Contents
Achilles tendinitis
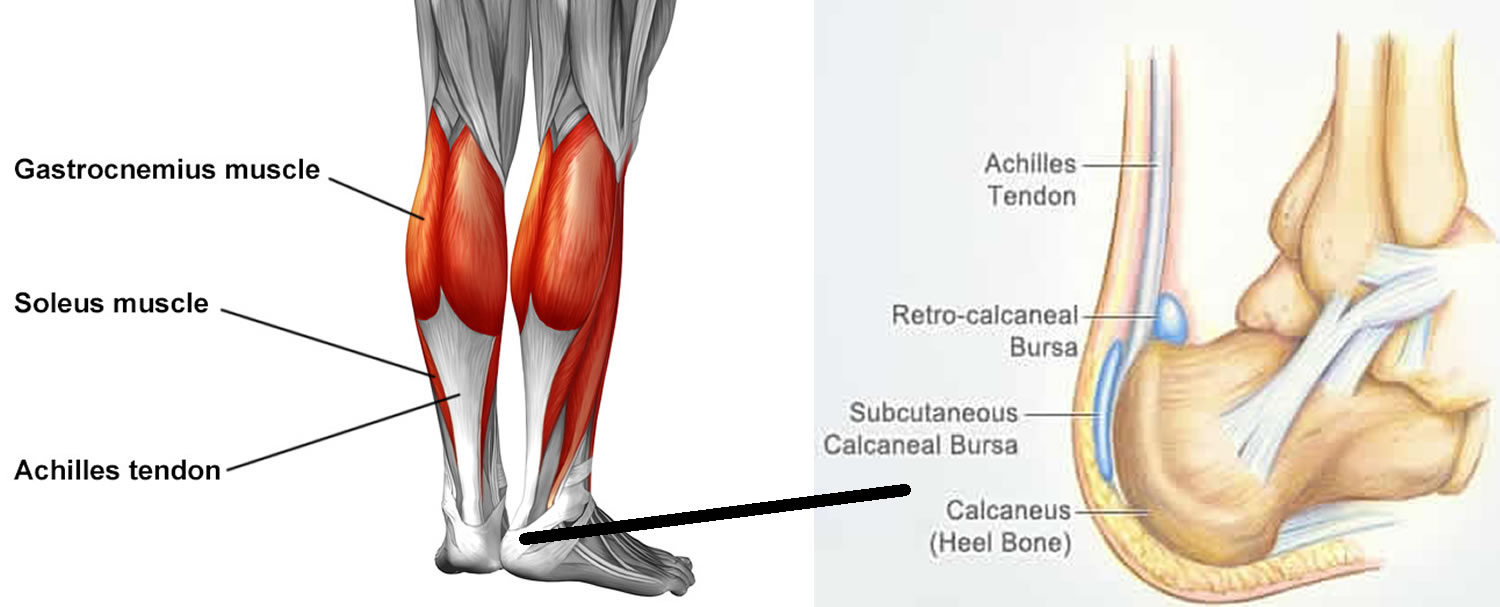
Achilles tendinitis also known as Achilles tendonitis or inflammation in the Achilles tendon, is an overuse injury of the Achilles tendon, the band of tissue that connects your calf muscles at the back of the lower leg to your heel bone. Achilles tendon is part of your calf muscles (gastrocnemius and soleus muscles) and attaches these muscles to your heel bone (the calcaneus) (Figure 1). When your calf muscles contract, your Achilles tendon pulls on your heel bone to bend your foot and ankle towards the ground – a movement called plantar flexion. The Achilles tendon is used when you walk, run, jump or push up on your toes. The injury to the Achilles tendon causes an inflammatory response and presence of inflammatory cells. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It’s common for runners to overdo it. In fact, up to 70% of runners develop injuries each year. They most often occur because of a training error. You may run too far, too fast, or too soon after an injury. Achilles tendinitis is also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends.
