Contents
- What is prostate gland
- What does the prostate gland do
- What is prostatitis ?
- What is benign prostatic hyperplasia
- Symptoms of benign prostatic hyperplasia
- When to see a doctor
- Causes of benign prostatic hyperplasia
- Risk factors for benign prostatic hyperplasia
- Complications of benign prostatic hyperplasia
- How is benign prostatic hyperplasia diagnosed ?
- How is benign prostatic hyperplasia treated ?
- Home remedies for enlarged prostate
- What does the prostate gland do
What is prostate gland
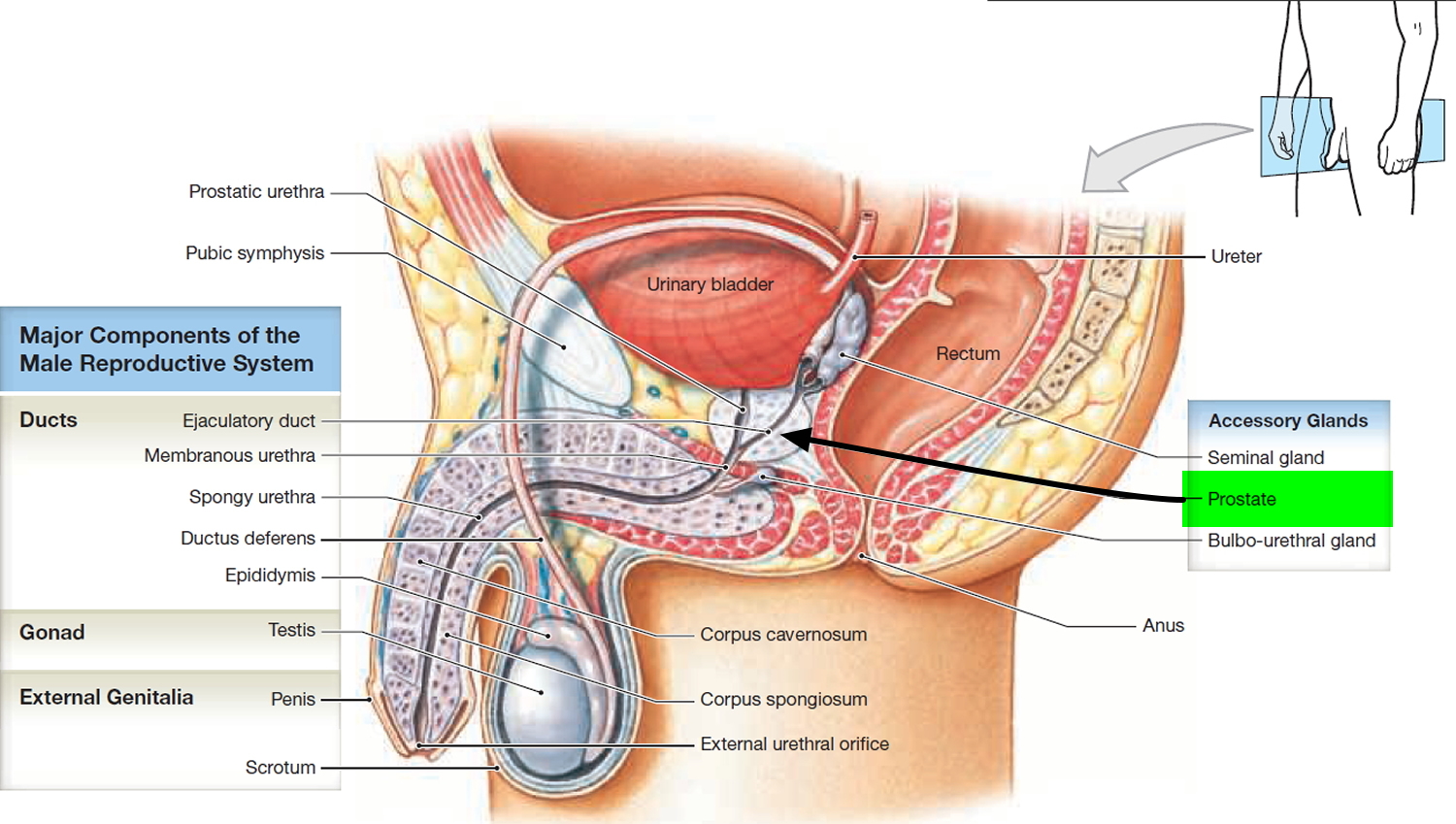
The prostate is a gland found only in men, which forms an important part of the male reproductive system. The prostate gland secretes a fluid that keeps sperm alive and healthy and that forms part of semen.
