Contents
What is anticholinergic
Anticholinergic drugs competitively inhibit the actions of acetylcholine (ACh) at muscarinic receptors, leading to a blockade of the actions of the parasympathetic nervous system and on smooth muscles that lack cholinergic innervation. Anticholinergics are therefore known as antimuscarinic agents or muscarinic cholinergic blocking agents. Because the main actions of all members of this class of anticholinergic drugs are qualitatively similar to those of the best-known member, atropine, the terms “atropinic” and “atropine-like” are also used.
Anticholinergics or antimuscarinic drugs, are drugs that competitively inhibit the parasympathetic nervous system ultimately leads to decreased production of secretions in the salivary, bronchial, and gastrointestinal tracts. These effects are often used for several symptoms that originate due to parasympathetic nervous system overactivity, such as the “death rattle” and malignant bowel obstruction. Anticholinergic agents are divided into either tertiary amines or quaternary ammonium compounds, which differ in their ability to cross into the central nervous system. Quaternary compounds do not cross into the central nervous system and have a different adverse effect profile than the tertiary amines.
Anticholinergics have antisecretory activities and decrease nasal and bronchial secretions, salivation, lacrimation, sweating and gastric acid production, and can be used to decrease secretions in allergic and inflammatory diseases. Anticholinergics relax smooth muscle in the gastrointestinal tract, bladder and lung and can be used for gastrointestinal, urological or respiratory conditions associated with spasm and dysmotility. Some anticholinergics have antiemetic properties and are used to prevent nausea and vomiting from motion sickness or during the perioperative period. Anticholinergics increase heart rate and can be used to treat bradycardia. They are also used to reverse cholinergic overstimulation caused by cholinesterase inhibitors and neuromuscular blockers in anesthesia.
The common side effects of anticholinergic agents are largely those of parasympathetic stimulation and include dryness of the mouth and eyes, decreased sweating and hyperthermia, headache, visual blurring, constipation, urinary retention, impotence, tachycardia and palpitations, anxiety, restlessness and in some instances agitation and delusions. Anticholinergics rarely cause liver injury. Their relative safety probably relates to their use in low doses for short periods of time only. Most anticholinergics are metabolized in the liver via the cytochrome P450 system.
Anticholinergic agents occur naturally as alkaloids in Atropa belladonna and other plants of the family Solanaceae 1. The natural or semisynthetic belladonna alkaloids include atropine (generic), hyoscyamine and scopolamine. Belladonna alkaloids and their synthetic analogues have been used for their cosmetic, therapeutic and toxic effects for centuries. The term ‘belladonna’ (means beautiful woman in Italian) refers to the Italian women who desired dilated pupils to appear more seductive. In modern times, synthetic anticholinergic drugs have been used for a variety of medical conditions, including Parkinsonism, depression, urinary incontinence, allergy, travel sickness, obstructive lung diseases, sleep disorders, peptic ulcer disease, cardiac arrhythmias and psychoses. As late as the 1950s, atropine-induced coma was used as a treatment for psychosis in Norwegian hospitals 2. In 1991, approximately 600 of the drugs on the United States market were reported to have anticholinergic activity 3.
Currently, many of these drugs have been withdrawn, but a large number of drugs with anticholinergic properties are still commonly used 1. Advanced age is a risk factor for the use of anticholinergic drugs because these drugs are prescribed for the symptomatic management of medical conditions that often occur in later life, such as urinary incontinence and sleep disorders 4. Other risk factors for anticholinergic prescriptions are polypharmacy and institutionalization. Elderly people in nursing home care use significantly more anticholinergic drugs than the home-dwelling elderly 5. Despite the anticholinergic hypersensitivity of patients with dementia, elderly patients with dementia are more frequently exposed to definite anticholinergic drugs than are those without dementia 6. Furthermore, epidemiological studies have reported that people using acetylcholinesterase inhibitors have an increased risk of receiving an anticholinergic drug with the potential to antagonize the effects of the cholinesterase inhibitor 7, possibly because the adverse effects of the cholinesterase inhibitor are misinterpreted 8. It has also been reported that among hospitalized people aged above 65 years, the prevalence of anticholinergic prescriptions increases significantly during their hospital stay, although it seems like Geriatric Units are more vigilant than others to the use of anticholinergic drugs 9. Finally, it has been shown that in palliative care, the use of anticholinergic drugs increases as death approaches 10.
The inhibitory effects of anticholinergic agents can be overcome by increasing sufficiently the concentration of acetylcholine (ACh) at receptor sites of the effector organ. The receptors affected are those of peripheral structures that are either stimulated or inhibited by muscarine—that is, exocrine glands and smooth and cardiac muscle.