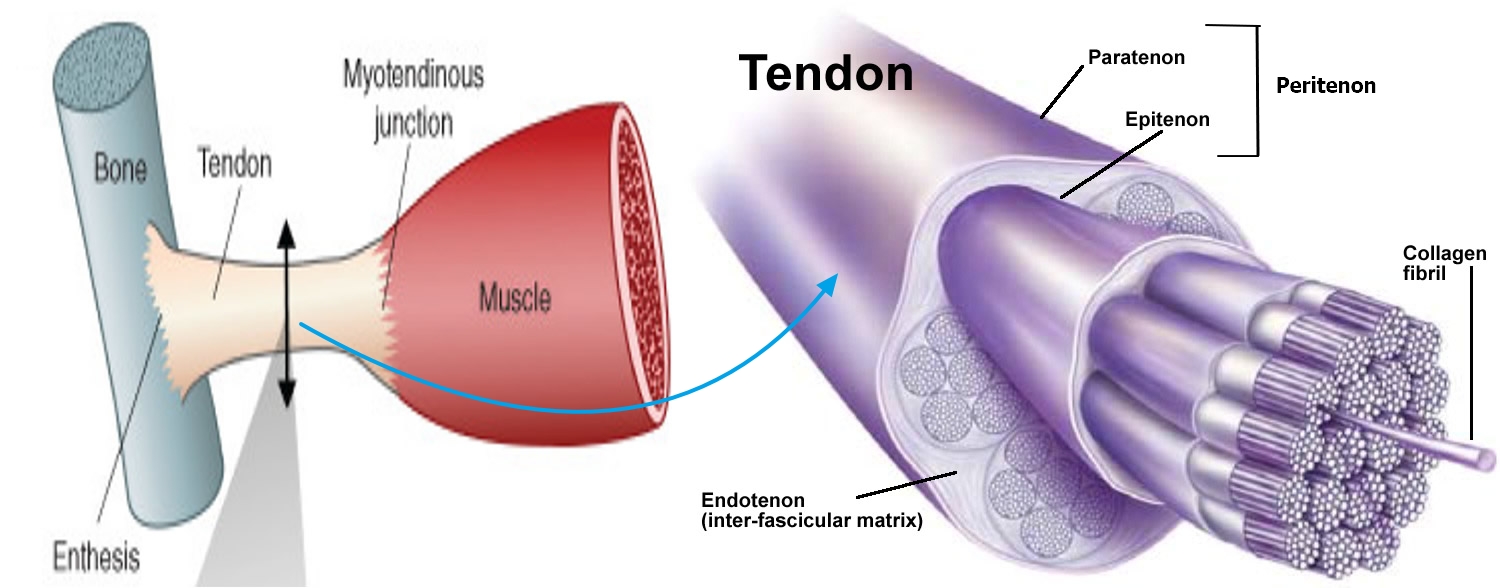
Tendons are biologically complex structures composed of multiple layers of tightly packed collagen fibers that are produced by tenocytes and tenoblasts (Figure 2) 1. Tenocytes are mechano-receptive cells that are able to change their gene expression in response to demand 2. Tendons’ unique combination of strength, flexibility, and elasticity allows them to carry loads and maintain tensile strength for long periods of time. Because they have a lower rate of oxygen consumption than skeletal muscle, they are also slow to heal. Tendons receive their blood supply from a variety of sources and pathology usually occurs in the hypovascular or watershed areas between two sources of blood supply 3. Appropriate loads on a tendon are anabolic (promoting growth), but overloading a tendon can be catabolic (promoting break down) and catastrophic. Disrupting the homeostasis between tendon stress and repair damages the tendon 4.
The Achilles tendon has two tendinous portions; one proximally and then another merging gradually distally, resulting in a single, homogenous tendon (see Figure 2 below). The Achilles tendon comprises three muscular heads; the soleus is monoarticular and the plantaris and gastrocnemius, which are biarticular. There are two sites where the mechanical tension of the Achilles tendon occurs, the medial/central portion of the paratenon and the middle part of the tendon which is the most common site of injury 5.
Achilles tendonitis tends to be an acute (or quick-onset) condition lasting 6 weeks or less. Some practitioners view this diagnosis as the first in a continuum of tendon injuries that subsequently increase in severity. For most people, Achilles tendinitis is short-lived and easily treated with rest and over-the-counter pain-relieving medications. Occasionally, the tendon becomes damaged by the inflammation, resulting in persistent pain or a tear (Achilles tendon rupture).
The pain associated with Achilles tendinitis typically begins as a mild ache in the back of your leg or above your heel after running or other sports activity. Episodes of more-severe pain may occur after prolonged running, stair climbing or sprinting. You might also experience tenderness or stiffness, especially in the morning, which usually improves with mild activity.
If you experience persistent pain around the Achilles tendon, see your doctor. Seek immediate medical attention if the pain or disability is severe. You may have a torn (ruptured) Achilles tendon.
Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor’s supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Figure 1. Achilles tendon
Footnote: The Achilles tendon connects the plantaris, gastrocnemius, and soleus to the calcaneus bone.
