Contents
What is argyria
Argyria is a rare disease caused by the chronic absorption silver content products which surpass the body’s kidney and liver excretory capacities, leading to silver granules being deposited in the skin and its appendages, mucosae and internal organs (including the eye, kidney, spleen, bone marrow and central nervous system), and causing them to acquire a blue-grey pigmentation 1. Argyria is characterized by gray to gray-black staining of the skin and mucous membranes produced by silver deposition. Silver may be deposited in the skin either from industrial exposure or as a result of medications containing silver salts. The amount of absorbed silver required to cause generalized Argyria pigmentation is unknown 2. Several different types of exposure (accidental, therapeutic, occupational and environmental), routes of administration (oral, intranasal and percutaneous) and intervals of exposure from 8 months to 5 years have been described 3.
Whether or not a person exposed to prolonged or high levels of silver develops argyria depends on many factors including the dose and form of exposure, the duration of exposure, and the route of exposure (ie: ingested, inhaled, skin contact). What is apparent is that the degree of hyperpigmentation in patients is directly correlated with the amount of silver present.
Generalized argyria usually begins with a grey-brown staining of the gums which later progresses to involve large areas of the skin.
- Over a period of months or years depending on the degree of exposure the skin turns a bluish-grey, metallic, to slate-grey colour.
- The hyperpigmentation is most pronounced in sun-exposed areas such as the face (particularly forehead and nose), neck, arms, and hands. Hence, the discoloration is thought to result from the presence of silver and silver-induced increase in melanin concentration.
- The fingernails, conjunctival membranes and mucous membranes may become hyperpigmented.
- In some cases, the entire skin turns a slate blue-grey color.
Localized argyria can occur in the eye (ocular argyrosis) from the overuse of silver containing eyedrops or cosmetic makeup. Sometimes, this may be the first objective sign of generalized argyria. Other forms of localized argyria are the appearance of blue macules at sites of acupuncture needles and silver earring sites.
How much colloidal silver causes argyria?
The normal human body contains approximately 1 mg of silver. Great individual variability exists in the length of exposure and total dose needed to result in argyria. The smallest amount of silver reported to produce generalized argyria in humans ranges from 4-5 g to 20-40 g. Silver at 50-500 mg/kg body weight is the lethal toxic dose in humans 4.
Bianchi et al 5 report a possible genetic predisposition for argyria.
Is argyria permanent?
Yes. Unfortunately, the pigmentation is permanent and almost untreatable.
How does silver toxicity occur?
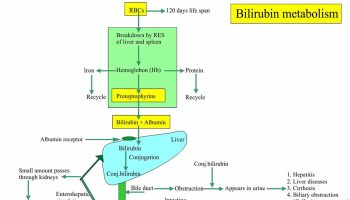
Silver enters the body either by mechanical impregnation of the skin by small silver particles or by ingestion of silver compounds. Most occupational argyria is due to the direct impregnation of silver salts from prolonged contact with skin. Silver taken orally or absorbed by mucous membranes is carried through blood bound to the plasma protein albumin. Some of this silver is carried as a salt and may be deposited in various tissues, with highest concentrations found in the skin, liver, spleen and adrenals. Most absorbed silver is excreted in feces and some in the urine.
Silver toxicity is rare today. However, there have been several reports of people getting argyria after using colloidal silver-based products as ‘cure-alls’. In several cases patients were manufacturing colloidal silver suspension at home using instructions downloaded from the Internet. Circus freak Captain Fred Walters the blue man, ingested silver nitrate to deepen his color and improve his income, but died from the habit.
There may be a genetic predisposition for argyria.
Argyria causes
There are several sources of exposure to silver.
- Occupational exposure – mainly in workers involved in silver mining, silver refining, silverware and metal alloy manufacturing, metallic films on glass and china electroplating solutions, and photographic processing.
- Medication with silver salts – prolonged use of silver salts for the irrigation of urethral or nasal mucous membranes, in eye drops, wound dressing, and excessive use of an oral smoking remedy containing silver acetate.
- Colloidal silver dietary supplements – marketed widely as a treatment for arthritis, diabetes, cancer, herpetic infections and AIDS.
- Surgical and dental procedures – silver sutures used in abdominal surgery and silver dental fillings (amalgam tattoos).
The most common cause of argyria is mechanical impregnation of the skin by small silver particles in workers involved in silver mining, silver refining, silverware and metal alloy manufacturing, metallic films on glass and china, electroplating solutions, and photographic processing. Colloidal silver dietary supplements are marketed widely for cancer, AIDS, diabetes mellitus, and herpetic infections 6. Cases have followed the prolonged use of silver salts for the irrigation of urethral or nasal mucous membranes, in eye drops, wound dressing, and the excessive use of an oral smoking remedy containing silver acetate 7.
Argyria has also been attributed to surgical and dental procedures (e.g., silver amalgam-tattooing, silver sutures used in abdominal surgery). Blue macules have appeared at sites of acupuncture needles and silver earring sites 8. Great individual variability exists in the length of exposure and total dose needed to result in argyria.
Argyria symptoms
Early on, a gray-brown staining of the gums develops, later progressing to involve the skin diffusely. The cutaneous pigmentation usually is a slate-gray, metallic, or blue-gray color and may be clinically apparent after a few months, but clinical appearance usually takes many years and depends on the degree of exposure.
The hyperpigmentation is most apparent in the sun-exposed areas of skin, especially the forehead, nose, and hands.
In some patients, the entire skin acquires a slate blue-gray color.
The sclerae, nail beds, and mucous membranes may become hyperpigmented.
