Contents
- Blood donation rules
Blood donation rules
Blood donation rules and requirements vary a lot between countries. For example, in the the United States (US) you must be at least 17 years old to donate blood at the National Institutes of Health Blood Bank 1. In Australia the minimum age to donate blood is 16 years with an upper limit of 70 years of age 2. In the US there is no upper age limit for donation 1.
The temperature of blood in the body is 38° C, which is about one degree higher than body temperature 3. How much blood you have depends mostly on your size and weight. A man who weighs about 70 kg (about 154 pounds) has about 5 to 6 liters of blood in his body.
The volume of blood removed during a donation (450 mL ± 10% of blood) represents only about 10% of the total blood mass of a subject weighing 70 Kg.
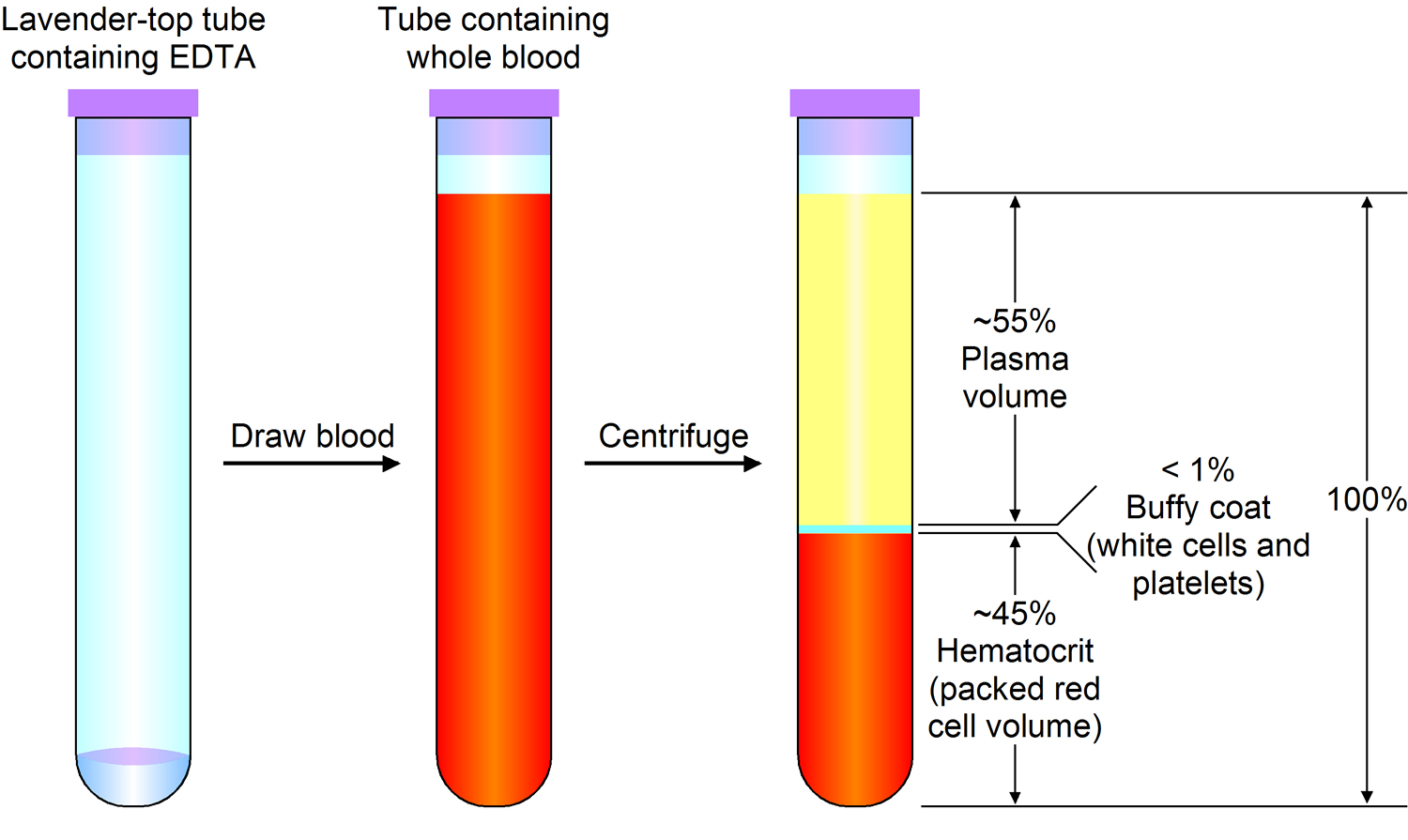
Blood is 55% blood plasma and about 45% different types of blood cells. The blood plasma is a light yellow liquid. Over 90% of blood plasma is water, while less than 10% is dissolved substances, mostly proteins. Blood plasma also contains electrolytes, vitamins and nutrients such as glucose and amino acids. Over 99% of the solid particles present in blood are cells that are called red blood cells (erythrocytes) due to their red color. The rest are pale or colorless white blood cells (leukocytes) and platelets (thrombocytes).
Note: Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
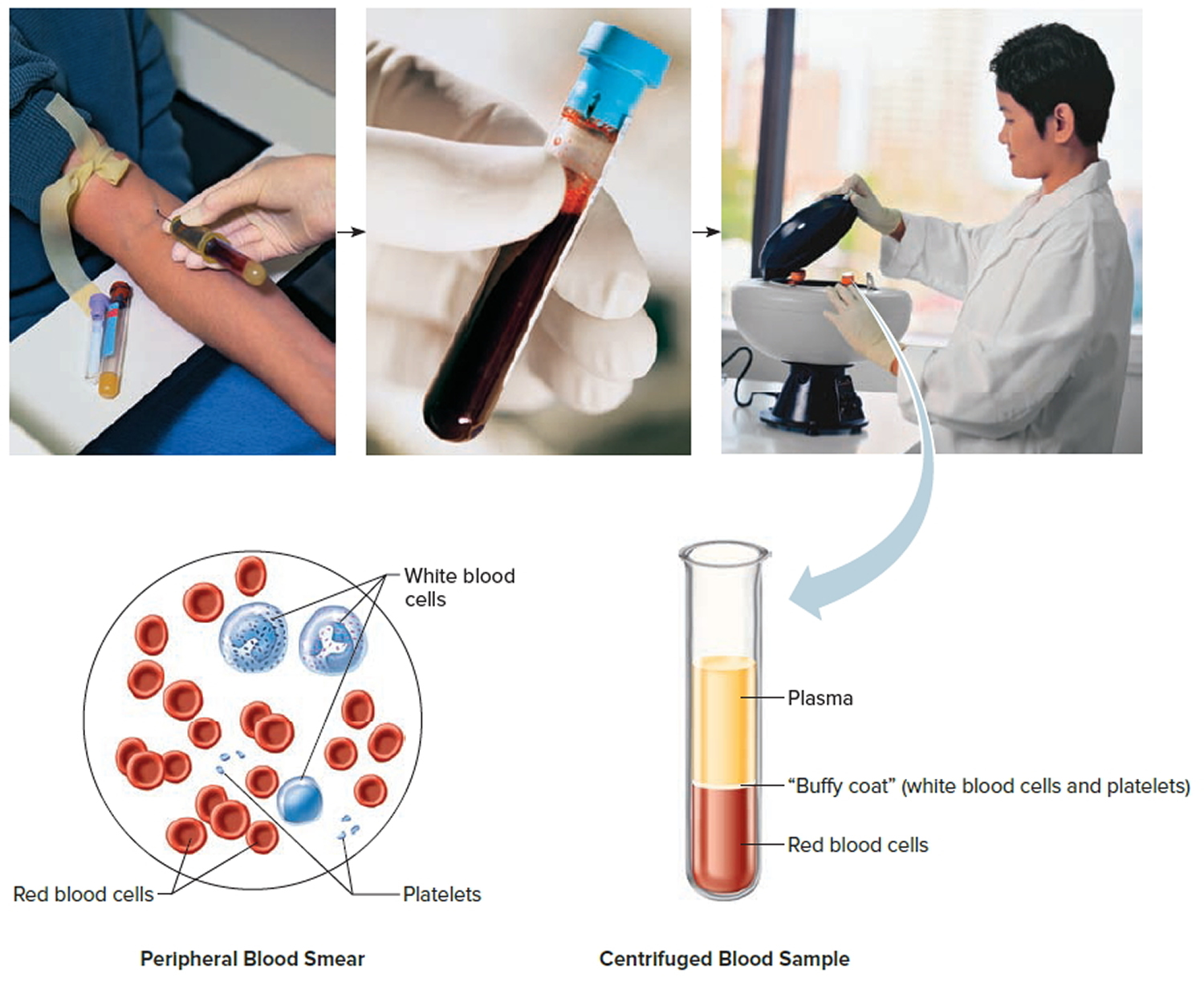
Figure 1. Blood composition
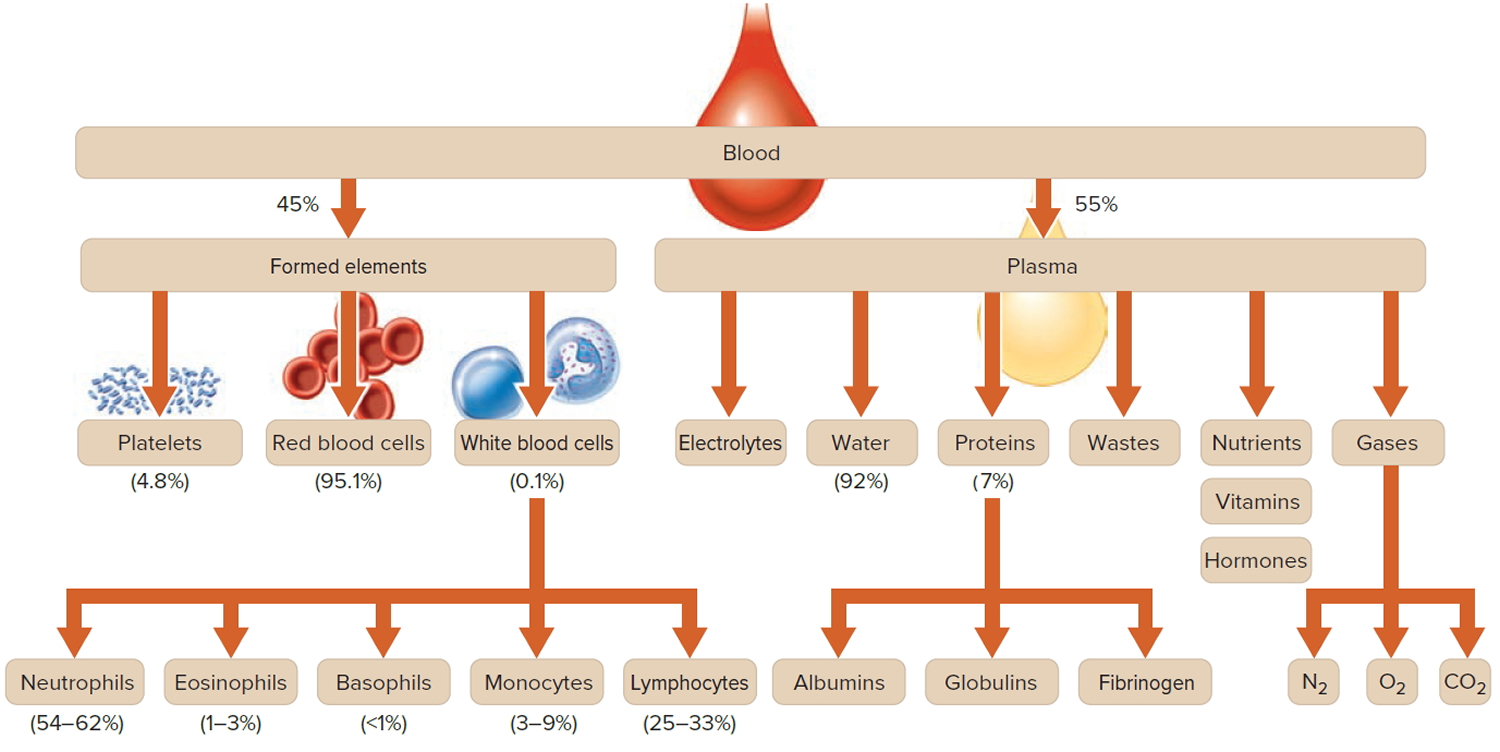
Note: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
Blood has three important functions:
- Transportation
The blood transports oxygen from the lungs to the cells of the body, where it is needed for metabolism. The carbon dioxide produced during metabolism is carried back to the lungs by the blood, where it is then exhaled. Blood also provides the cells with nutrients, transports hormones and removes waste products, which the liver, the kidneys or the intestine, for example, then get rid of.
- Regulation
The blood helps to keep certain values of the body in balance. For instance, it makes sure that the right body temperature is maintained. This is done both through blood plasma, which can absorb or give off heat, as well as through the speed at which the blood is flowing. When the blood vessels expand, the blood flows more slowly and this causes heat to be lost. When the environmental temperature is low the blood vessels can contract, so that as little heat as possible is lost. Even the so-called pH value of the blood is kept at a level ideal for the body. The pH value tells us how acidic or alkaline a liquid is. A constant pH value is very important for bodily functions.
- Protection
If a blood vessel is damaged, certain parts of the blood clot together very quickly and make sure that a scrape, for instance, stops bleeding. This is how the body is protected against losing blood. White blood cells and other messenger substances also play an important role in the immune system.
Blood donation eligibility 4
You can donate blood if you:
- Are healthy
- Are at least 17 years of age
- Weigh at least 110 pounds (50 kgs). There is no upper weight limit.
The tables below address specific situations affecting donation eligibility.