Figure 2. Histology of a normal tendon
Footnote: Tendon organization. Tendon links muscle to bone and is attached at one end to muscle by the myotendinous junction and at the other end to bone by the enthesis. Tendon is mainly composed of type 1 collagen fibers and of very few cells. Type 1 collagen displays a specific spatial organization parallel to the tendon axis. Type 1 collagen fibers are both very strong and very flexible. Tendon is formed of collagen fascicles, which are composed of collagen fibers, which are formed of collagen fibrils. The endotenon separates collagen fascicles. Tendon is surrounded by the tendon sheaths named the peritenon, which comprises paratenon and epitenon. The thin layer of connective tissue known as paratenon, is rich in elastin and supplies a significant portion of the blood supply to the tendon. The paratenon penetrates into the tendon, keeping the collagen bundles together while allowing movement between them 6. Studies have shown an area of hypovascularity 2 to 6 cm proximal to calcaneal insertion; this is a common area of injury. Paratenonitis is an inflammation of the outer layers of the tendon and encompasses conditions such as tenosynovitis and tenovaginitis 7. This pathology generates swelling and exudate with inflammatory cells, followed by a fibrinous exudate that causes crepitus and limitation of the tendinous course within the sheath. It can become chronic by developing an immature connective tissue that expands an organized fibrin network known as adhesions 8.
Figure 3. Achilles tendinitis
If you experience pain around your Achilles tendon that worsens with activity, see your doctor for an evaluation and to discuss treatment options.
See your doctor if you experience persistent pain near the back of your heel in the area of your Achilles tendon, and especially if the pain doesn’t markedly improve within one to two weeks despite self-care measures. See your doctor immediately if you experience signs or symptoms of an Achilles tendon rupture.
Achilles tendinitis types
There are two types of Achilles tendinitis:
Insertional Achilles tendinopathy
- Pain at the bottom of the Achilles tendon (where it connects into the heel bone)
- Caused by compressive forces of the tendon on the heel bone when the ankle is dorsiflexed (foot flexed upwards)
Mid-portion Achilles tendinopathy
- Pain 2-6 cm up from the bottom of the Achilles tendon
- Usually caused by overuse of the tendon
Achilles tendonitis symptoms
The signs and symptoms of Achilles tendinitis often develop gradually.
The signs and symptoms of Achilles tendinitis may include:
- Dull ache or pain when pushing off your foot during walking or when rising on your toes
- Tenderness over your Achilles tendon
- Stiffness that lessens as your tendon warms up
- Mild swelling or a “bump” on your tendon
- A crackling or creaking sound when you touch or move your Achilles tendon
The pain associated with Achilles tendinitis typically begins as a mild ache in the back of your leg or above your heel after running or other sports activity. Episodes of more-severe pain may occur after prolonged running, stair climbing or sprinting. You might also experience tenderness or stiffness, especially when you get up in the morning or after you’ve rested, which usually improves with mild activity and then worsens again when you increase your activity level.
If you have sudden pain and swelling near your heel and are unable to bend your foot downward or walk normally, you may have ruptured your Achilles tendon (Achilles tendon rupture). If you’ve ruptured the tendon completely, you won’t be able to rise on your toes on the injured leg. You may feel as if you’ve been kicked in the back of your ankle. See your doctor immediately if you suspect you have an Achilles tendon rupture.
Achilles tendinitis complications
Achilles tendinitis can progress to a degenerative condition called Achilles tendinosis. In this condition, the tendon begins to lose its organized structure, becoming weaker and more scarred. Continued stress to your Achilles tendon could cause it to tear (rupture) — a painful injury that usually requires surgical repair to correct the damage.
Achilles tendonitis causes
When you place a large amount of stress on your Achilles tendon too quickly, it can become inflamed from tiny tears that occur during the activity. A sudden increase in a repetitive activity that involves the Achilles tendon can be to blame. A number of other factors can cause Achilles tendinitis, include the following 9:
- Intrinsic factors: This includes:
- Flattened arch. Flattening of the arch of your foot (excessive pronation) can place you at increased risk of developing Achilles tendinitis. This is because of the extra stress placed on you Achilles tendon when walking. If you have excessive pronation, be sure to wear shoes with appropriate support to avoid further aggravating your Achilles tendon.
- Age,
- Sex,
- Metabolic dysfunction 10,
- Foot cavity,
- Dysmetria – a lack of coordination that occurs when the cerebellum isn’t functioning correctly ,
- Muscle weakness,
- Imbalance,
- Gastrocnemius dysfunction 11,
- Anatomical variation of the plantaris muscle 12,
- Tendon vascularization 13,
- Torsion of the Achilles tendons 14,
- Slippage of the fascicle 15 and
- Lateral instability of the ankle.
- Extrinsic factors: These include:
- Mechanical overload,
- Improper conditioning. Achilles tendinitis is most common among athletes whose bodies aren’t properly conditioned for their sport or activity. Inadequate flexibility and strength of the calf muscles can contribute to overload of the tendon. Frequent stops and starts during the activity, as well as activities that require repeated jumping — such as basketball or tennis — also can increase your risk of Achilles tendinitis.
- Too much, too soon. Achilles tendinitis resulting from overuse can occur when you begin a new exercise regimen. If you’re just beginning a new exercise program, be sure to stretch before and after exercising, and start slowly, increasing your activity over time. Don’t push yourself too quickly. If you’re a runner, excessive hill running can contribute to Achilles tendinitis.
