Contents
What is amputation
Amputation is the surgical removal of part of the body, such as an arm, hand, leg or foot. Every care should be taken to assure that the amputation is done only when clinically indicated. Amputation should only be considered if the limb is non-viable (gangrenous or grossly ischemic, dangerous, malignancy or infection), or non-functional 1.
Amputation is always a last resort and it will not be done unless it is absolutely necessary for a person’s health.
Unless you need to have an emergency amputation also called guillotine amputation, you’ll be fully assessed before surgery to identify the most suitable type of amputation and any factors that may affect your rehabilitation.
The assessment is likely to include:
- a thorough medical examination – assessing your physical condition, nutritional status, bowel and bladder function, your cardiovascular system (heart, blood and blood vessels) and your respiratory system (lungs and airways)
- an assessment of the condition and function of your healthy limb – removing one limb can place extra strain on the remaining limb, so it’s important to look after the healthy limb
- a psychological assessment – to determine how well you’ll cope with the psychological and emotional impact of amputation, and whether you’ll need additional support
- an assessment of your home, work and social environments – to determine whether any additional provisions will need to be made to help you cope
You’ll also be introduced to a physiotherapist, who will be involved in your post-operative care. A prosthetist (a specialist in prosthetic limbs) will advise you about the type and function of prosthetic limbs or other devices available.
If you’re having a planned amputation, you might find it reassuring to talk to someone who’s had a similar type of amputation. A member of your care team may be able to put you in touch with someone.
Causes of amputation
Most amputations in the United State are done because the arteries in the legs have become blocked and there is not enough blood getting to the limb. This can be a complication of diabetes, high blood pressure, smoking or kidney failure.
Diabetes is the most common reason people need an amputation in the US. People living with diabetes are prone to having foot problems, often because of two complications of diabetes: nerve damage (neuropathy) and poor circulation. Diabetic neuropathy causes loss of feeling in your feet, taking away your ability to feel pain and discomfort, so you may not detect an injury or irritation. Poor circulation in your feet reduces your ability to heal, making it hard for even a tiny cut to resist infection. With diabetes, small foot problems can turn into serious complications. However, most of these amputations could be prevented. If you have diabetes, it is very important to look after your feet and control your blood sugar.
Diabetes-related foot & leg problems:
- Infections and ulcers (sores) that do not heal. An ulcer is a sore in the skin that may go all the way to the bone. Because of poor circulation and neuropathy in the feet, cuts or blisters can easily turn into ulcers that become infected and will not heal. This is a common—and serious—complication of diabetes and can lead to a loss of your foot, your leg or your life.
- Corns and calluses. When neuropathy is present, you cannot tell if your shoes are causing pressure and producing corns or calluses. Corns and calluses must be properly treated or they can develop into ulcers.
- Dry, cracked skin. Poor circulation and neuropathy can make your skin dry. This may seem harmless, but dry skin can result in cracks that may become sores and can lead to infection.
- Nail disorders. Ingrown toenails (which curve into the skin on the sides of the nail) and fungal infections can go unnoticed because of loss of feeling. If they are not properly treated, they can lead to infection.
- Hammertoes and bunions. Nerve damage affecting muscles can cause muscle weakness and loss of tone in the feet, resulting in hammertoes and bunions. If left untreated, these deformities can cause ulcers.
- Charcot foot. This is a complex foot deformity. It develops as a result of loss of sensation and an undetected broken bone that leads to destruction of the soft tissue of the foot. Because of neuropathy, the pain of the fracture goes unnoticed and the patient continues to walk on the broken bone, making it worse. This disabling complication is so severe that surgery, and occasionally amputation, may become necessary.
- Poor blood flow. In diabetes, the blood vessels below the knee often become narrow and restrict blood flow. This prevents wounds from healing and may cause tissue death.
You play a vital role in reducing diabetes complications. Follow these guidelines and contact your podiatrist or doctor if you notice any problems:
- Inspect your feet daily. If your eyesight is poor, have someone else do it for you. Inspect for:
- Skin or nail problems: Look for cuts, scrapes, redness, drainage, swelling, bad odor, rash, discoloration, loss of hair on toes, injuries or nail changes (deformed, striped, yellowed or discolored, thickened or not growing).
- Signs of fracture: If your foot is swollen, red or hot or has changed in size, shape or direction, see your foot and ankle surgeon immediately.
- Wash your feet daily. Wash your feet in lukewarm (not hot) water once a day. Dry them gently, especially between the toes. Use a pumice stone to gently rub the skin where calluses easily form. Sprinkle talcum powder or cornstarch between your toes to keep the skin dry. Use a moisturizing cream or lotion on the tops and bottoms of your feet to keep the skin soft. Preventing cracks in dry skin helps keep bacteria from getting in.
- Do not ignore leg pain. Pain in the leg that occurs at night or with a little activity could mean you have a blocked artery. Seek care immediately.
- Trim your toenails carefully. Trim your nails straight across. Carefully file sharp ends with an emery board. Ask for assistance from a caregiver if you are unable to trim your nails yourself. If you have any nail problems, hard nails or reduced feeling in your feet, your toenails should be properly trimmed.
- Never trim calluses or corns yourself, and do not use over-the-counter medicated pads. See your doctor or foot specialist (podiatrist) for removal of any of these lesions.
- Keep floors free of sharp objects. Make sure no needles, insulin syringes or other sharp objects are on the floor.
- Do not go barefoot. Wear shoes, indoors and outdoors.
- Wear clean, dry socks. Wear socks made of fibers that pull sweat away from your skin, such as cotton and special acrylic fibers — not nylon. Avoid socks with tight elastic bands that reduce circulation or socks with seams that could irritate your skin.
- Buy shoes that fit properly. Buy comfortable shoes that provide support and cushioning for the heel, arch and ball of the foot. Avoid tightfitting shoes and high heels or narrow shoes that crowd your toes. If one foot is bigger than the other, buy shoes in the larger size. Your doctor may recommend specially designed shoes (orthopedic shoes) that fit the exact shape of your feet, cushion your feet and evenly distribute weight on your feet.
- Check shoes and socks. Shake out your shoes before putting them on. Make sure your socks are not bunched up.
- Have your circulation and sense of feeling tested. Your foot and ankle surgeon will perform tests to see if you have lost any feeling or circulation.
- Don’t smoke. Smoking impairs circulation and reduces the amount of oxygen in your blood. These circulatory problems can result in more-severe wounds and poor healing. Talk to your doctor if you need help to quit smoking.
- Schedule regular foot checkups. Your doctor or podiatrist can inspect your feet for early signs of nerve damage, poor circulation or other foot problems. Schedule foot exams at least once a year or more often if recommended by your doctor.
Signs of trouble in diabetic foot
Contact your doctor if you have:
- Ingrown toenails
- Blisters
- Plantar warts on the soles of your feet (flesh colored bumps with dark specks)
- Athlete’s foot
- An open sore or bleeding
- Swelling
- Redness
- Warmth in one area
- Pain (though you may not feel anything if you have nerve damage)
- Discolored skin
- A foul odor
- An ulcer that lasts longer than one to two weeks
- An ulcer bigger than 3/4 inch (2 centimeters)
- A sore that doesn’t quickly begin to heal
- An ulcer so deep you can see the bone underneath
Your doctor will inspect your foot to make a diagnosis and prescribe the appropriate course of treatment.
An amputation may also be needed if the limb:
- you have a severe infection in your limb
- is affected by cancer
- your limb has been affected by gangrene (often as a result of peripheral arterial disease)
- there’s serious trauma to your limb, such as a crush or blast wound
- your limb is deformed and has limited movement and function
Amputations can be done as emergency (guillotine amputation) or elective (planned) surgery. Before planned amputations, you will meet with the surgeon to discuss which operation is best for you.
You will have a thorough medical examination and psychological assessment. Your healthy limb will be assessed since it will have to carry extra strain after the operation. You will also be advised on any adaptations you may need to make at home or work. Physiotherapy will be planned to help with your rehabilitation after the operation.
Assessment for amputation
A decision to amputate a limb should be made through discussion with the interdisciplinary team – including the patient – wherever possible; in an emergency situation, the decision should be made based on medical need. There are a number of different investigations that can be carried out to assess the need for an amputation; these examinations assess the bones and soft tissues to establish limb viability.
- X-ray – images of bones to view fractures or disease
- Computerised Tomography (CT) scan – detailed images of bone, tissue and blood vessels
- Angiogram – outlines blood vessels
- Doppler ultrasound – occlusion of blood vessels
- Venogram and arteriogram – detailed imaging of blood vessels
These investigations will help the surgeons to find out if the blood supply to the limb is intact. The lower limb is supplied by the popliteal artery which subdivides into the:
- Posterior tibial artery
- Anterior tibial artery
- Fibular artery
In vascular disease these arteries can become blocked or narrowed over time which reduces the circulation to the legs; this can cause pain, ulceration and blackened areas. If left untreated this can lead to gangrene or infection and an amputation is needed to avoid this becoming life threatening.
In trauma one or more of these blood vessels may be ruptured beyond repair due to the nature of the injuries sustained – e.g. in a car accident, gunshot wound or blast. In this situation an amputation is performed as the limb does not have any blood supply beyond the level of injury and is therefore deemed non-viable.
There are a number of injury severity scores that may be used in conjunction with clinical investigations to establish the likelihood of limb salvage. Examples of this include:
- Nerve Injury, Ischemia, Soft-Tissue Injury, Skeletal Injury, Shock, and Age of Patient Score (NISSA) 2
- Limb salvage index (LSI) 3
- Mangled Extremity Severity Score (MESS) 4
Once a decision has been made to remove part of a limb the level of amputation needs to be decided; this can have significant consequences so there are a number of factors to take into account when planning the surgery:
- Boundary of dead or diseased tissue – if the infection or disease is not completely eradicated the patient may need to undergo further operations or treatment so it is important that the amputation is done at a level where this can be achieved
- Suitability for prosthesis – if the patient is likely to be a candidate for prosthetic rehab the level of amputation needs to be carefully considered
- Mobility and function – it is useful to consider the patients’ pre-morbid level of mobility and function
- Cosmesis – length and shape of stump affect the aesthetic appearance
Amputation procedure
Amputations can be carried out under general anaesthetic (where you’re unconscious) or using an epidural anaesthetic (which numbs the lower half of the body but you are still awake).
Once the limb has been removed, a number of additional techniques can be used to help improve the function of the remaining limb and reduce the risk of complications.