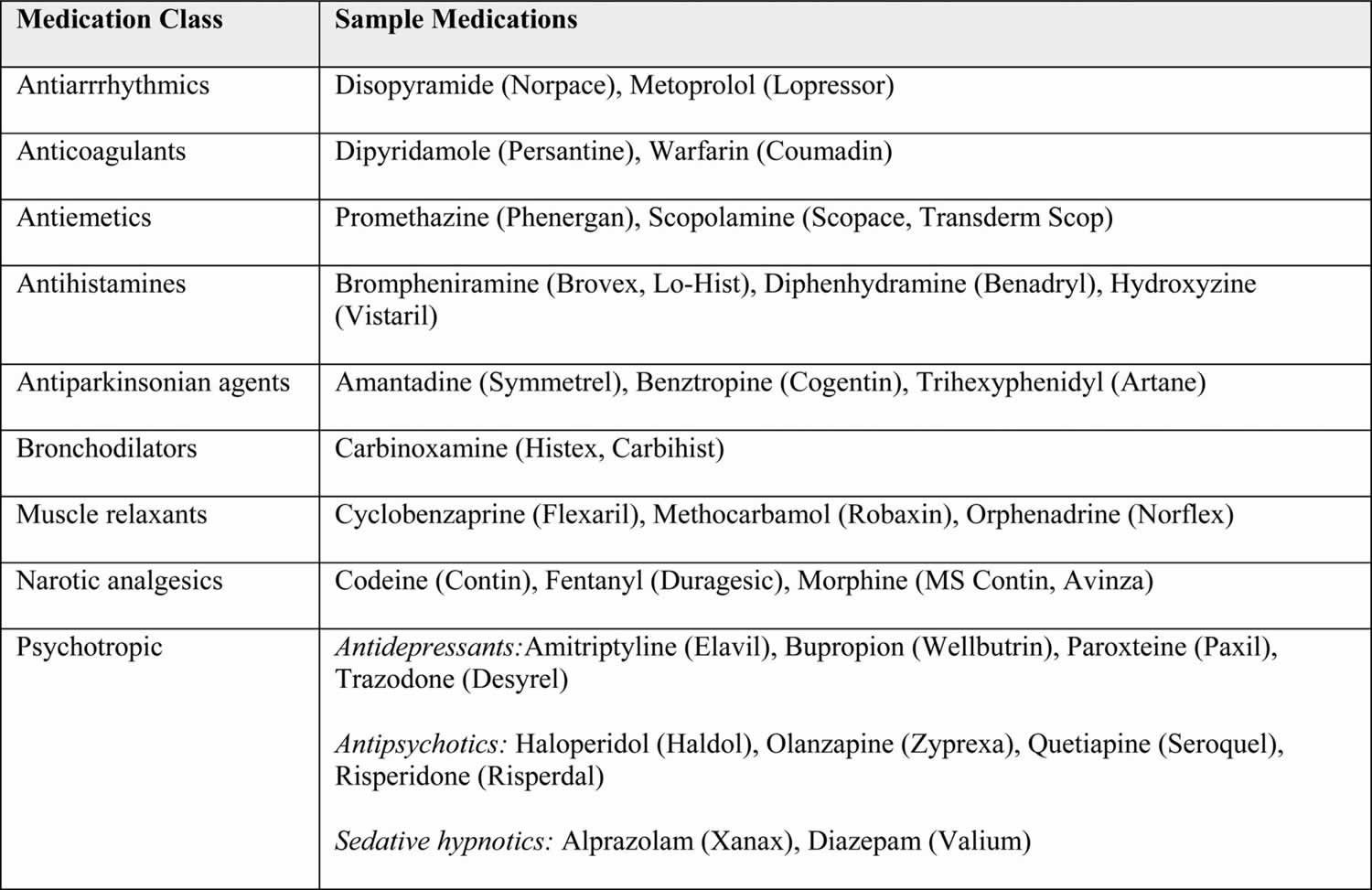
Table 1. Anticholinergic drugs list (medications with anticholinergic effects)
High anticholinergic properties
|
Detectable anticholinergic properties
|
Detectable anticholinergic properties
|
Table 2. Drugs with anticholinergic properties
[Source 1]Anticholinergic agents are typically used as treatment for anticholinesterase poisoning and vice versa. Physostigmine, tetrahydroaminoacridine, and other anticholinesterase inhibitors were used successfully as antidotes in several dozen subjects 12. The demonstration of physostigmine’s effectiveness led to the first controlled study of its ability to reverse delirium due to anticholinergic scopolamine 13. Physostigmine has been used to overcome anticholinergic toxicity.
In general, anticholinergics have little effect on the actions of acetylcholine (ACh) at nicotinic receptor sites. Thus, at autonomic ganglia, where transmission normally involves an action of acetylcholine (ACh) on nicotinic receptors, anticholinergic produces partial block only at relatively high doses. At neuromuscular junctions, where the receptors are nicotinic, extremely high doses of atropine or anticholinergic drugs are required to cause any degree of blockade. However, quaternary ammonium analogues of atropine and anticholinergic drugs generally have some degree of nicotinic blocking activity and consequently are more likely to interfere with ganglionic or neuromuscular transmission in doses only slightly greater than those that produce muscarinic block.
In the central nervous system (CNS), cholinergic transmission appears to be predominantly nicotinic in the spinal cord and both muscarinic and nicotinic at subcortical and cortical levels in the brain 14. Accordingly, many or most of the central nervous system (CNS) effects of atropine-like drugs at ordinary doses are probably attributable to their central anticholinergic actions. At high or toxic doses, the central effects of atropine and anticholinergic drugs consist, in general, of stimulation followed by depression; these are probably due to a combination of antimuscarinic and other actions. There is an increased release and turnover of acetylcholine (ACh) in the central nervous system (CNS) associated with the administration of anticholinergic drugs; this may result in the activation of nicotinic receptors in the brain and contribute to the central effects of this class of drugs 15. Because quaternary compounds penetrate the blood-brain barrier only poorly, antimuscarinic drugs of this type show little in the way of central effects.