- Inadequate equipment 16,
- Obesity 17,
- Medications (corticosteroids, anabolic steroids, fluoroquinolones,) 18, 19,
- Improper footwear,
- Insufficient warming or stretching 20,
- Hard training surfaces, and
- Direct trauma or infection. In some cases, inflammation of the Achilles tendon is due to trauma or infection near the tendon 21.
Achilles tendinitis is caused by repetitive or intense strain on the Achilles tendon, the band of tissue that connects your calf muscles to your heel bone. The Achilles tendon is used when you walk, run, jump or push up on your toes.
The structure of the Achilles tendon weakens with age, which can make it more susceptible to injury — particularly in people who may participate in sports only on the weekends or who have suddenly increased the intensity of their running programs.
Factors related to a high risk of rupture of the Achilles tendon link to advanced age due to a lack of uniformity of the tendons, slippage of the fascicles, and excessive exercise in athletes 22.
The Achilles tendon has a cumulative lifetime injury incidence of approximately 24% in athletes 9. Running-related injuries have a prevalence between 11% and 85% or 2.5 to 59 injuries per 1000 hours of running 23. Results from one study cite the frequency of Achilles tendinopathy to be 1 to 2% in elite adolescent athletes 24. Another study cited the frequency of injury as 9% in recreational runners 25. The lifetime injury incidence of 2.35 per 1000 is strongly associated with sporting activities 26. This incidence increases in older men 27. The overall incidence rate of Achilles tendinopathy ruptures is 2.1 per 100,000 person-years, and most Achilles tendon ruptures occur in males, with a 3.5 to 1 male to female ratio 28.
Achilles tendinitis risk factors
A number of factors may increase your risk of Achilles tendinitis, including:
- Your sex. Achilles tendinitis occurs most commonly in men.
- Age. Achilles tendinitis is more common as you age.
- Poor shoes – shoes that put excessive strain on the ligament can accelerate the inflammatory process.
- Physical problems. A naturally flat arch in your foot can put more strain on the Achilles tendon. Obesity and tight calf muscles also can increase tendon strain.
- Training choices. Running in worn-out shoes can increase your risk of Achilles tendinitis. Tendon pain occurs more frequently in cold weather than in warm weather, and running on hilly terrain also can predispose you to Achilles injury.
- Foot deformity – people with deformities of the feet, like flatfoot deformity, are more likely to develop Achilles tendinitis.
- Medical conditions. People who have psoriasis or high blood pressure are at higher risk of developing Achilles tendinitis.
- Excess weight or obesity.
- Medications. Certain types of antibiotics, called fluoroquinolones, have been associated with higher rates of Achilles tendinitis.
Achilles tendinitis prevention
While it may not be possible to prevent Achilles tendinitis, you can take measures to reduce your risk:
- Increase your activity level gradually. If you’re just beginning an exercise regimen, start slowly and gradually increase the duration and intensity of the training. Start slow if you’re new to running. Alternate walking and running to ease into it.
- Don’t increase your running mileage by more than 10% per week.
- Don’t run more than 45 miles per week.
- Take it easy. Avoid activities that place excessive stress on your tendons, such as hill running. If you participate in a strenuous activity, warm up first by exercising at a slower pace. If you notice pain during a particular exercise, stop and rest.
- A change to another sport (swimming, weight training, rowing, cycling) to allow the tendon to rest.
- Choose your shoes carefully. The shoes you wear while exercising should provide adequate cushioning for your heel and should have a firm arch support to help reduce the tension in the Achilles tendon. Choose running shoes that provide enough cushioning for the heel strike. Replace your worn-out shoes. If your shoes are in good condition but don’t support your feet, try arch supports in both shoes.
- Change your running shoes every 500 miles. At this distance, shoes can no longer absorb the shock of running.
- Don’t run on slanted or uneven surfaces. The best running surface is soft, flat ground.
- Stretch daily. Take the time to stretch your calf muscles and Achilles tendon in the morning, before exercise and after exercise to maintain flexibility. This is especially important to avoid a recurrence of Achilles tendinitis.
- Strengthen your calf muscles. Strong calf muscles enable the calf and Achilles tendon to better handle the stresses they encounter with activity and exercise.
- Cross-train. Alternate high-impact activities, such as running and jumping, with low-impact activities, such as cycling and swimming.
- Don’t “run through pain.” Pain is a sign that something is wrong. You shouldn’t ignore it. If you have pain when you run, rest for 2 to 3 days and use ice. See your doctor if the pain continues for 1 week.
Achilles tendonitis diagnosis
In many cases, your doctor or physiotherapist can diagnose Achilles tendinitis just by listening to you and examining your feet. During your physical exam, your doctor will gently press on the affected area to determine the location of pain, tenderness or swelling. He or she will also evaluate your flexibility, alignment, range of motion and reflexes of your foot and ankle.