The prostate is a chestnut-shaped structure that surrounds the urethra and ejaculatory ducts. The prostate is found behind the base of the penis and immediately underneath the urinary bladder. It measures about 2 × 4 × 3 cm and is an aggregate of 30 to 50 compound tubuloacinar glands enclosed in a single fibrous capsule. These glands empty through about 20 pores in the urethral wall. The stroma of the prostate consists of connective tissue and smooth muscle, like that of the seminal vesicles. The thin, milky secretion of the prostate constitutes about 30% of the semen.
The urethra, the tube that carries urine from the bladder to the penis, runs through the middle of the prostate.
The prostate slowly increases in size from birth to puberty. It then expands rapidly until about age 30, after which time its size typically remains stable until about age 40-45, when further enlargement may occur, constricting the urethra and interfering with urine flow.
In addition to its susceptibility to prostate cancer and tumors, the prostate is also subject to infection in sexually transmitted diseases (STDs). Prostatitis, inflammation of the prostate, is the single most common reason that men consult a urologist.
Figure 1. Prostate gland
What does the prostate gland do
The fluid expelled during orgasm is called semen (seminal fluid). A typical ejaculation discharges 2 to 5 mL of semen, composed of about 10% sperm and spermatic duct secretions, 30% prostatic fluid, 60% seminal vesicle fluid, and a trace of bulbourethral fluid. Most of the sperm emerge in the first one or two jets of semen. The semen usually has a sperm count of 50 to 120 million sperm/mL. A sperm count any lower than 20 to 25 million sperm/mL is usually associated with infertility (sterility), the inability to fertilize an egg.
The prostate and seminal vesicles contribute the following constituents to the semen:
- The prostate produces a thin, milky, slightly acidic (pH about 6.5) white fluid containing calcium, citrate, and phosphate ions, which is a nutrient for the sperm,; a clotting enzyme; and a protein-hydrolyzing enzyme called serine protease (prostate-specific antigen, PSA), which is an enzyme that helps liquefy semen. Measuring the levels of PSA (prostate-specific antigen) in a man’s blood is the most important method of screening for prostate cancer. The citric acid in prostatic fluid is used by sperm for ATP production via the Krebs cycle. Several proteolytic enzymes, such as prostate-specific antigen (PSA), pepsinogen, lysozyme, amylase, and hyaluronidase, eventually break down the clotting proteins from the seminal vesicles. The function of the acid phosphatase secreted by the prostate is unknown. Seminalplasmin in prostatic fluid is an antibiotic that can destroy bacteria. Seminalplasmin may help decrease the number of naturally occurring bacteria in semen and in the lower female reproductive tract. Secretions of the prostate enter the prostatic urethra through many prostatic ducts. Prostatic secretions make up about 30% of the volume of semen and contribute to sperm motility and viability.
- The seminal vesicles contribute a viscous yellowish fluid, the last component of the semen to emerge. It contains fructose and other carbohydrates, citrate, prostaglandins and a clotting protein called prosemenogelin.
What is prostatitis ?
Prostatitis is a frequently painful condition that involves inflammation of the prostate and sometimes the areas around the prostate 1.
Scientists have identified four types of prostatitis:
- chronic prostatitis/chronic pelvic pain syndrome
- acute bacterial prostatitis
- chronic bacterial prostatitis
- asymptomatic inflammatory prostatitis
Men with asymptomatic inflammatory prostatitis do not have symptoms. A health care provider may diagnose asymptomatic inflammatory prostatitis when testing for other urinary tract or reproductive tract disorders. This type of prostatitis does not cause complications and does not need treatment.