Table 1. Medical Condition
| Medical Condition | Eligibility |
| Acquired Immune Deficiency Syndrome (AIDS), individuals at high risk and their partners |  cannot donate cannot donate |
| Colds and flu within 2 days |  cannot donate cannot donate |
| Diabetes, on or off medication and under control. If well-controlled by diet, oral medication, or insulin, you can donate. *However, the use of insulin made from beef is a cause for permanent deferral. |  can donate can donate |
| Hepatitis or jaundice after age 11 |  cannot donate cannot donate |
| Pregnancy. You cannot donate until six weeks after the conclusion of the pregnancy. |  cannot donate cannot donate |
| Pregnancy, after delivery, miscarriage, abortion |  6-week wait 6-week wait |
| Menstruation |  can donate can donate |
| Cancer, treatment complete and disease-free; most types |  2-year wait 2-year wait |
Table 2. Medical Procedures
| Medical Procedures | Eligibility |
| Surgery, without transfusion (except for autologous blood) |  can donate can donate |
| Surgery, with transfusion |  1-year wait 1-year wait |
Table 3. Vaccinations
| Vaccinations | Eligibility |
| Measles (rubella); measles, mumps, and rubella (MMR); chicken pox (varicella) |  1-month wait 1-month wait |
| Flu |  can donate can donate |
| Hepatitis A or B |  can donate can donate |
Table 4. Other Possible Restrictions
| Other Possible Restrictions | Eligibility |
| Ear/Body piercing, sterile procedure/equipment used |  can donate can donate |
| Ear/Body piercing, nonsterile procedure/equipment used |  1-year wait 1-year wait |
| Tattooing |  1-year wait 1-year wait |
| Travel outside the United States or Canada | Contact the National Institutes of Health Blood Bank |
If you have traveled to other countries
There is a slight risk of exposure to infectious agents outside the United States that could cause serious disease. Donor deferral criteria for travel outside the US are designed to prevent the transmission of three specific organisms from donor to recipient:
- Malaria. Malaria is caused by a parasite that can be transmitted from mosquitoes to humans. It is found in several hundred countries, and is one of the leading causes of death from infectious diseases world-wide. Donors who have traveled to areas listed by the Centers for Disease Control 5 as malarial risk areas are deferred for 1 year after their travel ends 1.
- Bovine Spongiform Encephalopathy (BSE). BSE is commonly referred to as “Mad Cow disease” and is caused by an abnormal, transmissible protein called a prion. In the 1990s, the United Kingdom experienced an epidemic of the disorder in cows, with subsequent cow-to-human transmission, presumably through the food chain. BSE-infected cattle were also detected in other countries in Western Europe. Transfusion-transmission of BSE among donor-recipient pairs has been documented in a handful of cases 1. Donors who have spent more than three months in the United Kingdom from 1980-1996, and donors who resided in Western Europe for greater than five years since 1980, are permanently deferred from blood donation 6.
Other blood donation restrictions
- If you have low Hemoglobin (Hb) or anemia, female donors must have a hemoglobin level of at least 12.5g/dL and male donors are required to have a minimum level of 13.0g/dL. The deferral is 30 days for both whole blood and apheresis donations. The most common reason for low hemoglobin is iron deficiency, and you will be given information about maintaining a healthy iron balance.
- If you have sickle cell disease, you cannot donate if you have sickle cell disease. You should not donate whole blood if you have sickle cell trait, because your blood will clog the filter that is applied to whole blood units. You can donate platelets if you are a sickle cell trait carrier.
- If you have received a blood transfusion, you must wait one year to donate.
- You cannot donate if you are currently experiencing severe allergy symptoms.
- Taking antibiotics, you can donate 24 hours after the last dose if you have no further signs of infection. You may donate while taking antibiotics for acne.
- You cannot donate while taking narcotics to relieve pain.
- You may donate blood while taking nonnarcotic pain relievers.
- Aspirin interferes with platelet function and should be discontinued prior to platelet donation as follows. You cannot donate platelets if you have taken aspirin in the last 48 hours.
- Special Caution: Many medications contain aspirin, so check the container carefully before making a platelet donation,
- Nonaspirin: You can donate platelets if you have taken ibuprofen or other nonaspirin, nonsteroidal anti-inflammatory drugs (NSAIDS).
- You can donate if you had skin cancer (basal cell or squamous cell) or cervical cancer in situ and the surgical site is completely healed.
- If you had another type of cancer, you can donate two years after the date of surgery or other definitive therapy, as long as your doctor informs you that there is no evidence of persistent or recurrent cancer.
- You are permanently deferred if you had leukemia or lymphoma.
- If you have a cold or the flu, you can donate once you have been symptom-free for 48 hours.
- If you have had dental work, there is a 24-hour waiting period after a routine cleaning and a 72-hour wait after extractions, root canals, or oral surgery.
- If you have epilepsy, you can donate if you have been seizure free for at least one week.
- If you have high blood pressure, you can donate if your blood pressure is controlled by medication.
- If you have low blood pressure, you can donate with low blood pressure.
- If you have heart disease or had a heart attack, in some situations, you may donate if you have heart disease or have had a heart attack. Contact the National Institutes of Health Blood Bank 7 for more details.
- If you have had angioplasty, you will need to contact the National Institutes of Health Blood Bank 7 for more details.
- If you had major surgery, you must wait until you have completely recovered and returned to normal activity before donating.
- If you have had hepatitis, you cannot donate if you have had hepatitis after age 11.
- If you received the hepatitis vaccine, you can donate if you have received the hepatitis vaccine (a series of three vaccinations).
- You must wait one year if you received Hepatitis B Immune Globulin or if you experienced a needlestick injury contaminated with untested blood.
- If you have herpes, you cannot donate with herpes or a cold sore when the lesions are active. You can donate if the lesions are dry and almost healed.
- If you have had malaria, you may donate if you have been asymptomatic of malaria for more than 3 years while residing in a non-endemic country.
Benefits of blood donation
There is no substitute for human blood. Human blood cannot be manufactured. People are the only source of blood. Much of the medical care of an National Institutes of Health patient depends on the steady supply of blood from healthy, caring individuals like yourself. No miracle of modern medicine can help the patients who need blood if blood is not available. The blood you donate at the National Institutes of Health Blood Bank is used to support the many patients who come from all over the world to receive treatment.
Blood in the umbilical cord at birth is rich in stem cells that can be used to treat a variety of disorders, including leukemias, sickle cell disease and other hemoglobin abnormalities, and certain inborn errors of metabolism. The United States and the United Kingdom have public umbilical cord blood banks that provide stem cells for free. For many illnesses it is more effective to receive donor stem cells, because receiving one’s own could reintroduce the disease.
Types of Blood Donations
You can make the following types of donations:
Blood components for transfusion
- Whole blood
- Red cells by apheresis
- Platelets by apheresis
- Granulocytes by apheresis
- AB Plasma by apheresis
Hemochromatosis donations
Hemochromatosis is a relatively common inherited condition in which the body absorbs excess iron. Over many years, iron overload can develop, with deposition of excess iron in body tissues and organs. Disabling arthritis, glandular failure, and severe liver disease can occur if the disorder is not treated. The treatment is phlebotomy therapy, or removal of 1 unit (1 pint) of blood every 1 – 16 weeks, depending on the level of iron overload. One pint of blood contains 250 mg of iron. Serial frequent phlebotomy sessions are a highly effective way to lower body iron levels. The National Institutes of Health Blood Bank has a protocol for treatment of hemochromatosis by phlebotomy therapy, which uses a simple and easy method to determine the pace of therapy.
The blood units removed therapeutically may be made available for transfusion into others if the donor (the hemochromatosis subject) meets standard blood donor eligibility criteria. Phlebotomy therapy and medical care for hemochromatosis are offered free of charge to all study participants. All persons with hemochromatosis are eligible for participation in this study, regardless of whether they meet blood donor criteria.
