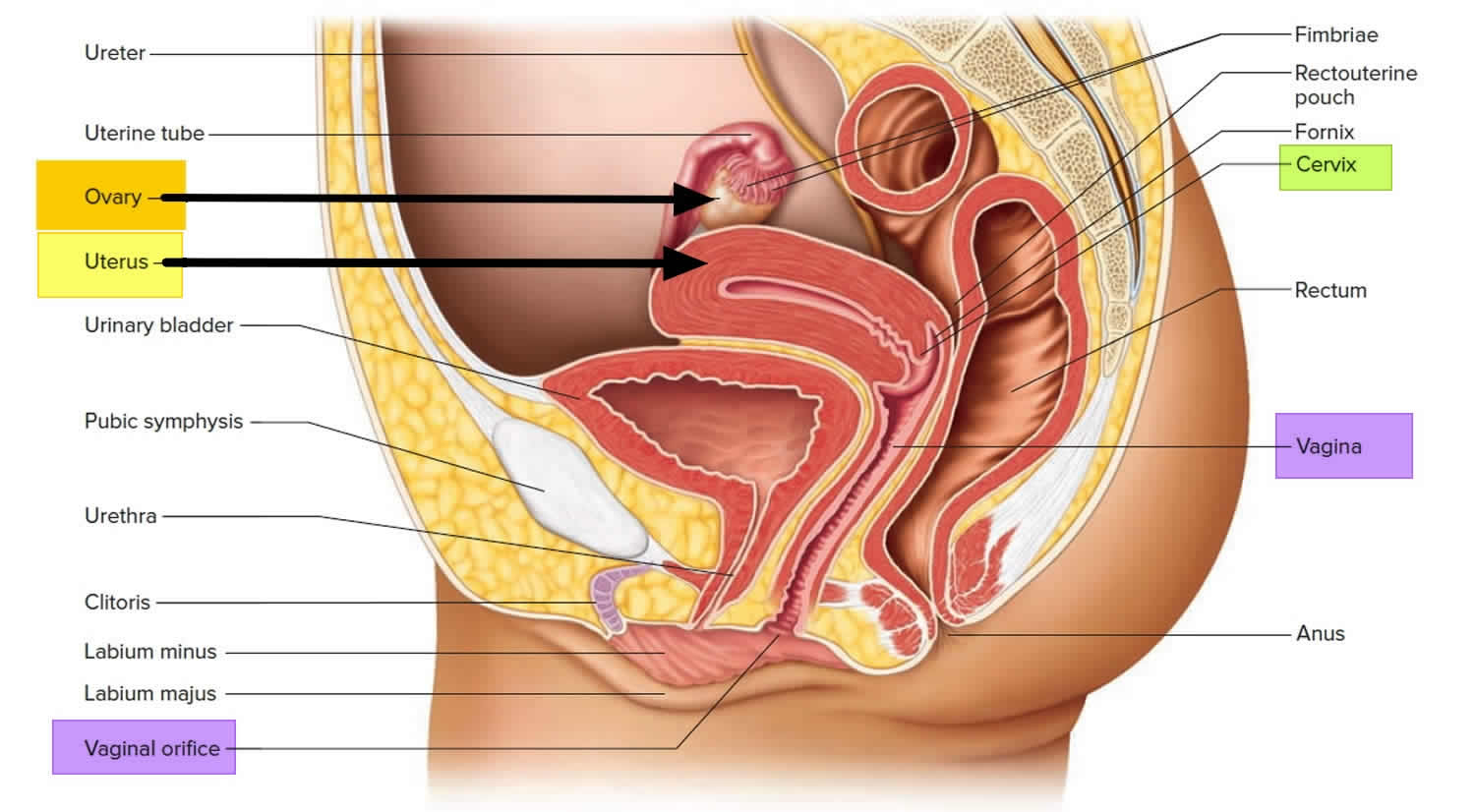
Figure 1. Female reproductive organs
Figure 3. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Figure 4. Ovarian activity during the Menstrual cycle
 Footnote: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
Footnote: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
What happens if a pregnancy occurs?
Fertilization
After ovulation, the egg (ovum) moves down the fallopian tube (also called uterine tube). The sperm can fertilize the egg at this point. After the sperm is ejaculated into the vagina, it moves into the cervix and through the uterus into the fallopian tube (uterine tube). Sperm can live up to 5 days in a woman’s body.
If fertilization occurs, the newly formed embryo travels through the fallopian tube into the uterus, where it implants in the wall of the uterus. If fertilization does not occur, the egg naturally breaks down, and the uterine wall is lost in the form of menstrual bleeding.
Implantation
The embryo must successfully implant into the thickened wall of the uterus for the pregnancy to occur. The embryo first attaches to the wall of the uterus around 5 or 6 days after ovulation. It becomes more firmly implanted between 6 and 12 days after ovulation. Implantation causes a release of human chorionic gonadotropin (hCG)—a hormone that signals the body to change to support the pregnancy. This hormone is what a pregnancy test detects.
Progesterone test
Progesterone test measures the level of progesterone in the blood. Most of the time, blood is drawn from a vein located on the inside of the elbow or the back of the hand.
Progesterone plays a key role in pregnancy. Progesterone is produced after ovulation in the second half of the menstrual cycle (see Figure 4 above). It helps make a woman’s uterus ready for a fertilized egg to be implanted. Progesterone also prepares the uterus for pregnancy by inhibiting the uterine muscle to contract and the breasts for milk production.
Levels of progesterone will be naturally higher during pregnancies that involve multiples (twins, triplets, etc.) than those in which there is only one fetus.