Peripheral effects
Parasympathetic neuroeffector junctions in different organs are not equally sensitive to anticholinergic agents. However, the relative sensitivity of various parasympathetically innervated organs to blockade by anticholinergic agents varies little among the drugs. Small doses inhibit salivary and bronchial secretion and sweating. Larger doses cause the pupils to dilate, inhibit accommodation of the eyes, and block vagal effects on the heart, so that the heart rate is increased. Still larger doses inhibit the parasympathetic control of the urinary bladder and gastrointestinal tract, thus inhibiting micturition and decreasing intestinal tone and motility. Even larger doses are required to inhibit gastric secretion and motility. Because only the primary phase of gastric secretion is controlled by the vagus, the remaining hormonally controlled secretion is unaffected. Thus, doses of any anticholinergic drug that reduce the tone and motility of the stomach and the duodenum and inhibit gastric secretion also invariably affect salivary secretion, ocular accommodation, and micturition.
Anticholinergic drugs produce reversibly the functional equivalent of resection or paralysis of postganglionic cholinergic nerves. The actions and effects of particular anticholinergic agents usually differ only quantitatively from those of atropine, a belladonna alkaloid, which is considered as the prototype of the group.
Central effects
Anticholinergic atropine stimulates the medulla and higher cerebral centers. In doses used clinically (0.5–1.0 mg), this effect is usually confined to mild vagal excitation. The rate and occasionally the depth of breathing are increased. With toxic doses of anticholinergic atropine, central excitation becomes more prominent, leading to restlessness, irritability, disorientation, hallucinations, or delirium. With still larger doses, stimulation is followed by depression, coma, and medullary paralysis. The latter may be primarily responsible for a fatal outcome. Even moderate doses of anticholinergic atropine may depress some central motor mechanisms that control muscle tone and movement. This anticholinergic effect has been used to advantage in the management of the tremor and rigidity of Parkinsonism.
Anticholinergic scopolamine in therapeutic doses normally causes drowsiness, euphoria, amnesia, fatigue, and dreamless sleep with a reduction in rapid-eye-movement (REM) sleep. However, the same doses of anticholinergic scopolamine occasionally cause excitement, restlessness, hallucinations, or delirium, especially in the presence of severe pain.
Doses of anticholinergic atropine required to inhibit peripheral responses to choline esters or anticholinesterase (anti-ChE) agents produce almost no detectable central effects. This may reflect difficulty of penetration of the drug into the CNS. In animals, anticholinergic atropine antagonizes the action of acetylcholine applied locally to the cerebral cortex and spinal cord. However, anticholinergic atropine also depresses the effects of noncholinergic stimuli, indicating that the drug has central actions other than blocking cholinergic synapses.
The rise in body temperature due to the anticholinergic belladonna alkaloids is usually significant only after large doses. Nevertheless, in infants and small children, moderate doses induce “atropine fever.” In anticholinergic atropine poisoning in infants, the temperature may reach 43°C or higher. Suppression of sweating is doubtless an important factor in the production of the fever, especially when the environmental temperature is high, but other mechanisms also may be important when large doses are taken. It has been suggested that atropine may exert a central effect on temperature regulation; however, animals that do not sweat, such as dogs, do not exhibit fever after anticholinergic atropine.
What are anticholinergic effects
Anticholinergic drugs act on the muscarinic receptors in the central and peripheral nervous systems and inhibit acetylcholine-mediated responses by competitively binding to these receptors. Hence, ‘muscarinic receptor antagonists’ would be a more pharmacologically precise term. There are five subtypes of
muscarinic receptors, M1, M2, M3, M4 and M5, which have been characterized by molecular cloning 16. The G-protein coupled muscarinic receptors have seven transmembrane regions, and there are probably three classes of muscarinic antagonist binding sites 17. Muscarinic receptors are widely distributed throughout the human body and mediate distinct physiological responses according to their location and receptor subtype 18. All five receptor subtypes are expressed in the brain, and there is a potential interplay between the excitatory (M1, M3, M5) and the inhibitory (M2, M4) receptor subtypes responsible for the diversity of central acetylcholine mediated responses. The M1 receptor outnumbers the other receptor subtypes in the brain and constitutes 40–50% of the total number of muscarinic receptors in the human body 18.
Activation of M1 and M2 receptor is important for higher cognitive processes, and antagonism of central M1 and M2 receptors impairs memory and learning processes 18. Moreover, M2 receptor is important for the acetylcholine homeostasis by pre-synaptic regulation of acetylcholine release 19. Antagonism of the M4 and M5 receptors alters the regulation of other neurotransmitters such as dopamine, while M3 receptors are found in lower concentration in the brain and M3 antagonism does not affect behaviour or cognition 18. Almost every anticholinergic drug on the market is a non-selective antimuscarinic agent which means that the drug does not discriminate among the five muscarinic receptor subtypes. Thereby, the drugs inhibit all the central acetylcholine-mediated muscarinic responses that are involved in a widespread of different mechanisms such as controlling autonomic responses, regulation of the release of other neurotransmitters, synaptic plasticity and cognitive functions.
Central Anticholinergic Adverse Effects
The symptoms of central adverse effect of anticholinergic drugs may be dramatic such as delirium, but are more often subtle and easily discounted as the natural consequences of ageing, such as mild alterations in memory skills. The symptoms are linked to the inhibition of acetylcholine transmission in certain brain areas, including the forebrain, cerebral cortex, hippocampus and corpus striatum. Acetylcholine transmission is involved especially in memory processes, particularly in
short-term memory and attention 20, but cholinergic blockade in the brain has been related to widespread undesired adverse effects, including delirium, behavioural disturbances, reduced executive functions, altered emotions and reduced motor functions 21.