Viscera tend to show a blue discoloration, including the spleen, liver, and gut, findings evident during abdominal surgery or at postmortem examination.
Rarely, black tears (melanodacryorrhea) can appear during argyrosis of the conjunctiva.
The systemic toxic effects of silver may include the following:
- Gastrointestinal catarrh
- Tissue wasting
- Uremia
- Albuminuria
- Fatty degeneration of the liver, kidney, and heart
- Hemorrhage
- Idiopathic thrombocytopenia
- Fluidity of the blood
- Chronic bronchitis
- Loss of coordination
- Decreased night vision
- Gustatory disturbance
- Vestibular impairment
- Seizure of the grand mal type
- Death by paralysis of the respiratory system
Current thought holds that the substantial amounts of silver in argyria usually result in no serious effects on human health. However, a few cases have notable clinical symptoms and signs. This lack of significant systemic silver toxicity in argyria may be due to the interaction of selenium and sulfur with silver in vivo.
It was reported that argyria can be associated with unexpected and quickly developing severe radiation dermatitis during chemoradiotherapy treatment 9.
Argyria diagnosis
Argyria is a rare condition and unfamiliarity with this condition may lead to its misdiagnosis. The diagnosis of argyria is established by skin biopsy with formaldehyde-fixed paraffin-embedded sections stained with hematoxylin-eosin.
In vivo silver concentrations can be measured using x-ray fluorescence 10.
Dermoscopy, reflectance confocal microscopy, and high-definition optical coherence tomography can be used in the diagnosis of generalized argyria 11.
Corneal confocal microscopy and electrophysiological tests may help confirm the diagnosis of ocular argyrosis 12.
Argyria treatment
Unfortunately, the argyria pigmentation is permanent and almost untreatable.
- Depigmentary agents and chelation are unsuccessful.
- Some reports have suggested using 5% hydroquinone to reduce the number of silver granules in the upper dermis and around sweat glands.
- Selenium and sulfur form complexes with silver, However, they are not as stable as silver-selenium complexes and this treatment has not proved effective.
- A 1064 nm QS Nd:YAG laser is reported to offer effective treatment for argyria.
To prevent further exposure, stop ingestion of silver and application of all silver containing remedies. Protective wear can be used to prevent occupational exposure.
Sunscreens and opaque cosmetics may be helpful in preventing further pigmentary darkening and aid in masking obvious discoloration. Cosmetic camouflage may be useful in disguising the appearance.
Chelation attempts to remove silver from the body have been unsuccessful.
The treatment of argyria caused by colloidal silver ingestion using the Q-switched 1064-nm Nd:YAG laser has been reported 13 and a picosecond 755-nm Q-switched alexandrite laser has also been used with success for treatment 14.
- Lansdown A. A pharmacological and toxicological profile of silver as an antimicrobial agent in medical devices. Adv Pharmacol Sci. 2010 doi: 10.1155/2010/910686[↩]
- Lencastre A, Lobo M, João A. Argyria — case report. An Bras Dermatol. 2013;88(3):413-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3754374/[↩]
- Bowden L, Rover M, Hallman J, Lewin-Smith M, Lupton G. Rapid onset of Argyria induced by a silver-containing dietary supplement. J Cutan Pathol. 2011;38:832–835[↩]
- Argyria. https://emedicine.medscape.com/article/1069121-overview[↩]
- Bianchi L, Orlandi A, Di Stefani A, Ricci R, Chimenti S. “Familial” generalized argyria. Arch Dermatol. 2006 Jun. 142(6):789-90[↩]
- Gulbranson SH, Hud JA, Hansen RC. Argyria following the use of dietary supplements containing colloidal silver protein. Cutis. 2000 Nov. 66(5):373-4.[↩]
- Gaslin MT, Rubin C, Pribitkin EA. Silver nasal sprays: misleading Internet marketing. Ear Nose Throat J. 2008 Apr. 87(4):217-20[↩]
- Rackoff EM, Benbenisty KM, Maize JC, Maize JC Jr. Localized cutaneous argyria from an acupuncture needle clinically concerning for metastatic melanoma. Cutis. 2007 Nov. 80(5):423-6.[↩]
- Gorayski P, Pinkham MB, Muir JB, Pullar AP. Severe acute radiation dermatitis in a patient with argyria. Case Rep Oncol Med. 2014.[↩]
- Graham SA, O’Meara JM. The feasibility of measuring silver concentrations in vivo with x-ray fluorescence. Phys Med Biol. 2004 Aug 7. 49(15):N259-66.[↩]
- Cinotti E, Labeille B, Douchet C, Cambazard F, Perrot JL. Dermoscopy, reflectance confocal microscopy, and high-definition optical coherence tomography in the diagnosis of generalized argyria. J Am Acad Dermatol. 2017 Feb. 76 (2S1):S66-S68.[↩]
- Sarnat-Kucharczyk M, Pojda-Wilczek D, Mrukwa-Kominek E. Diagnostic methods in ocular argyrosis: case report. Doc Ophthalmol. 2016 Oct. 133 (2):129-138.[↩]
- Han TY, Chang HS, Lee HK, Son SJ. Successful treatment of argyria using a low-fluence Q-switched 1064-nm Nd:YAG laser. Int J Dermatol. 2011 Jun. 50 (6):751-3.[↩]
- Friedmann DP, Buckley S, Mishra V. Localized Cutaneous Argyria From a Nasal Piercing Successfully Treated With a Picosecond 755-nm Q-Switched Alexandrite Laser. Dermatol Surg. 2017 Aug. 43 (8):1094-1095.[↩]