Taking estrogen and progesterone supplements can affect results.
Men will also have small amounts of progesterone in their blood.
A limited number of laboratories can perform progesterone testing on saliva.
A progesterone test may be used:
- To help recognize and manage some causes of infertility. Since progesterone levels vary throughout the menstrual cycle, multiple (serial) measurements can be used for this purpose.
- To determine whether or not a woman has ovulated, when ovulation occurred, or to monitor the success of induced ovulation
- In early pregnancy to help diagnose an ectopic or failing pregnancy, along with human chorionic gonadotropin (hCG) testing
- To monitor a high-risk pregnancy to help evaluate placenta and fetal health
- If a woman is receiving progesterone injections to help support her early pregnancy, to help determine the effectiveness of the replacement treatment
- Along with other tests such as an follicle-stimulating hormone (FSH), luteinizing hormone (LH), human chorionic gonadotropin (hCG), thyroid tests, clotting tests, and a complete blood count (CBC) to help determine the cause of abnormal uterine bleeding in non-pregnant women.
How to prepare for the progesterone test
Many medicines can interfere with blood test results.
- Your health care provider will tell you if you need to stop taking any medicines before you have this test.
- DO NOT stop or change your medicines without talking to your provider first.
If I am menopausal and on hormone replacement therapy, is there ever a need to monitor my progesterone level?
Sometimes. If you still have your uterus and are having symptoms, such as unexplained uterine bleeding, your health care provider may order a progesterone test along with other tests and procedures. If you do not have a uterus (removed during a hysterectomy), your hormone replacement therapy (HRT) will not include progesterone and it will not need to be checked.
Are men tested for progesterone?
Not usually, unless specific adrenal diseases are suspected. Progesterone does not have an established role in males.
When is progesterone test ordered?
Progesterone levels are measured:
- During an infertility assessment, when a woman is having trouble getting pregnant and her health care provider wants to verify that she is ovulating normally; the test may be ordered a few times during a woman’s menstrual cycle to evaluate the change in progesterone concentrations.
- When it is necessary to determine when ovulation has occurred and following drug therapy to induce ovulation
- When symptoms, such as abdominal pain and spotting, suggest an ectopic pregnancy or threatened miscarriage
- On a regular basis when a woman requires progesterone replacement therapy to help maintain her pregnancy
- Periodically throughout a high-risk pregnancy to monitor placenta and fetal health
- When a non-pregnant woman is experiencing abnormal uterine bleeding
Normal progesterone levels
Progesterone levels vary, depending on the timing when the progesterone test is done. Blood progesterone levels start to rise midway through the menstrual cycle. It continues to rise for about 6 to 10 days, and then falls if the egg is not fertilized.
Levels continue to rise in early pregnancy.
The following are normal progesterone levels based upon certain phases of the menstrual cycle and pregnancy:
- Female (pre-ovulation): less than 1 nanogram per mililiter (ng/mL) or 3.18 nanomoles per liter (nmol/L)
- Female (mid-cycle): 5 to 20 ng/mL or 15.90 to 63.60 nmol/L
- Male: less than 1 ng/mL or 3.18 nmol/L
- Postmenopausal: less than 1 ng/mL or 3.18 nmol/L
- Pregnancy 1st trimester: 11.2 to 90.0 ng/mL or 35.62 to 286.20 nmol/L
- Pregnancy 2nd trimester: 25.6 to 89.4 ng/mL or 81.41 to 284.29 nmol/L
- Pregnancy 3rd trimester: 48 to 150 to 300 or more ng/mL or 152.64 to 477 to 954 or more nmol/L
Normal progesterone value ranges may vary slightly among different laboratories. Talk to your healthcare provider about the meaning of your specific test results.
The examples above show the common measurements for results for progesterone tests. Some laboratories use different measurements.
What does abnormal progesterone test result mean?
Interpretation of progesterone test results depends on the reason for testing and requires knowledge of the point at which a woman is in her menstrual cycle or pregnancy. Progesterone levels usually start to elevate when an egg is released from the ovary, rise for several days, and then either continue to rise with early pregnancy or fall to initiate menstruation.
If progesterone levels do not rise and fall on a monthly basis, a woman may not be ovulating nor having regular menstrual periods. This may be a cause of infertility.
If levels do not rise normally during an early pregnancy, the pregnancy may be ectopic and/or may be failing. If serial measurements do not show increasing progesterone levels over time, there may be problems with the viability of the placenta and fetus.
High progesterone levels
High progesterone levels are seen occasionally with:
- Pregnancy
- Some ovarian cysts
- Non-viable pregnancies known as molar pregnancies
- A rare form of ovarian cancer
- Overproduction of progesterone by the adrenal glands
- Adrenal cancer
- Congenital adrenal hyperplasia (CAH)
Low progesterone levels
Low progesterone levels may be associated with:
- Toxemia late in pregnancy (preeclampsia)
- Decreased function of ovaries
- Lack of menstruation (amenorrhea) – no periods as result of anovulation (ovulation does not occur)
- Irregular periods
- Ectopic pregnancy
- Fetal death/miscarriage
Progesterone in pregnancy
Progesterone is a hormone secreted by the ovary and plays an important role in normal pregnancy. A number of studies 3, 4, 5, 6 have been undertaken to determine whether the use of progesterone supplements have a benefit in the luteal phase of the menstrual cycle and in early pregnancy. There is no evidence to suggest that giving progesterone supplements, either natural or synthetic progesterone, to otherwise healthy women in the first trimester of pregnancy reduces the risk of spontaneous miscarriage and should not be used 7. However, for some women who experience bleeding in early pregnancy, the use of progesterone supplements may reduce the risk of miscarriage. This conclusion is based on data from a meta-analysis of four randomized controlled trials including 411 women 8. For women who become pregnant with in-vitro fertilization (IVF), the use of progesterone supplements is beneficial and improves pregnancy outcomes 5.