Hemochromatosis patients participating in the NIH Blood Bank Hemochromatosis Donor Program may donate:
- Whole blood
- Double red cells
Blood components for laboratory research use
Donated blood is never wasted. It is used every day of the year to treat patients who are participating in the medical treatment and research programs of the National Institutes of Health. If your blood is not required for immediate use, it may be frozen and stored. Fractions of blood that cannot be used for transfusion are used for research. Occasionally, the blood you give may not be required for a patient here but may be sent to another hospital, where it can be used to help save a life.
What is Whole Blood ?
Whole blood consists of red blood cells, white blood cells, and platelets suspended in a protective yellow liquid known as plasma. Most patients receiving transfusions do not need all of these elements.
Red blood cells have no nucleus, in contrast to many other cells. Each red blood cell contains hemoglobin, which can transport oxygen. In tiny blood vessels in the lung the red blood cells pick up oxygen from inhaled air and carry it through the bloodstream to all parts of the body. When they reach their goal, they release it again. The cells need oxygen for metabolism, which also creates carbon dioxide as a waste product. The red blood cells then pick up the carbon dioxide and transport it back to the lung. There we exhale it when we breathe out.
Red blood cells can also pick up or release hydrogen and nitrogen. When picking up or releasing hydrogen they help to keep the pH level of the blood steady; by releasing nitrogen the blood vessels expand, and blood pressure falls. Red blood cells have a life cycle of about 120 days. When they are too old or damaged they are broken down in the bone marrow, spleen or liver.
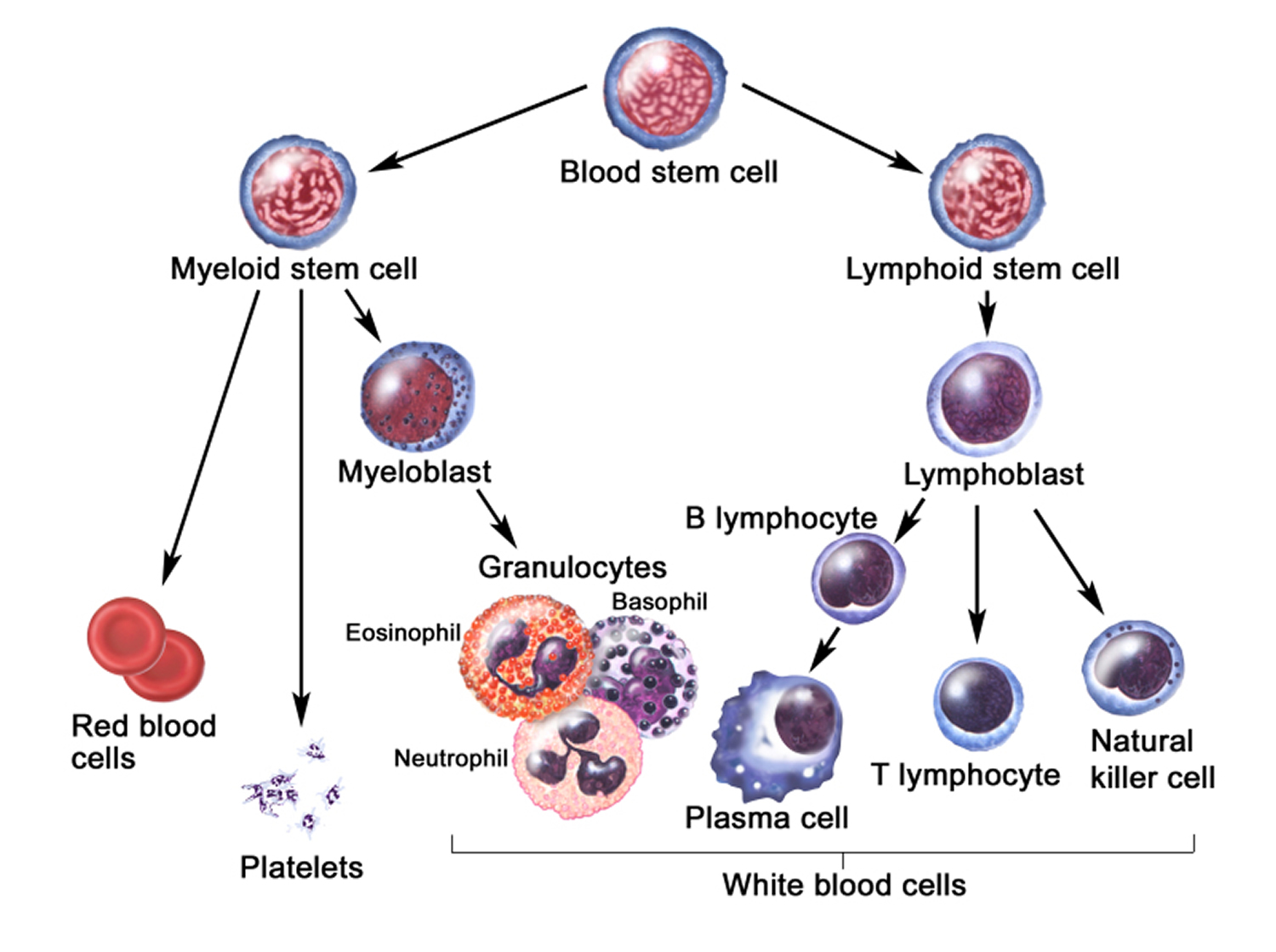
All solid parts of the blood originate from common parent cells, the so-called stem cells. In adults blood cells are produced mainly in the bone marrow. The various blood cells develop in several stages from stem cells to blood cells or blood platelets. White blood cells such as lymphocytes do not mature only in the bone marrow, but also in the lymph nodes. When the cells are completed, they are released into the bloodstream. In addition to these mature cells, the blood still contains a small number of precursor cells.
Figure 2. Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
Certain messenger substances regulate the production of blood cells. The hormone erythropoietin, which is produced in the kidneys, promotes the production of red blood cells, while so-called cytokines stimulate the production of white blood cells.
One pint (473 ml) of whole blood is usually processed by a spinning method into:
- Red blood cells, which carry the oxygen needed by patients who are anemic;
- Platelets: Platelets are small cells that help the blood to clot. Manufactured in the bone marrow and stored in the spleen, their job is to rush to the site of an injury. Once there, they form a barrier, help the damaged organ or blood vessel stop bleeding, and give the body a chance to begin healing. Platelets needed by patients who are bleeding.
- Plasma: Plasma is the pale yellow liquid part of whole blood, in which the cellular elements are suspended. It is enriched in proteins that help fight infection and aid the blood in clotting. AB plasma is plasma collected from blood group AB donors. It is considered “universal donor” plasma because it is suitable for all recipients, regardless of blood group. Due to its value as a transfusion component, it is sometimes referred to as “liquid gold.” Plasma is transfused to patients whose blood is not clotting.
Therefore, one donation of whole blood can treat three different patients!
Used for:
- Cancer, blood diseases, haemophilia, anaemia, heart disease, stomach disease, kidney disease, childbirth, operations, blood loss, trauma, burns.
Is it Safe to Give Whole Blood ?