Symptoms of prostatitis
Prostatitis signs and symptoms depend on the cause. They can include:
- Pain or burning sensation when urinating (dysuria)
- Difficulty urinating, such as dribbling or hesitant urination
- Frequent urination, particularly at night (nocturia)
- Urgent need to urinate
- Cloudy urine
- Blood in the urine
- Pain in the abdomen, groin or lower back
- Pain in the area between the scrotum and rectum (perineum)
- Pain or discomfort of the penis or testicles
- Painful ejaculation
- Flu-like signs and symptoms (with bacterial prostatitis)
When to see a doctor
If you have pelvic pain, difficult or painful urination, or painful ejaculation, see your doctor. If left untreated, some types of prostatitis can cause worsening infection or other health problems.
Causes of prostatitis
Acute bacterial prostatitis is often caused by common strains of bacteria. The infection can start when bacteria in urine leak into your prostate. Antibiotics are used to treat the infection. If they don’t eliminate the bacteria prostatitis might recur or be difficult to treat (chronic bacterial prostatitis).
Nerve damage in the lower urinary tract, which can be caused by surgery or trauma to the area, might contribute to prostatitis not caused by a bacterial infection. In many cases of prostatitis, the cause isn’t identified.
Risk factors for prostatitis
Risk factors for prostatitis include:
- Being a young or middle-aged
- Having had prostatitis
- Having an infection in the bladder or the tube that transports semen and urine to the penis (urethra)
- Having pelvic trauma, such as an injury from bicycling or horseback riding
- Using a tube inserted into the urethra to drain the bladder (urinary catheter)
- Having HIV/AIDS
- Having had a prostate biopsy
Complications of prostatitis
Complications of prostatitis can include:
- Bacterial infection of the blood (bacteremia)
- Inflammation of the coiled tube attached to the back of the testicle (epididymitis)
- Pus-filled cavity in the prostate (prostatic abscess)
- Semen abnormalities and infertility, which can occur with chronic prostatitis
There’s no direct evidence that prostatitis can lead to prostate cancer.
Diagnosis of prostatitis
Diagnosing prostatitis involves ruling out other conditions as the cause of your symptoms and determining what kind of prostatitis you have. Your doctor will ask about your medical history and your symptoms. He or she will also do a physical exam, which will likely include a digital rectal examination.
Initial diagnostic tests might include:
- Urine tests. Your doctor might have a sample of your urine analyzed to look for signs of infection in your urine (urinalysis). Your doctor might also send a sample of your urine to a lab to determine if you have an infection.
- Blood tests. Your doctor might examine samples of your blood for signs of infection and other prostate problems.
- Post-prostatic massage. In rare cases, your doctor might massage your prostate and test the secretions.
- Imaging tests. In some cases, your doctor might order a CT scan of your urinary tract and prostate or a sonogram of your prostate. CT scan images provide more detailed information than plain X-rays do. A sonogram is the visual image produced by an ultrasound.
Based on your symptoms and test results, your doctor might conclude that you have one of the following types of prostatitis:
- Acute bacterial prostatitis. Often caused by common strains of bacteria, this type of prostatitis generally starts suddenly and causes flu-like signs and symptoms, such as fever, chills, nausea and vomiting.
- Chronic bacterial prostatitis. When antibiotics don’t eliminate the bacteria causing prostatitis, you can develop recurring or difficult-to-treat infections. Between bouts of chronic bacterial prostatitis, you might have no symptoms or only minor ones.
- Chronic prostatitis/chronic pelvic pain syndrome. This type of prostatitis — the most common —isn’t caused by bacteria. Often an exact cause can’t be identified. For some men, symptoms stay about the same over time. For others, the symptoms go through cycles of being more and less severe.
- Asymptomatic inflammatory prostatitis. This type of prostatitis doesn’t cause symptoms and is usually found only by chance when you’re undergoing tests for other conditions. It doesn’t require treatment.
Treatment for prostatitis
Prostatitis treatments depend on the underlying cause. They can include:
- Antibiotics. This is the most commonly prescribed treatment for prostatitis. Your doctor will choose your medication based on the type of bacteria that might be causing your infection.
If you have severe symptoms, you might need intravenous (IV) antibiotics. You’ll likely need to take oral antibiotics for four to six weeks but might need longer treatment for chronic or recurring prostatitis.
- Alpha blockers. These medications help relax the bladder neck and the muscle fibers where your prostate joins your bladder. This treatment might ease symptoms, such as painful urination.