Footnote: Progestogens, also sometimes written progestagens or gestagens 9, are a class of steroid hormones that bind to and activate the progesterone receptor 10. The progestogens are named for their function in maintaining pregnancy (i.e., progestational), although they are also present at other phases of the estrous and menstrual cycles 10. Progestogen is the generic term for a progestational agent and progesterone (P4) is a single chemical entity and the primary progestogenic hormone synthesised by the human body 11. Progesterone should not be confused with or considered the same as progestins (synthetic progestogens). The term progestin can be used to refer to synthetic progestational agents.
What is the role of progestogen supplementation in unselected populations of women in the first trimester of pregnancy?
For an unselected population of women in the first trimester of pregnancy, there is no evidence of benefit of progestogen therapy, either natural or synthetic, to in the prevention of miscarriage and should not be used 12, 13.
In women presenting with a clinical diagnosis of threatened miscarriage
For women presenting with a clinical diagnosis of threatened miscarriage, there is preliminary evidence of a reduction in the rate of spontaneous miscarriage with the use of progestins. This conclusion is based on data from a meta-analysis of four randomized controlled trials including 411 women 8. Miscarriage was significantly less likely to occur in women receiving progestogens than those receiving placebo or no treatment. There was no evidence of increase in the rate of antepartum hemorrhage, hypertensive disorders of pregnancy, or fetal anomalies 14. A further systematic review of the use of oral dydrogesterone (progestin medication) demonstrated a significant reduction in the rate of miscarriage for women presenting with a threatened miscarriage from 24% to 11% with a favorable safety profile 8.
The current evidence for the use of progestogen support in threatened miscarriage is limited by methodological inconsistencies. Whilst the current evidence shows potential benefit, further well-designed clinical trials would add strength to the current evidence base.
What is the role of progestogen supplementation in women presenting with a clinical diagnosis of threatened miscarriage?
Progestogen supplementation until the second trimester in women presenting with a clinical diagnosis of threatened miscarriage may reduce the rate of spontaneous miscarriage and may be considered 14, 15.
In women with a history of unexplained recurrent miscarriage
In women with a history of unexplained recurrent miscarriage the PROMISE trial 6 showed no difference in the rate of miscarriage in women using vaginal micronized progesterone compared to placebo. This trial included 836 women who conceived spontaneously who were randomly assigned to receive either twice-daily progesterone from 6-12 weeks’ gestation (404 women) or placebo (432 women). The live birth rate by intention to treat analysis was 66% in the trial group and 63% controls. There were no significant differences in adverse events.
By contrast, a recent meta-analysis 4 of ten trials including 1,586 women with recurrent miscarriage showed that women with a history of unexplained recurrent miscarriage who were randomised to receive progestogens in the first trimester had a lower risk of miscarriage. However, the addition of the negative result of the PROMISE trial 4 to this meta-analysis 4 would likely eliminate any significant benefit of progestogens in this context.
It should be noted that there is significant heterogeneity in the clinical trials of progestogens and the possibility of a benefit from some forms of progestogen supplementation in women with recurrent miscarriage cannot be excluded. Further well-designed studies are required to address this question, but at this stage there is insufficient evidence to support this practice and it is not recommended outside of the setting of appropriately designed clinical trials.
What is the role of progestogen supplementation in women with a history of recurrent miscarriage?
The routine use of progestogens for patients presenting with recurrent spontaneous miscarriage does not improve pregnancy outcomes and is not recommended 6, 4.
Role of luteal phase progestogen support in assisted reproductive technologies (ART)
For luteal support in in-vitro-fertilization (IVF), exogenous progesterone is associated with a significantly higher pregnancy rate than placebo or no treatment, with better results obtained with synthetic progestogens than micronized progesterone 5, 16. Furthermore, there is no evidence to favour a specific route or duration of administration of progestogens. Currently, synthetic progesterone is the best option for luteal phase support in women undergoing assisted reproductive technologies ART treatment.
A recent non-inferiority randomized controlled trial demonstrated equal efficacy and tolerability of oral dydrogesterone and vaginal micronized progesterone. It is important to note that in this study luteal support was continued to 12 weeks’ gestation which is not routine practice.
What is the role of luteal phase progestogen support in assisted reproductive technologies?
Luteal phase support with synthetic progestogens should be provided in in-vitro-fertilization (IVF) as it is associated with an improved live birth rate 5.
Progesterone use in the second and third trimester of pregnancy for the prevention of preterm birth
Preterm birth is the leading cause of neonatal mortality, and so prevention of preterm birth is a high priority in obstetric care. Approximately two thirds of all preterm birth occur spontaneously, with the other third being so-called ‘indicated preterm births’, usually where there is concern about fetal growth, or maternal medical conditions, such as pre-eclampsia.
The role of progesterone in the prevention of preterm birth has been the subject of several randomized controlled trials in the last decade, both for women with a previous spontaneous preterm birth or for those with a sonographically confirmed short cervix at the time of routine midtrimester ultrasound. These trials have re-ignited interest in the use of progesterone to reduce the risk of preterm birth. These studies 17, 18, 19 have contributed to recent meta-analyses, suggesting that progesterone reduces the risk of preterm birth in women with a previous history of spontaneous preterm birth. A recent large randomized controlled trial 20 however published in 2016, showing no benefit, was not included.