Absolutely. Many safeguards are taken to assure that no harm comes to you during or after donation. First, we obtain a medical history and check your blood pressure, pulse, and temperature to assure that you are in good health. We take a small sample of blood from your finger to confirm that you have an ample number of red cells to share. All equipment used to collect your blood is sterile and disposable. After donation, we provide delicious snacks and drinks.
Who is Eligible to Give Whole Blood?
Please see detailed description of donor criteria above (Tables 1-4 plus eligibility criteria and restrictions).
How often can you donate whole blood ?
You must wait 56 days between whole-blood donations to allow the number of red blood cells in your body to return to a predonation level.
How long does blood donation take ?
15 minutes to donate, 45 minutes for the appointment.
How Do You Arrange to Donate ?
You can contact the National Institutes of Health Blood Bank 7 for more details.
What is Donating Red Cells by Apheresis
Double Red Cell Apheresis (DRCA) is a procedure that allows a donor to give 2 units of red cells at the same time. This is done by a procedure called “apheresis,” which separates whole blood into component parts such as red blood cells, platelets, and plasma 8. To remove red cells, a needle is placed in your arm, and the blood flows into a sterile, disposable plastic kit installed in a machine designed specifically for this purpose. As blood enters the machine, the bowl is spinning at high speed. This causes the components of the blood to separate so that the red blood cells can be siphoned into a blood bag. Plasma and other parts of the blood are then returned to you through the same needle. The process is repeated to collect 2 units of red blood cells.
Is Double Red Cell Apheresis Safe ?
Absolutely. The machine and the procedure have been evaluated and approved by the Food and Drug Administration (FDA), and all plastics and needles coming into contact with you are used once and discarded 8. At no time during the procedure is the blood being returned to you detached from the needle in your arm, so there is no risk of returning the wrong blood to you.
What Are The Double Red Cell Apheresis Donor Requirements ?
Because you will be losing more red blood cells than usual during this procedure, donor criteria differ from those for whole blood donation:
Men
- Minimum weight – 130 pounds (59 kgs)
- Minimum height – 5’1″
Women
- Minimum weight – 150 pounds (68 kgs)
- Minimum height – 5’5″
Donors must have a slightly higher red cell count, specifically, a fingerstick hemoglobin level of at least 13.3 gm/dL. To assure that you do not become anemic, the interval between Double Red Cell Apheresis and subsequent blood donation is 4 months 8.
How Long Does Double Red Cell Apheresis Procedure Take ?
The time required to remove 2 units of reds cells is about 45 minutes 8. Because you’ll be with us longer, there will be time to watch TV, read, or just chat with staff and other donors. Every effort will be made to make the experience relaxing and enjoyable.
What is Donating Platelets by Apheresis
Plateletpheresis is the standard procedure by which platelets are separated from whole blood, concentrated, and collected 9. To remove platelets, a needle is placed in each arm. Blood flows through a needle into a machine that contains a sterile, disposable plastic kit specifically designed for this purpose. The platelets are isolated and channeled out into a special bag, and red blood cells and other parts of the blood are returned to you through a needle in the opposite arm. There is also a plateletpheresis procedure that can be performed with a single needle.
Is Plateletpheresis Safe ?
Absolutely. The machine and the procedure have been evaluated and approved by the Food and Drug Administration, and all plastics and needles coming into contact with you are used once and discarded 9. At no time during the procedure is the blood being returned to you detached from the needle in your arm, so there is no risk of returning the wrong blood to you.
Who Is Eligible to Give Platelets ?
The interval between consecutive platelet donations at National Institutes of Health Blood Bank is 1 month. However, because the body replaces platelets within a few days, you are allowed to give more frequently when you are donating for a relative or for a patient who responds particularly well to your platelets. In addition to standard donor eligibility requirements, platelet donors should refrain from taking aspirin for 48 hours prior to donation.
How Long Does Plateletpheresis Take ?
Plateletpheresis procedures take about 90 minutes 9, but you should allow another 30 minutes for staff to obtain your medical history.
What is Plasmapheresis ?
Plasmapheresis is the standard procedure by which plasma is separated from whole blood and collected 10. Blood flows through a single needle placed in an arm vein, into a machine that contains a sterile, disposable plastic kit. The plasma is isolated and channeled out into a special bag, and red blood cells and other parts of the blood are returned to you through the same needle.
Is Plasmapheresis Safe ?
Absolutely. The machine and the procedure have been evaluated and approved by the Food and Drug Administration (FDA), and all plastics and needles coming into contact with you are used once and discarded 10. At no time during the procedure is the blood being returned to you detached from the needle in your arm, so there is no risk of returning the wrong blood to you.
Who Is Eligible to Participate in the AB Plasma Program ?
Donors must have blood group AB and must be male, because men lack plasma proteins (antibodies) directed against blood cell elements 10. Otherwise, eligibility for plasmapheresis procedures is the same as that for whole-blood donation. The interval between consecutive group AB plasmapheresis donations at National Institutes of Health Blood Bank is 1 month.
How Long Does Plasmapheresis Take ?
Plasmapheresis procedures take about 40 minutes, but you should allow another 20 minutes for staff to obtain your medical history 10.
What is Granulocytes by Apheresis
A granulocyte is a type of white blood cell which fights bacteria and fungi. Patients with bone marrow failure syndromes, or those undergoing chemotherapy or marrow transplantation, often do not make enough of their own granulocytes to prevent serious infections. Such patients may benefit from a course of granulocyte transfusions.
What is Granulocytapheresis ?
Granulocytapheresis is the process by which granulocytes are collected from a healthy donor 11. Similar to plateletpheresis, blood is withdrawn from a vein and directed into a machine that contains a sterile disposable kit. Granulocytes are separated by a spinning process and concentrated in a plastic bag. The remaining parts of the blood are returned to the donor through a second needle.
Is Granulocytapheresis Safe ?
Yes. The machine and the procedure used for granulocyte collection are approved by the Food and Drug Administration, and all plastics and needles coming into contact with the donor are discarded after use 11. Two medications are given to the donor the day before collection to boost the donor’s granulocyte count. These medications are approved for donor use under an NIH protocol.
Who Is Eligible to Give Granulocytes ?
Granulocyte donors are healthy, unpaid volunteers between the age of 18 and 75 who meet the criteria for blood and platelet donors described below 11. Granulocyte donors must meet some additional criteria described in the protocol. Granulocyte donors should refrain from taking aspirin for 48 hours prior to donation.
How Long Does Granulocytapheresis Take ?
Giving granulocytes with use of an apheresis machine takes about 2.5 hours, which is slightly longer than a plateletpheresis donation 11. The donor has enough time to enjoy a full-length movie.
INCLUSION CRITERIA for Granulocytapheresis:
- Donors shall meet all donor eligibility criteria for allogeneic blood donors, as defined in the most recent editions of the AABB Standards and FDA Code of Federal Regulations (21CFR640).
In addition, donors shall meet the following restrictions:
- Age greater than or equal to 18 and less than or equal to 75 years
- If hypertension is present, must be well-controlled on medications
- If peptic ulcer disease has been diagnosed in the past, symptoms must be well-controlled on medications
- If cataracts have been diagnosed in the past, records from subject’s ophthalmologist must be obtained indicating type of cataract. If posterior subcapsular cataract was diagnosed in the past, subject may receive G-CSF but not dexamethasone. The only exception to this is a history of bilateral cataract extractions due to posterior subcapsular cataract.