Your doctor may order one or more of the following imaging tests to assess your condition:
- X-rays. While X-rays can’t visualize soft tissues such as tendons, they may help rule out other conditions (e.g., bone tumors) that can cause similar symptoms 29. Also, x-rays may detect calcifications in the proximal extension of the tendon insertion or bony prominences in the upper portion of the calcaneus.
- Ultrasound. This device uses sound waves to visualize soft tissues like tendons. Ultrasound can also produce real-time images of the Achilles tendon in motion, and color-Doppler ultrasound can evaluate blood flow around the tendon. Ultrasound may reveal increased thickness of the Achilles tendon with hyperemia associated with hypervascularity, a decrease in the gastrocnemius-soleus rotation angle and a decrease in the length of the Kager fat pad. Ultrasound is also useful during interventional treatment 30.
- Magnetic resonance imaging (MRI). Using radio waves and a very strong magnet, MRI machines can produce very detailed images of the Achilles tendon.
Achilles tendonitis treatment
Management of Achilles tendinopathy can divide into conservative and surgical. Achilles tendinitis usually responds well to self-care measures. But if your signs and symptoms are severe or persistent, your doctor might suggest other treatment options.
Self-care measures include the following steps, often known by the acronym R.I.C.E.:
- Rest. You may need to avoid exercise for several days or switch to an activity that doesn’t strain your Achilles tendon, such as swimming or cycling. In severe cases, you may need to wear a walking boot and use crutches.
- Ice. To decrease pain or swelling, apply an ice pack to the tendon for about 15 minutes after exercising or when you experience pain. Ice packs, ice massage or ice water slush baths all can help. For an ice massage, freeze a plastic foam cup full of water so that you can hold the cup while applying the ice directly to the skin.
- Compression. Wraps or compressive elastic bandages can help reduce swelling and reduce movement of the tendon.
- Elevation. Raise the affected foot above the level of your heart to reduce swelling. Sleep with your affected foot elevated at night.
Although rest is a key part of treating tendinitis, prolonged inactivity can cause stiffness in your joints. Move the injured ankle through its full range of motion and perform gentle Achilles tendon stretches to maintain joint flexibility.
Anti-inflammatory medications
If over-the-counter pain nonsteroidal anti-inflammatory drugs (NSAIDs) — such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve) — aren’t enough, your doctor might prescribe stronger medications to reduce inflammation and relieve pain.
Be sure to talk to your doctor if you feel you need nonsteroidal anti-inflammatory drugs (NSAIDs) for an extended time because some of these drugs should be used for only short periods — around seven to 10 days — to avoid complications.
If you take NSAIDs frequently or take more than the recommended dose, these medications can cause stomach pain, stomach bleeding and ulcers. Rarely, prolonged use can disrupt normal kidney function. If you have liver problems, talk to your doctor before using products containing paracetamol.
Physical therapy
A physical therapist might suggest some of the following treatment options:
- Exercises. Therapists often prescribe specific stretching and strengthening exercises to promote healing and strengthening of the Achilles tendon and its supporting structures.
- A special type of strengthening called “eccentric” strengthening, involving a slow let down of a weight after raising it, has been found to be especially helpful for persistent Achilles problems 31. There is evidence to support the use of eccentric exercises by providing short-term benefits over brace for persistent Achilles tendinopathy 32.
- Orthotic devices. A temporary shoe insert (orthotic device) or wedge that elevates your heel within your shoe may relieve strain on the stretched tendon and provide a cushion that lessens the amount of force exerted on your Achilles tendon. Your specialist might also prescribe special heel pads or cups to wear in your shoes to cushion and support your heel, or a splint to wear at night that will keep the Achilles tendon stretched while you sleep.
- Boot and crutches. In severe cases, a walking boot or gait aid (e.g., crutch) may be prescribed to allow the tendon to heal.
Achilles tendinitis stretching
Here are some stretching exercises to try:
Calf stretch
Stand with your hands against a wall and your right leg behind your left leg. Keep your right leg straight, heel flat on the floor, and foot pointed straight ahead. Bend your left leg, making sure your knees are over your toes, and lean forward. You should feel the stretch in the middle of your calf. Hold the stretch for 10 to 15 seconds. Repeat and switch legs. This exercise may be helpful for:
- Achilles tendinitis: Inflammation of the Achilles tendon, the large tendon at the back of the ankle.
- Plantar fasciitis: Heel pain.
- Calcaneal apophysitis: Inflammation where the Achilles tendon attaches to the heel. This is more common in children.
Plantar fascia stretch
Stand straight with your hands against a wall and your right leg slightly behind your other leg. Keep your heels flat on the floor. Bend both knees, making sure your knees are over your toes. You should feel the stretch in your heel, arch, and lower part of your leg. Hold the stretch for 10 to 15 seconds. Repeat and switch legs. This exercise may be helpful for plantar fasciitis, calcaneal apophysitis, and Achilles tendinitis.