These meta-analysis do however confirm that progesterone reduces the risk of preterm birth in women found to have a short cervix using a standardized transvaginal technique at the time of the routine anomaly scan.
Conclusion
Vaginal progesterone therapy is recommended for women who are found to have a short cervix at the time of the routine midtrimester scan. Current evidence suggests that progesterone reduces the risk of preterm birth in these women, with evidence of improved perinatal outcomes. It remains to be determined how these benefits will translate into long term health benefits, and further research is also needed to determine both the optimal timing, dose and administration of progesterone. Participation in relevant clinical trials should be encouraged.
Summary of recommendations 21
- Recommendation 1: Vaginal progesterone therapy is recommended for asymptomatic women with a short cervix (<25 mm) on transvaginal cervical length assessment in the midtrimester.
- Recommendation 2: Progesterone therapy should be considered for women with a singleton pregnancy with a history of previous spontaneous preterm singleton birth.
What are the management considerations for patients with a history of spontaneous preterm birth?
Systematic review and meta-analysis of five randomized trials in women with a history of spontaneous preterm birth suggest a significant risk reduction in both preterm birth, perinatal mortality and major morbidity among women receiving progesterone 19. However, this meta-analysis does not include the OPPTIMUM trial 20 published in 2016, that shows no reduction in preterm birth with the use of progesterone in women with a previous history of preterm birth. An updated meta-analysis including this trial is awaited.
It needs to be appreciated that there are many potential contributors to spontaneous preterm birth, which may account for significant heterogeneity between study findings. For example, among women with a past history of preterm birth, cervical surveillance may identify those with cervical shortening (see below) who may benefit most from progesterone administration. In addition, the majority of these studies have used intramuscular rather than transvaginal progesterone, and further studies are needed to better define the role of vaginal progesterone in women with a past history of preterm birth. Further studies will also address the optimal dose, timing and administration of progesterone, and provide useful data on how these short term benefits may translate into longer term health outcomes in infancy and childhood.
What are the management considerations for asymptomatic women with a short cervix at 18-24 weeks?
A short cervix detected with transvaginal ultrasound in the mid trimester is a powerful predictor of spontaneous preterm birth. Several large randomized controlled trials have confirmed a significant reduction in the risk of spontaneous preterm birth among asymptomatic women administered progesterone following the diagnosis of a short cervix on transvaginal ultrasound 22. A recent updated meta-analysis 23 demonstrated that vaginal progesterone reduces the risk of preterm birth prior to 34 weeks’ from 27.5% to 18.1% among women with a short cervix (25mm or less). The largest trial included women with a transvaginal sonographic cervical length between 10 and 20mm 22. Treatment with progesterone was also shown to reduce the risk of preterm birth at <28 to <36 weeks’ gestation, as well as showing significant reductions in respiratory distress, composite neonatal morbidity and mortality, birth weight <1500g and admission to NICU (neonatal intensive care unit), although the risk reduction for perinatal mortality was not significant.
What other indications should be considered when using Progesterone to prevent preterm birth?
Despite their increased risk of preterm birth, routine administration of progesterone from 24 weeks has not been shown to reduce the risk of preterm birth in multiple pregnancies 24. In multiple pregnancies where a short cervix has been noted, progesterone has also not been shown to significantly reduce the risk of preterm birth 25, but it should be noted that the numbers in some of these trials are small. In one metaanalysis, progesterone administration in twins with a short cervix has been reported to be associated with a significant reduction in preterm birth <33 weeks’ gestation and in composite neonatal morbidity/ mortality 26. More research is needed to determine if there is a subset of multiple pregnancies that may benefit from progesterone.
Several studies have evaluated the role of progesterone in populations with varied risk factors, including a history of uterine malformation or of ‘cervical incompetence’. The heterogeneity of the studies, and the numbers involved do not give sufficient power to determine whether treatment for these indications is effective 17. There are limited data supporting its use as a long term tocolytic for women who present with threatened preterm labour at <34 weeks gestation and further research is needed to examine the role of progesterone in this context 27.
What is the ideal route of administration and the correct dosage?
A variety of progestins have been used in the preterm birth prevention trials. The US datasets predominantly use 17-alpha-hydroxyprogesterone caproate, given as a weekly intramuscular injection.
Vaginal pessaries of progesterone are available and have the potential advantage of high uterine bioavailability and few systemic side effects, although vaginal irritation can be problematic. This route of administration has been studied using doses of 90mg – 400mg and the optimal dosage is not clearly established, although the recent meta-analysis of Romero et al. 23 showed no difference in effect between 90-100mg and 200 mg progesterone pessaries for women with a short cervix.
Timing of therapy has also varied between studies, stating as early as 16 weeks of gestation in women with a previous history of spontaneous preterm delivery and continuing to 37 weeks is some trials. Early cessation of 17 alpha-hydroxyprogesterone caproate has been associated with an increased risk for recurrent preterm delivery 28.
Commencing progesterone therapy in the second trimester (i.e. 16-24 weeks) of pregnancy appears to be safe for both the mother and the fetus and no teratogenic effects have been observed. Infants recruited to the NICHD (National Institute of Child Health and Human Development) trial whose mothers received 17 alpha-hydroxyprogesterone caproate were followed to four years of age and no detrimental effects were observed 29.