EXCLUSION CRITERIA for Granulocytapheresis:
- Information obtained from health history screen that does not meet the allogeneic donor eligibility criteria of the AABB Standards or the FDA CFR.
- Weight less than 50 kg (110 lbs)
- History of coronary heart disease
- Uncontrolled hypertension (systolic BP >160, diastolic BP >100)
- History of hepatitis or injection drug use
- Diabetes mellitus requiring insulin
- Active, symptomatic peptic ulcer disease
- History of iritis or episcleritis
- Sickle cell disease (sickle trait is acceptable). Testing for hemoglobin S is not required.
- Lithium therapy
- Pregnancy or nursing (breast feeding)
Blood donation side effects
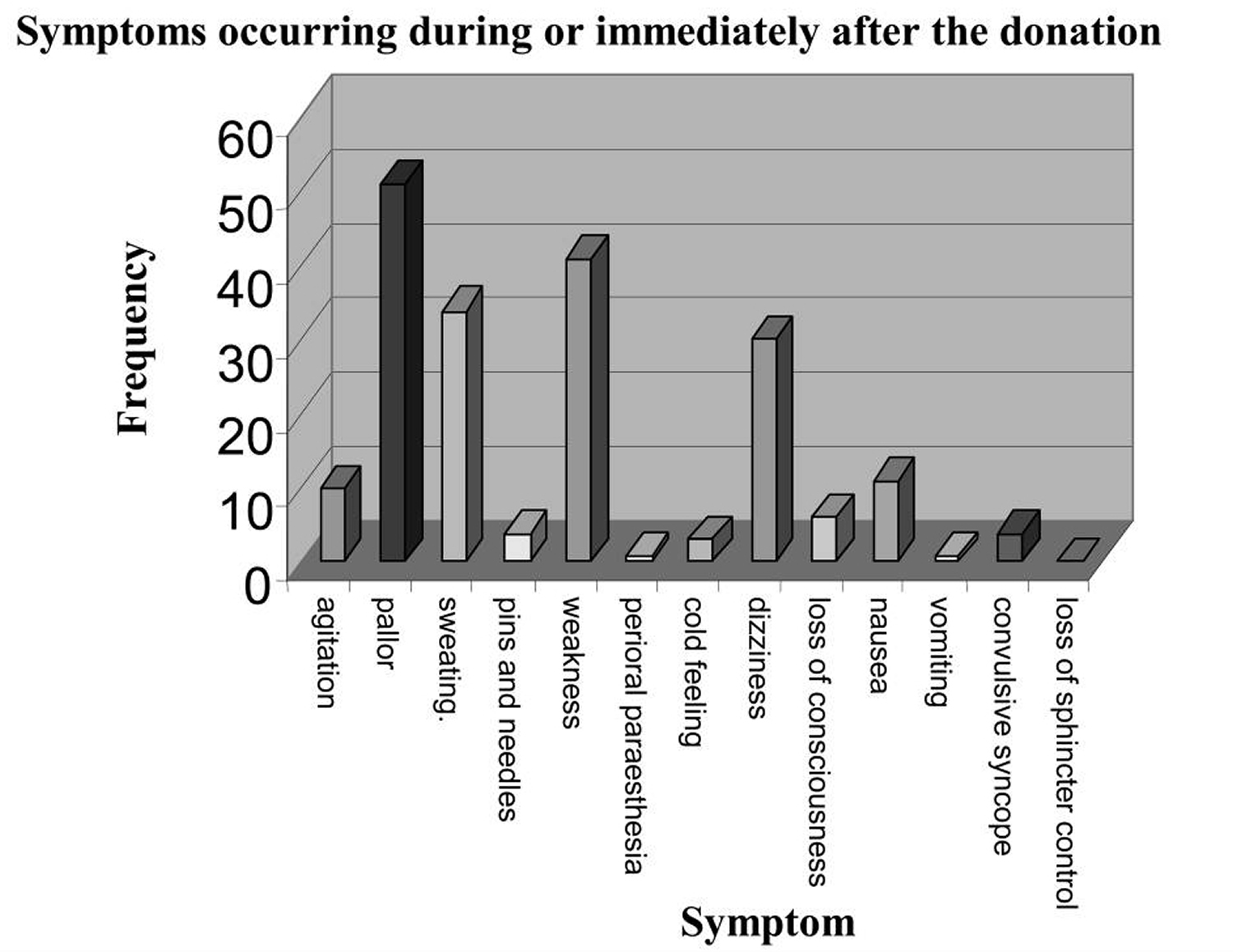
Blood donors normally tolerate the donation very well, but occasionally adverse reactions of variable severity may occur during or at the end of the collection. The adverse reactions that occur in donors can be divided into local reactions and systemic reactions. In a small study involving 4,906 donors (3,716 male and 1,190 female), only 63 donors (1.2% of all the volunteers) suffered some kind of adverse reaction: 59 (1.08% of the subjects) had mild reactions (agitation, sweating, pallor, cold feeling, sense of weakness, nausea), and only 4 (3 males and 1 female, 0.2%) had more severe disorders, including vomiting, loss of consciousness, and convulsive syncope.
The statistical probability of an episode of complete loss of consciousness was equivalent to an incidence of 0.1%, that is, one case every 1,000 donors 12.
Of the 63/4,906 (1.2%) donors who had adverse reactions to blood donation, only 40 (0.8%) were administered oral vasopressors (a drug or other agent which causes the constriction of blood vessels), while the other 23 (0.4%) recovered from the vasovagal reaction simply from being placed in the antishock position. Of the 63 donors who had a vasovagal reaction, only 18 (0.36%) were given crystalloid solutions, while less than five (0.1%) required additional therapy with cortisone 12. In no case was re-animation based on oxygen therapy or administration of adrenaline needed.
The greatest number of reactions occurred during or after donations of whole blood, with there being fewer after donations of other blood components.
Local reactions
Local reactions occur predominantly because of problems related to venous access 12. They are usually haematomas due to extravasation from the veins, caused by incorrect placement of the needle during the venipuncture. Pain, hyperaemia and swelling may develop at the site of the extravasation. Other local events include pain due to slight trauma to the subcutaneous nerve endings. In most cases, however, these are banal complications that do not require any treatment. Local phlebitis and thrombophlebitis are more serious complications than the foregoing, but are very rare.
Systemic reactions
The systemic reactions, in contrast to the local reactions, can be divided into mild or severe. In most cases, they are vasovagal reactions than can be triggered by the pain of the venipuncture, by the donor seeing his or her own blood, by the donor seeing another donor unwell, by the anxiety and state of tension of undergoing the donation, etc. The systemic reactions are characterised by the appearance of pallor, sweating, dizziness, gastrointestinal disorders, nausea, hypotension, and bradycardia. Therapeutic intervention must be swift, otherwise this clinical picture, typical of a vasovagal reaction, will progress into an episode of syncope, of variable severity, which may or may not be complicated by the onset of tonic-clonic muscle spasms (convulsive syncope), accompanied by vomiting and loss of sphincter control.