Hamstring stretch
Sit with your right leg straight in front of you and your left leg bent to the side. With your back straight and your head up, lean forward at your waist. Try to touch your toes. You should feel the stretch along the underside of your thigh. Hold the stretch for 10 to 15 seconds. Repeat and switch legs.
Quadriceps stretch
Stand straight on both legs. Bend your right leg behind you and take hold of your foot. Pull your right heel toward your buttocks. You should feel the stretch in the front of your thigh. Hold the stretch for 10 to 15 seconds. Repeat and switch legs.
Surgery
If several months of conservative treatments (e.g., physiotherapy, medications and change in your exercise program) don’t work or if the Achilles tendon has torn, your doctor may suggest surgery to repair your Achilles tendon. Surgical therapy is optional for 10 to 30% of patients who fail conservative therapy after six months 33.
Surgical options include:
- Debridement – trimming away any significantly damaged areas of the tendon. This is the most commonly used surgical option and often yields very good results. If significant portions of the tendon are damaged, a tendon graft may be needed in conjunction with the debridement.
- Removal of bursa
- Osteotomy (bone reshaping)
The success rate is higher than 70%, but reports show complication rates of 3 to 40% 34. The Achilles tendon should undergo reattachment with a tendon rupture of more than 50% 35.
Surgery complications
In a systematic review, Lohrer and colleagues 36, concluded that the open and minimally invasive surgical treatment success rates did not differ (83.4%) and that there were no differences in patient satisfaction, but complication rates were lower for the minimally invasive procedures. Baltes and his colleagues classified the complications as follows 37:
- Major complications: Such as ruptured Achilles tendon, any reoperation, deep vein thrombosis, reflex dystrophy, persistent neuralgia, deep infections, major wound problems
- Minor complications Such as discomfort. Infections superficial, minor wound problems, scar sensitivity, hypertrophy, mild paraesthesia, prolonged hospitalization.
In another review, the surgical results were excellent or good in 89.6% of the cases and fair or poor in 10.4% 38. The average complication rate was 18.3%, with 15.7% minor complications and 2.6% major complications for surgical treatment of the Achilles tendinopathy insertion 38.
Achilles tendonitis prognosis
Achilles tendinopathy has a better prognosis with early and adequate initial management. Surgical intervention for Achilles tendinosis of insertion is successful in over 80% of cases. Stenson and his colleagues 39, discovered that as the number of risk factors increased, the possibility of failure in non-operative treatment also increased. With the usage of the visual analog scale (VAS), limited range of motion of the ankle, prior injection of corticosteroids, and the presence of enthesophytes of the Achilles tendon, the probability of failure of the conservative treatment was 55%. Therefore, usage of the risk factors mentioned above can help the surgeon in the decision to perform surgery in the appropriate clinical setting. In a retrospective study of Sanalla and colleagues 40, they found that strengthening of the Achilles tendon with bone-tendon autograft was an effective procedure with a low risk of complications and reliable results.
- Sakabe T, Sakai T. Musculoskeletal diseases—tendon. Br Med Bull. 2011;99:211–225.[↩]
- Maffulli N, Longo UG. How do eccentric exercises work in tendinopathy? Rheumatology (Oxford). 2008;47(10):1444–1445.[↩]
- Childress MA, Beutler A. Management of chronic tendon injuries. Am Fam Physician. 2013;87(7):486–490.[↩]
- Wang JH, Guo Q, Li B. Tendon biomechanics and mechanobiology—a minireview of basic concepts and recent advancements. J Hand Ther. 2012;25(2):133–140.[↩]
- Li, H. Y., & Hua, Y. H. (2016). Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. BioMed research international, 2016, 6492597. https://doi.org/10.1155/2016/6492597[↩]