The risk of central anticholinergic adverse effects is determined by the drugs’ distribution to the brain and their competitive binding affinities for the cerebral muscarinic receptors. The concentrations of the drugs within the brain are regulated by the balance between their passive influx and active efflux across the blood–brain barrier (BBB). Factors that influence the permeability of the blood–brain barrier (BBB) are factors that contribute to the risk assessment of adverse central effects. Certain drug characteristics, such as small molecular size, apolarity and high lipophilicity, allow their passive influx through the blood–brain barrier (BBB). In general, tertiary amines such as the natural alkaloid atropine cross the blood–brain barrier, while positively charged quaternary amines such as ipatropium bromide have little CNS penetrance. It has also been observed in mice that quaternary compounds have much weaker central anticholinergic effects than their corresponding tertiary analogoues 22. The drugs’ efflux across the blood–brain barrier is facilitated by the drugs’ specificity for the active transporter molecule permeability glycoprotein (PgP). Moreover, PgP-mediated efflux can be affected by genetic polymorphisms and/or drug-induced inhibition of the transporter protein 18. As an example, anticholinergic drugs used to treat urinary incontinence show different propensities to cause central anticholinergic effects because their different molecular characteristics differentially affect their penetration of the blood–brain barrier 23.
Anticholinergic Hypersensitivity
Normal ageing is accompanied by increased pharmacodynamic sensitivity to the blockade of the muscarinic receptors in the central nervous system. Different changes in the cholinergic nervous system can lead to reduced cholinergic reserves in the ageing brain. A structural change in the muscarinic binding sites that leads to lower binding affinity for acetylcholine has been identified in rat models 24. A reduction in the activity of the pre-synaptic enzyme choline acetyltransferase that reduces the amount of acetylcholine in the central nervous system has been described, and a lower muscarinic receptor density in the aged brain is also reported 25. Age-related pharmacokinetic changes also contribute to a further increase in an individual’s susceptibility to central adverse effects, particularly the increased permeability of the blood–brain barrier. The mechanisms involved in increased blood–brain barrier permeability include epithelial shrinkage, the opening of tight junctions and the dilation of blood vessels, resulting in increased blood flow and the leakage of larger molecules, as has been demonstrated in a rat model 18. Auxiliary leakage through the blood–brain barrier is reported in certain conditions that are common in the elderly, including neurodegenerative diseases and diabetes 18. Vulnerability to central muscarinic antagonism is further increased in patients with Alzheimer’s disease. These patients have severely impaired cholinergic neurotransmission, secondary to the degeneration of neurons, and it has been shown that older people with dementia are more sensitive to central anticholinergic adverse effects than their age-matched controls 26.
That being said, Kersten and Wyller 27 also reported that, after anticholinergic drug burden was reduced, no significant cognitive improvements have been demonstrated in randomized controlled trials, thus indicating that cognitive impairment may be prolonged well past the period of drug discontinuation and/or other factors may be involved in contributing to these deficits. Indeed, studies evaluating the use of these medications in the geriatric population have identified objective neuropsychological deficits that appear to increase with the number of medications, including general cognitive decline, increased proneness to errors, reductions in psychomotor speed, and executive dysfunction 28. These changes may be more substantial for older adults given the age-related changes in central cholinergic receptor function, blood–brain barrier integrity, and slowed medication metabolism/elimination 29. Of note, older adults who used medications with anticholinergic effects for as little as 90 days were 2.73 times more likely to have a diagnosis of mild cognitive impairment (MCI), and have an increased likelihood of amyloid and neurofibrillary neuropathology with a 2-year duration of use 30.
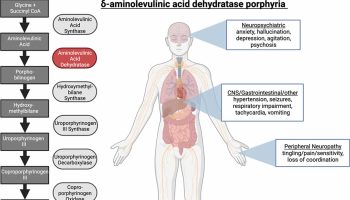
Anticholinergic syndrome
Anticholinergic syndrome is produced by the inhibition of cholinergic neurotransmission at muscarinic receptor sites. Anticholinergic syndrome may follow the ingestion of a wide variety of prescription and over-the-counter medications 31. Anticholinergic syndrome may involve peripheral receptors (e.g, in the heart, salivary glands, sweat glands, gastrointestinal tract, and genitourinary tract) with resulting tachycardia (fast heart beat), hyperthermia, dry skin and mucous membranes, mydriasis (dilated pupils), decreased bowel sounds and urinary retention. Central nervous system (CNS) receptors may also be affected with resulting hallucinations, psychoses, seizures, and coma, which generally occurs late in the course of the syndrome. The central anticholinergic syndrome occurs frequently, but is often unrecognized because many patients’ symptoms do not appear in a well defined pattern. The response to medications varies among patients, and there is temporal fluctuation in the course of an anticholinergic syndrome. 32 Anticholinergic syndrome has been reported following the ingestion of a wide variety of prescription and over-the-counter medications.