Systemic reactions can occur during apheresis procedures, which require the use of anticoagulants such as acid-citrate-dextrose for the collection of the blood component 12. This anticoagulant can cause hypocalcaemia, because of chelation. The lowered concentration of calcium ions leads to episodes of paraesthesia of the lips, oral cavity and limbs. These symptoms resolve after interruption of the apheresis procedure, although it may sometimes be necessary to use a therapeutic intervention, such as the administration of calcium gluconate. Much more rarely, tremor, muscle spasms, hypotension, tachycardia, arrhythmia, convulsions and tetany develop.
There are rare reports of acute intoxication due to overdoses of acid-citrate-dextrose 13. Another rare complication, that can occur during apheresis procedures, is severe arrhythmias 12.
Figure 3. Frequency of the symptoms occurring in donors during or immediately after the donation
Note: The donor population analysed consisted of 4,906 donors (3,716 male and 1,190 female). In total, 3,983 (81%) voluntaries have donated whole blood, 851 (17%) plasma from apheresis, 64 (1.3%) experienced multicomponent donation, and 8 (0.1%) were donors of plasma-platelet apheresis in the year from 24th October, 2005 to 24th April 2006.
[Source 12]Blood Transfusions
Early attempts to transfer blood from one person to another produced varied results. Sometimes, the recipient improved. Other times, the recipient suffered a blood transfusion reaction in which the red blood cells clumped, obstructing vessels and producing great pain and organ damage.
Eventually scientists determined that blood is of differing types and that only certain combinations of blood types are compatible. These discoveries led to the development of procedures for typing blood. Today, safe transfusions of whole blood depend on two blood tests—“type and cross match.” First the recipient’s ABO blood type and Rh status are determined. Following this, a “cross match” is done of the recipient’s serum with a small amount of the donor’s red blood cells that have the same ABO type and Rh status as the recipient. Compatibility is determined by examining the mixture under a microscope for agglutination, the clumping of red blood cells. Agglutination (“clumping”) is a reaction between antigens and specific antibodies. This is what happens when antigens on mismatched donated red blood cells react with antibodies in plasma.
Blood Antigens and Antibodies
An antigen, is any molecule that triggers an immune response, the body’s reaction to invasion by a foreign substance or organism. When the immune system encounters an antigen not found on the body’s own cells, it will attack, producing antibodies. In a transfusion reaction, antigens (agglutinogens) on the surface of the donated red blood cells react with antibodies (agglutinins) in the plasma of the recipient, resulting in the agglutination of the donated red blood cells.
A mismatched blood transfusion quickly produces telltale signs of agglutination—anxiety, breathing difficulty, facial flushing, headache, and severe pain in the neck, chest, and lumbar area. Red blood cells burst, releasing free hemoglobin. Liver cells and macrophages phagocytize the hemoglobin, converting it to bilirubin, which may sufficiently accumulate to cause the yellow skin of jaundice. Free hemoglobin reaching the kidneys may ultimately cause them to fail.
Only a few of the 32 known antigens on red blood cell membranes can produce serious transfusion reactions. These include the antigens of the ABO group and those of the Rh group. Avoiding the mixture of certain kinds of antigens and antibodies prevents adverse transfusion reactions.
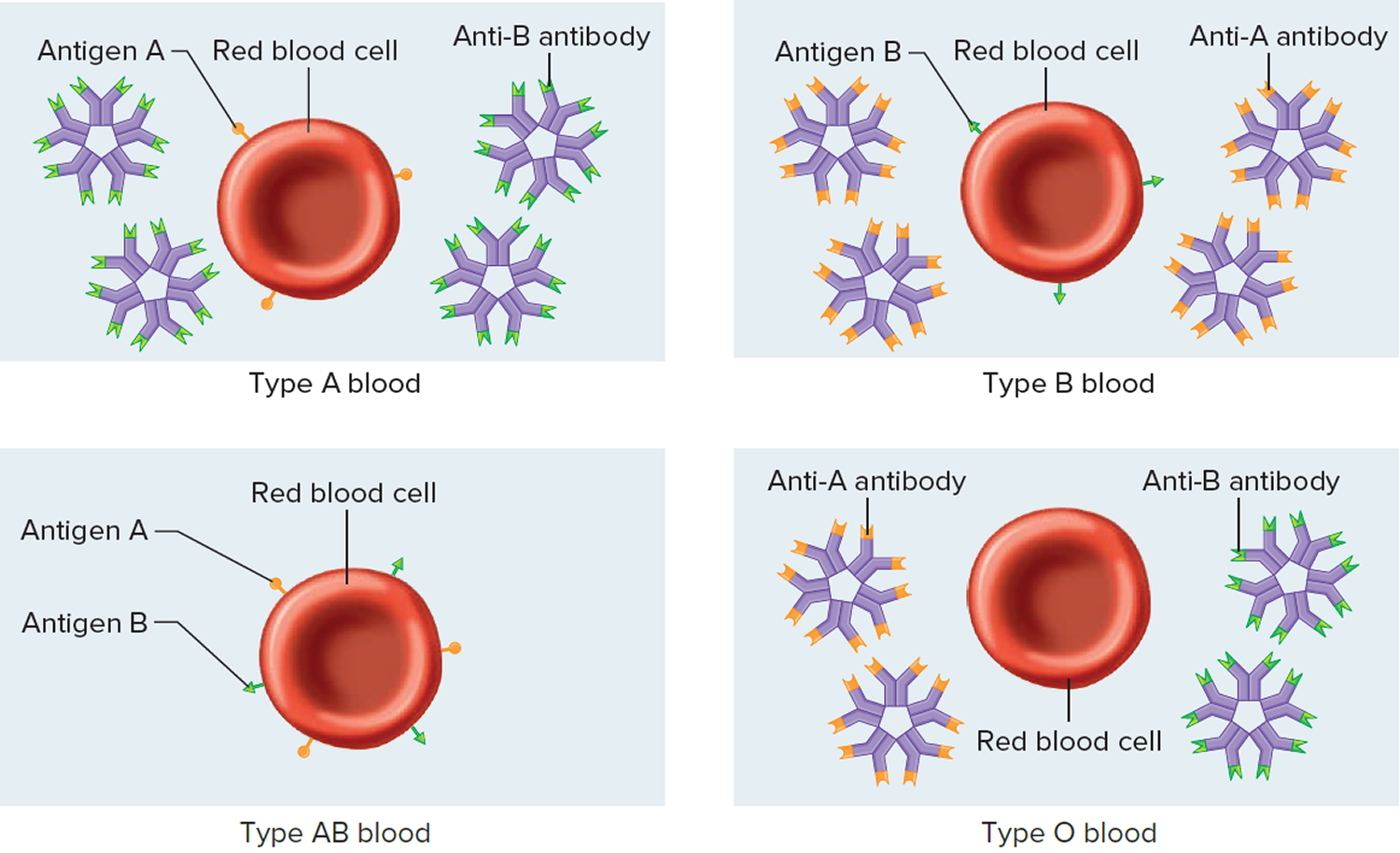
ABO Blood Group
The ABO blood group is based on the presence (or absence) of two major antigens on red blood cell membranes—antigen A and antigen B. A and B antigens are carbohydrates attached to glycolipids projecting from the red blood cell surface. A person’s erythrocytes have on their surfaces one of four antigen combinations: only A, only B, both A and B, or neither A nor B.