- Kvist M, Józsa L, Järvinen MJ, Kvist H. Chronic Achilles paratenonitis in athletes: a histological and histochemical study. Pathology. 1987 Jan;19(1):1-11. doi: 10.3109/00313028709065127[↩]
- Feilmeier M. Noninsertional Achilles Tendinopathy Pathologic Background and Clinical Examination. Clin Podiatr Med Surg. 2017 Apr;34(2):129-136. doi: 10.1016/j.cpm.2016.10.003[↩]
- DeCarbo WT, Bullock MJ. Midsubstance Tendinopathy, Surgical Management. Clin Podiatr Med Surg. 2017 Apr;34(2):175-193. doi: 10.1016/j.cpm.2016.10.006[↩]
- Medina Pabón MA, Naqvi U. Achilles Tendonitis. [Updated 2021 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538149[↩][↩]
- Abate M, Salini V. Mid-portion Achilles tendinopathy in runners with metabolic disorders. Eur J Orthop Surg Traumatol. 2019 Apr;29(3):697-703. doi: 10.1007/s00590-018-2336-2[↩]
- Zhao, H., Ren, Y., Roth, E. J., Harvey, R. L., & Zhang, L. Q. (2015). Concurrent deficits of soleus and gastrocnemius muscle fascicles and Achilles tendon post stroke. Journal of applied physiology (Bethesda, Md. : 1985), 118(7), 863–871. https://doi.org/10.1152/japplphysiol.00226.2014[↩]
- Olewnik, Ł., Wysiadecki, G., Podgórski, M., Polguj, M., & Topol, M. (2018). The Plantaris Muscle Tendon and Its Relationship with the Achilles Tendinopathy. BioMed research international, 2018, 9623579. https://doi.org/10.1155/2018/9623579[↩]
- Yang X, Coleman DP, Pugh ND, Nokes LD. The volume of the neovascularity and its clinical implications in achilles tendinopathy. Ultrasound Med Biol. 2012 Nov;38(11):1887-95. doi: 10.1016/j.ultrasmedbio.2012.07.002[↩]
- Slane, L. C., Dandois, F., Bogaerts, S., Vandenneucker, H., & Scheys, L. (2018). Non-uniformity in the healthy patellar tendon is greater in males and similar in different age groups. Journal of biomechanics, 80, 16–22. https://doi.org/10.1016/j.jbiomech.2018.08.021[↩]
- Pękala PA, Henry BM, Ochała A, Kopacz P, Tatoń G, Młyniec A, Walocha JA, Tomaszewski KA. The twisted structure of the Achilles tendon unraveled: A detailed quantitative and qualitative anatomical investigation. Scand J Med Sci Sports. 2017 Dec;27(12):1705-1715. doi: 10.1111/sms.12835. Epub 2017 Jan 30. Erratum in: Scand J Med Sci Sports. 2019 Nov;29(11):1842.[↩]
- Federer AE, Steele JR, Dekker TJ, Liles JL, Adams SB. Tendonitis and Tendinopathy: What Are They and How Do They Evolve? Foot Ankle Clin. 2017 Dec;22(4):665-676. doi: 10.1016/j.fcl.2017.07.002[↩]
- Moon JL, Moon KM, Carlisle DM. Obesity-Related Foot Pain: Diagnosis and Surgical Planning. Clin Podiatr Med Surg. 2019 Jan;36(1):141-151. doi: 10.1016/j.cpm.2018.08.008[↩]
- Bolon B. Mini-Review: Toxic Tendinopathy. Toxicol Pathol. 2017 Oct;45(7):834-837. doi: 10.1177/0192623317711614[↩]
- Alušík Š, Paluch Z. Poškození šlach vyvolané léky [Drug induced tendon injury]. Vnitr Lek. 2018 Winter;63(12):967-971. Czech[↩]
- Camargo, P. R., Alburquerque-Sendín, F., & Salvini, T. F. (2014). Eccentric training as a new approach for rotator cuff tendinopathy: Review and perspectives. World journal of orthopedics, 5(5), 634–644. https://doi.org/10.5312/wjo.v5.i5.634[↩]
- Godoy-Santos AL, Bruschini H, Cury J, Srougi M, de Cesar-Netto C, Fonseca LF, Maffulli N. Fluoroquinolones and the Risk of Achilles Tendon Disorders: Update on a Neglected Complication. Urology. 2018 Mar;113:20-25. doi: 10.1016/j.urology.2017.10.017[↩]
- Almekinders LC, Engle CR. Common and Uncommon Injuries in Ultra-endurance Sports. Sports Med Arthrosc Rev. 2019 Mar;27(1):25-30. doi: 10.1097/JSA.0000000000000217[↩]
- Colbert LH, Hootman JM, Macera CA. Physical activity-related injuries in walkers and runners in the aerobics center longitudinal study. Clin J Sport Med. 2000 Oct;10(4):259-63. doi: 10.1097/00042752-200010000-00006[↩]
- Cassel M, Risch L, Intziegianni K, Mueller J, Stoll J, Brecht P, Mayer F. Incidence of Achilles and Patellar Tendinopathy in Adolescent Elite Athletes. Int J Sports Med. 2018 Sep;39(9):726-732. doi: 10.1055/a-0633-9098[↩]
- Mulvad, B., Nielsen, R. O., Lind, M., & Ramskov, D. (2018). Diagnoses and time to recovery among injured recreational runners in the RUN CLEVER trial. PloS one, 13(10), e0204742. https://doi.org/10.1371/journal.pone.0204742[↩]