Anticholinergic syndrome signs and symptoms
Clinical manifestations are caused by CNS effects, peripheral nervous system effects, or both. Common manifestations are as follows:
- Flushing
- Dry skin and mucous membranes
- Mydriasis with loss of accommodation
- Altered mental status
- Fever
Additional manifestations include the following:
- Sinus tachycardia
- Decreased bowel sounds
- Functional ileus
- Urinary retention
- Hypertension
- Tremulousness
- Myoclonic jerking
Anticholinergic syndrome diagnosis
No specific diagnostic studies exist for anticholinergic overdoses. Laboratory studies that may be helpful include the following:
- Acetaminophen and salicylate screening – in all intentional poisonings
- Blood and urine cultures – in febrile patients
- Serum chemistry and electrolyte analysis
- Electrolyte and arterial blood gas (ABG) analysis
- Urine pregnancy test – in all women of childbearing age
Additional studies that may be useful are as follows:
- CT of the head and MRI imaging – for patients in whom altered mental status is insufficiently explained by the ingested agent or who are unresponsive to appropriate intervention
- ECG – for all patients with suspected toxic ingestions
- Lumbar puncture – for patients with fever and altered mental status in whom CNS infection is suspected as a possible etiology
Anticholinergic syndrome management
Patients presenting with anticholinergic toxicity should be transported to the nearest emergency facility with advanced life support capabilities. Avoid administering ipecac syrup.
In patients with recent (< 1 hour), clinically significant ingestions that are anticipated to result in moderate-to-severe anticholinergic toxicity, single-dose activated charcoal may be administered to minimize absorption of the ingested medication. In patients with depressed level of consciousness or impaired airway reflexes, definitive control of the airway (endotracheal intubation with a cuffed endotracheal tube) should be obtained prior to adminstration of activated charcoal via orogastric tube to minimize the risk of charcoal aspiration.
Medical therapy consists of anticonvulsants, antitachydysrhythmics, sodium bicarbonate, physostigmine, and sedatives. The standard dose of physostigmine is 0.5-2 mg, given by slow iintravenous push (not to exceed 1 mg/min). However, because higher doses of physostigmine can lead to cholinergic toxicity (e.g, seizures, cardiotoxic effects), Dawson and Buckley recommend giving a titrated dose of 0.5 to 1 mg in adults and waiting at least 10-15 min before re-dosing 33.
The antidote for anticholinergic toxicity is physostigmine salicylate. Most patients can be safely treated without it, but it is recommended when tachydysrhythmia with subsequent hemodynamic compromise, intractable seizure, severe agitation or psychosis, or some combination thereof is present. Physostigmine is contraindicated in patients with cardiac conduction disturbancese agitation or psychosis, or some combination thereof is present. Physostigmine is contraindicated in patients with cardiac conduction disturbances on ECG.
Most anticholinergic agents have large volumes of distribution and are highly protein bound. Therefore, hemodialysis and hemoperfusion are ineffective treatment methods.
Patients often recover well with supportive care. Tachycardia may be responsive to crystalloid infusions, control of agitation (eg, benzodiazepines), and control of hyperthermia (eg, fluids, antipyretics, active cooling measures). Administer a trial dose of physostigmine over 2-5 minutes for patients with narrow QRS supraventricular tachydysrhythmias resulting in hemodynamic deterioration or ischemic pain. Ventricular arrhythmias can be treated with lidocaine.
Manage seizures with benzodiazepines, preferably diazepam or lorazepam. Use phenobarbital and other barbiturates for intractable seizures. Phenytoin has no proven role for toxin-induced seizures and should not be used. Perform a repeat ECG immediately following seizure activity because acidosis can potentiate conduction aberrancies with certain agents.
Patients with hallucinations often respond to reassurance and do not require specific treatment unless they also have significant psychomotor agitation. Agitation may be treated with the specific antidote, physostigmine, or nonspecifically with benzodiazepines. Although its use is controversial, physostigmine is safe and effective for controlling agitated delirium if the ECG indicates the absence of prolonged PR and QRS intervals. Phenothiazines are contraindicated because of their anticholinergic properties. Perform bladder catheterization if the patient shows signs or symptoms of urinary retention.
The antidote for anticholinergic toxicity is physostigmine salicylate. Physostigmine is the only reversible acetylcholinesterase inhibitor capable of directly antagonizing the CNS manifestations of anticholinergic toxicity; it is an uncharged tertiary amine that efficiently crosses the blood-brain barrier.
By inhibiting acetylcholinesterase, the enzyme responsible for the hydrolysis of acetylcholine, an increased concentration of acetylcholine augments stimulation at muscarinic and nicotinic receptors. Physostigmine can reverse the central effects of coma, seizures, severe dyskinesias, hallucinations, agitation, and respiratory depression. The most common indication for physostigmine is to control agitated delirium.
The most common adverse effects from physostigmine are peripheral cholinergic manifestations (eg, vomiting, diarrhea, abdominal cramps, diaphoresis). Physostigmine also may produce seizures, a complication frequently reported when administered to individuals with tricyclic antidepressant poisoning. Rarely, physostigmine may produce bradyasystole; three cases of this complication have been reported in literature, and all occurred in patients given physostigmine for severe tricyclic antidepressant poisoning. To avoid bradyasystole, do not administer physostigmine to patients whose ECG shows a prolonged PR or QRS interval.
Most patients can be treated safely without physostigmine, but its use is recommended when at least one of the following aberrations is present:
- Tachydysrhythmias with subsequent hemodynamic compromise
- Intractable seizures
- Severe agitation or psychosis (in which the patient is considered a threat to self or others)
Although some authors recommend the use of benzodiazepines as first-line agents for the control of agitation associated with the anticholinergic syndrome, one study suggests that physostigmine is significantly more effective and no less safe for use in this setting 34.