Progesterone Medications
Progesterone is used as a part of hormone replacement therapy in women who have passed menopause (the change of life) and have not had a hysterectomy (surgery to remove the uterus). Hormone replacement therapy usually includes estrogen, which is used to treat symptoms of menopause and reduce the risk of developing certain diseases. However, estrogen can also cause abnormal thickening of the lining of the uterus and increase the risk of developing uterine cancer. Progesterone helps to prevent this thickening and decreases the risk of developing uterine cancer. Progesterone is also used to bring on menstruation (period) in women of childbearing age who have had normal periods and then stopped menstruating. Progesterone is in a class of medications called progestins (female hormones). It works as part of hormone replacement therapy by decreasing the amount of estrogen in the uterus. It works to bring on menstruation by replacing the natural progesterone that some women are missing.
How should progesterones medicine be used?
Progesterone comes as a capsule to take by mouth. It is usually taken once a day in the evening or at bedtime. You will probably take progesterone on a rotating schedule that alternates 10 to 12 days when you take progesterone with 16 to 18 days when you do not take the medication. Your doctor will tell you exactly when to take progesterone. To help you remember to take progesterone, take it around the same time in the evening. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take progesterone exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Continue to take progesterone as directed even if you feel well. Do not stop taking progesterone without talking to your doctor.
Progesterone medicine special precautions
Before taking progesterone:
- tell your doctor and pharmacist if you are allergic to progesterone, oral contraceptives (birth control pills), hormone replacement therapy, any other medications, or peanuts.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements you are taking. Be sure to mention any of the following: amiodarone (Cordarone, Pacerone); antifungals such as fluconazole (Diflucan), itraconazole (Sporanox), and ketoconazole (Nizoral); cimetidine (Tagamet); clarithromycin (Biaxin); cyclosporine (Neoral, Samdimmune); danazol (Danocrine); delaviridine (Rescriptor); diltiazem (Cardizem, Dilacor, Tiazac); erythromycin (E.E.S, E-Mycin, Erythrocin); fluoxetine (Prozac, Sarafem); fluvoxamine (Luvox); HIV protease inhibitors such as indinavir (Crixivan), ritonavir (Norvir), and saquinavir (Fortovase); isoniazid (INH, Nydrazid); lansoprazole (Prevacid, Prevpac); metronidazole (Flagyl); nefazodone (Serzone); omeprazole (Prilosec); oral contraceptives (birth control pills); ticlopidine (Ticlid); troleandomycin (TAO); verapamil (Calan, Covera, Isoptin, Verelan); and zafirlukast (Accolate). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking, especially St. John’s wort.
- tell your doctor if you have or have ever had unexplained vaginal bleeding between periods; a miscarriage in which some tissue was left in the uterus; cancer of the breasts or female organs; seizures; migraine headaches; asthma; diabetes; depression; blood clots in the legs, lungs, eyes, brain, or anywhere in the body; stroke or ministroke; vision problems; or liver, kidney, heart, or gallbladder disease .
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking progesterone, call your doctor.
if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking progesterone. - you should know that progesterone may make you dizzy or drowsy. Do not drive a car or operate machinery until you know how this medication affects you. If progesterone does make you dizzy or drowsy, take your daily dose at bedtime.
- you should know that progesterone may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. This is more common when you first start taking progesterone. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up.
Progesterone dosage
Adult Dose for Amenorrhea
Use: Treatment of secondary amenorrhea
Oral capsules and tablets:
- 400 mg orally once a day (at bedtime) for 10 days
4% vaginal gel:
- Administer 45 mg vaginally every other day, up to a total of 6 doses
- If no response, may try 90 mg of the 8% gel vaginally every other day, up to a total of 6 doses
- Dosage increase may only be accomplished using the 8% gel; increasing the volume of the 4% gel does not increase the amount of progesterone absorbed.
Intramuscular injection:
- 5 to 10 mg intramuscularly once a day for 6 to 8 consecutive days
- If ovarian activity is sufficient to produce a proliferative endometrium, withdrawal bleeding is expected 48 to 72 hours after the last injection.
- Spontaneous normal cycles may follow withdrawal bleeding.
Adult Dose for Uterine Bleeding
Use: Abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology, such as submucous fibroids or uterine cancer
- 5 to 10 mg intramuscularly once a day for 6 doses
Comments:
- Bleeding may be expected to cease within 6 days.
- If estrogen is also given, start progesterone 2 weeks after starting estrogen.
- Discontinue if menstrual flow begins during the injections.
Adult Dose for Endometrial Hyperplasia – Prophylaxis
Use: Prevention of endometrial hyperplasia in postmenopausal women with uteruses who are receiving daily conjugated estrogens
- 200 mg orally once a day (at bedtime) for 12 consecutive days per 28 day cycle
Adult Dose for Fetal Maturation
Use: To support embryo implantation and early pregnancy by supplementation of corpus luteal function as part of an assisted reproductive technology (ART) treatment program for infertile women.
Vaginal insert:
- Initial dose: 100 mg vaginally 2 to 3 times a day, starting the day after oocyte retrieval
- Duration of therapy: Up to 10 weeks total.
8% vaginal gel:
- 90 mg vaginally once a day for progesterone supplementation
or - 90 mg vaginally twice a day with partial or complete ovarian failure requiring progesterone supplementation
- Duration of therapy: Up to 10 to 12 weeks, until placental autonomy is achieved
Comments:
- Efficacy and dosing in women over 35 has not been clearly established.
Adult Dose for Progesterone Insufficiency
Use: To support embryo implantation and early pregnancy by supplementation of corpus luteal function as part of an assisted reproductive technology (ART) treatment program for infertile women.
