Contents
What is seminal vesicle
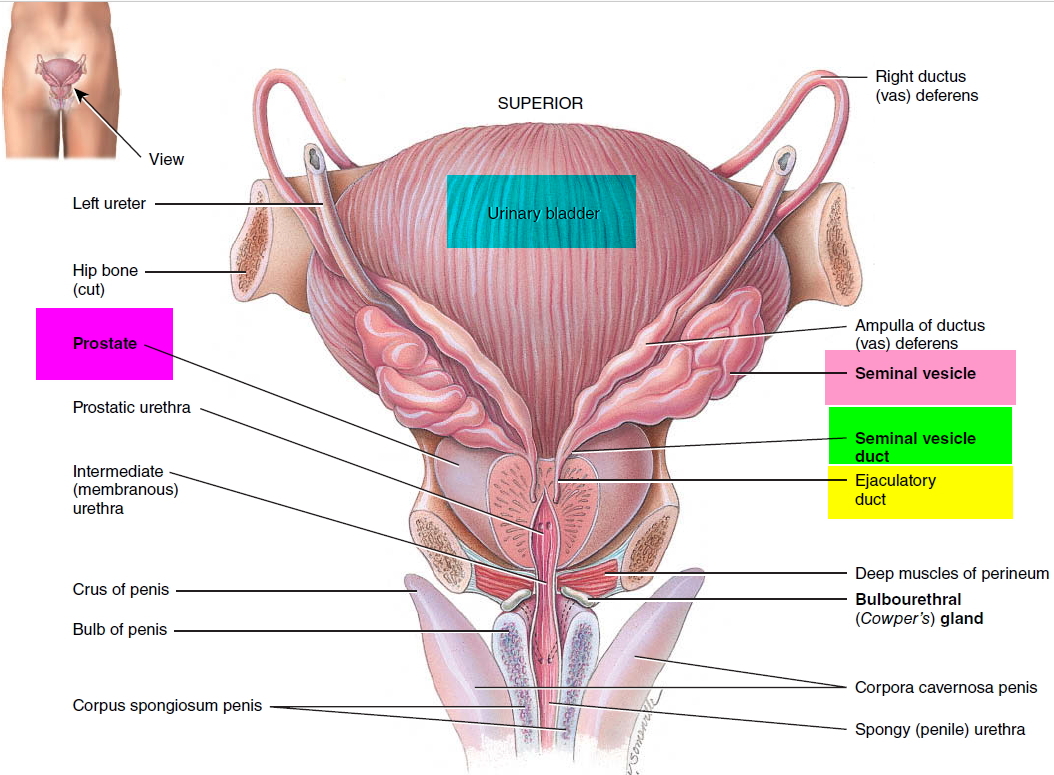
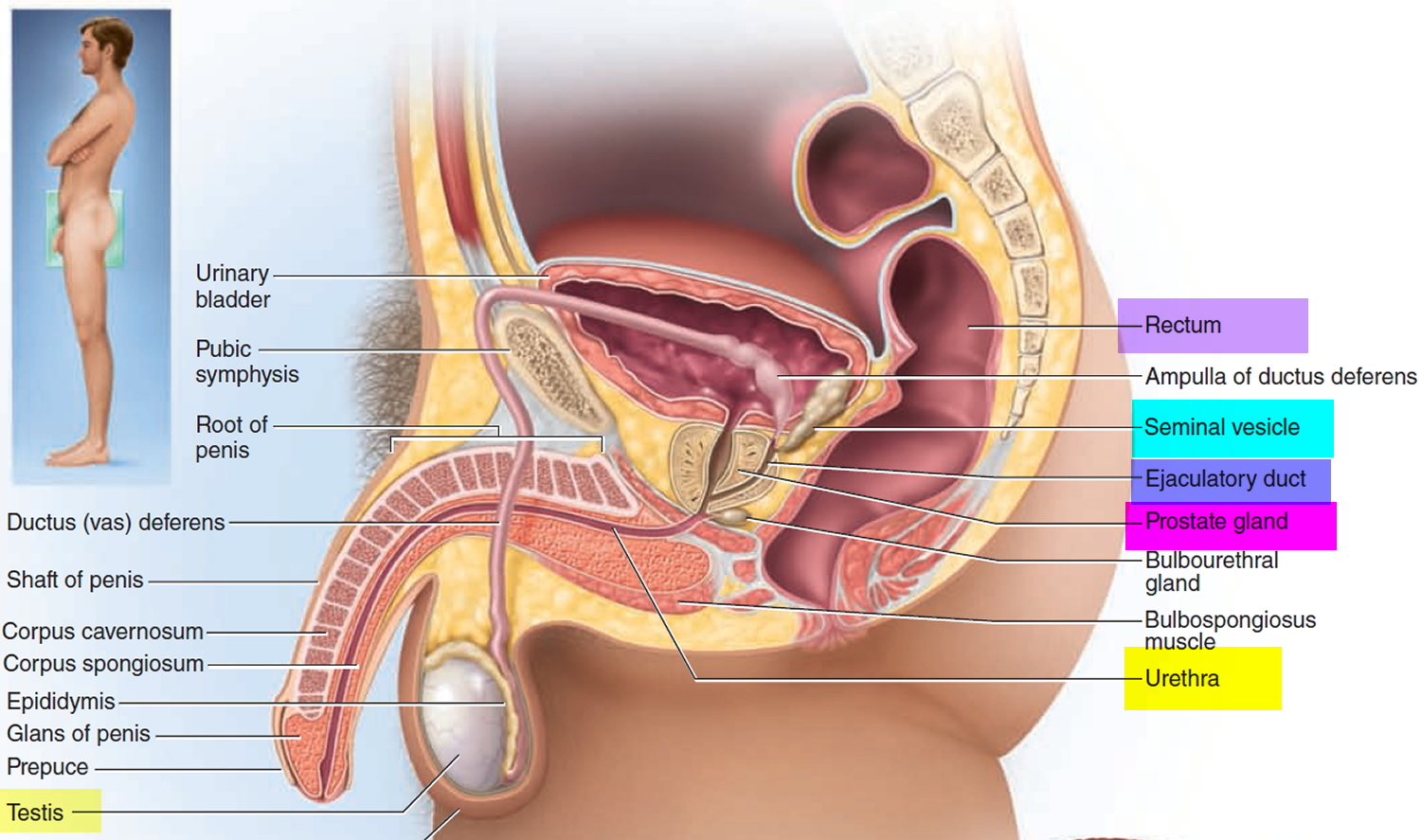
The seminal vesicles (seminal glands) are convoluted pouchlike structures (pair of seminal glands) posterior to the urinary bladder; one is associated with each ductus deferens. A seminal vesicle is about 5 cm long, with approximately the dimensions of one’s little finger. It has a connective tissue capsule and underlying layer of smooth muscle. The secretory portion is a very convoluted duct with numerous branches that form a complex labyrinth. It empties into the ejaculatory duct. Each ejaculatory duct is about 2 cm (1 in.) long and is formed by the union of the duct from the seminal vesicle and the ampulla of the ductus (vas) deferens. The short ejaculatory ducts form just superior to the base (superior portion) of the prostate and pass inferiorly and anteriorly through the prostate. They terminate in the prostatic urethra, where they eject sperm and seminal vesicle secretions just before the release of semen from the urethra to the exterior.
The yellowish secretion of the seminal vesicles constitutes about 60% of the semen.
Figure 1. Seminal vesicle location
Figure 2. Seminal vesicle
What does the seminal vesicle do
The fluid expelled during orgasm is called semen (seminal fluid). A typical ejaculation discharges 2 to 5 mL of semen, composed of about 10% sperm and spermatic duct secretions, 30% prostatic fluid, 60% seminal vesicle fluid, and a trace of bulbourethral fluid. Most of the sperm emerge in the first one or two jets of semen. The semen usually has a sperm count of 50 to 120 million sperm/mL. A sperm count any lower than 20 to 25 million sperm/mL is usually associated with infertility (sterility), the inability to fertilize an egg.
The prostate and seminal vesicles contribute the following constituents to the semen:
- The prostate produces a thin, milky white fluid containing calcium, citrate, and phosphate ions, which is a nutrient for the sperm,; a clotting enzyme; and a protein-hydrolyzing enzyme called serine protease (prostate-specific antigen, PSA), which is an enzyme that helps liquefy semen. Measuring the levels of PSA (prostate-specific antigen) in a man’s blood is the most important method of screening for prostate cancer
- The seminal vesicles contribute an alkaline viscous yellowish fluid, the last component of the semen to emerge. It contains fructose and other carbohydrates, citrate, prostaglandins and clotting proteins called prosemenogelin that are different from those in blood. The alkaline nature of the seminal
fluid helps to neutralize the acidic environment of the male urethra and female reproductive tract that otherwise would inactivate and kill sperm. The fructose is used for ATP production by sperm. Prostaglandins contribute to sperm motility and viability and may stimulate smooth muscle contractions within the female reproductive tract. The clotting proteins help semen coagulate after ejaculation. It is thought that coagulation occurs in order to keep sperm cells from leaking from the vagina. Fluid secreted by the seminal vesicles normally constitutes about 60% of the volume of semen.