Physostigmine is contraindicated in patients with cardiac conduction disturbances (prolonged PR and QRS intervals) on ECG.
Anticholinergic side effects
Anticholinergic side effects can be caused by a wide range of medications, including some over-the-counter medications 35. Being aware of what types of medications a patient is taking and eliminating unnecessary medications can help reduce the potential for anticholinergic side effects. Anticholinergic delirium, however, constitutes a medical emergency. Symptoms of anticholinergic delirium include hot, dry skin; dry mucous membranes; dilated pupils; absent bowel sounds; and tachycardia. Physicians must first determine and remove the offending agent because patients are at a high risk for cholinergic crisis. Atropine can be used to treat anticholinergic delirium symptoms once the anticholinergic agent has been removed.
Anticholinergic side effects can be divided into 2 types of side effects, peripheral and central. Physicians need to be attuned to the possibility of these side effects in order to effectively treat patients. The potential medical complications of the anticholinergic side effects are appreciable, and in susceptible patients, particularly older patients or patients with a preexisting condition like asthma, these side effects can be debilitating.
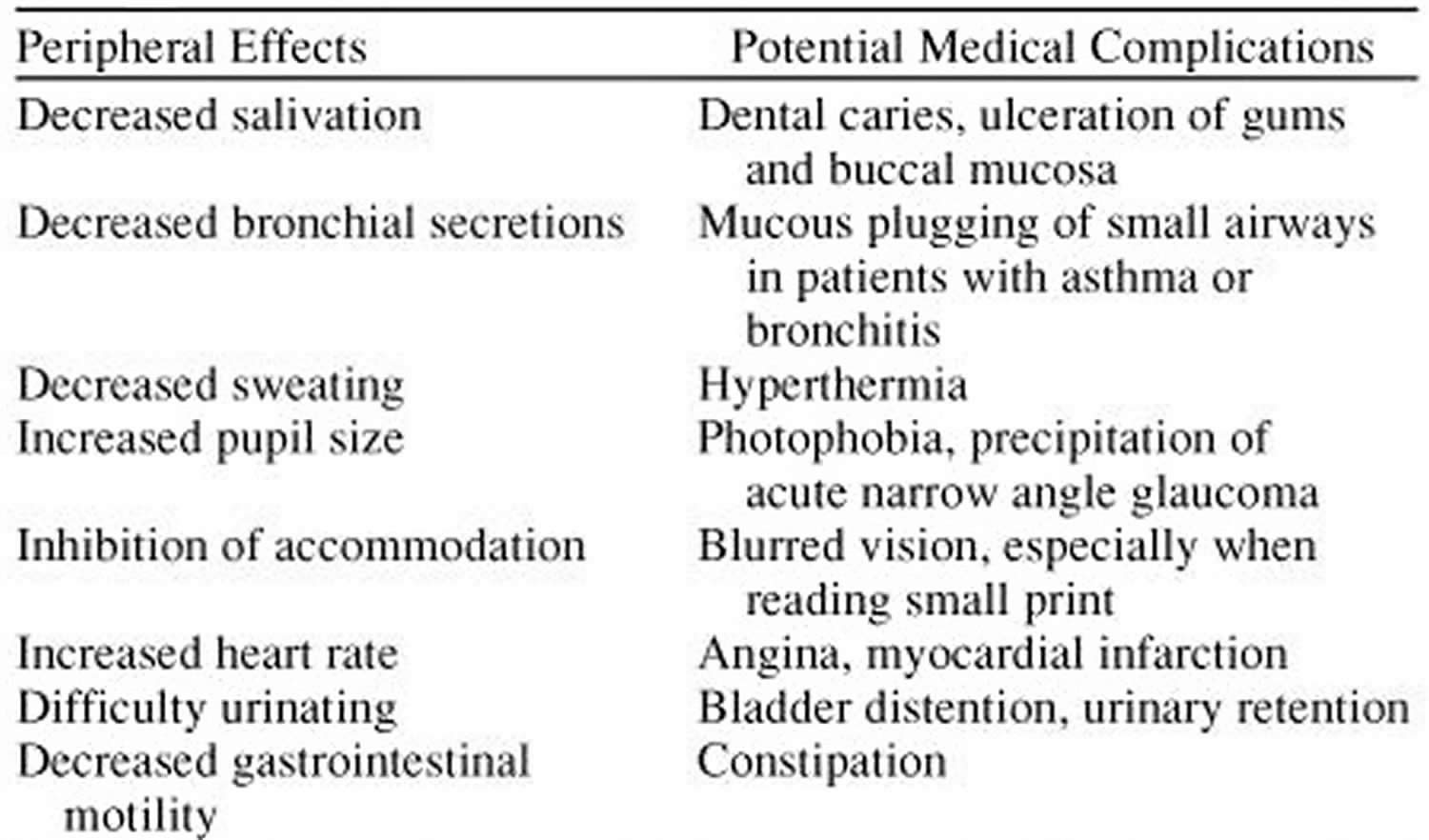
Peripheral Side Effects
Peripheral side effects are more physical than central side effects and therefore might be easier to diagnose. Typical symptoms include dry mouth, constipation, urinary retention, bowel obstruction, dilated pupils, blurred vision, increased heart rate, and decreased sweating (Table 3) 36.