Vaginal insert:
- Initial dose: 100 mg vaginally 2 to 3 times a day, starting the day after oocyte retrieval
- Duration of therapy: Up to 10 weeks total.
8% vaginal gel:
- 90 mg vaginally once a day for progesterone supplementation
or - 90 mg vaginally twice a day with partial or complete ovarian failure requiring progesterone supplementation
- Duration of therapy: Up to 10 to 12 weeks, until placental autonomy is achieved
Comments:
- Efficacy and dosing in women over 35 has not been clearly established.
Adult Dose for Female Infertility
Use: To support embryo implantation and early pregnancy by supplementation of corpus luteal function as part of an assisted reproductive technology (ART) treatment program for infertile women.
Vaginal insert:
- Initial dose: 100 mg vaginally 2 to 3 times a day, starting the day after oocyte retrieval
- Duration of therapy: Up to 10 weeks total.
8% vaginal gel:
- 90 mg vaginally once a day for progesterone supplementation
or - 90 mg vaginally twice a day with partial or complete ovarian failure requiring progesterone supplementation
- Duration of therapy: Up to 10 to 12 weeks, until placental autonomy is achieved
Comments:
- Efficacy and dosing in women over 35 has not been clearly established.
Renal Dose Adjustments
- Data not available.
Liver Dose Adjustments
- Contraindicated
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Progesterone side effects
Progesterone may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- headache
- breast tenderness or pain
- upset stomach
- vomiting
- diarrhea
- constipation
- tiredness
- muscle, joint, or bone pain
- mood swings
- irritability
- excessive worrying
- runny nose
- sneezing
- cough
- vaginal discharge
- problems urinating
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
- breast lumps
- migraine headache
- severe dizziness or faintness
- slow or difficult speech
- weakness or numbness of an arm or leg
- lack of coordination or loss of balance
- shortness of breath
- fast heartbeat
- sharp chest pain
- coughing up blood
- leg swelling or pain
- loss of vision or blurred vision
- bulging eyes
- double vision
- unexpected vaginal bleeding
- shaking hands that you cannot control
- seizures
- stomach pain or swelling
- depression
- hives
- skin rash
- itching
- difficulty breathing or swallowing
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- hoarseness
Laboratory animals who were given progesterone developed tumors. It is not known if progesterone increases the risk of tumors in humans. Talk to your doctor about the risks of taking this medication.
Medications like progesterone may cause abnormal blood clotting. This may cut off the blood supply to the brain, heart, lungs, or eyes and cause serious problems. Call your doctor if you experience any of the symptoms listed above as serious side effects. Talk to your doctor about the risks of taking this medication.
Progesterone may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting program online (https://www.fda.gov/Safety/MedWatch/default.htm).
Progesterone injection
Indications and usage:
Progesterone injection is intended for administration by injection into a muscle mass. Following injection, the medication is absorbed into the bloodstream.
Progesterone injection is indicated in amenorrhea and abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology, such as submucous fibroids or uterine cancer.
Your doctor will provide instructions regarding the dose and manner in which progesterone injection should be injected. Follow your doctor’s instructions closely. If you have any questions about progesterone injection administration, ask your doctor or health-care provider.
Contraindications
- Current or past history of thrombophlebitis, thromboembolic disorders, or cerebral apoplexy.
- Liver dysfunction or disease.
- Known or suspected malignancy of breast or genital organs.
- Undiagnosed vaginal bleeding.
- Missed abortion.
- Known sensitivity to Progesterone injection.
Warnings
The physician should be alert to the earliest manifestations of thrombotic disorders (thrombophlebitis, cerebrovascular disorders, pulmonary embolism, and retinal thrombosis). Should any of these occur or be suspected, the drug should be discontinued immediately.
Medication should be discontinued pending examination if there is a sudden partial or complete loss of vision, or if there is a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, medication should be withdrawn.
When you should not use progesterone injection:
- If you are allergic to Progesterone, Progesterone-like drugs, benzyl alcohol or sesame oil/seeds.
- If you have unusual vaginal bleeding which has not been evaluated by your doctor.
- If you have liver disease.
- If you have known or suspected cancer of the breast or genital organs.
- If you have a miscarriage and your physician suspects some tissue is still in the uterus.
- If you have or have had blood clots in the legs, lungs, eyes, or elsewhere.
Risks of progesterone injection
Abnormal blood clotting. Blood clots have been reported with the use of estrogens and progestational drugs (alone or in combination). If blood clots do form in your bloodstream, they can cut off the blood supply to vital organs, causing serious problems. These problems may include a stroke (by cutting off blood to part of the brain), a heart attack (by cutting off blood to part of the heart), a pulmonary embolus (by cutting off blood to part of the lungs), or other problems. Any of these conditions may cause death or serious long-term disability. Call your doctor immediately if you suspect you have any of these conditions. He or she may advise you to stop using this drug.
Be alert for unusual signs and symptoms. If any of these warning signals (or any other unusual symptoms) happen while you are using Progesterone Injection, call your doctor immediately:
- Abnormal bleeding from the vagina.
- Pains in the calves or chest, a sudden shortness of breath or coughing blood indicating possible clots in the legs, heart, or lungs.
- Severe headache or vomiting, dizziness, faintness, or changes in vision or speech, weakness or numbness of an arm or leg indicating possible clots in the brain or eye.
- Breast lumps, which could be associated with fibrocystic disorders, fibroadenoma, or breast cancer. (Ask your doctor or health-care provider to show you how to examine your breasts monthly.)
- Yellowing of the skin and/or white of the eyes indicating possible liver problems.