- Anti-inflammatory agents. Nonsteroidal anti-inflammatory drugs (NSAIDs) might make you more comfortable.
Home remedies for prostatitis
The following might ease some symptoms of prostatitis:
- Soak in a warm bath (sitz bath) or use a heating pad.
- Limit or avoid alcohol, caffeine, and spicy or acidic foods, which can irritate your bladder.
- Avoid activities that can irritate your prostate, such as prolonged sitting or bicycling.
- Drink plenty of caffeine-free beverages. This will cause you to urinate more and help flush bacteria from your bladder.
Alternative therapies that show some promise for reducing symptoms of prostatitis include:
- Biofeedback. A biofeedback specialist uses signals from monitoring equipment to teach you to control certain body functions and responses, including relaxing your muscles.
- Acupuncture. This involves inserting very thin needles through your skin to various depths at certain points on your body.
- Herbal remedies and supplements. There’s no evidence that herbs and supplements improve prostatitis, although many men take them. Some herbal treatments for prostatitis include rye grass (cernilton), a chemical found in green tea, onions and other plants (quercetin) and extract of the saw palmetto plant.
Discuss your use of alternative medicine practices and supplements with your doctor.
What is benign prostatic hyperplasia
An enlarged prostate is also called benign prostatic hyperplasia (BPH) 2. Most men will have enlarged prostate (benign prostatic hyperplasia) as they get older. Symptoms often start after age 50.
In 2010, as many as 14 million men in the United States had lower urinary tract symptoms suggestive of benign prostatic hyperplasia 3. Although benign prostatic hyperplasia rarely causes symptoms before age 40, the occurrence and symptoms increase with age. Benign prostatic hyperplasia affects about 50 percent of men between the ages of 51 and 60 and up to 90 percent of men older than 80 4.
Benign prostatic hyperplasia (BPH) is not cancer, and it does not seem to increase your chance of getting prostate cancer 2. But the early symptoms are the same. Check with your doctor if you have:
- A frequent and urgent need to urinate, especially at night
- Trouble starting a urine stream or making more than a dribble
- A urine stream that is weak, slow, or stops and starts several times
- The feeling that you still have to go, even just after urinating
- Small amounts of blood in your urine
Severe benign prostatic hyperplasia (BPH) can cause serious problems over time. Untreated, prostate gland enlargement can block the flow of urine out of the bladder and cause bladder, urinary tract or kidney problems.. If it is found early, you are less likely to develop these problems.
Tests for benign prostatic hyperplasia (BPH) include a digital rectal exam, blood and imaging tests, a urine flow study, and examination with a scope called a cystoscope. Treatments include watchful waiting, medicines, nonsurgical procedures, and surgery.
Symptoms of benign prostatic hyperplasia
The severity of symptoms in people who have prostate gland enlargement varies, but symptoms tend to gradually worsen over time. Common signs and symptoms of benign prostatic hyperplasia include:
- Frequent or urgent need to urinate
- Increased frequency of urination at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Straining while urinating
- Inability to completely empty the bladder
Less common signs and symptoms include:
- Urinary tract infection
- Inability to urinate
- Blood in the urine
The size of your prostate doesn’t necessarily mean your symptoms will be worse. Some men with only slightly enlarged prostates can have significant symptoms, while other men with very enlarged prostates can have only minor urinary symptoms.
In some men, symptoms eventually stabilize and might even improve over time.
Other possible causes of urinary symptoms
Conditions that can lead to symptoms similar to those caused by enlarged prostate include:
- Urinary tract infection
- Inflammation of the prostate (prostatitis)
- Narrowing of the urethra (urethral stricture)
- Scarring in the bladder neck as a result of previous surgery
- Bladder or kidney stones
- Problems with nerves that control the bladder
- Cancer of the prostate or bladder
When to see a doctor
If you’re having urinary problems, discuss them with your doctor. Even if you don’t find urinary symptoms bothersome, it’s important to identify or rule out any underlying causes. Untreated, urinary problems might lead to obstruction of the urinary tract.
If you’re unable to pass any urine, seek immediate medical attention.
Causes of benign prostatic hyperplasia
The prostate gland is located beneath your bladder. The tube that transports urine from the bladder out of your penis (urethra) passes through the center of the prostate. When the prostate enlarges, it begins to block urine flow.