- Molyneux, P., Carroll, M., Stewart, S., Brenton-Rule, A., & Rome, K. (2017). Ultrasound characteristics of the mid-portion of the Achilles tendon in runners: a systematic review protocol. Systematic reviews, 6(1), 108. https://doi.org/10.1186/s13643-017-0501-z[↩]
- Wezenbeek E, De Clercq D, Mahieu N, Willems T, Witvrouw E. Activity-Induced Increase in Achilles Tendon Blood Flow Is Age and Sex Dependent. Am J Sports Med. 2018 Sep;46(11):2678-2686. doi: 10.1177/0363546518786259[↩]
- Lemme, N. J., Li, N. Y., DeFroda, S. F., Kleiner, J., & Owens, B. D. (2018). Epidemiology of Achilles Tendon Ruptures in the United States: Athletic and Nonathletic Injuries From 2012 to 2016. Orthopaedic journal of sports medicine, 6(11), 2325967118808238. https://doi.org/10.1177/2325967118808238[↩]
- Bulstra GH, van Rheenen TA, Scholtes VA. Can We Measure the Heel Bump? Radiographic Evaluation of Haglund’s Deformity. J Foot Ankle Surg. 2015 May-Jun;54(3):338-40. doi: 10.1053/j.jfas.2014.07.006[↩]
- Romero-Morales C, Martín-Llantino PJ, Calvo-Lobo C, Palomo-López P, López-López D, Pareja-Galeano H, Rodríguez-Sanz D. Comparison of the sonographic features of the Achilles Tendon complex in patients with and without achilles tendinopathy: A case-control study. Phys Ther Sport. 2019 Jan;35:122-126. doi: 10.1016/j.ptsp.2018.12.003[↩]
- McCormack, J. R., Underwood, F. B., Slaven, E. J., & Cappaert, T. A. (2016). Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy. Sports health, 8(3), 230–237. https://doi.org/10.1177/1941738116631498[↩]
- Woitzik E, Jacobs C, Wong JJ, Côté P, Shearer HM, Randhawa K, Sutton D, Southerst D, Varatharajan S, Brison RJ, Yu H, van der Velde G, Stern PJ, Taylor-Vaisey A, Stupar M, Mior S, Carroll LJ. The effectiveness of exercise on recovery and clinical outcomes of soft tissue injuries of the leg, ankle, and foot: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man Ther. 2015 Oct;20(5):633-45. doi: 10.1016/j.math.2015.03.012[↩]
- Hardy A, Rousseau R, Issa SP, Gerometta A, Pascal-Moussellard H, Granger B, Khiami F. Functional outcomes and return to sports after surgical treatment of insertional Achilles tendinopathy: Surgical approach tailored to the degree of tendon involvement. Orthop Traumatol Surg Res. 2018 Sep;104(5):719-723. doi: 10.1016/j.otsr.2018.05.003[↩]
- Aicale R, Tarantino D, Maffulli N. Surgery in Tendinopathies. Sports Med Arthrosc Rev. 2018 Dec;26(4):200-202. doi: 10.1097/JSA.0000000000000214[↩]
- Baumbach SF, Braunstein M, Mack MG, Maßen F, Böcker W, Polzer S, Polzer H. Ansatznahe Erkrankungen der Achillessehne : Differenzierte Diagnostik und Therapie [Insertional Achilles tendinopathy : Differentiated diagnostics and therapy]. Unfallchirurg. 2017 Dec;120(12):1044-1053. German. doi: 10.1007/s00113-017-0415-1[↩]
- Lohrer, H., David, S., & Nauck, T. (2016). Surgical treatment for achilles tendinopathy – a systematic review. BMC musculoskeletal disorders, 17, 207. https://doi.org/10.1186/s12891-016-1061-4[↩]
- Baltes, T., Zwiers, R., Wiegerinck, J. I., & van Dijk, C. N. (2017). Surgical treatment for midportion Achilles tendinopathy: a systematic review. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 25(6), 1817–1838. https://doi.org/10.1007/s00167-016-4062-9[↩]
- Traina F, Perna F, Ruffilli A, Mazzotti A, Meliconi R, Berti L, Faldini C. Surgical treatment of insertional Achilles tendinopathy: a systematic review. J Biol Regul Homeost Agents. 2016 Oct-Dec;30(4 Suppl 1):131-138.[↩][↩]
- Stenson JF, Reb CW, Daniel JN, Saini SS, Albana MF. Predicting Failure of Nonoperative Treatment for Insertional Achilles Tendinosis. Foot Ankle Spec. 2018 Jun;11(3):252-255. doi: 10.1177/1938640017729497[↩]
- Sanalla H, Hart R, Komzák M, Paša L. Augmentace BT štěpem z m. quadriceps femoris při řešení úponové tendinopatie Achillovy šlachy [Surgical Treatment of the Achilles Insertional Tendinopathy Using the Augmentation with the BT Graft from M. Quadriceps Femoris]. Acta Chir Orthop Traumatol Cech. 2018;85(4):266-270. Czech.[↩]