These include shortening and smoothing the bone in your remaining limb so it’s covered by an adequate amount of soft tissue and muscle, and stitching the remaining muscle to the bones to help strengthen your remaining limb (a technique known as myodesis). In myodesis the muscle is secured to the bone by suturing the distal tendon via pre-drilled holes to the bone 5. Myodesis technique prevents deformity of the residual limb by preventing excessive shift of the muscle during contraction (when this happens it interferes with the muscle control in the prosthesis) 5. Myodesis can be performed on below knee- or above knee amputation.
After the amputation, your wound will be sealed with stitches or surgical staples. It will be covered with a bandage and a tube may be placed under your skin to drain away any excess fluid. The bandage will usually need to be kept in place for a few days to reduce the risk of infection.
Amputation recovery
After surgery, you’ll usually be given oxygen through a mask and fluids through a drip for the first few days while you recover on the ward.
A small flexible tube (a urinary catheter) may be placed in your bladder during surgery to drain away urine. This means you won’t need to worry about going to the toilet for the first few days after surgery.
The site of the operation may be painful, so you’ll be given painkillers if you need them. Tell a member of your care team if the painkillers aren’t working, as you may need a larger dose or a stronger painkiller. A small tube may be used to deliver local anaesthetic to the nerves in your stump to help reduce pain.
Your physiotherapist will teach you some exercises to help prevent blood clots and improve your blood supply while you’re recovering in hospital.
Compression garments
You’ll notice swelling (edema) of your stump after surgery. This is normal and it may continue after you’ve been discharged.
Using a compression garment will help with swelling and the shape of the stump. It may also reduce phantom pain and help support the limb.
You’ll be fitted with a compression garment once your wound has healed. It should be worn every day, but taken off at bedtime. You should be given at least two garments, which should be washed regularly.
Rehabilitation
Physical rehabilitation is an important part of the recovery process. It can be a long, difficult and frustrating process, but it’s important to persevere. After rehabilitation, you should be able to return to work and other activities.
Your rehabilitation programme will be tailored to your individual needs and requirements, and will aim to allow you to carry out as many of your normal activities as possible.
You’ll work closely with physiotherapists and occupational therapists who will discuss with you what you’d like to achieve from rehabilitation so that some realistic goals can be set.
Your rehabilitation programme will usually start within a few days of surgery, beginning with some simple exercises you can do while lying down or sitting. If you’ve had a leg amputation, you’ll be encouraged to move around as soon as possible using a wheelchair.
You’ll also be taught “transfer techniques” to help you move around more easily, such as how to get into a wheelchair from your bed.
Once your wound has started to heal, you may start working on an exercise programme with a physiotherapist in the hospital gym to help you maintain your mobility and muscle strength.
If you have a prosthetic limb fitted (see below), your physiotherapist will teach you how to use it – for example, how to walk on a prosthetic leg or grip with a prosthetic hand.
Going home and follow-up
The length of time it will take before you’re ready to go home will depend on the type of amputation you’ve had and your general state of health.
Before you’re discharged from hospital, an occupational therapist may arrange to visit you at home to see whether your home environment needs to be adapted to make it more accessible.
For example, you may need a wheelchair ramp or a stairlift. If these types of modifications are required, the issue can be referred to your local social services department. Read about mobility, wheelchairs and scooters and assessing your care and support needs.
It can take several months before you’re fitted with a prosthetic limb (if you’re a suitable for one), so you may be given a wheelchair to help you get around if you’ve had a lower limb amputation.
You’ll probably need to attend a follow-up appointment a few weeks after being discharged to discuss how well you’re coping at home and whether you require additional help, support or equipment.
At your appointment, you may also be given details of your nearest amputee support group, made up of both healthcare professionals and people living with an amputation.
Prosthetics
After an amputation, you may be able to have a prosthetic limb fitted.
Prosthetic limbs aren’t suitable for everyone who’s had an amputation because an extensive course of physiotherapy and rehabilitation is required (see below).
Adjusting to life with a prosthetic limb takes a considerable amount of energy because you have to compensate for the loss of muscle and bone in the amputated limb.
This is why frail people or those with a serious health condition, such as heart disease, may not be suitable for a prosthetic limb.
If you’re able to have a prosthetic limb, the type of limb that’s recommended for you will depend on:
- the type of amputation you had
- the amount of muscle strength in the remaining section of the limb
- your general state of health
- tasks the prosthetic limb will be expected to perform
- whether you want the limb to look as real as possible or whether you’re more concerned with function
If it’s thought that you would find it difficult to withstand the strain of using a prosthetic limb, a purely cosmetic limb may be recommended. This is a limb that looks like a real limb, but can’t be used.
It’s possible to have a prosthetic limb that’s both physically realistic and functional, but there may have to be an element of compromise between the two.
Preparing to have a prosthetic limb fitted
If a prosthetic limb is suitable for you, you’ll begin a programme of activities while still in hospital to prepare for the prosthetic.
Before a prosthetic limb is fitted, the skin covering your stump may be made less sensitive (known as desensitization). This will make the prosthetic more comfortable to wear.
Skin desensitization involves the following steps:
- gently tapping the skin with a face cloth
- using compression bandages to help reduce swelling and prevent a build-up of fluid inside and around your stump
- rubbing and pulling the skin around your bone to prevent excessive scarring
Your physiotherapist will teach you a range of exercises to strengthen the muscles in your remaining limb and improve your general energy levels, so you’re able to cope better with the demands of an artificial limb.
Depending on what’s available in your local area, it can be several months before you get your first appointment with a prosthetist (specialist in prosthetic limbs).
Stump care
It’s very important to keep the skin on the surface of your stump clean to reduce the risk of it becoming irritated or infected.
Gently wash your stump at least once a day (more frequently in hot weather) with mild unscented soap and warm water, and dry it carefully.
If you have a prosthetic limb, you should also regularly clean the socket using soap and warm water.
When taking a bath, avoid leaving your stump submerged in water for long periods because the water will soften the skin on your stump, making it more vulnerable to injury.
If your skin becomes dry, use a moisturizing cream before bedtime or when you’re not wearing your prosthesis.
Some people find wearing one or more socks around their stump helps absorb sweat and reduces skin irritation. The size of your stump may change as the swelling goes down, so the number of socks you need to use may vary. You should change the socks every day.
Check your stump carefully every day for signs of infection, such as:
- warm, red and tender skin
- discharge of fluid or pus
- increasing swelling
Contact your care team for advice if you think you may be developing a skin infection.
Caring for your remaining limb
After having a leg or foot amputated, it’s very important to avoid injuring your remaining “good” leg and foot, particularly if your amputation was needed because of diabetes. Your remaining leg and foot may also be at risk.
Avoid wearing poorly fitting footwear and ensure that an appropriately trained healthcare professional, such as a podiatrist, is involved in the care of your remaining foot. You should also be offered a regular review of your foot by the foot care team.
Amputation risks and complications
Like any type of surgery, an amputation carries a risk of complications. It also carries a risk of additional problems directly related to the loss of a limb.
There are a number of factors that influence the risk of complications from amputation, such as your age, the type of amputation you’ve had, and your general health.
The risk of serious complications is lower in planned amputations than in emergency amputations.
Complications associated with having an amputation include:
- heart complications – such as heart attack
- deep vein thrombosis (DVT)
- slow wound healing and wound infection
- pneumonia
- stump and “phantom limb” pain
In some cases, further surgery may be needed to correct problems that develop or to help relieve pain. For example, if neuromas (thickened nerve tissue) are thought to be causing pain, the affected cluster of nerves may need to be removed.
Stump and “phantom limb” pain
Many people who have an amputation experience some degree of stump pain or “phantom limb” pain.
Phantom limb sensations are sensations that seem to be coming from the amputated limb. Occasionally, these can be painful (phantom limb pain).
The term “phantom” doesn’t mean the painful symptoms are imaginary. Phantom limb pain is a real phenomenon, which has been confirmed using brain imaging scans to study how nerve signals are transmitted to the brain.
The symptoms of phantom limb pain can range from mild to severe. Some people have described brief “flashes” of mild pain, similar to an electric shock, that last for a few seconds. Others have described constant severe pain.
Stump pain can have many different causes, including rubbing or sores where the stump touches a prosthetic limb, nerve damage during surgery and the development of neuromas.
Treating stump and phantom limb pain
Stump and phantom limb pain will usually improve over time, but treatments are available to help relieve the symptoms.
Medications
Medications that may be used to help relieve pain include:
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen
- anticonvulsants – such as carbamazepine or gabapentin
- antidepressants – such as amitriptyline or nortriptyline (these medications work directly on the nerves in your leg)
- opioids – such as codeine or morphine
- corticosteroid or local anaesthetic injections
Self-help measures and complementary therapy
There are several non-invasive techniques that may help relieve pain in some people. They include:
- checking the fit of your prosthesis and making adjustments to make it feel more comfortable
- applying heat or cold to your limb, such as using heat or ice packs, rubs and creams
- massage – to increase circulation and stimulate muscles
- acupuncture – thought to stimulate the nervous system and relieve pain
- transcutaneous electrical nerve stimulation (TENS) – where a small, battery-operated device is used to deliver electrical impulses to the affected area of your body, to block or reduce pain signals
- mental imagery
Research has shown that people who spend 40 minutes a day imagining using their phantom limb, such as stretching out their “fingers” or bunching up their “toes”, experience a reduction in pain symptoms.
This may be related to the central theory of phantom limb pain (that the brain is looking to receive feedback from the amputated limb), and these mental exercises may provide an effective substitution for this missing feedback.
Another technique, known as mirror visual feedback, involves using a mirror to create a reflection of the other limb. Some people find that exercising and moving their other limb can help relieve the pain from a phantom limb.
Psychological impact of amputation
The loss of a limb can have a considerable psychological impact. Many people who’ve had an amputation report feeling emotions such as grief and bereavement, similar to experiencing the death of a loved one.
Coming to terms with the psychological impact of an amputation is therefore often as important as coping with the physical demands.
Having an amputation can have a considerable psychological impact for three main reasons:
- you have to cope with the loss of sensation from your amputated limb
- you have to cope with the loss of function from your amputated limb
- your sense of body image, and other people’s perception of your body image, has changed
Negative thoughts and emotions are common after an amputation. This is particularly true in people who’ve had an emergency amputation because they don’t have time to mentally prepare for the effects of surgery.