Seminal vesicle cancer
Seminal vesicle cancer (primary malignancy) are extremely rare in clinical practice 1 and only 100 such cases have been reported in the literature 2. However secondary spread is quite common either due to disseminated disease or by contiguous spread from adjacent organ, most commonly from prostate cancer 3. Most common organs from where malignancies spread to seminal vesicle are prostate, bladder and rectum. About 12% of prostate malignancy involves seminal vesicle. Bladder and rectal malignancies involve seminal vesicle only when the primary is locally advanced.
It is important to differentiate between primary and secondary spread as the former is a localized disease with possibility of cure while the later is usually an advanced disease with dismal prognosis. There is paucity of data regarding management protocols and most of the time the treatment is individualized.
Symptoms of seminal vesicle cancer can be hematospermia (blood in semen) and pain during ejaculation 1.
Types of seminal vesicle cancers
Seminal vesicle malignancies are classified as adenocarcinoma, mesenchymal tumors and mixed epithelial tumors. Adenocarcinoma is the most common primary malignant tumor of the seminal vesicle with the tumour confined to the seminal vesicle without prostatic involvement 1. Immunohistochemical studies should be negative for both PSA and prostate specific acid phosphatise 4. Mixed epithelial tumors 5 should have no normal seminal vesicle inside the tumor, without invasion of the prostate and immunohistochemical studies should be negative for both PSA and prostate specific acid phosphatase.
Operable primary seminal vesicle adenocarcinomas are treated with radical surgery – cystoprostosemino-vesiculolectomy with bilateral pelvic lymphadenectomy. Long term survival data are not available. No definite recommendations are available for adjuvant therapy, which must be individualized.
Inflammation of the seminal vesicle
Seminal vesiculitis is the seminal vesicles inflammation 6. It is a common disease of male urogenital tract. Its cause is unclear, but the lack of semenogelin I secretion is believed to be the cause of seminal vesiculitits, as it has antibacterial properties to prevent bacterial inflammation 7. Patients with seminal vesiculitis present with hematospermia (blood in semen), discomfort and pain in lumbosacral or perineal region, irritative and obstructive urinary symptoms, decreased semen volume, and/or azoospermia (absence of motile and hence viable sperm in the semen) 8. CT and MRI diagnose the complication and transurethral surgery corrected the issue 8. Transrectal ultrasonography (TRUS) can diagnosis cases of seminal vesiculitis, as well 9. Furuya et. al 10 determined that patients with urethritis are likely to have seminal vesiculitis, suggesting a close relationship between them. It is also known that epididymitis is possible along with seminal vesiculitis 11.
Seminal vesicle cyst infection
Seminal vesicle cyst infection occurs because of bacterial infection and can result in many complications. Palmer et. al 12 reported a case of patient presenting symptoms of perineal pain and fever. The patient had come in earlier with methicillin-sensitive staphylococcus aureus bacterium, and was treated with antibiotics. CT revealed an expansion of a seminal vesicle cyst, and MRI was used to confirm the diagnosis as infected cyst. Cyst was drained and it was determined that methicillin-sensitive bacterium was the cause of infection and the patient was discharged on vancomycin 12. Xu et al 13 study revealed hematospermia due to seminal vesicle cyst infection. Transvesical removal of mass was an effective surgical procedure to alleviate the disease.
Seminal vesicle abscess
Seminal vesicles abscess is a rare pathology that is rarely encountered 14. It is an infection that develops on seminal vesicles due to bacterial or viral microorganisms. Patients suffering from seminal vesicles abscess present with many uro-genital symptoms 15. Abscesses of the seminal vesicles may develop secondary to a surgical procedure due to infection. Seminal vesicles abscess may be developed secondary to vasectomy, tuberculosis, and prostate biopsy (38-41). There are different diagnostic modalities present to diagnosis seminal vesicles abscess, CT, MRI, but TRUS should be primary means of diagnosis 16. Cui et al 17 described another modality, transurethral seminal vesiculoscopy, which is used to diagnosis and treat hematospermia secondary to seminal vesicles. Drainage of abscess is the most common means of treatment 18.