Precautions
General
The pretreatment physical examination should include special reference to breast and pelvic organs, as well as a Papanicolaou smear.
Because progestational drugs may cause some degree of fluid retention, conditions which might be influenced by this condition, such as epilepsy, migraine, asthma, cardiac, or renal dysfunction, require careful observation.
In cases of breakthrough bleeding, as in all cases of irregular bleeding per vaginum, nonfunctional causes should be borne in mind, and adequate diagnostic measures undertaken.
Patients who have a history of psychic depression should be carefully observed and the drug discontinued if the depression recurs to a serious degree.
The age of the patient constitutes no absolute limiting factor although treatment with progestin may mask the onset of the climacteric.
The pathologist should be advised of progestin therapy when relevant specimens are submitted.
There are possible risks which may be associated with the use of progestin treatment, including adverse effects on carbohydrate and lipid metabolism. The dosage used may be important in minimizing these adverse effects.
A decrease in glucose tolerance has been observed in a small percentage of patients on estrogen-progestin combination treatment. The mechanism of this decrease is obscure. For this reason, diabetic patients should be carefully observed while receiving such therapy.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Long-term intramuscular administration of MedroxyProgesterone acetate (MPA) has been shown to produce mammary tumors in beagle dogs. There is no evidence of a carcinogenic effect associated with the oral administration of MPA to rats and mice.
MedroxyProgesterone acetate was not mutagenic in a battery of in vitro or in vivo genetic toxicity assays.
Progesterone at high doses is an antifertility drug and high doses would be expected to impair fertility until the cessation of treatment.
Geriatric Use
The safety and effectiveness in geriatric patients (over age 65) have not been established.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Nursing Mothers
Detectable amounts of drug have been identified in the milk of mothers receiving progestational drugs. The effect of this on the nursing infant has not been determined.
Side effects
Breakthrough bleeding; spotting; change in menstrual flow; amenorrhea; edema; change in weight (increase or decrease); changes in cervical erosion and cervical secretions; cholestatic jaundice; breast tenderness and galactorrhea; pain, irritation, and/or redness at the injection area; skin sensitivity reactions consisting of urticaria, pruritus, edema and generalized rash; acne, alopecia and hirsutism; rash (allergic) with and without pruritus; anaphylactoid reactions; mental depression; pyrexia; insomnia; nausea; and somnolence.
A statistically significant association has been demonstrated between use of estrogen-progestin combination drugs and pulmonary embolism and cerebral thrombosis and embolism. For this reason patients on progestin therapy should be carefully observed. There is also evidence suggestive of an association with neuro-ocular lesions, e.g., retinal thrombosis and optic neuritis.
The following adverse reactions have been observed in patients receiving estrogen-progestin combination drugs: Rise in blood pressure in susceptible individual, premenstrual syndrome, changes in libido, changes in appetite, cystitis-like syndrome, headache, nervousness, fatigue, backache, hirsutism, loss of scalp hair, erythema multiforme, erythema nodosum, hemorrhagic eruption, itching, and dizziness.
The following laboratory results may be altered by the use of estrogen-progestin combination drugs: increased sulfobromophthalein retention and other hepatic function tests; coagulation tests: increase in prothrombin factors VII, VIII, IX, and X; metyrapone test; pregnanediol determinations; thyroid function: increase in PBI, and butanol extractable protein bound iodine and decrease in T3 uptake values.
Possible side effects of progesterone injection
The following side effects have been reported with Progesterone Injection. Consult your doctor if you experience any of the side effects mentioned below, or other side effects:
- breakthrough bleeding
- spotting
- changes in menstrual flow
- amenorrhea
- change in weight (increase or decrease)
- pain, irritation, swelling, and/or redness at the injection area
- general swelling
- vaginal discharge
- yellow discoloration of skin or white of eyes
- breast tenderness, discharge from the nipple
- skin reactions including rash, hives, itching, and swelling
- acne
- hair loss or growth of new hair
- mental depression
- fever
- insomnia or sleepiness*
- nausea
- anaphylactoid (life-threatening allergic) reaction with symptoms that may include a sense of uneasiness or apprehension; flushing; fast, throbbing
- heartbeat; itching; hives; difficult breathing; swelling of the throat; fainting; nausea; vomiting; or convulsions.
*If you experience sleepiness, do not drive or operate machinery.
Dosage and administration
Progesterone is administered by intramuscular (IM) injection. It differs from other commonly used steroids in that it is irritating at the place of injection.
Amenorrhea
Five to 10 mg are given for six to eight consecutive days. If there has been sufficient ovarian activity to produce a proliferative endometrium, one can expect withdrawal bleeding 48 to 72 hours after the last injection. This may be followed by spontaneous normal cycles.
Functional Uterine Bleeding
Five to 10 mg are given daily for six doses. Bleeding may be expected to cease within six days. When estrogen is given as well, the administration of Progesterone is begun after two weeks of estrogen therapy. If menstrual flow begins during the course of injections of Progesterone, they are discontinued.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever the solution and container permit.