Common negative emotions and thoughts experienced by people after an amputation include:
- depression
- anxiety
- denial (refusing to accept that they need to make changes, such as having physiotherapy, to adapt to life with an amputation)
- grief
- feeling suicidal
People who’ve had an amputation as a result of trauma (particularly members of the armed forces) also have an increased risk of developing post-traumatic stress disorder (PTSD).
Talk to your care team about your thoughts and feelings, particularly if you’re feeling depressed or suicidal. You may need additional treatment, such as antidepressants or counseling, to improve your ability to cope after having an amputation.
Help and support
Being told you need to have a limb amputated can be a devastating and frightening experience. Adjusting to life after an amputation can be challenging, but many people enjoy a good quality of life once they have managed to adapt.
You may find it useful to contact a support group for people living with amputations.
Types of amputation
Sometimes only a toe or part of the foot is amputated (known as a minor amputation). Major amputations involve removing the foot, part of the leg – usually below or above the knee – or an entire arm.
The type of amputation a person might need usually depends on how well the wound is likely to heal. If the blood supply is very limited, it may not be possible for the tissues to heal even after a minor amputation, so a major amputation may be the best option.
Above knee amputation
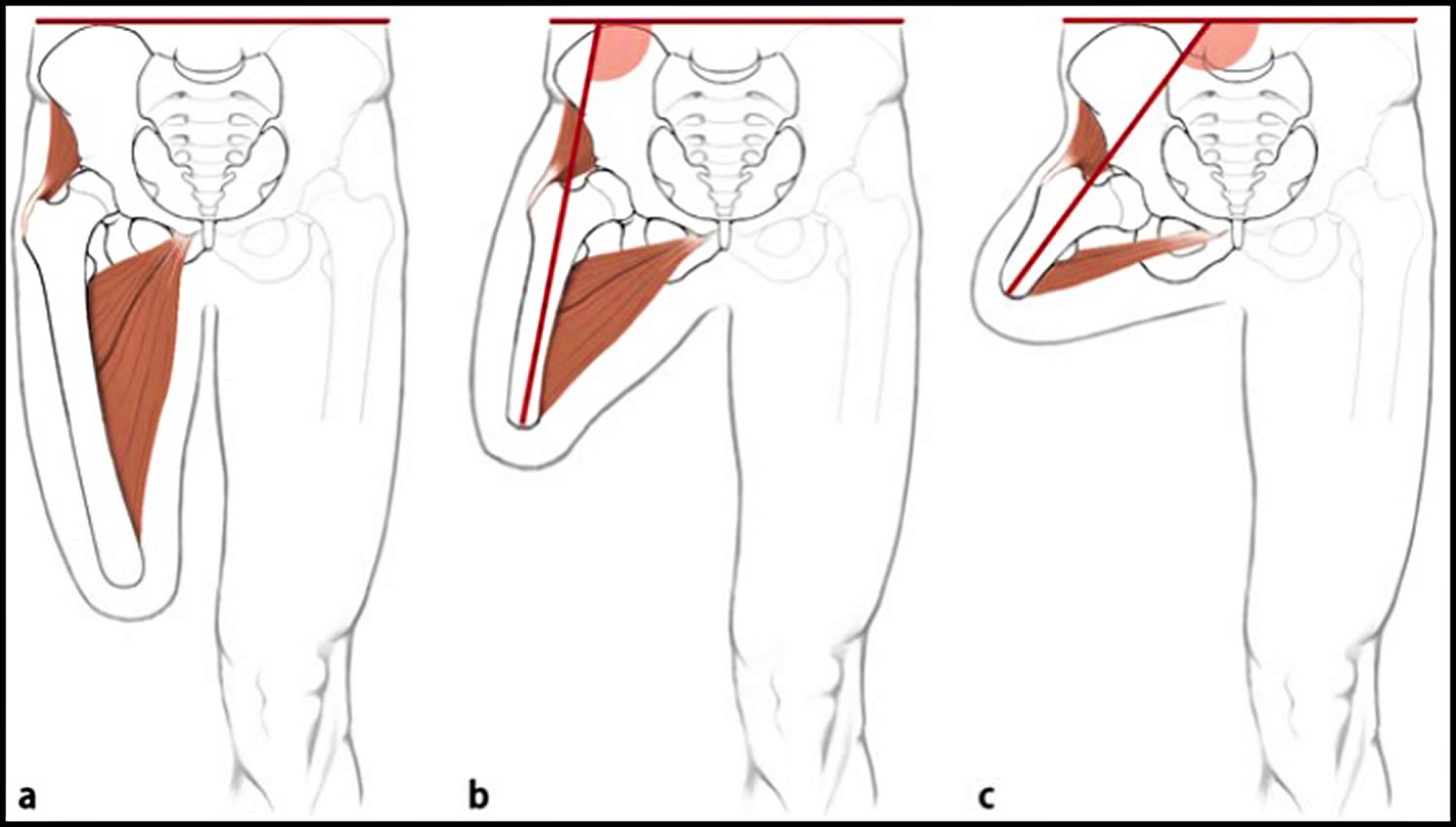
Above-knee amputation (AKA) is a transfemoral amputation (amputation done through the femur), measurements are taken and flap lines marked out. The surgeon dissects through the skin to then isolate and ligate the nerves and blood vessels. In order to minimise the risk of neuropathic pain (see complications) the nerves are dissected on tension so the end will retract back into the tissues where they can heal away from the stump end. The femur is dissected on its perpendicular axis using an oscillating saw.
The optimum length of residual bone is approximately 7.5-10cm proximal to the superior border of patella. Very short trans-femoral stumps often end up in abduction because there is an imbalance between the adductor and abductor muscles.
With a transfemoral amputation the distal attachments of the thigh muscles is lost, in order to preserve their function and length a myodesis may be performed to anchor the adductor (and sometimes hamstring) muscles to bone. The hamstrings and quadriceps may then be sutured together over the distal end of the femur – a technique called a myoplasty. Myoplasty is attaching sectioned muscles to opposing muscles 6. It is a myoplasty of the antagonist muscles to help pad the end of the stump to perform Gottchaltk myodesis (adductor magnus trans-osseously fixed and covering the distal femoral end).
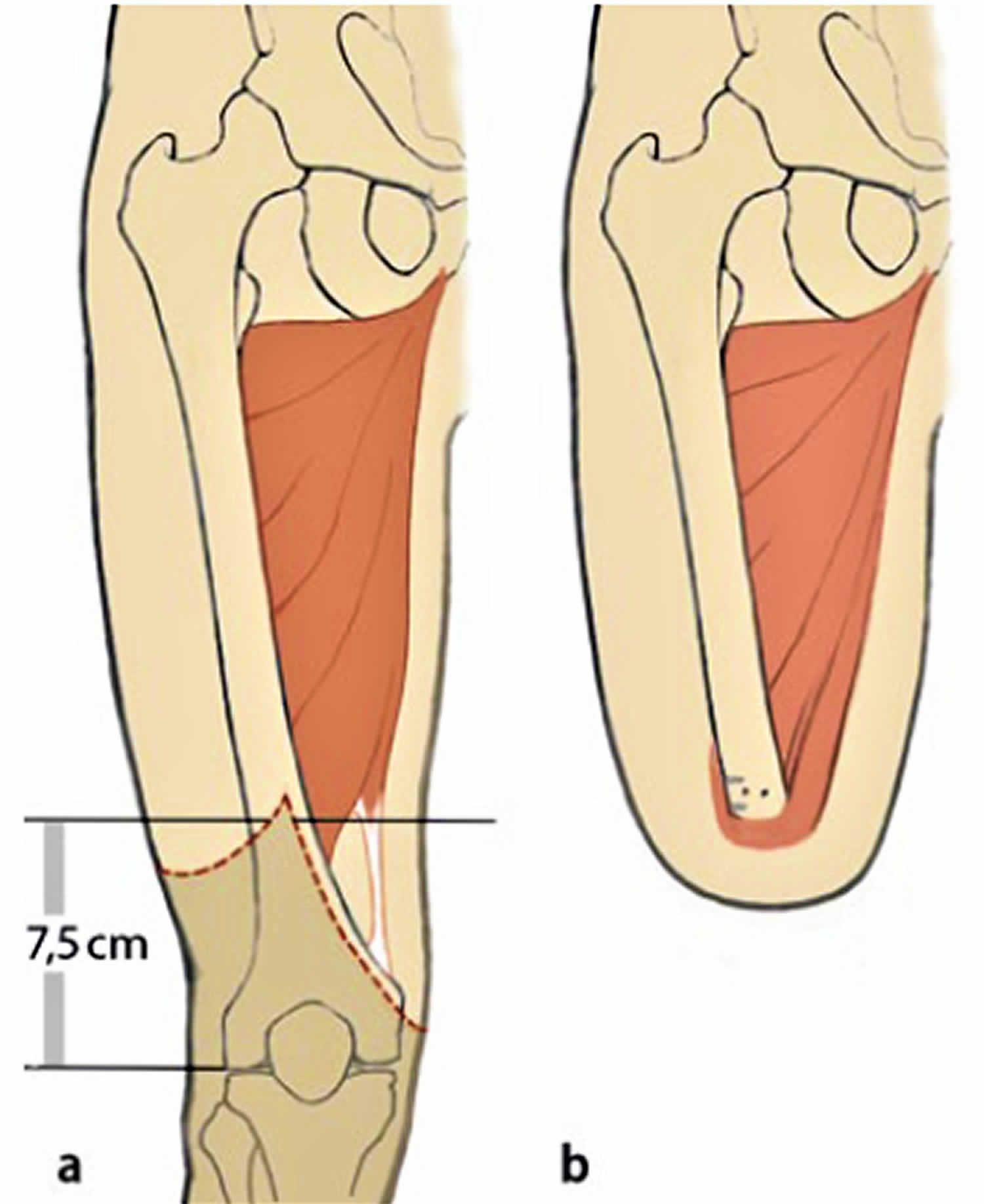
Figure 1. Above-knee amputation
Advantages and Disadvantages For Long stump (a)
- best lever
- better muscular balance while preserving the strength of the adductors
- energy efficient
- candidate for ischial tuberosity bearing prosthesis
Medium-length stump (b)
- reduced strength of the adductors
- increased flexion and abduction
- increased energy expenditure
Short stump (c)
- weak adductor muscles, causing severe imbalance
- the position of the stump often ends up in flexion and abduction
- causes massive energy expenditure (effort) and prosthesis can be heavy
Below knee amputation
A below-knee amputation (“BKA”) is a transtibial amputation that involves removing the foot, ankle joint, and distal tibia and fibula with related soft tissue structures 7.