Most men have continued prostate growth throughout life. In many men, this continued growth enlarges the prostate enough to cause urinary symptoms or to significantly block urine flow.
It isn’t entirely clear what causes the prostate to enlarge. However, it might be due to changes in the balance of sex hormones as men grow older.
Risk factors for benign prostatic hyperplasia
Risk factors for prostate gland enlargement include:
- Aging. Prostate gland enlargement rarely causes signs and symptoms in men younger than age 40. About one-third of men experience moderate to severe symptoms by age 60, and about half do so by age 80.
- Family history. Having a blood relative, such as a father or brother, with prostate problems means you’re more likely to have problems.
- Ethnic background. Prostate enlargement is less common in Asian men than in white and black men. Black men might experience symptoms at a younger age than white men.
- Diabetes and heart disease. Studies show that diabetes, as well as heart disease and use of beta blockers, might increase the risk of benign prostatic hyperplasia.
- Lifestyle. Obesity increases the risk of benign prostatic hyperplasia, while exercise can lower your risk.
Complications of benign prostatic hyperplasia
Complications of enlarged prostate can include:
- Sudden inability to urinate (urinary retention). You might need to have a tube (catheter) inserted into your bladder to drain the urine. Some men with an enlarged prostate need surgery to relieve urinary retention.
- Urinary tract infections (UTIs). Inability to fully empty the bladder can increase the risk of infection in your urinary tract. If UTIs occur frequently, you might need surgery to remove part of the prostate.
- Bladder stones. These are generally caused by an inability to completely empty the bladder. Bladder stones can cause infection, bladder irritation, blood in the urine and obstruction of urine flow.
- Bladder damage. A bladder that hasn’t emptied completely can stretch and weaken over time. As a result, the muscular wall of the bladder no longer contracts properly, making it harder to fully empty your bladder.
- Kidney damage. Pressure in the bladder from urinary retention can directly damage the kidneys or allow bladder infections to reach the kidneys.
Most men with an enlarged prostate don’t develop these complications. However, acute urinary retention and kidney damage can be serious health threats.
Having an enlarged prostate doesn’t affect your risk of developing prostate cancer.
How is benign prostatic hyperplasia diagnosed ?
Your doctor will start by asking detailed questions about your symptoms and doing a physical exam. This initial exam is likely to include:
- Digital rectal exam. The doctor inserts a finger into the rectum to check your prostate for enlargement.
- Urine test. Analyzing a sample of your urine can help rule out an infection or other conditions that can cause similar symptoms.
- Blood test. The results can indicate kidney problems.
- Prostate-specific antigen (PSA) blood test. PSA is a substance produced in your prostate. PSA levels increase when you have an enlarged prostate. However, elevated PSA levels can also be due to recent procedures, infection, surgery or prostate cancer.
- Neurological exam. This brief evaluation of your mental functioning and nervous system can help identify causes of urinary problems other than enlarged prostate.
After that, your doctor might recommend additional tests to help confirm an enlarged prostate and to rule out other conditions. These additional tests might include:
- Urinary flow test. You urinate into a receptacle attached to a machine that measures the strength and amount of your urine flow. Test results help determine over time if your condition is getting better or worse.
- Postvoid residual volume test. This test measures whether you can empty your bladder completely. The test can be done using ultrasound or by inserting a catheter into your bladder after you urinate to measure how much urine is left in your bladder.
- 24-hour voiding diary. Recording the frequency and amount of urine might be especially helpful if more than one-third of your daily urinary output occurs at night.
If your condition is more complex, your doctor may recommend:
- Transrectal ultrasound. An ultrasound probe is inserted into your rectum to measure and evaluate your prostate.
- Prostate biopsy. Transrectal ultrasound guides needles used to take tissue samples (biopsies) of the prostate. Examining the tissue can help your doctor diagnose or rule out prostate cancer.
- Urodynamic and pressure flow studies. A catheter is threaded through your urethra into your bladder. Water — or, less commonly, air — is slowly injected into your bladder. Your doctor can then measure bladder pressure and determine how well your bladder muscles are working.
- Cystoscopy. A lighted, flexible cystoscope is inserted into your urethra, allowing your doctor to see inside your urethra and bladder. You will be given a local anesthetic before this test.