- Ramamurthy R, Periasamy S, Mettupalayam V. Primary malignancy of seminal vesicle: A rare entity. Indian Journal of Urology : IJU : Journal of the Urological Society of India. 2011;27(1):137-139. doi:10.4103/0970-1591.78417. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114576/[↩][↩][↩]
- Bostwick DG. Urologic surgical pathology. In: Bostwick DG, editor. Seminal Vesicles. 2nd ed. China: Mosby Elsevier; 2008. pp. 582–90.[↩]
- Turek PJ. Seminal vesicle and Ejaculatory duct surgery. In: Graham SD, editor. Glenn’s urologic surgery. 6th ed. Philadelphia: Lippincott: Williams and Wilkins; 2004. pp. 439–49.[↩]
- Primary adenocarcinoma of the seminal vesicle. Tarján M, Ottlecz I, Tot T. Indian J Urol. 2009 Jan; 25(1):143-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684320/[↩]
- Low-grade phyllodes tumor of the seminal vesicle treated with laparoscopic excision. Khan MS, Zaheer LU, Ahmed K, Cahill D, Horsfield C, Rottenberg G, Dasgupta P. Nat Clin Pract Urol. 2007 Jul; 4(7):395-400. https://www.ncbi.nlm.nih.gov/pubmed/17615551/[↩]
- Dagur G, Warren K, Suh Y, Singh N, Khan SA. Detecting diseases of neglected seminal vesicles using imaging modalities: A review of current literature. International Journal of Reproductive Biomedicine. 2016;14(5):293-302. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4910035/[↩]
- Liu B, Song Z, Xu A, Su S, Wang Z, Yin C. Is abnormal expression of semenogelin I involved with seminal vesiculitis? Med Hypotheses. 2014;82:338–340. https://www.ncbi.nlm.nih.gov/pubmed/24472869[↩]
- Li YF, Liang PH, Sun ZY, Zhang Y, Bi G, Zhou B, et al. Imaging diagnosis, transurethral endoscopic observation, and management of 43 cases of persistent and refractory hematospermia. J Androl. 2012;33:906–916. https://www.ncbi.nlm.nih.gov/pubmed/22323622[↩][↩]
- Xu B, Li P, Niu X, Zhang X, Wang Z, Qin C, et al. A new method of chronic and recurrent seminal vesiculitis treatment. J Endourol. 2011;25:1815–1818. https://www.ncbi.nlm.nih.gov/pubmed/21870960[↩]
- Furuya R, Takahashi S, Furuya S, Saitoh N, Ogura H, Kurimura Y, et al. Is urethritis accompanied by seminal vesiculitis? Int J Urol. 2009;16:628–631. https://www.ncbi.nlm.nih.gov/pubmed/19456989[↩]
- Furuya R, Takahashi S, Furuya S, Takeyama K, Masumori N, Tsukamoto T. Chlamydial seminal vesiculitis without symptomatic urethritis and epididymitis. Int J Urol. 2006;13:466–467. https://www.ncbi.nlm.nih.gov/pubmed/16734877[↩]
- Palmer WC, Patel NC, Renew JR, Bridges MD, Stancampiano FF. Acute infection of a documented seminal vesicle cyst via hematogenous seeding. Urol J. 2013;10:1157–1159. http://www.urologyjournal.org/index.php/uj/article/view/1181/768[↩][↩]
- Xu LW, Cheng S, Zhang ZG, Li XD. [Transvesical removal of seminal vesicle mass: a report of 5 cases] Zhonghua Nan Ke Xue. 2009;15:357–359. https://www.ncbi.nlm.nih.gov/pubmed/19472913[↩]
- Saha S, Wright G, Arulampalam T, Corr J. An unusual groin mass. Seminal vesicle abscess: a case report. Cases Journal. 2009;2:6531. doi:10.1186/1757-1626-2-6531. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740224/[↩]
- Madrid Garcia FJ, Madronero Cuevas C, Rivas Escudero JA, Parra Muntaner L, Monsalve Rodriguez M, Garcia Alonso J. [Conservative treatment of a seminal vesicle abscess Report of one case] Arch Esp Urol. 2004;57:438–440. https://www.ncbi.nlm.nih.gov/pubmed/15270290[↩]
- Bayne CE, Davis WA, Rothstein CP, Engel JD. Seminal vesicle abscess following prostate biopsy requiring transgluteal percutaneous drainage. Can J Urol. 2013;20:6811–6814. https://www.ncbi.nlm.nih.gov/pubmed/23783054[↩]
- Cui ZQ, Wang YC, Du J, Zhou HJ, Yu ZY, Gao EJ, et al. [Transurethral seminal vesiculoscopy combined with finasteride for recurrent hematospermia] Zhonghua Nan Ke Xue. 2014;20:536–538. https://www.ncbi.nlm.nih.gov/pubmed/25029861[↩]
- Monzo JI, Lledo Garcia E, Cabello Benavente R, Moralejo Garate M, Diez Cordero JM, Hernandez Fernandez C. [Primary seminal vesicle abscess: diagnosis and treatment by transrectal ultrasound] Actas Urol Esp. 2005;29:523–525. https://www.ncbi.nlm.nih.gov/pubmed/16013801[↩]