Below-knee amputation advantages 5:
- Preservation of the knee joint leads to less energy expenditure and better proprioception than an above knee amputee
- Candidates for patella tendon bearing prosthesis
- Near normal level of function (more energy expenditure than a non-amputee)
- Decreased mortality rate and increases the likelihood for ambulation of the older person when compared to the above knee amputation population
Below-knee amputation disadvantages:
- At risk of knee flexion contractures (see Amputation risks and complications)
- May need ‘bone bridge’ surgery due to distal fibula pain (see Amputation risks and complications)
In general, a below-knee amputation is preferred over an above-knee amputation (AKA), because below-knee amputation (“BKA”) has better rehabilitation and functional outcomes 8. The rates of lower extremity amputation have declined in recent years, but still, 3,500 trauma-related amputations are performed in the United States each year 9. A below-knee amputation carries significant morbidity, yet it remains a treatment modality with vital clinical and often life-saving significance given appropriate indications 10.
The timely performance of a below-knee amputation can be both life-saving in severe illness or trauma, and restorative through improving function with an appropriate prosthesis 7. Many patients with severe non-healing foot ulcers, for instance, have difficulty ambulating and can regain function with the removal of the infected limb and fitting for a prosthesis. Similarly, patients with chronic pain from lower extremity trauma may undergo a below-knee amputation as a palliative or similarly functional measure, often with satisfactory results. It is important to note that, an individual’s metabolic demands with ambulation will rise significantly after a below-knee amputation, although this depends in part on the postoperative maintenance of lower extremity muscle strength 11. Hence, for the frail or elderly patient, this is a procedure which must be undertaken in conjunction with nutritional guidance and an overall discussion of patient health and mobility. Additionally, the long-term clinical survival of below-knee amputation patients is notably poor in certain populations; patients with end-stage diabetes mellitus who receive a below-knee amputation for foot ulcers have been shown to have an average postoperative life expectancy around 3 years 12.
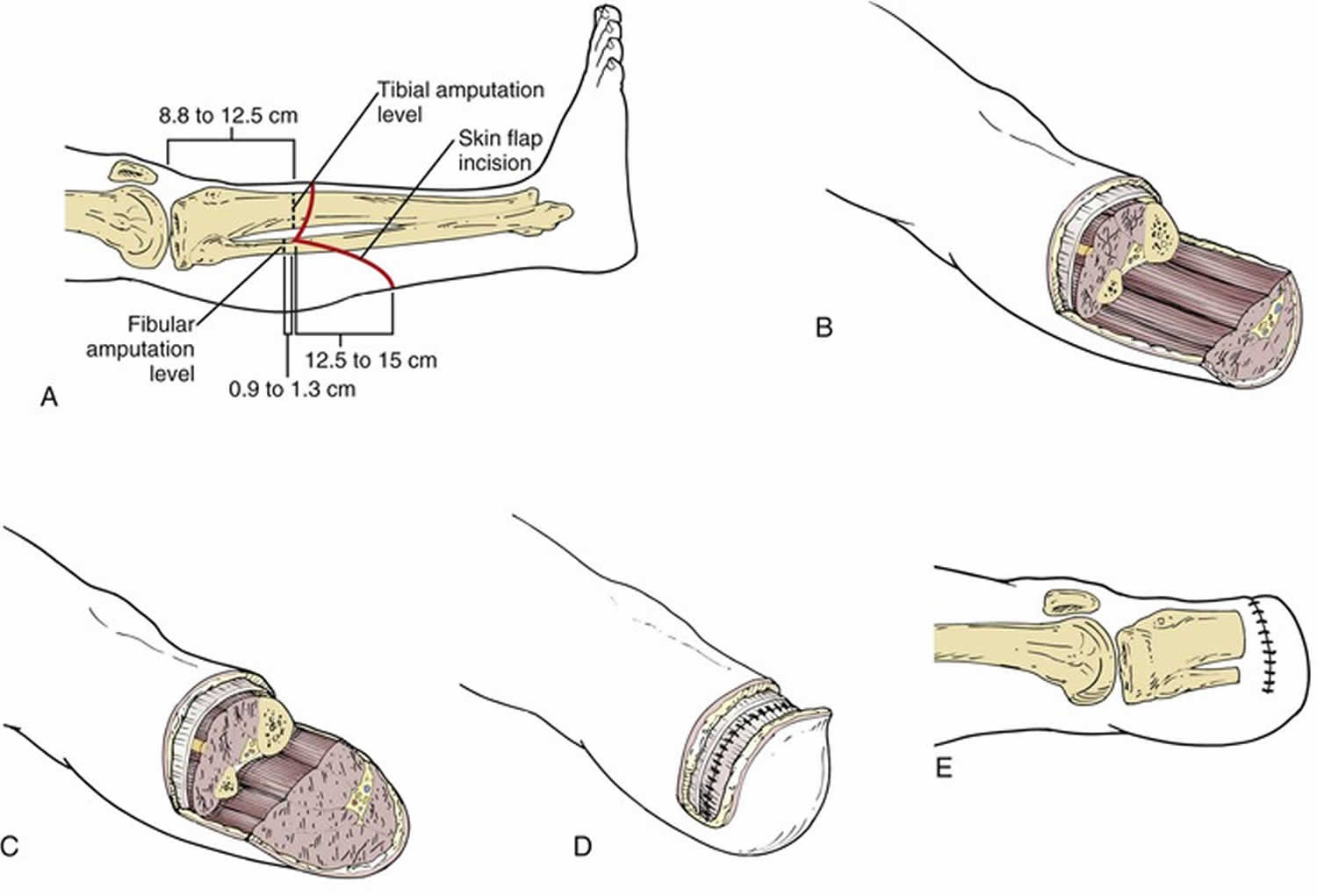
Figure 2. Below-knee amputation
Footnote: Below-knee amputation. A, Marking the skin incisions. B, Fashioning the flaps after bone transection. C, The soleus muscle is tailored to create a proper flap. D, The posterior deep fascia is sutured to the anterior deep fascia and periosteum. E, Closure of skin flaps.
Indications for below-knee amputation
There are three major categories of indications for proceeding with a below-knee amputation. These include urgent cases where source control of necrotizing infections or hemorrhagic injuries outweighs limb preservation. These operations are performed when death is imminent, and may at times, necessitate bedside operation if there is insufficient time to reach the operative suite.
Less acutely, urgent below-knee amputations may be performed for chronic nonhealing ulcers or significant infections with the risk of impending systemic infection or sepsis. These patients are typically sick with multiple significant comorbidities and a chronic progressive or waxing/waning course of illness. Definitive source control/debridement is critical, yet there is typically the time to medically optimize a patient over a few hours or days. Intravenous (IV) antibiotics are an important adjunct to operative treatment in these cases, limiting morbidity associated with systemic bacterial infection 13.
In addition, relatively urgent below-knee amputations may be performed where limb salvage has failed to preserve a mangled lower extremity 14. Adequate resuscitation and stabilization must always have occurred before such a decision, as judged by vital signs, lactate, base deficit, and the management of concomitant injuries. In cases of full-thickness burns to a majority of an extremity, serious or complete neurovascular compromise, or irreparable soft tissue defects, definitive below-knee amputation may be appropriate 15.
Finally, elective below-knee amputations are appropriate in the non-septic or imminently sick population with problems such as venous stasis ulceration, multiple distal to mid-foot amputations with persistent infection or vascular insufficiency, or lack of distal foot/ankle function with refractory pain 16.
Below-knee amputation contraindications
The most significant contraindication to performing a non-urgent below-knee amputation is vascular insufficiency at the planned amputation site or poor wound healing ability such that the surgical wound will not heal 7. This contraindicates elective or semi-elective procedures until the patient condition can be optimized. These patients should undergo a thorough preoperative workup including measurement of pulse volume recordings in bilateral distal extremities to determine adequate vascular flow. Doppler may be used to assess for gross blood flow, and ankle brachial indices can evaluate an individual and lower versus upper extremities. Oxygen pressures in the toes and transcutaneous oxygen pressure are useful for determining oxygenation on a microvascular level. In cases of profound vascular insufficiency, bypass grafting or the placement of stents may be necessary before performing a below-knee amputation.
In patients who are in extremis due to sepsis, blood loss, acute major organ failure, or other cause, every attempt should be made to stabilize the patient before starting a major surgical procedure. The one exception to this is the case of uncontrolled, spreading necrotizing infection, where source control is often life-saving 7. Conversely, in cases of acute hemorrhage, local tourniquets may be applied for several hours while resuscitation takes place.
Below-knee amputation technique
There are several ways to perform a below-knee amputation, one of the most significant differences being guillotine versus completed amputation. A guillotine amputation is performed quickly with the goal of controlling infection or blood loss, or when completing a near-total amputation of a mangled extremity at bedside. This can be effective when tissue planes must demarcate over hours or days, with serial debridements taking place before closure can be performed. In contrast, where time and tissue allow, a completed amputation involves all steps as outlined below, resulting in a closed, sutured stump ready for application of a stump shrinker and prosthesis planning 17. The following outlines several of the basic steps commonly used to perform an uncomplicated below-knee amputation 18.
Once the patient is prepped and draped, the tibial tubercle and joint line are marked, with the below-knee amputation incision marked distally, typically 10 to 15 cm from the tibial tubercle. An anterior skin flap is drawn to include the anterior two-thirds of the leg, while the posterior flap is drawn 150% longer than the anterior flap to allow ample soft tissue for closure. The tourniquet is inflated. A skin incision is made down to the fascia circumferentially. The fascia incised and the muscles carefully divided down to the tibia and fibula.
The tibial nerve and deep and superficial peroneal nerves are identified within their respective neurovascular bundles. Each nerve is injected with 1% lidocaine (optional), placed under gentle traction, and sharply divided with a fresh scalpel blade. This allows for retraction of the nerve, avoiding development of a painful neuroma distally at the below-knee amputation stump. Each major artery, including the anterior and posterior tibial arteries, are identified and ligated with a silk tie.
The tibial and fibular shafts are cut with an oscillating saw, and the corners beveled with a rongeur or saw. A small hole is placed with a drill in the distal tibial shaft; the gastrocnemius aponeurosis is secured to this via a nonabsorbable suture.
The tourniquet is released and adequate hemostasis obtained through a cautery or ligation of major bleeding vessels. A drain is placed in the wound, and the fascia is then approximated, followed by the subcutaneous tissue and finally the skin. This may be sutured or stapled based on surgeon preference.