While the peripheral side effects may not all appear serious, physicians should be wary because these side effects can lead to a plethora of medical complications. Complications can range from ulceration of the gums and respiratory problems to hyperthermia and heart attack (myocardial infarction) 37.
Table 3. Peripheral Anticholinergic Side Effects of Antipsychotic Agents
[Source 37]Central Side Effects
Impairment in cognitive function has long been recognized as central to the abnormalities in schizophrenia 38. This preexisting impairment can be exacerbated by the presence of central side effects caused by anticholinergic properties of antipsychotic agents. Central side effects are cerebral and include impaired concentration, confusion, attention deficit, and memory impairment.
Central anticholinergic side effects of antipsychotic agents 37:
- Impaired concentration
- Confusion
- Attention deficit
- Memory impairment
One study 39 conducted among the elderly found that delirium was associated with higher serum anticholinergic activity. Participants aged 75 years and older and without a high premorbid risk of delirium were included in the study. High premorbid risk was defined as a greater than partial dependency in all activities of daily living scale items, known terminal illness with a life expectancy of less than 6 months, or intensive care unit admission. Among 67 participants, data were collected for a broad range of factors that have been reported to have an association with delirium such as age, residence, comorbidity, functional status, number of medications used, white blood cell count, presence of infection, hematocrit, glucose level, sodium level, blood urea, nitrogen, and creatinine. Also noted was the use of medications that have been proposed as potential iatrogenic agents for delirium such as anticholinergic medications, neuroleptics, narcotics, and benzodiazepines. Delirium was diagnosed using the Confusion Assessment Method and the Delirium Symptom Interview. Delirium occurred in 30% of participants (N = 20). High serum anticholinergic activity was associated with delirium. While this study did not include atypical antipsychotics, the high presence of delirium among patients administered medication with anticholinergic properties indicates that physicians need to be attuned to the possibility of central side effects among patients prescribed atypical antipsychotics.
Since schizophrenia inherently carries with it certain mental problems, central side effects must be differentiated from the problems associated with a patient’s psychosis. This differentiation can sometimes be difficult. Physicians must thoroughly interview patients suspected to suffer from central side effects and pay close attention to their responses.
- Kersten H., Wyller T. B.. Anticholinergic drug burden in older people’s brain—How well is it measured?, Basic & Clinical Pharmacology & Toxicology , 2014, vol. 114 (pg. 151-159) https://onlinelibrary.wiley.com/doi/pdf/10.1111/bcpt.12140[↩][↩][↩]
- Forrer GR. MILLER JJ. Atropine coma: a somatic therapy in psychiatry. Am J Psychiatry 1958;115:455–8.[↩]
- Tollefson GD, Montague-Clouse J, Lancaster SP. The relationship of serum anticholinergic activity to mental status performance in an elderly nursing home population. J Neuropsychiatry Clin Neurosci 1991;3:314–9.[↩]
- Chew ML, Mulsant BH, Pollock BG, Lehman ME, Greenspan A, Mahmoud RA et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc 2008;56:1333–41.[↩]
- Tamura BK, Bell CL, Inaba M, Masaki KH. Outcomes of polypharmacy in nursing home residents. Clin Geriatr Med 2012;28:217–36.[↩]
- Giron MS, Wang HX, Bernsten C, Thorslund M, Winblad B, Fastbom J. The appropriateness of drug use in an older nondemented and demented population. J Am Geriatr Soc 2001;49:277–83.[↩]
- Johnell K, Fastbom J. Concurrent use of anticholinergic drugs and cholinesterase inhibitors: register-based study of over 700,000 elderly patients. Drugs Aging 2008;25:871–7.[↩]
- Gill SS, Mamdani M, Naglie G, Streiner DL, Bronskill SE, Kopp A et al. A prescribing cascade involving cholinesterase inhibitors and anticholinergic drugs. Arch Intern Med 2005;165:808–13.[↩]
- Wawruch M, Macugova A, Kostkova L, Luha J, Dukat A, Murin J et al. The use of medications with anticholinergic properties and risk factors for their use in hospitalised elderly patients. Pharmacoepidemiol Drug Saf 2011;21:170–6.[↩]
- Agar M, Currow D, Plummer J, Seidel R, Carnahan R, Abernethy AP. Changes in anticholinergic load from regular prescribed medications in palliative care as death approaches. Palliat Med 2009;23:257–65.[↩]
- Luukkanen MJ, Uusvaara J, Laurila JV, et al. Anticholinergic Drugs and Their Effects on Delirium and Mortality in the Elderly. Dementia and Geriatric Cognitive Disorders EXTRA. 2011;1(1):43-50. doi:10.1159/000322883. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199880/[↩]
- National Research Council (US) Panel on Anticholinesterase Chemicals; National Research Council (US) Panel on Anticholinergic Chemicals. Possible Long-Term Health Effects of Short-Term Exposure to Chemical Agents: Volume 1 Anticholinesterases and Anticholinergics. Washington (DC): National Academies Press (US); 1982. 3, ANTICHOLINERGICS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK217767[↩]