- Intravenous pyelogram or CT urogram. A tracer is injected into a vein. X-rays or CT scans are then taken of your kidneys, bladder and the tubes that connect your kidneys to your bladder (ureters). These tests can help detect urinary tract stones, tumors or blockages above the bladder.
How is benign prostatic hyperplasia treated ?
A wide variety of treatments are available for enlarged prostate, including medication, minimally invasive therapies and surgery. The best treatment choice for you depends on several factors, including:
- The size of your prostate
- Your age
- Your overall health
- The amount of discomfort or bother you are experiencing
If your symptoms are tolerable, you might decide to postpone treatment and simply monitor your symptoms. For some men, symptoms can ease without treatment.
Medication
Medication is the most common treatment for mild to moderate symptoms of prostate enlargement. The options include:
- Alpha blockers. These medications relax bladder neck muscles and muscle fibers in the prostate, making urination easier. Alpha blockers — which include alfuzosin (Uroxatral), doxazosin (Cardura), tamsulosin (Flomax), and silodosin (Rapaflo) — usually work quickly in men with relatively small prostates. Side effects might include dizziness and a harmless condition in which semen goes back into the bladder instead of out the tip of the penis (retrograde ejaculation).
- 5-alpha reductase inhibitors. These medications shrink your prostate by preventing hormonal changes that cause prostate growth. These medications — which include finasteride (Proscar) and dutasteride (Avodart) — might take up to six months to be effective. Side effects include retrograde ejaculation.
- Combination drug therapy. Your doctor might recommend taking an alpha blocker and a 5-alpha reductase inhibitor at the same time if either medication alone isn’t effective.
- Tadalafil (Cialis). Studies suggest this medication, which is often used to treat erectile dysfunction, can also treat prostate enlargement. However, this medication is not routinely used for enlarged prostate and is generally prescribed only to men who also experience erectile dysfunction.
Minimally invasive or surgical therapy
Minimally invasive or surgical therapy might be recommended if:
- Your symptoms are moderate to severe
- Medication hasn’t relieved your symptoms
- You have a urinary tract obstruction, bladder stones, blood in your urine or kidney problems
- You prefer definitive treatment
Minimally invasive or surgical therapy might not be an option if you have:
- An untreated urinary tract infection
- Urethral stricture disease
- A history of prostate radiation therapy or urinary tract surgery
- A neurological disorder, such as Parkinson’s disease or multiple sclerosis
Any type of prostate procedure can cause side effects. Depending on the procedure you choose, complications might include:
- Semen flowing backward into the bladder instead of out through the penis during ejaculation
- Temporary difficulty with urination
- Urinary tract infection
- Bleeding
- Erectile dysfunction
- Very rarely, loss of bladder control (incontinence)
There are several types of minimally invasive or surgical therapy.
Transurethral resection of the prostate (TURP)
A lighted scope is inserted into your urethra, and the surgeon removes all but the outer part of the prostate. TURP generally relieves symptoms quickly, and most men have a stronger urine flow soon after the procedure. After TURP you might temporarily need a catheter to drain your bladder, and you’ll be able to do only light activity until you’ve healed.
Transurethral incision of the prostate (TUIP)
A lighted scope is inserted into your urethra, and the surgeon makes one or two small cuts in the prostate gland — making it easier for urine to pass through the urethra. This surgery might be an option if you have a small or moderately enlarged prostate gland, especially if you have health problems that make other surgeries too risky.
Transurethral microwave thermotherapy (TUMT)
Your doctor inserts a special electrode through your urethra into your prostate area. Microwave energy from the electrode destroys the inner portion of the enlarged prostate gland, shrinking it and easing urine flow. This surgery is generally used only on small prostates in special circumstances because re-treatment might be necessary.
Transurethral needle ablation (TUNA)
In this outpatient procedure, a scope is passed into your urethra, allowing your doctor to place needles into your prostate gland. Radio waves pass through the needles, heating and destroying excess prostate tissue that’s blocking urine flow.
This procedure might be a good choice if you bleed easily or have certain other health problems. However, like TUMT, TUNA might only partially relieve your symptoms and it might take some time before you notice results.