The stump is dressed with a sterile dressing and placed into a well-padded splint or knee immobilizer. This will both protect healing soft tissue and prevent the development of early flexion contracture at the knee which would limit postoperative mobility with a prosthesis.
In the immediate postoperative setting, the limb stump should be serially examined every 24 to 48 hours for necrosis of the skin edges, bleeding, and signs of infection. Any drains should be removed once there is sufficiently minimal drainage according to surgeon preference. Once the wound is healing well, a stump shrinker may be placed, providing circumferential compression around the stump and distal extremity. A prosthetics company should be contacted, with a formal patient evaluation performed and the provisional prosthetic is chosen. Ultimately, there are many forms of prosthetics for lower limbs, and patient preference, condition, and insurance, among other factors, will dictate which prosthetic is the best long-term option.
Below-knee amputation complications
As with all surgical procedures, there are possible acute complications of uncontrolled bleeding, infection, and acute postoperative pain, and broader medical complications including acute blood loss anemia and stress-induced cardiac ischemia. With a below-knee amputation performed for infection or acute soft tissue trauma, a second operation may be necessary if distal skin edges further demarcate or if the area of infection was not adequately resected 19.
Chronic complications of below-knee amputations include the development of painful neuromas from transected nerves, highlighting the importance of proper intraoperative technique as described above. Phantom limb pain, or the perception of pain or troubling sensation in the missing limb, is a common complaint. They address this with a mirror box, local injections, adjustment to the prosthesis, or a variety of other modalities. The psychiatric and psychosomatic effects of a below-knee amputation should not be overlooked in postoperative patients as this cohort has been shown to have higher rates of depression and suicide 20.
Foot amputation
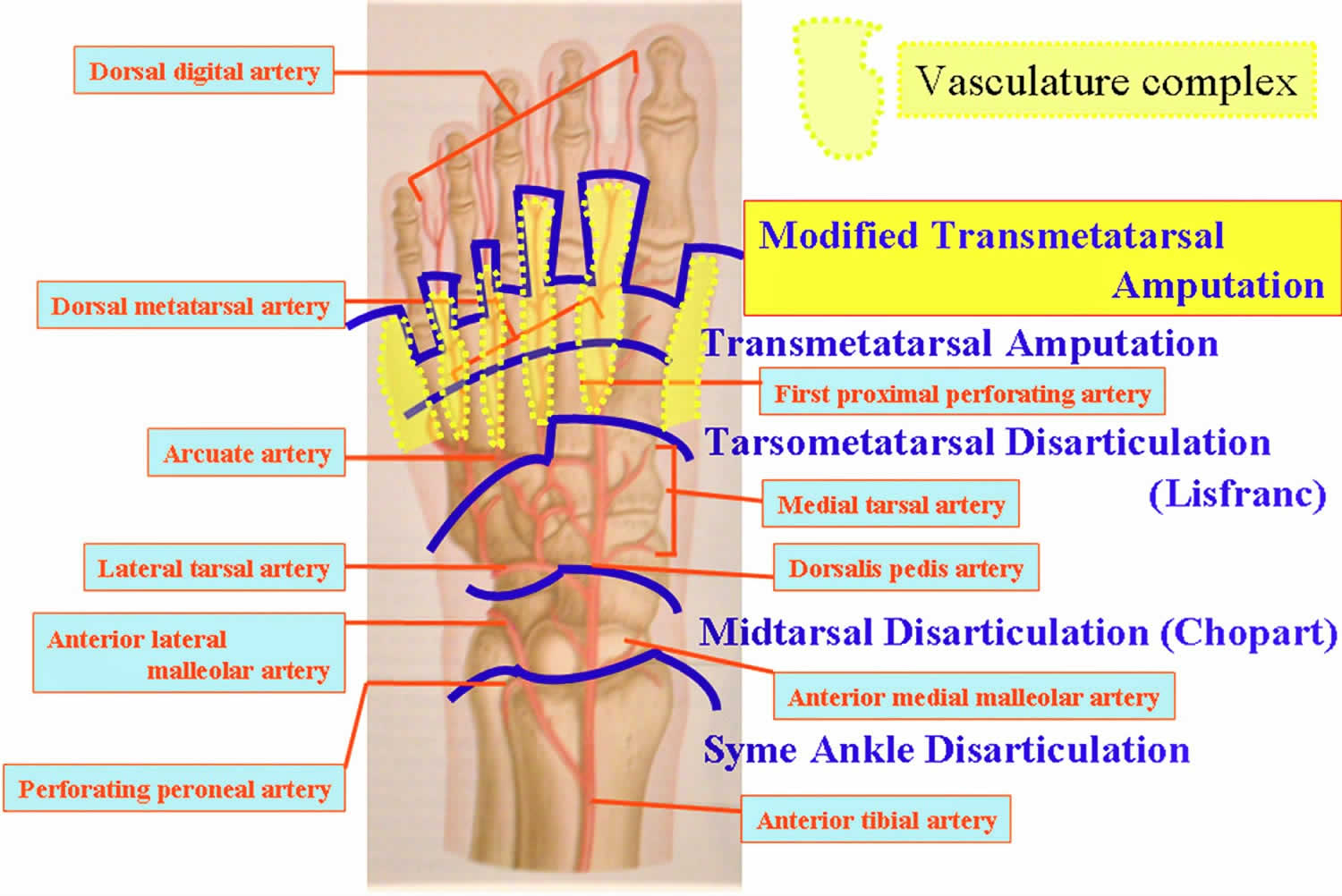
Midfoot and hindfoot amputations
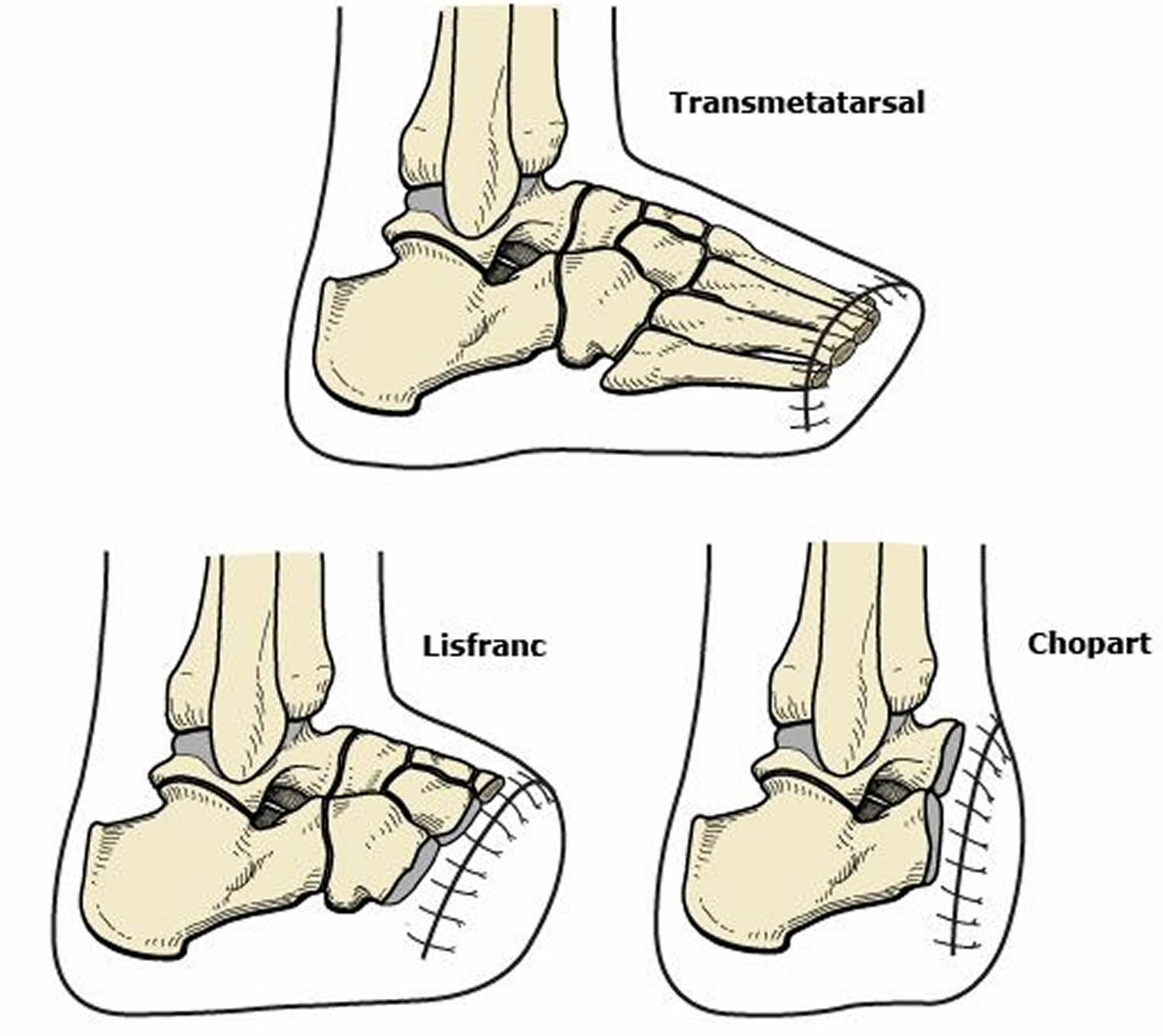
- Tarsometatarsal (Lisfranc amputation) – amputation of the forefoot at the tarsometatarsal line.
- Mid-tarsal (Chopart amputation) – amputation between the talus and the calcaneus proximally and the cuboid and the navicular distally.
- Ankle disarticulation (Syme amputation) – amputation through the ankle joint
These 3-type of amputations are mainly performed in children to preserve the length of the residual limb and to keep the epiphyseal plate intac.
Equinus varus foot deformity is possible due to the following: a gastrox-soleus and dorsiflexor imbalance, as well as a shortened lever arm. Surgical techniques to prevent this deformity include Achilles Tendon lengthening and the “reattachment of the peroneal and anterior tibial muscles to the more advantageous biomechanical position”.
Advantages
- Range of prosthetic options such as insoles, toe fillers or ankle-foot orthosis (exception for ankle disarticulation)
Disadvantages
- May need further surgery in future
- Can lead to skin breakdown and joint pain
- Cosmesis might be not accepted by the patient
Figure 3. Foot amputation
[Source 21 ]Chopart amputation
Chopart described this amputation in 1814. Chopart amputation involves a long plantar flap similar to that used in the Lisfranc amputation (see Figures 3). Chopart amputation is performed through the talocalcaneonavicular joint and the calcaneocuboid joint. To prevent equinovarus deformity resulting from unopposed plantar flexion, an Achilles tenectomy is recommended. The extensor hallucis longus and the tibialis anterior tendons may be reattached to the talar neck. The extensor digitorum longus may be reattached to the calcaneus. The wound is irrigated and closed in layers.