- McDowell, M. A., Brody, D. J., & Hughes, J.P. (2007). Has age at menarche changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999-2004. Journal of Adolescent Health, 40, 227–231.[↩]
- Krohn, P. L. (1949). Intermenstrual pain (the “Mittelschmerz”) and the time of ovulation. British Medical Journal, 1(4609), 803–805. Retrieved September 27, 2016[↩]
- Tournaye H, Sukhikh GT, Kahler E, Griesinger G. A Phase III randomized controlled trial comparing the efficacy, safety and tolerability of oral dydrogesterone versus micronized vaginal progesterone for luteal support in in vitro fertilization. Hum Reprod. 2017;32(5):1019-27.[↩]
- Saccone G, Schoen C, Franasiak JM, Scott RT, Jr., Berghella V. Supplementation with progestogens in the first trimester of pregnancy to prevent miscarriage in women with unexplained recurrent miscarriage: a systematic review and meta-analysis of randomized, controlled trials. Fertil Steril. 2017;107(2):430-8 e3.[↩][↩][↩][↩][↩]
- van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database Syst Rev. 2015(7):CD009154.[↩][↩][↩][↩]
- Coomarasamy A, Williams H, Truchanowicz E, Seed PT, Small R, Quenby S, et al. A Randomized Trial of Progesterone in Women with Recurrent Miscarriages. The New England journal of medicine. 2015;373(22):2141-8.[↩][↩][↩]
- Progesterone support of the luteal phase and in the first trimester. https://www.ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Progesterone-support-of-the.pdf[↩]
- Carp H. A systematic review of dydrogesterone for the treatment of threatened miscarriage. Gynecol Endocrinol. 2012;28(12):983-90.[↩][↩][↩]
- Tekoa L. King; Mary C. Brucker (25 October 2010). Pharmacology for Women’s Health. Jones & Bartlett Publishers. p. 373. ISBN 978-1-4496-5800-7.[↩]
- Michelle A. Clark; Richard A. Harvey; Richard Finkel; Jose A. Rey; Karen Whalen (15 December 2011). Pharmacology. Lippincott Williams & Wilkins. p. 322. ISBN 978-1-4511-1314-3.[↩][↩]
- Dorland’s illustrated medical dictionary. 29th ed. Philadelphia: W.B. Saunders Company, 2000.[↩]
- Haas DM, Ramsey PS. Progestogen for preventing miscarriage. Cochrane Database Syst Rev. 2013(10):CD003511.[↩]
- Practice Committee of the American Society for Reproductive M. The clinical relevance of luteal phase deficiency: a committee opinion. Fertil Steril. 2012;98(5):1112-7.[↩]
- Wahabi HA, Fayed AA, Esmaeil SA, Al Zeidan RA. Progestogen for treating threatened miscarriage. The Cochrane database of systematic reviews. 2011(12):CD005943.[↩][↩]
- Carp H. A systematic review of dydrogesterone for the treatment of threatened miscarriage.
Gynecol Endocrinol. 2012;28(12):983-90.[↩] - van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles. The Cochrane database of systematic reviews. 2011(10):CD009154.[↩]
- Likis FE, Edwards DR, Andrews JC, Woodworth AL, Jerome RN, Fonnesbeck CJ, et al. Progestogens for preterm birth prevention: a systematic review and meta-analysis. Obstet Gynecol. 2012;120(4):897-907.[↩][↩]
- Romero R, Nicolaides KH, Conde-Agudelo A, O’Brien JM, Cetingoz E, Fonseca E, et al. Vaginal progesterone decreases preterm birth 34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol 2016;48: 380-317.[↩]
- Dodd JM, Jones L, Flenady V, Cincotta R, Crowther CA. Prenatal administration of progesterone for preventing preterm birth in women considered to be at risk of preterm birth. Cochrane Database Syst Rev. 2013;7:Cd004947.[↩][↩]
- Norman JE, Marlow N, Messow C-M, Shennan A, Bennett PR, Thornton S, et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM study): a multicentre, randomised, double-blind trial. Lancet 2016; 387(10033):2106-2116.[↩][↩]
- Progesterone: Use in the second and third trimester of pregnancy for the prevention of preterm birth. https://www.ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women’s Health/Statement and guidelines/Clinical-Obstetrics/Progesterone-use-in-the-second-and-third-trimester-(C-Obs-29b)-Review-July-2017.pdf[↩]
- Hassan SS, Romero R, Vidyadhari D, Fusey S, Baxter JK, Khandelwal M, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18-31.[↩][↩]
- Romero R, Nicolaides KH, Conde-Agudelo A, O’Brien JM, Cetingoz E, Fonseca E, et al. Vaginal progesterone decreases preterm birth <34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol 2016;48: 380-317.[↩][↩]
- Norman JE, Mackenzie F, Owen P, Mactier H, Hanretty K, Cooper S, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): a randomised, double-blind, placebocontrolled study and meta-analysis. Lancet. 2009;373(9680):2034-40.[↩]
- Durnwald CP, Momirova V, Rouse DJ, Caritis SN, Peaceman AM, Sciscione A, et al. Second trimester cervical length and risk of preterm birth in women with twin gestations treated with 17-alpha hydroxyprogesterone caproate. J Matern Fetal Neonatal Med. 2010;23(12):1360-4.[↩]
- Romero R, Conde-Agudelo A, El-Refaie W, Rode L, Brizot ML, Ctingoz E, et al. Vaginal progesterone decreases preterm birth and neonatal morbidity and mortality in women with a twin gestation and a short cervix: an updated meta-analysis of individual patient data. Ultrasound obstet Gynecol 2017;49(3):303-314.[↩]
- Borna S, Sahabi N. Progesterone for maintenance tocolytic therapy after threatened preterm labour: a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2008;48(1):58-63.[↩]
- Rebarber A, Ferrara LA, Hanley ML, Istwan NB, Rhea DJ, Stanziano GJ, et al. Increased recurrence of preterm delivery with early cessation of 17-alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 2007;196(3):224.e1-4.[↩]
- O’Brien JM, Adair CD, Lewis DF, Hall DR, Defranco EA, Fusey S, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):687-96.[↩]