A person with only antigen A has type A blood. A person with only antigen B has type B blood. An individual with both antigens A and B has type AB blood. A person with neither antigen A nor B has type O blood. Thus, all people have one of four possible ABO blood types—A, B, AB, or O. The resulting ABO blood type is inherited. It is the consequence of DNA encoding enzymes to synthesize A or B antigens on erythrocytes in one of these four combinations.
- In the United States, the most common ABO blood types are O (47%) and A (41%). Rarer are type B (9%) and type AB (3%). These percentages vary in subpopulations and over time, reflecting changes in the genetic structure of populations.
Antibodies that affect the ABO blood group antigens are present in the plasma about two to eight months following birth, as a result of exposure to foods or microorganisms containing the antigen(s) that are not present on the individual’s red blood cells. Specifically, whenever antigen A is absent in red blood cells, an antibody called anti-A is produced, and whenever antigen B is absent on cells, an antibody called anti-B is produced. Therefore, individuals with type A blood have anti-B antibody in their plasma; those with type B blood have anti-A antibody; those with type AB blood have neither antibody; and those with type O blood have both anti-A and anti-B antibodies (Figure 4 and Table 5). The antibodies anti-A and anti-B are large and do not cross the placenta. Thus, a pregnant woman and her fetus may be of different ABO blood types, but agglutination in the fetus will not occur.
An antibody of one type will react with an antigen of the same type and clump red blood cells; therefore, such combinations must be avoided. The major concern in blood transfusion procedures is that the cells in the donated blood not clump due to antibodies in the recipient’s plasma. For this reason, a person with type A (anti-B) blood must not receive blood of type B or AB, either of which would clump in the presence of anti-B in the recipient’s type A blood. Likewise, a person with type B (anti-A) blood must not receive type A or AB blood, and a person with type O (anti-A and anti-B) blood must not receive type A, B, or AB blood.
Type AB blood does not have anti-A or anti-B antibodies, so an AB person can receive a transfusion of blood of any other type. For this reason, individuals with type AB blood are called universal recipients. However, type A (anti-B) blood, type B (anti-A) blood, and type O (anti-A and anti-B) blood still contain antibodies (either anti-A and/or anti-B) that could agglutinate type AB cells if transfused rapidly.
Consequently, even for AB individuals, using donor blood of the same type as the recipient is best (Table 6). Type O blood has neither antigen A nor antigen B. Therefore, theoretically this type could be transfused into persons with blood of any other type. Individuals with type O blood are called universal donors. Type O blood, however, does contain both anti-A and anti-B antibodies. If type O blood is given to a person with blood type A, B, or AB, it should be transfused slowly so that the recipient’s larger blood volume will dilute the donor blood, minimizing the chance of an adverse reaction.
Figure 4. ABO Blood Types and Antibodies (different combinations of antigens and antibodies distinguish blood types)
Table 5. Antigens and Antibodies of the ABO Blood Group
Blood Type | Antigen | Antibody |
A | A | Anti-B |
B | B | Anti-A |
AB | A and B | Neither anti-A nor anti-B |
O | Neither A nor B | Both anti-A and anti-B |
Table 6. Preferred and Permissible Blood Types for Transfusions
Blood Type of Recipient | Preferred Blood Type of Donor | If Preferred Blood Type Unavailable, Permissible Blood Type of Donor |
A | A | O |
B | B | O |
AB | AB | A, B, O |
O | O | No alternate types |
Rh Blood Group
The Rh (Rhesus) blood group was named after the rhesus monkey in which it was first studied. In humans, this group includes several Rh antigens (factors). The most prevalent of these is antigen D, a transmembrane protein.
If the Rh antigens are present on the red blood cell membranes, the blood is said to be Rh-positive. Conversely, if the red blood cells do not have Rh antigens, the blood is called Rh-negative. The presence (or absence) of Rh antigens is an inherited trait. Anti-Rh antibodies (anti-Rh) form only in Rh-negative individuals in response to the presence of red blood cells with Rh antigens. This happens, for example, if an individual with Rh-negative blood receives a transfusion of Rh-positive blood. The Rh antigens stimulate the recipient to begin producing anti-Rh antibodies. Generally, this initial transfusion has no serious consequences, but if an individual with Rh-negative blood—who is now sensitized to Rh-positive blood—receives another transfusion of Rh-positive blood some months later, the donated red cells are likely to agglutinate.
A similar situation of Rh incompatibility arises when an Rh-negative woman is pregnant with an Rh-positive fetus. Her first pregnancy with an Rh-positive fetus would probably be uneventful. However, if at the time of the infant’s birth (or if a miscarriage occurs) the placental membranes that separated the maternal blood from the fetal blood during the pregnancy tear, some of the infant’s Rh-positive blood cells may enter the maternal circulation. These Rh-positive cells may then stimulate the maternal tissues to produce anti-Rh antibodies. If a woman who has already developed anti-Rh antibodies becomes pregnant with a second Rh-positive fetus, these antibodies, called hemolysins, cross the placental membrane and destroy the fetal red blood cells. The fetus then develops a condition called erythroblastosis fetalis, or hemolytic disease of the fetus and newborn.
Erythroblastosis fetalis is extremely rare today because obstetricians carefully track Rh status. An Rh-negative woman who might carry an Rh-positive fetus is given an injection of a drug called RhoGAM at week 28 of her pregnancy and after delivery of an Rh-positive baby. Rhogam is a preparation of anti-Rh antibodies, which bind to and shield any Rh-positive fetal cells that might contact the woman’s cells and sensitize her immune system. RhoGAM must be given within 72 hours of possible contact with Rh-positive cells—including giving birth, terminating a pregnancy, miscarrying, or undergoing amniocentesis (a prenatal test in which a needle is inserted into the uterus).
- NIH BLOOD BANK. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/can_i_donate.html[↩][↩][↩][↩][↩][↩][↩][↩]
- Age – How does age affect my ability to donate ? Australian Red Cross Blood Service. http://donateblood.com.au/faq/age[↩]
- What does blood do ? National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072576/[↩]
- About Donating Blood. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/about_donating_blood.html[↩]
- Explore Travel Health with the CDC Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/yellowbook-home[↩]
- Bovine Spongiform Encephalopathy (BSE) Questions and Answers. U.S. Food and Drug Administration. https://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm111482.htm[↩]
- National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/index.html[↩][↩][↩]
- Red Cells by Apheresis. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/donationtypes/red_cells.html[↩][↩][↩][↩]
- Platelets by Apheresis. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/donationtypes/platelets.html[↩][↩][↩]
- AB Plasma Donor Program. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/donationtypes/ab_plasma.html[↩][↩][↩][↩]
- Granulocytes by Apheresis. National Institutes of Health Blood Bank. https://clinicalcenter.nih.gov/blooddonor/donationtypes/granulocytes.html[↩][↩][↩][↩]
- Crocco A, D’Elia D. Adverse reactions during voluntary donation of blood and/or blood components. A statistical-epidemiological study. Blood Transfusion. 2007;5(3):143-152. doi:10.2450/2007.0005-07. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2535889/[↩][↩][↩][↩][↩][↩]
- Winters JL. Complications of donor apheresis. J Clin Apher. 2006;21:132–41. https://www.ncbi.nlm.nih.gov/pubmed/15880355[↩]