Postoperative considerations
Because the Chopart amputation results in a dramatic alteration in normal foot biomechanics, its durability may be limited. A short-leg plaster cast is used over the sterile dressings. The cast must be molded to ensure that the talus is slightly dorsiflexed in relation to the tibia and that the calcaneal tuberosity is parallel to the long axis of the tibia. The cast is changed weekly to check wound healing. Weight bearing is allowed after 6 weeks. Patients with a Chopart amputation need a custom-fitted ankle-foot orthosis with a filler to hold the shoe adequately.
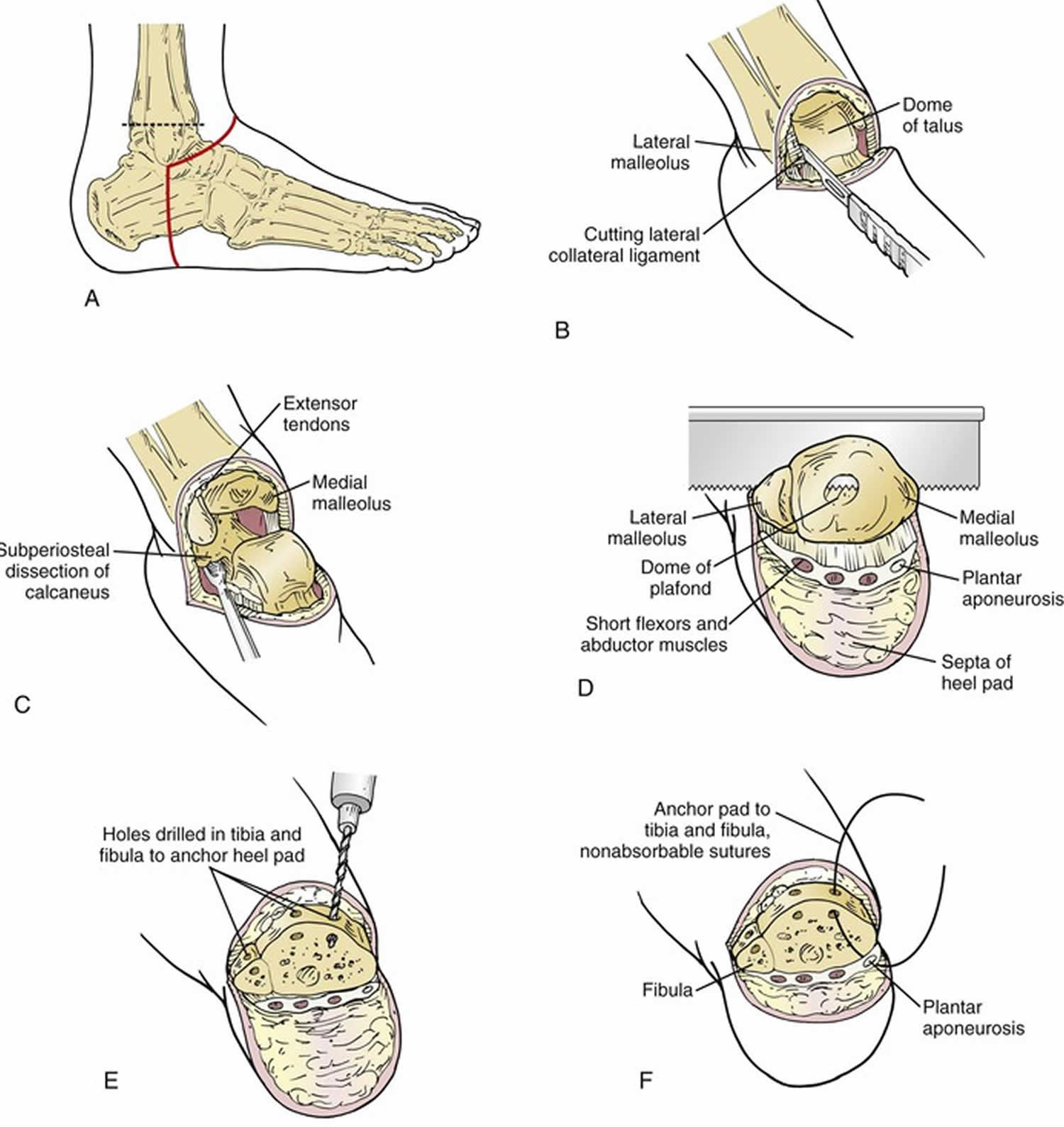
Syme amputation
Syme first described this amputation in 1843. Syme amputation is amputation of the foot done through the ankle joint. The foot is removed but the heel pad is saved so the patient can put weight on the leg without a prosthesis (artificial limb). Syme amputation is indicated for foot trauma, infection or tumors as well as certain types of limb deformities when the foot cannot be saved.
A Syme amputation is NOT appropriate in the following situations:
- In those with medical conditions where the risks of surgery outweigh the benefits. If the medical conditions can be improved, surgery can be reconsidered.
- Poor blood flow through the artery that supplies the heel pad. Without good blood flow, the surgical wound will not heal.
- Lack of an intact heel pad. If there is any ulcer, wound or dead tissue at the heel, a Syme amputation should not be performed and a higher level amputation is recommended.
- Infection, tumor or trauma that involves the ankle. A Syme amputation will not adequately treat the problem so a higher level of amputation is needed.
- The presence of diabetic neuropathy is a specific contraindication to Syme’s amputation because of the inability to protect the stump from injuries such as scalding and pressure.
The surgery is usually performed with the patient asleep under general anesthesia. For patients with risk factors that make general anesthesia dangerous, the surgery can be done with spinal anesthesia or a leg nerve block with sedating medication. A tourniquet can be used to help minimize blood loss.
The incision is made where the foot and ankle meet. The heel pad is protected. The heel fat pad is carefully dissected by staying close to the calcaneus to avoid buttonholing. The anterior incision extends across the ankle just distal to the tip of each malleolus. The posterior incision extends from the malleoli vertically down and across the sole of the foot. The ligaments and tendons attaching the foot to the ankle are cut and the soft tissues are removed from the foot bones. Arteries are tied off and then cut as well. The bony prominences at the ankle are removed so that the end of the leg has a flat surface after wound closure. A drain is sometimes used to help prevent a pool of blood from developing deep in the tissue that might cause failure of the procedure. Lastly, a bulky soft dressing and a cast are applied.
In a one-stage amputation, the malleoli are divided with a saw at the level of the articular surface of the tibia, and the width is reduced by vertical bone excision. Holes are drilled in the medial, anterior, and lateral parts of the distal tibia and fibula to secure the heel pad directly under the tibia. In a two-stage Syme amputation, the wound is closed by suturing the heel flap to the dorsal fascia. Six weeks later, the malleoli are removed through separate vertical incisions.
After the surgery, patients are monitored in the recovery unit for a short time. Patients may start walking once the wound is healed. Length of stay in a hospital can vary. Patients who can get around safely on one leg with crutches or a front-wheeled walker and have help at home can go home after surgery. Patients who need more assistance or daily physical therapy may go to a rehabilitation center, transitional care unit, or skilled nursing facility temporarily before going home.
Skin staples or sutures are removed in clinic when the wound is healed. Swelling can be managed with a compression stocking, but it is normal to have swelling for up to a year after surgery.
After the wound is healed and the majority of the leg swelling is gone, an experienced prosthetist makes a prosthesis (artificial limb) for the lower leg and stump. The prosthesis may need multiple adjustments so it fits properly. When the prosthesis is ready, additional therapy is done to learn how to walk well with the prosthesis.
Potential complications
The most significant complication is failure to heal the wound. This can lead to infection, death of tissue, and the need for an amputation at a higher level. Another potential problem after this procedure is too much motion of the heel pad stump, which can cause areas of increased pressure at the bottom of the amputation and lead to ulcers. These ulcers can sometimes be treated with local wound care and prosthesis modification. If there is a bony prominence causing the ulcer, additional surgery should be done to remove the bony prominence and allow healing.
Many patients start out with a sensation the foot is still there (phantom limb sensation). This is normal and not painful. However, some patients may develop nerve pain where major nerves were cut (phantom limb pain).
Because of potential complications of Syme amputations discussed earlier, sometimes a Syme amputation has to be revised to a below the knee amputation (BKA). If the risk of developing complications is high after a Syme amputation, it may be better to choose a below-knee amputation from the beginning. Multiple surgeries can be emotionally and physically stressful. A below-knee prosthesis can be more cosmetically appealing. The ankle portion of a Syme amputation prosthesis has to be wider to fit the end of the stump.
There are multiple aspects to consider in the decision-making process for an amputation. Your orthopedic surgeon will work with you to decide what is best for you.
Postoperative considerations.
The chief advantage of the Syme amputation is the preservation of limb length, patients with Syme amputations have the ability to be walk on the limb without a prosthesis during brief periods of weight bearing, such as during transfer from bed to wheelchair. This may be beneficial in situations like getting up in the middle of the night to go to the bathroom. Prosthesis training is easier with a Syme amputation than with a below-knee amputation because it feels more functionally “normal.” The increased energy demands on the body are also less with a Syme amputation than with a below-knee amputation.
The disadvantages include the slight leg-length discrepancy, which may lead to biomechanical side effects in more proximal or contralateral joints. Further, the prosthesis is typically bulky at the ankle and less cosmetically appealing than a conventional below-knee prosthesis, which can be designed with a near-normal ankle profile. In addition, because it is an end weight-bearing stump, the heel fat pad may be unstable and can migrate medially, exposing the distal tibia to excessive force. Thus, the Syme amputation has its greatest utility in young, healthy trauma patients with extensive forefoot injuries who are highly motivated to avoid transtibial amputation.
Figure 4. Syme amputation
Footnote: Syme’s amputation. A, Skin incision and bone transection level. B, Exposure of the ankle and division of the ligaments. C, Soft tissue dissection from the calcaneus. D, Division of the tibia and fibula. E, Holes drilled in the anterior aspect of the tibia and fibula. F, Fascia lining the heel pad sutured to the bone.