Laser therapy
A high-energy laser destroys or removes overgrown prostate tissue. Laser therapy generally relieves symptoms right away and has a lower risk of side effects than does nonlaser surgery. Laser therapy might be used in men who shouldn’t have other prostate procedures because they take blood-thinning medications.
The options for laser therapy include:
- Ablative procedures. These procedures vaporize obstructive prostate tissue to increase urine flow. Examples include photoselective vaporization of the prostate (PVP) and holmium laser ablation of the prostate (HoLAP). Ablative procedures can cause irritating urinary symptoms after surgery, so in rare situations another resection procedure might be needed at some point.
- Enucleative procedures. Enucleative procedures, such as holmium laser enucleation of the prostate (HoLEP), generally remove all the prostate tissue blocking urine flow and prevent regrowth of tissue. The removed tissue can be examined for prostate cancer and other conditions. These procedures are similar to open prostatectomy.
Prostate lift
In this experimental transurethral procedure, special tags are used to compress the sides of the prostate to increase the flow of urine. Long-term data on the effectiveness of this procedure aren’t available.
Embolization
In this experimental procedure, the blood supply to or from the prostate is selectively blocked, causing the prostate to decrease in size. Long-term data on the effectiveness of this procedure aren’t available.
Open or robot-assisted prostatectomy
The surgeon makes an incision in your lower abdomen to reach the prostate and remove tissue. Open prostatectomy is generally done if you have a very large prostate, bladder damage or other complicating factors. The surgery usually requires a short hospital stay and is associated with a higher risk of needing a blood transfusion.
Follow-up care
Your follow-up care will depend on the specific technique used to treat your enlarged prostate.
Your doctor might recommend limiting heavy lifting and excessive exercise for seven days if you have laser ablation, transurethral needle ablation or transurethral microwave therapy. If you have open or robot-assisted prostatectomy, you might need to restrict activity for six weeks.
Whichever procedure you have, your doctor likely will suggest that you drink plenty of fluids afterward.
Home remedies for enlarged prostate
To help control the symptoms of an enlarged prostate, try to:
- Limit beverages in the evening. Don’t drink anything for an hour or two before bedtime to avoid middle-of-the-night trips to the toilet.
- Limit caffeine and alcohol. They can increase urine production, irritate the bladder and worsen symptoms.
- Limit decongestants or antihistamines. These drugs tighten the band of muscles around the urethra that control urine flow, making it harder to urinate.
- Go when you first feel the urge. Waiting too long might overstretch the bladder muscle and cause damage.
- Schedule bathroom visits. Try to urinate at regular times — such as every four to six hours during the day — to “retrain” the bladder. This can be especially useful if you have severe frequency and urgency.
- Follow a healthy diet. Obesity is associated with enlarged prostate.
- Stay active. Inactivity contributes to urine retention. Even a small amount of exercise can help reduce urinary problems caused by an enlarged prostate.
- Urinate — and then urinate again a few moments later. This practice is known as double voiding.
- Keep warm. Colder temperatures can cause urine retention and increase the urgency to urinate.
The Food and Drug Administration hasn’t approved any herbal medications for treatment of an enlarged prostate.
Studies on herbal therapies as a treatment for enlarged prostate have had mixed results. One study found that saw palmetto extract was as effective as finasteride in relieving symptoms of benign prostatic hyperplasia, although prostate volumes weren’t reduced. But a subsequent placebo-controlled trial found no evidence that saw palmetto is better than a placebo.
Other herbal treatments — including beta-sitosterol extracts, pygeum and rye grass — have been suggested as helpful for reducing enlarged prostate symptoms. But the safety and efficacy of these treatments hasn’t been proved.
If you take any herbal remedies, tell your doctor. Certain herbal products might increase the risk of bleeding or interfere with other medications you’re taking.
- Prostatitis: Inflammation of the Prostate. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate[↩]
- Prostate Enlargement (Benign Prostatic Hyperplasia). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia[↩][↩]
- Deters LA. Benign prostatic hypertrophy. https://emedicine.medscape.com/article/437359-overview[↩]
- BPH: surgical management. Urology Care Foundation. http://www.urologyhealth.org/urologic-conditions/benign-prostatic-hyperplasia-(bph)/treatment/surgery?article=31[↩]