- Crowell, E.B., Jr., and Ketchum J.S. 1967: The treatment of scopolamine-induced delirium with physostigmine. Edgewood Arsenal Tech. Rept. 4115.[↩]
- Brimblecombe, R.W. 1974: Drug Actions on Cholinergic Systems. University Park Press, Baltimore[↩]
- Weiner, N. Neurotransmitter systems in the central nervous system. In Drugs and the Developing Brain. (Vernadakis, A., editor; , and Weiner, N., editor. , eds.) Plenum Press, New York, 1974, pp.105–131.[↩]
- Volpicelli LA, Levey AI. Muscarinic acetylcholine receptor subtypes in cerebral cortex and hippocampus. Prog Brain Res 2004;145:59–66.[↩]
- Nilvebrant L. On the muscarinic receptors in the urinary bladder and the putative subclassification of muscarinic receptors. Acta Pharmacol Toxicol (Copenh) 1986;59(Suppl 1):1–45.[↩]
- Abrams P, Andersson KE, Buccafusco JJ, Chapple C, de Groat WC, Fryer AD et al. Muscarinic receptors: their distribution and function in body systems, and the implications for treating overactive bladder. Br J Pharmacol 2006;148:565–78.[↩][↩][↩][↩][↩][↩][↩]
- Scarr E. Muscarinic receptors: their roles in disorders of the central nervous system and potential as therapeutic targets. CNS Neurosci Ther 2012;18:369–79.[↩]
- Aleman A. Effects of anticholinergic drug withdrawal on memory, regional cerebral blood flow and extrapyramidal side effects in schizophrenic patients by K Mori et al.. Pharmacopsychiatry 2003;36:43–4.[↩]
- Cancelli I, Beltrame M, Gigli GL, Valente M. Drugs with anticholinergic properties: cognitive and neuropsychiatric side-effects in elderly patients. Neurol Sci 2009;30:87–92.[↩]
- Scheel-Kruger J. Central effects of anticholinergic drugs measured by the apomorphine gnawing test in mice. Acta Pharmacol Toxicol (Copenh) 1970;28:1–16.[↩]
- Jakobsen SM, Kersten H, Molden E. Evaluation of brain anticholinergic activities of urinary spasmolytic drugs using a high-throughput radio receptor bioassay. J Am Geriatr Soc 2011;59:501–5.[↩]
- Smith DO, Chapman MR. Acetylcholine receptor binding properties at the rat neuromuscular junction during aging. J Neurochem 1987;48:1834–41.[↩]
- Ray PG, Meador KJ, Loring DW, Zamrini EW, Yang XH, Buccafusco JJ. Central anticholinergic hypersensitivity in aging. J Geriatr Psychiatry Neurol 1992;5:72–7.[↩]
- Sunderland T, Tariot PN, Cohen RM, Weingartner H, Mueller EA III, Murphy DL et al. Anticholinergic sensitivity in patients with dementia of the Alzheimer type and age-matched controls. A doseresponse study. Arch Gen Psychiatry 1987;44:418–26.[↩]
- Kersten H., Wyller T. B.. Anticholinergic drug burden in older people’s brain—How well is it measured?, Basic & Clinical Pharmacology & Toxicology , 2014, vol. 114, pg. 151-159[↩]
- Pasina L., Djade C. D., Lucca U., Nobili A., Tettamanti M., Franchi C., et al. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: Comparison of the Anticholinergic Burden Scale and Anticholinergic Risk Scale, Drugs and Aging , 2013, vol. 30, pg. 103-112[↩]
- Koyoma A., Steinman M., Ensrud K., Hillier T. A., Yaffe K.. Long-term cognitive and functional effects of potentially inappropriate medications in older women, The Journals of Gerontology Series A: Biological Sciences & Medical Sciences , 2014, vol. 69, pg. 423-9[↩]
- Cai X., Campbell N., Khan B., Callahan C., Boustani M.. Long-term anticholinergic use and the aging brain, Alzheimer‘s & Dementia , 2013, vol. 9, pg. 377-385[↩]
- Magin PJ, Morgan S, Tapley A, McCowan C, Parkinson L, Henderson KM, et al. Anticholinergic medicines in an older primary care population: a cross-sectional analysis of medicines’ levels of anticholinergic activity and clinical indications. J Clin Pharm Ther. 2016 Jun 27. 59 (5):582-90.[↩]
- Anticholinergic psychosis: differential diagnosis and management. Hall RC, Feinsilver DL, Holt RE. Psychosomatics. 1981 Jul; 22(7):581-3, 587.[↩]
- Dawson AH, Buckley NA. Pharmacological management of anticholinergic delirium – theory, evidence and practice. Br J Clin Pharmacol. 2016 Mar. 81 (3):516-24.[↩]
- Burns MJ, Linden CH, Graudins A, et al. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning. Ann Emerg Med. 2000 Apr. 35(4):374-81.[↩]
- Mintzer J, Burns A. Anticholinergic side-effects of drugs in elderly people. J R Soc Med. 2000;93:457–462[↩]
- The clinical use of anticholinergic drugs as treatment for extrapyramidal side effects of neuroleptic drugs. McEvoy JP. J Clin Psychopharmacol. 1983 Oct; 3(5):288-302.[↩]
- Lieberman JA. Managing Anticholinergic Side Effects. Primary Care Companion to The Journal of Clinical Psychiatry. 2004;6(suppl 2):20-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC487008/[↩][↩][↩]
- Cognitive effects and antipsychotic treatment. Kasper S, Resinger E. Psychoneuroendocrinology. 2003 Jan; 28 Suppl 1():27-38.[↩]
- The association of serum anticholinergic activity with delirium in elderly medical patients. Flacker JM, Cummings V, Mach JR Jr, Bettin K, Kiely DK, Wei J. Am J Geriatr Psychiatry. 1998 Winter; 6(1):31-41.[↩]