Figure 5. Syme amputation
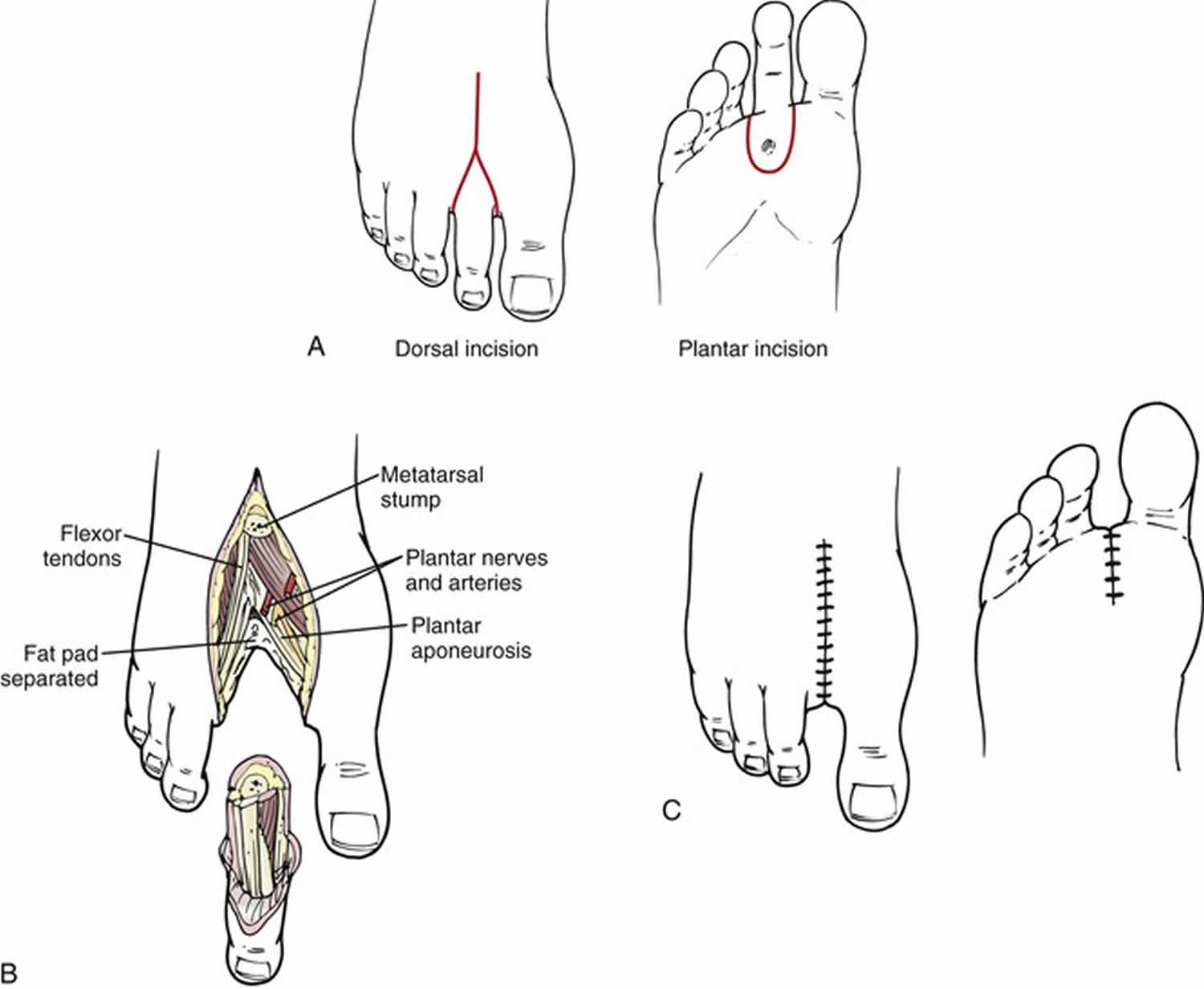
Toe amputation
Toe amputation is amputation through phalanges or disarticulation of metatarsal-phalangeal joint.
Toe amputation is indicated for foot disease (usually due to ulcers) where the tissues (skin and muscles) of your foot are dying. Because leaving dead or infected tissue untreated can be dangerous as the infection can spread. This usually happens as a result of atherosclerosis, where abnormal fatty material coats the inside of an artery, causing it to narrow or ‘harden’. The amount of blood flowing through the artery is reduced.
Toe amputation should relieve any pain, prevent the spread of infection, remove dead tissue, improve your mobility and can sometimes help you to return to normal activities.
Toe amputation complications
General complications:
- pain
- bleeding
- unsightly scarring
- blood clots
- difficulty passing urine
Specific complications:
- damage to small blood vessels
- amputation failure
- infection of the surgical site (wound)
- phantom limb sensation
- severe pain, stiffness and loss of use of your foot
- Great toe amputation affects balance, and ambulation because the late stance phase of gait and push off is disrupted without a first toe/ray to act as the final point of weight transfer.
- The second toe acts as lateral support to the great toe and amputation of the second toe may lead to halux valgus
- The transverse arch of the foot get affected with the removal of any toe
Toe amputation recovery
It is difficult to predict the length of recovery. You will usually stay in hospital for a few days so your wound can be checked. You may be transferred to a rehabilitation ward to prepare for leaving hospital. Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your doctor for advice. You can expect to make a good recovery with a better quality of life.
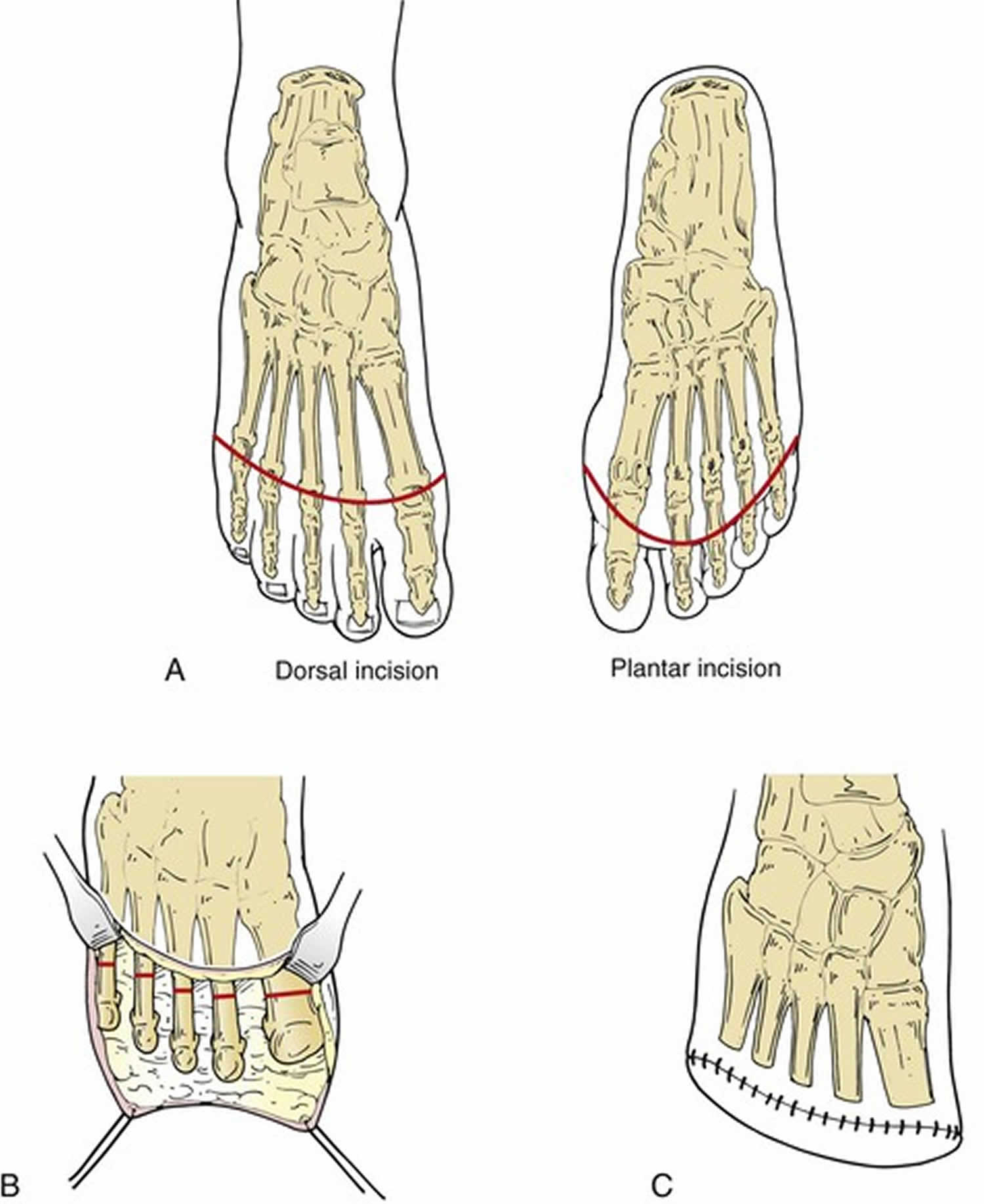
Transmetatarsal amputation
Transmetatarsal amputation is partial foot amputation through metatarsals. Transmetatarsal amputation is appropriate for wounds involving the entire forefoot. Transmetatarsal amputation may be preferable to isolated first ray amputation in selected patients because transmetatarsal amputation has better healing rates and, owing to improved foot mechanics, better rehabilitation rates. transmetatarsal amputation also offers the benefits of full limb length, normal shoe wear, and near-normal ambulation. A one-stage transmetatarsal amputation should generally not be undertaken in the setting of severe forefoot infection. In this situation, a guillotine débriding amputation should be considered, followed by formal wound closure after control of sepsis. A partial-thickness skin graft may be an effective method to salvage an open transmetatarsal amputation wound if it is restricted to non–weight-bearing surfaces. transmetatarsal amputation is contraindicated if there is excessive bone deformity in the midfoot and hindfoot, which would not be structurally sound.
- usually due to wounds in the forefoot
- a guillotine amputation is sometimes done in order to rid the foot of infection
- dorsal split thickness grafts on the plantar aspect of the foot is used instead of skin grafts because it is more resilient
- the dorsal contact area of the foot is decreased and this leads to an increase of pressure and may result in calluses, ulcers, and wounds
- stance and gait (forward propulsion) is negatively influenced because the lever arm of the foot is shortened
- plantar flexion contracture should be avoided – this may occur because of the gastroc-soleus strength dominance over the dorsiflexors
Postoperative considerations
A posterior plaster splint that maintains the foot at 90 degrees is applied. Weight bearing is prohibited until adequate healing is observed, usually after 3 to 4 weeks. transmetatarsal amputation is a relatively durable procedure following initial healing. Primary healing can be expected in 50% to 75% of patients following transmetatarsal amputation. Revision to a higher level is necessary in approximately 25% to 40% of transmetatarsal amputations. A vacuum dressing may be effective in avoiding more proximal amputation. With appropriate orthoses, patients can be expected to ambulate with an almost imperceptible gait alteration following complete healing.
Figure 6. Transmetatarsal amputation
Ray amputation
Ray amputation involves amputation of the toe along with all or part of the corresponding metatarsal head. Although a single isolated ray amputation sometimes proves durable, multiple ray amputations narrow the foot excessively and create biomechanical instability. This increases the amount of weight that must be borne by the remaining metatarsal heads and can lead to new areas of increased pressure, callus formation, and ulceration. Ray amputation may be useful in the treatment of blue toe syndrome caused by microatheroembolism involving the entire toe if there is insufficient skin to cover the exposed metatarsal head. Ray amputation may also be useful in the treatment of mal perforans ulcers in the neuropathic diabetic foot, especially in the setting of osteomyelitis of the metatarsal head. Because a hallux valgus deformity commonly develops following isolated second toe amputation, complete second ray amputation may be preferable because it reduces the angle between the first and third metatarsals.
In comparison to the lateral four rays, the first metatarsal and great toe contribute disproportionately to the mechanics of normal ambulation. In a normal stride, the foot contacts the ground on the posterolateral aspect of the heel. The weight is transferred progressively along the lateral plantar surface of the foot and then across the metatarsal heads from lateral to medial. Finally, the foot lifts off primarily from the first metatarsal head and the great toe. Although near-normal foot mechanics can be achieved after amputation of one of the lateral four rays, amputation of the great toe and first metatarsal head markedly alters normal ambulation and may result in destructive forces within the architecture of the foot. Recurrent ulceration following first ray amputation has been reported in up to 60% of patients. Some orthopedic surgeons recommend formal transmetatarsal amputation of all five rays rather than isolated first ray amputation. The contrarian viewpoint holds that transmetatarsal amputation may require revision or reamputation in 20% to 40% of patients and that above-ankle amputation is necessary in one of five patients. Thus, there is a lack of consensus in the literature, and the final decision between first ray amputation and complete transmetatarsal amputation should be individualized, based on patient and surgeon preferences.
- First ray along with great toe amputations affects balance and gait negatively
- Amputation of the 2nd through 4th ray disrupts the transverse arch because the ligamentous structure is removed
- Single ray amputations decrease the “structural integrity of the arch”
- When the fifth ray is resected it negatively impacts gait during midstance to terminal stance because it changes the rollover action of the foot
Postoperative considerations
Weight bearing is prohibited until the wound is thoroughly healed. We usually use a simple bulky soft dressing to protect the wound. A rocker-bottom shoe with a metatarsal bar that unloads pressure from the toes may be effective in selected patients. Approximately 25% of toe amputations fail to heal and require additional amputation at a higher level. Of these higher amputations, approximately 40% are at the transtibial level. With the use of appropriate orthoses and foot care, many patients achieve durable ambulation following toe or ray amputation.
Figure 5. Ray amputation
Finger amputation
Traumatic finger amputations are common and often debilitating, totaling 45,000 cases annually in the United States 22. In the United States, close to a third of traumatic finger amputations are work-related, with even greater numbers world-wide 23. Up to 90% of these injuries are treated with revision amputations and other non-replantation techniques 24. If your injury has cut off a large part of your fingertip, your surgeon may consider the pros and cons of reattaching the amputated part. This is called “replantation.” This is a complicated surgical procedure during which blood vessels are repaired to allow both the inflow and outflow of blood to the amputated part. A replantation can require significant recovery time for the patient.
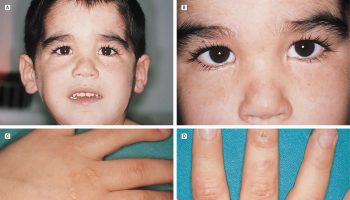
Fingertip amputations in young children
Doctors treat fingertip amputations somewhat differently in children younger than 6 years of age. After thoroughly cleaning and preparing an amputated fingertip, the surgeon may reattach it to the finger. The fingertip may continue to grow relatively normally, even if bone was exposed. This is especially possible in children younger than 2 years of age.
Your doctor will consider many things when determining whether to reattach your child’s amputated fingertip, including:
- Your child’s age and general health
- The condition of the amputated part
- How the injury occurred.
Complications
In many cases, surgery can return a large degree of feeling and function to a fingertip injury. However, there are complications associated with the injury itself and with surgery for fingertip injuries. Your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications.
Possible risks and complications include:
- Infection
- Poor wound healing
- Persisting numbness or hypersensitivity
- Stiffness
- Abnormal nail growth
- Loss of viability in the amputated part
- Neuroma, or painful nerve regeneration following the injury
- Adverse reaction to anesthesia
Outcomes
Recovery from a fingertip injury may take several months. After your injury heals, mild to severe pain and sensitivity to cold may continue for up to a year or may even be permanent.
Your doctor or a hand therapist may recommend specific exercises to improve range of motion and strengthen your hand and fingers. They may also suggest additional therapies to help promote healing and function. These therapies may include:
- Heat and massage
- Fingertip desensitization
- Electrical stimulation of the nerves in the hand
- Splinting
- Special compression wrappings to control swelling
- Activities to improve fine motor skills such as pinching and grasping
- Clinical Practice Guideline for Rehabilitation of Lower Limb Amputation. Department of Veterans Affairs, Department of Defence. 2007. https://www.healthquality.va.gov/guidelines/Rehab/amp/amp_sum_correction.pdf[↩]
- McNamara et al (1994) Severe Open Fractures of the Lower Extremity: A Retrospective Evaluation of the Mangled Extremity Severity Score (MESS). J Orthop Trauma 8: 81-7[↩]
- Russell et al (1991) Limb Salvage Versus Traumatic Amputation A Decision Based on a Seven-part Predictive Index Ann Surg. 213: 473-81[↩]
- Johansen et al (1990) Objective Criteria Accurately Predict Amputation following Lower Extremity Trauma. J Trauma.30: 568-73[↩]
- Spires MC, Kelly BM, Davis AJ, editors. Prosthetic restoration and rehabilitation of the upper and lower extremity. Demos Medical Publishing; 2013 Dec 19.[↩][↩][↩]
- Burgess EM, Zettl JH. Amputations below the knee. Artif Limbs. 1969 Jan 1;13(1):1-2.[↩]
- Adams CT, Lakra A. Below Knee Amputation (BKA) [Updated 2018 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534773[↩][↩][↩][↩]
- Hong CC, Tan JH, Lim SH, Nather A. Multiple limb salvage attempts for diabetic foot infections: is it worth it? Bone Joint J. 2017 Nov;99-B(11):1502-1507.[↩]
- Phair J, DeCarlo C, Scher L, Koleilat I, Shariff S, Lipsitz EC, Garg K. Risk factors for unplanned readmission and stump complications after major lower extremity amputation. J. Vasc. Surg. 2018 Mar;67(3):848-856.[↩]
- Ladlow P, Phillip R, Coppack R, Etherington J, Bilzon J, McGuigan MP, Bennett AN. Influence of Immediate and Delayed Lower-Limb Amputation Compared with Lower-Limb Salvage on Functional and Mental Health Outcomes Post-Rehabilitation in the U.K. Military. J Bone Joint Surg Am. 2016 Dec 07;98(23):1996-2005.[↩]
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South. Med. J. 2002 Aug;95(8):875-83.[↩]
- Russell Esposito E, Miller RH. Maintenance of muscle strength retains a normal metabolic cost in simulated walking after transtibial limb loss. PLoS ONE. 2018;13(1):e0191310[↩]
- Tisi PV, Than MM. Type of incision for below knee amputation. Cochrane Database Syst Rev. 2014 Apr 08;(4):CD003749.[↩]
- Penn-Barwell JG. Outcomes in lower limb amputation following trauma: a systematic review and meta-analysis. Injury. 2011 Dec;42(12):1474-9.[↩]
- Narula N, Dannenberg AJ, Olin JW, Bhatt DL, Johnson KW, Nadkarni G, Min J, Torii S, Poojary P, Anand SS, Bax JJ, Yusuf S, Virmani R, Narula J. Pathology of Peripheral Artery Disease in Patients With Critical Limb Ischemia. J. Am. Coll. Cardiol. 2018 Oct 30;72(18):2152-2163.[↩]
- Chiodo CP, Stroud CC. Optimal surgical preparation of the residual limb for prosthetic fitting in below-knee amputations. Foot Ankle Clin. 2001 Jun;6(2):253-64.[↩]
- Harris AM, Althausen PL, Kellam J, Bosse MJ, Castillo R., Lower Extremity Assessment Project (LEAP) Study Group. Complications following limb-threatening lower extremity trauma. J Orthop Trauma. 2009 Jan;23(1):1-6.[↩]
- Busse JW, Jacobs CL, Swiontkowski MF, Bosse MJ, Bhandari M., Evidence-Based Orthopaedic Trauma Working Group. Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J Orthop Trauma. 2007 Jan;21(1):70-6.[↩]
- Fergason J, Keeling JJ, Bluman EM. Recent advances in lower extremity amputations and prosthetics for the combat injured patient. Foot Ankle Clin. 2010 Mar;15(1):151-74.[↩]
- Pedersen HE. The problem of the geriatric amputee. Artif Limbs. 1968 Autumn;12(2):Suppl:1-3.[↩]
- Terashi, Hiroto et al. “A modified transmetatarsal amputation.” The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons 50 4 (2011): 441-4.[↩]
- McCall B, Horwitz I. An assessment and quantification of the rates, costs, and risk factors of occupational amputations: analysis of Kentucky workers’ compensation claims, 1994–2003. Am J Ind Med. 2006;49:1031–8.[↩]
- Yuan F, McGlinn EP, Giladi AM, Chung KC. A Systematic Review of Outcomes after Revision Amputation for Treatment of Traumatic Finger Amputation. Plast Reconstr Surg. 2015;136(1):99-113. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4481863/[↩]
- Omoke N, Chukwu C, Madubueze C. Traumatic extremity amputation in a Nigerian setting: patterns and challenges of care. Int Orthop. 2012;36:613–8.[↩]